Low Albumin Levels Are Associated with Poorer Outcomes in a Case Series of COVID-19 Patients in Spain: A Retrospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Statistical Analysis
2.4. Study Approval
3. Results
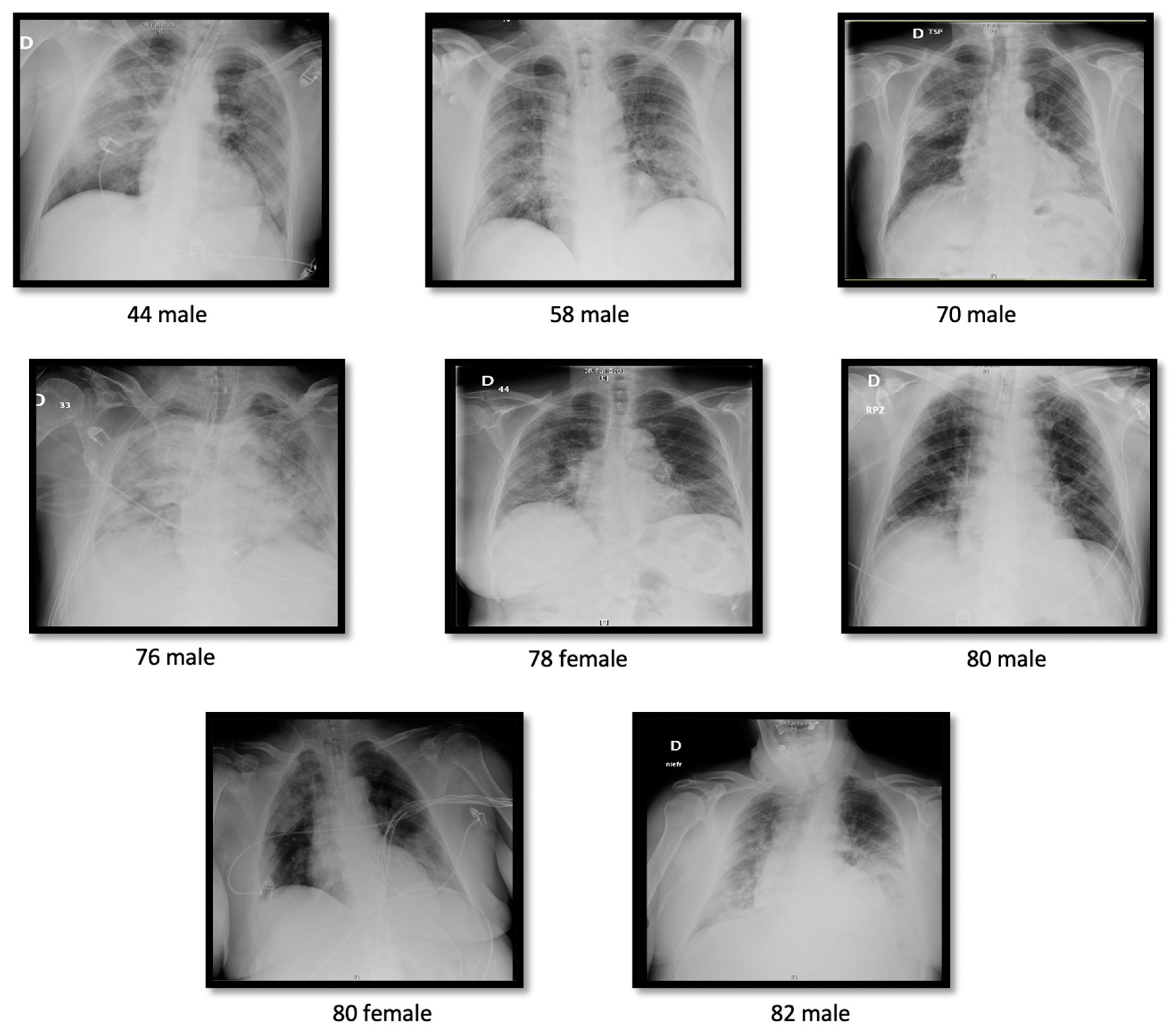
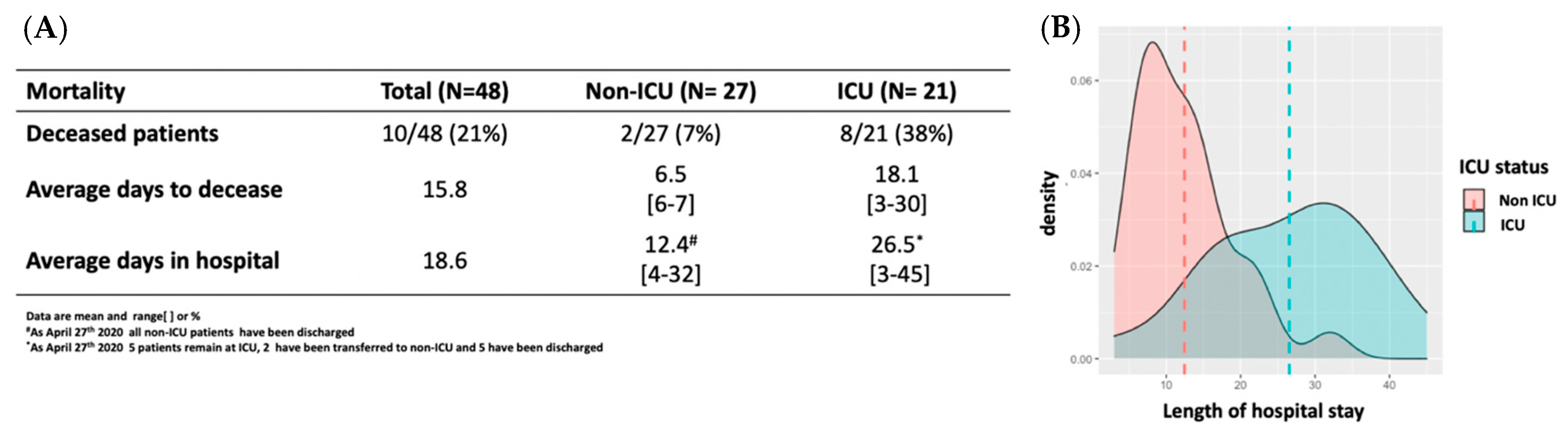
3.1. Clinical Features
3.2. Laboratory Findings
3.2.1. Hematologic Measures
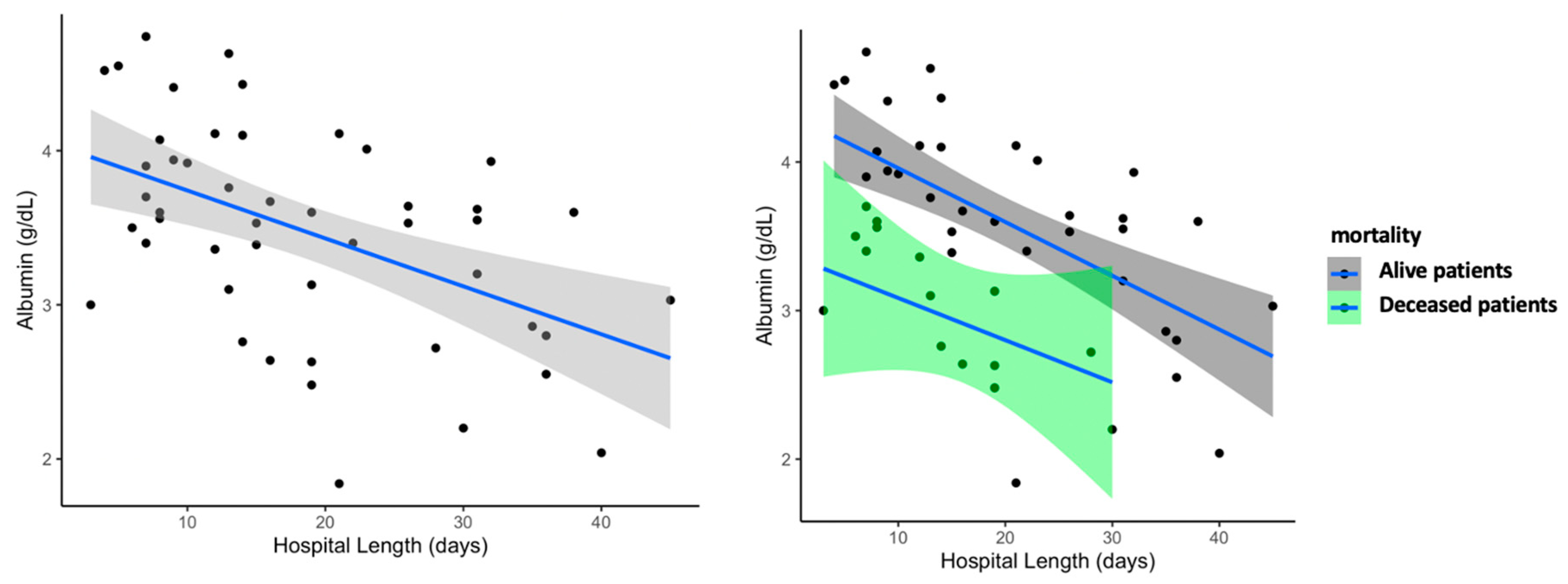
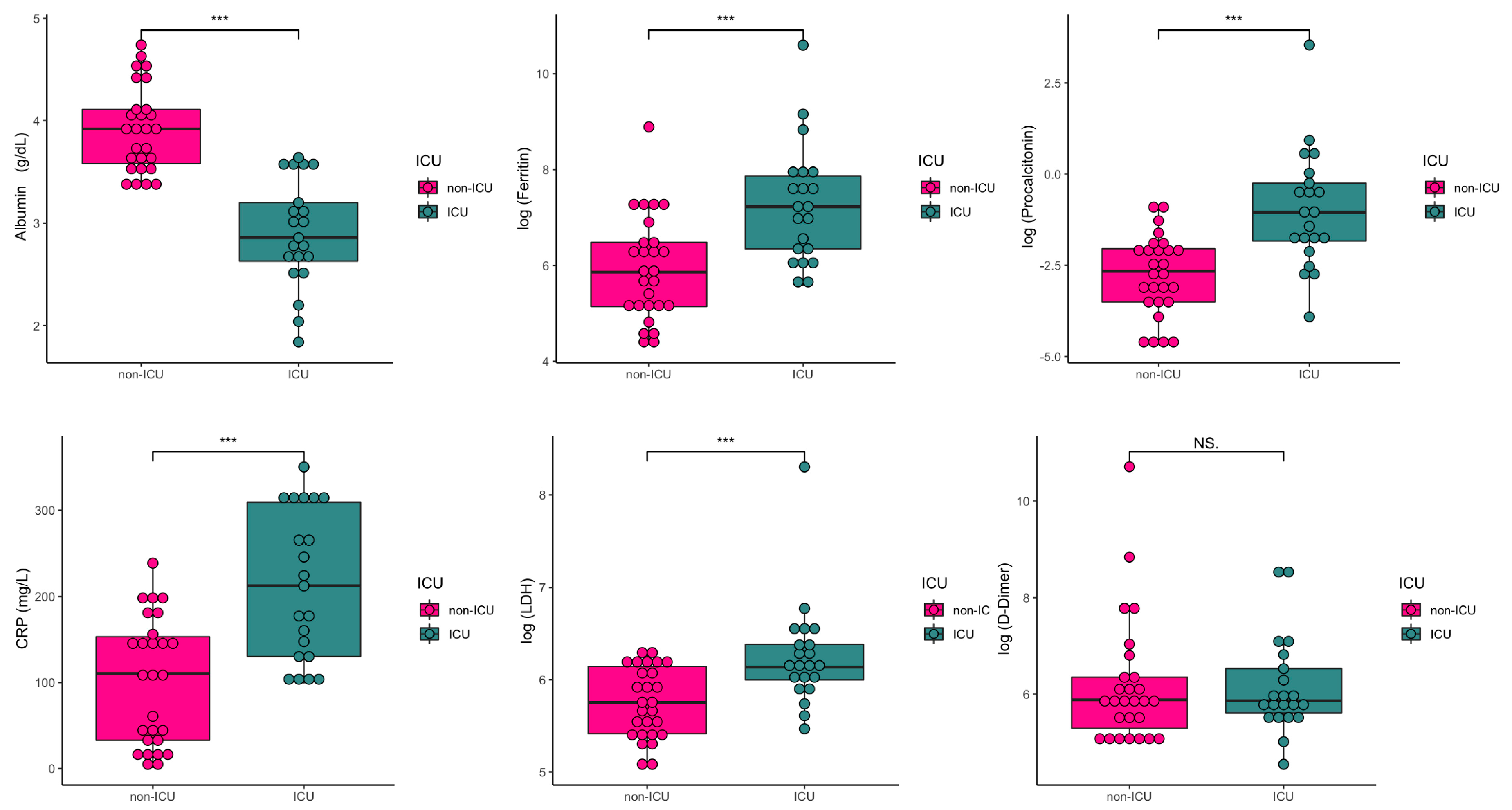
3.2.2. Coagulation Function, Biochemical and Inflammation Measures
4. Discussion
5. Conclusions
Supplementary Materials
Disclaimer
Author Contributions
Funding
Conflicts of Interest
References
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.; Xu, H.; Yang, M.; Zeng, Y.; Chen, H.; Liu, R.; Li, Q.; Zhang, N.; Wang, D. Epidemiological characteristics and clinical features of 32 critical and 67 noncritical cases of COVID-19 in Chengdu. J. Clin. Virol. 2020, 127, 104366. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Liu, W.; Zhao, J.; Lu, Y.; Yu, C.; Hu, S.; Shen, N.; Sun, Z.; Wang, X.; Liu, W.; et al. Clinical characteristics of 80 hospitalized frontline medical workers infected with COVID-19 in Wuhan, China. J. Hosp. Infect. 2020, 105, 399–403. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Wu, D.; Guo, W.; Cao, Y.; Huang, D.; Wang, H.; Wang, T.; Zhang, X.; Chen, H.; Yu, H.; et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J. Clin. Investig. 2020, 130, 2620–2629. [Google Scholar] [CrossRef] [Green Version]
- Pedersen, S.F.; Ho, Y.-C. SARS-CoV-2: A storm is raging. J. Clin. Investig. 2020, 130, 2202–2205. [Google Scholar] [CrossRef]
- Lagunas-Rangel, F.A.; Chávez-Valencia, V. High IL-6/IFN-γ ratio could be associated with severe disease in COVID-19 patients. J. Med. Virol. 2020, 10. [Google Scholar] [CrossRef]
- Chau, V.Q.; Oliveros, E.; Mahmood, K.; Singhvi, A.; Lala, A.; Moss, N.; Gidwani, U.; Mancini, D.M.; Pinney, S.P.; Parikh, A. The Imperfect Cytokine Storm. JACC Case Rep. 2020. [Google Scholar] [CrossRef]
- Wu, D.; Yang, X.O. TH17 responses in cytokine storm of COVID-19: An emerging target of JAK2 inhibitor Fedratinib. J. Microbiol. Immunol. Infect. 2020, 53, 368–370. [Google Scholar] [CrossRef]
- Henderson, L.A.; Canna, S.W.; Schulert, G.S.; Volpi, S.; Lee, P.Y.; Kernan, K.F.; Caricchio, R.; Mahmud, S.; Hazen, M.M.; Halyabar, O.; et al. On the Alert for Cytokine Storm: Immunopathology in COVID-19. Arthritis Rheumatol. 2020, 72, 1059–1063. [Google Scholar] [CrossRef] [Green Version]
- Channappanavar, R.; Perlman, S. Pathogenic human coronavirus infections: Causes and consequences of cytokine storm and immunopathology. Semin. Immunopathol. 2017, 39, 529–539. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zhao, B.; Qu, Y.; Chen, Y.; Xiong, J.; Feng, Y.; Men, D.; Huang, Q.; Liu, Y.; Yang, B.; et al. Detectable serum SARS-CoV-2 viral load (RNAaemia) is closely correlated with drastically elevated interleukin 6 (IL-6) level in critically ill COVID-19 patients. Clin. Infect. Dis. 2020, 6. [Google Scholar] [CrossRef]
- Limper, M.; De Kruif, M.; Duits, A.; Brandjes, D.; Van Gorp, E. The diagnostic role of Procalcitonin and other biomarkers in discriminating infectious from non-infectious fever. J. Infect. 2010, 60, 409–416. [Google Scholar] [CrossRef]
- World Health Organization. Coronavirus Disease (COVID-19) Technical Guidance: Laboratory Testing for 2019-nCoV in Humans. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technicalguidance/laboratory-guidance (accessed on 27 April 2020).
- Dowd, J.B.; Andriano, L.; Brazel, D.M.; Rotondi, V.; Block, P.; Ding, X.; Liu, Y.; Mills, M.C. Demographic science aids in understanding the spread and fatality rates of COVID-19. Proc. Natl. Acad. Sci. USA 2020, 117, 9696–9698. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lauren, A.; Alyson, J.; Walter, L.A. Sex- and Gender-specific Observations and Implications for COVID-19. West. J. Emerg. Med. 2020, 21, 507–509. [Google Scholar] [CrossRef] [Green Version]
- Singh, A.K.; Gupta, R.; Ghosh, A.; Misra, A. Diabetes in COVID-19: Prevalence, pathophysiology, prognosis and practical considerations. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 303–310. [Google Scholar] [CrossRef]
- Zhao, Q.; Meng, M.; Kumar, R.; Wu, Y.; Huang, J.; Lian, N.; Deng, Y.; Lin, S. The impact of COPD and smoking history on the severity of COVID-19: A systemic review and meta-analysis. J. Med. Virol. 2020, 10. [Google Scholar] [CrossRef] [Green Version]
- Grasselli, G.; Zangrillo, A.; Zanella, A.; Antonelli, M.; Cabrini, L.; Castelli, A.; Cereda, D.; Coluccello, A.; Foti, G.; Fumagalli, R.; et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA 2020, 323, 1574. [Google Scholar] [CrossRef] [Green Version]
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, K.W.; Barnaby, D.P.; Becker, L.B.; Chelico, J.D.; Cohen, S.L.; et al. Presenting Characteristics, Comorbidities, and Outcomes among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA 2020, 323, 2052. [Google Scholar] [CrossRef]
- Arentz, M.; Yim, E.; Klaff, L.; Lokhandwala, S.; Riedo, F.X.; Chong, M.; Lee, M. Characteristics and Outcomes of 21 Critically Ill Patients with COVID-19 in Washington State. JAMA 2020, 323, 1612. [Google Scholar] [CrossRef] [Green Version]
- Young, B.E.; Ong, S.W.X.; Kalimuddin, S.; Low, J.G.; Tan, S.Y.; Loh, J.; Ng, O.-T.; Marimuthu, K.; Ang, L.W.; Mak, T.M.; et al. Epidemiologic Features and Clinical Course of Patients Infected With SARS-CoV-2 in Singapore. JAMA. 2020, 323, 1488–1494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, C.; Chen, X.; Cai, Y.; Xia, J.; Zhou, X.; Xu, S.; Huang, H.; Zhang, L.; Zhou, X.; Du, C.; et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern. Med. 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jellinge, M.E.; Henriksen, D.P.; Hallas, P.; Brabrand, M. Hypoalbuminemia Is a Strong Predictor of 30-Day All-Cause Mortality in Acutely Admitted Medical Patients: A Prospective, Observational, Cohort Study. PLoS ONE 2014, 9, e105983. [Google Scholar] [CrossRef] [PubMed]
- Wi, Y.M.; Kim, J.M.; Peck, K. Serum albumin level as a predictor of intensive respiratory or vasopressor support in influenza A (H1N1) virus infection. Int. J. Clin. Pract. 2013, 68, 222–229. [Google Scholar] [CrossRef] [PubMed]
- Dirajlal-Fargo, S.; Kulkarni, M.; Bowman, E.; Shan, L.; Sattar, A.; Funderburg, N.T.; Mccomsey, G.A. Serum Albumin Is Associated with Higher Inflammation and Carotid Atherosclerosis in Treated Human Immunodeficiency Virus Infection. Open Forum Infect. Dis. 2018, 5, ofy291. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Cheng, A.; Kumar, R.; Fang, Y.; Chen, G.; Zhu, Y.; Lin, S. Hypoalbuminemia predicts the outcome of COVID-19 independent of age and co-morbidity. J. Med. Virol. 2020, 10. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Zhu, L.; Cai, J.; Lei, F.; Qin, J.-J.; Xie, J.; Liu, Y.-M.; Zhao, Y.-C.; Huang, X.; Lin, L.; et al. Association of Inpatient Use of Angiotensin-Converting Enzyme Inhibitors and Angiotensin II Receptor Blockers with Mortality Among Patients with Hypertension Hospitalized With COVID-19. Circ. Res. 2020, 126, 1671–1681. [Google Scholar] [CrossRef]
- Delanghe, J.R.; Speeckaert, M.M.; De Buyzere, M.L. COVID-19 infections are also affected by human ACE1 D/I polymorphism. Clin. Chem. Lab. Med. 2020, 58, 1125–1126. [Google Scholar] [CrossRef] [Green Version]
- Delanghe, J.R.; Speeckaert, M.M.; De Buyzere, M.L. The host’s angiotensin-converting enzyme polymorphism may explain epidemiological findings in COVID-19 infections. Clin. Chim. Acta 2020, 505, 192–193. [Google Scholar] [CrossRef]
| Clinical Characteristics | All (n = 48) | Non-ICU (n = 27) | ICU (n = 21) | p Value |
|---|---|---|---|---|
| At triage | ||||
| Age, yrs. | 65.98 (13.91) [33–88] | 66.30 (14.90) [33–88] | 65.57 (12.87) [44–82] | 0.856 |
| Males, n% | 32 (67%) | 18 (67%) | 14 (67%) | 1 |
| Fever, °C | 37.03 (0.94) [36–39] | 36.84 (0.88) [36–39] | 37.28 (0.98) [36–39] | 0.147 |
| Systolic Pressure, mmHg | 129.6 (18.9) [90–180] | 130.7 (16.6) [90–180] | 128.1(21.9) [90–180] | 0.642 |
| Diastolic Pressure, mmHg | 73.3 (11.7) [50–111] | 75.9 (12.1) [50–110] | 70.03 (10.44) [52–92] | 0.058 |
| Heart Rate, bpm | 85.6 (14.59) [58–120] | 86.9(17.4) [58–120] | 83.8 (11.2) [58–106] | 0.712 |
| Sp02,% | 89.31(10.64) [38–99] | 93.44(6.63) [66–99] | 84(12.51) [38–99] | <0.001 * |
| Symptoms Reported n% | ||||
| Asthenia | 10/46(21%) | 6/25 (22%) | 4/21 (19.1%) | 1 |
| Dyspnea | 35/46 (76%) | 16/26 (61%) | 19/20 (95) | 0.022 * |
| Vomiting | 6/47 (13%) | 4/25 (16%) | 2/21 (9%) | 0.870 |
| Diarrhea | 16/38 (42%) | 12/25 (44%) | 4/13 (31%) | 0.070 |
| Coughing | 39/46 (85%) | 20/27 (74%) | 19/20 (95%) | 0.225 |
| Fever | 48/48 (100%) | 27/27 (100%) | 21/21 (100%) | 1 |
| ARDS | 20/46 (44%) | 0/27 (0%) | 21/21 (100%) | <0.001 * |
| Pneumonia | 44/47 (94%) | 24/27 (89%) | 20/20 (100%) | 0.078 |
| Bilateral pneumonia | 44/47 (94%) | 21/27 (77%) | 20/20 (100%) | NA |
| Comorbidities n% | ||||
| Hypertension | 33/47 (70%) | 22/27 (82%) | 11/20 (55%) | 0.101 |
| Dyslipidemia | 29/47 (62%) | 16/27 (60%) | 13/20 (65%) | 1 |
| Type 2 Diabetes | 11/45 (24%) | 9/27 (33%) | 5/20 (25%) | 0.286 |
| Cardiovascular disease | 14/47 (30%) | 7/27 (26%) | 7/20 (35%) | 0.726 |
| Ictus | 3/46 (6%) | 2/27 (7%) | 1/20 (5%) | 0.662 |
| Cancer or another malignancy | 10/47 (21%) | 4/27 (15%) | 6/20 (30%) | 0.640 |
| COPD | 5/47 (11%) | 4/27 (15%) | 1/20 (5%) | 0.544 |
| VIH | 1/46 (2%) | 0/26 (0) | 1/20 (5%) | 0.894 |
| Renal chronic disease | 8/46 (17%) | 4/27 (15%) | 4/19 (21%) | 0.877 |
| Other, n% | 26/47 (55%) | 13/27 (52%) | 12/20 (60%) | 0.921 |
| Smoking | 10/47 (21%) | 6/26 (22%) | 4/20 (19%) | 0.934 |
| Normal Range | All (n = 48) | Non-ICU (n = 27) | ICU (n = 21) | p Value | p Value # | p Value ## | p Value $ | |
|---|---|---|---|---|---|---|---|---|
| Leukocytes, 109/L | 4.00–11.0 | 7.69 (3.40) [2.51–18.4] | 7.48 (3.28) [3.76–18.4] | 7.95 (3.61) [2.51–16.7] | 0.582 | 0.987 | 0.897 | 0.345 |
| Neutrophil count, 109/L | 1.80–7.50 | 6.11 (3.34) [1.66–16] | 5.62 (3.12) [2.17–16] | 6.76 (3.58) [1.66–15.7] | 0.199 | 0.365 | 0.641 | 0.591 |
| Lymphocyte count, 109/L | 1.00–4.5 | 1.03 (0.55) [0.29–2.82] | 1.23 (0.57) [0.45–2.82] | 0.77 (0.40) [0.29–2.03] | 0.002 * | <0.001 * | 0.045 | 0.158 |
| Monocyte count, 109/L | 0.00–1.0 | 0.50 (0.29) [0.12–1.56] | 0.58 (0.33) [0.12–1.56] | 0.40 (0.20) [0.12–0.88] | 0.029 * | 0.032 * | 0.040 | 0.055 |
| Red Blood cells, 1012/L | 4.50–5.8 | 4.45 (0.76) [2.35–6.8] | 4.51 (0.68) [3.02–6.18] | 4.37 (0.87) [2.35–6.8] | 0.454 | 0.798 | 0.848 | 0.661 |
| Hemoglobin, g/dL | 13.00–16.7 | 13.29 (1.80) [7.66–16.3] | 13.38 (1.70) [10.3–16.3] | 13.16(19.96) [7.66–15.7] | 0.795 | 0.730 | 0.640 | 0.277 |
| Hematocrit, % | 40.00–50.00 | 40.25(5.67) [22.5–50.3] | 40.57(5.42) [30.6–50.3] | 39.84(6.08) [22.5–50] | 0.827 | 0.735 | 0.633 | 0.287 |
| Mean Corpuscular Volume (MCV), fl | 80.00–99.00 | 91.04 (7.94) [60.8–102] | 90.16(7.91) [60.8–102] | 92.17 (8.04) [63.9–101] | 0.137 | 0.311 | 0.243 | 0.513 |
| Mean Corpuscular Hemoglobin (MCH), pg | 27.00–32.00 | 30.18 (2.91) [19.1–34.3] | 29.93(2.96) [19.1–34.3] | 30.49 (2.88) [20.3–33.7] | 0.266 | 0.404 | 0.353 | 0.612 |
| Red Blood Cell Distribution Width (RDW), % | 10.00–14.00 | 12.57 (1.41) [10.90–19.8] | 12.39(1.01) [10.9–15] | 12.192(1.80) [11.40–19.8] | 0.423 | 0.579 | 0.874 | 0.733 |
| Platelet Distribution width (PDW), % | 14.00–18.00 | 16.91 (1.13) [15–19.8] | 16.81(1.24) [15–19.8] | 16.99(0.97) [15.4–19.7] | 0.333 | 0.930 | 0.960 | 0.864 |
| Platelets, 109/L | 150.00–400.00 | 219.94 (96.04) [46.8–518] | 228.02(108.82) [46.8–518] | 209.56 (77.97) [81.7–429] | 0.678 | 0.741 | 0.814 | 0.909 |
| Mean Platelet Volume (MPV), fl | 7.50–11.00 | 8.03 (1.22) [5.78–11.1] | 7.92(1.25) [5.78–10.9] | 8.18 (1.19) [6.71–11.1] | 0.596 | 0.185 | 0.119 | 0.464 |
| Normal Range | All (n = 48) | Non-ICU (n = 27) | ICU (n = 21) | p Value | p Value # | p Value $ | |
|---|---|---|---|---|---|---|---|
| Prothrombin time, s | 8.5–15.0 | 13.70 (1.59) [11.4–20.2] | 13.20(1.12) [11.40–15.50] | 14.33(1.89) [11.9–20.2] | 0.038 * | 0.614 | 0.461 |
| Fibrinogen, mg/dL | 200–500 | 713.63 (160.50) [405–1185] | 686.44(151.77) [420–1118] | 748.57 (168.27) [405–1185] | 0.212 | 0.093 | 0.078 |
| D-Dimer, ng/mL & | 0.00–255 | 1745.08 (6495.60)/358 (262–609) & [94–44,808] | 2405.93(8583.03)/358 (201–2406) & [150–44,808] | 895.43(1427.10)/350 (272–895)& [94–5105] | 0.731 | 0.279 | 0.020 * |
| Log (D-Dimer) | 6.17(1.17) [4.5–10.7] | 6.18(1.32) [5.0–10.7] | 6.16(1.0) [4.5–8.5] | 0.967 | 0.412 | 0.121 | |
| Creatinine, mg/dL | 0.72–1.25 | 1.10 (0.83) [0.6–5.4] | 1.09(0.68) [0.64–3.82] | 1.11(1.01) [0.57–5.40] | 0.739 | 0.842 | 0.405 |
| Glomerular Filtration Rate, mL/min | 77.17(25.44) [11–125] | 76.15(25.99) [16–116] | 78.48(25.28) [11–125] | 0.830 | 0.852 | 0.883 | |
| Ferritin, ng/mL | 20–274 | 2074.37 (5903)/572 (279–1401) & [76.9–40,000] | 750.58(1374.38)/352(172–652)& [76.9–7245.9] | 3776.39(8603.70)/1373(571–2598)& [261.8–40,000] | <0.001 * | 0.054 | 0.084 |
| Log(Ferritin) | 6.51(1.32) [4.3–10.6] | 5.93(1.09) [4.3–8.8] | 7.26(1.24) [5.57–10.6] | <0.001 | <0.001 * | 0.008 * | |
| Total Bilirubin, mg/dL | 0.2–1.2 | 0.79 (0.45) [0.3–22] | 0.70(0.28) [0.34–1.43] | 0.91(0.58) [0.41–2.20] | 0.339 | 0.399 | 0.387 |
| Albumin, g/dL | 3.50–5.50 | 3.47 (0.69) [1.8–4.7] | 3.92(0.42) [3.36–4.74] | 2.90(0.52) [1.84–3.64] | <0.001 * | <0.001 * | <0.001 |
| Aspartate aminotransferase (AST), U/L | 5.0–34.0 | 44.50(27.66) [3–125] | 40.41(30.15) [3–118] | 49.76(23.77) [22–125] | 0.040 * | 0.062 | 0.369 |
| Alanine aminotransferase (ALT), U/L | 1.0–55.0 | 39.75(30.28) [9–121] | 40.67(35.23) [9–121] | 38.57(23.19) [14–94] | 0.323 | 0.367 | 0.665 |
| Phosphatase, U/L | 40–150 | 80.88(45.19) [25–250] | 74.96(27.59) [34–143] | 88.48(60.83) [25–250] | 0.909 | 0.890 | 0.311 |
| Gamma-glutamyl transferase (GGT), U/L | 12.0–64.0 | 79.60(80.77) [11–433] | 69.04(51.16) [13–186] | 93.19(106.99) [11–433] | 0.843 | 0.338 | 0.227 |
| Lactate dehydrogenase (LDH), U/L | 125–243 | 479.04(548.36) [156–4038] | 335.82(123.6) [156–545] | 663.19(789.6) [237–4038] | <0.001 * | 0.005 * | 0.113 |
| Creatine Kinase (CK), U/L | 30–200 | 181.79(298.45) [27–1909] | 202.89(375.21) [29–1909] | 154.67(157.89) [27–736] | 0.473 | 0.321 | 0.265 |
| Log(CK) | 4.64(0.95) [3.3–7.5] | 4.60(1.04) [3.37–7.55] | 4.69(0.84) [3.3–6.0] | 0.744 | 0.601 | 0.536 | |
| Triglycerides, mg/dL | 0–150 | 173.79 (74.46) [64–399] | 163.22(68.40) [64–388] | 187.38(81.26) [79–399] | 0.284 | 0.215 | 0.651 |
| Glucose, mg/dL | 70–110 | 131.23 (59.18) [80–431] | 131.78(65.38) [80–431] | 130.52(51.69) [89–337] | 0.868 | 0.601 | 0.347 |
| Urea, mg/dL | 15–50 | 47.46 (38.64) [14–193] | 51.04(40.51) [16–176] | 42.86(36.55) [14–193] | 0.442 | 0.423 | 0.045 * |
| Troponin I, ng/L | 0.00–34.0 | 210.76(1094.37) [1.9–7572.6] | 76.01(184.38) [1.90–723.1] | 384.00(1647.5) [1.9–7572.6] | 0.412 | 0.475 | 0.034 * |
| C reactive protein (CRP), mg/L | 0.0–5.0 | 150.43(96.62) [0.5–350.4] | 101.30(73.27) [0.5–238.9] | 213.59(86.68) [98.80–350.4] | <0.001 * | 0.011 * | 0.028 |
| Procalcitonin, ng/mL | 0.00–0.05 | 1.02(4.98) [0.01–34.7] | 0.10(0.11) [0.01–0.43] | 2.21(7.47) [0.02–34.66] | <0.001 * | <0.001 * | 0.016 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
de la Rica, R.; Borges, M.; Aranda, M.; del Castillo, A.; Socias, A.; Payeras, A.; Rialp, G.; Socias, L.; Masmiquel, L.; Gonzalez-Freire, M. Low Albumin Levels Are Associated with Poorer Outcomes in a Case Series of COVID-19 Patients in Spain: A Retrospective Cohort Study. Microorganisms 2020, 8, 1106. https://doi.org/10.3390/microorganisms8081106
de la Rica R, Borges M, Aranda M, del Castillo A, Socias A, Payeras A, Rialp G, Socias L, Masmiquel L, Gonzalez-Freire M. Low Albumin Levels Are Associated with Poorer Outcomes in a Case Series of COVID-19 Patients in Spain: A Retrospective Cohort Study. Microorganisms. 2020; 8(8):1106. https://doi.org/10.3390/microorganisms8081106
Chicago/Turabian Stylede la Rica, Roberto, Marcio Borges, Maria Aranda, Alberto del Castillo, Antonia Socias, Antoni Payeras, Gemma Rialp, Lorenzo Socias, Lluis Masmiquel, and Marta Gonzalez-Freire. 2020. "Low Albumin Levels Are Associated with Poorer Outcomes in a Case Series of COVID-19 Patients in Spain: A Retrospective Cohort Study" Microorganisms 8, no. 8: 1106. https://doi.org/10.3390/microorganisms8081106
APA Stylede la Rica, R., Borges, M., Aranda, M., del Castillo, A., Socias, A., Payeras, A., Rialp, G., Socias, L., Masmiquel, L., & Gonzalez-Freire, M. (2020). Low Albumin Levels Are Associated with Poorer Outcomes in a Case Series of COVID-19 Patients in Spain: A Retrospective Cohort Study. Microorganisms, 8(8), 1106. https://doi.org/10.3390/microorganisms8081106





