First Report of Anthelmintic Resistance in Gastrointestinal Nematodes in Goats in Romania
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
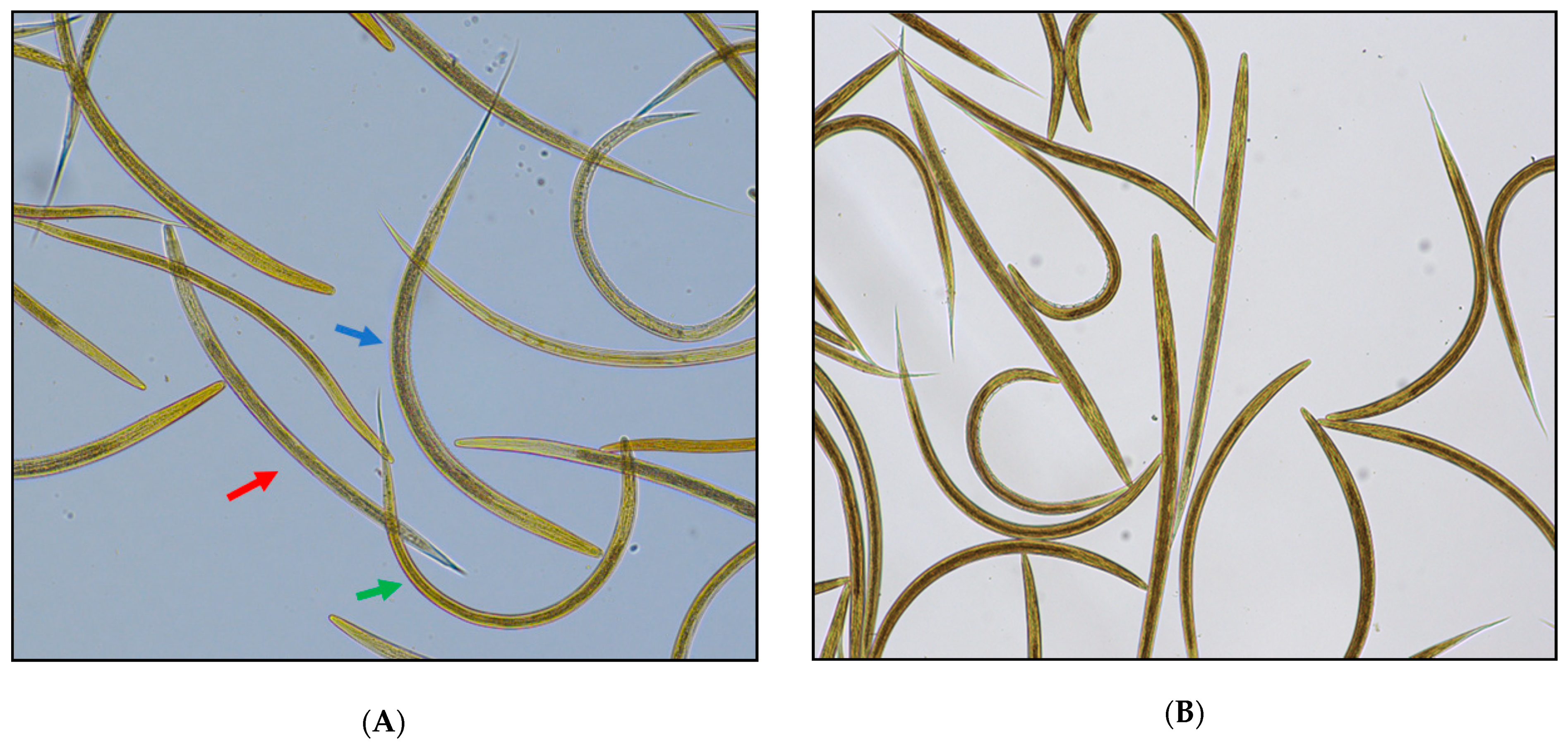
2.2. Sampling and Laboratory Analysis
2.2.1. Faecal Egg Count Reduction Test (FECRT)
2.2.2. Egg Hatch Test (EHT)
2.2.3. Larval Development Test (LDT)
2.3. Data Analysis
2.3.1. FECRT
- (a)
- FECR1 = 100 × (1 − [T1/T0]) [45], where T0 and T1 represent the arithmetic mean of eggs per gram (EPGs) of the treated group before (day 0) and after treatment (day 14).
- (b)
- FECR2 = (1/n)Σ(100 × (1 − [Ti1/Ti0]) [46], where Ti0 and Ti1 represent the EPGs (before and after treatment) in host i from a total n hosts. In this case, each host serves as its own control.
2.3.2. EHT
2.3.3. LDT
3. Results
3.1. FECRT
3.2. EHT
3.3. LDT
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Charlier, J.; Rinaldi, L.; Musella, V.; Ploeger, H.; Chartier, C.; Vineer, H.R.; Hinney, B.; von Samson-Himmelstjerna, G.; Băcescu, B.; Mickiewicz, M.; et al. Corrigendum to “Initial assessment of the economic burden of major parasitic helminth infections to the ruminant livestock industry in Europe” [Prev. Vet. Med. 182 (2020) 105103]. Prev. Vet. Med. 2021, 188, 105213. [Google Scholar] [CrossRef] [PubMed]
- Vineer, H.R.; Morgan, E.R.; Hertzberg, H.; Bartley, D.J.; Bosco, A.; Charlier, J.; Chartier, C.; Claerebout, E.; De Waal, T.; Hendrickx, G.; et al. Increasing importance of anthelmintic resistance in European livestock: Creation and meta-analysis of an open database. Parasite 2020, 27, 69. [Google Scholar] [CrossRef] [PubMed]
- Hoste, H.; Sotiraki, S.; Torres-Acosta, J.F.D.J. Control of Endoparasitic Nematode Infections in Goats. Vet. Clin. N. Am. Food Anim. Pr. 2011, 27, 163–173. [Google Scholar] [CrossRef] [PubMed]
- Coles, G.; Bauer, C.; Borgsteede, F.; Geerts, S.; Klei, T.; Taylor, M.; Waller, P. World Association for the Advancement of Veterinary Parasitology (W.A.A.V.P.) methods for the detection of anthelmintic resistance in nematodes of veterinary importance. Vet. Parasitol. 1992, 44, 35–44. [Google Scholar] [CrossRef]
- Coles, G.; Jackson, F.; Pomroy, W.; Prichard, R.; von Samson-Himmelstjerna, G.; Silvestre, A.; Taylor, M.; Vercruysse, J. The detection of anthelmintic resistance in nematodes of veterinary importance. Vet. Parasitol. 2006, 136, 167–185. [Google Scholar] [CrossRef]
- Rose, H.; Rinaldi, L.; Bosco, A.; Mavrot, F.; de Waal, T.; Skuce, P.; Charlier, J.; Torgerson, P.; Hertzberg, H.; Hendrickx, G.; et al. Widespread anthelmintic resistance in European farmed ruminants: A systematic review. Vet. Rec. 2015, 176, 546. [Google Scholar] [CrossRef] [Green Version]
- Mickiewicz, M.; Czopowicz, M.; Kawecka-Grochocka, E.; Moroz, A.; Szaluś-Jordanow, O.; Várady, M.; Königová, A.; Spinu, M.; Górski, P.; Bagnicka, E.; et al. The first report of multidrug resistance in gastrointestinal nematodes in goat population in Poland. BMC Vet. Res. 2020, 16, 1–12. [Google Scholar] [CrossRef]
- Holm, S.A.; Sörensen, C.R.L.; Thamsborg, S.M.; Enemark, H.L. Gastrointestinal nematodes and anthelmintic resistance in Danish goat herds. Parasite 2014, 21, 37. [Google Scholar] [CrossRef] [Green Version]
- Kaplan, R.M. Drug resistance in nematodes of veterinary importance: A status report. Trends Parasitol. 2004, 20, 477–481. [Google Scholar] [CrossRef]
- Hong, C.; Hunt, K.R.; Coles, G.C. Occurrence of anthelmintic resistant nematodes on sheep farms in England and goat farms in England and Wales. Vet. Rec. 1996, 139, 83–86. [Google Scholar] [CrossRef] [PubMed]
- Borgsteede, F.; Pekelder, J.; Dercksen, D. Anthelmintic resistant nematodes in goats in the Netherlands. Vet. Parasitol. 1996, 65, 83–87. [Google Scholar] [CrossRef]
- Requejo-Fernández, J.; Martínez, A.; Meana, A.; Rojo-Vázquez, F.; Osoro, K.; Ortega-Mora, L. Anthelmintic resistance in nematode parasites from goats in Spain. Vet. Parasitol. 1997, 73, 83–88. [Google Scholar] [CrossRef] [Green Version]
- Cringoli, G.; Veneziano, V.; Rinaldi, L.; Sauve, C.; Rubino, R.; Fedele, V.; Cabaret, J. Resistance of trichostrongyles to benzimidazoles in Italy: A first report in a goat farm with multiple and repeated introductions. Parasitol. Res. 2007, 101, 577–581. [Google Scholar] [CrossRef] [PubMed]
- Kupčinskas, T.; Stadalienė, I.; Šarkūnas, M.; Riškevičienė, V.; Várady, M.; Höglund, J.; Petkevičius, S. Prevalence of anthelmintic resistance on Lithuanian sheep farms assessed by in vitro methods. Acta Vet. Scand. 2015, 57, 88. [Google Scholar] [CrossRef] [Green Version]
- Paraud, C.; Kulo, A.; Pors, I.; Chartier, C. Resistance of goat nematodes to multiple anthelmintics on a farm in France. Vet. Rec. 2009, 164, 563–564. [Google Scholar] [CrossRef] [PubMed]
- Chartier, C.; Soubirac, F.; Pors, I.; Silvestre, A.; Hubert, J.; Couquet, C.; Cabaret, J. Prevalence of anthelmintic resistance in gastrointestinal nematodes of dairy goats under extensive management conditions in southwestern France. J. Helminthol. 2001, 75, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Schnyder, M.; Torgerson, P.; Schönmann, M.; Kohler, L.; Hertzberg, H. Multiple anthelmintic resistance in Haemonchus contortus isolated from South African Boer goats in Switzerland. Vet. Parasitol. 2005, 128, 285–290. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peña-Espinoza, M.; Thamsborg, S.M.; Demeler, J.; Enemark, H.L. Field efficacy of four anthelmintics and confirmation of drug-resistant nematodes by controlled efficacy test and pyrosequencing on a sheep and goat farm in Denmark. Vet. Parasitol. 2014, 206, 208–215. [Google Scholar] [CrossRef] [Green Version]
- Domke, A.V.M.; Chartier, C.; Gjerde, B.; Höglund, J.; Leine, N.; Vatn, S.; Stuen, S. Prevalence of anthelmintic resistance in gastrointestinal nematodes of sheep and goats in Norway. Parasitol. Res. 2012, 111, 185–193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bauer, C. Multispecific resistance of trichostrongyles to benzimidazoles in a goat herd in Germany. DTW. Dtsch. Tierarztliche Wochenschr. 2001, 108, 49–50. [Google Scholar]
- Babják, M.; Königová, A.; Dolinská, M.U.; Vadlejch, J.; Várady, M. Anthelmintic resistance in goat herds—In vivo versus in vitro detection methods. Vet. Parasitol. 2018, 254, 10–14. [Google Scholar] [CrossRef]
- Vadlejch, J.; Kyriánová, I.A.; Várady, M.; Charlier, J. Resistance of strongylid nematodes to anthelmintic drugs and driving factors at Czech goat farms. BMC Vet. Res. 2021, 17, 1–11. [Google Scholar] [CrossRef]
- Mickiewicz, M.; Czopowicz, M.; Gorski, P.; Kaba, J. The first reported case of resistance of gastrointestinal nematodes to ben-zimidazole anthelmintic in goats in Poland. Ann. Parasitol. 2017, 63, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Mickiewicz, M.; Czopowicz, M.; Moroz, A.; Szalus-Jordanow, O.; Gorski, P.; Várady, M.; Konigová, A.; Spinu, M.; Lefkaditis, M.; Kaba, J. Development of resistance to eprinomectin in gastrointestinal nematodes in a goat herd with pre-existing resistance to benzimidazoles. Pol. J. Vet. Sci. 2019, 22, 753–760. [Google Scholar] [CrossRef]
- Mickiewicz, M.; Czopowicz, M.; Moroz, A.; Potărniche, A.-V.; Szaluś-Jordanow, O.; Spinu, M.; Górski, P.; Markowska-Daniel, I.; Várady, M.; Kaba, J. Prevalence of anthelmintic resistance of gastrointestinal nematodes in Polish goat herds assessed by the larval development test. BMC Vet. Res. 2021, 17, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Howell, S.B.; Burke, J.M.; Miller, J.E.; Terrill, T.H.; Valencia, E.; Williams, M.J.; Williamson, L.H.; Zajac, A.M.; Kaplan, R. Prevalence of anthelmintic resistance on sheep and goat farms in the southeastern United States. J. Am. Vet. Med Assoc. 2008, 233, 1913–1919. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vatta, A.; Lindberg, A. Managing anthelmintic resistance in small ruminant livestock of resource-poor farmers in South Africa: Review article. J. S. Afr. Vet. Assoc. 2006, 77, 2–8. [Google Scholar] [CrossRef] [Green Version]
- Wanyangu, S.; Bain, R.; Rugutt, M.; Nginyi, J.; Mugambi, J. Anthelmintic resistance amongst sheep and goats in Kenya. Prev. Vet. Med. 1996, 25, 285–290. [Google Scholar] [CrossRef]
- Arece-García, J.; López-Leyva, Y.; Olmedo-Juárez, A.; Ramírez, G.; Reyes-Guerrero, D.; Arellano, M.E.L.; De Gives, P.M.; Várady, M.; Rubio, R.R.; Garduño, R.G. First report of multiple anthelmintic resistance in goat farm in Cuba. Helminthologia 2017, 54, 358–362. [Google Scholar] [CrossRef] [Green Version]
- Dorny, P.; Claerebout, E.; Vercruysse, J.; Sani, R.; Jalila, A. Anthelmintic resistance in goats in peninsular Malaysia. Vet. Parasitol. 1994, 55, 327–342. [Google Scholar] [CrossRef]
- Manikkavasagan, I.; Binosundar, S.T.; Raman, M. Survey on anthelmintic resistance to gastrointestinal nematodes in unorganized goat farms of Tamil Nadu. J. Parasit. Dis. 2013, 39, 258–261. [Google Scholar] [CrossRef] [Green Version]
- Veale, P.I. Resistance to macrocyclic lactones in nematodes of goats. Aust. Vet. J. 2002, 80, 303–304. [Google Scholar] [CrossRef] [PubMed]
- Kettle, P.R.; Vlassoff, A.; Reid, T.C.; Hotton, C.T. A survey of nematode control measures used by milking goat farmers and of anthelmintic resistance on their farms. N. Z. Vet. J. 1983, 31, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Babják, M.; Königová, A.; Várady, U. Multiple anthelmintic resistance at a goat farm in Slovakia. Helminthologia 2021, 58, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Königová, A.; Dolinská, M.U.; Babják, M.; Von Samson-Himmelstjerna, G.; Komáromyová, M.; Várady, M. Experimental evidence for the lack of sensitivity of in vivo faecal egg count reduction testing for the detection of early development of benzimidazole resistance. Parasitol. Res. 2021, 120, 153–159. [Google Scholar] [CrossRef]
- Crook, E.; O’Brien, D.; Howell, S.; Storey, B.; Whitley, N.; Burke, J.; Kaplan, R. Prevalence of anthelmintic resistance on sheep and goat farms in the mid-Atlantic region and comparison of in vivo and in vitro detection methods. Small Rumin. Res. 2016, 143, 89–96. [Google Scholar] [CrossRef] [Green Version]
- Babják, M.; Königová, A.; Dolinská, M.U.; Kupčinskas, T.; Vadlejch, J.; von Samson-Himmelstjerna, G.; Petkevičius, S.; Várady, M. Does the in vitro egg hatch test predict the failure of benzimidazole treatment in Haemonchus contortus? Parasite 2021, 28, 62. [Google Scholar] [CrossRef]
- Cernea, M.; Cristina, R.T.; Stefanut, L.C.; de Carvalho, L.M.; Taulescu, M.A.; Cozma, V. Screening for anthelmintic resistance in equid strongyles (Nematoda) in Romania. Folia Parasitol. 2015, 62, 23. [Google Scholar] [CrossRef] [Green Version]
- Matthews, J. Diseases of the Goat, 4th ed.; Wiley BlackWell: Hoboken, NJ, USA, 2016. [Google Scholar]
- Wyk, J.V.; Jan, A.; Mayhew, E. Morphological identification of parasitic nematode infective larvae of small ruminants and cattle: A practical lab guide. Onderstepoort J. Vet. Res. 2013, 80, 14. [Google Scholar] [CrossRef]
- Hunt, K.R.; Taylor, M.A. Use of the egg hatch assay on sheep faecal samples for the detection of benzimidazole resistant nematodes. Vet. Rec. 1989, 125, 153–154. [Google Scholar] [CrossRef] [PubMed]
- Von Samson-Himmelstjerna, G.; Coles, G.C.; Jackson, F.; Bauer, C.; Borgsteede, F.; Cirak, V.Y.; Demeler, J.; Donnan, A.; Dorny, P.; Epe, C.; et al. Standardization of the egg hatch test for the detection of benzimidazole resistance in parasitic nematodes. Parasitol. Res. 2009, 105, 825–834. [Google Scholar] [CrossRef] [PubMed]
- Hubert, J.; Kerboeuf, D. A microlarval development assay for the detection of anthelmintic resistance in sheep nematodes. Vet. Rec. 1992, 130, 442–446. [Google Scholar] [CrossRef]
- Várady, M.; Bjørn, H.; Nansen, P. In vitro characterization of anthelmintic susceptibility of field isolates of the pig nodular worm Oesophagostomum spp., susceptible or resistant to various anthelmintics. Int. J. Parasitol. 1996, 26, 733–740. [Google Scholar] [CrossRef]
- Kochapakdee, S.; Pandey, V.S.; Pralomkarn, W.; Choldumrongkul, S.; Ngampongsai, W.; Lawpetchara, A. Anthelmintic resistance in goats in southern Thailand. Vet. Rec. 1995, 137, 124–125. [Google Scholar] [CrossRef] [PubMed]
- Cabaret, J.; Berrag, B. Faecal egg count reduction test for assessing anthelmintic efficacy: Average versus individually based estimations. Vet. Parasitol. 2004, 121, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Dobson, R.J.; Griffiths, D.A.; Donald, A.D.; Waller, P.J. A Genetic Model Describing the Evolution of Levamisole Resistance in Trichostrongylus colubriformis, a Nematode Parasite of Sheep. Math. Med. Biol. 1987, 4, 279–293. [Google Scholar] [CrossRef] [PubMed]
- Dolinská, M.; Ivanišinová, O.; Königová, A.; Várady, M. Anthelmintic resistance in sheep gastrointestinal nematodes in Slovakia detected by in-vitro methods. BMC Vet. Res. 2014, 10, 233. [Google Scholar] [CrossRef] [Green Version]
- Taylor, M. A larval development test for the detection of anthelmintic resistance in nematodes of sheep. Res. Vet. Sci. 1990, 49, 198–202. [Google Scholar] [CrossRef]
- Kaplan, R.M. Biology, Epidemiology, Diagnosis, and Management of Anthelmintic Resistance in Gastrointestinal Nematodes of Livestock. Vet. Clin. N. Am. Food Anim. Pr. 2020, 36, 17–30. [Google Scholar] [CrossRef]
- Várady, M.; Čudeková, P.; Corba, J. In vitro detection of benzimidazole resistance in Haemonchus contortus: Egg hatch test versus larval development test. Vet. Parasitol. 2007, 149, 104–110. [Google Scholar] [CrossRef]
- Dolinská, M.U.; Königová, A.; Letková, V.; Molnár, L.; Várady, M. Detection of ivermectin resistance by a larval development test—Back to the past or a step forward? Vet. Parasitol. 2013, 198, 154–158. [Google Scholar] [CrossRef] [PubMed]
- Čudeková, P.; Várady, M.; Dolinská, M.; Königová, A. Phenotypic and genotypic characterisation of benzimidazole susceptible and resistant isolates of Haemonchus contortus. Vet. Parasitol. 2010, 172, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Várady, M.; Papadopoulos, E.; Dolinská, M.; Königová, A. Anthelmintic resistance in parasites of small ruminants: Sheep versus goats. Helminthologia 2011, 48, 137–144. [Google Scholar] [CrossRef] [Green Version]
- Martin, P.J.; Anderson, N.; Jarrett, R.G. Detecting benzimidazole resistance with faecal egg count reduction tests and in vitro assays. Aust. Vet. J. 1989, 66, 236–240. [Google Scholar] [CrossRef] [PubMed]
- Baños, P.D.; Pedreira, J.; Sánchez-Andrade, R.; Francisco, I.; Suárez, J.L.; Díaz, P.; Panadero, R.; Arias, M.; Painceira, A.; Paz-Silva, A.; et al. Field Evaluation for Anthelmintic-Resistant Ovine Gastrointestinal Nematodes by In Vitro and In Vivo Assays. J. Parasitol. 2008, 94, 925–928. [Google Scholar] [CrossRef]
- Dobson, R.J.; Lejambre, L.; Gill, J.H. Management of anthelmintic resistance: Inheritance of resistance and selection with persistent drugs. Int. J. Parasitol. 1996, 26, 993–1000. [Google Scholar] [CrossRef]
- Maingi, N.; Bjørn, H.; Thamsborg, S.M.; Bøgh, H.; Nansen, P. A survey of anthelmintic resistance in nematode parasites of goats in Denmark. Vet. Parasitol. 1996, 66, 53–66. [Google Scholar] [CrossRef]
- Jackson, F.; Coop, R. Evidence of multiple anthelmintic resistance in a strain of Teladorsagia circumcincta (Ostertagia circumcincta) isolated from goats in Scotland. Res. Vet. Sci. 1992, 53, 371–374. [Google Scholar] [CrossRef]
- Várady, M.; Praslicka, J.; Corba, J.; Vesely, L. Multiple anthelmintic resistance of nematodes in imported goats. Vet. Rec. 1993, 132, 387–388. [Google Scholar] [CrossRef] [PubMed]
- Artho, R.; Schnyder, M.; Kohler, L.; Torgerson, P.; Hertzberg, H. Avermectin-resistance in gastrointestinal nematodes of Boer goats and Dorper sheep in Switzerland. Vet. Parasitol. 2007, 144, 68–73. [Google Scholar] [CrossRef] [Green Version]
- Murri, S.; Knubben-Schweizer, G.; Torgerson, P.; Hertzberg, H. Frequency of eprinomectin resistance in gastrointestinal nematodes of goats in canton Berne, Switzerland. Vet. Parasitol. 2014, 203, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Scheuerle, M.C.; Mahling, M.; Pfister, K. Anthelminthic resistance of Haemonchus contortus in small ruminants in Switzerland and Southern Germany. Wien. Klin. Wochenschr. 2009, 121, 46–49. [Google Scholar] [CrossRef]
- Lespine, A.; Ménez, C.; Bourguinat, C.; Prichard, R.K. P-glycoproteins and other multidrug resistance transporters in the pharmacology of anthelmintics: Prospects for reversing transport-dependent anthelmintic resistance. Int. J. Parasitol. Drugs Drug Resist. 2012, 2, 58–75. [Google Scholar] [CrossRef] [PubMed]
- Mottier, M.D.L.; Prichard, R.K. Genetic analysis of a relationship between macrocyclic lactone and benzimidazole anthelmintic selection on Haemonchus contortus. Pharmacogenet. Genom. 2008, 18, 129–140. [Google Scholar] [CrossRef] [PubMed]
- Fleming, S.A.; Craig, T.; Kaplan, R.M.; Miller, J.E.; Navarre, C.; Rings, M. Anthelmintic resistance of gastrointestinal parasites in small ruminants. J. Vet. Intern. Med. 2006, 20, 435–444. [Google Scholar] [CrossRef]
- Sharma, D.; Vatsya, S.; Kumar, R.R. Impact of treatment of gastrointestinal nemathelminths on body weight of sheep and goats. J. Parasit. Dis. 2014, 40, 801–804. [Google Scholar] [CrossRef] [Green Version]
- Cringoli, G.; Rinaldi, L.; Veneziano, V.; Capelli, G.; Rubino, R. Effectiveness of eprinomectin pour-on against gastrointestinal nematodes of naturally infected goats. Small Rumin. Res. 2004, 55, 209–213. [Google Scholar] [CrossRef]
- Papadopoulos, E. Anthelmintic resistance in sheep nematodes. Small Rumin. Res. 2008, 76, 99–103. [Google Scholar] [CrossRef]
| Goat No. (>6 Months) | Pre-Treatment (Day 0) | Post-Treatment (Day 14) |
|---|---|---|
| 1 | 1600 | 2100 |
| 2 | 550 | 6950 |
| 3 | 150 | 1000 |
| 4 | 2350 | 2950 |
| 5 | 1600 | 1400 |
| 6 | 750 | 1350 |
| 7 | 1350 | 2850 |
| 8 | 1750 | 2500 |
| 9 | 700 | 1050 |
| 10 | 1500 | 950 |
| Mean ± SD a | 1230 ± 669 | 2310 ± 1802 |
| Median | 1425 | 1750 |
| IQR b (range) | 700–1600 (150–2350) | 1050 −2850 (950–6950) |
| FECR1 c (CI 95%) | −88% (CI 95%: −248, −1) | |
| FECR2 c | –202% | |
| TBZ | |
|---|---|
| IC50 | 221.1 μg/mL |
| IC99 | undeterminable * |
| Percentage of eggs hatching at the DC (0.1 μg/mL) (CI 95%) | 96.2% (CI 95%: 92.6, 98.1) |
| TBZ | IVM-AG | LEV | |
|---|---|---|---|
| LC50 | Undeterminable * | 121.5 ng/mL | 0.082 µg/mL |
| LC90 | Undeterminable * | 315.9 ng/mL | 0.154 µg/mL |
| LC99 | Undeterminable * | 895.9 ng/mL | 0.305 µg/mL |
| Corrected % inhibited at DC(CI 95%) | 5.1% (2.6%, 10.0%) | 5.2% (2.8%, 9.5%) | 100% (89.6%, 100%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Potârniche, A.V.; Mickiewicz, M.; Olah, D.; Cerbu, C.; Spînu, M.; Hari, A.; Györke, A.; Moroz, A.; Czopowicz, M.; Várady, M.; et al. First Report of Anthelmintic Resistance in Gastrointestinal Nematodes in Goats in Romania. Animals 2021, 11, 2761. https://doi.org/10.3390/ani11102761
Potârniche AV, Mickiewicz M, Olah D, Cerbu C, Spînu M, Hari A, Györke A, Moroz A, Czopowicz M, Várady M, et al. First Report of Anthelmintic Resistance in Gastrointestinal Nematodes in Goats in Romania. Animals. 2021; 11(10):2761. https://doi.org/10.3390/ani11102761
Chicago/Turabian StylePotârniche, Adrian Valentin, Marcin Mickiewicz, Diana Olah, Constantin Cerbu, Marina Spînu, Attila Hari, Adriana Györke, Agata Moroz, Michał Czopowicz, Marián Várady, and et al. 2021. "First Report of Anthelmintic Resistance in Gastrointestinal Nematodes in Goats in Romania" Animals 11, no. 10: 2761. https://doi.org/10.3390/ani11102761
APA StylePotârniche, A. V., Mickiewicz, M., Olah, D., Cerbu, C., Spînu, M., Hari, A., Györke, A., Moroz, A., Czopowicz, M., Várady, M., & Kaba, J. (2021). First Report of Anthelmintic Resistance in Gastrointestinal Nematodes in Goats in Romania. Animals, 11(10), 2761. https://doi.org/10.3390/ani11102761








