Non-Contact Vital Signs Monitoring of Dog and Cat Using a UWB Radar
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. UWB Radar System
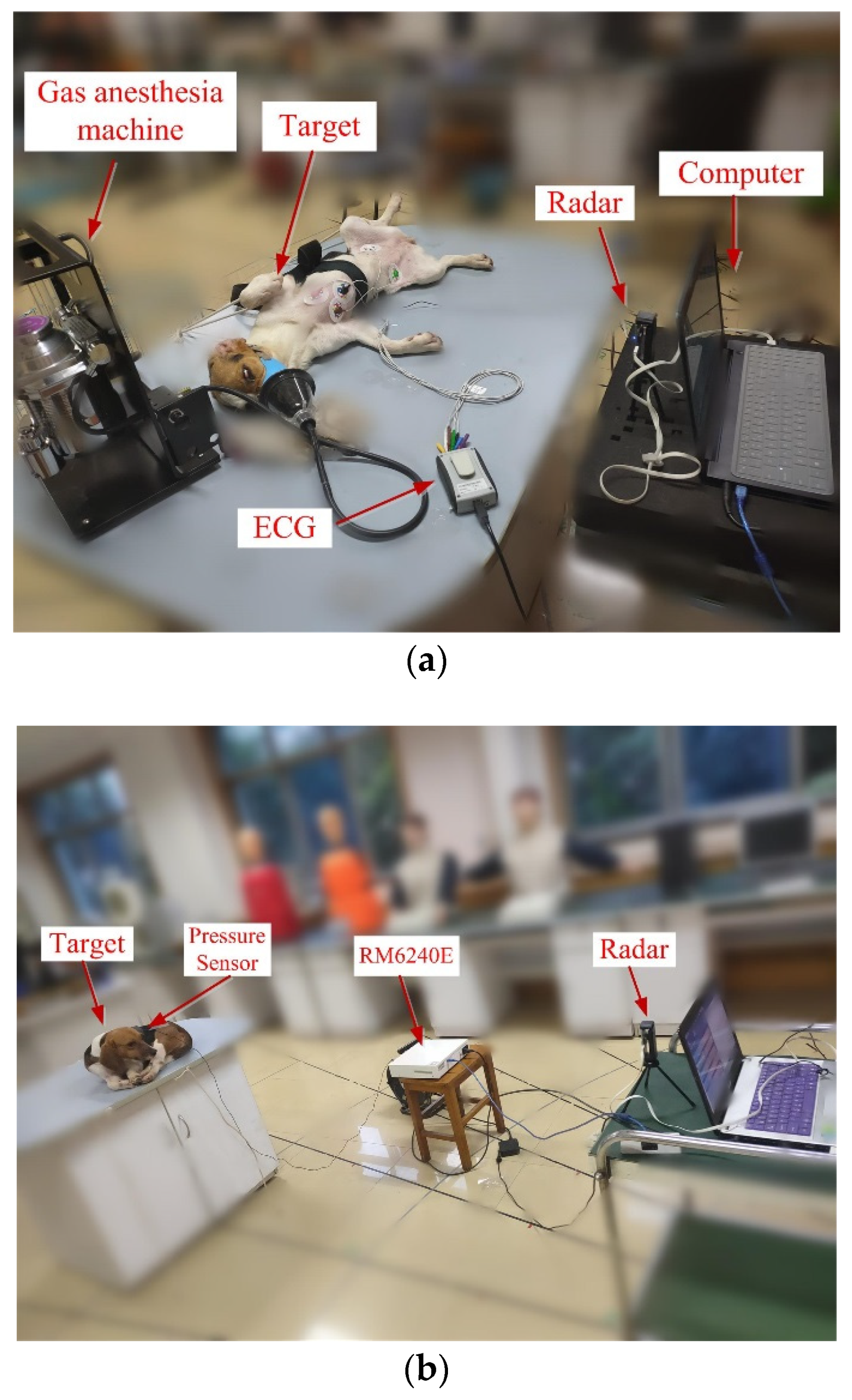
2.3. Data Acquisition
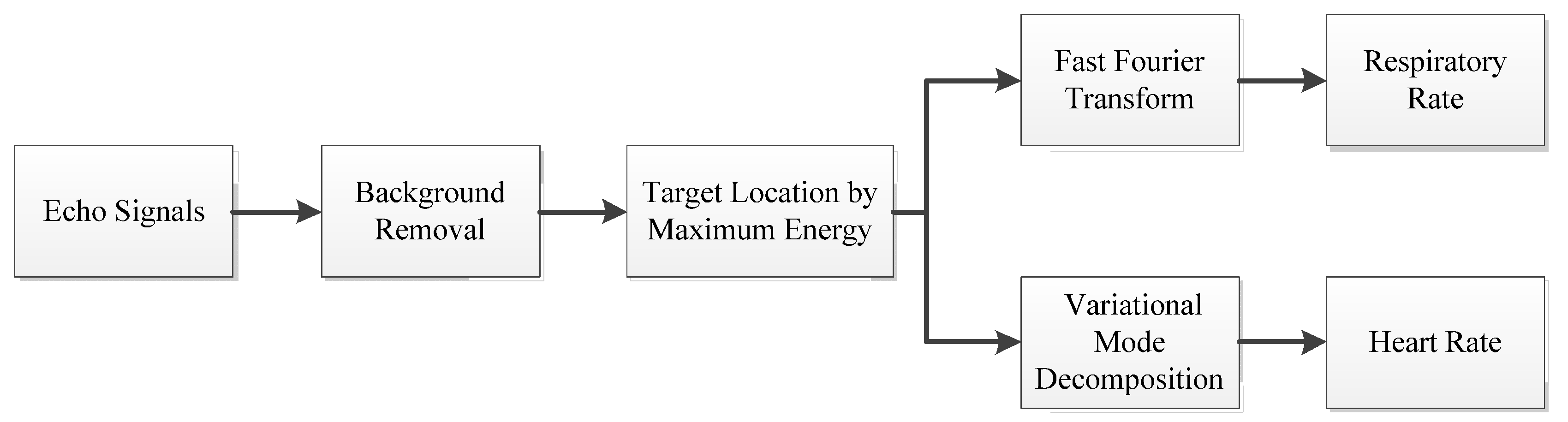
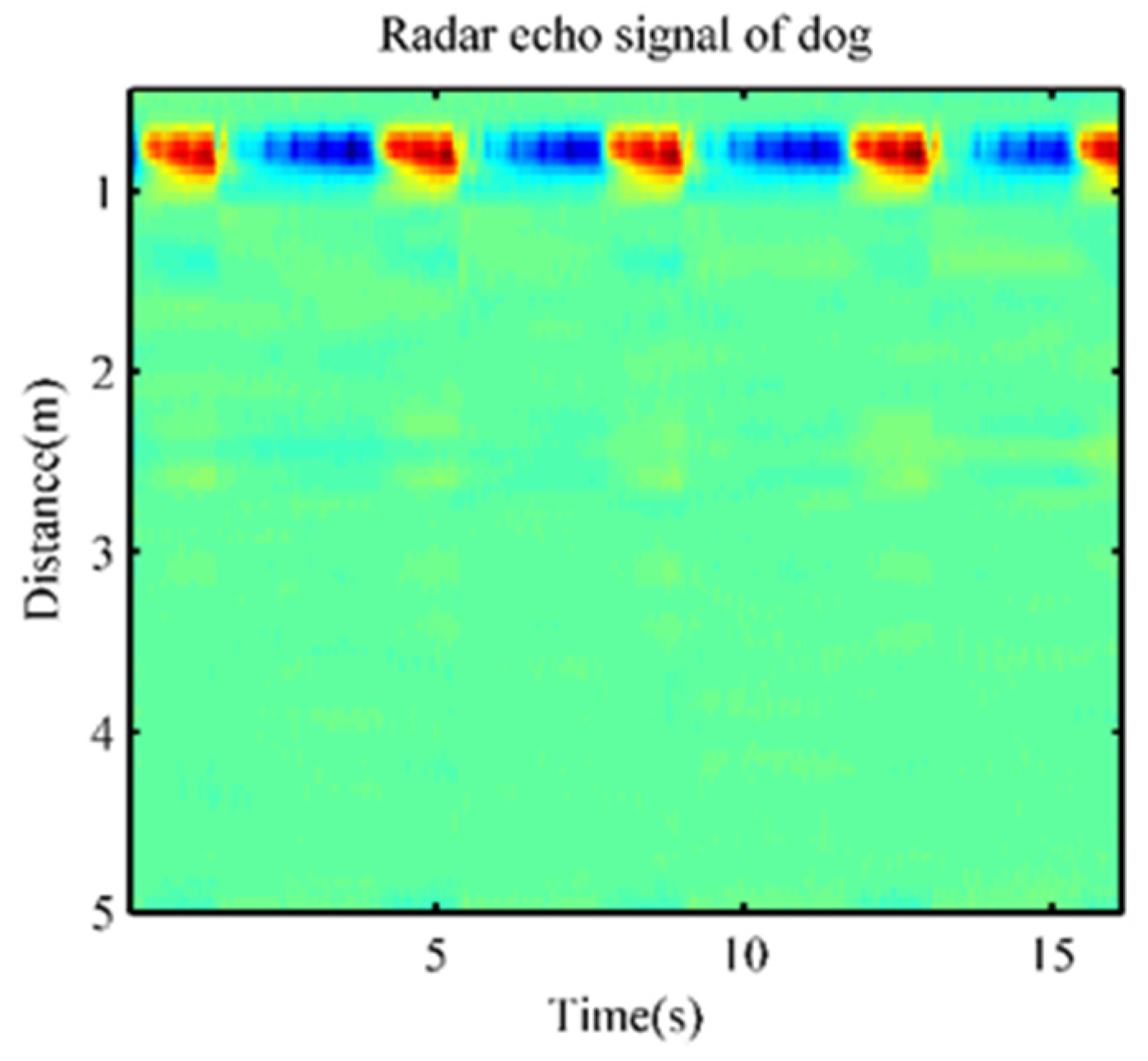
2.4. Signal Preprocessing
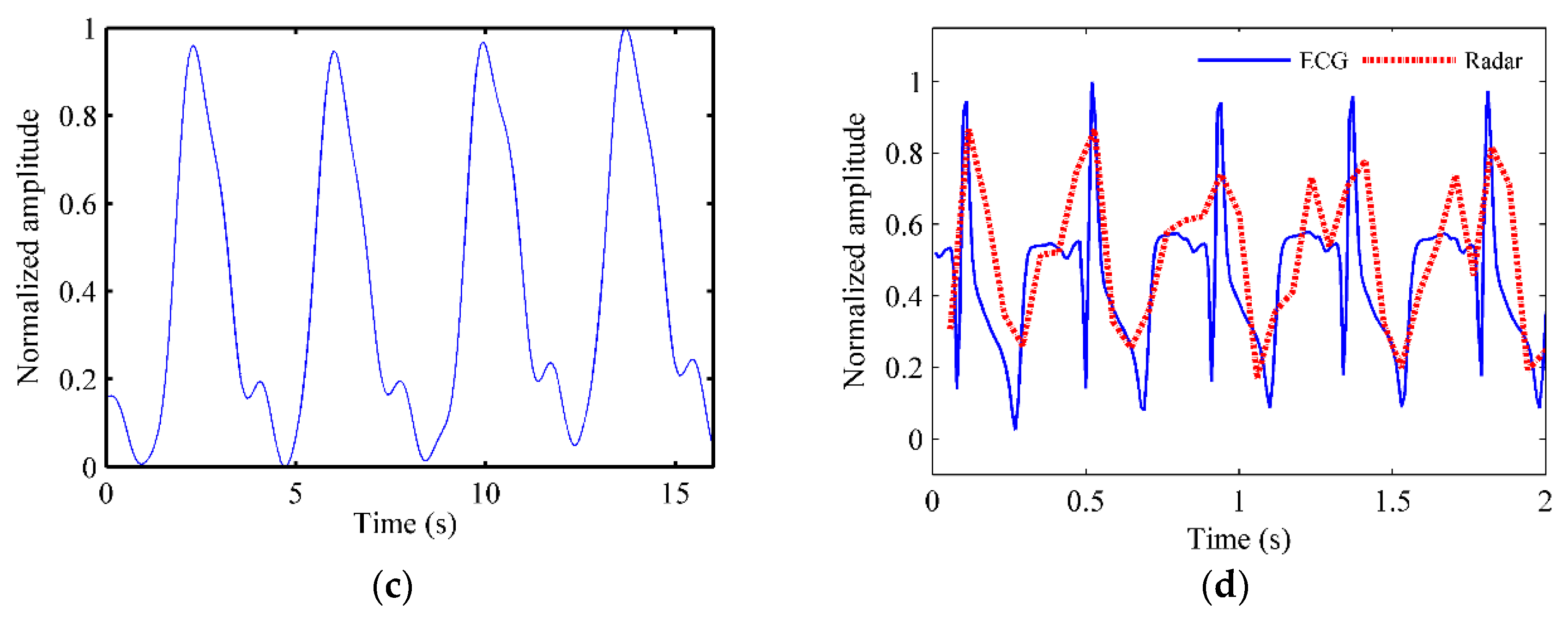
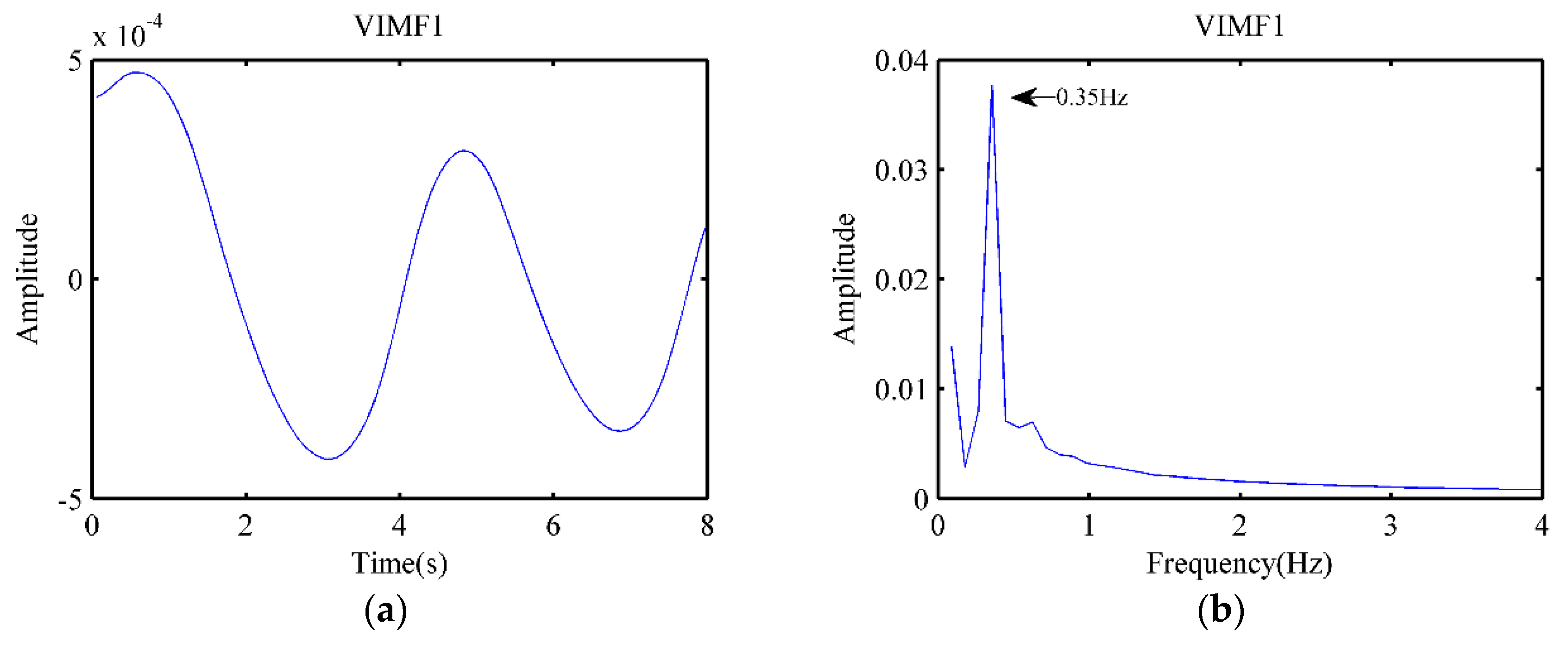
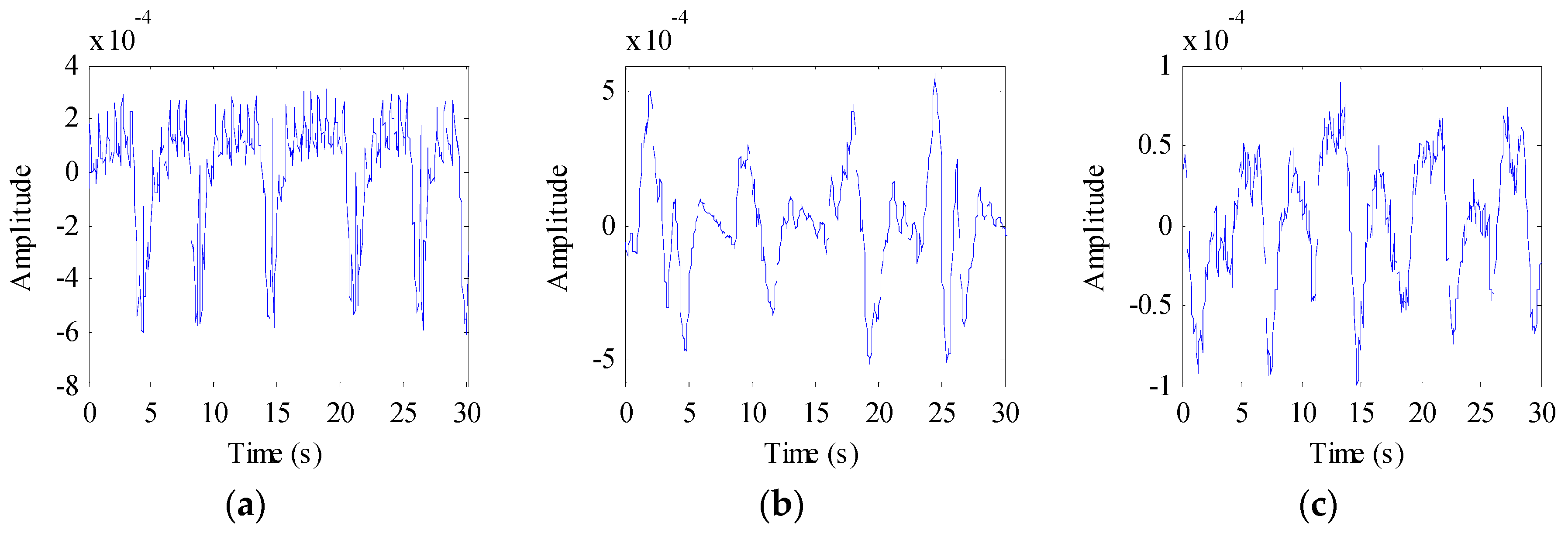
2.5. Variational Mode Decomposition
3. Results
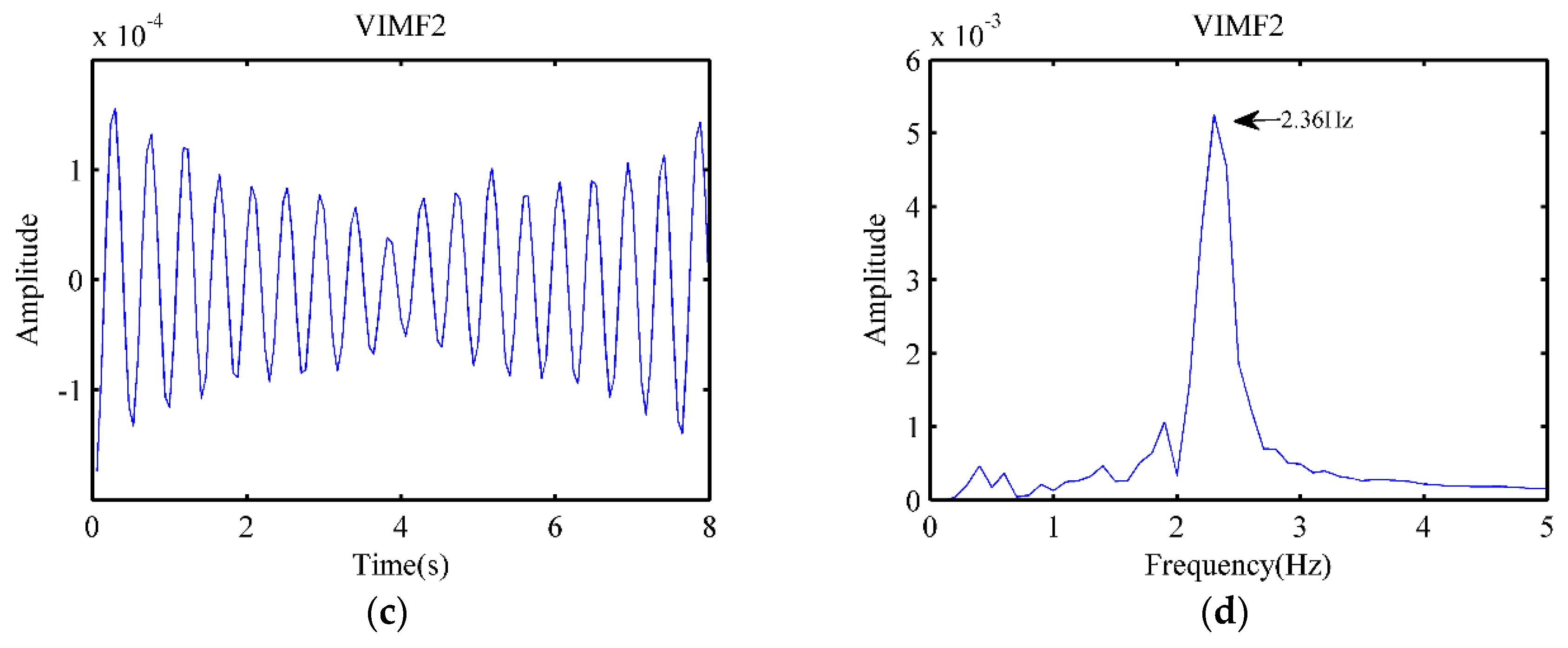
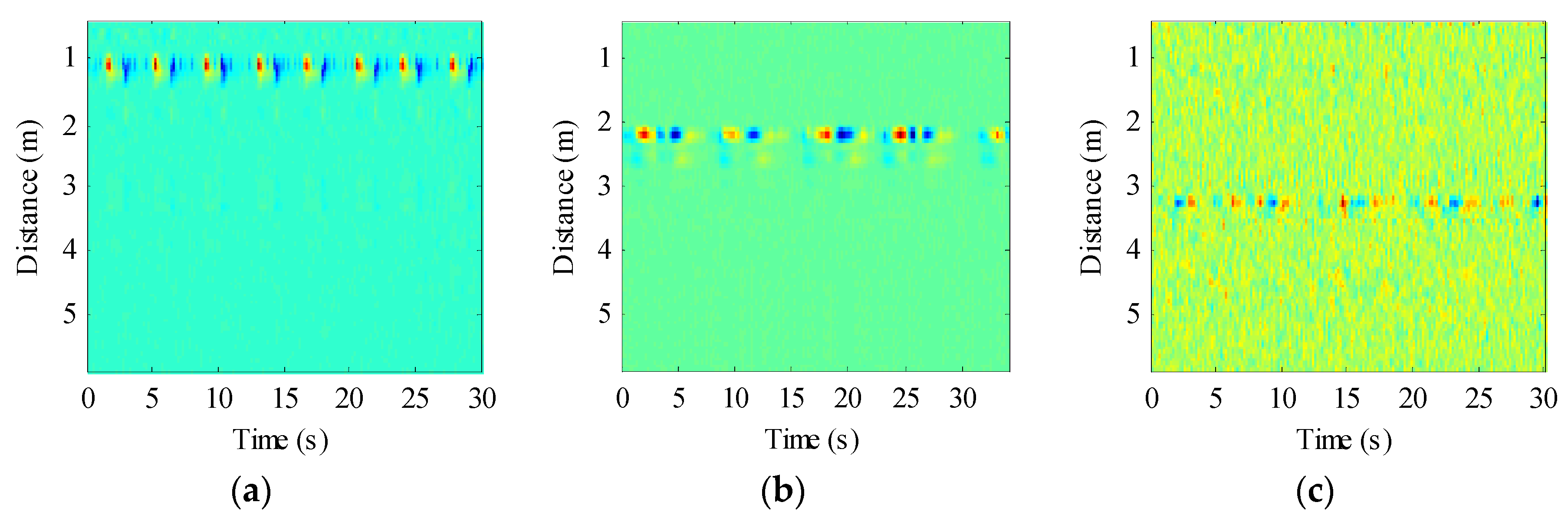
3.1. Results of Dog
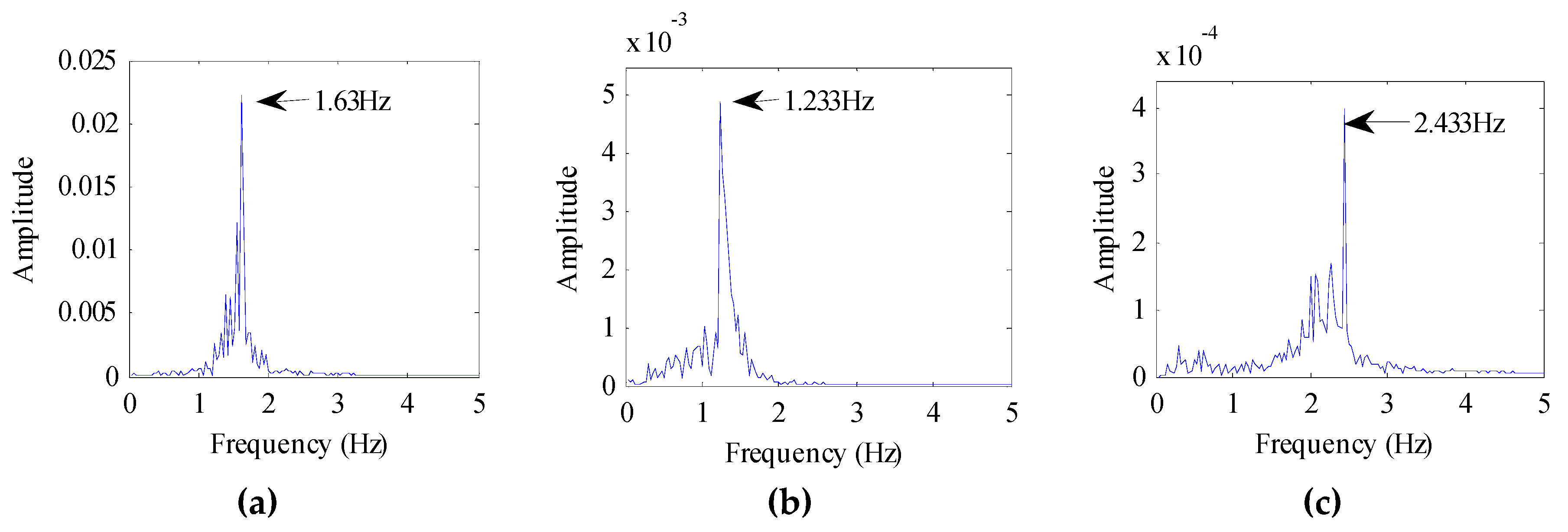
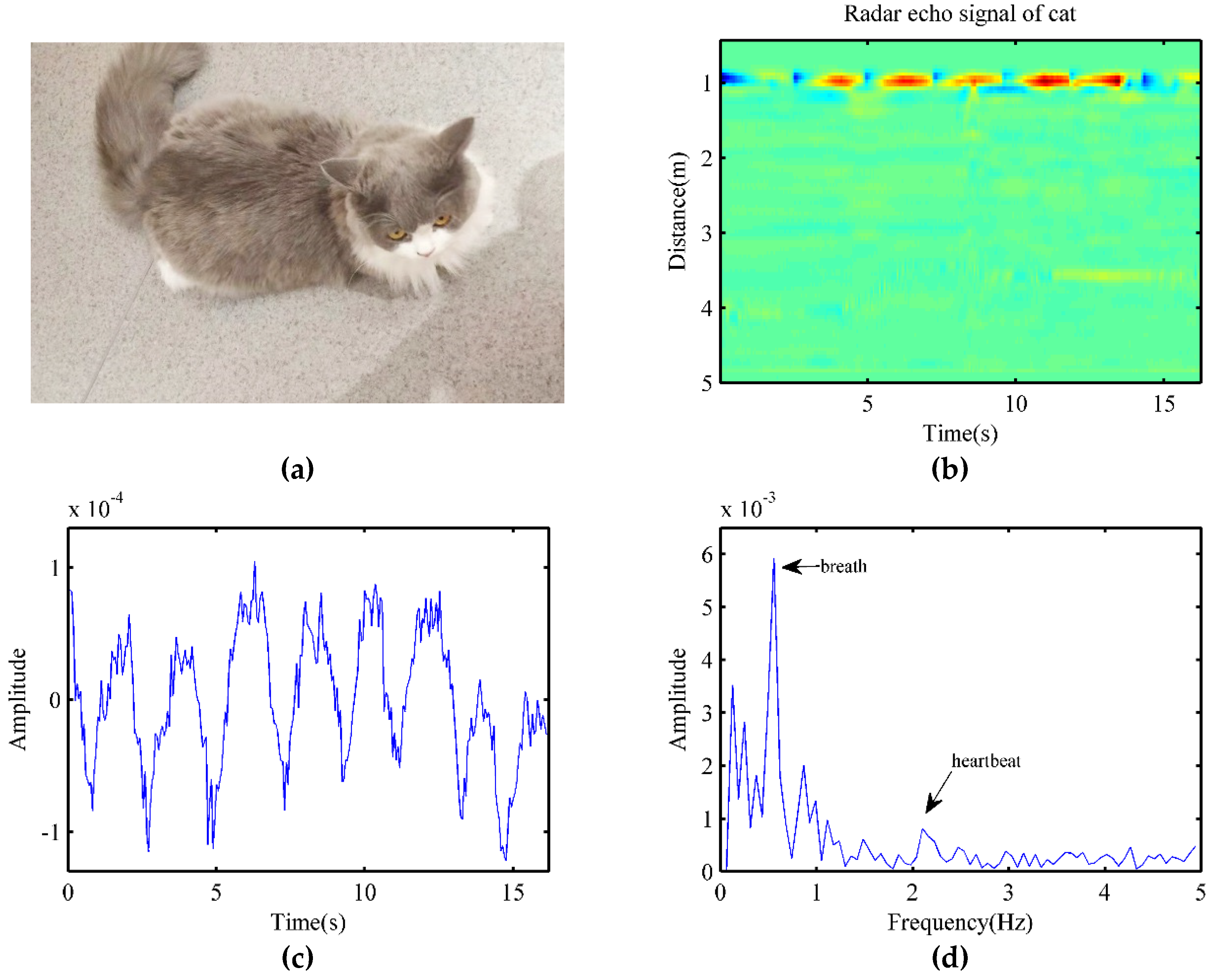
3.2. Experiment on Cat
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Whole-Body Average SAR (W/kg) | Localized SAR (Head and trunk) (W/kg) | Localized SAR (Limbs) (W/kg) | |
|---|---|---|---|
| SAR limit, general public | 0.08 | 2 | 4 |
| Frequency Range | E-field Strength (V/m) | H-field Strength (A/m) | B-Field (QT) | Equivelant Plane Wave Power Density Seq (w/m2) |
|---|---|---|---|---|
| 2–300 GHz | 61 | 0.61 | 0.20 | 10 |
References
- Von Borell, E.; Langbein, J.; Després, G.; Hansen, S.; Leterrier, C.; Marchant-Forde, J.; Marchant-Forde, R.; Minero, M.; Mohr, E.; Prunier, A.; et al. Heart rate variability as a measure of autonomic regulation of cardiac activity for assessing stress and welfare in farm animals—A review. Physiol. Behav. 2007, 92, 293–316. [Google Scholar] [CrossRef] [PubMed]
- Eckstein, S. Depression in Dogs: Even Dogs Can Get the Blues. Learn about Symptoms and Treatments for Dog Depression. Available online: http://pets.webmd.com/features/depression-in-dogs (accessed on 20 January 2019).
- Varga, B.; Gergely, A.; Galambos, Á.; Kis, A. Heart Rate and Heart Rate Variability during Sleep in Family Dogs (Canis familiaris). Moderate Effect of Pre-Sleep Emotions. Animals 2018, 8, 107. [Google Scholar] [CrossRef] [PubMed]
- Wiepkema, P.R.; Koolhaas, J.M. The emotional brain. Anim. Welf. 1992, 1, 13–18. [Google Scholar]
- Rosselot, P.; Mendonça, T.; González, I.; Tadich, T. Behavioral and Physiological Differences between Working Horses and Chilean Rodeo Horses in a Handling Test. Animals 2019, 9, 397. [Google Scholar] [CrossRef] [PubMed]
- Pereira-Junior, P.P.; Marocolo, M.; Rodrigues, F.P.; Medei, E.; Nascimento, J.H. Noninvasive method for electrocardiogram recording in conscious rats: Feasibility for heart rate variability analysis. An. Acad. Bras. Ciências 2010, 82, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Tsukamoto, A.; Serizawa, K.; Sato, R.; Yamazaki, J.; Inomata, T. Vital signs monitoring during injectable and inhalant anesthesia in mice. Exp. Anim. 2014, 14-0050. [Google Scholar] [CrossRef]
- Bailey, J.E.; Pablo, L.S. Anesthetic monitoring and monitoring equipment: Application in small exotic pet practice. In Seminars in Avian and Exotic Pet Medicine; WB Saunders: Philadelphia, PA, USA, 1998; Volume 7, pp. 53–60. [Google Scholar]
- Detweiler, D.K. The dog electrocardiogram: A critical review. Compr. Electrocardiol. 2010, 1861–1908. [Google Scholar] [CrossRef]
- Farmer, J.B.; Levy, G.P. A simple method for recording the electrocardiogram and heart rate from conscious animals. Br. J. Pharmacol. Chemother. 1968, 32, 193–200. [Google Scholar] [CrossRef]
- Gonder, J.C.; Gard, E.A.; Lott, N.E., III. Electrocardiograms of Nine Species of Nonhuman Primates Sedated with Ketamine. 1980. Available online: https://www.ncbi.nlm.nih.gov/pubmed/6776852 (accessed on 21 January 2020).
- Eckenfels, A.; Trieb, G. The normal electrocardiogram of the conscious beagle dog. Toxicol. Appl. Pharmacol. 1979, 47, 567–584. [Google Scholar] [CrossRef]
- Menkes, A. Pet Animal Collar for Health & Vital Signs Monitoring, Alert and Diagnosis. U.S. Patent Application 13/400,595, 17 January 2013. [Google Scholar]
- Menkes, A.; Bukchin, M. Acoustically Enhanced Pet Animal Collar for Health & Vital Signs Monitoring, Alert and Diagnosis. U.S. Patent Application 13/743,383, 17 July 2014. [Google Scholar]
- Jackson, R. How to Take Your Pet’s Vital Signs: Heart Rate, Respiratory Rate and Body Temperature. Available online: https://www.gopetplan.com/blogpost/reading-the-signs-petplan-pet-insurance-talks-about-taking-vital-signs (accessed on 12 January 2019).
- Kindig, J.R.; Beeson, T.P.; Campbell, R.W. Acoustical performance of the stethoscope: A comparative analysis. Am. Heart J. 1982, 104, 269–275. [Google Scholar] [CrossRef]
- Liang, H.; Lukkarinen, S.; Hartimo, I. Heart sound segmentation algorithm based on heart sound envelogram. In Computers in Cardiology 1997; IEEE: Piscataway, NJ, USA, 1997; pp. 105–108. [Google Scholar]
- Nyland, T.G.; Mattoon, J.S. Small Animal Diagnostic Ultrasound; Elsevier Health Sciences: Amsterdam, The Netherlands, 2002. [Google Scholar]
- Frinking, P.J.; Bouakaz, A.; Kirkhorn, J.; Ten Cate, F.J.; De Jong, N. Ultrasound contrast imaging: Current and new potential methods. Ultrasound Med. Biol. 2000, 26, 965–975. [Google Scholar] [CrossRef]
- Allen, J. Photoplethysmography and its application in clinical physiological measurement. Physiol. Meas. 2007, 28, R1. [Google Scholar] [CrossRef] [PubMed]
- Tamura, T.; Maeda, Y.; Sekine, M.; Yoshida, M. Wearable photoplethysmographic sensors—Past and present. Electronics 2014, 3, 282–302. [Google Scholar] [CrossRef]
- Poh, M.-Z.; McDuff, D.J.; Picard, R.W. Advancements in Noncontact Multiparameter Physiological Measurements Using a Webcam. IEEE Trans. Biomed. Eng. 2011, 58, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; den Brinker, A.C.; Stuijk, S.; de Haan, G. Robust heart rate from fitness videos. Physiol. Meas. 2017, 38, 1023–1044. [Google Scholar] [CrossRef]
- Wang, C.; Pun, T.; Chanel, G. A Comparative Survey of Methods for Remote Heart Rate Detection From Frontal Face Videos. Front. Bioeng. Biotechnol. 2018, 6, 33. [Google Scholar] [CrossRef]
- Li, C.; Lubecke, V.M.; Boric-Lubecke, O.; Lin, J. A review on recent advances in Doppler radar sensors for noncontact healthcare monitoring. IEEE Trans. Microw. Theory Tech. 2013, 61, 2046–2060. [Google Scholar] [CrossRef]
- Li, C.; Peng, Z.; Huang, T.Y.; Fan, T.; Wang, F.-K.; Horng, T.-S.; Muñoz-Ferreras, J.-M.; Gómez-García, R.; Ran, L.; Lin, J.; et al. A review on recent progress of portable short-range noncontact microwave radar systems. IEEE Trans. Microw. Theory Tech. 2017, 65, 1692–1706. [Google Scholar] [CrossRef]
- Zhang, Y.; Qi, F.; Lv, H.; Liang, F.; Wang, J. Bioradar Technology: Recent Research and Advancements. IEEE Microw. Mag. 2019, 20, 58–73. [Google Scholar] [CrossRef]
- Andersen., N.; Granhaug, K.; Michaelsen, J.A.; Bagga, S.; Hjortland, H.A.; Knutsen, M.R.; Lande, T.S.; Wisland, D.T. A 118-mW pulse-based radar soc in 55-nm CMOS for non-contact human vital signs detection. IEEE J. Solid-State Circuits 2017, 52, 3421–3433. [Google Scholar] [CrossRef]
- Wang, P.; Zhang, Y.; Ma, Y.; Liang, F.; An, Q.; Xue, H.; Yu, X.; Lv, H.; Wang, J. Method for Distinguishing Humans and Animals in Vital Signs Monitoring Using IR-UWB Radar. Int. J. Environ. Res. Public Health 2019, 16, 4462. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Qi, F.; Liu, M.; Liang, F.; Xue, H.; Zhang, Y.; Lv, H.; Wang, J. Noncontact Heart Rate Measurement Based on an Improved Convolutional Sparse Coding Method Using IR-UWB Radar. IEEE Access 2019, 7, 158492–158502. [Google Scholar] [CrossRef]
- Huang, T.Y.; Lin, J.; Hayward, L. Non-invasive measurement of laboratory rat’s cardiorespiratory movement using a 60-GHz radar and nonlinear Doppler phase modulation. In 2015 IEEE MTT-S 2015 International Microwave Workshop Series on RF and Wireless Technologies for Biomedical and Healthcare Applications (IMWS-BIO); IEEE: Piscataway, NJ, USA, 2015; pp. 83–84. [Google Scholar]
- Huang, T.Y.; Hayward, L.F.; Lin, J. Noninvasive measurement and analysis of laboratory rat’s cardiorespiratory movement. IEEE Trans. Microw. Theory Tech. 2016, 65, 574–581. [Google Scholar] [CrossRef]
- Churkin, S.; Anishchenko, L. Millimeter-wave radar for vital signs monitoring. In 2015 IEEE International Conference on Microwaves, Communications, Antennas and Electronic Systems (COMCAS); IEEE: Piscataway, NJ, USA, 2015; pp. 1–4. [Google Scholar]
- Hui, X.; Kan, E.C. No-touch measurements of vital signs in small conscious animals. Sci. Adv. 2019, 5, eaau0169. [Google Scholar] [CrossRef]
- Lazaro, A.; Girbau, D.; Villarino, R. Analysis of vital signs monitoring using an IR-UWB radar. Prog. Electromagn. Res. 2010, 100, 265–284. [Google Scholar] [CrossRef]
- Dragomiretskiy, K.; Zosso, D. Variational Mode Decomposition. IEEE Trans. Signal Process. 2014, 62, 531–544. [Google Scholar] [CrossRef]
- Wang, Y.; Markert, R.; Xiang, J.; Zheng, W. Research on variational mode decomposition and its application in detecting rub-impact fault of the rotor system. Mech. Syst. Signal Process. 2015, 60–61, 243–251. [Google Scholar] [CrossRef]
- Ming, Z.; Jiang, Z.; Feng, K. Research on variational mode decomposition in rolling bearings fault diagnosis of the multistage centrifugal pump. Mech. Syst. Signal Process. 2017, 93, 460–493. [Google Scholar]
- Lahmiri, S. Comparative study of ECG signal denoising by wavelet thresholding in empirical and variational mode decomposition domains. Healthc. Technol. Lett. 2014, 1, 104–109. [Google Scholar] [CrossRef]
- Shen, H.; Xu, C.; Yang, Y.; Sun, L.; Cai, Z.; Bai, L.; Clancy, E.; Huang, X. Respiration and Heartbeat Rates Measurement Based on Autocorrelation Using IR-UWB Radar. IEEE Trans. Circuits Syst. II Express Briefs 2018, 65, 1470–1474. [Google Scholar] [CrossRef]
- Xue, Y.J.; Cao, J.X.; Wang, D.X.; Du, H.-K.; Yao, Y. Application of the Variational-Mode Decomposition for Seismic Time–frequency Analysis. IEEE J. Sel. Top. Appl. Earth Obs. Remote Sens. 2017, 9, 3821–3831. [Google Scholar] [CrossRef]
- Pinheiro, E.; Postolache, O.; Girão, P. Theory and developments in an unobtrusive cardiovascular system representation: Ballistocardiography. Open Biomed. Eng. J. 2010, 4, 201. [Google Scholar] [CrossRef] [PubMed]
- Inan, O.T.; Migeotte, P.F.; Park, K.S.; Etemadi, M.; Tavakolian, K.; Casanella, R.; Zanetti, J.; Tank, J.; Funtova, I.; Prisk, G.K.; et al. Ballistocardiography and seismocardiography: A review of recent advances. IEEE J. Biomed. Health Inform. 2014, 19, 1414–1427. [Google Scholar] [CrossRef] [PubMed]
- Dong, S.; Zhang, Y.; Ma, C.; Zhu, C.; Gu, Z.; Lv, Q.; Zhang, B.; Li, C.; Ran, L. Doppler Cardiogram: A Remote Detection of Human Heart Activities. IEEE Trans. Microw. Theory Tech. 2019, 1–10. [Google Scholar] [CrossRef]
- Ferris, D.D., Jr.; Currie, N.C. Microwave and millimeter-wave systems for wall penetration. In Targets and Backgrounds: Characterization and Representation IV; International Society for Optics and Photonics: Bellingham, WA, USA, 1998; Volume 3375, pp. 269–279. [Google Scholar]
- Rong, Y.; Bliss, D.W. Smart Homes: See Multiple Heartbeats Through Wall Using Wireless Signals. In 2019 IEEE Radar Conference (RadarConf); IEEE: Piscataway, NJ, USA, 2019; pp. 1–6. [Google Scholar]
- International Commission on Non-Ionizing Radiation Protection (ICNIRP). Guidelines for limiting exposure to time-varying electric, magnetic, and electromagnetic fields (up to 300 GHz). Health Phys. 1998, 74, 494–522. [Google Scholar]


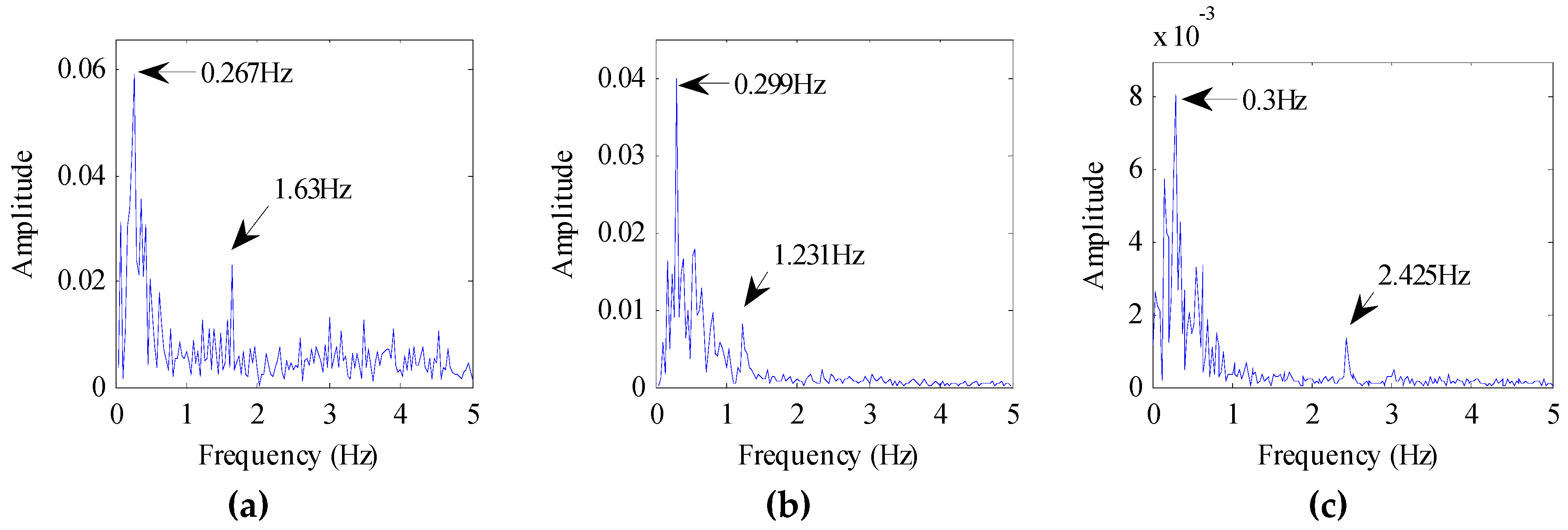
| Subject | Breathing (Hz) | Error | Heartbeat (Hz) | |
|---|---|---|---|---|
| Radar | Pressure Sensor | |||
| S1 | 0.266 | 0.27 | 1.5% | 1.63 |
| S2 | 0.412 | 0.42 | 1.9% | 2.10 |
| S3 | 0.219 | 0.23 | 4.8% | 1.83 |
| Subject | Breathing (Hz) | Error Rate | Heartbeat (Hz) | |
|---|---|---|---|---|
| Radar | Pressure Sensor | |||
| S1 | 0.556 | 0.56 | 0.7% | 2.10 |
| S2 | 0.447 | 0.46 | 2.9% | 2.68 |
| S3 | 0.497 | 0.49 | 1.4% | 2.88 |
| S4 | 0.547 | 0.56 | 2.2% | 1.99 |
| S5 | 0.483 | 0.47 | 2.8% | 2.17 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, P.; Ma, Y.; Liang, F.; Zhang, Y.; Yu, X.; Li, Z.; An, Q.; Lv, H.; Wang, J. Non-Contact Vital Signs Monitoring of Dog and Cat Using a UWB Radar. Animals 2020, 10, 205. https://doi.org/10.3390/ani10020205
Wang P, Ma Y, Liang F, Zhang Y, Yu X, Li Z, An Q, Lv H, Wang J. Non-Contact Vital Signs Monitoring of Dog and Cat Using a UWB Radar. Animals. 2020; 10(2):205. https://doi.org/10.3390/ani10020205
Chicago/Turabian StyleWang, Pengfei, Yangyang Ma, Fulai Liang, Yang Zhang, Xiao Yu, Zhao Li, Qiang An, Hao Lv, and Jianqi Wang. 2020. "Non-Contact Vital Signs Monitoring of Dog and Cat Using a UWB Radar" Animals 10, no. 2: 205. https://doi.org/10.3390/ani10020205
APA StyleWang, P., Ma, Y., Liang, F., Zhang, Y., Yu, X., Li, Z., An, Q., Lv, H., & Wang, J. (2020). Non-Contact Vital Signs Monitoring of Dog and Cat Using a UWB Radar. Animals, 10(2), 205. https://doi.org/10.3390/ani10020205





