OXA-48 Carbapenemase in Klebsiella pneumoniae Sequence Type 307 in Ecuador
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient History
2.2. Antimicrobial Susceptibility
2.3. DNA Extraction and Polymerase Chain Reaction
2.4. Conjugation Assays
2.5. Whole Genome Sequencing and Bioinformatic Analysis
3. Results and Discussion
3.1. OXA-48 was Identified a K. pneumoniae MLST ST307 Isolate
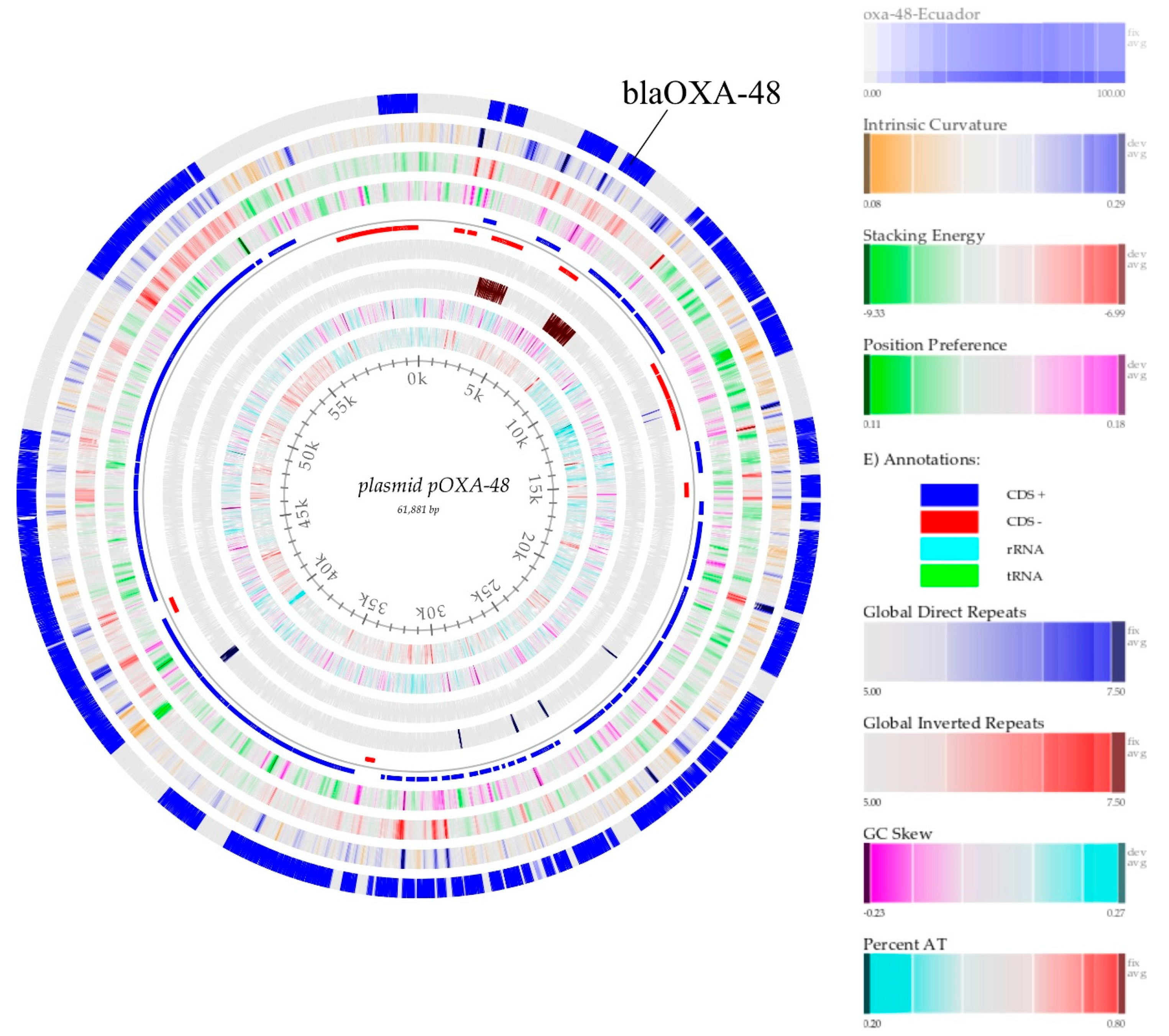
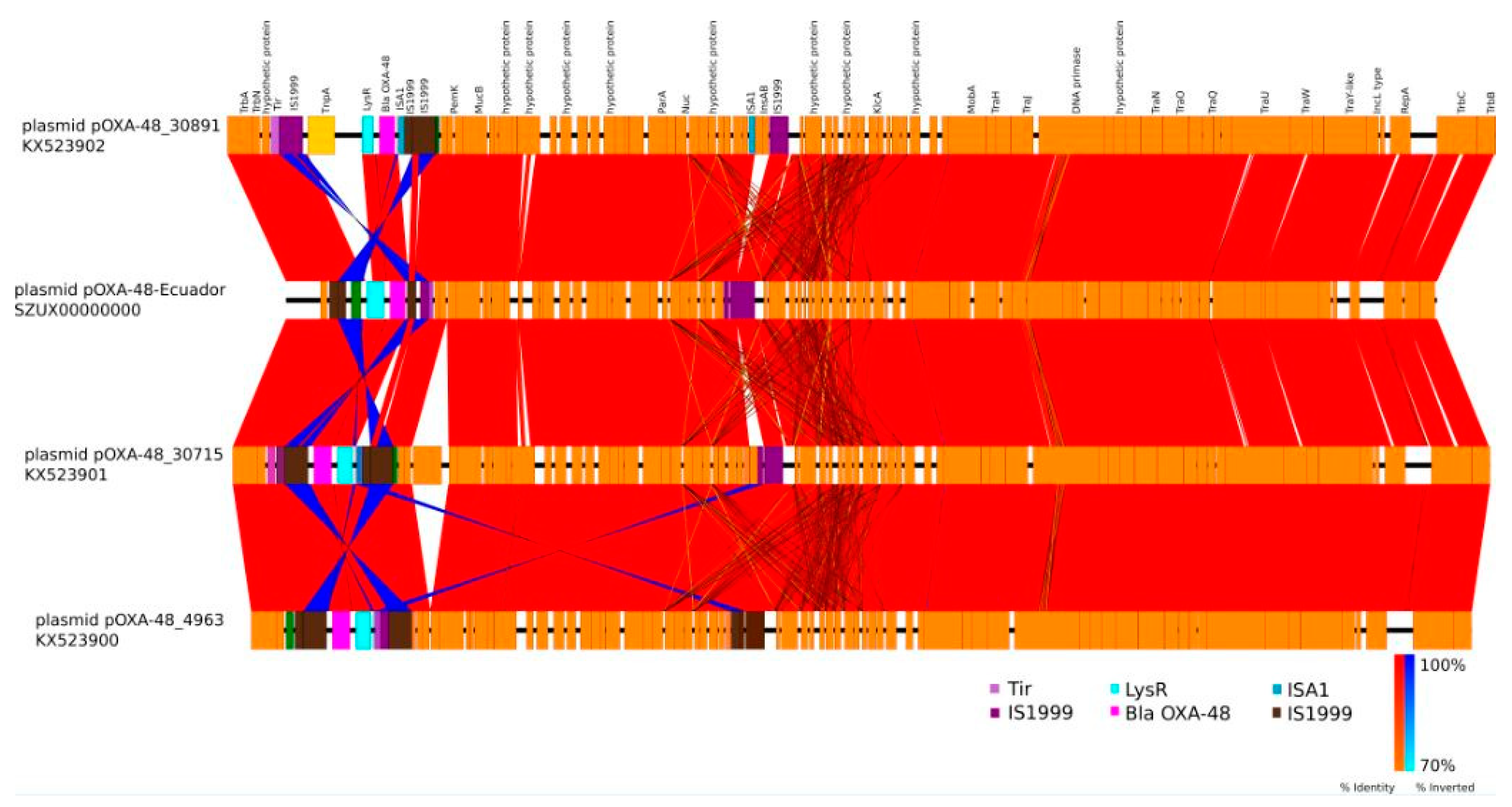
3.2. pOXA-48 is Found on the HEEJev_01 Plasmid
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Antimicrobial Resistance: Global Report on Surveillance 2014; The Organization: Geneva, Switzerland, 2014; Available online: https://www.who.int/drugresistance/documents/surveillancereport/en (accessed on 5 April 2019).
- World Health Organization. Global Action Plan on Antimicrobial Resistance 2015; The Organization: Geneva, Switzerland, 2014; Available online: https://www.who.int/ (accessed on 5 April 2019).
- CDC. Antibiotic Resistance Threats in the United States, 2019; U.S. Department of Health and Human Services, CDC: Atlanta, GA, USA, 2019. [Google Scholar]
- Bonomo, R.A. β-Lactamases: A Focus on Current Challenges. Cold Spring Harb. Perspect. Med. 2016, 7, a025239. [Google Scholar] [CrossRef] [PubMed]
- Mathers, A.J.; Peirano, G.; Pitout, J. The Role of Epidemic Resistance Plasmids and International High-Risk Clones in the Spread of Multidrug-Resistant Enterobacteriaceae. Clin. Microbiol. Rev. 2015, 28, 565–591. [Google Scholar] [CrossRef] [PubMed]
- Tangden, T.; Giske, C.G. Global dissemination of extensively drug-resistant carbapenemase-producing Enterobacteriaceae: Clinical perspectives on detection, treatment and infection control. J. Intern. Med. 2015, 277, 501–512. [Google Scholar] [CrossRef] [PubMed]
- Yigit, H.; Queenan, A.M.; Anderson, G.J.; Doménech-Sánchez, A.; Biddle, J.W.; Steward, C.D.; Alberti, S.; Bush, K.; Tenover, F.C. Novel Carbapenem-Hydrolyzing β-Lactamase, KPC-1, from a Carbapenem-Resistant Strain of Klebsiella pneumoniae. Antimicrob. Agents Chemother. 2008, 52, 809. [Google Scholar] [CrossRef]
- Bowers, J.R.; Kitchel, B.; Driebe, E.M.; MacCannell, D.R.; Roe, C.; Lemmer, D.; De Man, T.; Rasheed, J.K.; Engelthaler, D.M.; Keim, P.; et al. Genomic Analysis of the Emergence and Rapid Global Dissemination of the Clonal Group 258 Klebsiella pneumoniae Pandemic. PLoS ONE 2015, 10, e0133727. [Google Scholar] [CrossRef] [PubMed]
- Escandón-Vargas, K.; Reyes, S.; Gutiérrez, S.; Villegas, M.V. The epidemiology of carbapenemases in Latin America and the Caribbean. Expert Rev. Anti-Infective Ther. 2016, 15, 277–297. [Google Scholar] [CrossRef] [PubMed]
- Nordmann, P.; Naas, T.; Poirel, L. Global Spread of Carbapenemase-producing Enterobacteriaceae. Emerg. Infect. Dis. 2011, 17, 1791–1798. [Google Scholar] [CrossRef]
- Canton, R.; Akova, M.; Carmeli, Y.; Giske, C.; Glupczynski, Y.; Gniadkowski, M.; Livermore, D.; Miriagou, V.; Naas, T.; Rossolini, G.M.; et al. Rapid evolution and spread of carbapenemases among Enterobacteriaceae in Europe. Clin. Microbiol. Infect. 2012, 18, 413–431. [Google Scholar] [CrossRef]
- Lowe, M.; Kock, M.M.; Coetzee, J.; Hoosien, E.; Peirano, G.; Strydom, K.-A.; Ehlers, M.M.; Mbelle, N.M.; Shashkina, E.; Haslam, D.B.; et al. Klebsiella pneumoniae ST307 with blaOXA-181, South Africa, 2014-2016. Emerg. Infect. Dis. 2019, 25, 739–747. [Google Scholar] [CrossRef]
- Wyres, K.L.; Hawkey, J.; Hetland, M.A.K.; Fostervold, A.; Wick, R.R.; Kupfer, S.S.; Hamidian, M.; Howden, B.P.; Löhr, I.H.; Holt, K.E. Emergence and rapid global dissemination of CTX-M-15-associated Klebsiella pneumoniae strain ST307. J. Antimicrob. Chemother. 2019, 74, 577–581. [Google Scholar] [CrossRef]
- Djahmi, N.; Dunyach-Rémy, C.; Pantel, A.; Dekhil, M.; Sotto, A.; Lavigne, J.-P. Epidemiology of Carbapenemase-Producing Enterobacteriaceae and Acinetobacter baumannii in Mediterranean Countries. BioMed Res. Int. 2014, 2014, 305784. [Google Scholar] [CrossRef] [PubMed]
- Poirel, L.; Potron, A.; Nordmann, P. OXA-48-like carbapenemases: The phantom menace. J. Antimicrob. Chemother. 2012, 67, 1597–1606. [Google Scholar] [CrossRef] [PubMed]
- Skálová, A.; Chudějová, K.; Rotová, V.; Medvecky, M.; Študentová, V.; Chudáčková, E.; Lavicka, P.; Bergerova, T.; Jakubu, V.; Zemlickova, H.; et al. Molecular Characterization of OXA-48-Like-Producing Enterobacteriaceae in the Czech Republic and Evidence for Horizontal Transfer of pOXA-48-Like Plasmids. Antimicrob. Agents Chemother. 2017, 61, e01889-16. [Google Scholar] [CrossRef] [PubMed]
- Mairi, A.; Pantel, A.; Sotto, A.; Lavigne, J.-P.; Touati, A. OXA-48-like carbapenemases producing Enterobacteriaceae in different niches. Eur. J. Clin. Microbiol. Infect. Dis. 2017, 37, 587–604. [Google Scholar] [CrossRef] [PubMed]
- Vanegas, J.M.; Ospina, W.P.; Higuita-Gutiérrez, L.F.; Jiménez-Quiceno, J.N.; Higuita, L.F. First reported case of an OXA-48-producing isolate from a Colombian patient. J. Glob. Antimicrob. Resist. 2016, 6, 67–68. [Google Scholar] [CrossRef] [PubMed]
- Lascols, C.; Peirano, G.; Hackel, M.; Laupland, K.B.; Pitout, J. Surveillance and Molecular Epidemiology of Klebsiella pneumoniae Isolates That Produce Carbapenemases: First Report of OXA-48-Like Enzymes in North America. Antimicrob. Agents Chemother. 2012, 57, 130–136. [Google Scholar] [CrossRef]
- Sampaio, J.L.M.; Ribeiro, V.B.; Campos, J.C.; Rozales, F.P.; Magagnin, C.M.; Falci, D.R.; Da Silva, R.C.F.; Dalarosa, M.G.; Luz, D.I.; Vieira, F.J.; et al. Detection of OXA-370, an OXA-48-Related Class D β-Lactamase, in Enterobacter hormaechei from Brazil. Antimicrob. Agents Chemother. 2014, 58, 3566–3567. [Google Scholar] [CrossRef]
- Pitout, J.; Peirano, G.; Kock, M.M.; Strydom, K.-A.; Matsumura, Y. The Global Ascendency of OXA-48-Type Carbapenemases. Clin. Microbiol. Rev. 2019, 33, e00102-19. [Google Scholar] [CrossRef]
- Giani, T.; Conte, V.; Di Pilato, V.; Aschbacher, R.; Weber, C.; Larcher, C.; Rossolini, G.M. Escherichia coli from Italy Producing OXA-48 Carbapenemase Encoded by a Novel Tn1999 Transposon Derivative. Antimicrob. Agents Chemother. 2012, 56, 2211–2213. [Google Scholar] [CrossRef]
- Beyrouthy, R.; Robin, F.; Delmas, J.; Gibold, L.; Dalmasso, G.; Dabboussi, F.; Hamzé, M.; Bonnet, R. IS1R-Mediated Plasticity of IncL/M Plasmids Leads to the Insertion of blaOXA-48 into the Escherichia coli Chromosome. Antimicrob. Agents Chemother. 2014, 58, 3785–3790. [Google Scholar] [CrossRef]
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing, 28th ed.; CLSI Supplement M100; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2018. [Google Scholar]
- Poirel, L.; Walsh, T.R.; Cuvillier, V.; Nordmann, P. Multiplex PCR for detection of acquired carbapenemase genes. Diagn. Microbiol. Infect. Dis. 2011, 70, 119–123. [Google Scholar] [CrossRef] [PubMed]
- Diancourt, L.; Passet, V.; Verhoef, J.; Grimont, P.A.D.; Brisse, S. Multilocus Sequence Typing of Klebsiella pneumoniae Nosocomial Isolates. J. Clin. Microbiol. 2005, 43, 4178–4182. [Google Scholar] [CrossRef] [PubMed]
- Gruber, T.M.; Göttig, S.; Mark, L.; Christ, S.; Kempf, V.A.J.; Wichelhaus, T.A.; Hamprecht, A. Pathogenicity of pan-drug-resistant Serratia marcescens harbouring blaNDM-1. J. Antimicrob. Chemother. 2014, 70, 1026–1030. [Google Scholar] [CrossRef] [PubMed]
- Bou, G.; Cartelle, M.; Tomas, M.; Canle, D.; Molina, F.; Moure, R.; Eiros, J.M.; Guerrero, A. Identification and Broad Dissemination of the CTX-M-14 β-Lactamase in Different Escherichia coli Strains in the Northwest Area of Spain. J. Clin. Microbiol. 2002, 40, 4030–4036. [Google Scholar] [CrossRef]
- Fernández, A.; Gil, E.; Cartelle, M.; Pérez, A.; Beceiro, A.; Mallo, S.; Tomás, M.M.; Pérez-Llarena, F.J.; Villanueva, R.; Bou, G. Interspecies spread of CTX-M-32 extended-spectrum beta-lactamase and the role of the insertion sequence IS1 in down-regulating bla CTX-M gene expression. J. Antimicrob. Chemother. 2007, 59, 841–847. [Google Scholar] [CrossRef]
- Carattoli, A.; Bertini, A.; Villa, L.; Falbo, V.; Hopkins, K.L.; Threlfall, E.J. Identification of plasmids by PCR-based replicon typing. J. Microbiol. Methods 2005, 63, 219–228. [Google Scholar] [CrossRef]
- Poirel, L.; Héritier, C.; Tolün, V.; Nordmann, P. Emergence of oxacillinase-mediated resistance to imipenem in Klebsiella pneumoniae. Antimicrob. Agents Chemother. 2004, 48, 15–22. [Google Scholar] [CrossRef]
- Andrews, S. FastQC: A Quality Control Tool for High Throughput Sequence Data. 2011. Available online: http://www.bioinformatics.babraham.ac.uk/projects/fastqc (accessed on 24 October 2019).
- Li, Y.-L.; Weng, J.-C.; Hsiao, C.-C.; Chou, M.-T.; Tseng, C.-W.; Hung, J.-H. PEAT: An intelligent and efficient paired-end sequencing adapter trimming algorithm. BMC Bioinform. 2015, 16 (Suppl. 1), S2. [Google Scholar] [CrossRef]
- Krueger, F. Trim Galore. A Wrapper Tool around Cutadapt and fastQC to Consistently Apply Quality and Adapter Trimming to FastQ Files. Available online: https://www.bioinformatics.babraham.ac.uk/projects/trim_galore/ (accessed on 24 October 2019).
- Bankevich, A.; Sergey, N.; Dmitry, A.; Alexey, G.; Mikhail, D.; Alexander, K.; Lesin, V.M.; Nikolenko, S.; Pham, S.; Prjibelski, A.D.; et al. Spades: A new genome assembly algorithm and its applications to single-cell sequencing. J. Comput. Biol. 2012, 19, 455–477. [Google Scholar] [CrossRef]
- Gurevich, A.; Saveliev, V.; Vyahhi, N.; Tesler, G. QUAST: Quality assessment tool for genome assemblies. Bioinformatics 2013, 29, 1072–1075. [Google Scholar] [CrossRef]
- McNair, K.; Edwards, R.A. GenomePeek—An online tool for prokaryotic genome and metagenome analysis. PeerJ 2015, 3, e1025. [Google Scholar] [CrossRef] [PubMed]
- Seemann, T. Prokka: Rapid prokaryotic genome annotation. Bioinformatics 2014, 30, 2068–2069. [Google Scholar] [CrossRef] [PubMed]
- Tatusova, T.; DiCuccio, M.; Badretdin, A.; Chetvernin, V.; Nawrocki, E.P.; Zaslavsky, L.; Lomsadze, A.; Pruitt, K.D.; Borodovsky, M.; Ostell, J. NCBI prokaryotic genome annotation pipeline. Nucleic Acids Res. 2016, 44, 6614–6624. [Google Scholar] [CrossRef] [PubMed]
- Huerta-Cepas, J.; Forslund, K.; Coelho, L.P.; Szklarczyk, D.; Jensen, L.J.; Von Mering, C.; Bork, P. Fast Genome-Wide Functional Annotation through Orthology Assignment by eggNOG-Mapper. Mol. Boil. Evol. 2017, 34, 2115–2122. [Google Scholar] [CrossRef] [PubMed]
- Carattoli, A.; Zankari, E.; García-Fernández, A.; Larsen, M.V.; Lund, O.; Villa, L.; Aarestrup, F.M.; Hasman, H. In Silico Detection and Typing of Plasmids using PlasmidFinder and Plasmid Multilocus Sequence Typing. Antimicrob. Agents Chemother. 2014, 58, 3895–3903. [Google Scholar] [CrossRef] [PubMed]
- Bushnell, B. BBMap Short Read Aligner; University of California: Berkeley, CA, USA, 2016; Available online: http://sourceforgenet/projects/bbmap (accessed on 24 October 2019).
- Golosova, O.; Henderson, R.; Vaskin, Y.; Gabrielian, A.; Grekhov, G.; Nagarajan, V.; Oler, A.J.; Quinones, M.; Hurt, D.; Fursov, M.; et al. Unipro UGENE NGS pipelines and components for variant calling, RNA-seq and ChIP-seq data analyses. PeerJ 2014, 2, e644. [Google Scholar] [CrossRef]
- Romero-Alvarez, D.; Reyes, J.; Quezada, V.; Satán, C.; Cevallos, N.; Barrera, S.; Trueba, G.; Escobar, L.E.; Villacís, J.E. First case of New Delhi metallo-β-lactamase in Klebsiella pneumoniae from Ecuador: An update for South America. Int. J. Infect. Dis. 2017, 65, 119–121. [Google Scholar] [CrossRef]
- Boutal, H.; Vogel, A.; Bernabeu, S.; Devilliers, K.; Creton, E.; Cotellon, G.; Plaisance, M.; Oueslati, S.; Dortet, L.; Jousset, A.; et al. A multiplex lateral flow immunoassay for the rapid identification of NDM-, KPC-, IMP- and VIM-type and OXA-48-like carbapenemase-producing Enterobacteriaceae. J. Antimicrob. Chemother. 2018, 73, 909–915. [Google Scholar] [CrossRef]
- Jing, X.; Min, X.; Zhang, X.; Gong, L.; Wu, T.; Sun, R.; Chen, L.; Liu, R.; Zeng, J. The Rapid Carbapenemase Detection Method (rCDM) for Rapid and Accurate Detection of Carbapenemase-Producing Enterobacteriaceae and Pseudomonas aeruginosa. Front. Microbiol. 2019, 9, 371. [Google Scholar] [CrossRef]
- Evans, B.; Amyes, S.G.B. OXA -Lactamases. Clin. Microbiol. Rev. 2014, 27, 241–263. [Google Scholar] [CrossRef]
- Pierce, V.M.; Simner, P.J.; Lonsway, D.R.; Roe-Carpenter, D.E.; Johnson, J.K.; Brasso, W.B.; Bobenchik, A.M.; Lockett, Z.C.; Charnot-Katsikas, A.; Ferraro, M.J.; et al. Modified Carbapenem Inactivation Method for Phenotypic Detection of Carbapenemase Production among Enterobacteriaceae. J. Clin. Microbiol. 2017, 55, 2321–2333. [Google Scholar] [CrossRef]
- Tijet, N.; Patel, S.N.; Melano, R. Detection of carbapenemase activity in Enterobacteriaceae: Comparison of the carbapenem inactivation method versus the Carba NP test: Table 1. J. Antimicrob. Chemother. 2015, 71, 274–276. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Villa, L.; Feudi, C.; Fortini, D.; Brisse, S.; Passet, V.; Bonura, C.; Endimiani, A.; Mammina, C.; Ocampo, A.M.; Jimenez, J.N.; et al. Diversity, virulence, and antimicrobial resistance of the KPC-producing Klebsiella pneumoniae ST307 clone. Microb. Genom. 2017, 3, e000110. [Google Scholar] [CrossRef] [PubMed]
- Domokos, J.; Damjanova, I.; Kristof, K.; Ligeti, B.; Kocsis, B.; Szabo, R. Multiple Benefits of Plasmid-Mediated Quinolone Resistance Determinants in Klebsiella pneumoniae ST11 High-Risk Clone and Recently Emerging ST307 Clone. Front. Microbiol. 2019, 10, 157. [Google Scholar] [CrossRef] [PubMed]
- Long, S.W.; Olsen, R.J.; Eagar, T.N.; Beres, S.B.; Zhao, P.; Davis, J.J.; Brettin, T.; Xia, F.; Musser, J.M. Population Genomic Analysis of 1,777 Extended-Spectrum Beta-Lactamase-Producing Klebsiella pneumoniae Isolates, Houston, Texas: Unexpected Abundance of Clonal Group 307. mBio 2017, 8, e00489-17. [Google Scholar] [CrossRef]
- Salipante, S.J.; Sengupta, D.J.; Cummings, L.A.; Land, T.A.; Hoogestraat, D.R.; Cookson, B.T. Application of Whole-Genome Sequencing for Bacterial Strain Typing in Molecular Epidemiology. J. Clin. Microbiol. 2015, 53, 1072–1079. [Google Scholar] [CrossRef]
- Bocanegra-Ibarias, P.; Garza-González, E.; Padilla-Orozco, M.; Mendoza-Olazarán, S.; Perez-Alba, E.; Flores-Treviño, S.; Garza-Ramos, U.; Silva-Sanchez, J.; Camacho-Ortiz, A. The successful containment of a hospital outbreak caused by NDM-1-producing Klebsiella pneumoniae ST307 using active surveillance. PLoS ONE 2019, 14, e0209609. [Google Scholar] [CrossRef]
- Haller, S.; Kramer, R.; Becker, K.; Bohnert, J.A.; Eckmanns, T.; Hans, J.B.; Hecht, J.; Heidecke, C.-D.; Hübner, N.-O.; Kramer, A.; et al. Extensively drug-resistant Klebsiella pneumoniae ST307 outbreak, north-eastern Germany, June to October 2019. Euro Surveill. 2019, 24, 1900734. [Google Scholar] [CrossRef]
- Mahérault, A.-C.; Kemble, H.; Magnan, M.; Gachet, B.; Roche, D.; Le Nagard, H.; Tenaillon, O.; Denamur, E.; Branger, C.; Landraud, L. Advantage of the F2:A1:B- IncF Pandemic Plasmid over IncC Plasmids in In Vitro Acquisition and Evolution of blaCTX-M Gene-Bearing Plasmids in Escherichia coli. Antimicrob. Agents Chemother. 2019, 63, e01130-19. [Google Scholar] [CrossRef]
- Peirano, G.; Bradford, P.A.; Kazmierczak, K.M.; Chen, L.; Kreiswirth, B.N.; Pitout, J. Importance of Clonal Complex 258 and IncFK2-like Plasmids among a Global Collection of Klebsiella pneumoniae with blaKPC. Antimicrob. Agents Chemother. 2017, 61, e02610-16. [Google Scholar] [CrossRef]
- Villa, L.; García-Fernández, A.; Fortini, D.; Carattoli, A. Replicon sequence typing of IncF plasmids carrying virulence and resistance determinants. J. Antimicrob. Chemother. 2010, 65, 2518–2529. [Google Scholar] [CrossRef] [PubMed]
- Reyes, J.; Villavicencio, F.; Villacís, J.E.; Pavón, E.; Campoverde, N.; Espinel, M.; Núñez, B.; Trueba, G. First report of a clinical isolate of blaOXA-48- carbapenemase producing Raoultella ornithinolytica in South America. Revista Argentina de Microbiología 2020, 52, 82–83. [Google Scholar] [CrossRef] [PubMed]
- Bedenić, B.; Slade, M.; Starcevic, L.Z.; Sardelic, S.; Vranić-Ladavac, M.; Benčić, A.; Atalić, V.Z.; Bogdan, M.; Bubonja-Sonje, M.; Tomić-Paradzik, M.; et al. Epidemic spread of OXA-48 beta-lactamase in Croatia. J. Med Microbiol. 2018, 67, 1031–1041. [Google Scholar] [CrossRef] [PubMed]
- Khajuria, A.; Praharaj, A.K.; Kumar, M.; Grover, N. Emergence of Escherichia coli, Co-Producing NDM-1 and OXA-48 Carbapenemases, in Urinary Isolates, at a Tertiary Care Centre at Central India. J. Clin. Diagn. Res. 2014, 8, DC01–DC04. [Google Scholar] [CrossRef] [PubMed]
- Jelić, M.; Škrlin, J.; Bejuk, D.; Koscak, I.; Butic, I.; Guzvinec, M.; Andrasević, A.T. Characterization of Isolates Associated with Emergence of OXA-48-Producing Klebsiella pneumoniae in Croatia. Microb. Drug Resist. 2018, 24, 973–979. [Google Scholar] [CrossRef] [PubMed]
- Salloum, T.; Arabaghian, H.; Alousi, S.; Abboud, E.; Tokajian, S. Genome sequencing and comparative analysis of an NDM-1-producing Klebsiella pneumoniae ST15 isolated from a refugee patient. Pathog. Glob. Heal. 2017, 111, 166–175. [Google Scholar] [CrossRef]
- Munoz-Price, L.S.; Poirel, L.; Bonomo, R.A.; Schwaber, M.J.; Daikos, G.L.; Cormican, M.; Cornaglia, G.; Garau, J.; Gniadkowski, M.; Hayden, M.K.; et al. Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases. Lancet Infect. Dis. 2013, 13, 785–796. [Google Scholar] [CrossRef]
- Lee, C.-R.; Lee, J.H.; Park, K.S.; Kim, Y.B.; Jeong, B.C.; Lee, S.H. Global Dissemination of Carbapenemase-Producing Klebsiella pneumoniae: Epidemiology, Genetic Context, Treatment Options, and Detection Methods. Front. Microbiol. 2016, 7, 895. [Google Scholar] [CrossRef]
- Machuca, J.; López-Cerero, L.; Fernández-Cuenca, F.; Mora-Navas, L.; Mediavilla-Gradolph, C.; López-Rodríguez, I.; Pascual, Á. OXA-48-Like-Producing Klebsiella pneumoniae in Southern Spain in 2014–2015. Antimicrob. Agents Chemother. 2018, 63, e01396-18. [Google Scholar] [CrossRef]
| MIC (μg/mL) * | K. pneumoniae OXA-48-like | E. coli J 53 Transconjugant |
|---|---|---|
| IMI | 2 (Intermediate) | 2 (Intermediate) |
| MER | 2 (Intermediate) | <1 (Susceptible) |
| ERT | 4 (Resistant) | 4 (Resistant) |
| CAZ | <1 * (Susceptible) | <1 (Susceptible) |
| CTX | <1 * (Susceptible) | <1 (Susceptible) |
| FEP | <2 * (Susceptible) | <2 (Susceptible) |
| ATM | <2 (Susceptible) | <2 (Susceptible) |
| PIP/TAZ | >64/4 (Intermediate) | >64/4 (Intermediate) |
| CIP | >2 (Resistant) | <0.25 (Susceptible) |
| COL | 0.5 (Susceptible) | 0.25 (Susceptible) |
| AK | <4 (Susceptible) | <4 (Susceptible) |
| GEN | 8 (Intermediate) | 8 (Intermediate) |
| TGC | <0.25 (Susceptible) | <0.25 (Susceptible) |
| mCIM | POS | POS |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Villacís, J.E.; Reyes, J.A.; Castelán-Sánchez, H.G.; Dávila-Ramos, S.; Lazo, M.A.; Wali, A.; Bodero, L.A.; Toapanta, Y.; Naranjo, C.; Montero, L.; et al. OXA-48 Carbapenemase in Klebsiella pneumoniae Sequence Type 307 in Ecuador. Microorganisms 2020, 8, 435. https://doi.org/10.3390/microorganisms8030435
Villacís JE, Reyes JA, Castelán-Sánchez HG, Dávila-Ramos S, Lazo MA, Wali A, Bodero LA, Toapanta Y, Naranjo C, Montero L, et al. OXA-48 Carbapenemase in Klebsiella pneumoniae Sequence Type 307 in Ecuador. Microorganisms. 2020; 8(3):435. https://doi.org/10.3390/microorganisms8030435
Chicago/Turabian StyleVillacís, José E., Jorge A. Reyes, Hugo G. Castelán-Sánchez, Sonia Dávila-Ramos, Miguel Angel Lazo, Ahmad Wali, Luis A. Bodero, Yadira Toapanta, Cristina Naranjo, Lorena Montero, and et al. 2020. "OXA-48 Carbapenemase in Klebsiella pneumoniae Sequence Type 307 in Ecuador" Microorganisms 8, no. 3: 435. https://doi.org/10.3390/microorganisms8030435
APA StyleVillacís, J. E., Reyes, J. A., Castelán-Sánchez, H. G., Dávila-Ramos, S., Lazo, M. A., Wali, A., Bodero, L. A., Toapanta, Y., Naranjo, C., Montero, L., Campos, J., Galas, M. G., & Gestal, M. C. (2020). OXA-48 Carbapenemase in Klebsiella pneumoniae Sequence Type 307 in Ecuador. Microorganisms, 8(3), 435. https://doi.org/10.3390/microorganisms8030435







