A New Strategy to Identify Naturally Presenting SLA-I Bound Peptides Derived from the O Serotype of Foot-and-Mouth Disease Virus, by Mild Acid Elution in a VP1 Stably Expressed PK15 Cell Line
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Plasmids, Reagents, Cell Lines, and Primers
2.2. Cell Culture
2.3. G418 Lethal Concentration Curve Measurement
2.4. PK15 Cell Transfection Efficiency Assay
2.5. PK15 Cell Transfection and G418 Screening
2.6. Identification of the Stable Expression of the VP1 Gene in pEGFP-N1-VP1/PK15 Cells
2.7. Detection of the Peptides Eluted with Mild Weak Acids from the Surface of pEGFP-N1-VP1/PK15 Cells by LC–MS/MS
2.8. Detection of the Eluted Peptides Associated to SLA Class I-Presenting
2.9. Statistical Analysis
3. Results
3.1. G418 Lethal Concentration Curve
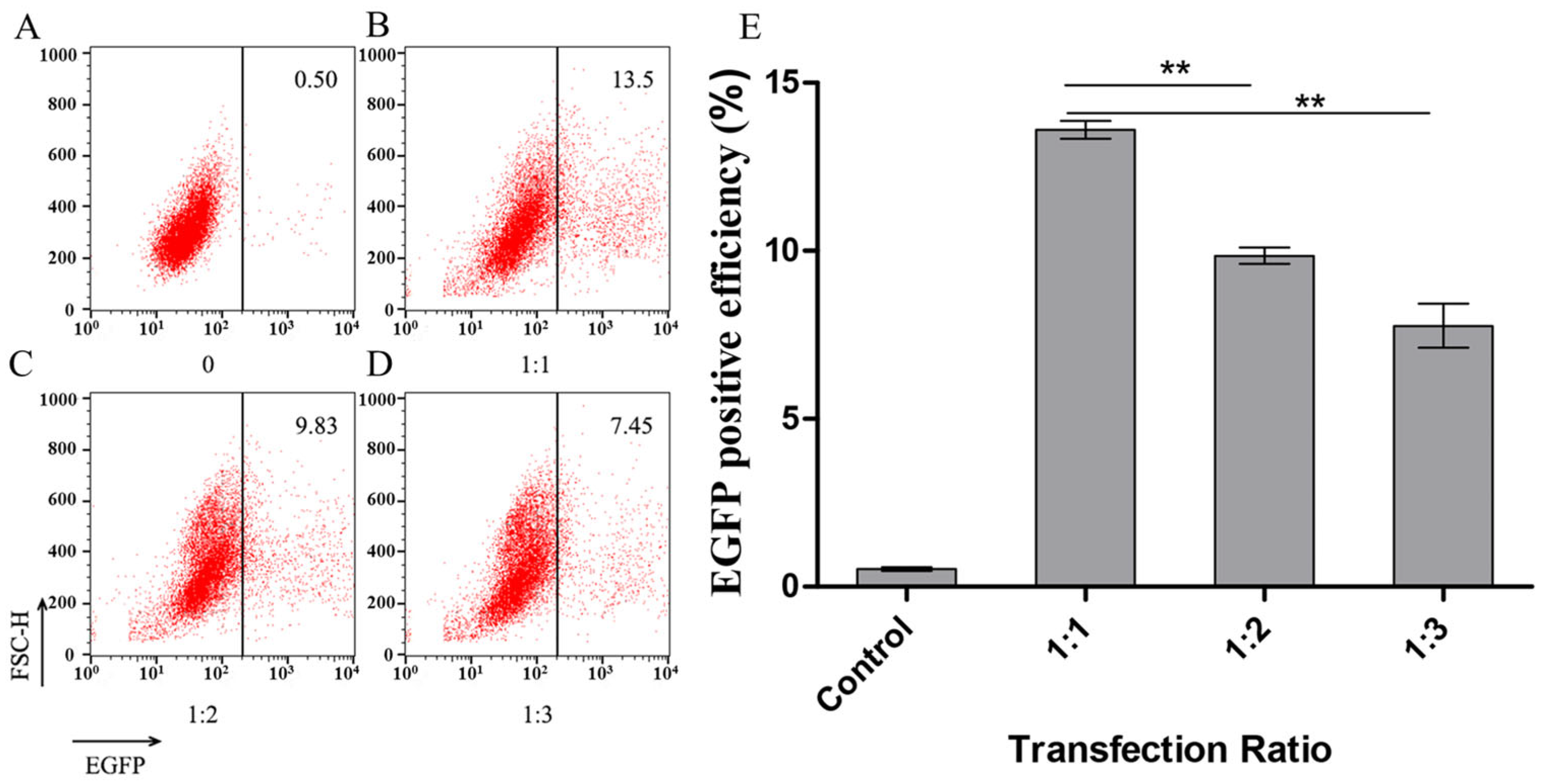
3.2. Detection of the Transfection Efficiency of PK15 Cells by Flow Cytometry for Different Liposome Complex Ratios
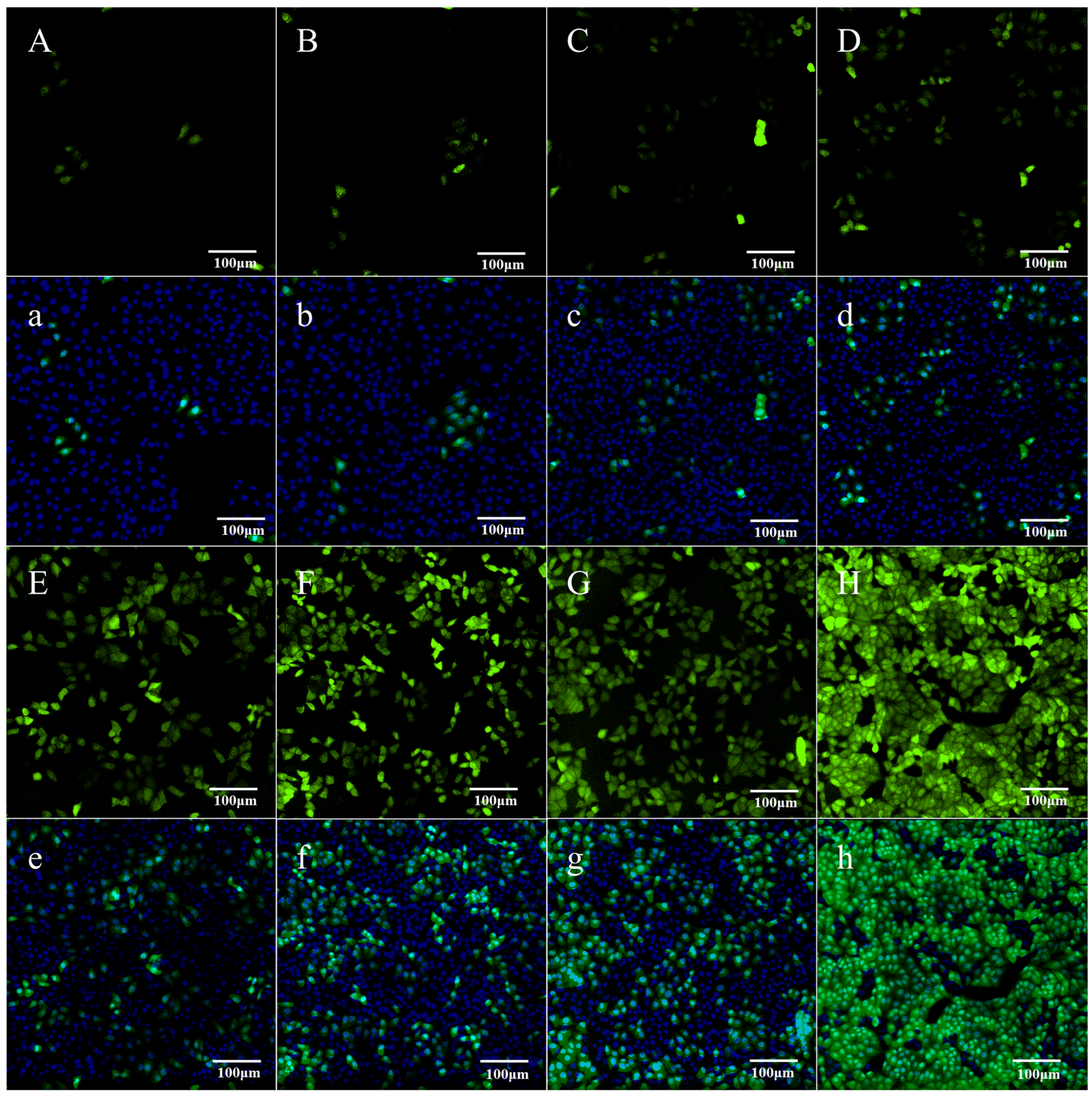
3.3. Detection of the VP1-Fused Green Fluorescent Protein Expression in Stably Transfected Cells
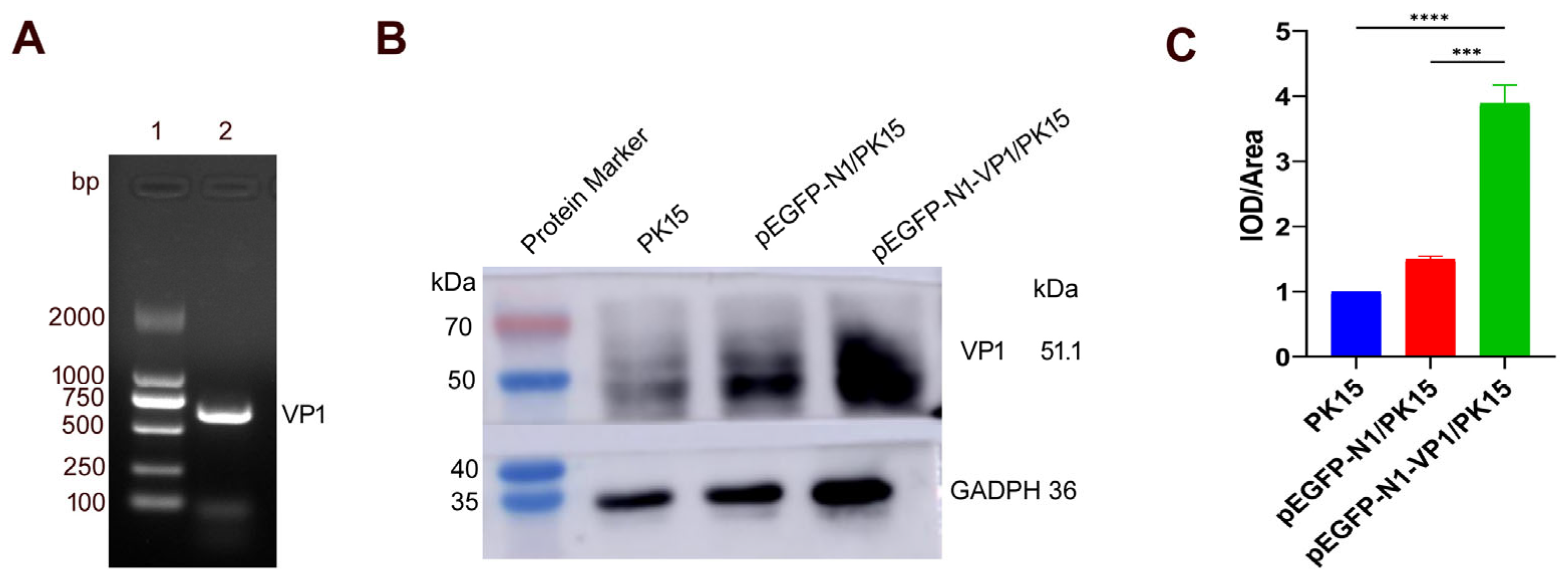
3.4. Detection of the Expression of the VP1 Gene in pEGFP-N1-VP1/PK15 Cells
3.5. Detection of the Peptides Eluted with Mild Weak Acids by LC–MS/MS
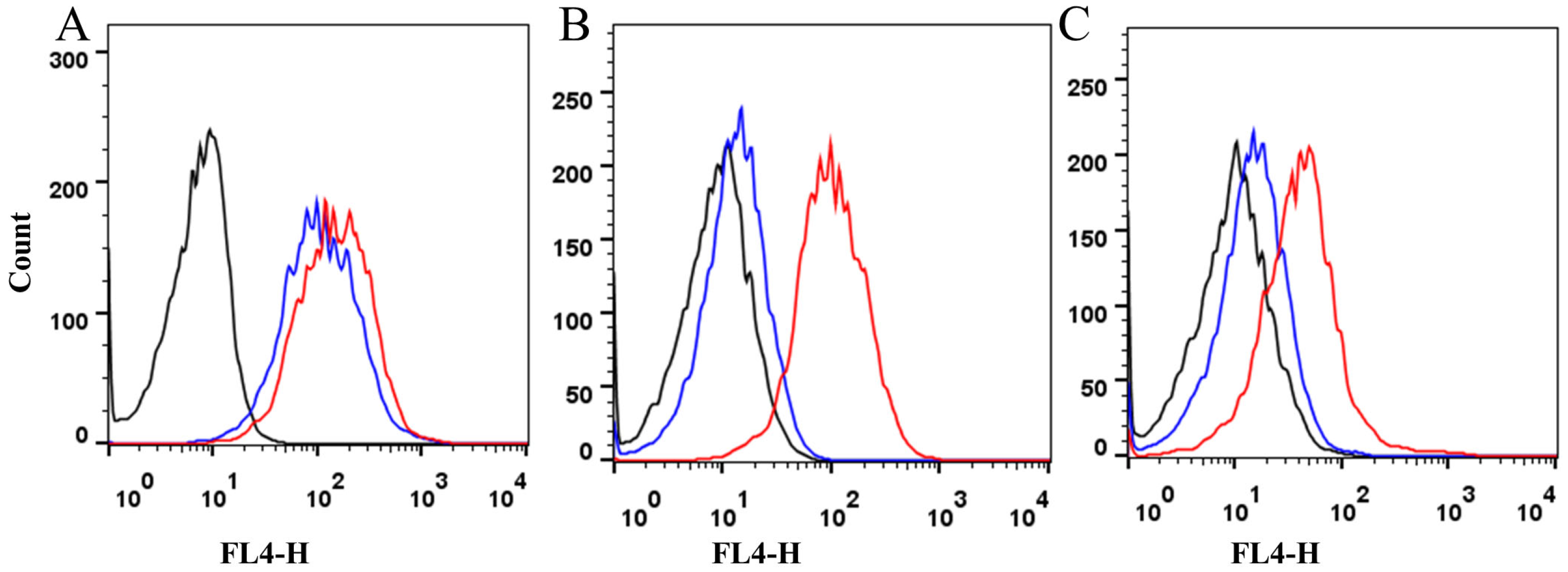
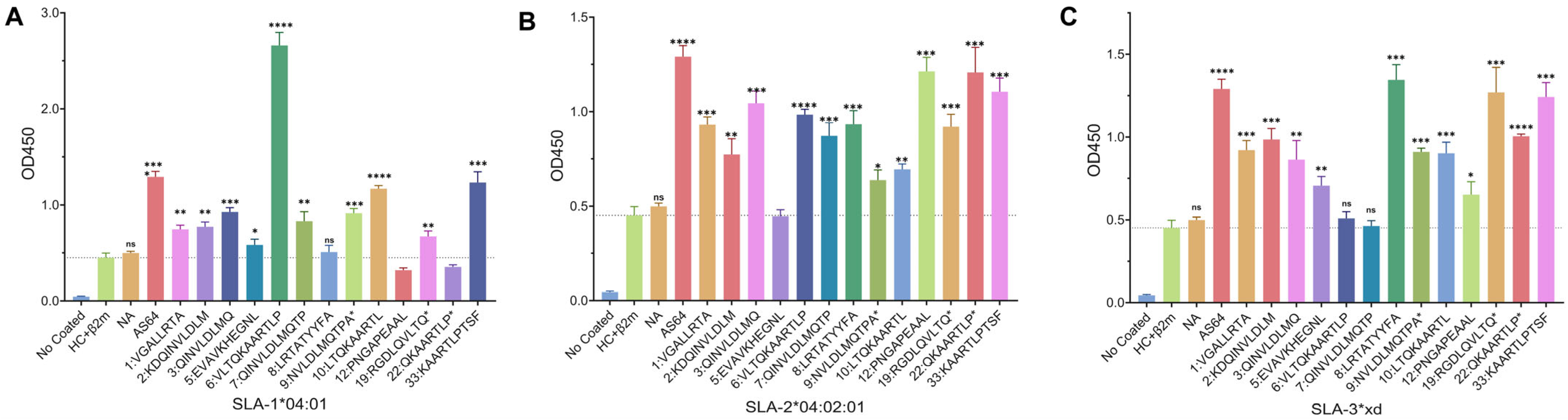
3.6. Detection of the Eluted Peptides Associated with SLA-I Binding and Presenting
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stenfeldt, C.; Eschbaumer, M.; Humphreys, J.; Medina, G.N.; Arzt, J. The pathogenesis of foot-and-mouth disease virus: Current understandings and knowledge gaps. Vet. Res. 2025, 56, 119. [Google Scholar] [CrossRef]
- Saraiva, V. Foot-and-mouth disease in the Americas: Epidemiology and ecologic changes affecting distribution. Ann. N. Y. Acad. Sci. 2004, 1026, 73–78. [Google Scholar] [CrossRef]
- Dehoux, J.P.; Hounsou-Ve, G. Outbreak of foot-and-mouth disease in Northern Benin during the 1990–1991 dry season. Rev. Elev. Med. Vet. Pays Trop. 1991, 44, 261–262. [Google Scholar] [CrossRef]
- Paton, D.J.; King, D.P.; Knowles, N.J.; Hammond, J. Recent spread of foot-and-mouth disease in the Far East. Vet. Rec. 2010, 166, 569–570. [Google Scholar] [CrossRef]
- Dahiya, S.S.; Subramaniam, S.; Rautaray, S.S.; Rout, M.; Mohapatra, J.K.; Singh, R.P. A foot-and-mouth disease virus serotype O field strain from an outbreak in India has a three-codon deletion in the 3A coding region. Arch. Virol. 2025, 170, 112. [Google Scholar] [CrossRef]
- Dinana, Z.; Suwarno, S.; Mustofa, I.; Rahmahani, J.; Kusnoto, K.; Maharani, A.T.; Fitria, A.L.; Witaningrum, A.M.; Maulana, F.K.; Said, N.S.; et al. Molecular characterization of VP1 gene during the foot and mouth disease virus outbreak in East Java, Indonesia, in 2022. Vet. World 2024, 17, 2469–2476. [Google Scholar] [CrossRef] [PubMed]
- Tesfaye, Y.; Khan, F.; Gelaye, E. Molecular characterization of foot-and-mouth disease viruses collected from Northern and Central Ethiopia during the 2018 outbreak. Vet. World 2020, 13, 542–548. [Google Scholar] [CrossRef] [PubMed]
- WOAH. Event 6177 Germany-Foot and Mouth Disease Virus (Inf. with). Available online: https://wahis.woah.org/#/in-event/6177/dashboard (accessed on 16 May 2025).
- WOAH. Event 6317 Hungary-Foot and Mouth Disease Virus (Inf. with). Available online: https://wahis.woah.org/#/in-event/6317/dashboard (accessed on 16 May 2025).
- WOAH. Event 6359 Slovakia-Foot and Mouth Disease Virus (Inf. with). Available online: https://wahis.woah.org/#/in-event/6359/dashboard (accessed on 16 May 2025).
- Tully, D.C.; Fares, M.A. Unravelling selection shifts among foot-and-mouth disease virus (FMDV) serotypes. Evol. Bioinform. Online 2007, 2, 211–225. [Google Scholar] [CrossRef]
- Seeyo, K.B.; Nishi, T.; Kawaguchi, R.; Ungvanijban, S.; Udon, R.; Fukai, K.; Yamakawa, M.; Rukkwamsuk, T. Evolution of antigenic and genetic characteristics of foot-and-mouth disease virus serotype A circulating in Thailand, 2007-2019. Virus Res. 2020, 290, 198166. [Google Scholar] [CrossRef]
- Mason, P.W.; Grubman, M.J.; Baxt, B. Molecular basis of pathogenesis of FMDV. Virus Res. 2003, 91, 9–32. [Google Scholar] [CrossRef] [PubMed]
- Tosh, C.; Hemadri, D.; Sanyal, A. Evidence of recombination in the capsid-coding region of type A foot-and-mouth disease virus. J. Gen. Virol. 2002, 83, 2455–2460. [Google Scholar] [CrossRef]
- Parry, N.; Fox, G.; Rowlands, D.; Brown, F.; Fry, E.; Acharya, R.; Logan, D.; Stuart, D. Structural and serological evidence for a novel mechanism of antigenic variation in foot-and-mouth disease virus. Nature 1990, 347, 569–572. [Google Scholar] [CrossRef]
- Dus Santos, M.J.; Wigdorovitz, A.; Trono, K.; Rios, R.D.; Franzone, P.M.; Gil, F.; Moreno, J.; Carrillo, C.; Escribano, J.M.; Borca, M.V. A novel methodology to develop a foot and mouth disease virus (FMDV) peptide-based vaccine in transgenic plants. Vaccine 2002, 20, 1141–1147. [Google Scholar] [CrossRef]
- Nanda, R.K.; Hajam, I.A.; Edao, B.M.; Ramya, K.; Rajangam, M.; Chandra Sekar, S.; Ganesh, K.; Bhanuprakash, V.; Kishore, S. Immunological evaluation of mannosylated chitosan nanoparticles based foot and mouth disease virus DNA vaccine, pVAC FMDV VP1-OmpA in guinea pigs. Biologicals 2014, 42, 153–159. [Google Scholar] [CrossRef]
- Song, B.M.; Lee, G.H.; Kang, S.M.; Tark, D. Evaluation of vaccine efficacy with 2B/T epitope conjugated porcine IgG-Fc recombinants against foot-and-mouth disease virus. J. Vet. Med. Sci. 2024, 86, 999–1007. [Google Scholar] [CrossRef] [PubMed]
- Diaz-San Segundo, F.; Medina, G.N.; Stenfeldt, C.; Arzt, J.; de Los Santos, T. Foot-and-mouth disease vaccines. Vet. Microbiol. 2017, 206, 102–112. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.C.; Lee, I.K.; Kong, H.S.; Shin, S.H.; Hwang, S.Y.; Ahn, Y.J.; Park, J.H.; Kim, B.Y.; Song, Y.C. Foot-and-Mouth Disease Virus-like Particles Produced in E. coli as Potential Antigens for a Novel Vaccine. Vet. Sci. 2025, 12, 539. [Google Scholar] [CrossRef] [PubMed]
- Zheng, M.; Jin, N.; Zhang, H.; Jin, M.; Lu, H.; Ma, M.; Li, C.; Yin, G.; Wang, R.; Liu, Q. Construction and immunogenicity of a recombinant fowlpox virus containing the capsid and 3C protease coding regions of foot-and-mouth disease virus. J. Virol. Methods 2006, 136, 230–237. [Google Scholar] [CrossRef]
- Li, J.; Zhong, Y.; Li, H.; Zhang, N.; Ma, W.; Cheng, G.; Liu, F.; Liu, F.; Xu, J. Enhancement of Astragalus polysaccharide on the immune responses in pigs inoculated with foot-and-mouth disease virus vaccine. Int. J. Biol. Macromol. 2011, 49, 362–368. [Google Scholar] [CrossRef]
- Shao, J.; Liu, W.; Gao, S.; Chang, H.; Guo, H. A recombinant multi-epitope trivalent vaccine for foot-and-mouth disease virus serotype O in pigs. Virology 2024, 596, 110103. [Google Scholar] [CrossRef]
- Bhutta, M.S.; Awais, M.; Sadaqat, S.; Zanchi, F.B.; Shahid, N.; Qayyum Rao, A. A novel immunoinformatics approach for developing a poly-epitope vaccine targeting foot and mouth disease virus, exploiting structural VP proteins. J. Biomol. Struct. Dyn. 2025, 43, 6171–6187. [Google Scholar] [CrossRef]
- de Leon, P.; Canas-Arranz, R.; Defaus, S.; Torres, E.; Forner, M.; Bustos, M.J.; Revilla, C.; Dominguez, J.; Andreu, D.; Blanco, E.; et al. Swine T-Cells and Specific Antibodies Evoked by Peptide Dendrimers Displaying Different FMDV T-Cell Epitopes. Front. Immunol. 2020, 11, 621537. [Google Scholar] [CrossRef]
- Francis, M.J.; Hastings, G.Z.; Syred, A.D.; McGinn, B.; Brown, F.; Rowlands, D.J. Non-responsiveness to a foot-and-mouth disease virus peptide overcome by addition of foreign helper T-cell determinants. Nature 1987, 330, 168–170. [Google Scholar] [CrossRef]
- Feng, L.; Sun, M.W.; Jiang, P.; Li, Z.B.; Gao, H.; Zhai, X.X.; Han, Y.; Zhang, Z.H.; Gao, F.S. Purification, crystallization and preliminary X-ray crystallographic studies of swine MHC class I complexed with an FMDV CTL epitope Hu64. Res. Vet. Sci. 2018, 119, 205–208. [Google Scholar] [CrossRef]
- Guzman, E.; Taylor, G.; Charleston, B.; Ellis, S.A. Induction of a cross-reactive CD8(+) T cell response following foot-and-mouth disease virus vaccination. J. Virol. 2010, 84, 12375–12384. [Google Scholar] [CrossRef] [PubMed]
- Feng, L.; Gao, Y.Y.; Sun, M.; Li, Z.B.; Zhang, Q.; Yang, J.; Qiao, C.; Jin, H.; Feng, H.S.; Xian, Y.H.; et al. The Parallel Presentation of Two Functional CTL Epitopes Derived from the O and Asia 1 Serotypes of Foot-and-Mouth Disease Virus and Swine SLA-2*HB01: Implications for Universal Vaccine Development. Cells 2022, 11, 4017. [Google Scholar] [CrossRef] [PubMed]
- Gao, F.S.; Feng, L.; Zhang, Q.; Yan, R.Q.; Li, Y.G.; Li, X.S. Immunogenicity of two FMDV nonameric peptides encapsulated in liposomes in mice and the protective efficacy in guinea pigs. PLoS ONE 2013, 8, e68658. [Google Scholar] [CrossRef]
- Gao, F.S.; Zhai, X.X.; Jiang, P.; Zhang, Q.; Gao, H.; Li, Z.B.; Han, Y.; Yang, J.; Zhang, Z.H. Identification of two novel foot-and-mouth disease virus cytotoxic T lymphocyte epitopes that can bind six SLA-I proteins. Gene 2018, 653, 91–101. [Google Scholar] [CrossRef]
- Gao, F.S.; Fang, Q.M.; Li, Y.G.; Li, X.S.; Hao, H.F.; Xia, C. Reconstruction of a swine SLA-I protein complex and determination of binding nonameric peptides derived from the foot-and-mouth disease virus. Vet. Immunol. Immunopathol. 2006, 113, 328–338. [Google Scholar] [CrossRef]
- Gao, F.S.; Feng, L.; Jiang, P.; Li, Z.B.; Gao, H.; Zhai, X.X.; Zhang, Z.H.; Hu, X. Expression, purification, crystallization and preliminary X-ray diffraction analysis of swine leukocyte antigen 2 complexed with a CTL epitope AS64 derived from Asia1 serotype of foot-and-mouth disease virus. BMC Vet. Res. 2018, 14, 407. [Google Scholar] [CrossRef] [PubMed]
- Delluc, S.; Tourneur, L.; Fradelizi, D.; Rubio, M.T.; Marchiol-Fournigault, C.; Chiocchia, G.; Buzyn, A. DC-based vaccine loaded with acid-eluted peptides in acute myeloid leukemia: The importance of choosing the best elution method. Cancer Immunol. Immunother. 2007, 56, 1–12. [Google Scholar] [CrossRef]
- Zitvogel, L.; Mayordomo, J.I.; Tjandrawan, T.; DeLeo, A.B.; Clarke, M.R.; Lotze, M.T.; Storkus, W.J. Therapy of murine tumors with tumor peptide-pulsed dendritic cells: Dependence on T cells, B7 costimulation, and T helper cell 1-associated cytokines. J. Exp. Med. 1996, 183, 87–97. [Google Scholar] [CrossRef]
- Storkus, W.J.; Zeh, H.J., 3rd; Salter, R.D.; Lotze, M.T. Identification of T-cell epitopes: Rapid isolation of class I-presented peptides from viable cells by mild acid elution. J. Immunother. Emphas. Tumor Immunol. 1993, 14, 94–103. [Google Scholar] [CrossRef]
- Li, X.; Wang, J.; Liu, J.; Li, Z.; Wang, Y.; Xue, Y.; Li, X.; Cao, H.; Zheng, S.J. Engagement of soluble resistance-related calcium binding protein (sorcin) with foot-and-mouth disease virus (FMDV) VP1 inhibits type I interferon response in cells. Vet. Microbiol. 2013, 166, 35–46. [Google Scholar] [CrossRef] [PubMed]
- Furusawa, Y.; Yamanouchi, Y.; Iizumi, T.; Zhao, Q.L.; Mitsuhashi, Y.; Morita, A.; Enomoto, A.; Tabuchi, Y.; Kondo, T. Checkpoint kinase 2 is dispensable for regulation of the p53 response but is required for G2/M arrest and cell survival in cells with p53 defects under heat stress. Apoptosis 2017, 22, 1225–1234. [Google Scholar] [CrossRef]
- Gao, F.S.; Bai, J.; Gong, X.J.; Zhang, X.H.; Zhang, W.J.; Guo, D.; Zhang, S. Analyzing the genetic characteristics and function of the swine leukocyte antigen 2 gene in a Chinese inbreed of pigs. Microbiol. Immunol. 2012, 56, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Walker, J.M. The bicinchoninic acid (BCA) assay for protein quantitation. Methods Mol. Biol. 1994, 32, 5–8. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Yu, Y.; Qi, Y.; Wang, F.; Yan, J.; Zou, H. Peptide profiling and the bioactivity character of yogurt in the simulated gastrointestinal digestion. J. Proteom. 2016, 141, 24–46. [Google Scholar] [CrossRef]
- Santin, A.D.; Bellone, S.; Ravaggi, A.; Pecorelli, S.; Cannon, M.J.; Parham, G.P. Induction of ovarian tumor-specific CD8+ cytotoxic T lymphocytes by acid-eluted peptide-pulsed autologous dendritic cells. Obs. Obstet. Gynecol. 2000, 96, 422–430. [Google Scholar]
- Sylvester-Hvid, C.; Kristensen, N.; Blicher, T.; Ferre, H.; Lauemoller, S.L.; Wolf, X.A.; Lamberth, K.; Nissen, M.H.; Pedersen, L.O.; Buus, S. Establishment of a quantitative ELISA capable of determining peptide—MHC class I interaction. Tissue Antigens 2002, 59, 251–258. [Google Scholar] [CrossRef]
- Walters, L.C.; Harlos, K.; Brackenridge, S.; Rozbesky, D.; Barrett, J.R.; Jain, V.; Walter, T.S.; O'Callaghan, C.A.; Borrow, P.; Toebes, M.; et al. Pathogen-derived HLA-E bound epitopes reveal broad primary anchor pocket tolerability and conformationally malleable peptide binding. Nat. Commun. 2018, 9, 3137. [Google Scholar] [CrossRef]
- Hopkins, L.M.; Schall, M.; Leykam, J.F.; Gerlach, J.A. Characterization of major histocompatibility complex-associated peptides from a small volume of whole blood. Anal. Biochem. 2004, 328, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Qi, J.; Feng, S.; Gao, F.; Liu, J.; Pan, X.; Chen, R.; Li, Q.; Chen, Z.; Li, X.; et al. Crystal structure of swine major histocompatibility complex class I SLA-1 0401 and identification of 2009 pandemic swine-origin influenza A H1N1 virus cytotoxic T lymphocyte epitope peptides. J. Virol. 2011, 85, 11709–11724. [Google Scholar] [CrossRef]
- Hu, B.; Li, C.; Lu, H.; Zhu, Z.; Du, S.; Ye, M.; Tan, L.; Ren, D.; Han, J.; Kan, S.; et al. Immune responses to the oral administration of recombinant Bacillus subtilis expressing multi-epitopes of foot-and-mouth disease virus and a cholera toxin B subunit. J. Virol. Methods 2011, 171, 272–279. [Google Scholar] [CrossRef]
- Li, Q.; Wubshet, A.K.; Wang, Y.; Heath, L.; Zhang, J. B and T Cell Epitopes of the Incursionary Foot-and-Mouth Disease Virus Serotype SAT2 for Vaccine Development. Viruses 2023, 15, 797. [Google Scholar] [CrossRef] [PubMed]
- Patch, J.R.; Pedersen, L.E.; Toka, F.N.; Moraes, M.; Grubman, M.J.; Nielsen, M.; Jungersen, G.; Buus, S.; Golde, W.T. Induction of foot-and-mouth disease virus-specific cytotoxic T cell killing by vaccination. Clin. Vaccine Immunol. 2011, 18, 280–288. [Google Scholar] [CrossRef]
- Krensky, A.M. The HLA system, antigen processing and presentation. Kidney Int. Suppl. 1997, 58, S2–S7. [Google Scholar] [PubMed]
- Brodsky, F.M.; Guagliardi, L.E. The cell biology of antigen processing and presentation. Annu. Rev. Immunol. 1991, 9, 707–744. [Google Scholar] [CrossRef]
- Billetta, R.; Filaci, G.; Zanetti, M. Major histocompatibility complex class I-restricted presentation of influenza virus nucleoprotein peptide by B lymphoma cells harboring an antibody gene antigenized with the virus peptide. Eur. J. Immunol. 1995, 25, 776–783. [Google Scholar] [CrossRef]
- Nakagawa, Y.; Shimizu, M.; Norose, Y.; Takahashi, M.; Takahashi, H. Induction of rapid apoptosis for class I MHC molecule-restricted CD8(+) HIV-1 gp160-specific murine activated CTLs by free antigenic peptide in vivo. Int. Immunol. 2013, 25, 11–24. [Google Scholar] [CrossRef][Green Version]
- Wolk, B.; Trautwein, C.; Buchele, B.; Kersting, N.; Blum, H.E.; Rammensee, H.G.; Cerny, A.; Stevanovic, S.; Moradpour, D.; Brass, V. Identification of naturally processed hepatitis C virus-derived major histocompatibility complex class I ligands. PLoS ONE 2012, 7, e29286. [Google Scholar] [CrossRef] [PubMed]
- Calhoun, R.F., 2nd; Naziruddin, B.; Enriquez-Rincon, F.; Duffy, B.F.; Ritter, J.M.; Sundaresan, S.; Patterson, G.A.; Cooper, J.D.; Mohanakumar, T. Evidence for cytotoxic T lymphocyte response against human lung cancer: Reconstitution of antigenic epitope with peptide eluted from lung adenocarcinoma MHC class I. Surgery 2000, 128, 76–85. [Google Scholar] [CrossRef] [PubMed]
- Chromik, J.; Schnurer, E.; Georg Meyer, R.; Wehler, T.; Tuting, T.; Wolfel, T.; Huber, C.; Herr, W. Proteasome-inhibited dendritic cells demonstrate improved presentation of exogenous synthetic and natural HLA-class I peptide epitopes. J. Immunol. Methods 2006, 308, 77–89. [Google Scholar] [CrossRef]
- Murphy, J.P.; Yu, Q.; Konda, P.; Paulo, J.A.; Jedrychowski, M.P.; Kowalewski, D.J.; Schuster, H.; Kim, Y.; Clements, D.; Jain, A.; et al. Multiplexed Relative Quantitation with Isobaric Tagging Mass Spectrometry Reveals Class I Major Histocompatibility Complex Ligand Dynamics in Response to Doxorubicin. Anal. Chem. 2019, 91, 5106–5115. [Google Scholar] [CrossRef]
- Ando, A.; Kawata, H.; Shigenari, A.; Anzai, T.; Ota, M.; Katsuyama, Y.; Sada, M.; Goto, R.; Takeshima, S.N.; Aida, Y.; et al. Genetic polymorphism of the swine major histocompatibility complex (SLA) class I genes, SLA-1, -2 and -3. Immunogenetics 2003, 55, 583–593. [Google Scholar] [CrossRef] [PubMed]

| No. | Amino Acid Sequence | Observed Mass (Da) | m/z | Charge | Sequence Length | XCorr Sequest High Throughput a |
|---|---|---|---|---|---|---|
| 1 | VGALLRTA | 800.4989 | 400.7527 | 2 | 8 | 1.6470474 |
| 2 | TDVSFILDR * | 1205.608 | 402.5445 | 3 | 10 | 1.264194489 |
| 3 | QINVLDLMQ | 1073.566 | 537.2855 | 2 | 9 | 1.230585575 |
| 4 | QINVLDLMQ * | 1074.55 | 537.7767 | 2 | 9 | 1.215035796 |
| 5 | EVAVKHEGNL * | 1096.563 | 548.7848 | 2 | 10 | 1.133248448 |
| 6 | VLTQKAARTLP | 1197.731 | 399.9142 | 3 | 11 | 1.12214005 |
| 7 | QINVLDLMQTP *b | 1289.629 | 645.3178 | 2 | 11 | 1.096101761 |
| 8 | LRTATYYFA | 1105.568 | 553.2893 | 2 | 9 | 1.094873786 |
| 9 | NVLDLMQTPA * | 1103.529 | 552.2638 | 2 | 10 | 1.065254211 |
| 10 | LTQKAARTL * | 1002.594 | 501.8008 | 2 | 9 | 1.051743507 |
| 11 | QINVLDLMQTP *b | 1273.634 | 637.3219 | 2 | 11 | 1.041987658 |
| 12 | PNGAPEAAL | 839.4258 | 420.2158 | 2 | 9 | 1.041754007 |
| 13 | KVTPKDQIN * | 1043.573 | 522.2921 | 2 | 9 | 0.987775028 |
| 14 | VAVKHEGNLT * | 1068.568 | 534.7877 | 2 | 10 | 0.986433804 |
| 15 | INVLDLMQTP | 1143.608 | 572.3118 | 2 | 10 | 0.978185475 |
| 16 | KDQINVLDLM * | 1206.592 | 603.796 | 2 | 10 | 0.948512673 |
| 17 | QINVLDLMQT * | 1176.582 | 588.7997 | 2 | 10 | 0.942279458 |
| 18 | VTNPRGDL * | 872.4472 | 436.7239 | 2 | 8 | 0.904682457 |
| 19 | RGDLQVLTQ * | 1030.553 | 515.7751 | 2 | 9 | 0.901747465 |
| 20 | PNGAPEAAL * | 840.4098 | 420.7085 | 2 | 9 | 0.896400273 |
| 21 | LTWVPNGAPE | 1083.547 | 420.7085 | 2 | 10 | 0.881147504 |
| 22 | QKAARTLP * | 885.5152 | 443.2597 | 2 | 8 | 0.85133779 |
| 23 | NLTWVPNGA | 971.4945 | 486.2554 | 2 | 9 | 0.841899395 |
| 24 | TPKDQINVLD * | 1143.589 | 572.293 | 2 | 10 | 0.839494526 |
| 25 | GDLQVLTQ | 873.4676 | 437.2395 | 2 | 8 | 0.83877182 |
| 26 | ENYGGETQVQ | 1124.485 | 562.7462 | 2 | 10 | 0.837942123 |
| 27 | QINVLDLMQ * | 1075.534 | 538.2697 | 2 | 9 | 0.837528408 |
| 28 | PRGDLQVLTQ | 1126.621 | 563.814 | 2 | 10 | 0.83436358 |
| 29 | KAARTLPTSFN | 1205.664 | 603.3296 | 2 | 11 | 0.831243873 |
| 30 | INVLDLMQTP | 1145.576 | 573.2885 | 2 | 10 | 0.830663443 |
| 31 | INVLDLMQTP * | 1144.592 | 572.8013 | 2 | 10 | 0.829244375 |
| 32 | LQVLTQKA * | 901.5353 | 451.2715 | 2 | 8 | 0.817822039 |
| 33 | KAARTLPTSF | 1091.621 | 546.3091 | 2 | 10 | 0.812230647 |
| 34 | IKATRVTE | 917.5415 | 459.2744 | 2 | 8 | 0.80939424 |
| 35 | INVLDLMQ * | 946.4914 | 473.7455 | 2 | 8 | 0.807365835 |
| 36 | TQVQRRQH * | 1055.523 | 528.267 | 2 | 8 | 0.803292811 |
| 37 | RGDLQVLTQ * | 1031.537 | 516.2765 | 2 | 9 | 0.802214622 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gao, Y.-Y.; Zhang, Z.-H.; Sang, C.-J.; Han, Y.; Cao, Y.-D.; Tang, Y.; Hu, G.-X.; Li, Z.-B.; Gao, F.-S. A New Strategy to Identify Naturally Presenting SLA-I Bound Peptides Derived from the O Serotype of Foot-and-Mouth Disease Virus, by Mild Acid Elution in a VP1 Stably Expressed PK15 Cell Line. Animals 2025, 15, 3097. https://doi.org/10.3390/ani15213097
Gao Y-Y, Zhang Z-H, Sang C-J, Han Y, Cao Y-D, Tang Y, Hu G-X, Li Z-B, Gao F-S. A New Strategy to Identify Naturally Presenting SLA-I Bound Peptides Derived from the O Serotype of Foot-and-Mouth Disease Virus, by Mild Acid Elution in a VP1 Stably Expressed PK15 Cell Line. Animals. 2025; 15(21):3097. https://doi.org/10.3390/ani15213097
Chicago/Turabian StyleGao, Yong-Yu, Zong-Hui Zhang, Chen-Jun Sang, Yong Han, Yu-Die Cao, Yue Tang, Gui-Xue Hu, Zi-Bin Li, and Feng-Shan Gao. 2025. "A New Strategy to Identify Naturally Presenting SLA-I Bound Peptides Derived from the O Serotype of Foot-and-Mouth Disease Virus, by Mild Acid Elution in a VP1 Stably Expressed PK15 Cell Line" Animals 15, no. 21: 3097. https://doi.org/10.3390/ani15213097
APA StyleGao, Y.-Y., Zhang, Z.-H., Sang, C.-J., Han, Y., Cao, Y.-D., Tang, Y., Hu, G.-X., Li, Z.-B., & Gao, F.-S. (2025). A New Strategy to Identify Naturally Presenting SLA-I Bound Peptides Derived from the O Serotype of Foot-and-Mouth Disease Virus, by Mild Acid Elution in a VP1 Stably Expressed PK15 Cell Line. Animals, 15(21), 3097. https://doi.org/10.3390/ani15213097






