Distribution of HPV Genotypes Differs Depending on Behavioural Factors among Young Women
Abstract
1. Introduction
2. Materials and Methods
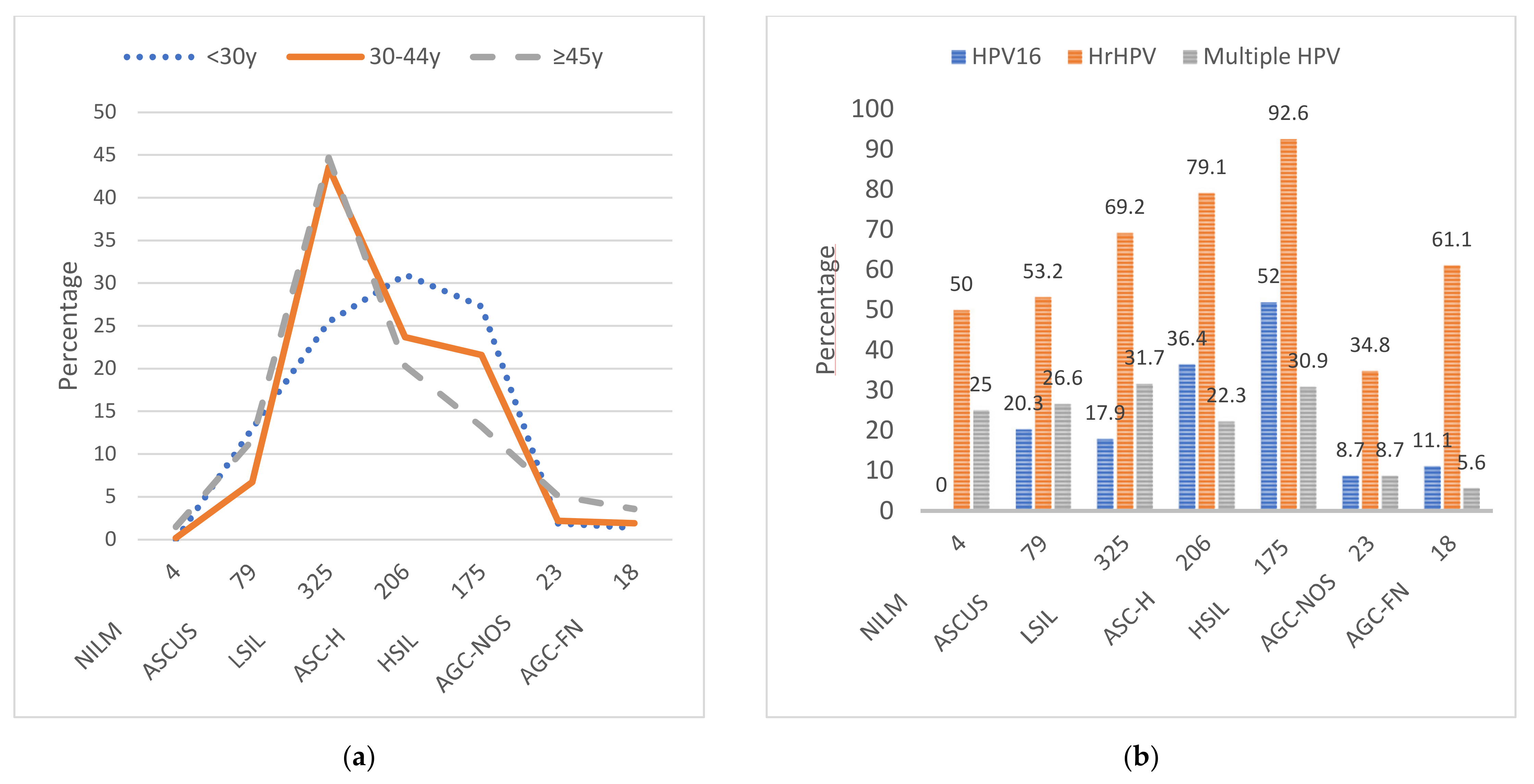
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Walboomers, J.M.; Jacobs, M.V.; Manos, M.M.; Bosch, F.X.; Kummer, J.A.; Shah, K.V.; Snijders, P.J.; Peto, J.; Meijer, C.J.; Muñoz, N. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J. Pathol. 1999, 189, 12–19. [Google Scholar] [CrossRef]
- Bruni, L.; Albero, G.; Serrano, B.; Mena, M.; Gómez, D.; Muñoz, J.; Bosch, F.X.; de Sanjosé, S.; ICO/IARC Information Centre on HPVand Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases in the World. Summary Report 17 June 2019. Available online: http//:www.hpvcentre.net/statistics/reports/XWX.pdf (accessed on 1 February 2021).
- Castellsagué, X. Natural history and epidemiology of HPV infection and cervical cancer. Gynecol. Oncol. 2008, 110, S4–S7. [Google Scholar] [CrossRef]
- Castle, P.E.; Schiffman, M.; Herrero, R.; Hildesheim, A.; Rodriguez, A.C.; Bratti, M.C.; Sherman, M.E.; Wacholder, S.; Tarone, R.; Burk, R.D. A prospective study of age trends in cervical human papillomavirus acquisition and persistence in Guanacaste, Costa Rica. J. Infect. Dis. 2005, 191, 1808–1816. [Google Scholar] [CrossRef]
- Kjaer, S.K.; Chackerian, B.; Brule, A.J.V.D.; Svare, E.I.; Paull, G.; Walbomers, J.M.; Schiller, J.T.; Bock, J.E.; Sherman, M.E.; Lowy, D.R.; et al. High-risk human papillomavirus is sexually transmitted: Evidence from a follow-up study of virgins starting sexual activity (intercourse). Cancer Epidemiol. Biomarkers Prev. 2001, 10, 101–106. [Google Scholar] [PubMed]
- Castellsagué, X.; for the HPV PATRICIA Study Group; Paavonen, J.; Jaisamrarn, U.; Wheeler, C.M.; Skinner, S.R.; Lehtinen, M.; Naud, P.; Chow, S.-N.; Del Rosario-Raymundo, M.R.; et al. Risk of first cervical HPV infection and pre-cancerous lesions after onset of sexual activity: Analysis of women in the control arm of the randomized, controlled PATRICIA trial. BMC Infect. Dis. 2014, 14, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Deacon, J.M.; Evans, C.D.; Yule, R.; Desai, M.; Binns, W.; Taylor, C.; Peto, J. Sexual behaviour and smoking as determinants of cervical HPV infection and of CIN3 among those infected: A case-control study nested within the Manchester cohort. Br. J. Cancer 2000, 83, 1565–1572. [Google Scholar] [CrossRef] [PubMed]
- International Collaboration of Epidemiological Studies of Cervical Cancer. Cervical carcinoma and sexual behavior: Collaborative reanalysis of individual data on 15,461 women with cervical carcinoma and 29,164 women without cervical carcinoma from 21 epidemiological studies. Cancer Epidemiol. Biomarkers Prev. 2009, 18, 1060–1069. [Google Scholar] [CrossRef] [PubMed]
- Luhn, P.; Walker, J.; Schiffman, M.; Zuna, R.E.; Dunn, S.T.; Gold, M.A.; Smith, K.; Mathews, C.; Allen, R.A.; Zhang, R.; et al. The role of co-factors in the progression from human papillomavirus infection to cervical cancer. Gynecol. Oncol. 2013, 128, 265–270. [Google Scholar] [CrossRef]
- Bouvard, V.; Baan, R.; Straif, K.; Grosse, Y.; Secretan, B.; El Ghissassi, F.; Benbrahim-Tallaa, L.; Guha, N.; Freeman, C.; Galichet, L.; et al. A review of human carcinogens—Part B: Biological agents. Lancet Oncol. 2009, 10, 321–322. [Google Scholar] [CrossRef]
- Rotondo, J.C.; Oton-Gonzalez, L.; Mazziotta, C.; Lanzillotti, C.; Iaquinta, M.R.; Tognon, M.; Martini, F. Simultaneous detection and viral DNA load quantification of different human papillomavirus types in clinical specimens by the high analytical droplet digital PCR method. Front. Microbiol. 2020, 11, 591452. [Google Scholar] [CrossRef] [PubMed]
- Working Group Set Up by the Finnish Medical Society Duodecim. Cytological Changes in the Cervix, Vagina and Vulva. In Current Care Guidelines; Duodecim: Helsinki, Finland, 2019; Available online: http://www.kaypahoito.fi (accessed on 17 April 2019).
- Söderlund-Strand, A.; Carlson, J.; Dillner, J. Modified general primer PCR system for sensitive detection of multiple types of oncogenic human papillomavirus. J. Clin. Microbiol. 2009, 47, 541–546. [Google Scholar] [CrossRef]
- Webropol Oy. Webropol Web-Based Questionnaire Application. Available online: https://new.webropolsurveys.com/Account/Login?ReturnUrl=%2f (accessed on 3 March 2016).
- Leinonen, M.K.; Anttila, A.; Malila, N.; Dillner, J.; Forslund, O.; Nieminen, P. Type- and age-specific distribution of human papillomavirus in women attending cervical cancer screening in Finland. Br. J. Cancer 2013, 109, 2941–2950. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tobacco Statistics 2018. 44/2019. Finnish National Institute of Health and Welfare. Available online: http//www.thl.fi/tilastot/tupakka (accessed on 11 December 2019).
- Roura, E.; Castellsagué, X.; Pawlita, M.; Travier, N.; Waterboer, T.; Margall, N.; Bosch, F.X.; De Sanjosé, S.; Dillner, J.; Gram, I.T.; et al. Smoking as a major risk factor for cervical cancer and pre-cancer: Results from the EPIC cohort. Int. J. Cancer 2013, 135, 453–466. [Google Scholar] [CrossRef] [PubMed]
- Simen-Kapeu, A.; Kataja, V.; Yliskoski, M.; Syrjänen, K.; Dillner, J.; Koskela, P.; Paavonen, J.; Lehtinen, M. Smoking impairs human papillomavirus (HPV) type 16 and 18 capsids antibody response following natural HPV infection. Scand. J. Infect. Dis. 2008, 40, 745–751. [Google Scholar] [CrossRef]
- Koshiol, J.; Schroeder, J.; Jamieson, D.J.; Marshall, S.W.; Duerr, A.; Heilig, C.M.; Shah, K.V.; Klein, R.S.; Cu-Uvin, S.; Schuman, P.; et al. Smoking and time to clearance of human papillomavirus infection in HIV-seropositive and HIV-seronegative women. Am. J. Epidemiol. 2006, 164, 176–183. [Google Scholar] [CrossRef]
- Eldridge, R.C.; Pawlita, M.; Wilson, L.; Castle, P.E.; Waterboer, T.; Gravitt, P.E.; Schiffman, M.; Wentzensen, N. Smoking and subsequent human papillomavirus infection: A mediation analysis. Ann. Epidemiol. 2017, 27, 724–730.e1. [Google Scholar] [CrossRef] [PubMed]
- Sierra, M.S.; Tsang, S.H.; Hu, S.; Porras, C.; Herrero, R.; Kreimer, A.R.; Schussler, J.; Boland, J.; Wagner, S.; Cortes, B.; et al. Risk factors for non–human papillomavirus (HPV) type 16/18 cervical infections and associated lesions among HPV DNA–negative women vaccinated against HPV-16/18 in the Costa Rica vaccine trial. J. Infect. Dis. 2020, 20, 1–14. [Google Scholar] [CrossRef]
- Ribeiro, A.A.; Costa, M.C.; Alves, R.R.F.; Villa, L.L.; Saddi, V.A.; Carneiro, M.A.D.S.; Zeferino, L.C.; Rabelo-Santos, S.H. HPV infection and cervical neoplasia: Associated risk factors. Infect. Agents Cancer 2015, 10, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Burger, E.A.; Kim, J.J.; Sy, S.; Castle, P.E. Age of acquiring causal human papillomavirus (HPV) infections: Leveraging simulation models to explore the natural history of HPV-induced cervical cancer. Clin. Infect. Dis. 2017, 65, 893–899. [Google Scholar] [CrossRef] [PubMed]
- Olesen, T.B.; Jensen, K.E.; Nygård, M.; Tryggvadottir, L.; Sparén, P.; Hansen, B.T.; Liaw, K.-L.; Kjaer, S.K. Young age at first intercourse and risk-taking behaviours—A study of nearly 65,000 women in four Nordic countries. Eur. J. Public Health 2011, 22, 220–224. [Google Scholar] [CrossRef]
- Lehtinen, M.; Kaasila, M.; Pasanen, K.; Patama, T.; Palmroth, J.; Laukkanen, P.; Pukkala, E.; Koskela, P. Seroprevalence atlas of infections with oncogenic and non-oncogenic human papillomaviruses in Finland in the 1980s and 1990s. Int. J. Cancer 2006, 119, 2612–2619. [Google Scholar] [CrossRef]
- Mercer, C.H.; Tanton, C.; Prah, P.; Erens, B.; Sonnenberg, P.; Clifton, S.; Macdowall, W.; Lewis, R.; Field, N.; Datta, J.; et al. Changes in sexual attitudes and lifestyles in Britain through the life course and over time: Findings from the National Surveys of Sexual Attitudes and Lifestyles (Natsal). Lancet 2013, 382, 1781–1794. [Google Scholar] [CrossRef]
- Castellsagué, X.; Díaz, M.; Vaccarella, S.; De Sanjosé, S.; Muñoz, N.; Herrero, R.; Franceschi, S.; Meijer, C.J.L.M.; Bosch, F.X. Intrauterine device use, cervical infection with human papillomavirus, and risk of cervical cancer: A pooled analysis of 26 epidemiological studies. Lancet Oncol. 2011, 12, 1023–1031. [Google Scholar] [CrossRef]
- Cortessis, V.K.; Barrett, M.; Wade, N.B.; Enebish, T.; Perrigo, J.L.; Tobin, J.; Zhong, C.; Zink, J.; Isiaka, V.; Muderspach, L.I.; et al. Intrauterine device use and cervical cancer risk. Obstet. Gynecol. 2017, 130, 1226–1236. [Google Scholar] [CrossRef] [PubMed]
- Averbach, S.H.; Ma, Y.; Smith-McCune, K.; Shiboski, S.; Moscicki, A.B. The effect of intrauterine devices on acquisition and clearance of human papillomavirus. Am. J. Obstet. Gynecol. 2017, 216, 386.e1–386.e5. [Google Scholar] [CrossRef]
- Averbach, S.; Silverberg, M.J.; Leyden, W.; Smith-McCune, K.; Raine-Bennett, T.; Sawaya, G.F. Recent intrauterine device use and the risk of precancerous cervical lesions and cervical cancer. Contraception 2018, 98, 130–134. [Google Scholar] [CrossRef] [PubMed]
- Roura, E.; Travier, N.; Waterboer, T.; De Sanjosé, S.; Bosch, F.X.; Pawlita, M.; Pala, V.; Weiderpass, E.; Margall, N.; Dillner, J.; et al. The influence of hormonal factors on the risk of developing cervical cancer and pre-cancer: Results from the EPIC cohort. PLoS ONE 2016, 11, e0147029. [Google Scholar] [CrossRef]
- Hildesheim, A.; Herrero, R.; Castle, P.E.; Wacholder, S.; Bratti, M.C.; Sherman, M.E.; Lorincz, A.T.; Burk, R.D.; Morales, J.; Rodriguez, A.C.; et al. HPV co-factors related to the development of cervical cancer: Results from a population-based study in Costa Rica. Br. J. Cancer 2001, 84, 1219–1226. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.; Wang, X.; Feng, H.; Yan, G. Is oral contraceptive use associated with an increased risk of cervical cancer? An evidence-based meta-analysis. J. Obstet. Gynaecol. Res. 2017, 43, 913–922. [Google Scholar] [CrossRef]
- Rousseau, M.C.; Franco, E.L.; Villa, L.L.; Sobrinho, J.P.; Termini, L.; Prado, J.M.; Rohan, T.E. A cumulative case-control study of risk factor profiles for oncogenic and nononcogenic cervical human papillomavirus infections. Cancer Epidemiol. Biomarkers Prev. 2000, 9, 469–476. [Google Scholar]
- Leinonen, M.; Kotaniemi-Talonen, L.; Anttila, A.; Dyba, T.; Tarkkanen, J.; Nieminen, P. Prevalence of oncogenic human papillomavirus infection in an organised screening population in Finland. Int. J. Cancer 2008, 123, 1344–1349. [Google Scholar] [CrossRef] [PubMed]
- Cotton, S.C.; on behalf of the TOMBOLA Group; Sharp, L.; Seth, R.; Masson, L.F.; Little, J.; Cruickshank, M.E.; Neal, K.; Waugh, N. Lifestyle and socio-demographic factors associated with high-risk HPV infection in UK women. Br. J. Cancer 2007, 97, 133–139. [Google Scholar] [CrossRef] [PubMed]
| <30 y | 30–44 y | ≥45 y | All Women | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |
| High-Risk HPV Genotypes | (n = 234) | (n = 444) | (n = 201) | (n = 879) p 4 |
| 16 | 90 (38.5) | 136 (30.6) | 30 (14.9) | 256 (29.1) 0.000 |
| 18 | 15 (6.4) | 27 (6.1) | 14 (7.0) | 56 (6.4) 0.913 |
| 31 | 25 (10.7) | 47 (10.6) | 9 (4.5) | 81 (9.2) 0.022 |
| 33 | 14 (6.0) | 16 (3.6) | 7 (3.5) | 37 (4.2) 0.302 |
| 35 | 5 (2.1) | 8 (1.8) | 4 (2.0) | 17 (1.9) 0.949 |
| 39 | 11 (4.7) | 14 (3.2) | 8 (4.0) | 33 (3.8) 0.571 |
| 45 | 7 (3.0) | 23 (5.2) | 4 (2.0) | 34 (3.9) 0.133 |
| 51 | 24 (10.3) | 22 (5.0) | 13 (6.5) | 59 (6.7) 0.032 |
| 52 | 21 (9.0) | 33 (7.4) | 9 (4.5) | 63 (7.2) 0.173 |
| 56 | 10 (4.3) | 31 (7.0) | 11 (5.5) | 52 (5.9) 0.369 |
| 58 | 8 (3.4) | 17 (3.8) | 5 (2.5) | 30 (3.4) 0.781 |
| 59 | 6 (2.6) | 14 (3.2) | 5 (2.5) | 25 (2.8) 0.896 |
| 66 | 19 (8.1) | 26 (5.9) | 11 (5.5) | 56 (6.4) 0.434 |
| 68 | 4 (1.7) | 10 (2.3) | 9 (4.5) | 23 (2.6) 0.174 |
| Low-Risk HPV Genotypes | ||||
| 6 | 8 (3.4) | 5 (1.1) | 1 (0.5) | 14 (1.6) 0.042 |
| 11 | 0 (0.0) | 2 (0.5) | 1 (0.5) | 3 (0.3) 0.611 |
| 30 | 0 (0.0) | 1 (0.2) | 0 (0.0) | 1 (0.1) 1.000 |
| 40 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) - |
| 42 | 9 (3.8) | 11 (2.5) | 9 (4.5) | 29 (3.3) 0.345 |
| 43 | 2 (0.9) | 3 (0.7) | 0 (0.0) | 5 (0.6) 0.611 |
| 53 | 11 (4.7) | 13 (2.9) | 10 (5.0) | 34 (3.9) 0.330 |
| 61 | 0 (0.0) | 1 (0.2) | 1 (0.5) | 2 (0.2) 0.476 |
| 67 | 7 (3.0) | 8 (1.8) | 3 (1.5) | 18 (2.0) 0.522 |
| 69 | 1 (0.4) | 4 (0.9) | 1 (0.5) | 6 (0.7) 0.874 |
| 70 | 3 (1.3) | 17 (3.8) | 8 (4.0) | 28 (3.2) 0.137 |
| 73 | 1 (0.4) | 1 (0.2) | 1 (0.5) | 3 (0.3) 0.796 |
| 74 | 4 (1.7) | 2 (0.5) | 1 (0.5) | 7 (0.8) 0.215 |
| 81 | 4 (1.7) | 2 (0.5) | 2 (1.0) | 8 (0.9) 0.262 |
| 83 | 3 (1.3) | 3 (0.7) | 2 (1.0) | 8 (0.9) 0.651 |
| 86 | 0 (0.0) | 2 (0.5) | 2 (1.0) | 4 (0.5) 0.266 |
| 87 | 9 (3.8) | 10 (2.3) | 3 (1.5) | 22 (2.5) 0.274 |
| 89 | 4 (1.7) | 2 (0.5) | 3 (1.5) | 9 (1.0) 0.179 |
| 90 | 13 (5.6) | 1 (0.2) | 3 (1.5) | 17 (1.9) 0.000 |
| 91 | 5 (2.1) | 8 (1.8) | 2 (1.0) | 15 (1.7) 0.699 |
| Different HPV Groups | ||||
| Any HPV+ | 209 (89.3) | 380 (85.6) | 143 (71.1) | 732 (83.3) 0.000 |
| HPV-negative | 25 (10.7) | 64 (14.4) | 58 (28.9) | 147 (16.7) 0.000 |
| High-risk HPV+ 1 | 186 (79.5) | 342 (77.0) | 116 (57.7) | 644 (73.3) 0.000 |
| Low-risk HPV+ 2 | 66 (28.2) | 82 (18.5) | 48 (23.9) | 196 (22.3) 0.013 |
| Single HPV | 116 (55.5) | 275 (72.4) | 104 (72.7) | 495 (67.6) 0.000 |
| Multiple HPV (≥2+) 3 | 93 (44.5) | 105 (27.6) | 39 (27.3) | 237 (32.4) 0.000 |
| Recorded Risk Factors OR (95% CI) | HPV 16 vs. lr-HPV/HPV-Negative | nonHPV16-hrHPV vs. lrHPV/HPV-Negative | ||||||
|---|---|---|---|---|---|---|---|---|
| <30 y | 30–44 y | ≥45 y | All Women | <30 y | 30–44 y | ≥45 y | All Women | |
| Contraception | ||||||||
| Condom | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| No | 1.85 (0.59–5.75) | 0.72 (0.35–1.48) | 2.26 (0.67–7.60) | 0.80 (0.50–1.30) | 2.08 (0.65–6.70) | 0.94 (0.49–1.79) | 1.39 (0.63–3.08) | 1.01 (0.65–1.56) |
| E+P 1 | 1.12 (0.47–2.69) | 1.56 (0.69–3.56) | 1.38 (0.12–15.72) | 1.65 (0.97–2.83) | 1.67 (0.69–4.05) | 1.69 (0.78–3.66) | 0.73 (0.12–4.53) | 1.65 (0.99–2.74) |
| Progestin 2 | 1.83 (0.54–6.13) | 0.94 (0.33–2.64) | 3.67 (0.46–29.42) | 1.60 (0.79–3.24) | 2.17 (0.63–7.47) | 0.93 (0.35–2.45) | 0.98 (0.15–6.58) | 1.34 (0.67–2.65) |
| Hormonal IUD | 1.30 (0.21–8.03) | 1.06 (0.49–2.28) | 2.75 (0.61–12.48) | 1.12 (0.62–2.04) | 5.00 (0.96–25.94) | 1.25 (0.62–2.54) | 3.81 (1.43–10.17) | 1.98 (1.17–3.35) |
| Cu IUD | 0.65 (0.04–11.24) | 1.00 (0.32–3.16) | NPa | 0.99 (0.37–2.63) | 1.67 (0.14–20.23) | 0.53 (0.16–1.78) | 0.73 (0.06–8.83) | 0.74 (0.28–1.95) |
| Oral sex | 1.40 (0.30–6.53) | 0.87 (0.34–2.23) | 2.32 (0.73–7.39) | 1.96 (1.10–3.52) | 3.13 (0.51–19.42) | 0.82 (0.35–1.95) | 1.11 (0.56–2.21) | 1.37 (0.85–2.23) |
| Anal sex | 3.56 (1.36–9.35) | 0.78 (0.45–1.36) | 0.85 (0.28–2.56) | 1.28 (0.85–1.92) | 2.24 (0.84–5.93) | 0.74 (0.44–1.23) | 1.51 (0.73–3.13) | 1.12 (0.77–1.64) |
| Parity | ||||||||
| 0 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1–2 | 0.70 (0.30–1.62) | 0.90 (0.51–1.59) | 1.30 (0.37–4.55) | 0.61 (0.41–0.90) | 0.69 (0.30–1.59) | 1.17 (0.70–1.96) | 1.30 (0.55–3.07) | 0.92 (0.64–1.31) |
| ≥3 | NPb | 0.90 (0.43–1.88) | 1.25 (0.33–4.70) | 0.48 (0.29–0.81) | NPb | 0.58 (0.28–1.20) | 0.81 (0.31–2.07) | 0.48 (0.29–0.78) |
| Alcohol use | ||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| <6 doses/use | 2.86 (0.42–19.65) | 1.87 (0.63–5.55) | 0.47 (0.12–1.89) | 1.07 (0.52–2.22) | 2.86 (0.42–19.65) | 1.60 (0.63–4.09) | 1.44 (0.44–4.77) | 1.47 (0.78–2.79) |
| >6 doses/use | 2.32 (0.78–6.86) | 1.83 (0.73–4.57) | 0.52 (0.15–1.82) | 1.59 (0.87–2.91) | 2.47 (0.83–7.30) | 1.23 (0.57–2.67) | 1.38 (0.45–4.26) | 1.50 (0.87–2.57) |
| Smoking | ||||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 3.74 (1.42–9.88) | 3.29 (1.69–6.40) | 1.15 (0.35–3.81) | 2.94 (1.84–4.70) | 2.31 (0.88–6.07) | 1.75 (0.94–3.26) | 1.38 (0.61–3.15) | 1.76 (1.14–2.72) |
| Ex-smoker | 2.42 (1.05–5.58) | 2.51 (1.35–4.67) | 1.34 (0.53–3.34) | 2.02 (1.33–3.07) | 1.63 (0.72–3.71) | 1.60 (0.91–2.81) | 1.08 (0.55–2.11) | 1.37 (0.94–2.00) |
| >1 partner in 12 months | 0.88 (0.37–2.12) | 0.63 (0.31–1.25) | 1.71 (0.46–6.33) | 0.96 (0.59–1.57) | 1.20 (0.52–2.77) | 0.93 (0.51–1.69) | 1.14 (0.40–3.30) | 1.16 (0.75–1.79) |
| Age at first intercourse | ||||||||
| ≤15 y | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 16–19 y | 0.37 (0.17–0.81) | 1.17 (0.64–2.12) | 0.30 (0.11–0.86) | 0.56 (0.37–0.85) | 0.69 (0.32–1.53) | 1.24 (0.71–2.16) | 0.63 (0.27–1.48) | 0.84 (0.57–1.25) |
| ≥20 y | 0.59 (0.10–3.60) | 0.62 (0.25–1.54) | 0.56 (0.15–2.09) | 0.43 (0.23–0.83) | 0.77 (0.13–4.79) | 0.81 (0.36–1.80) | 0.74 (0.25–2.17) | 0.69 (0.39–1.24) |
| Lifetime partners | ||||||||
| 1–3 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 4–10 | 1.54 (0.51–4.66) | 1.39 (0.62–3.14) | 3.73 (0.96–14.51) | 2.01 (1.15–3.49) | 1.50 (0.50–4.54) | 1.47 (0.70–3.08) | 2.40 (1.03–5.59) | 1.83 (1.13–2.98) |
| 11–20 | 2.15 (0.66–7.01) | 1.51 (0.64–3.55) | 3.00 (0.65–13.76) | 2.36 (1.30–4.26) | 1.85 (0.56–6.07) | 2.06 (0.95–4.46) | 2.50 (0.96–6.50) | 2.42 (1.44–4.07) |
| >20 | 5.00 (1.03–24.28) | 2.20 (0.89–5.45) | 2.86 (0.59–13.81) | 2.94 (1.55–5.58) | 9.33 (2.00–43.63) | 1.55 (0.65–3.65) | 2.57 (0.96–6.88) | 2.75 (1.54–4.88) |
| TOP | 1.40 (0.59–3.35) | 0.95 (0.52–1.73) | 0.65 (0.22–1.92) | 1.00 (0.66–1.53) | 1.07 (0.44–2.58) | 0.94 (0.54–1.63) | 0.74 (0.35–1.56) | 0.91 (0.62–1.35) |
| Vitamin D usage | 0.95 (0.47–1.93) | 0.49 (0.29–0.82) | 2.27 (0.91–5.68) | 0.73 (0.51–1.05) | 1.07 (0.53–2.15) | 0.72 (0.44–1.18) | 1.15 (0.63–2.10) | 0.91 (0.66–1.27) |
| Atopia | 0.83 (0.34–2.01) | 0.50 (0.26–0.97) | 1.99 (0.73–5.41) | 0.79 (0.50–1.24) | 0.98 (0.41–2.31) | 0.76 (0.43–1.33) | 1.17 (0.52–2.64) | 0.93 (0.62–1.40) |
| Miscarriages | 1.07 (0.26–4.49) | 0.53 (0.28–1.02) | 1.54 (0.56–4.29) | 0.68 (0.42–1.12) | 0.65 (0.14–3.04) | 0.64 (0.36–1.13) | 0.99 (0.44–2.22) | 0.74 (0.48–1.14) |
| Drugs | 1.36 (0.54–3.38) | 1.25 (0.67–2.32) | NPa | 1.47 (0.92–2.36) | 1.67 (0.69–4.05) | 1.12 (0.62–2.00) | 2.14 (0.76–5.98) | 1.54 (1.00–2.37) |
| Recorded Risk Factors OR (95% CI) | lrHPV (Including Low-Risk Multiple Infections 3) vs. HPV-Negative | |||
|---|---|---|---|---|
| <30 y | 30–44 y | ≥45 y | All Women | |
| Contraception | ||||
| Condom | 1.00 | 1.00 | 1.00 | 1.00 |
| No | 0.44 (0.06–3.16) | 0.55 (0.17–1.76) | 1.33 (0.42–4.21) | 0.73 (0.36–1.47) |
| E+P 1 | 1.09 (0.28–4.33) | 1.75 (0.46–6.65) | NPa | 1.50 (0.66–3.45) |
| Progestin 2 | 0.22 (0.02–2.45) | 1.05 (0.21–5.19) | NPa | 0.56 (0.16–1.93) |
| Hormonal IUD | 0.88 (0.05–16.74) | 1.56 (0.47–5.10) | 1.78 (0.37–8.59) | 1.38 (0.57–3.31) |
| Cu IUD | NPa | 0.88 (0.14–5.51) | 2.67 (0.14–49.76) | 0.85 (0.19–3.67) |
| Oral sex | 1.91 (0.16–22.63) | 4.42 (0.52–37.44) | 0.83 (0.30–2.28) | 1.50 (0.68–3.31) |
| Anal sex | 2.42 (0.40–14.69) | 1.17 (0.50–2.71) | 1.02 (0.31–3.30) | 1.18 (0.64–2.18) |
| Parity | ||||
| 0 | 1.00 | 1.00 | 1.00 | 1.00 |
| 1–2 | 1.12 (0.30–4.13) | 1.03 (0.42–2.54) | 1.08 (0.29–4.09) | 0.85 (0.47–1.54) |
| ≥3 | NPb | 1.93 (0.62–5.95) | 1.39 (0.34–5.60) | 1.13 (0.55–2.32) |
| Alcohol use | ||||
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| <6 doses/use | 1.00 (0.05–22.18) | 0.70 (0.15–3.37) | 0.62 (0.23–1.68) | 0.62 (0.23–1.68) |
| >6 doses/use | 0.90 (0.20–4.14) | 0.83 (0.24–2.88) | 0.81 (0.17–3.79) | 0.82 (0.37–1.85) |
| Smoking | ||||
| No | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 1.43 (0.27–7.55) | 1.25 (0.43–3.59) | 1.67 (0.48–5.81) | 1.36 (0.66–2.80) |
| Ex-smoker | 0.77 (0.20–2.98) | 0.91 (0.34–2.40) | 0.85 (0.30–2.42) | 0.81 (0.44–1.52) |
| >1 partner in 12 mo | 1.85 (0.45–7.65) | 0.89 (0.32–2.46) | 3.19 (0.66–15.39) | 1.52 (0.75–3.09) |
| Age at first intercourse | ||||
| ≤15 y | 1.00 | 1.00 | 1.00 | 1.00 |
| 16–19 y | 0.89 (0.24–3.32) | 0.88 (0.35–2.22) | 1.21 (0.29–5.06) | 0.89 (0.47–1.72) |
| ≥20 y | 1.00 (0.05–19.96) | 0.77 (0.21–2.88) | 1.67 (0.29–9.45) | 0.90 (0.35–2.28) |
| Lifetime partners | ||||
| 1–3 | 1.00 | 1.00 | 1.00 | 1.00 |
| 4–10 | 2.54 (0.42–15.21) | 2.03 (0.56–7.40) | 7.00 (1.72–28.54) | 3.50 (1.53–8.04) |
| 11–20 | 4.80 (0.68–33.80) | 2.23 (0.57–8.69) | 2.33 (0.45–12.23) | 3.10 (1.26–7.60) |
| ≥20 | 6.00 (0.34–107.42) | 2.28 (0.52–9.99) | 2.80 (0.52–14.96) | 2.75 (1.01–7.48) |
| TOP | 0.84 (0.20–3.62) | 2.25 (0.90–5.64) | 0.90 (0.30–2.67) | 1.32 (0.71–2.46) |
| Vitamin D usage | 0.64 (0.20–2.03) | 1.22 (0.52–2.85) | 0.84 (0.34–2.11) | 0.90 (0.53–1.54) |
| Atopia | 0.67 (0.16–2.75) | 0.74 (0.28–1.92) | 1.49 (0.44–5.08) | 0.91 (0.47–1.76) |
| Miscarriages | 2.29 (0.19–27.05) | 1.33 (0.54–3.30) | 0.31 (0.06–1.48) | 0.87 (0.44–1.74) |
| Drugs | 2.04 (0.43–9.70) | 1.05 (0.39–2.81) | 1.08 (0.19–6.29) | 1.30 (0.63–2.70) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bergqvist, L.; Kalliala, I.; Aro, K.; Auvinen, E.; Jakobsson, M.; Kiviharju, M.; Virtanen, S.; Dillner, J.; Nieminen, P.; Louvanto, K. Distribution of HPV Genotypes Differs Depending on Behavioural Factors among Young Women. Microorganisms 2021, 9, 750. https://doi.org/10.3390/microorganisms9040750
Bergqvist L, Kalliala I, Aro K, Auvinen E, Jakobsson M, Kiviharju M, Virtanen S, Dillner J, Nieminen P, Louvanto K. Distribution of HPV Genotypes Differs Depending on Behavioural Factors among Young Women. Microorganisms. 2021; 9(4):750. https://doi.org/10.3390/microorganisms9040750
Chicago/Turabian StyleBergqvist, Laura, Ilkka Kalliala, Karoliina Aro, Eeva Auvinen, Maija Jakobsson, Mari Kiviharju, Seppo Virtanen, Joakim Dillner, Pekka Nieminen, and Karolina Louvanto. 2021. "Distribution of HPV Genotypes Differs Depending on Behavioural Factors among Young Women" Microorganisms 9, no. 4: 750. https://doi.org/10.3390/microorganisms9040750
APA StyleBergqvist, L., Kalliala, I., Aro, K., Auvinen, E., Jakobsson, M., Kiviharju, M., Virtanen, S., Dillner, J., Nieminen, P., & Louvanto, K. (2021). Distribution of HPV Genotypes Differs Depending on Behavioural Factors among Young Women. Microorganisms, 9(4), 750. https://doi.org/10.3390/microorganisms9040750







