Fecal Microbiota Transplantation in the Treatment of Chronic Pouchitis: A Systematic Review
Abstract
1. Introduction
2. Methods
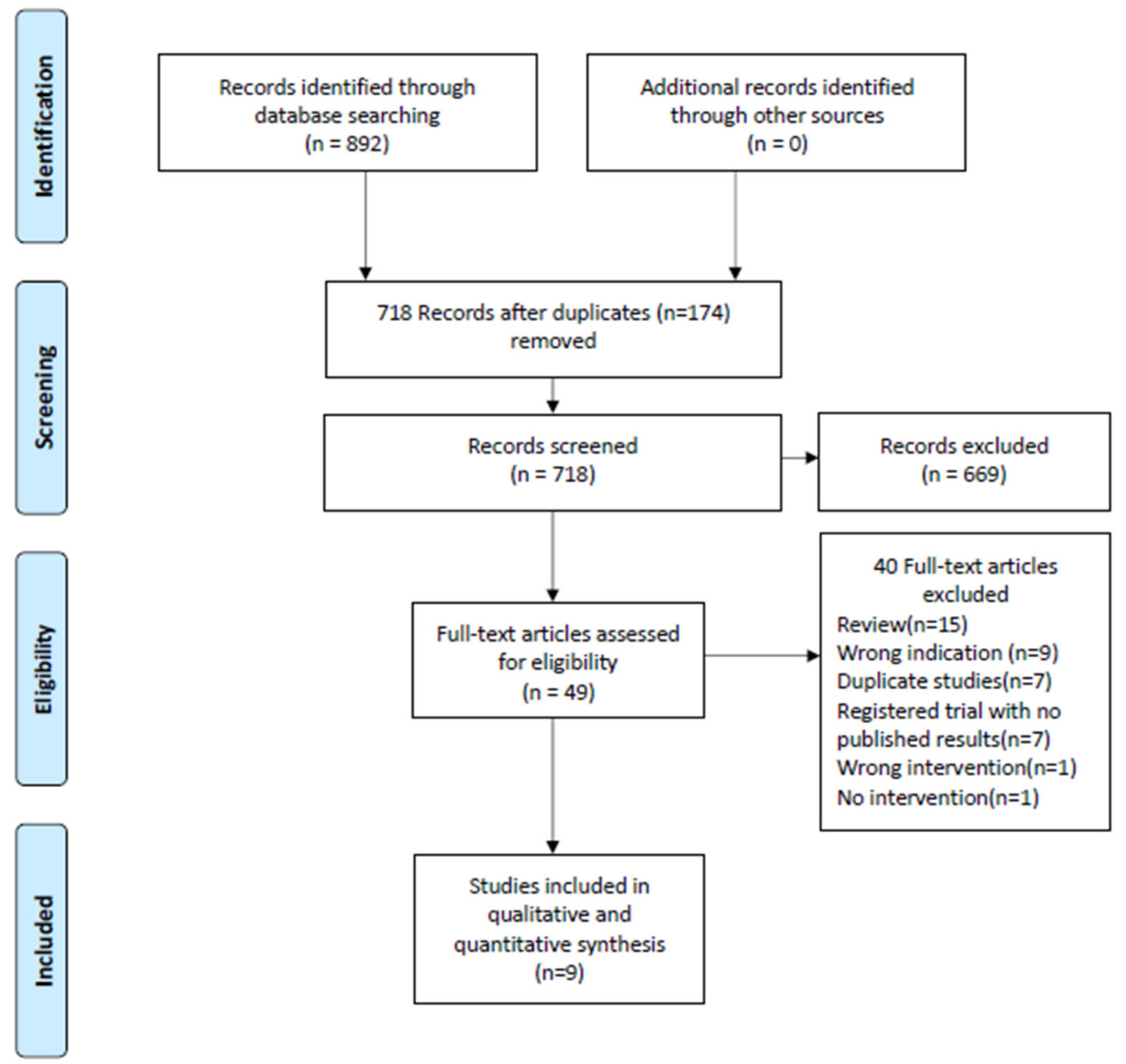
2.1. Search Strategy and Study Selection
2.2. Data Management and Analysis
2.3. Risk of Bias and Quality Assessment
3. Results
3.1. Patient Characteristics and Study Types
3.2. Clinical Effects of FMT Treatment
3.3. Safety/Adverse Events
3.4. Microbiome Changes after FMT
3.5. Preparation and Delivery of FMT Material
3.6. Quality Assessment of Studies and Risk Of Bias
4. Discussion
4.1. Main Findings
4.2. Strengths and Limitations
4.3. Clinical Efficacy of Treatment
4.4. Safety
4.5. Microbiome Changes
4.6. FMT Material: Donors
4.7. FMT Material: Preparation and Delivery
4.8. FMT Material: Route of Administration
4.9. Perspectives
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ng, K.S.; Gonsalves, S.J.; Sagar, P.M. Ileal-anal pouches: A review of its history, indications, and complications. World J. Gastroenterol. 2019, 25, 4320–4342. [Google Scholar] [CrossRef] [PubMed]
- Hata, K.; Ishihara, S.; Nozawa, H.; Kawai, K.; Kiyomatsu, T.; Tanaka, T.; Kishikawa, J.; Anzai, H.; Watanabe, T. Pouchitis after ileal pouch-anal anastomosis in ulcerative colitis: Diagnosis, management, risk factors, and incidence. Dig. Endosc. Off. J. Jpn. Gastroenterol. Endosc. Soc. 2017, 29, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.H.; Li, J.Q.; Khan, F.; Chouhan, H.; Yu, G.Y.; Remer, E.; Stocchi, L.; Hull, T.L.; Shen, B. Difference in the frequency of pouchitis between ulcerative colitis and familial adenomatous polyposis: Is the explanation in peripouch fat? Colorectal Dis. Off. J. Assoc. Coloproctology Great Br. Irel. 2019, 21, 1032–1044. [Google Scholar] [CrossRef] [PubMed]
- Shah, H.; Zezos, P. Pouchitis: Diagnosis and management. Curr. Opin. Gastroenterol. 2020, 36, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Fazio, V.W.; Kiran, R.P.; Remzi, F.H.; Coffey, J.C.; Heneghan, H.M.; Kirat, H.T.; Manilich, E.; Shen, B.; Martin, S.T. Ileal pouch anal anastomosis: Analysis of outcome and quality of life in 3707 patients. Ann. Surg. 2013, 257, 679–685. [Google Scholar] [CrossRef] [PubMed]
- Segal, J.P.; Ding, N.S.; Worley, G.; McLaughlin, S.; Preston, S.; Faiz, O.D.; Clark, S.K.; Hart, A.L. Systematic review with meta-analysis: The management of chronic refractory pouchitis with an evidence-based treatment algorithm. Aliment. Pharmacol. Ther. 2017, 45, 581–592. [Google Scholar] [CrossRef]
- Nguyen, N.; Zhang, B.; Holubar, S.D.; Pardi, D.S.; Singh, S. Treatment and prevention of pouchitis after ileal pouch-anal anastomosis for chronic ulcerative colitis. Cochrane Database Syst. Rev. 2019. [Google Scholar] [CrossRef]
- Segal, J.P.; Oke, S.; Hold, G.L.; Clark, S.K.; Faiz, O.D.; Hart, A.L. Systematic review: Ileoanal pouch microbiota in health and disease. Aliment. Pharmacol. Ther. 2018, 47, 466–477. [Google Scholar] [CrossRef]
- Zella, G.C.; Hait, E.J.; Glavan, T.; Gevers, D.; Ward, D.V.; Kitts, C.L.; Korzenik, J.R. Distinct microbiome in pouchitis compared to healthy pouches in ulcerative colitis and familial adenomatous polyposis. Inflamm. Bowel Dis. 2011, 17, 1092–1100. [Google Scholar] [CrossRef]
- McLaughlin, S.D.; Walker, A.W.; Churcher, C.; Clark, S.K.; Tekkis, P.P.; Johnson, M.W.; Parkhill, J.; Ciclitira, P.J.; Dougan, G.; Nicholls, R.J.; et al. The bacteriology of pouchitis: A molecular phylogenetic analysis using 16S rRNA gene cloning and sequencing. Ann. Surg. 2010, 252, 90–98. [Google Scholar] [CrossRef]
- Li, K.Y.; Wang, J.L.; Wei, J.P.; Gao, S.Y.; Zhang, Y.Y.; Wang, L.T.; Liu, G. Fecal microbiota in pouchitis and ulcerative colitis. World J. Gastroenterol. 2016, 22, 8929–8939. [Google Scholar] [CrossRef] [PubMed]
- Dubinsky, V.; Reshef, L.; Bar, N.; Keizer, D.; Golan, N.; Rabinowitz, K.; Godny, L.; Yadgar, K.; Zonensain, K.; Tulchinsky, H.; et al. Predominantly Antibiotic-resistant Intestinal Microbiome Persists in Patients With Pouchitis Who Respond to Antibiotic Therapy. Gastroenterology 2020, 158, 610–624. [Google Scholar] [CrossRef] [PubMed]
- Dalal, R.L.; Shen, B.; Schwartz, D.A. Management of Pouchitis and Other Common Complications of the Pouch. Inflamm. Bowel Dis. 2018, 24, 989–996. [Google Scholar] [CrossRef] [PubMed]
- Gionchetti, P.; Calabrese, C.; Lauri, A.; Rizzello, F. The therapeutic potential of antibiotics and probiotics in the treatment of pouchitis. Expert Rev. Gastroenterol. Hepatol. 2015, 9, 1175–1181. [Google Scholar] [CrossRef] [PubMed]
- Shen, B. Treatment of chronic and refractory pouchitis. Semin. Colon Rectal Surg. 2017, 28, 138–141. [Google Scholar] [CrossRef]
- Verbeke, K.A.; Boesmans, L.; Boets, E. Modulating the microbiota in inflammatory bowel diseases: Prebiotics, probiotics or fecal transplantation? Proc. Nutr. Soc. 2014, 73, 490–497. [Google Scholar] [CrossRef]
- Hvas, C.L.; Dahl Jorgensen, S.M.; Jorgensen, S.P.; Storgaard, M.; Lemming, L.; Hansen, M.M.; Erikstrup, C.; Dahlerup, J.F. Fecal Microbiota Transplantation Is Superior to Fidaxomicin for Treatment of Recurrent Clostridium difficile Infection. Gastroenterology 2019, 156, 1324–1332. [Google Scholar] [CrossRef]
- Paramsothy, S.; Kamm, M.A.; Kaakoush, N.O.; Walsh, A.J.; van den Bogaerde, J.; Samuel, D.; Leong, R.W.L.; Connor, S.; Ng, W.; Paramsothy, R.; et al. Multidonor intensive fecal microbiota transplantation for active ulcerative colitis: A randomised placebo-controlled trial. Lancet 2017, 389, 1218–1228. [Google Scholar] [CrossRef]
- Sokol, H.; Landman, C.; Seksik, P.; Berard, L.; Montil, M.; Nion-Larmurier, I.; Bourrier, A.; Le Gall, G.; Lalande, V.; De Rougemont, A.; et al. Fecal microbiota transplantation to maintain remission in Crohn’s disease: A pilot randomized controlled study. Microbiome 2020, 8, 12. [Google Scholar] [CrossRef]
- Steube, A.; Vital, M.; Sturm, A.; Buening, C.; Stallmach, A.; Pieper, D. Encapsulated fecal microbiota transfer in patients with chronic, antibiotic-refractory pouchitis. United Eur. Gastroenterol. J. 2017, 5, A307. [Google Scholar] [CrossRef]
- Schmid, M.; Frick, J.S.; Malek, N.; Goetz, M. Successful treatment of pouchitis with Vedolizumab, but not fecal microbiota transfer (FMT), after proctocolectomy in ulcerative colitis. Int. J. Colorectal Dis. 2017, 32, 597–598. [Google Scholar] [CrossRef] [PubMed]
- Stallmach, A.; Lange, K.; Buening, J.; Sina, C.; Vital, M.; Pieper, D.H. Fecal Microbiota Transfer in Patients With Chronic Antibiotic-Refractory Pouchitis. Am. J. Gastroenterol. 2016, 111, 441–443. [Google Scholar] [CrossRef] [PubMed]
- Herfarth, H.; Barnes, E.L.; Long, M.D.; Isaacs, K.L.; Leith, T.; Silverstein, M.; Gerardin, Y.; Kassam, Z. Combined Endoscopic and Oral Fecal Microbiota Transplantation in Patients with Antibiotic-Dependent Pouchitis: Low Clinical Efficacy due to Low Donor Microbial Engraftment. Inflamm. Intest. Dis. 2019, 4, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ (Clin. Res. Ed.) 2009, 339, b2535. [Google Scholar] [CrossRef]
- Fang, H.; Fu, L.; Wang, J. Protocol for Fecal Microbiota Transplantation in Inflammatory Bowel Disease: A Systematic Review and Meta-Analysis. Biomed Res. Int. 2018, 2018, 8941340. [Google Scholar] [CrossRef] [PubMed]
- Castano-Rodriguez, N.; Paramsothy, S.; Kaakoush, N.O. Promise of Fecal Microbiota Transplantation Therapy in Pouchitis. Dig. Dis. Sci. 2019. [Google Scholar] [CrossRef] [PubMed]
- Web of Science. Available online: https://clarivate.com/webofsciencegroup/solutions/web-of-science/ (accessed on 21 April 2020).
- (NIH) U.S. National Library of Medicine. Available online: https://clinicaltrials.gov/ (accessed on 21 April 2020).
- World Health Organisation. International Clinical Trials Registry Platform (ICTRP). Available online: https://apps.who.int/trialsearch/ (accessed on 21 April 2020).
- Opengrey. System for Information in Grey Litterature in Europe. Available online: http://opengrey.eu/ (accessed on 21 April 2020).
- Prospero International Prospective Registry of Systematic Reviews. Available online: https://www.crd.york.ac.uk/PROSPERO/ (accessed on 30 April 2020).
- Steinhart, A.H.; Ben-Bassat, O. Pouchitis: A practical guide. Frontline Gastroenterol. 2013, 4, 198–204. [Google Scholar] [CrossRef] [PubMed]
- Nishida, A.; Imaeda, H.; Inatomi, O.; Bamba, S.; Sugimoto, M.; Andoh, A. The efficacy of fecal microbiota transplantation for patients with chronic pouchitis: A case series. Clin. Case Rep. 2019, 7, 782–788. [Google Scholar] [CrossRef] [PubMed]
- Shen, B.; Achkar, J.P.; Connor, J.T.; Ormsby, A.H.; Remzi, F.H.; Bevins, C.L.; Brzezinski, A.; Bambrick, M.L.; Fazio, V.W.; Lashner, B.A. Modified pouchitis disease activity index: A simplified approach to the diagnosis of pouchitis. Dis. Colon Rectum 2003, 46, 748–753. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Altman, D.G.; Gotzsche, P.C.; Juni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clin. Res. Ed.) 2011, 343, d5928. [Google Scholar] [CrossRef]
- NHLBI. Study Quality Assessment Tools, National Heart, Blood and Lung Institute. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 21 April 2020).
- Lai, C.Y.; Sung, J.; Cheng, F.; Tang, W.; Wong, S.H.; Chan, P.K.S.; Kamm, M.A.; Sung, J.J.Y.; Kaplan, G.; Chan, F.K.L.; et al. Systematic review with meta-analysis: Review of donor features, procedures and outcomes in 168 clinical studies of fecal microbiota transplantation. Aliment. Pharmacol. Ther. 2019. [Google Scholar] [CrossRef] [PubMed]
- Landy, J.; Walker, A.W.; Li, J.V.; Al-Hassi, H.O.; Ronde, E.; English, N.R.; Mann, E.R.; Bernardo, D.; McLaughlin, S.D.; Parkhill, J.; et al. Variable alterations of the microbiota, without metabolic or immunological change, following fecal microbiota transplantation in patients with chronic pouchitis. Sci. Rep. 2015, 5, 12955. [Google Scholar] [CrossRef] [PubMed]
- Kousgaard, S.J.; Michaelsen, T.Y.; Nielsen, H.L.; Kirk, K.F.; Brandt, J.; Albertsen, M.; Thorlacius-Ussing, O. Clinical results and microbiota changes after fecal microbiota transplantation for chronic pouchitis: A pilot study. Scand. J. Gastroenterol. 2020, 421–429. [Google Scholar] [CrossRef] [PubMed]
- Selvig, D.; Piceno, Y.; Terdiman, J.; Zydek, M.; Umetsu, S.E.; Balitzer, D.; Fadrosh, D.; Lynch, K.; Lamere, B.; Leith, T.; et al. Fecal Microbiota Transplantation in Pouchitis: Clinical, Endoscopic, Histologic, and Microbiota Results from a Pilot Study. Dig. Dis. Sci. 2019. [Google Scholar] [CrossRef]
- Theede, K.; Holck, S.; Ibsen, P.; Ladelund, S.; Nordgaard-Lassen, I.; Nielsen, A.M. Level of Fecal Calprotectin Correlates With Endoscopic and Histologic Inflammation and Identifies Patients With Mucosal Healing in Ulcerative Colitis. Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol. Assoc. 2015, 13, 1929–1936.e1921. [Google Scholar] [CrossRef]
- Fang, S.; Kraft, C.S.; Dhere, T.; Srinivasan, J.; Begley, B.; Weinstein, D.; Shaffer, V.O. Successful treatment of chronic Pouchitis utilizing fecal microbiota transplantation (FMT): A case report. Int. J. Colorectal Dis. 2016, 31, 1093–1094. [Google Scholar] [CrossRef]
- Lan, N.; Ashburn, J.; Shen, B. Fecal microbiota transplantation for Clostridium difficile infection in patients with ileal pouches. Gastroenterol. Rep. 2017, 5, 200–207. [Google Scholar] [CrossRef]
- Guo, X.Y.; Liu, X.J.; Hao, J.Y. Gut Microbiota in Ulcerative Colitis: Insights on Pathogenesis and Treatment. J. Dig. Dis 2020. [Google Scholar] [CrossRef]
- Costello, S.P.; Hughes, P.A.; Waters, O.; Bryant, R.V.; Vincent, A.D.; Blatchford, P.; Katsikeros, R.; Makanyanga, J.; Campaniello, M.A.; Mavrangelos, C.; et al. Effect of Fecal Microbiota Transplantation on 8-Week Remission in Patients With Ulcerative Colitis: A Randomized Clinical Trial. JAMA 2019, 321, 156–164. [Google Scholar] [CrossRef]
- Moayyedi, P.; Surette, M.G.; Kim, P.T.; Libertucci, J.; Wolfe, M.; Onischi, C.; Armstrong, D.; Marshall, J.K.; Kassam, Z.; Reinisch, W.; et al. Fecal Microbiota Transplantation Induces Remission in Patients With Active Ulcerative Colitis in a Randomized Controlled Trial. Gastroenterology 2015, 149, 102–109. [Google Scholar] [CrossRef]
- Lopetuso, L.R.; Ianiro, G.; Allegretti, J.R.; Bibbò, S.; Gasbarrini, A.; Scaldaferri, F.; Cammarota, G. Fecal transplantation for ulcerative colitis: Current evidence and future applications. Expert Opin. Biol. Ther. 2020, 20, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Costello, S.P.; Soo, W.; Bryant, R.V.; Jairath, V.; Hart, A.L.; Andrews, J.M. Systematic review with meta-analysis: Fecal microbiota transplantation for the induction of remission for active ulcerative colitis. Aliment. Pharmacol. Ther. 2017, 46, 213–224. [Google Scholar] [CrossRef] [PubMed]
- Wilson, B.C.; Vatanen, T.; Cutfield, W.S.; O′Sullivan, J.M. The Super-Donor Phenomenon in Fecal Microbiota Transplantation. Front. Cell. Infect. Microbiol. 2019, 9, 2. [Google Scholar] [CrossRef] [PubMed]
- Staley, C.; Kaiser, T.; Vaughn, B.P.; Graiziger, C.T.; Hamilton, M.J.; Rehman, T.U.; Song, K.; Khoruts, A.; Sadowsky, M.J. Predicting recurrence of Clostridium difficile infection following encapsulated fecal microbiota transplantation. Microbiome 2018, 6, 166. [Google Scholar] [CrossRef]
- Sandborn, W.J.; Tremaine, W.J.; Batts, K.P.; Pemberton, J.H.; Phillips, S.F. Pouchitis after ileal pouch-anal anastomosis: A Pouchitis Disease Activity Index. Mayo Clin. Proc. 1994, 69, 409–415. [Google Scholar] [CrossRef]
- El-Nachef, N.; Piceno, Y.M.; Kassam, Z.; Zydek, M.; Ablaza, A.J.; Leith, T.; Ma, A.; Somsouk, M.; Terdiman, J.P.; Lynch, S. Fecal microbiota transplantation is safe and effective in chronic pouchitis patients. Gastroenterology 2017, 152, S1009. [Google Scholar] [CrossRef]
- Baxter, M.; Colville, A. Adverse events in fecal microbiota transplant: A review of the literature. J. Hosp. Infect. 2016, 92, 117–127. [Google Scholar] [CrossRef]
- Perler, B.K.; Chen, B.; Phelps, E.; Allegretti, J.R.; Fischer, M.; Ganapini, V.; Krajiceck, E.; Kumar, V.; Marcus, J.; Nativ, L.; et al. Long-Term Efficacy and Safety of Fecal Microbiota Transplantation for Treatment of Recurrent Clostridioides difficile Infection. J. Clin. Gastroenterol. 2020. [Google Scholar] [CrossRef]
- Cammarota, G.; Ianiro, G.; Tilg, H.; Rajilic-Stojanovic, M.; Kump, P.; Satokari, R.; Sokol, H.; Arkkila, P.; Pintus, C.; Hart, A.; et al. European consensus conference on fecal microbiota transplantation in clinical practice. Gut 2017, 66, 569–580. [Google Scholar] [CrossRef]
- FDA. Important Safety Alert Regarding Use of Fecal Microbiota for Transplantation and Risk of Serious Adverse Reactions Due to Transmission of Multi-Drug Resistant Organisms. Available online: https://www.fda.gov/vaccines-blood-biologics/safety-availability-biologics/important-safety-alert-regarding-use-fecal-microbiota-transplantation-and-risk-serious-adverse (accessed on 13 June 2019).
- Lee, C.H.; Chai, J.; Hammond, K.; Jeon, S.R.; Patel, Y.; Goldeh, C.; Kim, P. Long-term durability and safety of fecal microbiota transplantation for recurrent or refractory Clostridioides difficile infection with or without antibiotic exposure. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 2019, 38, 1731–1735. [Google Scholar] [CrossRef]
- Rossen, N.G.; Fuentes, S.; van der Spek, M.J.; Tijssen, J.G.; Hartman, J.H.; Duflou, A.; Lowenberg, M.; van den Brink, G.R.; Mathus-Vliegen, E.M.; de Vos, W.M.; et al. Findings From a Randomized Controlled Trial of Fecal Transplantation for Patients With Ulcerative Colitis. Gastroenterology 2015, 149, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Quraishi, M.N.; Widlak, M.; Bhala, N.; Moore, D.; Price, M.; Sharma, N.; Iqbal, T.H. Systematic review with meta-analysis: The efficacy of fecal microbiota transplantation for the treatment of recurrent and refractory Clostridium difficile infection. Aliment. Pharmacol. Ther. 2017, 46, 479–493. [Google Scholar] [CrossRef] [PubMed]
- Ng, S.C.; Kamm, M.A.; Yeoh, Y.K.; Chan, P.K.S.; Zuo, T.; Tang, W.; Sood, A.; Andoh, A.; Ohmiya, N.; Zhou, Y.; et al. Scientific frontiers in fecal microbiota transplantation: Joint document of Asia-Pacific Association of Gastroenterology (APAGE) and Asia-Pacific Society for Digestive Endoscopy (APSDE). Gut 2020, 69, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Fuentes, S.; van Nood, E.; Tims, S.; Heikamp-de Jong, I.; ter Braak, C.J.; Keller, J.J.; Zoetendal, E.G.; de Vos, W.M. Reset of a critically disturbed microbial ecosystem: Fecal transplant in recurrent Clostridium difficile infection. ISME J. 2014, 8, 1621–1633. [Google Scholar] [CrossRef] [PubMed]
- Zuo, T.; Wong, S.H.; Lam, K.; Lui, R.; Cheung, K.; Tang, W.; Ching, J.Y.L.; Chan, P.K.S.; Chan, M.C.W.; Wu, J.C.Y.; et al. Bacteriophage transfer during fecal microbiota transplantation in Clostridium difficile infection is associated with treatment outcome. Gut 2018, 67, 634–643. [Google Scholar] [CrossRef]
- Zuo, T.; Wong, S.H.; Cheung, C.P.; Lam, K.; Lui, R.; Cheung, K.; Zhang, F.; Tang, W.; Ching, J.Y.L.; Wu, J.C.Y.; et al. Gut fungal dysbiosis correlates with reduced efficacy of fecal microbiota transplantation in Clostridium difficile infection. Nat. Commun. 2018, 9, 3663. [Google Scholar] [CrossRef]
- Lee, S.T.M.; Kahn, S.A.; Delmont, T.O.; Shaiber, A.; Esen, O.C.; Hubert, N.A.; Morrison, H.G.; Antonopoulos, D.A.; Rubin, D.T.; Eren, A.M. Tracking microbial colonization in fecal microbiota transplantation experiments via genome-resolved metagenomics. Microbiome 2017, 5, 50. [Google Scholar] [CrossRef]
- Paramsothy, S.; Nielsen, S.; Kamm, M.A.; Deshpande, N.P.; Faith, J.J.; Clemente, J.C.; Paramsothy, R.; Walsh, A.J.; van den Bogaerde, J.; Samuel, D.; et al. Specific Bacteria and Metabolites Associated With Response to Fecal Microbiota Transplantation in Patients With Ulcerative Colitis. Gastroenterology 2019, 156, 1440–1454. [Google Scholar] [CrossRef]
- El-Salhy, M.; Hatlebakk, J.G.; Gilja, O.H.; Brathen Kristoffersen, A.; Hausken, T. Efficacy of fecal microbiota transplantation for patients with irritable bowel syndrome in a randomised, double-blind, placebo-controlled study. Gut 2019. [Google Scholar] [CrossRef]
- Fuentes, S.; Rossen, N.G.; van der Spek, M.J.; Hartman, J.H.; Huuskonen, L.; Korpela, K.; Salojarvi, J.; Aalvink, S.; de Vos, W.M.; D′Haens, G.R.; et al. Microbial shifts and signatures of long-term remission in ulcerative colitis after fecal microbiota transplantation. ISME J. 2017, 11, 1877–1889. [Google Scholar] [CrossRef]
- Vrieze, A.; Van Nood, E.; Holleman, F.; Salojarvi, J.; Kootte, R.S.; Bartelsman, J.F.; Dallinga-Thie, G.M.; Ackermans, M.T.; Serlie, M.J.; Oozeer, R.; et al. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology 2012, 143, 913–916. [Google Scholar] [CrossRef] [PubMed]
- Kelly, C.R.; Kahn, S.; Kashyap, P.; Laine, L.; Rubin, D.; Atreja, A.; Moore, T.; Wu, G. Update on Fecal Microbiota Transplantation 2015: Indications, Methodologies, Mechanisms, and Outlook. Gastroenterology 2015, 149, 223–237. [Google Scholar] [CrossRef]
- Barnes, D.; Ng, K.; Smits, S.; Sonnenburg, J.; Kassam, Z.; Park, K.T. Competitively Selected Donor Fecal Microbiota Transplantation: Butyrate Concentration and Diversity as Measures of Donor Quality. J. Pediatr. Gastroenterol. Nutr. 2018, 67, 185–187. [Google Scholar] [CrossRef] [PubMed]
- Ramai, D.; Zakhia, K.; Ofosu, A.; Ofori, E.; Reddy, M. Fecal microbiota transplantation: Donor relation, fresh or frozen, delivery methods, cost-effectiveness. Ann. Gastroenterol. 2019, 32, 30–38. [Google Scholar] [CrossRef]
- Kao, D.; Roach, B.; Silva, M.; Beck, P.; Rioux, K.; Kaplan, G.G.; Chang, H.J.; Coward, S.; Goodman, K.J.; Xu, H.; et al. Effect of Oral Capsule- vs Colonoscopy-Delivered Fecal Microbiota Transplantation on Recurrent Clostridium difficile Infection: A Randomized Clinical Trial. JAMA 2017, 318, 1985–1993. [Google Scholar] [CrossRef] [PubMed]
- Cold, F.; Browne, P.D.; Günther, S.; Halkjaer, S.I.; Petersen, A.M.; Al-Gibouri, Z.; Hansen, L.H.; Christensen, A.H. Multidonor FMT capsules improve symptoms and decrease fecal calprotectin in ulcerative colitis patients while treated—An open-label pilot study. Scand. J. Gastroenterol. 2019, 54, 289–296. [Google Scholar] [CrossRef]
- Terveer, E.M.; van Beurden, Y.H.; Goorhuis, A.; Seegers, J.; Bauer, M.P.; van Nood, E.; Dijkgraaf, M.G.W.; Mulder, C.J.J.; Vandenbroucke-Grauls, C.; Verspaget, H.W.; et al. How to: Establish and run a stool bank. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2017, 23, 924–930. [Google Scholar] [CrossRef] [PubMed]
- Cammarota, G.; Ianiro, G.; Kelly, C.R.; Mullish, B.H.; Allegretti, J.R.; Kassam, Z.; Putignani, L.; Fischer, M.; Keller, J.J.; Costello, S.P.; et al. International consensus conference on stool banking for fecal microbiota transplantation in clinical practice. Gut 2019, 68, 2111–2121. [Google Scholar] [CrossRef]
- Barnes, E.L.; Herfarth, H.H.; Sandler, R.S.; Chen, W.; Jaeger, E.; Nguyen, V.M.; Robb, A.R.; Kappelman, M.D.; Martin, C.F.; Long, M.D. Pouch-Related Symptoms and Quality of Life in Patients with Ileal Pouch-Anal Anastomosis. Inflamm. Bowel Dis. 2017, 23, 1218–1224. [Google Scholar] [CrossRef]
| Total number of studies, n | 9 |
| Total patient population, n | 65 |
| Mean days of FMT treatment, days (range) | 4.8 (1–14) |
| Mean delivered amount of stool by FMT, grams (range) (n = 51) | 111.8 (11–525) |
| Mean follow-up, days (range) (n = 65) | 87.6 (28–365) |
| Male/Female patients, n (n = 51) | 22/29 |
| Mean age of patients, years (range) (n = 51) | 43.8 (22–77) |
| Time since restorative proctocolectomy, mean years (range) (n = 50) | 10.3 (1–33) |
| Single/Multi donor FMT, n (n = 65) | 56/9 |
| Related/Unrelated donor, n (n = 65) | 12/53 |
| Upper/Lower administration/Both, n (n = 51) | 13/32/6 |
| Study type. Patients in RCT/Patients in non-RCT, n (n = 65) | 6/59 |
| Author and Year | Study Type | Patient Population | Sample Size | FMT Treatment | Route | Dosage | Clinical Response (Reduction in PDAI ≥3) | Clinical Remission (Reduction in PDAI ≥3 and Total of <7) | Endoscopic Outcomes | Histologic Outcomes | Adverse Events | Follow-Up |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fang et al., 2016 | Case report | Chronic antibiotic resistant pouchitis | 1 | Single FMT | Sigmoidoscopy (delivered 40 cm into the afferent limb and pouch body) | Stool mixed with saline and diluted to 250 mL | 1/1 after 3 months (cPDAI decreased from 6 at baseline to 0) | 1/1 after 3 months (cPDAI decreased from 6 at baseline to 0) | NA | NA | No reported adverse events. | 3 months |
| Herfarth et al., 2019 | RCT with open-label follow-up | Chronic antibiotic dependent pouchitis >4 weeks. mPDAI ≥5 | 6 (FMT (4) Placebo (2)). 5 received open-label FMT afterwards | Single endoscopic FMT followed by daily oral encapsulated FMT for 2 weeks | Sigmoidoscopy and oral capsules | eFMT (2 × 30 mL, total of 24 g donor stool) and 6 capsules daily consisting of 4.2 g donor stool | 1/6 (Four patients receiving primary FMT and two patients receiving open-label FMT included) | 1/6 (clinical PDAI 1 and no need for antibiotics) | NA | NA | No FMT related safety events were observed. | 16 weeks |
| Kousgaard et al., 2020 | Cohort (open-label pilot study) | Chronic pouchitis (≥3 episodes of pouchitis within the last year) | 9 | 14 days of daily self-administered FMT | Enema | 20 g fecal material diluted in 100 mL saline | 3/9 after four weeks | 3/9 after four weeks | Mean ePDAI of 3.2 at baseline decreased to 2.2 after four weeks | Mean hPDAI of 1.7 decreased to 1.0 after four weeks | 7/9 patients reported adverse events while treated. Abdominal pain (5), uncomfortable (2), nausea (2), fever (2), bloating (1), dizziness (1), and fatigue (1). | 6 months |
| Landy et al., 2015 | Cohort (pilot study) | Chronic pouchitis with current PDAI ≥ 7 | 8 | Single FMT | Nasogastric | 30 mL of fecal-saline solution followed by 50 mL saline | 2/8 after 4 weeks | 0/8 after 4 weeks | Mean ePDAI of 5 at both baseline and after 4 weeks | Mean hPDAI of 3 at baseline decreased to 2 after four weeks | Nausea (3), bloating (2), vomiting (1), fever (1). All transient (<24 h). | 4 weeks |
| Nishida et al., 2019 | Case series | Chronic pouchitis with current PDAI ≥7 | 3 | Single FMT | Colonoscopy | 150–200 g donor stool mixed with 350–500 mL sterile saline | 1/3 after 8 weeks | 0/3 after 8 weeks | NA | NA | No reported adverse events. | 8 weeks |
| Schmid et al., 2017 | Case report | A severe flare of pouchitis in a patient diagnosed with pouchitis one year earlier | 1 | A total of three FMTs at baseline, after 5 and 9 weeks | Pouchoscopy | 250 mL fecal-saline suspension | 0/1 after 9 weeks | 0/1 after 9 weeks | NA | NA | No reported adverse events. | 9 weeks |
| Selvig et al., 2020 | Cohort (prospective open-label pilot study) | Chronic pouchitis. Prior endoscopic evaluation confirming inflammation and over 4 weeks of symptoms | 18 (7 of the 18 patients pre-treated with Rifaximin) | 1 or 2 FMTs. Single or optional re-treatment | Pouchoscopy. Delivered to the most proximal point of insertion (proximal pouch or neo-terminal ileum) | 250/500 mL in total derived from 25/50 g stool | 1/11 after 4 weeks. Only 11 underwent pouchoscopy at 4 weeks | 1/11 after 4 weeks | Mean ePDAI of 3.38 at baseline decreased to 3.36 after four weeks | Mean hPDAI of 1.05 at baseline increased to 1.36 after four weeks | One patient admitted to hospital 8 days after FMT because of abdominal pain considered not related to FMT. One patient diagnosed with Crohn’s disease at pouchoscopy after four weeks, which was suspected in advance. Minor self-limiting adverse events. Discomfort (4), flatulence (4), bloating or cramping (3), fatigue (3), and nausea (2). | 12 months |
| Stallmach et al., 2016 | Prospective open-label pilot study | Chronic antibiotics resistant pouchitis (three or more cycles of antibiotics) | 5 | 1–7 FMTs | FMT to the jejunum with intervals of 3–4 weeks | 275 mL fecal saline suspension derived from 75 g stool | 5/5 after last FMT. | 4/5 after last FMT | Mean ePDAI of 3.8 at baseline decreased to 1.2 after last FMT | Mean hPDAI of 3 at baseline decreased to 1.2 after last FMT | Mild transient fever and CRP increase in one patient. | 3 months. One patient followed for 12 months |
| Steube et al., 2017 | Prospective open-label pilot study | Chronic antibiotics resistant pouchitis | 14 | 2–4 FMTs | Nasojejunal or capsule application delivered every 4 weeks according to treatment outcome | NA | 7/14. PDAI scores however not described. Assessed through F-Calprotectin. | NA | NA | NA | No reported adverse events. | 8 weeks |
| Author and Year | Donor(s) | Fresh/Frozen | FMT Preparation | Concomitant Treatment | Pre-Treatment with Antibiotics | Single/Multi-donor | Bowel Cleansing |
|---|---|---|---|---|---|---|---|
| Fang et al., 2016 | Unrelated donor | Fresh | Stool mixed with sterile saline and diluted to 250 mL | The patient was off his usual antibiotics during the entire follow-up period but continued antidiarrheal medication. | Antibiotics stopped 48 h before FMT | Single | No |
| Herfarth et al., 2019 | Unrelated donor with high butyrate production | Frozen | Stool bank provided FMT for endoscopic administration, FMT capsules and matching placebos | NA | Antibiotics stopped 24 h before FMT | Single | NA |
| Kousgaard et al., 2020 | Unrelated | Frozen | 20 g stool mixed with 100 mL sterile water, blended and filtered, 10% glycerol | Concurrent therapies were permitted if stable with exception of antibiotics, probiotics, and biologic treatment. | Antibiotics stopped 7 days before FMT | Multi-donor (5 donors) | No |
| Landy et al., 2015 | Relative/partner (6) or anonymous (2) | Fresh (less than 6 h prior to FMT) | 30 g of stool was homogenized with a household blender in 50 mL of 0.9% saline and filtered through sterile gauze to produce a fecal-saline solution | Night before the procedure the recipient was treated with a proton pump inhibitor (Omeprazole 20 mg). | NA | Single | NA |
| Nishida et al., 2019 | Second degree relatives | Fresh (less than 4 h prior to FMT) | 150–200 g donor stool mixed with 350–500 mL sterile saline and filtered through gaze | NA | NA | Single | Polyethylene glycol solution |
| Schmid et al., 2017 | Patient’s son | Fresh (less than 6 h prior to FMT) | A fresh stool sample diluted with 500 mL saline and filtered through gaze | NA | NA | Single | Enemas |
| Selvig et al., 2020 | Unrelated | Frozen | 25 g of stool mixed with saline to a 250 mL fecal suspension | Accepted with antibiotics as exception. Three patients continued biologic treatment. | 7/18 patients received 5 days of 550 mg Rifaximin beginning 8 days prior to treatment | Single (from 11 different donors) | Magnesium citrate a day before FMT and phosphate enema at day of FMT |
| Stallmach et al., 2016 | Unrelated | Fresh (first FMT) and frozen | 150 g stool mixed with 400 mL saline. Then filtered and separated in two. The first immediately delivered to the patient and the second stored at −80 °C | NA | NA | Single (from 2 different donors) | No |
| Steube et al., 2017 | Unrelated | NA | NA | NA | NA | Single (from 3 different donors) | NA |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cold, F.; Kousgaard, S.J.; Halkjaer, S.I.; Petersen, A.M.; Nielsen, H.L.; Thorlacius-Ussing, O.; Hansen, L.H. Fecal Microbiota Transplantation in the Treatment of Chronic Pouchitis: A Systematic Review. Microorganisms 2020, 8, 1433. https://doi.org/10.3390/microorganisms8091433
Cold F, Kousgaard SJ, Halkjaer SI, Petersen AM, Nielsen HL, Thorlacius-Ussing O, Hansen LH. Fecal Microbiota Transplantation in the Treatment of Chronic Pouchitis: A Systematic Review. Microorganisms. 2020; 8(9):1433. https://doi.org/10.3390/microorganisms8091433
Chicago/Turabian StyleCold, Frederik, Sabrina Just Kousgaard, Sofie Ingdam Halkjaer, Andreas Munk Petersen, Hans Linde Nielsen, Ole Thorlacius-Ussing, and Lars Hestbjerg Hansen. 2020. "Fecal Microbiota Transplantation in the Treatment of Chronic Pouchitis: A Systematic Review" Microorganisms 8, no. 9: 1433. https://doi.org/10.3390/microorganisms8091433
APA StyleCold, F., Kousgaard, S. J., Halkjaer, S. I., Petersen, A. M., Nielsen, H. L., Thorlacius-Ussing, O., & Hansen, L. H. (2020). Fecal Microbiota Transplantation in the Treatment of Chronic Pouchitis: A Systematic Review. Microorganisms, 8(9), 1433. https://doi.org/10.3390/microorganisms8091433





