Presence of Francisella tularensis subsp. holarctica DNA in the Aquatic Environment in France
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Collection and DNA Extraction
2.2. Francisella Species Detection
2.3. Amebae Detection
2.4. Statistical Analysis
3. Results
3.1. qPCR Controls
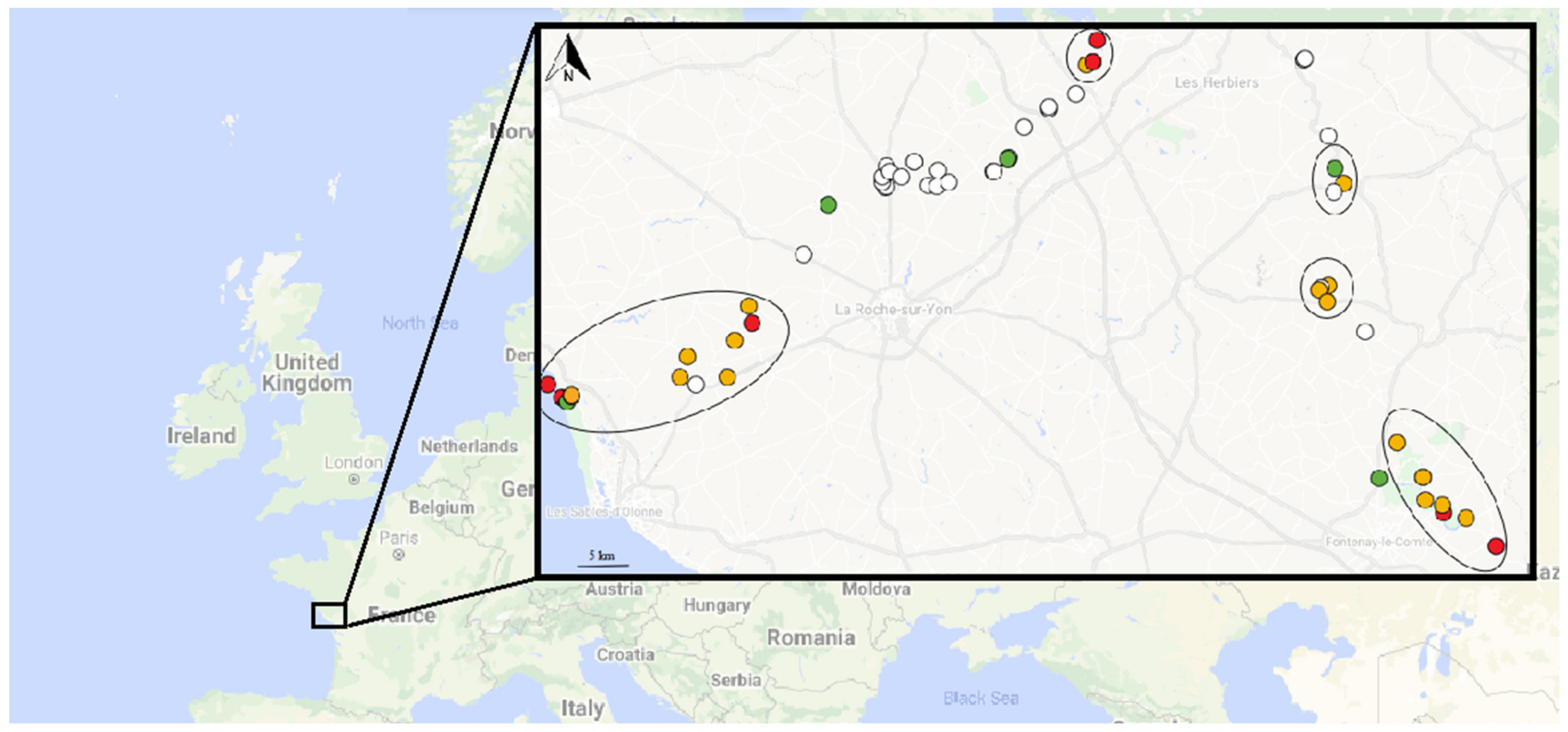
3.2. First Field Study
3.3. Second Field Study
4. Discussion
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Oyston, P.C.F.; Sjöstedt, A.; Titball, R.W. Tularaemia: Bioterrorism Defence Renews Interest in Francisella tularensis. Nat. Rev. Microbiol. 2004, 2, 967–978. [Google Scholar] [CrossRef]
- Sjostedt, A. Tularemia: History, Epidemiology, Pathogen Physiology, and Clinical Manifestations. Ann. N. Y. Acad. Sci. 2007, 1105, 1–29. [Google Scholar] [CrossRef]
- Jackson, J.; McGregor, A.; Cooley, L.; Ng, J.; Brown, M.; Ong, C.W.; Darcy, C.; Sintchenko, V. Francisella tularensis Subspecies Holarctica, Tasmania, Australia, 2011. Emerg. Infect. Dis. 2012, 18, 1484–1486. [Google Scholar] [CrossRef]
- Kuibagarov, M.; Kairzhanova, A.; Vergnaud, G.; Amirgazin, A.; Lukhnova, L.; Izbanova, U.; Ramankulov, Y.; Shevtsov, A. Draft Genome Sequence of the Strain Francisella tularensis Subsp. Mediasiatica 240, Isolated in Kazakhstan. Microbiol. Resour. Announc. 2020, 9. [Google Scholar] [CrossRef]
- Hennebique, A.; Boisset, S.; Maurin, M. Tularemia as a Waterborne Disease: A Review. Emerg. Microbes Infect. 2019, 8, 1027–1042. [Google Scholar] [CrossRef] [PubMed]
- Johansson, A.; Celli, J.; Conlan, W.; Elkins, K.L.; Forsman, M.; Keim, P.S.; Larsson, P.; Manoil, C.; Nano, F.E.; Petersen, J.M.; et al. Objections to the Transfer of Francisella Novicida to the Subspecies Rank of Francisella tularensis. Int. J. Syst. Evol. Microbiol. 2010, 60, 1717–1718, author reply 1718–1720. [Google Scholar] [CrossRef] [PubMed]
- Busse, H.-J.; Huber, B.; Anda, P.; Escudero, R.; Scholz, H.C.; Seibold, E.; Splettstoesser, W.D.; Kämpfer, P. Objections to the Transfer of Francisella Novicida to the Subspecies Rank of Francisella tularensis–Response to Johansson et al. Int. J. Syst. Evol. Microbiol. 2010, 60, 1718–1720. [Google Scholar] [CrossRef]
- Öhrman, C.; Sahl, J.W.; Sjödin, A.; Uneklint, I.; Ballard, R.; Karlsson, L.; McDonough, R.F.; Sundell, D.; Soria, K.; Bäckman, S.; et al. Reorganized Genomic Taxonomy of Francisellaceae Enables Design of Robust Environmental PCR Assays for Detection of Francisella tularensis. Microorganisms 2021, 9. [Google Scholar] [CrossRef] [PubMed]
- Maurin, M.; Gyuranecz, M. Tularaemia: Clinical Aspects in Europe. Lancet Infect. Dis. 2016, 16, 113–124. [Google Scholar] [CrossRef]
- Simşek, H.; Taner, M.; Karadenizli, A.; Ertek, M.; Vahaboğlu, H. Identification of Francisella tularensis by Both Culture and Real-Time TaqMan PCR Methods from Environmental Water Specimens in Outbreak Areas Where Tularemia Cases Were Not Previously Reported. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 2012, 31, 2353–2357. [Google Scholar] [CrossRef]
- Kilic, S.; Birdsell, D.N.; Karagöz, A.; Çelebi, B.; Bakkaloglu, Z.; Arikan, M.; Sahl, J.W.; Mitchell, C.; Rivera, A.; Maltinsky, S.; et al. Water as Source of Francisella tularensis Infection in Humans, Turkey. Emerg. Infect. Dis. 2015, 21, 2213–2216. [Google Scholar] [CrossRef] [PubMed]
- Janse, I.; van der Plaats, R.Q.J.; de Roda Husman, A.M.; van Passel, M.W.J. Environmental Surveillance of Zoonotic Francisella tularensis in the Netherlands. Front. Cell. Infect. Microbiol. 2018, 8, 140. [Google Scholar] [CrossRef] [PubMed]
- Kaysser, P.; Seibold, E.; Mätz-Rensing, K.; Pfeffer, M.; Essbauer, S.; Splettstoesser, W.D. Re-Emergence of Tularemia in Germany: Presence of Francisella tularensis in Different Rodent Species in Endemic Areas. BMC Infect. Dis. 2008, 8, 157. [Google Scholar] [CrossRef] [PubMed]
- Hightower, J.; Kracalik, I.T.; Vydayko, N.; Goodin, D.; Glass, G.; Blackburn, J.K. Historical Distribution and Host-Vector Diversity of Francisella tularensis, the Causative Agent of Tularemia, in Ukraine. Parasit. Vectors 2014, 7. [Google Scholar] [CrossRef] [PubMed]
- Broman, T.; Thelaus, J.; Andersson, A.-C.; Bäckman, S.; Wikström, P.; Larsson, E.; Granberg, M.; Karlsson, L.; Bäck, E.; Eliasson, H.; et al. Molecular Detection of Persistent Francisella tularensis Subspecies holarctica in Natural Waters. Int. J. Microbiol. 2011, 2011. [Google Scholar] [CrossRef] [PubMed]
- Duodu, S.; Larsson, P.; Sjödin, A.; Forsman, M.; Colquhoun, D.J. The Distribution of Francisella-like Bacteria Associated with Coastal Waters in Norway. Microb. Ecol. 2012, 64, 370–377. [Google Scholar] [CrossRef]
- Barns, S.M.; Grow, C.C.; Okinaka, R.T.; Keim, P.; Kuske, C.R. Detection of Diverse New Francisella-like Bacteria in Environmental Samples. Appl. Environ. Microbiol. 2005, 71, 5494–5500. [Google Scholar] [CrossRef]
- Petersen, J.M.; Carlson, J.; Yockey, B.; Pillai, S.; Kuske, C.; Garbalena, G.; Pottumarthy, S.; Chalcraft, L. Direct Isolation of Francisella Spp. from Environmental Samples. Lett. Appl. Microbiol. 2009, 48, 663–667. [Google Scholar] [CrossRef]
- Berrada, Z.L.; Telford, S.R. Diversity of Francisella Species in Environmental Samples from Martha’s Vineyard, Massachusetts. Microb. Ecol. 2010, 59, 277–283. [Google Scholar] [CrossRef][Green Version]
- Whitehouse, C.A.; Kesterson, K.E.; Duncan, D.D.; Eshoo, M.W.; Wolcott, M. Identification and Characterization of Francisella Species from Natural Warm Springs in Utah, USA. Lett. Appl. Microbiol. 2012, 54, 313–324. [Google Scholar] [CrossRef]
- Thompson, P.P.; Kowalski, R.P.; Shanks, R.M.Q.; Gordon, Y.J. Validation of Real-Time PCR for Laboratory Diagnosis of Acanthamoeba Keratitis. J. Clin. Microbiol. 2008, 46, 3232–3236. [Google Scholar] [CrossRef] [PubMed]
- Versage, J.L.; Severin, D.D.M.; Chu, M.C.; Petersen, J.M. Development of a Multitarget Real-Time TaqMan PCR Assay for Enhanced Detection of Francisella tularensis in Complex Specimens. J. Clin. Microbiol. 2003, 41, 5492–5499. [Google Scholar] [CrossRef]
- Kugeler, K.J.; Pappert, R.; Zhou, Y.; Petersen, J.M. Real-Time PCR for Francisella tularensis Types A and B. Emerg. Infect. Dis. 2006, 12, 1799–1801. [Google Scholar] [CrossRef]
- Feldman, K.A.; Matyas, B.T.; Stiles-Enos, D.; Hayes, E.B. An Outbreak of Primary Pneumonic Tularemia on Martha’s Vineyard. N. Engl. J. Med. 2001, 345, 1601–1606. [Google Scholar] [CrossRef] [PubMed]
- Johansson, A.; Lärkeryd, A.; Widerström, M.; Mörtberg, S.; Myrtännäs, K.; Öhrman, C.; Birdsell, D.; Keim, P.; Wagner, D.M.; Forsman, M.; et al. An Outbreak of Respiratory Tularemia Caused by Diverse Clones of Francisella tularensis. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2014, 59, 1546–1553. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, S.E.; Rose, L.J. Survival and Persistence of Nonspore-Forming Biothreat Agents in Water. Lett. Appl. Microbiol. 2012, 55, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Berrada, Z.L.; Telford, S.R., III. Survival of Francisella tularensis Type A in Brackish-Water. Arch. Microbiol. 2011, 193, 223–226. [Google Scholar] [CrossRef]
- Forsman, M.; Henningson, E.W.; Larsson, E.; Johansson, T.; Sandström, G. Francisella tularensis Does Not Manifest Virulence in Viable but Non-Culturable State. FEMS Microbiol. Ecol. 2000, 31, 217–224. [Google Scholar] [CrossRef]
- Golovliov, I.; Bäckman, S.; Granberg, M.; Salomonsson, E.; Lundmark, E.; Näslund, J.; Busch, J.D.; Birdsell, D.; Sahl, J.W.; Wagner, D.M.; et al. Long-Term Survival of Virulent Tularemia Pathogens Outside a Host in Conditions That Mimic Natural Aquatic Environments. Appl. Environ. Microbiol. 2021, 87. [Google Scholar] [CrossRef]
- Abd, H.; Johansson, T.; Golovliov, I.; Sandström, G.; Forsman, M. Survival and Growth of Francisella tularensis in Acanthamoeba castellanii. Appl. Environ. Microbiol. 2003, 69, 600–606. [Google Scholar] [CrossRef]
- El-Etr, S.H.; Margolis, J.J.; Monack, D.; Robison, R.A.; Cohen, M.; Moore, E.; Rasley, A. Francisella Tularensis Type A Strains Cause the Rapid Encystment of Acanthamoeba Castellanii and Survive in Amoebal Cysts for Three Weeks Postinfection. Appl. Environ. Microbiol. 2009, 75, 7488–7500. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Buse, H.Y.; Schaefer Iii, F.W.; Rice, E.W. Enhanced Survival but Not Amplification of Francisella Spp. in the Presence of Free-Living Amoebae. Acta Microbiol. Immunol. Hung. 2017, 64, 17–36. [Google Scholar] [CrossRef]
- Hennebique, A.; Peyroux, J.; Brunet, C.; Martin, A.; Henry, T.; Knezevic, M.; Santic, M.; Boisset, S.; Maurin, M. Amoebae Can Promote the Survival of Francisella Species in the Aquatic Environment. Emerg. Microbes Infect. 2021, 10, 277–290. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Zaragoza, S. Ecology of Free-Living Amoebae. Crit. Rev. Microbiol. 1994, 20, 225–241. [Google Scholar] [CrossRef] [PubMed]
- Van Hoek, M.L. Biofilms: An Advancement in Our Understanding of Francisella Species. Virulence 2013, 4, 833–846. [Google Scholar] [CrossRef] [PubMed]
- Thelaus, J.; Andersson, A.; Broman, T.; Bäckman, S.; Granberg, M.; Karlsson, L.; Kuoppa, K.; Larsson, E.; Lundmark, E.; Lundström, J.O.; et al. Francisella tularensis Subspecies holarctica Occurs in Swedish Mosquitoes, Persists through the Developmental Stages of Laboratory-Infected Mosquitoes and Is Transmissible during Blood Feeding. Microb. Ecol. 2014, 67, 96–107. [Google Scholar] [CrossRef]
| qPCR (Target) | Primers/Probes | 5′ to 3′ DNA Sequence | Amplicon Size | Species Detected | Reference |
|---|---|---|---|---|---|
| ISFtu2-qPCR (ISFtu2 insertion sequence element) | Forward | ttggtagatcagttggtgggataac | 97 bp | Francisella sp. | [22] |
| Reverse | tgagttttaccttctgacaacaatatttc | ||||
| Probe | FAM-aaatccatgctatgactgatgctttaggtaatcca-BHQ1 | ||||
| Tul4-qPCR (tul4 gene) | Forward | attacaatggcaggctccaga | 91 bp | F. tularensis and F. novicida | [22] |
| Reverse | tgcccaagttttatcgttcttct | ||||
| Probe | FAM-ttctaagtgccatgatacaagcttcccaattactaag-BHQ1 | ||||
| Type B-qPCR (junction between ISFtu2 and a specific flanking 3′ region) | Forward | cttgtacttttatttggctactgagaaact | 144 bp | F. tularensis subsp. holarctica | [23] |
| Reverse | cttgcttggtttgtaaatatagtggaa | ||||
| Probe | FAM-acctagttcaacc*t*caagacttttagtaatgggaatgtca-BHQ1 Internal quencher | ||||
| Acanth-qPCR (Acanthamoeba sp. 18 S rDNA) | Forward | cccagatcgtttaccgtgaa | 180 bp | Acanthamoeba sp. | [21] |
| Reverse | taaatattaatgcccccaactatcc | ||||
| Probe | FAM-ctgccaccgaatacattagcatgg-BHQ1 |
| DNA Extracts | ISFtu2-qPCR (Ct) | Tul4-qPCR (Ct) | Type B-qPCR (Ct) |
|---|---|---|---|
| Serratia marcescens CIP 103551 * | 37 | Negative | Negative |
| Streptococcus equi ATCC 43079 * | 37 | Negative | Negative |
| F. noatunensis LMG 23800 * | 36 | Negative | Negative |
| F. philomiragia ATCC 25015 * | 36 | Negative | Negative |
| F. novicida U112 * | 12 | 16 | Negative |
| Clinical strain Ft92 of F. tularensis subsp. holarctica * | 12 | 15 | 16 |
| LVS-spiked water 0.1 CFU/l | 38 | Negative | Negative |
| LVS-spiked water 1 CFU/l | 36 | Negative | Negative |
| LVS-spiked water 10 CFU/l | 36 | 37 | Negative |
| LVS-spiked water 100 CFU/l | 34 | 38 | 38 |
| LVS-spiked water 1000 CFU/l | 27 | 33 | 33 |
| LVS-spiked water 10,000 CFU/l | 25 | 30 | 30 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brunet, C.D.; Hennebique, A.; Peyroux, J.; Pelloux, I.; Caspar, Y.; Maurin, M. Presence of Francisella tularensis subsp. holarctica DNA in the Aquatic Environment in France. Microorganisms 2021, 9, 1398. https://doi.org/10.3390/microorganisms9071398
Brunet CD, Hennebique A, Peyroux J, Pelloux I, Caspar Y, Maurin M. Presence of Francisella tularensis subsp. holarctica DNA in the Aquatic Environment in France. Microorganisms. 2021; 9(7):1398. https://doi.org/10.3390/microorganisms9071398
Chicago/Turabian StyleBrunet, Camille D., Aurélie Hennebique, Julien Peyroux, Isabelle Pelloux, Yvan Caspar, and Max Maurin. 2021. "Presence of Francisella tularensis subsp. holarctica DNA in the Aquatic Environment in France" Microorganisms 9, no. 7: 1398. https://doi.org/10.3390/microorganisms9071398
APA StyleBrunet, C. D., Hennebique, A., Peyroux, J., Pelloux, I., Caspar, Y., & Maurin, M. (2021). Presence of Francisella tularensis subsp. holarctica DNA in the Aquatic Environment in France. Microorganisms, 9(7), 1398. https://doi.org/10.3390/microorganisms9071398







