Efficacy of Preemptive Analgesia with Amantadine for Controlling Postoperative Pain in Cats Undergoing Ovariohysterectomy
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals and Ethical Considerations
2.2. Experimental Groups and Anesthetic–Surgical Protocol
2.3. Intraoperative Evaluation of Physiological Parameters
2.4. Pain Assessment
2.5. Rescue Analgesia
2.6. Postsurgical Therapy
2.7. Statistical Analysis
3. Results
3.1. Assessment of the Physiological Parameters
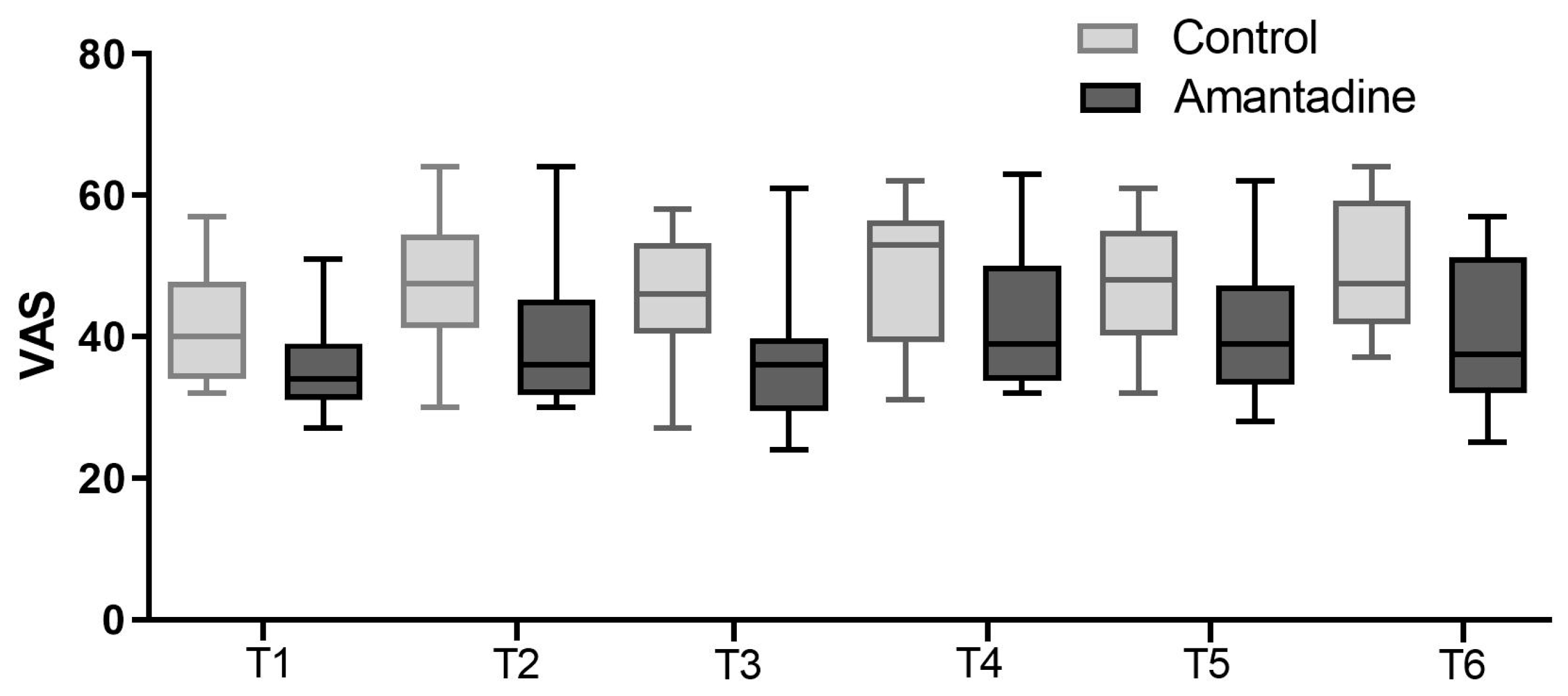
3.2. Pain Assessment
3.3. Rescue Analgesics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Williams, A.C.C.; Craig, K.D. Updating the definition of pain. Pain 2016, 11, 2420–2423. [Google Scholar] [CrossRef] [PubMed]
- Bell, A. The neurobiology of acute pain. Vet. J. 2018, 237, 55–62. [Google Scholar] [CrossRef]
- Tracey, W.D., Jr. Nociception. Curr. Biol. 2017, 27, 129–133. [Google Scholar] [CrossRef] [PubMed]
- Binder, C.; Reifinger, M.; Aurich, J.; Aurich, C. Histopathological findings in the uteri and ovaries of clinically healthy cats presented for routine spaying. J. Feline Med. Surg. 2021, 8, 770–776. [Google Scholar] [CrossRef]
- Lui, J.F.; Toniollo, G.H.; Savi, P.A.P.; Voorwald, F.A.; Silva, M.A.M.; Tosta, P.A. Esterilização cirúrgica de caninos e felinos em Jaboticabal. Interação entre o benefício social e a pesquisa científica. Rev. Ciência Extensão 2011, 7, 29–40. [Google Scholar]
- Misk, T.N.; El-Sherry, T.M. Pyometra in cats: Medical Versus Surgical Treatment. J. Vet. Res. 2020, 2, 86–92. [Google Scholar] [CrossRef]
- Carneiro, B.P.B.; Ribeiro, J.J.; Almeida, J.M.S.; Lima, A.; Kuhn, J.L.; Queiroz, S.S. Ovariosalpingohisterectomia em gata com cisto ovariano—Relato de caso. Sci. Rural. 2019, 1, 1–6. [Google Scholar]
- Prado, M.E.; Apel, T.L.; Augusto, I.L.; Manieri, A.F.; Fracácio, C.P.; Barros, F.S.; Jark, P.C. Levantamento do uso e riscos terapêuticos de anticoncepcionais em cadelas e gatas. Ars. Vet. 2020, 36, 52–58. [Google Scholar] [CrossRef]
- Sattasathuchana, P.; Phuwapattanachart, P.; Thengchaisri, N. Comparison of post-operative analgesic efficacy of tolfenamic acid and robenacoxib in ovariohysterectomized cats. J. Vet. Med. Sci. 2018, 6, 989–996. [Google Scholar] [CrossRef]
- Steagall, P.V.M.; Simon, B.T.; Teixeira Neto, F.J.; Luna, S.P.L. An update on drugs used for lumbosacral epidural anesthesia and analgesia in dogs. Front. Vet. Sci. 2017, 4, 68. [Google Scholar] [CrossRef]
- Niella, R.V.; Sena, A.S.; Corrêa, J.M.X.; Soares, P.C.L.R.; Pinto, T.M.; Junior, A.C.S.; Costa, B.A.; de Oliveira, J.N.S.; da Silva, E.B.; de Lavor, M.S.L. Preemptive effect of amantadine as adjuvant in postoperative analgesia of ovaryhisterectomy in dogs. Res. Soc. Dev. 2020, 9, e68091110128. [Google Scholar] [CrossRef]
- Carapeba, G.d.O.; Nicácio, I.P.G.A.; Stelle, A.B.F.; Bruno, T.S.; Nicácio, G.M.; Júnior, J.S.C.; Giuffrida, R.; Neto, F.J.T.; Cassu, R.N. Comparison of perioperative analgesia using the infiltration of the surgical site with ropivacaine alone and in combination with meloxicam in cats undergoing ovariohysterectomy. BMC Vet. Res. 2020, 16, 88. [Google Scholar] [CrossRef]
- Diep, T.N.; Monteiro, B.P.; Evangelista, M.C.; Balleydier, A.; Watanabe, R.; Ruel, H.L.M.; Doodnaught, G.M.; Le Quang, T.; Steagall, P.V. Anesthetic and analgesic effects of an opioid-free, injectable protocol in cats undergoing ovariohysterectomy: A prospective, blinded, randomized clinical trial. Can. Vet. J. 2020, 61, 621–628. [Google Scholar]
- Pereira, M.A.A.; Gonçalves, L.A.; Evangelista, M.C.; Thurler, R.S.; Campos, K.D.; Formenton, M.R.; Patricio, G.C.F.; Matera, J.M.; Ambrósio, A.M.; Fantoni, D.T. Postoperative pain and short-term complications after two elective sterilization techniques: Ovariohysterectomy or ovariectomy in cats. BMC Vet. Res. 2018, 14, 335. [Google Scholar] [CrossRef] [PubMed]
- McKune, C.M.; Murrell, J.C.; Nolan, A.M.; White, K.L.; Wright, B.D. Nociception and Pain. In Veterinary Anesthesia and Analgesia: The Fifth Edition of Lumb & Jones, 5th ed.; Grimm, K., Lamont, L., Tranquilli, W., Greene, S., Robertson, S., Eds.; Wiley Blackwell: Hoboken, NJ, USA, 2015; pp. 584–623. [Google Scholar]
- Blanpied, T.A.; Clarke, R.J.; Johnson, J.W. Amantadine inhibits NMDA receptors by accelerating channel closure during channel block. J. Neurosci. 2005, 13, 3312–3322. [Google Scholar] [CrossRef]
- Madden, M.; Gurney, M.; Bright, S. Amantadine, an N-Methyl-D-Aspartate antagonist, for treatment of chronic neuropathic pain in a dog. Vet. Anaesth. Analg. 2014, 4, 440–441. [Google Scholar] [CrossRef]
- Shipley, H.; Flynn, K.; Tucker, L.; Wendt-Hornickle, E.; Baldo, C.; Almeida, D.; Allweiler, S.; Guedes, A. Owner evaluation of quality of life and mobility in osteoarthritic catstreated with amantadine or placebo. J. Feline Med. Surg. 2020, 23, 568–574. [Google Scholar] [CrossRef]
- Snijdelaar, D.G.; Koren, G.; Katz, J. Effects of perioperative oral amantadine on postoperative pain and morphine consumption in patients after radical prostatectomy: Results of a preliminary study. Anesthesiology 2004, 1, 134–141. [Google Scholar] [CrossRef]
- Aiyer, R.; Mehta, N.; Gungor, S.; Gulati, A. A systematic review of NMDA receptor antagonists for treatment of neuropathic pain in clinical practice. Clin. J. Pain 2018, 5, 450–467. [Google Scholar] [CrossRef]
- Lascelles, B.D.; Gaynor, J.; Smith, E.S. Evaluation of amantadine as part of a multimodal analgesic regimen for the alleviation of refractory canine osteoarthritis pain. J. Vet. Intern. Med. 2008, 22, 53–59. [Google Scholar] [CrossRef]
- Mitch, P.M.; Hellyer, P.W. Métodos objetivos e categóricos para avaliar a dor e a analgesia. In Manual do Controle da dor em Medicina Veterinária, 2nd ed.; Gaynor, J.S., Muir, W.W., III, Eds.; MedVet: São Paulo, Brazil, 2009; pp. 78–109. [Google Scholar]
- Brondani, J.T.; Luna, S.P.L.; Minto, B.W.; Santos, B.P.R.; Beier, S.l.L.; Marsubara, L.M.; Padovani, C. Validade e responsividade de uma escala multidimensional para avaliação de dor pós-operatória em gatos. Arq. Bras. Med. Veterinária E Zootec. 2012, 64, 529–538. [Google Scholar] [CrossRef][Green Version]
- Slingsby, L.S.; Waterman-Pearson, A.E. Postoperative analgesia in the cat after ovariohysterectomy by use of carprofen, ketoprofen, meloxicam or tolfenamic acid. J. Small Anim. Pract. 2000, 41, 447–450. [Google Scholar] [CrossRef] [PubMed]
- Cochran, W.G. Sampling Techniques, 3rd ed.; John Wiley & Sons: New York, NY, USA, 1977; pp. 447–450. [Google Scholar]
- Siao, K.T.; Pypendop, B.H.; Stanley, S.D.; Ilkiw, J.E. Pharmacokinetics of amantadine in cats. J. Vet. Pharmacol. Ther. 2011, 34, 599–604. [Google Scholar] [CrossRef] [PubMed]
- Ong, C.K.; Lirk, P.; Seymour, R.A.; Jenkins, B.J. The efficacy of preemptive analgesia for acute postoperative pain management: A meta-analysis. Anesth. Analg. 2005, 3, 757–773. [Google Scholar] [CrossRef] [PubMed]
- Garcia, J.B.S.; Issy, A.M.; Sakata, R.K. Preemptive analgesia. Rev. Bras. Anestesiol. 2001, 51, 448–463. [Google Scholar] [CrossRef][Green Version]
- Galloway, D.S.; Ko, J.; Mandsager, R.E.; Reaugh, H.F.; Payton, M.E.; Portillo, E. Comparison of sevoflurane and isoflurane anesthetic index in unpremedicated dogs. Vet. Anaesth. Analg. 2003, 30, 103–104. [Google Scholar] [CrossRef] [PubMed]
- Abdelmawgound, A.; Rashwan, S. Effect of preoperative oral amantadine on intraoperative anesthetic and analgesic requirements in female patients during abdominoplasty. Egypt. J. Anaesth. 2013, 29, 7–11. [Google Scholar] [CrossRef][Green Version]
- Haskins, S.C. Monitoring anesthetized pacients. In Veterinary Anesthesia and Analgesia, 4th ed.; Tranquilli, W.J., Thurmon, J.C., Grimm, K.A., Eds.; Lumb & Jones; Blackwell Publishing: Hoboken, NJ, USA, 2007; pp. 533–560. [Google Scholar]
- Paepe, D.; Verjans, G.; Duchateau, L.; Piron, K.; Ghys, L.; Daminet, S. Routine health screening: Findings in apparently healthy middle-aged and old cats. J. Feline Med. Surg. 2013, 15, 8–19. [Google Scholar] [CrossRef]
- Silva, R.B.; Fuchs, T.; Galante, R.; Rodigheri, S.M. Analgesic effect of epidural administration of morphine and methadone with lidocaine in bitches submitted to ovariosalpingohisterectomy. Arc. Vet. Sci. 2016, 21, 86–99. [Google Scholar]
- Garcia, C.; Borges, I.S.; Padilha, V.S.; Valau, A.; Vargas, D. Avaliação do efeito analgésico do maropitant em gatas submetidas à ovariohisterectomia eletiva. Pubvet 2021, 15, 168. [Google Scholar] [CrossRef]
- Selmi, A.L.; Figueiredo, J.P.; Mendes, G.M.; Lavor, L.M.S.; Machado, P.M.L. Infusão contínua de propofol em gatos pré-medicados com cetamina-midazolam. Arq. Bras. Med. Vet. E Zootec. 2005, 57, 295–299. [Google Scholar] [CrossRef][Green Version]
- Grubb, T.; Sager, J.; Gaynor, J.S.; Montgomery, E.; Parker, J.A.; Shafford, H.; Tearney, C. AAHA Anesthesia and monitoring guidelines for dogs and cats. J. Am. Hosp. Assoc. 2020, 56, 59–82. [Google Scholar] [CrossRef] [PubMed]
- Nunes, N.; Pompermayer, L.G.; Pirolo, J. Emprego do metaraminol no bloqueio da hipotensão induzida pela levomepromazina em cães. Braz. J. Vet. Res. Anim. Sci. 1995, 32, 120–124. [Google Scholar] [CrossRef][Green Version]
- Short, C.E.; Bufalari, A. Propofol anesthesia. Vet. Clin. N. Am. Small Anim. Pract. 1999, 29, 747–778. [Google Scholar] [CrossRef] [PubMed]
- Elmawgood, A.A.; Rashwan, S.; Rashwan, D. Tourniquet-induced cardiovascular responses in anterior cruciate ligament reconstruction surgery under general anesthesia: Effect of reoperative oral amantadine. Egypt J. Anaesth. 2015, 31, 29–33. [Google Scholar] [CrossRef]
- Mata-Bermudez, A.; Ríos, C.; Burelo, M.; Pérez-González, C.; García-Martínez, B.A.; Jardon-Guadarrama, G.; Calderón-Estrella, F.; Manning-Balpuesta, N.; Diaz-Ruiz, A. Amantadine prevented hypersensitivity and decreased oxidative stress by NMDA receptor antagonism after spinal cord injury in rats. Eur. J. Pain 2021, 25, 1839–1851. [Google Scholar] [CrossRef]
- Gruen, M.E.; Lascelles, B.B.D.X.; Colleran, E.; Gottlieb, A.; Johnson, J.; Lotsikas, P.; Marcellin-Little, D.; Wright, B. 2022 AAHA Pain management guidelines for dogs and cats. J. Am. Anim. Hosp. Assoc. 2022, 58, 55–76. [Google Scholar] [CrossRef]

| Variables | C | A |
|---|---|---|
| Weight (kg) | 2.8 ± 0.44 | 2.7 ± 0.38 |
| Dose of Propofol (mg/kg) | 5.2 ± 0.63 | 5.6 ± 1.24 |
| Surgery time (min) | 25.3 ± 4.27 | 24.6 ± 1.17 |
| Extubation time (min) | 7.2 ± 1.32 | 7 ± 1.33 |
| Variables | Groups | M0 | M1 | M2 | M3 | M4 | M5 | M6 | M7 |
|---|---|---|---|---|---|---|---|---|---|
| HR (bpm) | C | 209 ± 4.87 | 157 ± 5.70 | 153 ± 7.05 | 192 ± 9.13 | 184 ± 9.59 | 173 ± 8.02 | 163 ± 122.5 | 163 ± 7.43 |
| A | 205 ± 5.84 | 154 ± 5.95 | 145 ± 8.76 | 170 ± 8.68 | 175 ± 7.23 | 167 ± 6.53 | 162 ± 5.80 | 158 ± 7.42 | |
| RR(rpm) | C | 63 ± 2.42 | 25 ± 1.97 | 26 ± 3.02 | 29 ± 3.04 | 29 ± 3.26 | 29 ± 3.02 | 25 ± 3.31 | 24 ± 2.62 |
| A | 61 ± 1.52 | 22 ± 2.05 | 20 ± 3.04 | 21 ± 2.85 | 22 ± 3.17 | 21 ± 3.44 | 19 ± 2.51 | 21 ± 2.92 | |
| SpO2 (%) | C | - | 98.3 ± 0.59 | 98.4 ± 0.61 | 99.1 ± 0.50 | 98.8 ± 0.48 | 98.9 ± 0.52 | 99.2 ± 0.48 | 99.7 ± 0.15 |
| A | - | 98.8 ± 0.51 | 98.3 ± 0.71 | 99.5 ± 0.22 | 99 ± 0.25 | 98.7 ± 0.42 | 98.8 ± 0.61 | 98.5 ± 0.67 | |
| ETCO2 | C | - | 32.0 ± 2.74 | 30.6 ± 2.61 | 31.4 ± 1.99 | 34.2 ± 2.1 | 34.4 ± 2.00 | 34.8 ± 2.07 | 31.4 ± 2.17 |
| A | - | 32.6 ± 1.99 | 36 ± 2.38 | 39.6 ± 2.38 | 40.8 ± 2.49 | 39.8 ± 2.49 | 36.8 ± 2.25 | 38.8 ± 2.93 | |
| Etiso(%) | C | - | 1.43 ± 0.08 | 1.32 ± 0.06 | 1.39 ± 0.08 | 1.46 ± 0.07 | 1.48 ± 0.12 | 1.27 ± 0.07 | 0.71 ± 0.08 |
| A | - | 1.43 ± 0.04 | 1.36 ± 0.06 | 1.33 ± 0.04 | 1.35 ± 0.05 | 1.4 ± 0.06 | 1.29 ± 0.06 | 0.79 ± 0.05 | |
| T(°C) | C | 38.67 ± 0.10 | 37.86 ± 0.17 | 37.43 ± 0.19 | 37.15 ± 0.20 | 36.9 ± 0.22 | 36.71 ± 0.26 | 36.52 ± 0.27 | 36.32 ± 1.33 |
| A | 38.66 ± 0.07 | 37.55 ± 0.16 | 37.09 ± 0.15 | 36.93 ± 0.14 | 36.65 ± 0.20 | 36.45 ± 0.27 | 36.22 ± 1.36 | 35.95 ± 1.40 | |
| SBP (mmHg) | C | - | 65.02 ± 3.32 | 79.1 ± 5.53 | 112.5 ± 14.17 | 121.4 ± 11.22 | 99.1 ± 5.33 | 93.4 ± 4.53 | 99.8 ± 2.23 |
| A | - | 80 ± 6.29 | 83.3 ± 5.00 | 114.9 ± 11.88 | 126.4 ± 11.29 | 106.4 ± 8.01 | 96.9 ± 7.01 | 107.3 ± 11.07 |
| T1 | T2 | T3 | T4 | T5 | T6 | Total | |
|---|---|---|---|---|---|---|---|
| C | 2 | 4 | 0 | 1 | 1 | 0 | 8/10 (80%) * |
| A | 0 | 3 | 0 | 1 | 0 | 0 | 4/10 (40%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guedes, P.E.B.; Pinto, T.M.; Corrêa, J.M.X.; Niella, R.V.; dos Anjos, C.M.; de Oliveira, J.N.S.; Marques, C.S.d.C.; de Souza, S.S.; da Silva, E.B.; de Lavor, M.S.L. Efficacy of Preemptive Analgesia with Amantadine for Controlling Postoperative Pain in Cats Undergoing Ovariohysterectomy. Animals 2024, 14, 643. https://doi.org/10.3390/ani14040643
Guedes PEB, Pinto TM, Corrêa JMX, Niella RV, dos Anjos CM, de Oliveira JNS, Marques CSdC, de Souza SS, da Silva EB, de Lavor MSL. Efficacy of Preemptive Analgesia with Amantadine for Controlling Postoperative Pain in Cats Undergoing Ovariohysterectomy. Animals. 2024; 14(4):643. https://doi.org/10.3390/ani14040643
Chicago/Turabian StyleGuedes, Paula Elisa Brandão, Taísa Miranda Pinto, Janaína Maria Xavier Corrêa, Raquel Vieira Niella, Carolina Moreira dos Anjos, Jéssica Natália Silva de Oliveira, Claire Souza da Costa Marques, Sophia Saraiva de Souza, Elisângela Barboza da Silva, and Mário Sérgio Lima de Lavor. 2024. "Efficacy of Preemptive Analgesia with Amantadine for Controlling Postoperative Pain in Cats Undergoing Ovariohysterectomy" Animals 14, no. 4: 643. https://doi.org/10.3390/ani14040643
APA StyleGuedes, P. E. B., Pinto, T. M., Corrêa, J. M. X., Niella, R. V., dos Anjos, C. M., de Oliveira, J. N. S., Marques, C. S. d. C., de Souza, S. S., da Silva, E. B., & de Lavor, M. S. L. (2024). Efficacy of Preemptive Analgesia with Amantadine for Controlling Postoperative Pain in Cats Undergoing Ovariohysterectomy. Animals, 14(4), 643. https://doi.org/10.3390/ani14040643






