Aerosol Dynamics in the Respiratory Tract of Food-Producing Animals: An Insight into Transmission Patterns and Deposition Distribution
Simple Summary
Abstract
1. Introduction
- Develop a 1:1 three-dimensional CFD model of a pig’s respiratory tract using CT scanning data.
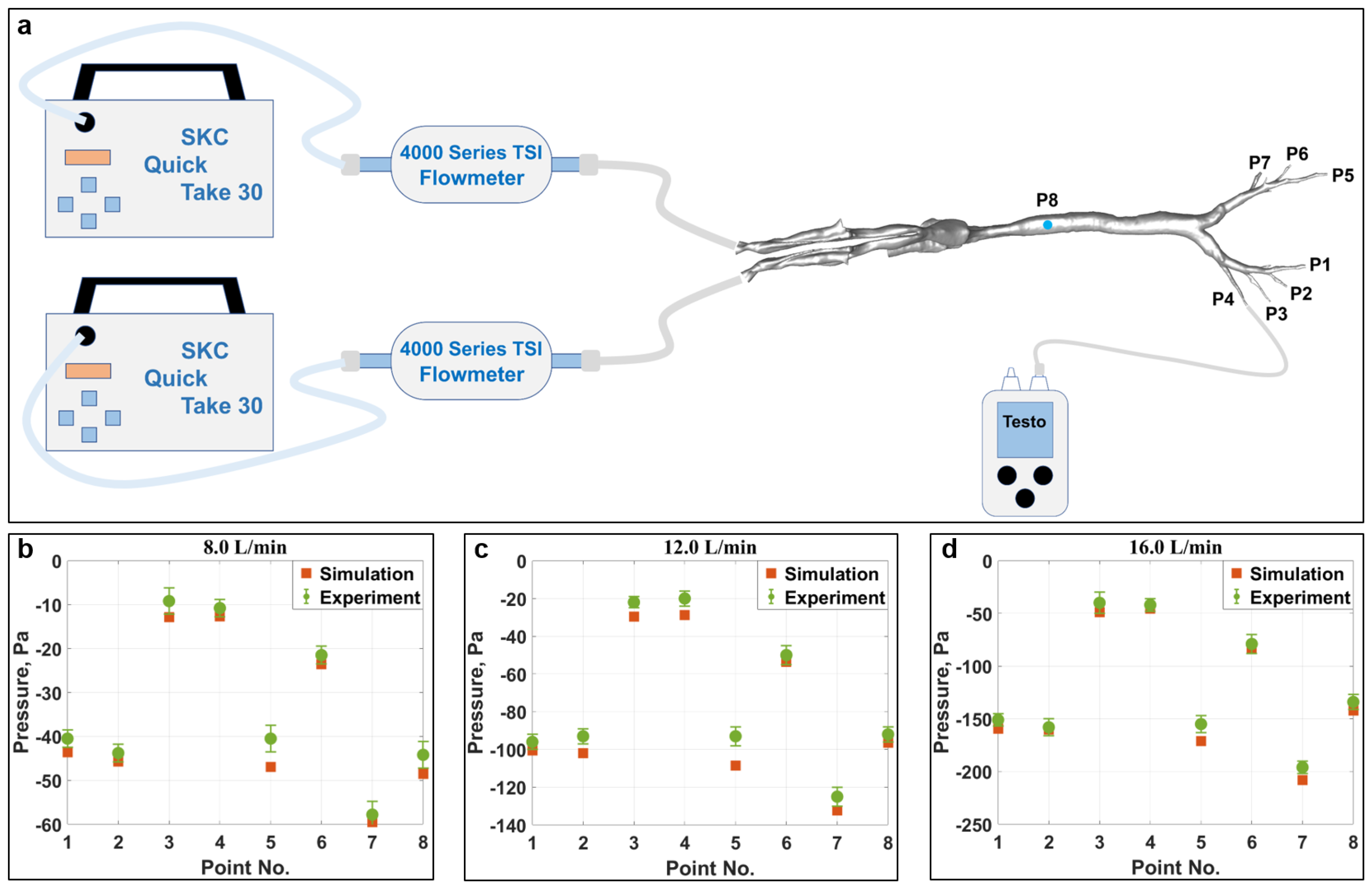
- Validate the computational model using a 3D-printed physical model.
- Simulate the aerosol dynamics in the respiratory tract under various conditions by using the Discrete Phase Model (DPM). Qualitatively and quantitively examine the aerosol deposition behaviors.
- Reveal the penetration characteristics of aerosols with different particle sizes in the respiratory tract and the deposition distribution across various regions.
- Contribute to fundamental scientific data for the development of aerosolized vaccines by targeting distinct regions of the respiratory tract with different particle sizes.
2. Materials and Methods
2.1. Model Development and Simulation Setup
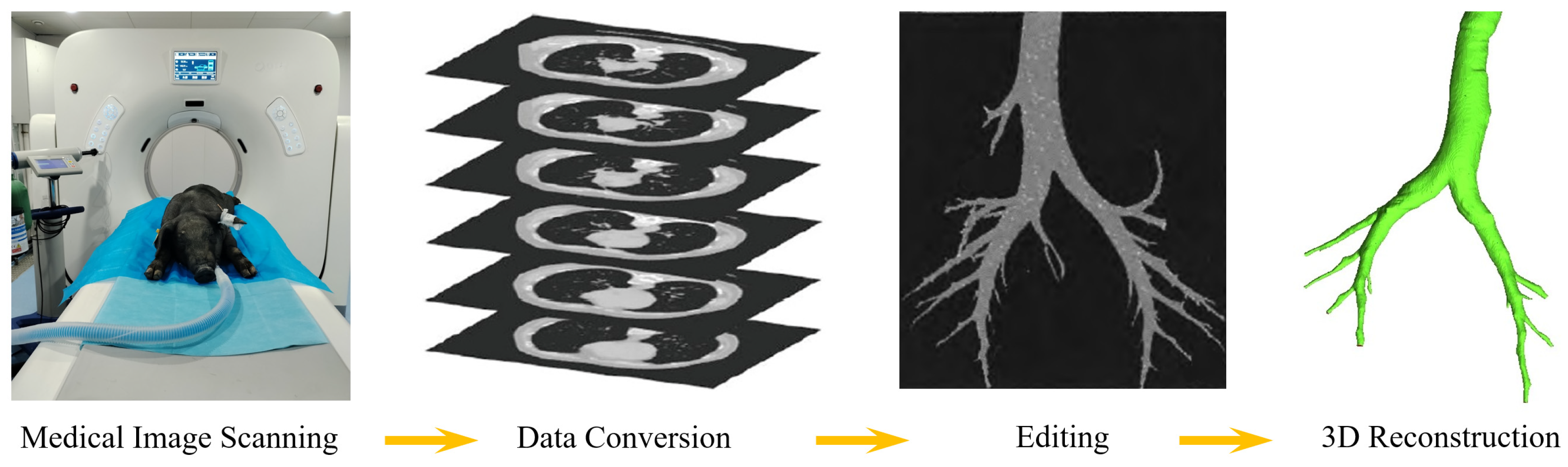
2.1.1. Reconstruction of the Respiratory Tract’s Geometry
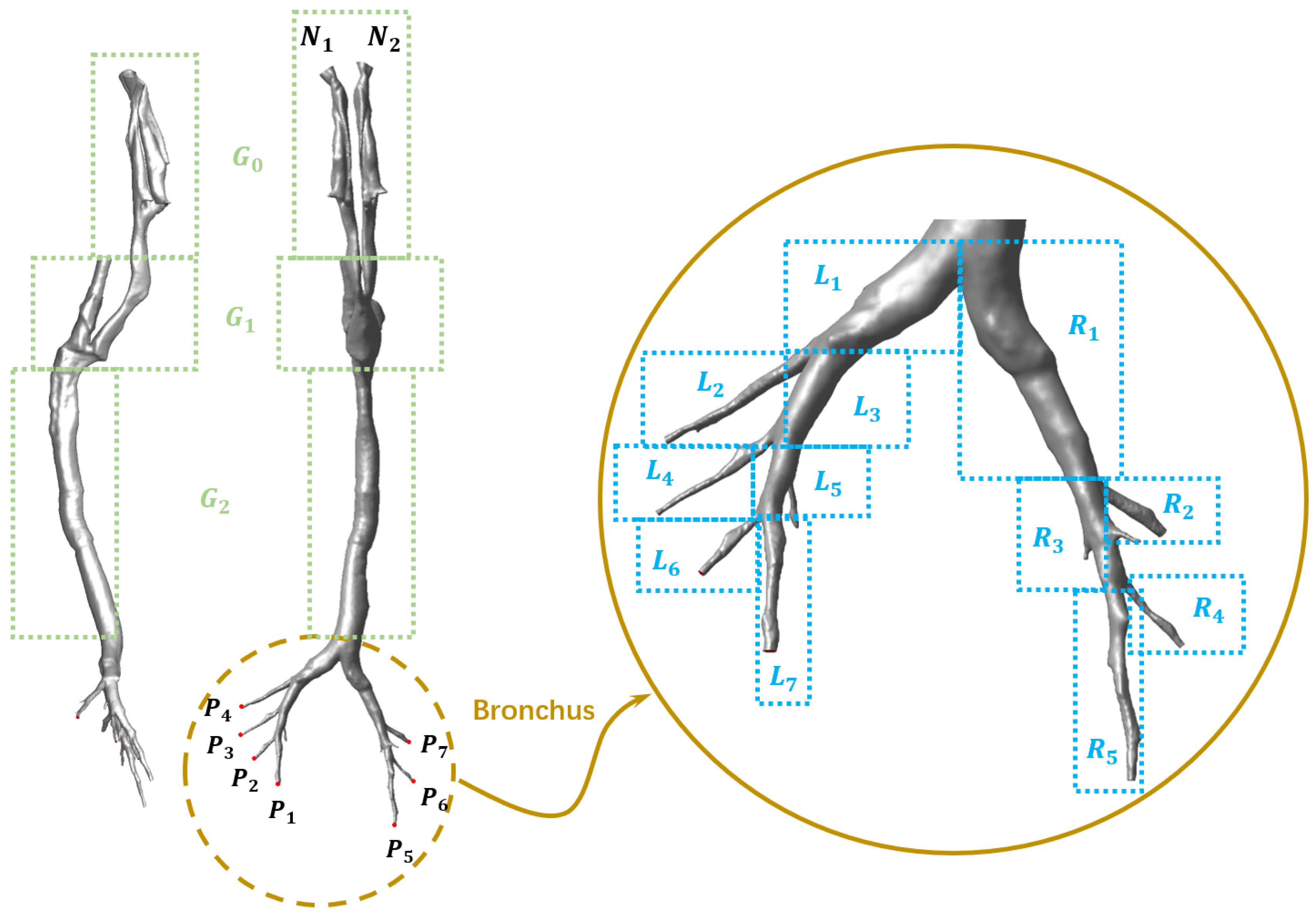
2.1.2. Mesh Generation and Regional Division
2.1.3. Particle Transport Model
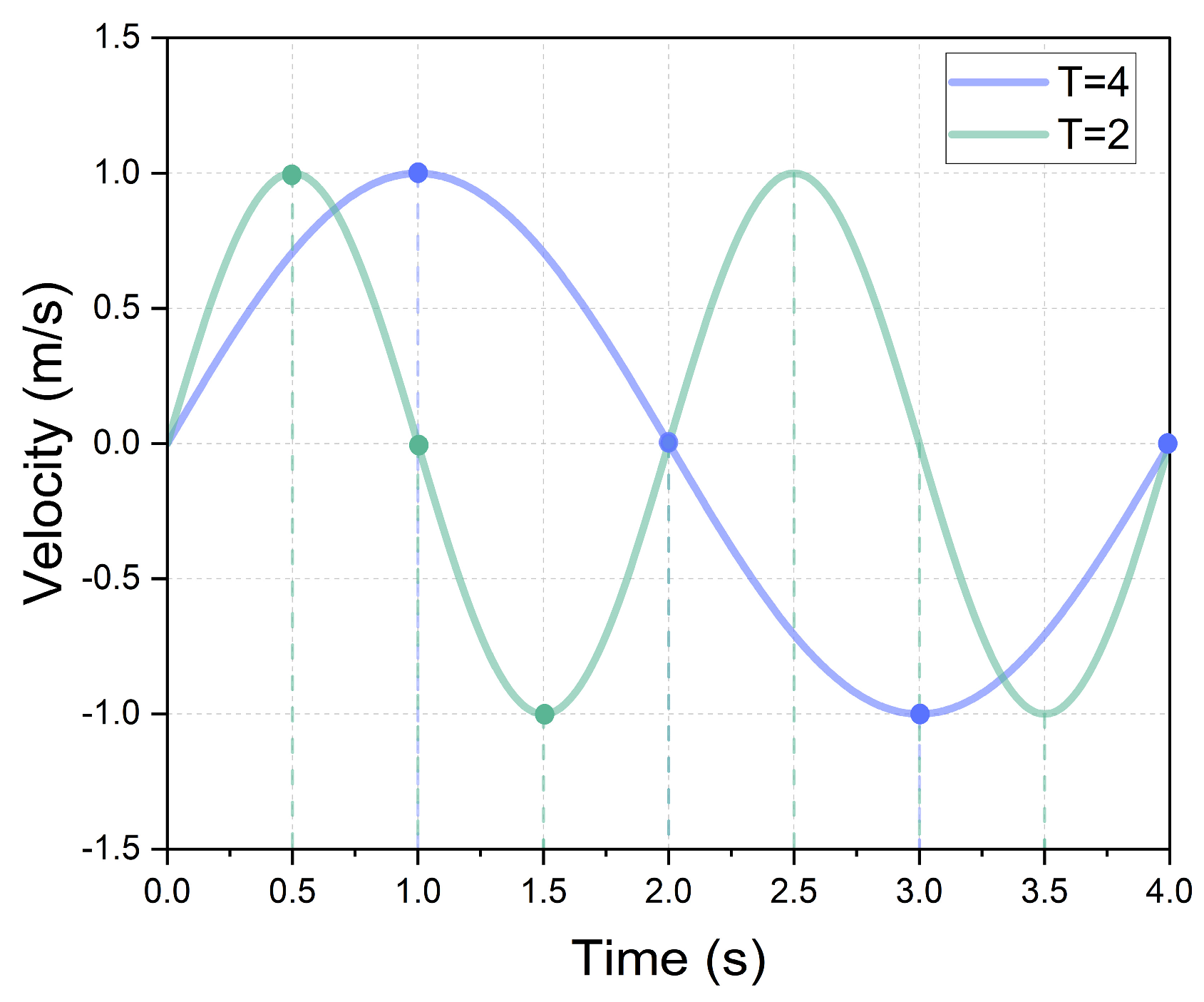
2.1.4. Boundary Condition
2.1.5. CFD Setup
2.1.6. Deposition and Escape Efficiency
2.2. Grid Independency Study and Model Validation
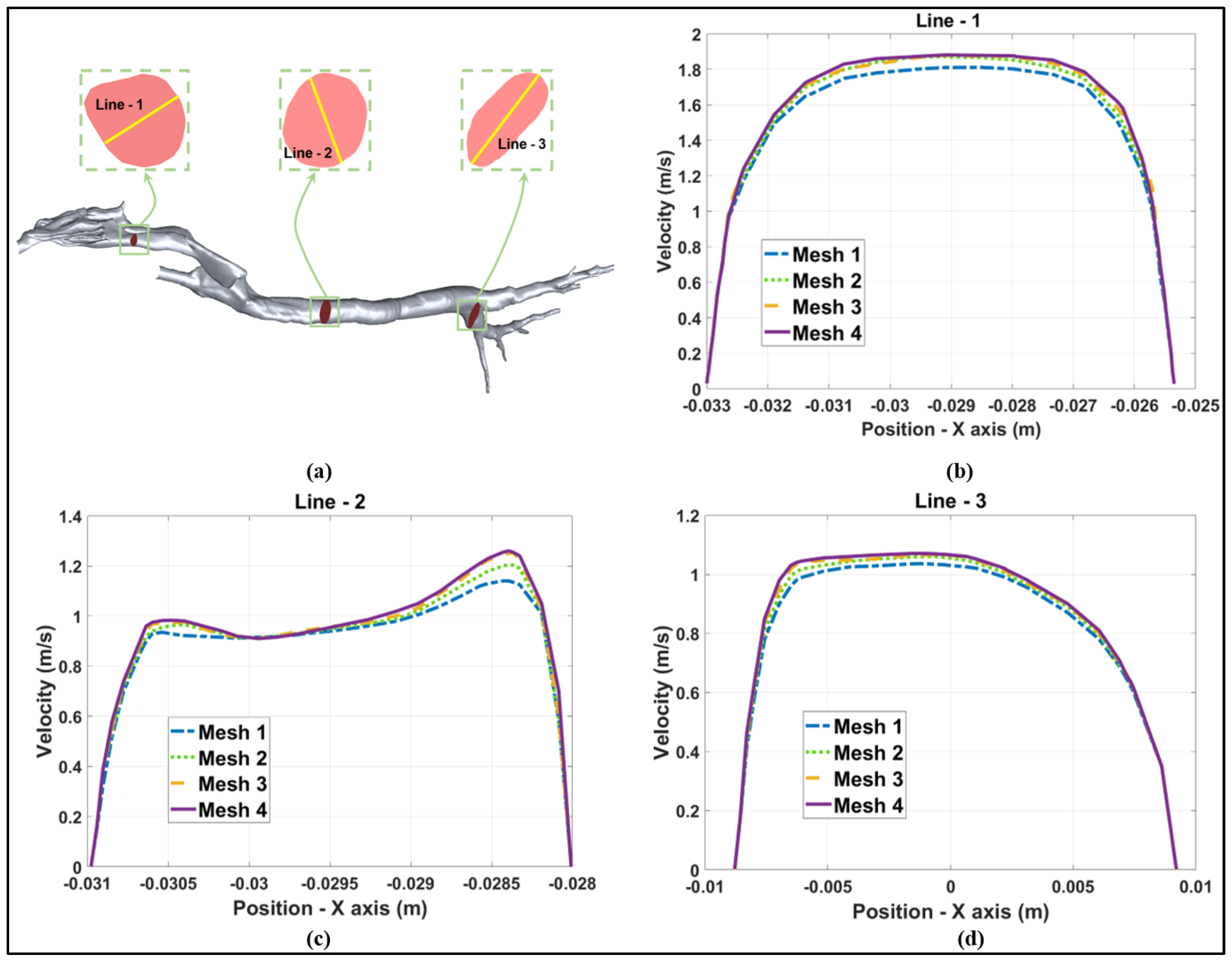
2.2.1. Grid Independency Test
2.2.2. Simulation Model Validation
3. Results and Discussion
3.1. Flow Structure and Characteristics
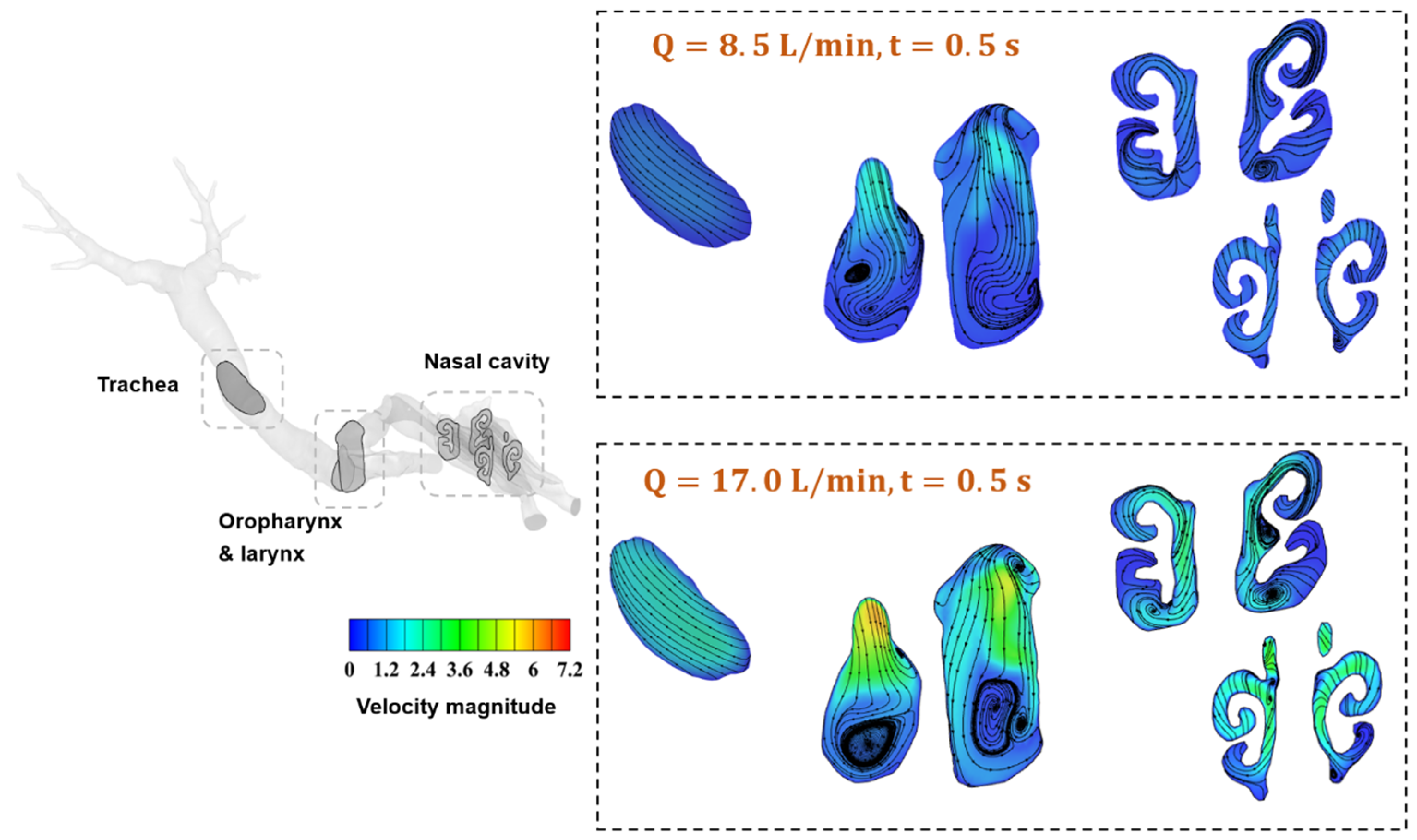
3.1.1. Streamlines of Airflow in Typical Regions of the Respiratory Tract
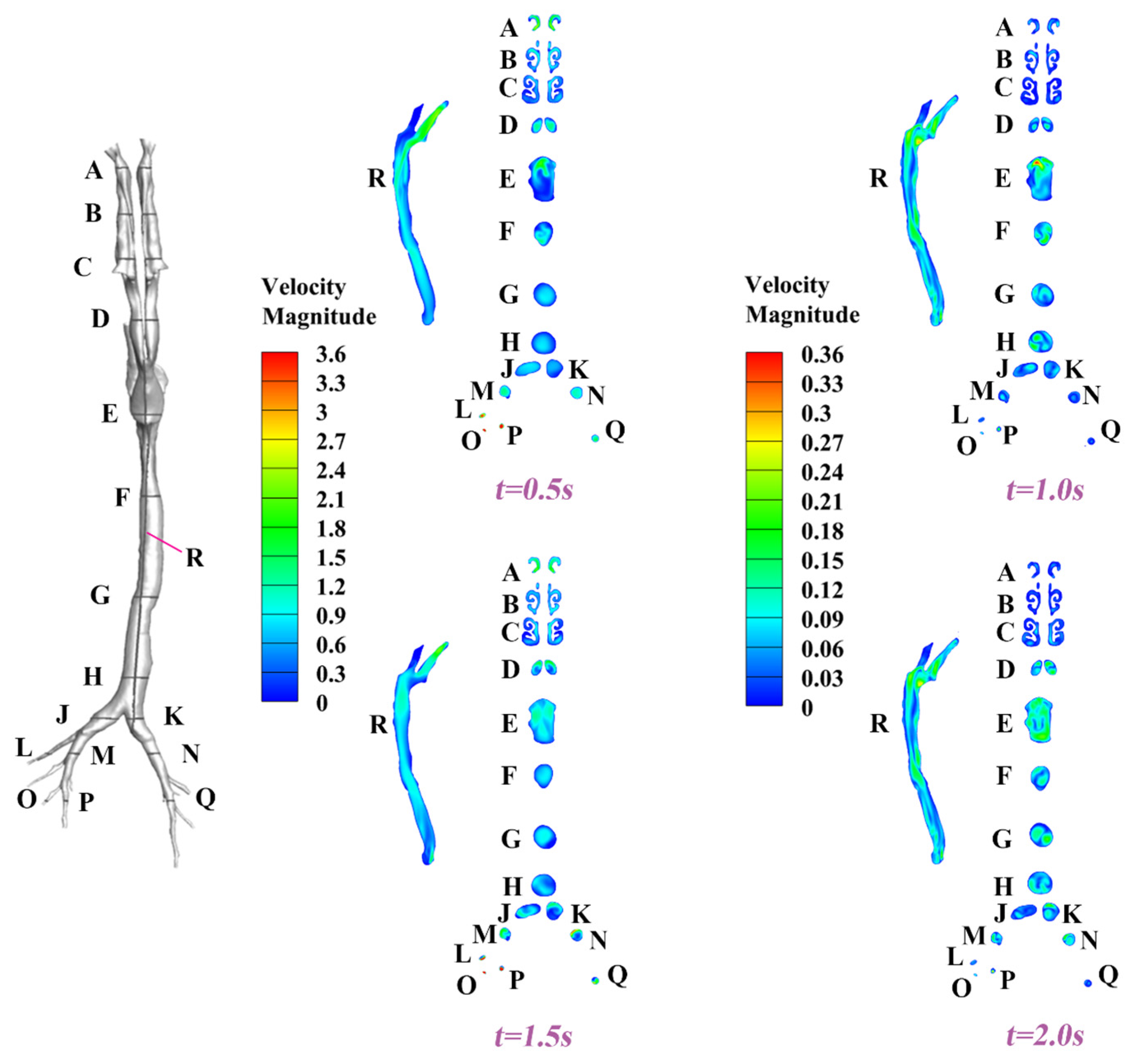
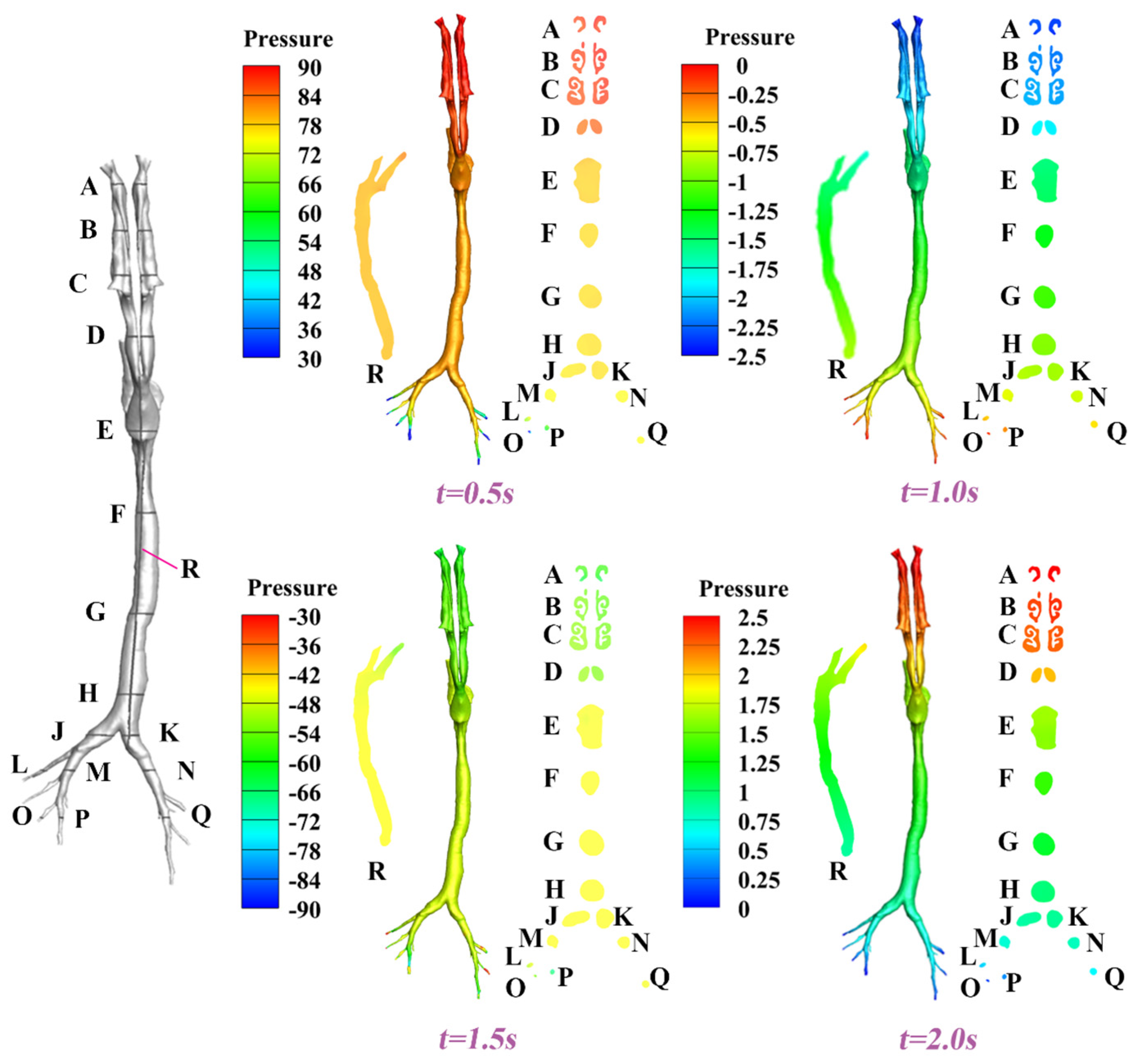
3.1.2. Dynamic Velocity and Pressure Pattern in the Airway
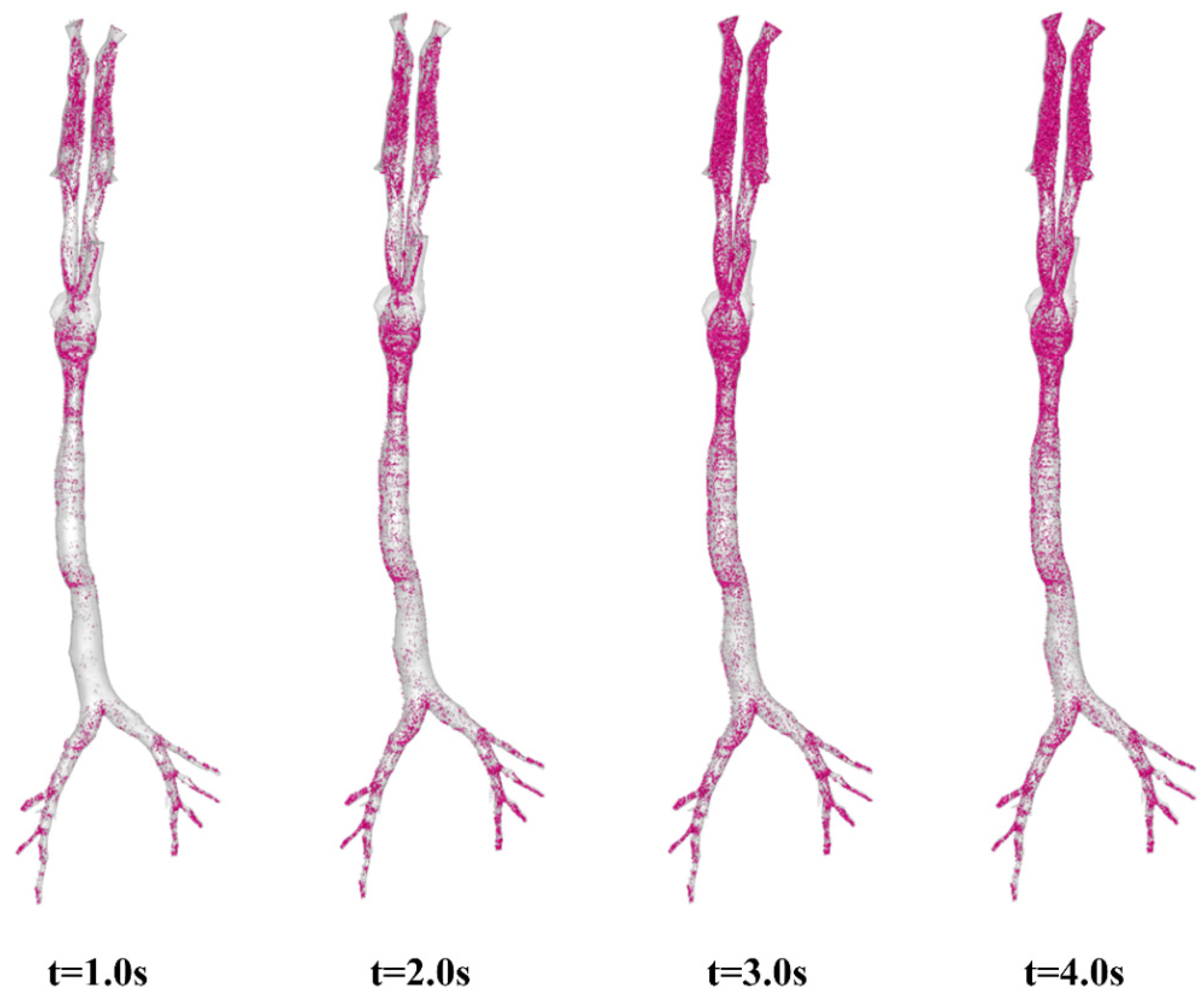
3.2. Visualization of Aerosol Dynamic Deposition
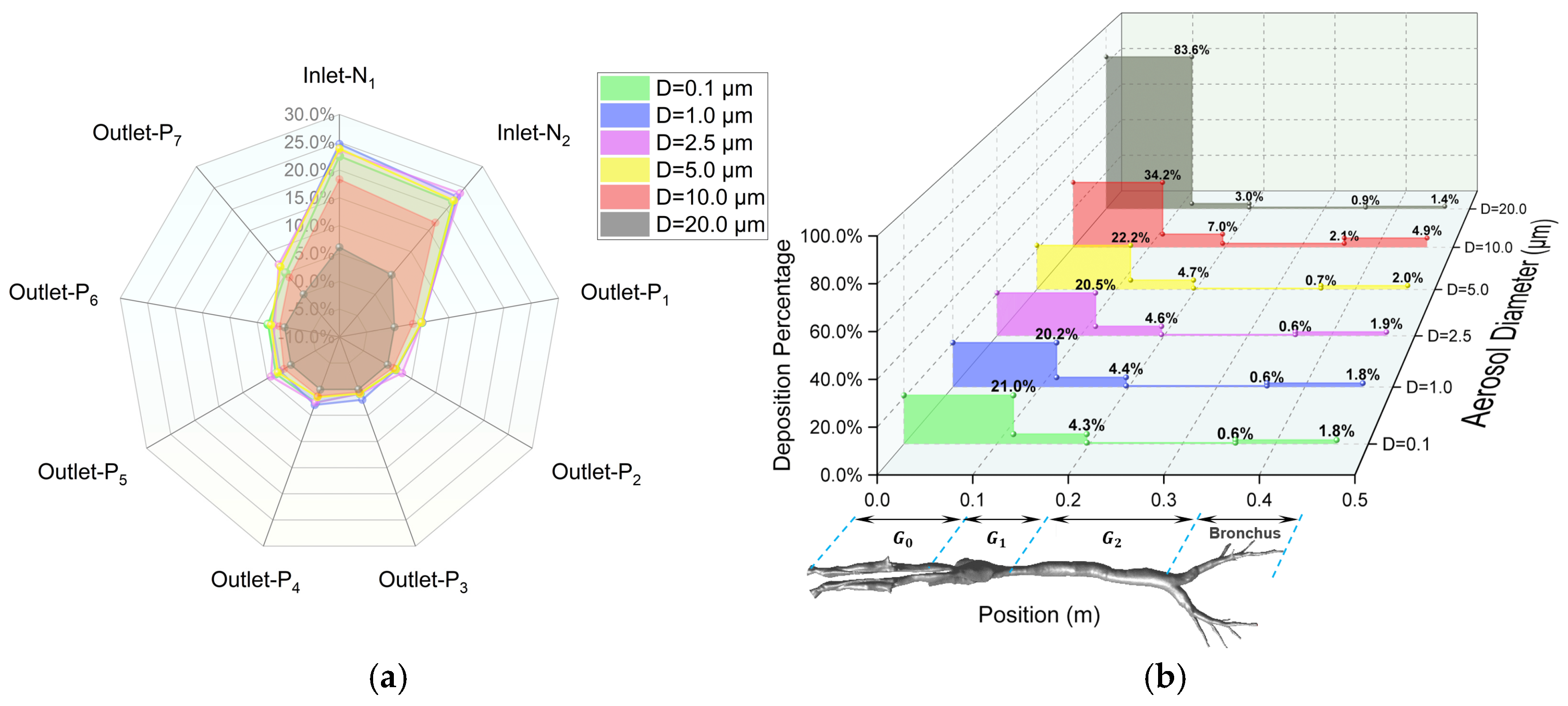
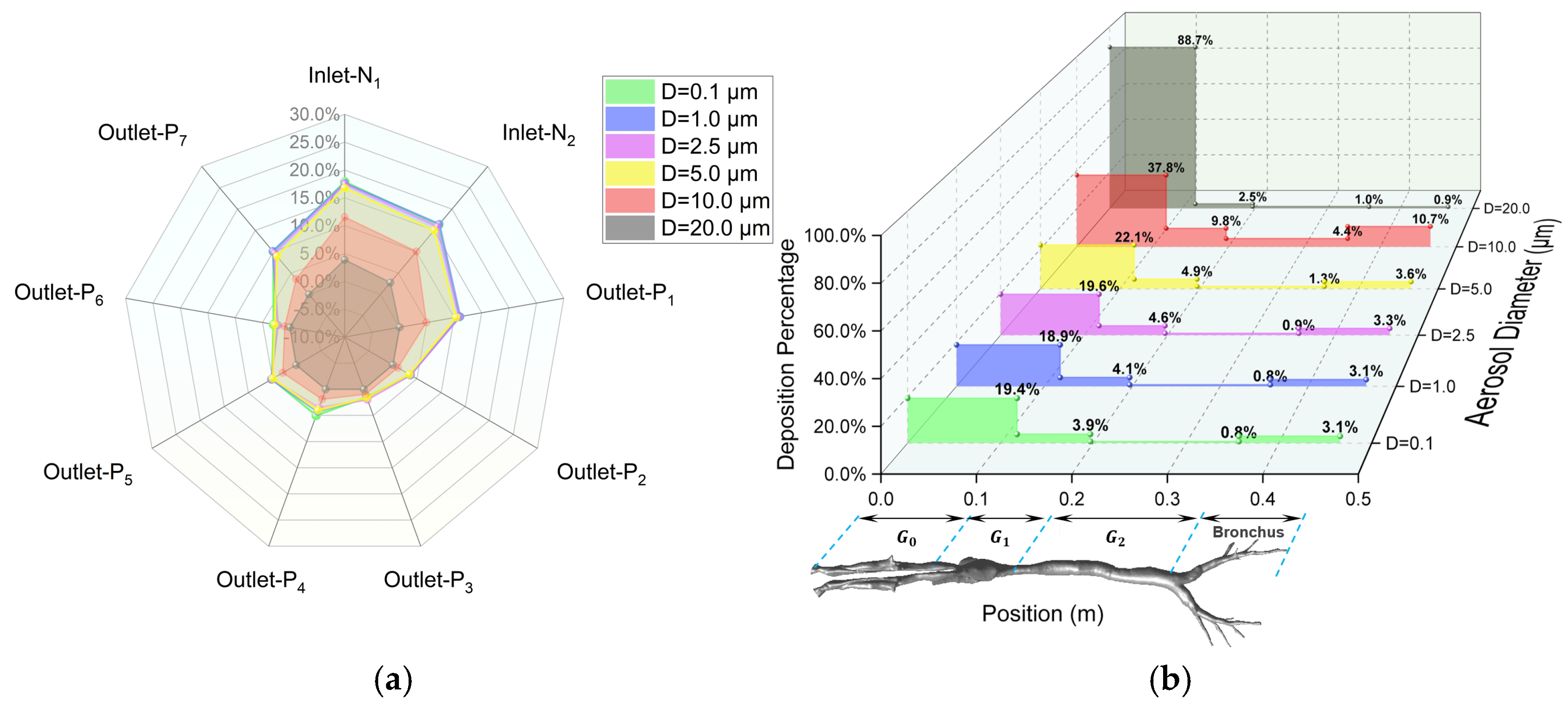
3.3. Regional Escape and Deposition Fraction
3.4. Limitations
4. Conclusions
- Aerosol Screening Mechanism Driven by Anatomical–Fluid Coupling Effect.
- Particle-Size-Dependent Regulation Patterns of Respiratory Dynamics Parameters.
- Bronchial Deposition Asymmetry Induced by Cardiac Anatomical Bias.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hu, Z.; Tian, X.; Lai, R.; Ji, C.; Li, X. Airborne transmission of common swine viruses. Porc. Health Manag. 2023, 9, 50. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Liu, R.; Zhang, X.; Li, F.; Wang, J.; Zhang, J.; Liu, X.; Wang, L.; Zhang, J.; Wu, X. Replication and virulence in pigs of the first African swine fever virus isolated in China. Emerg. Microbes Infect. 2019, 8, 438–447. [Google Scholar] [CrossRef] [PubMed]
- Desrosiers, R.; Kluber, E. Suspected aerosol transmission of swine pathogens: A field case. Can. Vet. J. 2024, 65, 707–711. [Google Scholar]
- Sedano, S.A.; Cantalejo, M.G.C.T.; Lapitan, C.G.A.R.; de Guzman, A.M.E.S.; Consignado, J.T.; Tandang, N.A.; Estacio, M.A.C.; Kerdsin, A.; Silva, B.B.I. Epidemiology and genetic diversity of Streptococcus suis in smallhold swine farms in the Philippines. Sci. Rep. 2023, 13, 21178. [Google Scholar] [CrossRef]
- Sun, H.; Li, H.; Tong, Q.; Han, Q.; Liu, J.; Yu, H.; Song, H.; Qi, J.; Li, J.; Yang, J.; et al. Airborne transmission of human-isolated avian H3N8 influenza virus between ferrets. Cell 2023, 186, 4074–4084. [Google Scholar] [CrossRef]
- Ul-Rahman, A.; Ishaq, H.M.; Raza, M.A.; Shabbir, M.Z. Zoonotic potential of Newcastle disease virus: Old and novel perspectives related to public health. Rev. Med. Virol. 2022, 32, e2246. [Google Scholar] [CrossRef]
- Kanankege, K.S.T.; Graham, K.; Corzo, C.A.; VanderWaal, K.; Perez, A.M.; Durr, P.A. Adapting an Atmospheric Dispersion Model to Assess the Risk of Windborne Transmission of Porcine Reproductive and Respiratory Syndrome Virus between Swine Farms. Viruses 2022, 14, 1658. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Hu, Z.; Fan, M.; Tian, X.; Wu, W.; Gao, W.; Bian, L.; Jiang, X. Evidence of aerosol transmission of African swine fever virus between two piggeries under field conditions: A case study. Front. Vet. Sci. 2023, 10, 1201503. [Google Scholar] [CrossRef]
- Liu, T.; Li, G.; Liu, Z.; Xi, L.; Ma, W.; Gao, X. Characteristics of aerosols from swine farms: A review of the past two-decade progress. Environ. Int. 2023, 178, 108074. [Google Scholar] [CrossRef]
- Fernstrom, A.; Goldblatt, M. Aerobiology and Its Role in the Transmission of Infectious Diseases. J. Pathog. 2013, 2013, 493960. [Google Scholar] [CrossRef]
- Kim, K.Y.; Ko, H.J. Indoor distribution characteristics of airborne bacteria in pig buildings as influenced by season and housing type. Anim. Biosci. 2019, 32, 742–747. [Google Scholar] [CrossRef]
- Huang, K.; Tang, Q.; Shen, D.; Dai, P.Y.; Liu, J.Z.; Li, Y.S.; Li, C.M. Distribution of particulate matter and microbial aerosol concentration in different types of swine houses in winter. J. Agro-Environ. Sci. 2019, 38, 1616–1623. [Google Scholar]
- Cui, H.; Zhang, C.; Liu, J.; Dong, S.; Zhao, K.; Chen, L.; Chen, Z.; Sun, Y.; Guo, Z. The distribution characteristics of aerosol bacteria in different types of pig houses. Animals 2022, 12, 1540. [Google Scholar] [CrossRef]
- Sowiak, M.; Bródka, K.; Buczy’ nska, A.; Cyprowski, M.; Kozajda, A.; Sobala, W.; Szadkowska-Sta’ nczyk, I. An Assessment of Potential Exposure to Bioaerosols among Swine Farm Workers with Particular Reference to Airborne Microorganisms in the Respirable Fraction under Various Breeding Conditions. Aerobiologia 2012, 28, 121–133. [Google Scholar] [CrossRef]
- Madsen, A.M.; Kurdi, I.; Feld, L.; Tendal, K. Airborne MRSA and Total Staphylococcus Aureus as Associated with Particles of Different Sizes on Pig Farms. Ann. Work Expo. Health 2018, 62, 966–977. [Google Scholar] [CrossRef] [PubMed]
- White, J.K.; Nielsen, J.L.; Madsen, A.M. Potential Respiratory Deposition and Species Composition of Airborne Culturable, Viable, and Non-Viable Fungi during Occupancy in a Pig Farm. Atmosphere 2020, 11, 639. [Google Scholar] [CrossRef]
- O’Brien, K.M.; Nonnenmann, M.W. Airborne influenza a is detected in the personal breathing zone of swine veterinarians. PLoS ONE 2016, 11, e0149083. [Google Scholar] [CrossRef] [PubMed]
- Alonso, C.; Raynor, P.C.; Goyal, S.; Olson, B.A.; Alba, A.; Davies, P.R.; Torremorell, M. Assessment of air sampling methods and size distribution of virus-laden aerosols in outbreaks in swine and poultry farms. J. Vet. Diagn. Investig. 2017, 29, 298–304. [Google Scholar] [CrossRef]
- Yu, L.; Zhu, Z.; Deng, J.; Tian, K.; Li, X. Antagonisms of ASFV towards Host Defense Mechanisms: Knowledge Gaps in Viral Immune Evasion and Pathogenesis. Viruses 2023, 15, 574. [Google Scholar] [CrossRef]
- Ayanwale, A.; Trapp, S.; Guabiraba, R.; Caballero, I.; Roesch, F. New Insights in the Interplay Between African Swine Fever Virus and Innate Immunity and Its Impact on Viral Pathogenicity. Front. Microbiol. 2022, 13, 958307. [Google Scholar] [CrossRef]
- Li, X.; Sun, L.; Zhao, J.; Tu, K.; Xue, J.; Guo, X.; Zhang, G. Mutations in the methyltransferase motifs of L protein attenuate Newcastle disease virus by regulating viral translation and cell-to-cell spread. Microbiol. Spectr. 2021, 9, e0131211. [Google Scholar] [CrossRef]
- Quinteros, J.A.; Noormohammadi, A.H.; Lee, S.W.; Browning, G.F.; Diaz-Mendez, A. Genomics and pathogenesis of the avian coronavirus infectious bronchitis virus. Aust. Vet. J. 2022, 100, 496–512. [Google Scholar] [CrossRef] [PubMed]
- Zhan, Y.; Yu, S.; Yang, S.; Qiu, X.; Meng, C.; Tan, L.; Song, C.; Liao, Y.; Liu, W.; Sun, Y.; et al. Newcastle Disease virus infection activates PI3K/Akt/mTOR and p38 MAPK/Mnk1 pathways to benefit viral mRNA translation via interaction of the viral NP protein and host eIF4E. PLoS Pathog. 2020, 16, e1008610. [Google Scholar] [CrossRef] [PubMed]
- Fiegel, J.; Garcia-Contreras, L.; Thomas, M.; VerBerkmoes, J.; Elbert, K.; Hickey, A.; Edwards, D. Preparation and in Vivo Evaluation of a Dry Powder for Inhalation of Capreomycin. Pharm. Res. 2008, 25, 805–811. [Google Scholar] [CrossRef]
- Sood, B.G.; Shen, Y.M.; Latif, Z.; Galli, B.; Dawe, E.J.; Haccke, E.M. Effective aerosol delivery during high-frequency ventilation in neonatal pigs. Respirol. 2010, 15, 551–555. [Google Scholar] [CrossRef]
- Asgharian, B.; Miller, F.J.; Price, O.; Schroeter, J.D.; Einstein, D.R.; Corley, R.A.; Bentley, T. Modeling particle deposition in the pig respiratory tract. J. Aerosol Sci. 2016, 99, 107–124. [Google Scholar] [CrossRef]
- Awadalla, M.; Miyawaki, S.; Abou Alaiwa, M.H.; Adam, R.J.; Bouzek, D.C.; Michalski, A.S.; Fuld, M.K.; Reynolds, K.J.; Hoffman, E.A.; Lin, C.; et al. Early Airway Structural Changes in Cystic Fibrosis Pigs as a Determinant of Particle Distribution and Deposition. Ann. Biomed. Eng. 2014, 42, 915–927. [Google Scholar] [CrossRef][Green Version]
- Li, H.; Li, G.; Sha, W.; Niu, W.; Zhang, X.; Jiang, C. Effective Research of Prevention and Treatment of Swine Atrophic Rhinitis with Nasal Spray. J. Jilin Agric. Sci. Technol. Univ. 2016, 25, 4–7. [Google Scholar]
- Landman, W.J.M.; Vervaet, C.; Remon, J.P.; Huyge, K.; van Eck, J.H.H. Primary Newcastle disease vaccination of broilers: Comparison of the antibody seroresponse and adverse vaccinal reaction after eye-nose drop or coarse spray application, and implication of the results for a previously developed coarse dry powder vaccine. Avian Pathol. 2017, 46, 451–461. [Google Scholar] [CrossRef]
- Deville, S.; Arous, J.B.; Bertrand, F.; Borisov, V.; Dupuis, L. Efficacy of intranasal and spray delivery of adjuvanted live vaccine against infectious bronchitis virus in experimentally infected poultry. Procedia Vaccinol. 2012, 6, 85–92. [Google Scholar] [CrossRef]
- Calderon-Nieva, D.; Goonewardene, K.B.; Gomis, S.; Foldvari, M. Veterinary vaccine nanotechnology: Pulmonary and nasal delivery in livestock animals. Drug Deliv. Transl. Res. 2017, 7, 558–570. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.J.; Tang, T.; Chen, Z.; Chen, L.; Cheng, J.L.; Li, F.; Sun, J.; Zhao, J.X.; Wang, Y.Q.; Yan, Q.H.; et al. Antibody dynamics for heterologous boosters with aerosolized Ad5-nCoV following inactivated COVID-19 vaccines. Hum. Vaccin. Immunother. 2024, 20, 2423466. [Google Scholar] [CrossRef]
- Ahookhosh, K.; Saidi, M.; Mohammadpourfard, M.; Aminfar, H.; Hamishehkar, H.; Farnoud, A.; Schmid, O. Flow Structure and Particle Deposition Analyses for Optimization of a Pressurized Metered Dose Inhaler (pMDI) in a Model of Tracheobronchial Airway. Eur. J. Pharm. Sci. 2021, 164, 105911. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Feng, B. Transmission of droplet aerosols in an elevator cabin: Effect of the ventilation mode. Build. Environ. 2023, 236, 110261. [Google Scholar] [CrossRef]
- Komperda, J.; Peyvan, A.; Li, D.; Kashir, B.; Yarin, A.L.; Megaridis, C.M.; Mirbod, P.; Paprotny, I.; Cooper, L.F.; Rowan, S.; et al. Computer simulation of the SARS-CoV-2 contamination risk in a large dental clinic. Phys. Fluids 2021, 33, 033328. [Google Scholar] [CrossRef] [PubMed]
- Barbosa Pereira, C.; Dohmeier, H.; Kunczik, J.; Hochhausen, N.; Tolba, R.; Czaplik, M. Contactless monitoring of heart and respiratory rate in anesthetized pigs using infrared thermography. PLoS ONE 2019, 14, e0224747. [Google Scholar] [CrossRef]
- Su, Z.; Oto, J.; Wang, J.; Kimball, W.R.; Chenelle, C.T.; Kacmarek, R.M.; King, D.R.; Jiang, Y.; Duggan, M.J. Validation of Respiratory Inductance Plethysmography for Measuring Tidal Volume in Swine. Comp. Med. 2015, 65, 225–231. [Google Scholar]
- Gautam, K.R.; Rong, L.; Iqbal, A.; Zhang, G. Full-scale CFD simulation of commercial pig building and comparison with porous media approximation of animal occupied zone. Comput. Electron. Agric. 2021, 186, 106206. [Google Scholar] [CrossRef]
- Islam, M.S.; Larpruenrudee, P.; Saha, S.C.; Pourmehran, O.; Paul, A.R.; Gemci, T.; Collins, R.; Paul, G.; Gu, Y. How severe acute respiratory syndrome coronavirus-2 aerosol propagates through the age-specific upper airways. Phys. Fluids 2021, 33, 081911. [Google Scholar] [CrossRef]
- Guo, Y.; Wei, J.; Ou, C.; Liu, L.; Sadrizadeh, S.; Jin, T.; Tang, L.; Zhang, Y.; Li, Y. Deposition of droplets from the trachea or bronchus in the respiratory tract during exhalation: A steady-state numerical investigation. Aerosol Sci. Technol. 2020, 54, 869–879. [Google Scholar] [CrossRef]
- Rahimi-Gorji, M.; Pourmehran, O.; Gorji-Bandpy, M.; Gorji, T.B. CFD simulation of airflow behavior and particle transport and deposition in different breathing conditions through the realistic model of human airways. J. Mol. Liq. 2015, 209, 121–133. [Google Scholar] [CrossRef]
- Du, L.; Tao, X.; Zhu, L.; Li, J.; Fu, M.; Lai, J.; Yang, C.; He, Z. Advantages of targeted ventilation for farrowing houses: An analysis from perspectives of thermal environment, biosecurity and ventilation efficacy. Comput. Electron. Agric. 2024, 225, 109308. [Google Scholar] [CrossRef]
- Cheng, Q.; Li, H.; Rong, L.; Feng, X.; Zhang, G.; Li, B. Using CFD to assess the influence of ceiling deflector design on airflow distribution in hen house with tunnel ventilation. Comput. Electron. Agric. 2018, 151, 165–174. [Google Scholar] [CrossRef]
- Du, L.; Yang, L.; Yang, C.; Hu, C.; Yu, C.; Qiu, M.; Liu, S.; Zhu, S.; Ye, X. Development and Validation of an Energy Consumption Model for Animal Houses Achieving Precision Livestock Farming. Animals 2022, 12, 2580. [Google Scholar] [CrossRef]
- Du, L.; Yang, C.; Dominy, R.; Yang, L.; Hu, C.; Du, H.; Li, Q.; Yu, C.; Xie, L.; Jiang, X. Computational Fluid Dynamics aided investigation and optimization of a tunnel-ventilated poultry house in China. Comput. Electron. Agric. 2019, 159, 1–15. [Google Scholar] [CrossRef]
- Rahman, M.M.; Zhao, M.; Islam, M.S.; Dong, K.; Saha, S.C. Nanoparticle transport and deposition in a heterogeneous human lung airway tree: An efficient one path model for CFD simulations. Eur. J. Pharm. Sci. 2022, 177, 106279. [Google Scholar] [CrossRef]
- Yang, X.Y.; Haleem, N.; Osabutey, A.; Cen, Z.; Albert, K.L.; Autenrieth, D. Particulate Matter in Swine Barns: A Comprehensive Review. Atmosphere 2022, 13, 490. [Google Scholar] [CrossRef]
- Sun, T.; Zhang, Y.S.; Pang, B.; Dong, C.H.; Yang, M.; Xia, Y. Engineered Nanoparticles for Drug Delivery in Cancer Therapy. Angew. Chem. 2014, 53, 12320–12364. [Google Scholar] [CrossRef]
- Babamiri, A.; Ahookhosh, K.; Abdollahi, H.; Taheri, M.H.; Cui, X.; Nabaei, M.; Farnoud, A. Effect of laryngeal jet on dry powder inhaler aerosol deposition: A numerical simulation. Comput. Methods Biomech. Biomed. Eng. 2023, 26, 1859–1874. [Google Scholar] [CrossRef]
- Zhou, Y.; Cheng, Y.S. Particle deposition in a cast of human tracheobronchial airways. Aerosol Sci. Technol. 2005, 39, 492–500. [Google Scholar] [CrossRef]
- Faizal, W.M.; Ghazali, N.N.N.; Khor, C.Y.; Badruddin, I.A.; Zainon, M.Z.; Yazid, A.A.; Ibrahim, N.B.; Razi, R.M. Computational fluid dynamics modelling of human upper airway: A review. Comput. Methods Programs Biomed. 2020, 196, 105627. [Google Scholar] [CrossRef] [PubMed]
- Sittitavornwong, S.; Waite, P.D.; Shih, A.M.; Cheng, G.C.; Koomullil, R.; Ito, Y.; Cure, J.K.; Harding, S.M.; Litaker, M. Computational fluid dynamic analysis of the posterior airway space after maxillomandibular advancement for obstructive sleep apnea syndrome. J. Oral Maxillofac. Surg. 2013, 71, 1397–1405. [Google Scholar] [CrossRef] [PubMed]
- Inthavong, K.; Choi, L.-T.; Tu, J.; Ding, S.; Thien, F. Micron particle deposition in a tracheobronchial airway model under different breathing conditions. Med. Eng. Phys. 2010, 32, 1198–1212. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.S.; Larpruenrudee, P.; Paul, A.R.; Paul, G.; Gemci, T.; Gu, Y.; Saha, S.C. SARS CoV-2 aerosol: How far it can travel to the lower airways? Phys. Fluids 2021, 33, 061903. [Google Scholar] [CrossRef]
- Phuong, N.L.; Yamashita, M.; Yoo, S.J.; Ito, K. Prediction of convective heat transfer coefficient of human upper and lower airway surfaces in steady and unsteady breathing conditions. Build. Environ. 2016, 100, 172–185. [Google Scholar] [CrossRef]
- Corcoran, T.E. New path for understanding mucociliary clearance. Thorax 2024, 79, 597–598. [Google Scholar] [CrossRef]
- Dai, X.; Xu, R.; Li, N. The Interplay between Airway Cilia and Coronavirus Infection, Implications for Prevention and Control of Airway Viral Infections. Cells 2024, 13, 1353. [Google Scholar] [CrossRef]


| Value | Unit | |
|---|---|---|
| Particle type | Droplet | - |
| Volatile mass fraction | 92 | % |
| Injection type | Surface injection | - |
| Particle initial velocity | 0 | m/s |
| Particle initial temperature | 23 | °C |
| Density | 1000 | kg/m3 |
| Mass flow rate | 1 × 10−12 | kg/s |
| Particle diameter | 0.1, 1.0, 2.5, 5.0 10.0, 20.0 | μm |
| Name | Type/Manufacturer | Unit | Resolution | Image |
|---|---|---|---|---|
| 3D-printed 1:1 respiratory tract model | Acrylonitrile Butadiene Styrene (ABS) | - | - | 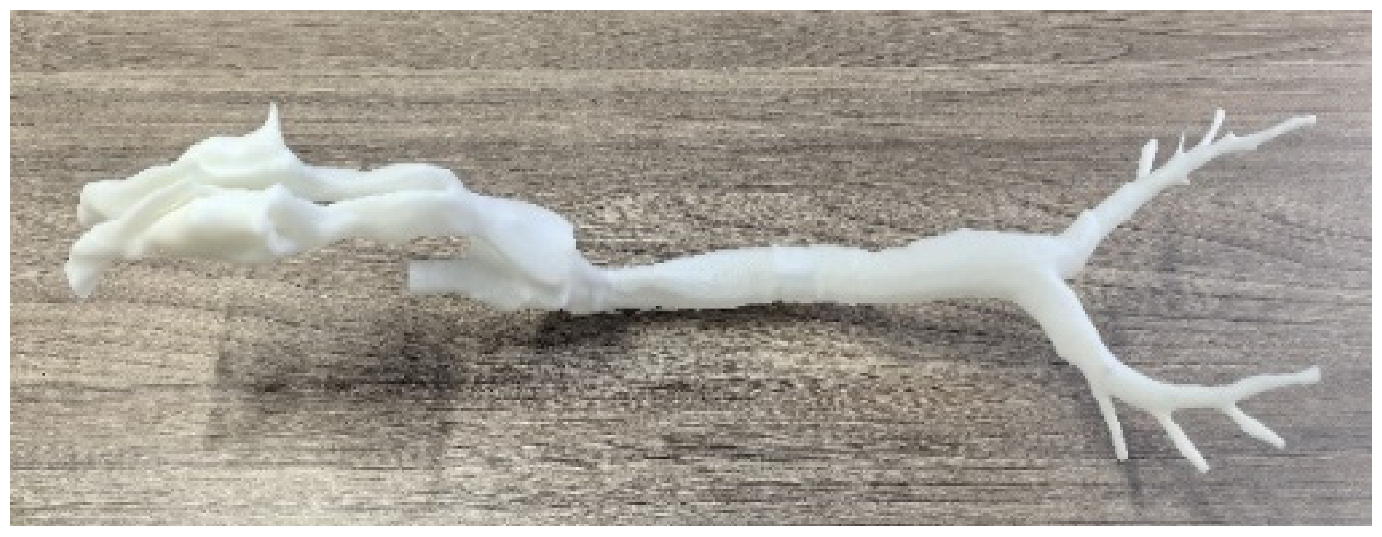 |
| Air pump | Quick Take 30, SKC, Eighty Four, PA, USA | L/min | 0.01 |  |
| Flow meter | 4000 Series, TSI, Shoreview, MN, USA | L/min | 0.01 |  |
| Pressure meter | Testo 510, Titisee-Neustadt, Baden-Württemberg, Germany | Pa | 1.0 |  |
| Regional DF | D = 0.1 μm | D = 1.0 μm | D = 2.5 μm | D = 5.0 μm | D = 10.0 μm |
|---|---|---|---|---|---|
| L1 | 0.11% | 0.10% | 0.10% | 0.09% | 0.25% |
| L2 | 0.14% | 0.15% | 0.15% | 0.17% | 0.38% |
| L3 | 0.16% | 0.16% | 0.16% | 0.18% | 0.43% |
| L4 | 0.12% | 0.13% | 0.14% | 0.15% | 0.33% |
| L5 | 0.16% | 0.16% | 0.16% | 0.17% | 0.39% |
| L6 | 0.10% | 0.11% | 0.12% | 0.13% | 0.22% |
| L7 | 0.18% | 0.19% | 0.19% | 0.22% | 0.63% |
| R1 | 0.16% | 0.16% | 0.17% | 0.17% | 0.44% |
| R2 | 0.17% | 0.18% | 0.19% | 0.22% | 0.56% |
| R3 | 0.17% | 0.17% | 0.17% | 0.19% | 0.52% |
| R4 | 0.11% | 0.12% | 0.13% | 0.15% | 0.40% |
| R5 | 0.19% | 0.19% | 0.19% | 0.18% | 0.31% |
| L/R ratio | 1.21 | 1.22 | 1.20 | 1.22 | 1.18 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Du, L.; Qiu, M.; Zhang, Z.; Hu, C.; Yang, L.; Xiong, Z.; Wang, J.; Xiong, X.; Peng, H.; Chen, J.; et al. Aerosol Dynamics in the Respiratory Tract of Food-Producing Animals: An Insight into Transmission Patterns and Deposition Distribution. Animals 2025, 15, 1396. https://doi.org/10.3390/ani15101396
Du L, Qiu M, Zhang Z, Hu C, Yang L, Xiong Z, Wang J, Xiong X, Peng H, Chen J, et al. Aerosol Dynamics in the Respiratory Tract of Food-Producing Animals: An Insight into Transmission Patterns and Deposition Distribution. Animals. 2025; 15(10):1396. https://doi.org/10.3390/ani15101396
Chicago/Turabian StyleDu, Longhuan, Mohan Qiu, Zengrong Zhang, Chenming Hu, Li Yang, Zhuxiang Xiong, Jiangxian Wang, Xia Xiong, Han Peng, Jialei Chen, and et al. 2025. "Aerosol Dynamics in the Respiratory Tract of Food-Producing Animals: An Insight into Transmission Patterns and Deposition Distribution" Animals 15, no. 10: 1396. https://doi.org/10.3390/ani15101396
APA StyleDu, L., Qiu, M., Zhang, Z., Hu, C., Yang, L., Xiong, Z., Wang, J., Xiong, X., Peng, H., Chen, J., Zhu, S., Song, X., Yu, C., & Yang, C. (2025). Aerosol Dynamics in the Respiratory Tract of Food-Producing Animals: An Insight into Transmission Patterns and Deposition Distribution. Animals, 15(10), 1396. https://doi.org/10.3390/ani15101396






