Bugs That Can Resist Antibiotics but Not Men: Gender-Specific Differences in Notified Infections and Colonisations in Germany, 2010–2019
Abstract
1. Introduction
2. Materials and Methods
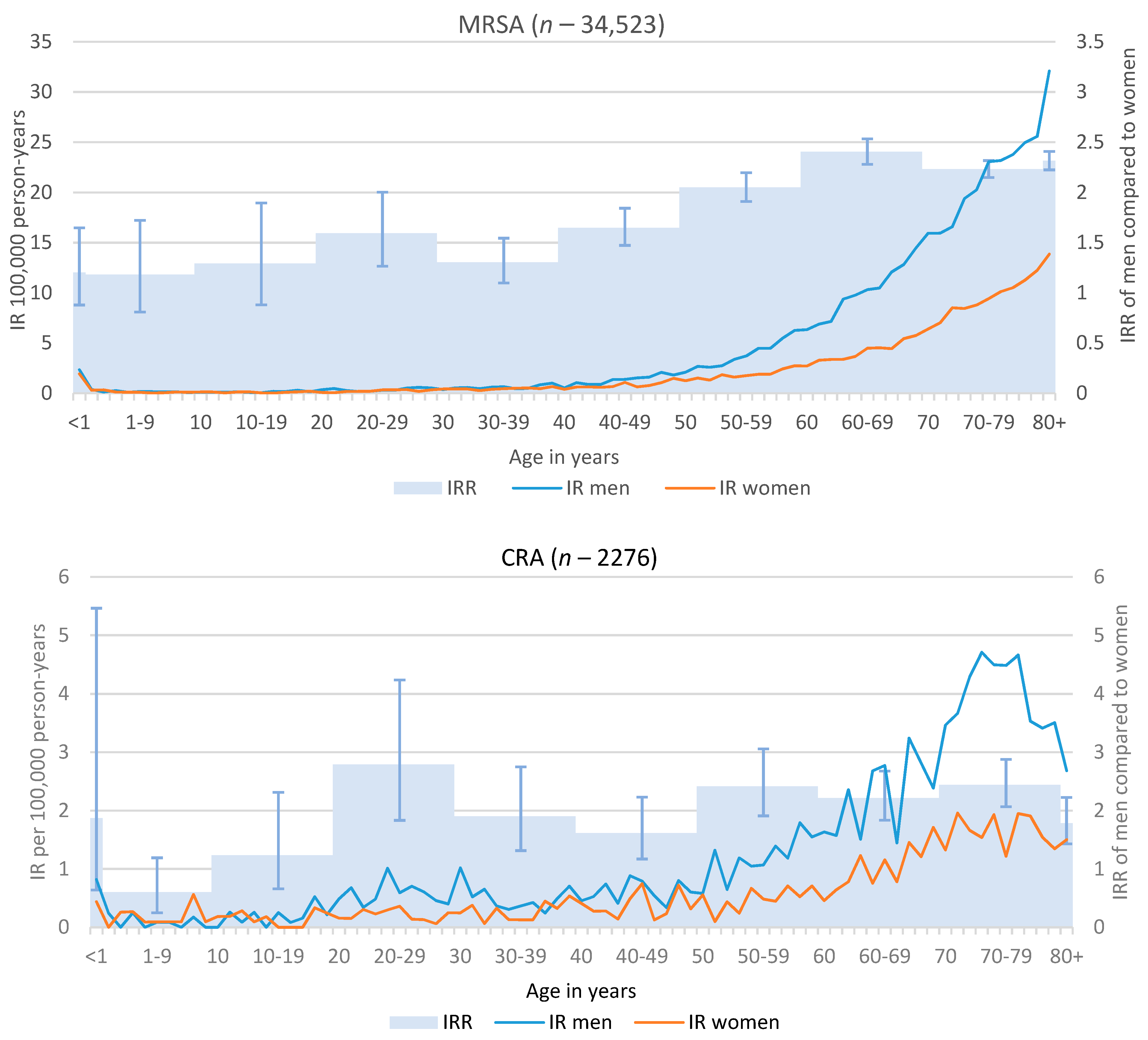
- Invasive infections with Methicillin-resistant Staphylococcus aureus (MRSA), i.e., detection of MRSA in laboratory specimen from blood or cerebrospinal fluid;
- Infections or colonisations with Acinetobacter spp. (CRA) with carbapenem-non-susceptibility or detection of a carbapenemase determinant;
- Infections or colonisations with Enterobacterales (CRE) with carbapenem-non-susceptibility or detection of a carbapenemase determinant.
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Ten Threats to Global Health in 2019. Available online: www.who.int/news-room/feature-stories/ten-threats-to-global-health-in-2019 (accessed on 2 February 2021).
- Cassini, A.; Högberg, L.D.; Plachouras, D.; Quattrocchi, A.; Hoxha, A.; Simonsen, G.S.; Colomb-Cotinat, M.; Kretzschmar, M.E.; Devleesschauwer, B.; Cecchini, M.; et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect. Dis. 2019, 19, 56–66. [Google Scholar] [CrossRef]
- Dunachie, S.J.; Day, N.P.J.; Dolecek, C. The challenges of estimating the human global burden of disease of antimicrobial resistant bacteria. Curr. Opin. Microbiol. 2020, 57, 95–101. [Google Scholar] [CrossRef]
- Limmathurotsakul, D.; Dunachie, S.; Fukuda, K.; Feasey, N.A.; Okeke, I.N.; Holmes, A.H.; Moore, C.E.; Dolecek, C.; van Doorn, H.R.; Shetty, N.; et al. Improving the estimation of the global burden of antimicrobial resistant infections. Lancet Infect. Dis. 2019, 19, e392–e398. [Google Scholar] [CrossRef]
- World Health Organization. Tackling Antimicrobial Resistance (AMR) Together. Working Paper 5.0: Enhancing the Focus on Gender and Equity; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- European Centre for Disease Prevention and Control. Country Summaries-Antimicrobial Resistance in the EU/EEA (EARS-Net) 2019. Available online: https://www.ecdc.europa.eu/en/publications-data/surveillance-antimicrobial-resistance-europe-2019 (accessed on 7 February 2021).
- Walter, J.; Haller, S.; Blank, H.-P.; Eckmanns, T.; Abu Sin, M.; Hermes, J. Incidence of invasive meticillin-resistant Staphylococcus aureus infections in Germany, 2010 to 2014. Eurosurveillance 2015, 20. [Google Scholar] [CrossRef] [PubMed]
- Koppe, U.; von Laer, A.; Kroll, L.E.; Noll, I.; Feig, M.; Schneider, M.; Claus, H.; Eckmanns, T.; Abu Sin, M. Carbapenem non-susceptibility of Klebsiella pneumoniae isolates in hospitals from 2011 to 2016, data from the German Antimicrobial Resistance Surveillance (ARS). Antimicrob. Resist. Infect. Control 2018, 7, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Humphreys, H.; Fitzpatick, F.; Harvey, B.J. Gender differences in rates of carriage and bloodstream infection caused by methicillin-resistant Staphylococcus aureus: Are they real, do they matter and why? Clin. Infect. Dis. 2015, 61, 1708–1714. [Google Scholar] [CrossRef] [PubMed]
- Shindo, Y.; Hasegawa, Y. Regional differences in antibiotic-resistant pathogens in patients with pneumonia: Implications for clinicians. Respirology 2017, 22, 1536–1546. [Google Scholar] [CrossRef]
- Allel, K.; García, P.; Labarca, J.; Munita, J.M.; Rendic, M.; Undurraga, E.A. Socioeconomic factors associated with antimicrobial resistance of Pseudomonas aeruginosa, Staphylococcus aureus, and Escherichia coli in Chilean hospitals (2008–2017). Rev. Panam. Salud Publica 2020, 44, e30. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Antimicrobial Resistance in the EU/EEA (EARS-Net)-Annual Epidemiological Report 2019; ECDC: Stockholm, Sweden, 2020. [Google Scholar]
- Federal Ministry of Justice and Consumer Protection. Section 7 of the German Infection Protection Act (IfSG). Available online: https://www.gesetze-im-internet.de/ifsg/__7.html (accessed on 10 February 2021).
- Robert Koch-Institut. Infektionsepidemiologisches Jahrbuch Meldepflichtiger Krankheiten Für 2019; Robert Koch-Institut: Berlin, Germany, 2020. Available online: https://www.rki.de/DE/Content/Infekt/Jahrbuch/Jahrbuch_2019.pdf?__blob=publicationFile (accessed on 7 February 2021).
- Bäurle, H.; Tamásy, C. Regionale Konzentrationen der Nutztierhaltung in Deutschland; ISPA: Augsburg, Germany, 2011. [Google Scholar]
- Federal Ministry of Food and Agriculture. Bevölkerungsdichte. Available online: https://www.landatlas.de/laendlich/bevdichte.html (accessed on 13 February 2021).
- Kroll, L.E.; Schumann, M.; Hoebel, J.; Lampert, T. Regional Health Differences—Developing a Socioeconomic Deprivation Index for Germany; Robert Koch-Institut: Berlin, Germany, 2017. [CrossRef]
- van Lunzen, J.; Altfeld, M. Sex differences in infectious diseases-common but neglected. J. Infect. Dis. 2014, 209 (Suppl. 3), S79–S80. [Google Scholar] [CrossRef]
- Schröder, W.; Sommer, H.; Gladstone, B.P.; Foschi, F.; Hellman, J.; Evengard, B.; Tacconelli, E. Gender differences in antibiotic prescribing in the community: A systematic review and meta-analysis. J. Antimicrob. Chemother. 2016, 71, 1800–1806. [Google Scholar] [CrossRef]
- Vincent, J.-L.; Sakr, Y.; Singer, M.; Martin-Loeches, I.; Machado, F.R.; Marshall, J.C.; Finfer, S.; Pelosi, P.; Brazzi, L.; Aditianingsih, D.; et al. Prevalence and Outcomes of Infection Among Patients in Intensive Care Units in 2017. JAMA 2020, 323, 1478–1487. [Google Scholar] [CrossRef]
- Neubeiser, A.; Bonsignore, M.; Tafelski, S.; Alefelder, C.; Schwegmann, K.; Rüden, H.; Geffers, C.; Nachtigall, I. Mortality attributable to hospital acquired infections with multidrug-resistant bacteria in a large group of German hospitals. J. Infect. Public Health 2020, 13, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Jansen, K.; Schmidt, A.J.; Drewes, J.; Bremer, V.; Marcus, U. Increased incidence of syphilis in men who have sex with men and risk management strategies, Germany, 2015. Eurosurveillance 2016, 21, 30382. [Google Scholar] [CrossRef] [PubMed]
- Werner, R.N.; Gaskins, M.; Nast, A.; Dressler, C. Incidence of sexually transmitted infections in men who have sex with men and who are at substantial risk of HIV infection—A meta-analysis of data from trials and observational studies of HIV pre-exposure prophylaxis. PLoS ONE 2018, 13, e0208107. [Google Scholar] [CrossRef]
- Naik, F.; Zhao, H.; Harrison, T.; Phin, N. Legionnaires’ disease in England and Wales, 2011. Health Prot Rep 2012, 2013. [Google Scholar]
- Farnham, A.; Alleyne, L.; Cimini, D.; Balter, S. Legionnaires’ Disease Incidence and Risk Factors, New York, New York, USA, 2002–2011. Emerg. Infect. Dis. J. 2014, 20, 1795. [Google Scholar] [CrossRef] [PubMed]
- Nhamoyebonde, S.; Leslie, A. Biological Differences Between the Sexes and Susceptibility to Tuberculosis. J. Infect. Dis. 2014, 209, S100–S106. [Google Scholar] [CrossRef]
- Leone, M.; Honstettre, A.; Lepidi, H.; Capo, C.; Bayard, F.; Raoult, D.; Mege, J.-L. Effect of Sex on Coxiella burnetii Infection: Protective Role of 17β-Estradiol. J. Infect. Dis. 2004, 189, 339–345. [Google Scholar] [CrossRef]
- Vázquez-Martínez, E.R.; García-Gómez, E.; Camacho-Arroyo, I.; González-Pedrajo, B. Sexual dimorphism in bacterial infections. Biol. Sex Differ. 2018, 9, 27. [Google Scholar] [CrossRef]
- Yuan, W.L.; Shen, Y.J.; Deng, D.Y. Sex bias of Acinetobacter baumannii nosocomial infection. Am. J. Infect. Control 2018, 46, 957–958. [Google Scholar] [CrossRef]
- Ayobami, O.; Willrich, N.; Suwono, B.; Eckmanns, T.; Markwart, R. The epidemiology of carbapenem-non-susceptible Acinetobacter species in Europe: Analysis of EARS-Net data from 2013 to 2017. Antimicrob. Resist. Infect. Control 2020, 9, 89. [Google Scholar] [CrossRef] [PubMed]
- Schmithausen, R.M.; Schulze-Geisthoevel, S.V.; Heinemann, C.; Bierbaum, G.; Exner, M.; Petersen, B.; Steinhoff-Wagner, J. Reservoirs and Transmission Pathways of Resistant Indicator Bacteria in the Biotope Pig Stable and along the Food Chain: A Review from a One Health Perspective. Sustainability 2018, 10, 3967. [Google Scholar] [CrossRef]
- Alvarez-Uria, G.; Gandra, S.; Laxminarayan, R. Poverty and prevalence of antimicrobial resistance in invasive isolates. Int. J. Infect. Dis. 2016, 52, 59–61. [Google Scholar] [CrossRef] [PubMed]

| MRSA * | CRA ** | CRE ** | |||
|---|---|---|---|---|---|
| All Notifications | All Notifications | Only Infections *** | All Notifications | Only Infections *** | |
| n (%) | n (%) | n (%) | n (%) | n (%) | |
| Gender | |||||
| Female | 12,510 (36.2) | 781 (34.3) | 191 (33.6) | 4553 (37.9) | 1076 (40.8) |
| Male | 22,013 (63.8) | 1495 (65.7) | 377 (66.4) | 7447 (62.1) | 1564 (59.2) |
| Age group in years | |||||
| <1 | 162 (0.5) | 15 (0.7) | 2 (0.4) | 352 (2.9) | 31 (1.1) |
| 1–9 | 109 (0.3) | 28 (1.2) | 3 (0.5) | 202 (1.7) | 46 (1.7) |
| 10–19 | 108 (0.3) | 40 (1.8) | 7 (1.2) | 154 (1.3) | 29 (1.1) |
| 20–29 | 313 (0.9) | 118 (5.2) | 21 (3.7) | 434 (3.6) | 95 (3.6) |
| 30–39 | 546 (1.6) | 127 (5.6) | 21 (3.7) | 536 (4.5) | 97 (3.7) |
| 40–49 | 1321 (3.8) | 158 (6.9) | 46 (8.1) | 650 (5.4) | 140 (5.3) |
| 50–59 | 3585 (10.4) | 342 (15.0) | 87 (15.3) | 1580 (13.1) | 355 (13.4) |
| 60–69 | 6594 (19.1) | 496 (21.8) | 138 (24.3) | 2633 (21.8) | 588 (22.2) |
| 70–79 | 11,940 (34.6) | 640 (28.1) | 168 (29.6) | 3277 (27.2) | 710 (26.7) |
| 80+ | 9873 (28.6) | 314 (13.8) | 75 (13.2) | 2237 (18.6) | 564 (21.2) |
| Federal state of residence | |||||
| Baden-Württemberg | 1859 (5.4) | 206 (9.0) | 54 (9.5) | 1316 (10.9) | 297 (11.2) |
| Bavaria | 2761 (8.0) | 284 (12.5) | 67 (11.8) | 1575 (13.1) | 350 (13.2) |
| Berlin | 2407 (7.0) | 268 (11.8) | 73 (12.9) | 1006 (8.4) | 304 (11.5) |
| Brandenburg | 1256 (3.6) | 46 (2.0) | 15 (2.6) | 257 (2.1) | 58 (2.2) |
| Bremen | 254 (0.7) | 14 (0.6) | 4 (0.7) | 87 (0.7) | 31 (1.2) |
| Hamburg | 431 (1.3) | 116 (5.1) | 31 (5.5) | 378 (3.1) | 82 (3.1) |
| Hessen | 1874 (5.4) | 300 (13.2) | 40 (7.0) | 1622 (13.5) | 209 (7.9) |
| Lower Saxony | 4427 (12.8) | 133 (5.8) | 37 (6.5) | 612 (5.1) | 107 (4.0) |
| Mecklenburg-Vorpommern | 1122 (3.3) | 18 (0.8) | 7 (1.2) | 109 (0.9) | 31 (1.2) |
| North Rhine-Westphalia | 10,654 (30.9) | 587 (25.8) | 157 (27.6) | 2813 (23.3) | 791 (29.8) |
| Rhineland-Palatinate | 1076 (3.1) | 79 (3.5) | 13 (2.3) | 577 (4.8) | 81 (3.1) |
| Saarland | 291 (0.8) | 7 (0.3) | 1 (0.2) | 124 (1.0) | 5 (0.2) |
| Saxony | 2321 (6.7) | 94 (4.1) | 30 (5.3) | 582 (4.8) | 115 (4.3) |
| Saxony-Anhalt | 1577 (4.6) | 31 (1.4) | 14 (2.5) | 387 (3.2) | 78 (2.9) |
| Schleswig-Holstein | 1276 (3.7) | 48 (2.1) | 10 (1.8) | 266 (2.2) | 42 (1.6) |
| Thuringia | 935 (2.7) | 47 (2.1) | 15 (2.6) | 341 (2.8) | 74 (2.8) |
| Year of notification | |||||
| 2010 | 3754 (10.9) | ||||
| 2011 | 4226 (12.2) | ||||
| 2012 | 4487 (13.0) | ||||
| 2013 | 4373 (12.7) | ||||
| 2014 | 3850 (11.1) | ||||
| 2015 | 3612 (10.5) | ||||
| 2016 | 3183 (9.2) | ||||
| 2017 | 2832 (8.2) | 787 (34.6) | 193 (34.0) | 3444 (28.6) | 695 (26.2) |
| 2018 | 2433 (7.0) | 780 (34.2) | 196 (34.5) | 3938 (32.7) | 910 (34.3) |
| 2019 | 1801 (5.2) | 710 (31.2) | 179 (31.5) | 4673 (38.8) | 1050 (39.6) |
| Hospitalisation status | |||||
| Inpatient | 31,315 (90.6) | 1905 (83.6) | 493 (86.8) | 10,329 (85.7) | 2281 (85.9) |
| Outpatient | 2026 (5.9) | 227 (10.0) | 50 (8.8) | 979 (8.1) | 290 (10.9) |
| Life status | |||||
| Deceased | 3781 (10.9) | 132 (5.8) | 58 (10.2) | 545 (4.5) | 188 (7.1) |
| Not deceased | 30,047 (87.0) | 2119 (93.0) | 506 (89.1) | 11,362 (94.3) | 2449 (92.2) |
| MRSA | CRA | CRE | ||||
|---|---|---|---|---|---|---|
| Cr. IRR (95%CI) | Adj. IRR * (95%CI) | Cr. IRR (95%CI) | Adj. IRR * (95%CI) | Cr. IRR (95%CI) | Adj. IRR * (95%CI) | |
| Infection | 2.0 (1.7–2.4) | 2.2 (1.9–2.7) | 1.5 (1.4–1.6) | 1.7 (1.6–1.8) | ||
| Colonisation | 2.1 (1.8–2.3) | 2.3 (2.0–2.6) | 1.8 (1.7–1.9) | 2.0 (1.9–2.1) | ||
| Inpatient | 1.8 (1.7–1.8) | 2.3 (2.2–2.3) | 2.0 (1.8–2.2) | 2.3 (2.0–2.5) | 1.7 (1.6–1.8) | 1.9 (1.9–2.0) |
| Outpatient | 1.8 (1.7–2.0) | 2.4 (2.1–2.6) | 1.4 (1.1–1.8) | 1.6 (1.2–2.0) | 1.3 (1.1–1.4) | 1.4 (1.3–1.6) |
| Deceased | 1.6 (1.5–1.7) | 2.2 (2.1–2.4) | 1.8 (1.3–2.6) | 2.1 (1.5–3.0) | 1.8 (1.5–2.1) | 2.2 (1.8–2.6) |
| Not deceased | 1.8 (1.8–1.8) | 2.4 (2.2–2.3) | 1.9 (1.7–2.1) | 2.1 (2.0–2.3) | 1.6 (1.6–1.7) | 1.9 (1.8–1.9) |
| All notifications | 1.8 (1.7–1.8) | 2.3 (2.2–2.3) | 1.9 (1.8–2.1) | 2.2 (2.0–2.4) | 1.6 (1.6–1.7) | 1.9 (1.8–2.0) |
| Age Group | HR Men | HR Women | HRR (Men/Women) | Adjusted HR 1 Women | Adjusted HRR 1 (Men/Women) |
|---|---|---|---|---|---|
| <1 | 127,842 | 122,316 | 1.05 | 122,316 | 1.05 |
| 1–9 | 9376 | 7430 | 1.26 | 7430 | 1.26 |
| 10–19 | 8653 | 11,000 | 0.79 | 10,281 | 0.84 |
| 20–29 | 9558 | 18,238 | 0.52 | 9553 | 1.00 |
| 30–39 | 10,757 | 20,842 | 0.52 | 10,012 | 1.07 |
| 40–49 | 14,496 | 14,846 | 0.98 | 13,965 | 1.04 |
| 50–59 | 21,415 | 18,167 | 1.18 | 18,164 | 1.18 |
| 60–69 | 33,608 | 25,517 | 1.32 | 25,517 | 1.32 |
| 70–79 | 53,561 | 42,981 | 1.25 | 42,981 | 1.25 |
| 80+ | 71,558 | 62,643 | 1.14 | 62,643 | 1.14 |
| Overall | 23,121 | 24,523 | 0.94 | 22,038 | 1.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brandl, M.; Hoffmann, A.; Willrich, N.; Reuss, A.; Reichert, F.; Walter, J.; Eckmanns, T.; Haller, S. Bugs That Can Resist Antibiotics but Not Men: Gender-Specific Differences in Notified Infections and Colonisations in Germany, 2010–2019. Microorganisms 2021, 9, 894. https://doi.org/10.3390/microorganisms9050894
Brandl M, Hoffmann A, Willrich N, Reuss A, Reichert F, Walter J, Eckmanns T, Haller S. Bugs That Can Resist Antibiotics but Not Men: Gender-Specific Differences in Notified Infections and Colonisations in Germany, 2010–2019. Microorganisms. 2021; 9(5):894. https://doi.org/10.3390/microorganisms9050894
Chicago/Turabian StyleBrandl, Michael, Alexandra Hoffmann, Niklas Willrich, Annicka Reuss, Felix Reichert, Jan Walter, Tim Eckmanns, and Sebastian Haller. 2021. "Bugs That Can Resist Antibiotics but Not Men: Gender-Specific Differences in Notified Infections and Colonisations in Germany, 2010–2019" Microorganisms 9, no. 5: 894. https://doi.org/10.3390/microorganisms9050894
APA StyleBrandl, M., Hoffmann, A., Willrich, N., Reuss, A., Reichert, F., Walter, J., Eckmanns, T., & Haller, S. (2021). Bugs That Can Resist Antibiotics but Not Men: Gender-Specific Differences in Notified Infections and Colonisations in Germany, 2010–2019. Microorganisms, 9(5), 894. https://doi.org/10.3390/microorganisms9050894






