Bacterial Contamination of Equine Dentistry Equipment—Effect of Cleaning and Disinfection
Abstract
Simple Summary
Abstract
1. Introduction
- (1)
- assessing the bacterial load on handpieces and the patient environment during equine dental care;
- (2)
- assessing if manual cleaning of handpieces with detergent or disinfection with surface disinfection is sufficient to meet the Swedish criteria for high-level disinfected equipment; and
- (3)
- determining the bacterial load on the immediate surroundings after surface disinfection, or cleaning followed by surface disinfection.
2. Materials and Methods
2.1. Sampling
2.2. Cleaning and Disinfecting Methods
2.3. Bacteriological Analyses
2.4. Data Management
3. Results
3.1. Handpieces
3.2. Dummies
3.3. Head Support
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
References
- Pusterla, N.; Rice, M.; Henry, T.; Barnum, S.; James, K. Investigation of the Shedding of Selected Respiratory Pathogens in Healthy Horses Presented for Routine Dental Care. J. Vet. Dent. 2020, 37, 88–93. [Google Scholar] [CrossRef]
- Lewis, D.L.; Boe, R.K. Cross-infection risks associated with current procedures for using high-speed dental handpieces. J. Clin. Microbiol. 1992, 30, 401–406. [Google Scholar] [CrossRef]
- Smith, G.; Smith, A. Microbial contamination of used dental handpieces. Am. J. Infect. Control. 2014, 42, 1019–1021. [Google Scholar] [CrossRef] [PubMed]
- Murali, S.; Madhulaxmi, M.; Muthuseka, M.R. To Evaluate Bacterial Contamination of Surgical Handpiece Used in Minor Oral Surgical Procedures in Dentistry. J. Evol. Med Dent. Sci. 2020, 9, 3463. [Google Scholar] [CrossRef]
- Herd, S.; Chin, J.; Palenik, C.J.; Ofner, S. The in vivo contamination of air-driven low-speed handpieces with prophylaxis angles. J. Am. Dent. Assoc. 2007, 138, 1360–1365. [Google Scholar] [CrossRef][Green Version]
- Innes, N.; Johnson, I.; Al-Yaseen, W.; Harris, R.; Jones, R.; Kc, S.; McGregor, S.; Robertson, M.; Wade, W.; Gallagher, J. A systematic review of droplet and aerosol generation in dentistry. J. Dent. 2021, 105, 103556-103556. [Google Scholar] [CrossRef] [PubMed]
- Ionescu, A.; Cagetti, M.G.; Ferracane, J.L.; Garcia-Godoy, F.; Brambilla, E. Topographic aspects of airborne contamination caused by the use of dental handpieces in the operative environment. J. Am. Dent. Assoc. 2020, 151, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Kohn, W.G.; Collins, A.S.; Cleveland, J.L.; Harte, J.A.; Eklund, K.J.; Malvitz, D.M. Guidelines for infection control in dental health-care settings—2003. MMWR. Recomm. Rep. 2003, 52, 1–61. [Google Scholar]
- Andersson, Y.; Bolle, A.-C.; Göransson, Å.; Jakobsson, C.; Skott, P.; Spencer, I. Riktlinjer för Vårdhygien Inom Svensk Tandvård [Guidelines for Infection Prevention and Control in Swedish Dentistry]. Available online: https://s3-eu-west-1.amazonaws.com/static.wm3.se/sites/16/media/281961_HOBIT_final_version_f%C3%B6r_publicering.pdf?1556447135 (accessed on 24 March 2021).
- The Swedish Veterinary Association and the Equine Section of the Committee for Veterinary Medicine. Infektionskontroll Inom Hästsjukvård [Infection Prevention and Control in Equine Healthcare]. Available online: https://svf.se/media/10mbpucp/infektionskontroll_inom_hastsjukvard.pdf (accessed on 28 June 2021).
- Terpak, C.H.; Verstraete, F.J.M. Instrumentation, Patient positioning, and aseptic technique. In Oral and Maxillofacial Surgery in Dogs and Cats; Verstraete, F.J.M., Lomer, M.J., Eds.; Saunders Elsvier: St. Louis, MO, USA, 2012; pp. 55–68. [Google Scholar]
- Pinto, F.M.G.; Bruna, C.Q.D.M.; Camargo, T.C.; Marques, M.; Silva, C.B.; Sasagawa, S.M.; Mimica, L.M.J.; Graziano, K.U. The practice of disinfection of high-speed handpieces with 70% w/v alcohol: An evaluation. Am. J. Infect. Control. 2017, 45, e19–e22. [Google Scholar] [CrossRef]
- Offner, D.; Brisset, L.; Musset, A.-M. Evaluation of the mechanical cleaning efficacy of dental handpieces. J. Hosp. Infect. 2019, 103, e73–e80. [Google Scholar] [CrossRef] [PubMed]
- Winter, S.; Smith, A.; Lappin, D.; McDonagh, G.; Kirk, B. Failure of non-vacuum steam sterilization processes for dental handpieces. J. Hosp. Infect. 2017, 97, 343–347. [Google Scholar] [CrossRef][Green Version]
- Welfare, N.B.O.H.A. Att Förebygga Vårdrelaterade Infektioner -ett Kunskapsunderlag [To Prevent Healthcare Associated Infections—A Basis of Knowledge]; Bergslagens Grafiska: Lindesberg, Sweden, 2006; pp. 304–305. [Google Scholar]
- Swedish Standards Institute (SIS). SS-EN 556-1/AC. Sterilisering av Medicintekniska Produkter—Krav för Märkning Med Symbolen "STERILE"—Del 1: Krav för Medicinska Produkter i Sluten Förpackning [Sterilization of Medical Devices—Requirements for Medical Devices to be Designated ‘STERILE’—Part 1: Requirements for Terminally Sterilized Medical Devices]; Swedish Standards Institute: Stockholm, Sweden, 2006. [Google Scholar]
- European Veterinary Dental College. E.V.D. Equine Training Programmes & Credentialing. Available online: https://www.evdc.org/resources/media/Documents/How_to_become_a_resident/EVDC_Equine_Training_and_Credential_Document.pdf (accessed on 24 March 2021).
- Lundström, T. (Djurtandvårdskliniken, Söderköping, Sweden). Personal communication, 2021. [Google Scholar]
- McDonnell, G.; Burke, P. Disinfection: Is it time to reconsider Spaulding? J. Hosp. Infect. 2011, 78, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Tessi, M.A.; Aríngoli, E.E.; Pirovani, M.E.; Vincenzini, A.Z.; Sabbag, N.G.; Costa, S.C.; García, C.C.; Zannier, M.S.; Silva, E.R.; Moguilevsky, M.A. Microbiological Quality and Safety of Ready-To-Eat Cooked Foods from a Centralized School Kitchen in Argentina. J. Food Prot. 2002, 65, 636–642. [Google Scholar] [CrossRef] [PubMed]
- 3M. Petrifilm Environmental Monitoring Procedures. Available online: https://multimedia.3m.com/mws/media/241111O/environmental-monitoring-procedures-article.pdf (accessed on 15 February 2021).
- Maertens, H.; De Reu, K.; Van Weyenberg, S.; Van Coillie, E.; Meyer, E.; Van Meirhaeghe, H.; Van Immerseel, F.; Vandenbroucke, V.; Vanrobaeys, M.; Dewulf, J. Evaluation of the hygienogram scores and related data obtained after cleaning and disinfection of poultry houses in Flanders during the period 2007 to 2014. Poult. Sci. 2018, 97, 620–627. [Google Scholar] [CrossRef] [PubMed]
- 3M. Interpretation Guide. Available online: https://multimedia.3m.com/mws/media/236194O/petrifilm-aerobic-interpretation-guide.pdf (accessed on 24 May 2021).
- Edwardsson, S.; Bäckman, N. Smittrisker Och Hygien i Tandvården [Risk of Infection and Hygiene in Dentistry]. Available online: http://static.wm3.se/sites/16/media/5627_Smittrisker_och_hygien_i_tandva_u030Arden_120926.pdf?1396533033 (accessed on 24 June 2021).
- Bellows, J.; Berg, M.L.; Dennis, S.; Harvey, R.; Lobprise, H.B.; Snyder, C.J.; Stone, A.E.; Van De Wetering, A.G. 2019 AAHA Dental Care Guidelines for Dogs and Cats. J. Am. Anim. Hosp. Assoc. 2019, 55, 49–69. [Google Scholar] [CrossRef]
- Niemiec, B.; Gawor, J.; Nemec, A.; Clarke, D.; McLeod, K.; Tutt, C.; Gioso, M.; Steagall, P.; Chandler, M.; Morgenegg, G.; et al. World Small Animal Veterinary Association Global Dental Guidelines. J. Small Anim. Pr. 2020, 61, E36-E161. [Google Scholar] [CrossRef]
- Adams, C.E.; Dancer, S.J. Dynamic Transmission of Staphylococcus Aureus in the Intensive Care Unit. Int. J. Environ. Res. Public Health 2020, 17, 2109. [Google Scholar] [CrossRef]
- Griffith, C.; Cooper, R.; Gilmore, J.; Davies, C.; Lewis, M. An evaluation of hospital cleaning regimes and standards. J. Hosp. Infect. 2000, 45, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Lewis, T.; Griffith, C.; Gallo, M.; Weinbren, M. A modified ATP benchmark for evaluating the cleaning of some hospital environmental surfaces. J. Hosp. Infect. 2008, 69, 156–163. [Google Scholar] [CrossRef]
- Pasquarella, C.; Veronesi, L.; Napoli, C.; Castiglia, P.; Liguori, G.; Rizzetto, R.; Torre, I.; Righi, E.; Farruggia, P.; Tesauro, M.; et al. Microbial environmental contamination in Italian dental clinics: A multicenter study yielding recommendations for standardized sampling methods and threshold values. Sci. Total Environ. 2012, 420, 289–299. [Google Scholar] [CrossRef]
- Mulvey, D.; Redding, P.; Robertson, C.; Woodall, C.; Kingsmore, P.; Bedwell, D.; Dancer, S. Finding a benchmark for monitoring hospital cleanliness. J. Hosp. Infect. 2011, 77, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Quinn, P.J.; Markey, B.K.; Leonard, F.C.; FitzPatrick, E.S.; Fanning, S.; Hartigan, P.J. Veterinary Microbiology and Microbial Disease, 2nd ed.; Blackwell Publishing Ltd.: Hoboken, NJ, USA, 2011; p. 211. [Google Scholar]

| Category | Use | Example of Equipment Used in Human Dentistry | Example of Equipment Used in Equine Dentistry | Microbial Definition of Category in Swedish Guidelines in Human Dentistry | Level of Cleaning, Disinfecting, and Sterilizing in Swedish Guidelines in Human Dentistry |
|---|---|---|---|---|---|
| Non-critical | In contact with intact skin | Spatulas | Mouth specula | Visibly clean [9] | Cleaning if not contaminated; if contaminated, cleaning and disinfecting in a washer-disinfector (WD) or manual cleaning followed by chemical disinfecting [9] |
| Semi-critical | In contact with mucus membranes, but not penetrating sterile tissue | Handpieces | Drills, burrs and handpieces used when not penetrating pulp, e.g., decreasing enamel ridges | Free from pathogenic micro- organisms and less than one microorganism on 1000 handpieces [9] | Cleaning and disinfecting in a WD [9] |
| Semi-critical | In contact with mucus membranes, but not penetrating sterile tissue | Compresses | Compresses | Free from pathogenic micro- organisms and occurrence of occasional vital micro- organisms [15] | Cleaning and disinfecting if the equipment is made for reuse |
| Critical | In contact with sterile tissue | Surgical instruments, like extraction forceps | Drills, burrs, handpieces, and other instruments used when penetrating pulp, e.g., endodontic treatments | Free from living micro- organisms/less than one microorganism on 1,000,000 handpieces [15,16] | Cleaning and disinfecting in a WD followed by sterilizing in a B-autoclave [9] |
| Sampling Surface | Sampling Method | Description of Method | Parallel Sampling Method | Description of Parallel Method |
|---|---|---|---|---|
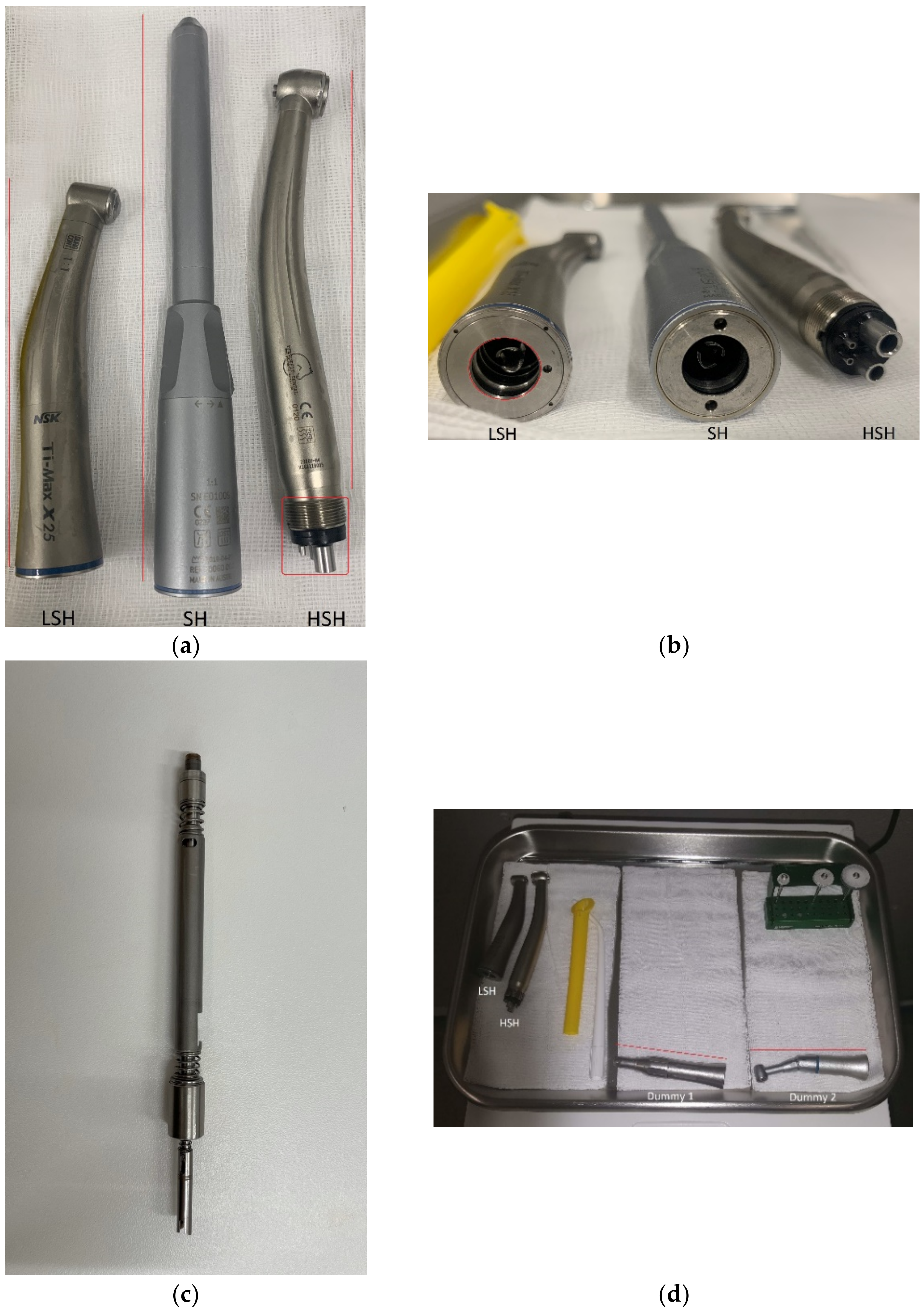
| External surface LSH 1/SH 2/HSH 3/ dummies | Modified swab sampler method (MSS) | Swabbed once, specification of surfaces (see Figure 1) | NA4 | NA |
| Coupling LSH/ dummies | MSS | Swab rotated 360° three times, swabbing possible 0,5 cm into the tunnel (see Figure 1) | NA | NA |
| Shaft SH | MSS | Shaft swabbed once (see Figure 1) | NA | NA |
| Coupling HSH | MSS | Swab rotated 360° three times (see Figure 1) | NA | NA |
| Head support | Swab sampler method [21] | Specified, 10 × 10 cm surface. Swab rubbed three times over area, changing direction, first by 90° then by 45°. | Dip slide | Pressed against surface 15 s, turned and pressed 15 s against an adjacent surface |
| Protocol | Equipment | Cleaning and Disinfecting Substance | Description of Cleaning and Disinfecting Methods |
|---|---|---|---|
| 1 | LSH 1, SH 2, and HSH 3 | LD 4 | Surface disinfection of external surfaces, including external surface of couplings, by rubbing with disinfection wipes (Wet Wipe Triamin Disinfection, Wet Wipes A/S, Vallensbæk, Denmark) until visibly clean for ≥12 s. |
| 2 | Head support | LD+EPT 5/LD+EIT 6 | Surface disinfection by rubbing with disinfection wipes until visibly clean for ≥15-s, followed by spraying a surface disinfectant (Dax 75+, KiiltoClean AB, Täby, Sweden or LiV72+, Clemondo, Helsingborg, Sweden) and rubbing the surface for ≥25 s until dry and thereafter spraying surface disinfectant on the surface to air-dry. |
| 3 | LSH and HSH | SL-11C+L-10 7 | Manual cleaning of external surfaces, including external surface of couplings, by rubbing with cleaning wipes (ICA Städservett, ICA, Solna, Sweden) until visibly clean for ≥12 s. |
| 4 | SH | Standard washing liquid+ SL-11C+L-10 | Dismantling of SH, manual cleaning with a brush (below the water surface) of SH shell and shaft in warm water until visibly clean for ≥30 s. Rinsing in lukewarm-to-warm water and rubbing with a cleaning wipe until visibly clean for ≥12 s. |
| 5 | Head support | SL-11C+L-10 + EPT/EIT | Rubbing with cleaning wipes until visibly clean, for ≥15 s. Followed by spraying a surface disinfectant (Dax 75+, KiiltoClean AB, Täby, Sweden or LiV72+, Clemondo, Helsingborg, Sweden) and rubbing the surface for ≥25 s until dry and thereafter spraying surface disinfectant and left to air-dry. |
| Cleaning or Disinfecting Substance | Type of Handpiece | Pulp Exposure | CFU after Dental Procedure, External Surface | CFU after Cleaning or Disinfecting, External Surface | CFU after Dental Procedure, Coupling or Shaft | CFU after Cleaning or Disinfecting, Coupling or Shaft |
|---|---|---|---|---|---|---|
| LD 1 | SH 3 | NA | NA | 4 7 | NA | 0 7 |
| LD | LSH 4 | NA | NA | 8 7 | NA | 0 7 |
| LD | HSH 5 | NA | NA | 3 7 | NA | 3 7 |
| LD | SH | No exposure | TNTC 6 | 1 | 0 | 1 |
| LD | SH | No exposure | TNTC | 28 | 0 | 0 |
| LD | SH | Risk for exposure | 620 | 0 | 2 | 0 |
| LD | LSH | Risk for exposure | 510 | 1 | 26 | 0 |
| LD | HSH | Risk for exposure | 820 | 1420 | TNTC | 10 |
| LD | SH | Risk for exposure | TNTC | 8 | 1 | 0 |
| LD | LSH | Risk for exposure | 420 | 1260 | 20 | 0 |
| LD | HSH | Risk for exposure | 720 | 70 | TNTC | 520 |
| LD | SH | No exposure | TNTC | 5 | 1 | 0 |
| SL-11C+L-10 2 | SH | NA | NA | 69 7 | NA | 0 7 |
| SL-11C+L-10 | LSH | NA | NA | TNTC 7 | NA | 0 7 |
| SL-11C+L-10 | HSH | NA | NA | 10 7 | NA | 8 7 |
| SL-11C+L-10 | SH | Risk for exposure | TNTC | TNTC | 5 | 0 |
| SL-11C+L-10 | LSH | Risk for exposure | TNTC | 231 | 88 | 0 |
| SL-11C+L-10 | HSH | Risk for exposure | TNTC | TNTC | TNTC | TNTC |
| SL-11C+L-10 | SH | No exposure | TNTC | 160 | 14 | 30 |
| SL-11C+L-10 | SH | No exposure | TNTC | TNTC | 4 | 0 |
| SL-11C+L-10 | SH | Risk for exposure | TNTC | 25 | 0 | 0 |
| SL-11C+L-10 | LSH | Risk for exposure | TNTC | 900 | 520 | 0 |
| SL-11C+L-10 | SH | No exposure | TNTC | 1350 | 0 | 0 |
| Dummy | Cleaning or Disinfection Substance | CFU after Dental Procedure, External Surface | CFU after Cleaning or Disinfection, External Surface | CFU after Cleaning or Disinfection, Couplings |
|---|---|---|---|---|
| 1 | NA | NA | 183 3 | 22 3 |
| 1 | LD 1 | TNTC | 1 | 0 |
| 1 | LD | 1340 | 18 | 3 |
| 1 | LD | 0 | 0 | 0 |
| 1 | LD | 67 | 0 | 0 |
| 1 | LD | 82 | 0 | 0 |
| 1 | LD | 1100 | 8 | 0 |
| 1 | LD | NA | 440 3 | 1 3 |
| 2 | NA | NA | 267 3 | 0 3 |
| 1 | SL-11C+L-10 2 | TNTC | 0 | 0 |
| 1 | SL-11C+L-10 | 330 | 2 | 1 |
| 1 | SL-11C+L-10 | 87 | 1 | 0 |
| 1 | SL-11C+L-10 | 18 | 0 | 0 |
| 1 | SL-11C+L-10 | 35 | 0 | 0 |
| 2 | NA | TNTC | NA | NA |
| Cleaning and Disinfecting Substances | Bacterial Load after Dental Procedure | Bacterial Load after Cleaning and/or Disinfecting | ||||
|---|---|---|---|---|---|---|
| Petrifilm TM | Dip Slide TSA + Neutralizer | Dip Slide TSA | Petrifilm TM | Dip Slide TSA + Neutralizer | Dip Slide TSA | |
| LD1+EPT2/LD+EIT 3 | NA | NA | NA | 0.03 5 | 0.11 5 | 0 5 |
| LD+EPT/LD+EIT | TNTC | 7.23 | TNTC | 3 | 0.11 | 0.96 |
| LD+EPT/LD+EIT | TNTC | TNTC | TNTC | 0.04 | 0.11 | 0 |
| LD+EPT/LD+EIT | TNTC | TNTC | TNTC | 0.07 | 0 | 0 |
| LD+EPT/LD+EIT | TNTC | 5.32 | 9.89 | 0.06 | 0 | 0.11 |
| LD+EPT/LD+EIT | TNTC | 1.49 | 6.38 | 0 | 0 | 0 |
| LD+EPT/LD+EIT | TNTC | TNTC | TNTC | 0.01 | 0 | 0.85 |
| SL-11C+L-10 4 + EPT/EIT | NA | NA | NA | TNTC 5 | NA | NA |
| SL-11C+L-10 + EPT/EIT | TNTC | NA | NA | 1.45 | NA | NA |
| SL-11C+L-10 + EPT/EIT | TNTC | NA | NA | 0.10 | NA | NA |
| SL-11C+L-10 + EPT/EIT | TNTC | NA | NA | TNTC | NA | NA |
| SL-11C+L-10 + EPT/EIT | TNTC | NA | NA | 0 | NA | NA |
| SL-11C+L-10 + EPT/EIT | TNTC | NA | NA | 0.73 | NA | NA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alsing-Johansson, T.; Pedersen, A.; Bergström, K.; Sternberg-Lewerin, S.; Penell, J.; Bergh, A. Bacterial Contamination of Equine Dentistry Equipment—Effect of Cleaning and Disinfection. Animals 2021, 11, 2320. https://doi.org/10.3390/ani11082320
Alsing-Johansson T, Pedersen A, Bergström K, Sternberg-Lewerin S, Penell J, Bergh A. Bacterial Contamination of Equine Dentistry Equipment—Effect of Cleaning and Disinfection. Animals. 2021; 11(8):2320. https://doi.org/10.3390/ani11082320
Chicago/Turabian StyleAlsing-Johansson, Todd, Anja Pedersen, Karin Bergström, Susanna Sternberg-Lewerin, Johanna Penell, and Anna Bergh. 2021. "Bacterial Contamination of Equine Dentistry Equipment—Effect of Cleaning and Disinfection" Animals 11, no. 8: 2320. https://doi.org/10.3390/ani11082320
APA StyleAlsing-Johansson, T., Pedersen, A., Bergström, K., Sternberg-Lewerin, S., Penell, J., & Bergh, A. (2021). Bacterial Contamination of Equine Dentistry Equipment—Effect of Cleaning and Disinfection. Animals, 11(8), 2320. https://doi.org/10.3390/ani11082320






