Cryptorchidism in Equid: A Retrospective Study on Diagnostic Approach, Anaesthesia Management, Surgical Treatment and Outcomes
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Cases
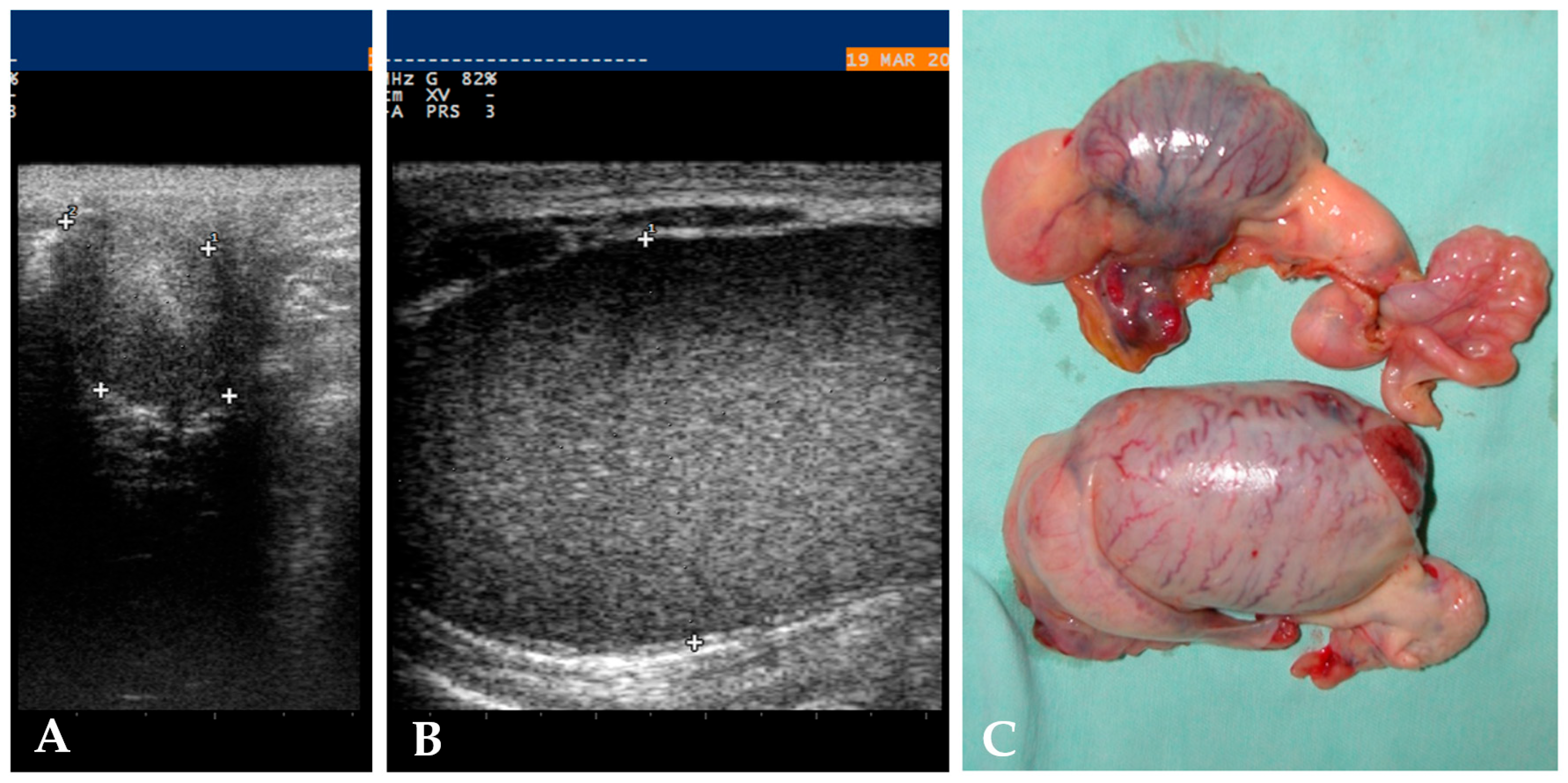
2.2. Diagnostics
2.3. Anaesthesia, Analgesia and Surgical Approach
2.3.1. Standing Flank Laparoscopic Cryptorchidectomy
2.3.2. Ventral Midline Laparoscopic Cryptorchidectomy
2.3.3. Open Inguinal Cryptorchidectomy
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arroyo, E.; Tibary, A. Cryptorchidism in stallions. Clin. Theriogenol. 2023, 15, 31–51. [Google Scholar] [CrossRef]
- Murase, H.; Ochi, A.; Tozaki, T.; Kakoi, H.; Munkhtuul, T.; Kurimoto, S.; Sato, F.; Hada, T. A case of equine cryptorchidism with undetectable serum anti-Müllerian hormone. J. Vet. Med. Sci. 2020, 82, 209–211. [Google Scholar] [CrossRef]
- Hartman, R.; Hawkins, J.F.; Adams, S.B.; Moore, G.E.; Fessler, J.F. Cryptorchidectomy in equid: 604 cases (1977–2010). J. Am. Vet. Med. Assoc. 2015, 246, 777–784. [Google Scholar] [CrossRef]
- Waqas, M.S.; Arroyo, E.; Tibary, A. Diagnostic Approach to Equine Testicular Disorders. Vet. Sci. 2024, 11, 243. [Google Scholar] [CrossRef]
- Straticò, P.; Varasano, V.; Guerri, G.; Celani, G.; Palozzo, A.; Petrizzi, L. A retrospective study of cryptorchidectomy in horses: Diagnosis, treatment, outcome and complications in 70 cases. Animals 2020, 10, 2446. [Google Scholar] [CrossRef]
- Gallagher, L.A.; Freeman, L.J.; Trenka-Benthin, S.; Stoloff, D.R. Laparoscopic castration for canine cryptorchidism. Vet. Surg. 1992, 21, 411–412. [Google Scholar]
- Vannozzi, I.; Benetti, C.; Rota, A. Laparoscopic cryptorchidectomy in a cat. J. Feline Med. Surg. 2002, 4, 201–203. [Google Scholar] [CrossRef] [PubMed]
- Kaneko, Y.; Torisu, S.; Kitahara, G.; Hidaka, Y.; Satoh, H.; Asanuma, T.; Mizutani, S.; Osawa, T.; Naganobu, K. Laparoscopic cryptorchidectomy in standing bulls. J. Vet. Med. Sci. 2015, 77, 631–635. [Google Scholar] [CrossRef] [PubMed]
- Lynch, N.; Adams, J.; Perrier, M. Laparoscopic cryptorchidectomy in a mature llama. Can. Vet. J. 2020, 61, 521. [Google Scholar] [PubMed]
- Vigani, A.; Garcia-Pereira, F.L. Anesthesia and analgesia for standing equine surgery. Vet. Clin. N. Am. Equine Pract. 2014, 30, 1–17. [Google Scholar] [CrossRef]
- Portela, D.A.; Romano, M.; Briganti, A. Retrospective clinical evaluation of ultrasound guided transverse abdominis plane block in dogs undergoing mastectomy. Vet. Anaesth. Analg. 2014, 41, 319–324. [Google Scholar] [CrossRef]
- Bettschart-Wolfensberger, R.; Ringer, S.K. General Anesthesia Techniques. In Manual of Equine Anesthesia and Analgesia, 2nd ed.; Doherty, T., Valverde, A., Reed, R.A., Eds.; Blackwell Pub: Hoboken, NJ, USA, 2022; pp. 339–351. [Google Scholar]
- Adams, A.; Hendrickson, D.A. Standing male urogenital surgery. Vet. Clin. N. Am. Pract. 2014, 30, 169–190. [Google Scholar] [CrossRef]
- Hendrickson, D.A. Standing laparoscopic cryptorchidectomy. In Equine Diagnostic Surgical Laparoscopy, 1st ed.; Fischer, A.T., Ed.; WB Saunders Co.: Philadelphia, PA, USA, 2002; pp. 155–161. [Google Scholar]
- Bracamonte, J.L.; Thomas, K.L. Laparoscopic cryptorchidectomy with a vessel-sealing device in dorsal recumbent horses: 43 cases. Vet. Surg. 2017, 46, 559–565. [Google Scholar] [CrossRef] [PubMed]
- Auer, J.A.; Kummerle, J.M. Reproductive System. In Equine Surgery, 5th ed.; Auer, J., Stick, J.M., Kummerle, J.M., Prange, T., Eds.; Elsevier: St. Louis, MO, USA, 2015; pp. 994–1033. [Google Scholar]
- Schumacher, J.; O’Brien, T. Complications of testicular surgery. In Complications in Equine Surgery, 1st ed.; Rubio-Martinez, L.M., Hendrickson, D.A., Eds.; Wiley-Blackwell: Hoboken, NJ, USA, 2021; pp. 498–521. [Google Scholar]
- Schambourg, M.A.; Farley, J.A.; Marcoux, M.; Laverty, S. Use of transabdominal ultrasonography to determine the location of cryptorchid testes in the horse. Equine Vet. J. 2006, 38, 242–245. [Google Scholar] [CrossRef] [PubMed]
- Sinovich, M.; Monné Rodriguez, J.; Pieńkowska-Schelling, A.; Schelling, C.; Kelly, P.G. An unusual case of a monorchid horse with an abdominally retained testicle. Sex. Dev. 2025, 19, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Cribb, N.C.; Koenig, J.; Sorge, U. Comparison of laparoscopic versus conventional open cryptorchidectomies on intraoperative and postoperative complications and duration of surgery, anesthesia, and hospital stay in horses. J. Am. Vet. Med. Assoc. 2015, 246, 885–892. [Google Scholar] [CrossRef]
- Baldo, C.F.; Almeida, D.; Wendt-Hornickle, E.; Guedes, A. Transversus abdominis plane block in ponies: A preliminary anatomical study. Vet. Anaesth. Analg. 2018, 45, 392–396. [Google Scholar] [CrossRef]
- Küls, N.; Trujanovic, R.; Otero, P.E.; Larenza-Menzies, M.P. Ultrasound-guided transversus abdominis plane block in Shetland ponies: A description of a three-point injection technique and evaluation of potential analgesic effects. J. Equine Vet. Sci. 2020, 90, 102994. [Google Scholar] [CrossRef]
- Medina-Bautista, F.; Nocera, I.; Sánchez de Medina, A.; Di Franco, C.; Briganti, A.; Morgaz, J.; Granados, M.D.M. An Ultrasound-Guided Thoracolumbar Erector Spinae Plane Block: An Experimental Preliminary Study in Horses. Animals 2025, 15, 2264. [Google Scholar] [CrossRef]
- Freitag, F.A.; Amora, D.D.S., Jr.; Muehlbauer, E.; Dornbusch, P.T.; Machado, M.; Montiani-Ferreira, F.; Moreno, J.C.D. Ultrasound-guided modified subcostal transversus abdominis plane block and influence of recumbency position on dye spread in equine cadavers. Vet. Anaesth. Analg. 2021, 48, 596–602. [Google Scholar] [CrossRef]
- Clements, P.E.; Coomer, R.P.C.; McKane, S.A.; Gorvy, D.; Bladon, B.; Mair, T. Clinical findings in 10 horses diagnosed with monorchidism following exploratory laparotomy or standing laparoscopic surgery. Equine Vet. Educ. 2020, 32, 431–436. [Google Scholar] [CrossRef]
- Searle, D.; Dart, A.J.; Dart, C.M.; Hodgson, D.R. Equine castration: Review of anatomy, approaches, techniques and complications in normal, cryptorchid and monorchid horses. Aust. Vet. J. 1999, 77, 428–434. [Google Scholar] [CrossRef]
- Kummer, M.; Gygax, D.; Jackson, M.; Bettschart-Wolfensberger, R.; Fuerst, A. Results and complications of a novel technique for primary castration with an inguinal approach in horses. Equine Vet. J. 2009, 41, 547–551. [Google Scholar] [CrossRef] [PubMed]
- Emberteson, R.M. Selected urogenital surgery concerns and complications. Vet. Clin. N. Am. Pract. 2008, 24, 643–661. [Google Scholar] [CrossRef] [PubMed]
- Shettko, D.L.; Hendrickson, D.A. Complications of equine laparoscopy. In Complications in Equine Surgery; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2021; pp. 391–403. [Google Scholar]
- Ireland, J.L.; Clegg, P.D.; McGowan, C.M.; McKane, S.A.; Chandler, K.J.; Pinchbeck, G.L. Comparison of owner-reported health problems with veterinary assessment of geriatric horses in the United Kingdom. Equine Vet. J. 2012, 44, 94–100. [Google Scholar] [CrossRef] [PubMed]
| Local Anaesthesia Technique 19/33 (58%) | Prevalence and Percentage |
|---|---|
| Local injection of lidocaine only | 7/19, 37% |
| Local injection and epidural anaesthesia | 5/19, 26% |
| Local injection and splash | 4/19, 21% |
| Epidural anaesthesia only | 2/19, 11% |
| TAP block | 1/19, 5% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nocera, I.; Moroni, R.; Fanelli, D.; Rota, A.; Di Franco, C.; Ungari, C.; Puccinelli, C.; Gandini, M.; Giusto, G.; Vannozzi, I. Cryptorchidism in Equid: A Retrospective Study on Diagnostic Approach, Anaesthesia Management, Surgical Treatment and Outcomes. Animals 2025, 15, 2923. https://doi.org/10.3390/ani15192923
Nocera I, Moroni R, Fanelli D, Rota A, Di Franco C, Ungari C, Puccinelli C, Gandini M, Giusto G, Vannozzi I. Cryptorchidism in Equid: A Retrospective Study on Diagnostic Approach, Anaesthesia Management, Surgical Treatment and Outcomes. Animals. 2025; 15(19):2923. https://doi.org/10.3390/ani15192923
Chicago/Turabian StyleNocera, Irene, Rebecca Moroni, Diana Fanelli, Alessandra Rota, Chiara Di Franco, Camilla Ungari, Caterina Puccinelli, Marco Gandini, Gessica Giusto, and Iacopo Vannozzi. 2025. "Cryptorchidism in Equid: A Retrospective Study on Diagnostic Approach, Anaesthesia Management, Surgical Treatment and Outcomes" Animals 15, no. 19: 2923. https://doi.org/10.3390/ani15192923
APA StyleNocera, I., Moroni, R., Fanelli, D., Rota, A., Di Franco, C., Ungari, C., Puccinelli, C., Gandini, M., Giusto, G., & Vannozzi, I. (2025). Cryptorchidism in Equid: A Retrospective Study on Diagnostic Approach, Anaesthesia Management, Surgical Treatment and Outcomes. Animals, 15(19), 2923. https://doi.org/10.3390/ani15192923






