Anti-Classical Swine Fever Virus Strategies
Abstract
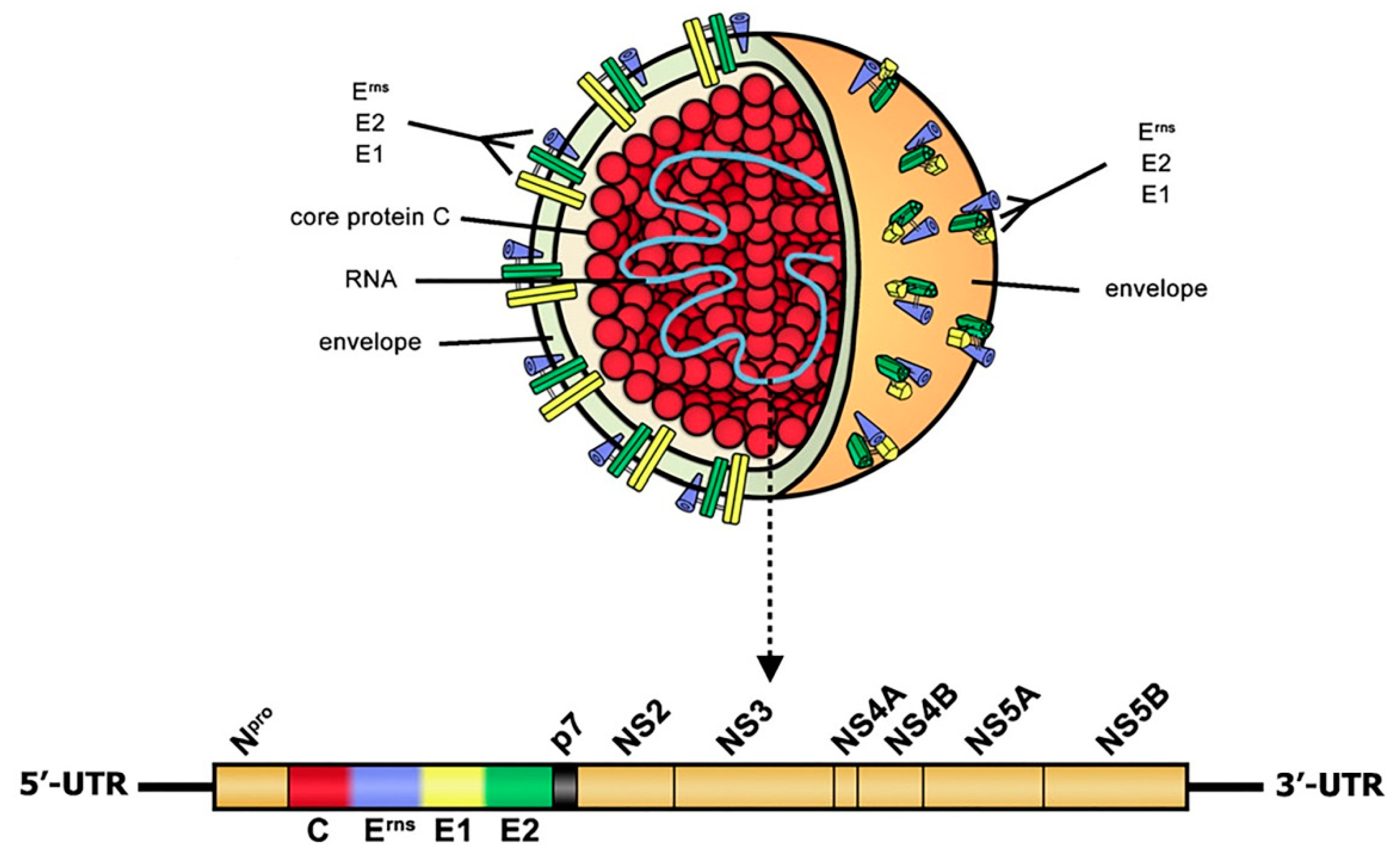
1. Introduction
2. Host Proteins with Anti-CSFV Effects
3. Host Proteins Whose Function Defect Exert Anti-CSFV Effects
4. Drug Candidates with Anti-CSFV Effects
5. RNA Interference (RNAi) Targeting Viral Genes
6. Concluding Remarks and Prospects
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Paton, D.J.; Greiser-Wilke, I. Classical swine fever—An update. Res. Vet. Sci. 2003, 75, 169–178. [Google Scholar] [CrossRef]
- Moennig, V. The control of classical swine fever in wild boar. Front. Microbiol. 2015, 6, 1211. [Google Scholar] [CrossRef] [PubMed]
- Thiel, H.J.; Stark, R.; Weiland, E.; Rümenapf, T.; Meyers, G. Hog cholera virus: Molecular composition of virions from a pestivirus. J. Virol. 1991, 65, 4705–4712. [Google Scholar] [CrossRef] [PubMed]
- Beer, M.; Reimann, I.; Hoffmann, B.; Depner, K. Novel marker vaccines against classical swine fever. Vaccine 2007, 25, 5665–5670. [Google Scholar] [CrossRef] [PubMed]
- Paton, D.J.; McGoldrick, A.; Greiser-Wilke, I.; Parchariyanon, S.; Song, J.Y.; Liou, P.P.; Stadejek, T.; Lowings, J.P.; Björklund, H.; Belák, S. Genetic typing of classical swine fever virus. Vet. Microbiol. 2000, 73, 137–157. [Google Scholar] [CrossRef]
- Postel, A.; Schmeiser, S.; Perera, C.L.; Rodríguez, L.J.; Frias-Lepoureau, M.T.; Becher, P. Classical swine fever virus isolates from Cuba form a new subgenotype 1.4. Vet. Microbiol. 2013, 161, 334–338. [Google Scholar] [CrossRef] [PubMed]
- Deng, M.C.; Huang, C.C.; Huang, T.S.; Chang, C.Y.; Lin, Y.J.; Chien, M.S.; Jong, M.H. Phylogenetic analysis of classical swine fever virus isolated from Taiwan. Vet. Microbiol. 2005, 106, 187–193. [Google Scholar] [CrossRef]
- Pan, C.H.; Jong, M.H.; Huang, T.S.; Liu, H.F.; Lin, S.Y.; Lai, S.S. Phylogenetic analysis of classical swine fever virus in Taiwan. Arch. Virol. 2005, 150, 1101–1119. [Google Scholar] [CrossRef]
- Jiang, D.L.; Gong, W.J.; Li, R.C.; Liu, G.H.; Hu, Y.F.; Ge, M.; Wang, S.Q.; Yu, X.L.; Tu, C. Phylogenetic analysis using E2 gene of classical swine fever virus reveals a new subgenotype in China. Infect. Genet. Evol. 2013, 17, 231–238. [Google Scholar] [CrossRef]
- Gong, W.; Wu, J.; Lu, Z.; Zhang, L.; Qin, S.; Chen, F.; Peng, Z.; Wang, Q.; Ma, L.; Bai, A.; et al. Genetic diversity of subgenotype 2.1 isolates of classical swine fever virus. Infect. Genet. Evol. 2016, 41, 218–226. [Google Scholar] [CrossRef]
- Zhou, B. Classical Swine Fever in China-An Update Minireview. Front. Vet. Sci. 2019, 6, 187. [Google Scholar] [CrossRef]
- Postel, A.; Nishi, T.; Kameyama, K.I.; Meyer, D.; Suckstorff, O.; Fukai, K.; Becher, P. Reemergence of Classical Swine Fever, Japan, 2018. Emerg. Infect. Dis. 2019, 25, 1228–1231. [Google Scholar] [CrossRef]
- Blome, S.; Staubach, C.; Henke, J.; Carlson, J.; Beer, M. Classical Swine Fever-An Updated Review. Viruses 2017, 9, 86. [Google Scholar] [CrossRef] [PubMed]
- Malik, Y.S.; Bhat, S.; Kumar, O.R.V.; Yadav, A.K.; Sircar, S.; Ansari, M.I.; Sarma, D.K.; Rajkhowa, T.K.; Ghosh, S.; Dhama, K. Classical Swine Fever Virus Biology, Clinicopathology, Diagnosis, Vaccines and a Meta-Analysis of Prevalence: A Review from the Indian Perspective. Pathogens 2020, 9, 500. [Google Scholar] [CrossRef] [PubMed]
- Brown, V.R.; Bevins, S.N. A Review of Classical Swine Fever Virus and Routes of Introduction into the United States and the Potential for Virus Establishment. Front. Vet. Sci. 2018, 5, 31. [Google Scholar] [CrossRef] [PubMed]
- Hao, G.; Zhang, H.; Chen, H.; Qian, P.; Li, X. Comparison of the Pathogenicity of Classical Swine Fever Virus Subgenotype 2.1c and 2.1d Strains from China. Pathogens 2020, 9, 821. [Google Scholar] [CrossRef]
- Choe, S.; Le, V.P.; Shin, J.; Kim, J.H.; Kim, K.S.; Song, S.; Cha, R.M.; Park, G.N.; Nguyen, T.L.; Hyun, B.H.; et al. Pathogenicity and Genetic Characterization of Vietnamese Classical Swine Fever Virus: 2014–2018. Pathogens 2020, 9, 169. [Google Scholar] [CrossRef]
- Kameyama, K.I.; Nishi, T.; Yamada, M.; Masujin, K.; Morioka, K.; Kokuho, T.; Fukai, K. Experimental infection of pigs with a classical swine fever virus isolated in Japan for the first time in 26 years. J. Vet. Med. Sci. 2019, 81, 1277–1284. [Google Scholar] [CrossRef]
- Zhang, H.; Leng, C.; Tian, Z.; Liu, C.; Chen, J.; Bai, Y.; Li, Z.; Xiang, L.; Zhai, H.; Wang, Q.; et al. Complete genomic characteristics and pathogenic analysis of the newly emerged classical swine fever virus in China. BMC Vet. Res. 2018, 14, 204. [Google Scholar] [CrossRef]
- The World Organisation for Animal Health (OIE). Official Disease Status-Classical Swine Fever. Available online: https://www.oie.int/en/animal-health-in-the-world/official-disease-status/classical-swine-fever/ (accessed on 22 March 2021).
- The World Organisation for Animal Health (OIE). Information on Aquatic and Terrestrial Animal Diseases-Classical Swine Fever (CSF). Available online: https://www.oie.int/en/animal-health-in-the-world/animal-diseases/Classical-swine-fever/ (accessed on 22 March 2021).
- Pan, C.H.; Jong, M.H.; Huang, Y.L.; Huang, T.S.; Chao, P.H.; Lai, S.S. Rapid detection and differentiation of wild-type and three attenuated lapinized vaccine strains of classical swine fever virus by reverse transcription polymerase chain reaction. J. Vet. Diagn. Investig. 2008, 20, 448–456. [Google Scholar] [CrossRef]
- Pérez, L.J.; Díaz de Arce, H.; Tarradas, J.; Rosell, R.; Perera, C.L.; Muñoz, M.; Frías, M.T.; Nuñez, J.I.; Ganges, L. Development and validation of a novel SYBR Green real-time RT-PCR assay for the detection of classical swine fever virus evaluated on different real-time PCR platforms. J. Virol. Methods 2011, 174, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, B.; Beer, M.; Schelp, C.; Schirrmeier, H.; Depner, K. Validation of a real-time RT-PCR assay for sensitive and specific detection of classical swine fever. J. Virol. Methods 2005, 130, 36–44. [Google Scholar] [CrossRef]
- Chen, L.; Fan, X.Z.; Wang, Q.; Xu, L.; Zhao, Q.Z.; Zhou, Y.C.; Liu, J.; Tang, B.; Zou, X.Q. A novel RT-LAMP assay for rapid and simple detection of classical swine fever virus. Virol. Sin. 2010, 25, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Coronado, L.; Perera, C.L.; Rios, L.; Frías, M.T.; Pérez, L.J. A Critical Review about Different Vaccines against Classical Swine Fever Virus and Their Repercussions in Endemic Regions. Vaccines 2021, 9, 154. [Google Scholar] [CrossRef]
- Holinka, L.G.; O’Donnell, V.; Risatti, G.R.; Azzinaro, P.; Arzt, J.; Stenfeldt, C.; Velazquez-Salinas, L.; Carlson, J.; Gladue, D.P.; Borca, M.V. Early protection events in swine immunized with an experimental live attenuated classical swine fever marker vaccine, FlagT4G. PLoS ONE 2017, 12, e0177433. [Google Scholar] [CrossRef]
- Gong, W.; Li, J.; Wang, Z.; Sun, J.; Mi, S.; Xu, J.; Cao, J.; Hou, Y.; Wang, D.; Huo, X.; et al. Commercial E2 subunit vaccine provides full protection to pigs against lethal challenge with 4 strains of classical swine fever virus genotype 2. Vet. Microbiol. 2019, 237, 108403. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Li, J.; Dou, Z.; Zheng, K.; Li, S.; Kou, C.; He, S. Protective efficacy of the classical swine fever E2 subunit vaccine in experimentally infected pigs. Chin. J. Anim. Infect. Dis. 2018, 26, 18–23. (In Chinese) [Google Scholar]
- Jang, G.; Kim, J.A.; Yoo, H.; Yang, K.; Yang, H.S.; Park, C.; Jeong, K.; Park, C.K.; Lyoo, Y.S.; Lee, C. Genomic characterization of classical swine fever virus LOM variants with 3’-UTR INDELs from pigs on Jeju Island, South Korea. Arch. Virol. 2020, 165, 1691–1696. [Google Scholar] [CrossRef]
- de Oliveira, L.G.; Gatto, I.R.H.; Mechler-Dreibi, M.L.; Almeida, H.M.S.; Sonálio, K.; Storino, G.Y. Achievements and Challenges of Classical Swine Fever Eradication in Brazil. Viruses 2020, 12, 1327. [Google Scholar] [CrossRef]
- Edwards, S.; Fukusho, A.; Lefèvre, P.C.; Lipowski, A.; Pejsak, Z.; Roehe, P.; Westergaard, J. Classical swine fever: The global situation. Vet. Microbiol. 2000, 73, 103–119. [Google Scholar] [CrossRef]
- Moennig, V. Introduction to classical swine fever: Virus, disease and control policy. Vet. Microbiol. 2000, 73, 93–102. [Google Scholar] [CrossRef]
- Li, C.; Wang, Y.; Zheng, H.; Dong, W.; Lv, H.; Lin, J.; Guo, K.; Zhang, Y. Antiviral activity of ISG15 against classical swine fever virus replication in porcine alveolar macrophages via inhibition of autophagy by ISGylating BECN1. Vet. Res. 2020, 51, 22. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Mao, L.; Cao, Y.; Zhou, B.; Yang, L.; Han, L.; Hao, F.; Lin, T.; Zhang, W.; Jiang, J. Porcine Viperin protein inhibits the replication of classical swine fever virus (CSFV) in vitro. Virol. J. 2017, 14, 202. [Google Scholar] [CrossRef]
- Xu, C.; Feng, L.; Chen, P.; Li, A.; Guo, S.; Jiao, X.; Zhang, C.; Zhao, Y.; Jin, X.; Zhong, K.; et al. Viperin inhibits classical swine fever virus replication by interacting with viral nonstructural 5A protein. J. Med. Virol. 2020, 92, 149–160. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Li, Y.; Li, L.F.; Shen, L.; Zhang, L.; Yu, J.; Luo, Y.; Sun, Y.; Li, S.; Qiu, H.J. RNA interference screening of interferon-stimulated genes with antiviral activities against classical swine fever virus using a reporter virus. Antivir. Res. 2016, 128, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Chen, J.; Zhang, X.M.; Gao, Z.C.; Liu, C.C.; Zhang, Y.N.; Hou, J.X.; Li, Z.Y.; Kan, L.; Li, W.L.; et al. Porcine Mx1 Protein Inhibits Classical Swine Fever Virus Replication by Targeting Nonstructural Protein NS5B. J. Virol. 2018, 92, e02147-02117. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Pang, D.; Wang, T.; Yang, X.; Wu, R.; Ren, L.; Yuan, T.; Huang, Y.; Ouyang, H. Human MxA protein inhibits the replication of classical swine fever virus. Virus Res. 2011, 156, 151–155. [Google Scholar] [CrossRef] [PubMed]
- He, D.N.; Zhang, X.M.; Liu, K.; Pang, R.; Zhao, J.; Zhou, B.; Chen, P.Y. In vitro inhibition of the replication of classical swine fever virus by porcine Mx1 protein. Antivir. Res. 2014, 104, 128–135. [Google Scholar] [CrossRef]
- Li, L.F.; Yu, J.; Li, Y.; Wang, J.; Li, S.; Zhang, L.; Xia, S.L.; Yang, Q.; Wang, X.; Yu, S.; et al. Guanylate-Binding Protein 1, an Interferon-Induced GTPase, Exerts an Antiviral Activity against Classical Swine Fever Virus Depending on Its GTPase Activity. J. Virol. 2016, 90, 4412–4426. [Google Scholar] [CrossRef]
- Li, L.F.; Yu, J.; Zhang, Y.; Yang, Q.; Li, Y.; Zhang, L.; Wang, J.; Li, S.; Luo, Y.; Sun, Y.; et al. Interferon-Inducible Oligoadenylate Synthetase-Like Protein Acts as an Antiviral Effector against Classical Swine Fever Virus via the MDA5-Mediated Type I Interferon-Signaling Pathway. J. Virol. 2017, 91, e01514–e01516. [Google Scholar] [CrossRef]
- Li, C.; Zheng, H.; Wang, Y.; Dong, W.; Liu, Y.; Zhang, L.; Zhang, Y. Antiviral Role of IFITM Proteins in Classical Swine Fever Virus Infection. Viruses 2019, 11, 126. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Wang, T.; Yao, L.; Liu, B.; Teng, C.; Ouyang, H. Classical swine fever virus replicated poorly in cells from MxA transgenic pigs. BMC Vet. Res. 2016, 12, 169. [Google Scholar] [CrossRef] [PubMed]
- Yan, Q.; Yang, H.; Yang, D.; Zhao, B.; Ouyang, Z.; Liu, Z.; Fan, N.; Ouyang, H.; Gu, W.; Lai, L. Production of transgenic pigs over-expressing the antiviral gene Mx1. Cell Regen. 2014, 3, 11. [Google Scholar] [CrossRef] [PubMed]
- Xie, Z.; Jiao, H.; Xiao, H.; Jiang, Y.; Liu, Z.; Qi, C.; Zhao, D.; Jiao, S.; Yu, T.; Tang, X.; et al. Generation of pRSAD2 gene knock-in pig via CRISPR/Cas9 technology. Antivir. Res. 2020, 174, 104696. [Google Scholar] [CrossRef]
- Lv, H.; Dong, W.; Cao, Z.; Li, X.; Wang, J.; Qian, G.; Lv, Q.; Wang, C.; Guo, K.; Zhang, Y. TRAF6 is a novel NS3-interacting protein that inhibits classical swine fever virus replication. Sci. Rep. 2017, 7, 6737. [Google Scholar] [CrossRef]
- Li, S.; Wang, J.; He, W.R.; Feng, S.; Li, Y.; Wang, X.; Liao, Y.; Qin, H.Y.; Li, L.F.; Dong, H.; et al. Thioredoxin 2 Is a Novel E2-Interacting Protein That Inhibits the Replication of Classical Swine Fever Virus. J. Virol. 2015, 89, 8510–8524. [Google Scholar] [CrossRef]
- Ling, S.; Luo, M.; Jiang, S.; Liu, J.; Ding, C.; Zhang, Q.; Guo, H.; Gong, W.; Tu, C.; Sun, J. Cellular Hsp27 interacts with classical swine fever virus NS5A protein and negatively regulates viral replication by the NF-κB signaling pathway. Virology 2018, 518, 202–209. [Google Scholar] [CrossRef]
- Li, D.; Dong, H.; Li, S.; Munir, M.; Chen, J.; Luo, Y.; Sun, Y.; Liu, L.; Qiu, H.J. Hemoglobin subunit beta interacts with the capsid protein and antagonizes the growth of classical swine fever virus. J. Virol. 2013, 87, 5707–5717. [Google Scholar] [CrossRef]
- Dong, W.; Lv, H.; Li, C.; Liu, Y.; Wang, C.; Lin, J.; Wang, Y.; Qian, G.; Guo, K.; Zhang, Y. MAVS induces a host cell defense to inhibit CSFV infection. Arch. Virol. 2018, 163, 1805–1821. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, H.; Zheng, G.L.; Yang, Q.; Yu, S.; Wang, J.; Li, S.; Li, L.F.; Qiu, H.J. Porcine RING Finger Protein 114 Inhibits Classical Swine Fever Virus Replication via K27-Linked Polyubiquitination of Viral NS4B. J. Virol. 2019, 93, e01248-01219. [Google Scholar] [CrossRef]
- Deng, S.; Yang, C.; Nie, K.; Fan, S.; Zhu, M.; Zhu, J.; Chen, Y.; Yuan, J.; Zhang, J.; Xu, H.; et al. Host cell protein PSMB10 interacts with viral NS3 protein and inhibits the growth of classical swine fever virus. Virology 2019, 537, 74–83. [Google Scholar] [CrossRef] [PubMed]
- Lv, H.; Dong, W.; Qian, G.; Wang, J.; Li, X.; Cao, Z.; Lv, Q.; Wang, C.; Guo, K.; Zhang, Y. uS10, a novel Npro-interacting protein, inhibits classical swine fever virus replication. J. Gen. Virol. 2017, 98, 1679–1692. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Zhang, Z.; Zhang, L.; Li, H.; Fan, S.; Zhu, E.; Fan, J.; Li, Z.; Chen, W.; Yi, L.; et al. Antiviral Role of Serine Incorporator 5 (SERINC5) Proteins in Classical Swine Fever Virus Infection. Front. Microbiol. 2020, 11, 580233. [Google Scholar] [CrossRef] [PubMed]
- Fan, S.; Wu, K.; Zhao, M.; Yuan, J.; Ma, S.; Zhu, E.; Chen, Y.; Ding, H.; Yi, L.; Chen, J. LDHB inhibition induces mitophagy and facilitates the progression of CSFV infection. Autophagy 2020, 1–20, Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Feng, S.; Wang, J.H.; He, W.R.; Qin, H.Y.; Dong, H.; Li, L.F.; Yu, S.X.; Li, Y.; Qiu, H.J. eEF1A Interacts with the NS5A Protein and Inhibits the Growth of Classical Swine Fever Virus. Viruses 2015, 7, 4563–4581. [Google Scholar] [CrossRef]
- Lin, J.; Wang, C.; Liang, W.; Zhang, J.; Zhang, L.; Lv, H.; Dong, W.; Zhang, Y. Rab1A is required for assembly of classical swine fever virus particle. Virology 2018, 514, 18–29. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Wang, T.; Song, M.; Jin, M.; Liu, S.; Guo, K.; Zhang, Y. Rab1b-GBF1-ARFs mediated intracellular trafficking is required for classical swine fever virus replication in swine umbilical vein endothelial cells. Vet. Microbiol. 2020, 246, 108743. [Google Scholar] [CrossRef]
- Liang, W.; Zheng, M.; Bao, C.; Zhang, Y. CSFV proliferation is associated with GBF1 and Rab2. J. Biosci. 2017, 42, 43–56. [Google Scholar] [CrossRef]
- Lin, J.; Wang, C.; Zhang, L.; Wang, T.; Zhang, J.; Liang, W.; Li, C.; Qian, G.; Ouyang, Y.; Guo, K.; et al. Rab5 Enhances Classical Swine Fever Virus Proliferation and Interacts with Viral NS4B Protein to Facilitate Formation of NS4B Related Complex. Front. Microbiol. 2017, 8, 1468. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.N.; Liu, Y.Y.; Xiao, F.C.; Liu, C.C.; Liang, X.D.; Chen, J.; Zhou, J.; Baloch, A.S.; Kan, L.; Zhou, B.; et al. Rab5, Rab7, and Rab11 Are Required for Caveola-Dependent Endocytosis of Classical Swine Fever Virus in Porcine Alveolar Macrophages. J. Virol. 2018, 92, e00797-00718. [Google Scholar] [CrossRef]
- Zhang, L.; Zhao, D.; Jin, M.; Song, M.; Liu, S.; Guo, K.; Zhang, Y. Rab18 binds to classical swine fever virus NS5A and mediates viral replication and assembly in swine umbilical vein endothelial cells. Virulence 2020, 11, 489–501. [Google Scholar] [CrossRef] [PubMed]
- Xu, P.; Jia, S.; Wang, K.; Fan, Z.; Zheng, H.; Lv, J.; Jiang, Y.; Hou, Y.; Lou, B.; Zhou, H.; et al. MiR-140 inhibits classical swine fever virus replication by targeting Rab25 in swine umbilical vein endothelial cells. Virulence 2020, 11, 260–269. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.J.; Yang, Y.T.; Zhao, M.Q.; Dong, X.Y.; Gou, H.C.; Pei, J.J.; Chen, J.D. PKR activation enhances replication of classical swine fever virus in PK-15 cells. Virus Res. 2015, 204, 47–57. [Google Scholar] [CrossRef]
- Li, D.; Li, S.; Sun, Y.; Dong, H.; Li, Y.; Zhao, B.; Guo, D.; Weng, C.; Qiu, H.J. Poly(C)-binding protein 1, a novel N(pro)-interacting protein involved in classical swine fever virus growth. J. Virol. 2013, 87, 2072–2080. [Google Scholar] [CrossRef]
- Zheng, G.; Li, L.F.; Zhang, Y.; Qu, L.; Wang, W.; Li, M.; Yu, S.; Zhou, M.; Luo, Y.; Sun, Y.; et al. MERTK is a host factor that promotes classical swine fever virus entry and antagonizes innate immune response in PK-15 cells. Emerg. Microbes Infect. 2020, 9, 571–581. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.C.; Liu, Y.Y.; Cheng, Y.; Zhang, Y.N.; Zhang, J.; Liang, X.D.; Gao, Y.; Chen, H.; Baloch, A.S.; Yang, Q.; et al. The ESCRT-I Subunit Tsg101 Plays Novel Dual Roles in Entry and Replication of Classical Swine Fever Virus. J. Virol. 2020, 95, e01928-20. [Google Scholar] [CrossRef]
- Chen, J.; He, W.R.; Shen, L.; Dong, H.; Yu, J.; Wang, X.; Yu, S.; Li, Y.; Li, S.; Luo, Y.; et al. The laminin receptor is a cellular attachment receptor for classical Swine Fever virus. J. Virol. 2015, 89, 4894–4906. [Google Scholar] [CrossRef]
- Yang, Z.; Shi, Z.; Guo, H.; Qu, H.; Zhang, Y.; Tu, C. Annexin 2 is a host protein binding to classical swine fever virus E2 glycoprotein and promoting viral growth in PK-15 cells. Virus Res. 2015, 201, 16–23. [Google Scholar] [CrossRef]
- Li, W.; Wang, G.; Liang, W.; Kang, K.; Guo, K.; Zhang, Y. Integrin β3 is required in infection and proliferation of classical swine fever virus. PLoS ONE 2014, 9, e110911. [Google Scholar] [CrossRef]
- Vuono, E.A.; Ramirez-Medina, E.; Berggren, K.; Rai, A.; Pruitt, S.; Silva, E.; Velazquez-Salinas, L.; Gladue, D.P.; Borca, M.V. Swine Host Protein Coiled-Coil Domain-Containing 115 (CCDC115) Interacts with Classical Swine Fever Virus Structural Glycoprotein E2 during Virus Replication. Viruses 2020, 12, 388. [Google Scholar] [CrossRef]
- Vuono, E.A.; Ramirez-Medina, E.; Azzinaro, P.; Berggren, K.A.; Rai, A.; Pruitt, S.; Silva, E.; Velazquez-Salinas, L.; Borca, M.V.; Gladue, D.P. SERTA Domain Containing Protein 1 (SERTAD1) Interacts with Classical Swine Fever Virus Structural Glycoprotein E2, Which Is Involved in Virus Virulence in Swine. Viruses 2020, 12, 421. [Google Scholar] [CrossRef] [PubMed]
- Borca, M.V.; Vuono, E.A.; Ramirez-Medina, E.; Azzinaro, P.; Berggren, K.A.; Singer, M.; Rai, A.; Pruitt, S.; Silva, E.B.; Velazquez-Salinas, L.; et al. Structural Glycoprotein E2 of Classical Swine Fever Virus Interacts with Host Protein Dynactin Subunit 6 (DCTN6) during the Virus Infectious Cycle. J. Virol. 2019, 94, e01642-01619. [Google Scholar] [CrossRef] [PubMed]
- Gladue, D.P.; Holinka, L.G.; Fernandez-Sainz, I.J.; Prarat, M.V.; O’Donnell, V.; Vepkhvadze, N.G.; Lu, Z.; Risatti, G.R.; Borca, M.V. Interaction between Core protein of classical swine fever virus with cellular IQGAP1 protein appears essential for virulence in swine. Virology 2011, 412, 68–74. [Google Scholar] [CrossRef]
- Sheng, C.; Yao, Y.; Chen, B.; Wang, Y.; Chen, J.; Xiao, M. RNA helicase is involved in the expression and replication of classical swine fever virus and interacts with untranslated region. Virus Res. 2013, 171, 257–261. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Wang, X.; Wang, Q.; Luo, M.; Guo, H.; Gong, W.; Tu, C.; Sun, J. The eukaryotic translation initiation factor 3 subunit E binds to classical swine fever virus NS5A and facilitates viral replication. Virology 2018, 515, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Gladue, D.P.; O’Donnell, V.; Fernandez-Sainz, I.J.; Fletcher, P.; Baker-Branstetter, R.; Holinka, L.G.; Sanford, B.; Carlson, J.; Lu, Z.; Borca, M.V. Interaction of structural core protein of classical swine fever virus with endoplasmic reticulum-associated degradation pathway protein OS9. Virology 2014, 460–461, 173–179. [Google Scholar] [CrossRef]
- Chengcheng, Z.; Fuxi, Z.; Mengjiao, G.; Baoyang, R.; Xuefeng, W.; Yantao, W.; Xiaorong, Z. CSFV protein NS5A activates the unfolded protein response to promote viral replication. Virology 2020, 541, 75–84. [Google Scholar] [CrossRef]
- Lv, H.; Dong, W.; Guo, K.; Jin, M.; Li, X.; Li, C.; Zhang, Y. Tumor Necrosis Factor Receptor-Associated Factor 5 Interacts with the NS3 Protein and Promotes Classical Swine Fever Virus Replication. Viruses 2018, 10, 305. [Google Scholar] [CrossRef]
- Wang, J.; Chen, S.; Liao, Y.; Zhang, E.; Feng, S.; Yu, S.; Li, L.F.; He, W.R.; Li, Y.; Luo, Y.; et al. Correction for Wang et al., “Mitogen-Activated Protein Kinase Kinase 2, a Novel E2-Interacting Protein, Promotes the Growth of Classical Swine Fever Virus via Attenuation of the JAK-STAT Signaling Pathway”. J. Virol. 2017, 91, e01523-01517. [Google Scholar] [CrossRef]
- Wang, J.; Chen, S.; Liao, Y.; Zhang, E.; Feng, S.; Yu, S.; Li, L.F.; He, W.R.; Li, Y.; Luo, Y.; et al. Mitogen-Activated Protein Kinase Kinase 2, a Novel E2-Interacting Protein, Promotes the Growth of Classical Swine Fever Virus via Attenuation of the JAK-STAT Signaling Pathway. J. Virol. 2016, 90, 10271–10283. [Google Scholar] [CrossRef]
- Pei, J.; Zhao, M.; Ye, Z.; Gou, H.; Wang, J.; Yi, L.; Dong, X.; Liu, W.; Luo, Y.; Liao, M.; et al. Autophagy enhances the replication of classical swine fever virus in vitro. Autophagy 2014, 10, 93–110. [Google Scholar] [CrossRef]
- Fan, S.; Wu, K.; Luo, C.; Li, X.; Zhao, M.; Song, D.; Ma, S.; Zhu, E.; Chen, Y.; Ding, H.; et al. Dual NDP52 Function in Persistent CSFV Infection. Front. Microbiol. 2019, 10, 2962. [Google Scholar] [CrossRef] [PubMed]
- Qian, G.; Lv, H.; Lin, J.; Li, X.; Lv, Q.; Wang, T.; Zhang, J.; Dong, W.; Guo, K.; Zhang, Y. FHC, an NS4B-interacting Protein, Enhances Classical Swine Fever Virus Propagation and Acts Positively in Viral Anti-apoptosis. Sci. Rep. 2018, 8, 8318. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Zhang, C.; Cui, H.; Guo, K.; Wang, F.; Zhao, T.; Liang, W.; Lv, Q.; Zhang, Y. FKBP8 interact with classical swine fever virus NS5A protein and promote virus RNA replication. Virus Genes 2016, 52, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Guo, K.; Li, H.; Tan, X.; Wu, M.; Lv, Q.; Liu, W.; Zhang, Y. Molecular chaperone Jiv promotes the RNA replication of classical swine fever virus. Virus Genes 2017, 53, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Kang, K.; Ning, P.; Peng, Y.; Lin, Z.; Cui, H.; Cao, Z.; Wang, J.; Zhang, Y. Heat shock protein 70 is associated with CSFV NS5A protein and enhances viral RNA replication. Virology 2015, 482, 9–18. [Google Scholar] [CrossRef]
- Shi, Z.; Sun, J.; Guo, H.; Yang, Z.; Ma, Z.; Tu, C. Down-regulation of cellular protein heme oxygenase 1 inhibits proliferation of classical swine fever virus in PK-15 cells. Virus Res. 2013, 173, 315–320. [Google Scholar] [CrossRef]
- Gong, X.; Li, X.; You, X.; Hu, A.; Liu, M.; Yao, H.; He, J.; Zhang, X.; Ning, P. AIF1 was identified as an up-regulated gene contributing to CSFV Shimen infection in porcine alveolar macrophage 3D4/21 cells. PeerJ 2020, 8, e8543. [Google Scholar] [CrossRef]
- Gladue, D.P.; Baker-Bransetter, R.; Holinka, L.G.; Fernandez-Sainz, I.J.; O’Donnell, V.; Fletcher, P.; Lu, Z.; Borca, M.V. Interaction of CSFV E2 protein with swine host factors as detected by yeast two-hybrid system. PLoS ONE 2014, 9, e85324. [Google Scholar] [CrossRef]
- Kang, K.; Guo, K.; Tang, Q.; Zhang, Y.; Wu, J.; Li, W.; Lin, Z. Interactive cellular proteins related to classical swine fever virus non-structure protein 2 by yeast two-hybrid analysis. Mol. Biol. Rep. 2012, 39, 10515–10524. [Google Scholar] [CrossRef]
- Zhang, C.; He, L.; Kang, K.; Chen, H.; Xu, L.; Zhang, Y. Screening of cellular proteins that interact with the classical swine fever virus non-structural protein 5A by yeast two-hybrid analysis. J. Biosci. 2014, 39, 63–74. [Google Scholar] [CrossRef] [PubMed]
- Shi, B.J.; Liu, C.C.; Zhou, J.; Wang, S.Q.; Gao, Z.C.; Zhang, X.M.; Zhou, B.; Chen, P.Y. Entry of Classical Swine Fever Virus into PK-15 Cells via a pH-, Dynamin-, and Cholesterol-Dependent, Clathrin-Mediated Endocytic Pathway That Requires Rab5 and Rab7. J. Virol. 2016, 90, 9194–9208. [Google Scholar] [CrossRef]
- Li, S.; Wang, J.; Yang, Q.; Naveed Anwar, M.; Yu, S.; Qiu, H.J. Complex Virus-Host Interactions Involved in the Regulation of Classical Swine Fever Virus Replication: A Minireview. Viruses 2017, 9, 171. [Google Scholar] [CrossRef]
- Vrancken, R.; Paeshuyse, J.; Haegeman, A.; Puerstinger, G.; Froeyen, M.; Herdewijn, P.; Kerkhofs, P.; Neyts, J.; Koenen, F. Imidazo[4,5-c]pyridines inhibit the in vitro replication of the classical swine fever virus and target the viral polymerase. Antivir. Res. 2008, 77, 114–119. [Google Scholar] [CrossRef]
- Vrancken, R.; Haegeman, A.; Paeshuyse, J.; Puerstinger, G.; Rozenski, J.; Wright, M.; Tignon, M.; Le Potier, M.F.; Neyts, J.; Koenen, F. Proof of concept for the reduction of classical swine fever infection in pigs by a novel viral polymerase inhibitor. J. Gen. Virol. 2009, 90, 1335–1342. [Google Scholar] [CrossRef] [PubMed]
- Vrancken, R.; Haegeman, A.; Dewulf, J.; Paeshuyse, J.; Puerstinger, G.; Tignon, M.; Le Potier, M.F.; Neyts, J.; Koenen, F. The reduction of CSFV transmission to untreated pigs by the pestivirus inhibitor BPIP: A proof of concept. Vet. Microbiol. 2009, 139, 365–368. [Google Scholar] [CrossRef] [PubMed]
- Baginski, S.G.; Pevear, D.C.; Seipel, M.; Sun, S.C.; Benetatos, C.A.; Chunduru, S.K.; Rice, C.M.; Collett, M.S. Mechanism of action of a pestivirus antiviral compound. Proc. Natl. Acad. Sci. USA 2000, 97, 7981–7986. [Google Scholar] [CrossRef] [PubMed]
- Musiu, S.; Pürstinger, G.; Stallinger, S.; Vrancken, R.; Haegeman, A.; Koenen, F.; Leyssen, P.; Froeyen, M.; Neyts, J.; Paeshuyse, J. Substituted 2,6-bis(benzimidazol-2-yl)pyridines: A novel chemical class of pestivirus inhibitors that targets a hot spot for inhibition of pestivirus replication in the RNA-dependent RNA polymerase. Antivir. Res. 2014, 106, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Jun, H.R.; Pham, C.D.; Lim, S.I.; Lee, S.C.; Kim, Y.S.; Park, S.; Kwon, M.H. An RNA-hydrolyzing recombinant antibody exhibits an antiviral activity against classical swine fever virus. Biochem. Biophys. Res. Commun. 2010, 395, 484–489. [Google Scholar] [CrossRef]
- Zhou, B.; Liu, K.; Wei, J.C.; Mao, X.; Chen, P.Y. Inhibition of replication of classical swine fever virus in a stable cell line by the viral capsid and Staphylococcus aureus nuclease fusion protein. J. Virol. Methods 2010, 167, 79–83. [Google Scholar] [CrossRef]
- Krol, E.; Pastuch-Gawolek, G.; Nidzworski, D.; Rychlowski, M.; Szeja, W.; Grynkiewicz, G.; Szewczyk, B. Synthesis and antiviral activity of a novel glycosyl sulfoxide against classical swine fever virus. Bioorg. Med. Chem. 2014, 22, 2662–2670. [Google Scholar] [CrossRef] [PubMed]
- Krol, E.; Wandzik, I.; Szeja, W.; Grynkiewicz, G.; Szewczyk, B. In vitro antiviral activity of some uridine derivatives of 2-deoxy sugars against classical swine fever virus. Antivir. Res. 2010, 86, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Tyborowska, J.; Zdunek, E.; Szewczyk, B. Effect of N-glycosylation inhibition on the synthesis and processing of classical swine fever virus glycoproteins. Acta Biochim. Pol. 2007, 54, 813–819. [Google Scholar] [CrossRef] [PubMed]
- Pastuch-Gawolek, G.; Chaubey, B.; Szewczyk, B.; Krol, E. Novel thioglycosyl analogs of glycosyltransferase substrates as antiviral compounds against classical swine fever virus and hepatitis C virus. Eur. J. Med. Chem. 2017, 137, 247–262. [Google Scholar] [CrossRef] [PubMed]
- Krol, E.; Pastuch-Gawolek, G.; Chaubey, B.; Brzuska, G.; Erfurt, K.; Szewczyk, B. Novel Uridine Glycoconjugates, Derivatives of 4-Aminophenyl 1-Thioglycosides, as Potential Antiviral Compounds. Molecules 2018, 23, 1435. [Google Scholar] [CrossRef] [PubMed]
- Chun, X.; Wu, D.; Wu, W.; Wan, J.; Wang, L.; Yang, T.; Wang, Q.; Ning, Y. Cloning and expression of interferon-alpha/gamma from a domestic porcine breed and its effect on classical swine fever virus. Vet. Immunol. Immunopathol. 2005, 104, 81–89. [Google Scholar] [CrossRef]
- Fernandez-Sainz, I.; Ramanathan, P.; O’Donnell, V.; Diaz-San Segundo, F.; Velazquez-Salinas, L.; Sturza, D.F.; Zhu, J.; de los Santos, T.; Borca, M.V. Treatment with interferon-alpha delays disease in swine infected with a highly virulent CSFV strain. Virology 2015, 483, 284–290. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zhang, X.; Jing, J.; Li, W.; Liu, K.; Shi, B.; Xu, Q.; Ma, Z.; Zhou, B.; Chen, P. Porcine Mx1 fused to HIV Tat protein transduction domain (PTD) inhibits classical swine fever virus infection in vitro and in vivo. BMC Vet. Res. 2015, 11, 264. [Google Scholar] [CrossRef]
- Yu, S.; Yin, C.; Song, K.; Li, S.; Zheng, G.L.; Li, L.F.; Wang, J.; Li, Y.; Luo, Y.; Sun, Y.; et al. Engagement of cellular cholesterol in the life cycle of classical swine fever virus: Its potential as an antiviral target. J. Gen. Virol. 2019, 100, 156–165. [Google Scholar] [CrossRef]
- Liang, X.D.; Zhang, Y.N.; Liu, C.C.; Chen, J.; Chen, X.N.; Sattar Baloch, A.; Zhou, B. U18666A inhibits classical swine fever virus replication through interference with intracellular cholesterol trafficking. Vet. Microbiol. 2019, 238, 108436. [Google Scholar] [CrossRef]
- Pei, J.; Deng, J.; Ye, Z.; Wang, J.; Gou, H.; Liu, W.; Zhao, M.; Liao, M.; Yi, L.; Chen, J. Absence of autophagy promotes apoptosis by modulating the ROS-dependent RLR signaling pathway in classical swine fever virus-infected cells. Autophagy 2016, 12, 1738–1758. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.; Mao, Q.; Chen, W.; Zhao, M.; Wu, K.; Song, D.; Li, X.; Zhu, E.; Fan, S.; Yi, L.; et al. Serum Lipidomics Analysis of Classical Swine Fever Virus Infection in Piglets and Emerging Role of Free Fatty Acids in Virus Replication In Vitro. Front. Cell. Infect. Microbiol. 2019, 9, 410. [Google Scholar] [CrossRef] [PubMed]
- Zhu, E.; Chen, W.; Qin, Y.; Ma, S.; Fan, S.; Wu, K.; Li, W.; Fan, J.; Yi, L.; Ding, H.; et al. Classical Swine Fever Virus Infection Induces Endoplasmic Reticulum Stress-Mediated Autophagy to Sustain Viral Replication in vivo and in vitro. Front. Microbiol. 2019, 10, 2545. [Google Scholar] [CrossRef]
- He, W.; Xu, H.; Gou, H.; Yuan, J.; Liao, J.; Chen, Y.; Fan, S.; Xie, B.; Deng, S.; Zhang, Y.; et al. CSFV Infection Up-Regulates the Unfolded Protein Response to Promote Its Replication. Front. Microbiol. 2017, 8, 2129. [Google Scholar] [CrossRef] [PubMed]
- Knoetig, S.M.; McCullough, K.C.; Summerfield, A. Lipopolysaccharide-induced impairment of classical swine fever virus infection in monocytic cells is sensitive to 2-aminopurine. Antivir. Res. 2002, 53, 75–81. [Google Scholar] [CrossRef]
- Cao, Z.; Zheng, M.; Lv, H.; Guo, K.; Zhang, Y. Tissue expression of Toll-like receptors 2, 3, 4 and 7 in swine in response to the Shimen strain of classical swine fever virus. Mol. Med. Rep. 2018, 17, 7122–7130. [Google Scholar] [CrossRef]
- Chen, Y.; Fan, S.; Zhao, M.; Wu, K.; Zhu, E.; Ma, S.; He, W.; Deng, S.; Xu, H.; Zhang, J.; et al. MG132 Attenuates the Replication of Classical Swine Fever Virus in vitro. Front. Microbiol. 2020, 11, 852. [Google Scholar] [CrossRef]
- Freitas, T.R.; Caldas, L.A.; Rebello, M.A. Prostaglandin A1 inhibits replication of classical swine fever virus. Mem. Inst. Oswaldo Cruz 1998, 93, 815–818. [Google Scholar] [CrossRef][Green Version]
- Freitas, T.R.; Caldas, L.A.; Rebello, M.A. Effect of prostaglandin A1 in porcine cells persistently infected with classical swine fever virus. J. Basic Microbiol. 2003, 43, 468–472. [Google Scholar] [CrossRef] [PubMed]
- Yin, L.; Luo, Y.; Liang, B.; Wang, F.; Du, M.; Petrenko, V.A.; Qiu, H.J.; Liu, A. Specific ligands for classical swine fever virus screened from landscape phage display library. Antivir. Res. 2014, 109, 68–71. [Google Scholar] [CrossRef] [PubMed]
- Vuono, E.A.; Ramirez-Medina, E.; Holinka, L.G.; Baker-Branstetter, R.; Borca, M.V.; Gladue, D.P. Interaction of Structural Glycoprotein E2 of Classical Swine Fever Virus with Protein Phosphatase 1 Catalytic Subunit Beta (PPP1CB). Viruses 2019, 11, 307. [Google Scholar] [CrossRef]
- Fire, A.; Xu, S.; Montgomery, M.K.; Kostas, S.A.; Driver, S.E.; Mello, C.C. Potent and specific genetic interference by double-stranded RNA in Caenorhabditis elegans. Nature 1998, 391, 806–811. [Google Scholar] [CrossRef]
- Xu, X.; Guo, H.; Xiao, C.; Zha, Y.; Shi, Z.; Xia, X.; Tu, C. In vitro inhibition of classical swine fever virus replication by siRNAs targeting Npro and NS5B genes. Antivir. Res. 2008, 78, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Porntrakulpipat, S.; Supankong, S.; Chatchawanchonteera, A.; Pakdee, P. RNA interference targeting nucleocapsid protein (C) inhibits classical swine fever virus replication in SK-6 cells. Vet. Microbiol. 2010, 142, 41–44. [Google Scholar] [CrossRef]
- Li, J.; Dai, Y.; Liu, S.; Guo, H.; Wang, T.; Ouyang, H.; Tu, C. In vitro inhibition of CSFV replication by multiple siRNA expression. Antivir. Res. 2011, 91, 209–216. [Google Scholar] [CrossRef]
- Wu, C.W.; Chien, M.S.; Huang, C. Characterization of the swine U6 promoter for short hairpin RNA expression and its application to inhibition of virus replication. J. Biotechnol. 2013, 168, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Guo, H.; Shi, Z.; Tu, C. In vitro inhibition of CSFV replication by retroviral vector-mediated RNA interference. J. Virol. Methods 2010, 169, 316–321. [Google Scholar] [CrossRef] [PubMed]
- Shen, L.; Li, Y.; Chen, J.; Li, C.; Huang, J.; Luo, Y.; Sun, Y.; Li, S.; Qiu, H.J. Generation of a recombinant classical swine fever virus stably expressing the firefly luciferase gene for quantitative antiviral assay. Antivir. Res. 2014, 109, 15–21. [Google Scholar] [CrossRef]
- Xie, Z.; Pang, D.; Yuan, H.; Jiao, H.; Lu, C.; Wang, K.; Yang, Q.; Li, M.; Chen, X.; Yu, T.; et al. Genetically modified pigs are protected from classical swine fever virus. PLoS Pathog. 2018, 14, e1007193. [Google Scholar] [CrossRef]
- Lu, C.; Pang, D.; Li, M.; Yuan, H.; Yu, T.; Huang, P.; Li, J.; Chen, X.; Jiao, H.; Xie, Z.; et al. CRISPR/Cas9-Mediated Hitchhike Expression of Functional shRNAs at the Porcine miR-17-92 Cluster. Cells 2019, 8, 113. [Google Scholar] [CrossRef] [PubMed]
- Simmonds, P.; Becher, P.; Bukh, J.; Gould, E.A.; Meyers, G.; Monath, T.; Muerhoff, S.; Pletnev, A.; Rico-Hesse, R.; Smith, D.B.; et al. ICTV Virus Taxonomy Profile: Flaviviridae. J. Gen. Virol. 2017, 98, 2–3. [Google Scholar] [CrossRef] [PubMed]
- Dai, Z.; Wu, R.; Zhao, Y.C.; Wang, K.K.; Huang, Y.Y.; Yang, X.; Xie, Z.C.; Tu, C.C.; Ouyang, H.S.; Wang, T.D.; et al. Early lethality of shRNA-transgenic pigs due to saturation of microRNA pathways. J. Zhejiang Univ. Sci. B 2014, 15, 466–473. [Google Scholar] [CrossRef]
- Wen, W.; He, Z.; Jing, Q.; Hu, Y.; Lin, C.; Zhou, R.; Wang, X.; Su, Y.; Yuan, J.; Chen, Z.; et al. Cellular microRNA-miR-548g-3p modulates the replication of dengue virus. J. Infect. 2015, 70, 631–640. [Google Scholar] [CrossRef] [PubMed]
- Ottosen, S.; Parsley, T.B.; Yang, L.; Zeh, K.; van Doorn, L.J.; van der Veer, E.; Raney, A.K.; Hodges, M.R.; Patick, A.K. In vitro antiviral activity and preclinical and clinical resistance profile of miravirsen, a novel anti-hepatitis C virus therapeutic targeting the human factor miR-122. Antimicrob. Agents Chemother. 2015, 59, 599–608. [Google Scholar] [CrossRef] [PubMed]
- Touret, F.; Gilles, M.; Barral, K.; Nougairède, A.; van Helden, J.; Decroly, E.; de Lamballerie, X.; Coutard, B. In vitro screening of a FDA approved chemical library reveals potential inhibitors of SARS-CoV-2 replication. Sci. Rep. 2020, 10, 13093. [Google Scholar] [CrossRef]

| No. | Host Protein | Possible Mechanisms Associated with Anti-CSFV Effects of the Host Protein | Ref. |
|---|---|---|---|
| 1. | ISG15 | Inhibit CSFV replication via inhibition of autophagy by ISGylating BECN1. | [34] |
| 2. | Viperin * | Interact with CSFV E2 and NS5A; its anti-CSFV function occurs during the viral genome and/or protein synthesis step. | [35,36] |
| 3. | NRAMP1, NT5C3A, CXCL10, OAS1 | Interferon-stimulated genes (ISGs); inhibit CSFV replication. | [37] |
| 4. | Mx * (porcine Mx1, porcine Mx2, human MxA, and mouse Mx1) | IFN-induced GTPases; inhibit CSFV replication; porcine Mx1 interacts with CSFV NS5B and undermines the RNA-dependent RNA polymerase (RdRp) activities of NS5B. | [38,39,40] |
| 5. | GBP1 | IFN-induced GTPase; interact with CSFV NS5A; act mainly on the early phase of CSFV replication. | [41] |
| 6. | pOASL | Inhibit CSFV replication via the MDA5-mediated type I IFN signaling pathway. | [42] |
| 7. | IFITM family (IFITM1, IFITM2, and IFITM3) | IFN-inducible transmembrane proteins; IFITM1, IFITM2, and IFITM3 colocalization with Lamp1, IFITM2 with Rab5 and Rab7, and IFITM3 with Rab7 appear in CSFV-infected cells. | [43] |
| 8. | TRAF6 | Interact with NS3 and inhibit CSFV replication via activation of NF-κB signaling pathway along with the increase in expression of IFN-β and IL-6. | [47] |
| 9. | Trx2 | Interact with CSFV E2 and inhibit CSFV replication via NF-κB signaling pathway. | [48] |
| 10. | Hsp27 | Interact with CSFV NS5A and inhibit CSFV replication by NF-κB signaling pathway. | [49] |
| 11. | HB | Interact with CSFV capsid (C) protein; antagonize CSFV replication by regulating RIG-I pathway and IFN pathway. | [50] |
| 12. | MAVS | The adaptor of the RIG-I-like receptor; induce antiviral cytokines and apoptosis to inhibit CSFV replication. | [51] |
| 13. | pRNF114 | RING domain E3 ubiquitin ligase; interact with the CSFV NS4B and mediate the K27-linked polyubiquitination and degradation of NS4B through a proteasome-dependent pathway. | [52] |
| 14. | PSMB10 | Interact with CSFV NS3 and mediate the degradation of NS3 through the ubiquitin-proteasome system; restore the function of MHC class I antigen presentation and inhibit CSFV proliferation. | [53] |
| 15. | uS10 | Interact with CSFV Npro and inhibit CSFV replication by modulating TLR3 expression. | [54] |
| 16. | SERINC5 | Inhibit CSFV replication via activation of MDA5-mediated type I IFN signaling pathway. | [55] |
| 17. | LDHB | Interact with CSFV NS3 and decrease CSFV replication possibly related to the regulation of mitophagy. | [56] |
| 18. | eEF1A | Interact with the CSFV NS5A; bind to the CSFV IRES; reduce the translation efficiency of CSFV IRES. | [57] |
| No. | Host Protein | Possible Mechanism by Which Host Proteins Influence CSFV Replication | Ref. |
|---|---|---|---|
| 1. | Rab1A | Be required for viral particle assembly; bind to viral particle assembly-related NS5A protein. | [58] |
| 2. | Rab1b | Rab1b-GBF1-ARFs mediated intracellular trafficking is required for CSFV replication. | [59] |
| 3. | Rab2 | Be involved in Golgi function and promote CSFV proliferation. | [60] |
| 4. | Rab5 | Enhance CSFV proliferation and interact with CSFV NS4B to facilitate the formation of NS4B-related complex. | [61] |
| 5. | Rab5, Rab7, and Rab11 | Rab5 and Rab7 are required for clathrin-mediated endocytic pathway of CSFV in porcine kidney cells; Rab5, Rab7, and Rab11 are needed for caveola-dependent endocytosis of CSFV in porcine alveolar macrophages. | [62,94] |
| 6. | Rab18 | Interact with CSFV NS5A and mediate viral RNA replication and virion assembly. | [63] |
| 7. | Rab25 | Promote CSFV replication. | [64] |
| 8. | PKR | PKR activation enhances CSFV replication; inhibition of PKR results in the reduction of CSFV replication and an increase in IFN induction. | [65] |
| 9. | PCBP1 | Interact with CSFV Npro and promote CSFV growth by downregulating type I IFN. | [66] |
| 10. | MERTK | Interact with CSFV E2 and facilitate virus entry; after virus entry, down-regulate IFN-β and promote CSFV infection. | [67] |
| 11. | Tsg101 | Participate in clathrin-mediated endocytosis of CSFV and regulate the viral replication process by interacting with CSFV NS4B and NS5B. | [68] |
| 12. | LamR | A cellular attachment receptor for CSFV; interact with the CSFV Erns. | [69] |
| 13. | Anx2 | Cellular membrane protein likely associated with CSFV entry into cells; interact with CSFV E2 and promote CSFV multiplication. | [70] |
| 14. | integrin β3 | Membrane-bound signal mediator; be required in CSFV infection and proliferation. | [71] |
| 15. | CCDC115 * | Interaction of CCDC115 with CSFV E2 plays an important role in virus replication and virulence. | [72] |
| 16. | SERTAD1 * | Interaction of SERTAD1 with CSFV E2 plays a critical role in virus replication and virulence. | [73] |
| 17. | DCTN6 * | Interaction of DCTN6 with CSFV E2 plays a role in virus replication and virulence. | [74] |
| 18. | IQGAP1 * | Interaction between IQGAP1 and CSFV C protein is essential for virus replication and virulence. | [75] |
| 19. | RHA | RNA helicase; bind the 5′-UTR and 3′-UTR of CSFV; be involved in the expression and replication of CSFV. | [76] |
| 20. | eIF3E | The component of eukaryotic translation initiation factor; interact with CSFV NS5A; enhance the translational activity of CSFV IRES. | [77] |
| 21. | GBF1 | Be involved in Golgi function and promote CSFV proliferation. | [60] |
| 22. | OS9 | Be involved in the endoplasmic reticulum-associated degradation pathway; interaction of OS9 with CSFV C protein is involved in CSFV replication. | [78] |
| 23. | GRP78 | The monitor of unfolded protein response (UPR) signaling pathways; interact with CSFV NS5A and enhance viral replication. | [79] |
| 24. | TRAF5 | Interact with CSFV NS3 and promote CSFV replication via p38 MAPK activation. | [80] |
| 25. | MEK2 | Interact with CSFV E2 and promote CSFV growth via attenuation of the JAK-STAT signaling pathway. | [81,82] |
| 26. | BECN1, LC3 | Be involved in cellular autophagy; affect progeny virus production. | [83] |
| 27. | NDP52 | An autophagy receptor; mediate CSFV infection. | [84] |
| 28. | FHC | Interact with CSFV NS4B, enhance CSFV replication and play a positive role in viral anti-apoptosis by regulating ROS accumulation. | [85] |
| 29. | FKBP8 | Interact with CSFV NS5A and promote viral RNA replication. | [86] |
| 30. | Jiv90 | Molecular chaperone; promote viral RNA replication. | [87] |
| 31. | HSP70 | Interact with CSFV NS5A and promote viral RNA synthesis. | [88] |
| 32. | HO-1 | Down-regulation of HO-1 inhibits CSFV proliferation. | [89] |
| 33. | AIF1 | Promote CSFV replication and IL-6 production. | [90] |
| No. | Drug Candidates | Possible Mechanism Related to the Antiviral Effect of Drug Candidates | Ref. |
|---|---|---|---|
| 1. | BPIP * | A viral polymerase inhibitor; inhibit CSFV replication by targeting the viral polymerase. | [96,97,98] |
| 2. | VP32947 | A small molecule inhibitor of pestivirus replication; possibly target RNA-dependent RNA polymerase. | [99] |
| 3. | BBP/CSFA-0 and its analogues | Pestivirus inhibitors; target the RNA-dependent RNA polymerase. | [100] |
| 4. | 3D8 scFv | A recombinant antibody with RNA-hydrolyzing and cell-penetrating activities; suppress CSFV replication possibly by targeting viral RNA genomes or transcripts. | [101] |
| 5. | Cap-SNase | The fusion protein of CSFV capsid (Cap) and Staphylococcus aureus nuclease (SNase); inhibit the production of CSFV based on the capsid-targeted viral inactivation. | [102] |
| 6. | GP6 | A novel glycosyl sulfoxide; probably target the late steps of the glycosylation process of CSFV E2 and Erns. | [103] |
| 7. | tunicamycin, IW3, IW7 | Inhibitor of glycosylation; inhibit N-glycosylation process of CSFV glycoproteins. | [104,105] |
| 8. | analogs of glycosyltransferase substrates | Inhibit CSFV replication possibly related to the glycosylation process of viral proteins. | [106,107] |
| 9. | IFN-α *, IFN-γ | IFNs induce the expression of interferon-stimulated genes (ISGs) for defense against viral infection. | [34,108,109] |
| 10. | PTD-poMx1 * | Porcine Mx1 fused to HIV Tat protein transduction domain (PTD); inhibit CSFV replication in vitro and in vivo via the antiviral activity of Mx1 protein. | [40,110] |
| 11. | MβCD, 25-hydroxycholesterol | Regulate the level of cellular cholesterol and inhibit CSFV replication. | [111] |
| 12. | U18666A, imipramine | Inhibitor of cholesterol transport; disrupt cholesterol trafficking and then affect CSFV replication. | [112] |
| 13. | 3-MA | Inhibit autophagy; decrease virus yield. | [83] |
| 14. | C75, TOFA | Inhibitors of fatty acid biosynthesis; inhibit CSFV replication. | [114] |
| 15. | etomoxir, TMZ | Inhibitors of fatty acid beta-oxidation; inhibit CSFV replication. | [114] |
| 16. | BFA, GCA, and CI-976 | Inhibitors of vesicular transport between Golgi and ER; inhibit CSFV infection. | [59,60] |
| 17. | 4-PBA, TUDCA | ER stress inhibitors; inhibit CSFV replication. | [115] |
| 18. | 4μ8c | A specific IRE1 endonuclease inhibitor; block the IRE1-XBP1 signal related to unfolded protein response (UPR); reduce CSFV replication. | [116] |
| 19. | LPS | Induce mRNA of IFN-α and IFN-β; impair CSFV replication possibly related to PKR activation. | [117] |
| 20. | LPS-B5, R837 | Lipopolysaccharide from Escherichia coli 055:B5 (LPS-B5) and imiquimod (R837); TLR-specific ligands; exert inhibitory effects on CSFV replication. | [118] |
| 21. | SB203580 | Inhibitor of p38 MAPK activation; suppress CSFV replication. | [80] |
| 22. | U0126 | A specific inhibitor for MEK1/2/ERK1/2; inhibit CSFV replication. | [82] |
| 23. | MG132 | A proteasome inhibitor; inhibit CSFV replication possibly via the activation of the JAK-STAT pathway and the up-regulation of ISGs expression. | [119] |
| 24. | PGA1 | Prostaglandin A1; inhibit CSFV replication. | [120,121] |
| 25. | phage-displayed E2-binding peptides | CSFV-specific ligands; phage displaying the octapeptide sequence DRATSSNA; inhibit CSFV replication possibly through binding CSFV E2 protein. | [122] |
| 26. | ceramide (C6) | Activator of the protein phosphatase 1 (PP1) pathway; inhibit CSFV replication via activation of the PP1 pathway. | [123] |
| 27. | Quercetin | Inhibit the function of HSP70; decrease CSFV replication. | [88] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fan, J.; Liao, Y.; Zhang, M.; Liu, C.; Li, Z.; Li, Y.; Li, X.; Wu, K.; Yi, L.; Ding, H.; et al. Anti-Classical Swine Fever Virus Strategies. Microorganisms 2021, 9, 761. https://doi.org/10.3390/microorganisms9040761
Fan J, Liao Y, Zhang M, Liu C, Li Z, Li Y, Li X, Wu K, Yi L, Ding H, et al. Anti-Classical Swine Fever Virus Strategies. Microorganisms. 2021; 9(4):761. https://doi.org/10.3390/microorganisms9040761
Chicago/Turabian StyleFan, Jindai, Yingxin Liao, Mengru Zhang, Chenchen Liu, Zhaoyao Li, Yuwan Li, Xiaowen Li, Keke Wu, Lin Yi, Hongxing Ding, and et al. 2021. "Anti-Classical Swine Fever Virus Strategies" Microorganisms 9, no. 4: 761. https://doi.org/10.3390/microorganisms9040761
APA StyleFan, J., Liao, Y., Zhang, M., Liu, C., Li, Z., Li, Y., Li, X., Wu, K., Yi, L., Ding, H., Zhao, M., Fan, S., & Chen, J. (2021). Anti-Classical Swine Fever Virus Strategies. Microorganisms, 9(4), 761. https://doi.org/10.3390/microorganisms9040761





