Uncommon Urinary Actinomycosis Mimicking Upper Urinary Tract Urothelial Tumor: Case Report and Literature Review
Abstract
1. Introduction
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Valour, F.; Karsenty, J.; Breton, P.; Gleizal, A.; Braun, E.; Chidiac, C.; Ader, F.; Senechal, A.; Dupieux, C.; Lustig, S.; et al. Actinomycosis: Etiology, Clinical Features, Diagnosis, Treatment, and Management. Infect. Drug Resist. 2014, 7, 183. [Google Scholar] [CrossRef] [PubMed]
- Könönen, E.; Wade, W.G. Actinomyces and related organisms in human infections. Clin. Microbiol. Rev. 2015, 28, 419–442. [Google Scholar] [CrossRef]
- Boyanova, L.; Kolarov, R.; Mateva, L.; Markovska, R.; Mitov, I. Actinomycosis: A frequently forgotten disease. Future Microbiol. 2015, 10, 613–628. [Google Scholar] [CrossRef] [PubMed]
- Wong, V.K.; Turmezei, T.D.; Weston, V.C. Actinomycosis. BMJ 2011, 343, d6099. [Google Scholar] [CrossRef] [PubMed]
- Najib, B.; Arab, W.; Khazen, J.; Abdelkhalek, Y.; Abdallah, W.; Khaddage, A.; Atallah, D. A case of pelvic actinomycosis affecting genital, urinary and digestive tracts: A rare misleading diagnosis. Future Sci. OA 2021, 7, FSO740. [Google Scholar] [CrossRef]
- Cvetkov, M.C.; Elenkov, C.; Georgiev, M.; Topov, U.; Stefanova, G. Renal actinomycosis complicated by renoduodenal fistula and diabetes mellitus. Br. J. Urol. 1995, 75, 104–105. [Google Scholar] [CrossRef]
- Hyldgaard-Jensen, J.; SandstrØm, H.R.; Pedersen, J.F. Ultrasound diagnosis and guided biopsy in renal actinomycosis. Br. J. Radiol. 1999, 72, 510–512. [Google Scholar] [CrossRef]
- Horváth, K.; Porkoláb, Z.; Palkó, A. Primary renal and retroperitoneal actinomycosis. Eur. Radiol. 2000, 10, 287–289. [Google Scholar] [CrossRef]
- Dieckmann, K.P.; Henke, R.P.; Ovenbeck, R. Renal actinomycosis mimicking renal carcinoma. Eur. Urol. 2001, 39, 357–359. [Google Scholar] [CrossRef]
- Hilfiker, M.L. Disseminated actinomycosis presenting as a renal tumor with metastases. J. Pediatr. Surg. 2001, 36, 1577–1578. [Google Scholar] [CrossRef]
- Horino, T.; Yamamoto, M.; Morita, M.; Takao, T.; Yamamoto, Y.; Geshi, T. Renal Actinomycosis Mimicking Renal Tumor: Case Report. South. Med. J. 2004, 97, 316–318. [Google Scholar] [CrossRef] [PubMed]
- Dhanani, N.N.; Jones, D.M.; Grossman, H.B. Medical management of renal actinomycosis. J. Urol. 2004, 171, 2373–2374. [Google Scholar] [CrossRef] [PubMed]
- Rubio Tortosa, I.; Sanchez Sanchis, M.; Coronel Sánchez, B.; Garcia Serrado, D.; Garcia Torrelles, M.; Vergés Prosper, A.; San Juan De La Orden, C. Actinomicosis ureteral: A propósito de un caso. Arch. Españoles. Urol. 2005, 58, 351–353. [Google Scholar] [CrossRef] [PubMed]
- Gidwami, A.L.; Connolly, D.; Khan, A.; Kemohan, R.; Brown, M.; Kenny, B. Renal, colonic and retroperitoneal actinomycosis—A case report. West Afr. J. Med. 2005, 24, 343–345. [Google Scholar] [CrossRef][Green Version]
- Sallami, S.; Nouira, Y.; Hmidi, M.; Mekni, A.; Hendaoui, L. Pseudotumoral Renal Actinomycosis: A Case Report. Int. J. Urol. 2006, 13, 803–804. [Google Scholar] [CrossRef]
- Jalón Monzón, A.; Álvarez Múgica, M.; Seco Navedo, M.Á.; Fernández Gómez, J.M.; Bulnes Vázquez, V.; González Álvarez, R.C.; Gómez, F.J.; Sejas, F.J. A new form of presentation of renal actinomycosis: Renal tumor with retroperitoneal bleeding. Arch. Esp. Urol. 2006, 59, 756–759. Available online: https://www.redalyc.org/articulo.oa?id=181013928018 (accessed on 20 December 2024). [CrossRef]
- Yenarkarn, P.; Thoeni, R.F.; Hanks, D. Actinomycosis of left kidney with sinus tracts. Radiology 2007, 244, 309–313. [Google Scholar] [CrossRef]
- Efthimiou, I.; Mamoulakis, C.; Petraki, K.; Zorzos, I. Renal actinomycosis presenting as a suppurated solitary cyst. Indian J. Urol. 2008, 24, 416–418. [Google Scholar] [CrossRef]
- Lin, Y.-H.; Chen, H.-W.; Chuang, C.-K.; Ng, K.-F.; Wang, H.-H. Renal Actinomycosis Presented as Emphysematous Pyelonephritis: A Case Report. JTUA 2009, 20, 181–183. [Google Scholar]
- Baburaj, P.; Antony, T.; Madhu, C.S.; Harikrishnan, B.L. A rare case of Pyrexia of Unknown Origin due to Renal Actinomycosis. Kerala Med. J. 2009, 2, 91–92. [Google Scholar] [CrossRef]
- Manasanch, E.E.; Grivas, P.D.; Walter, O.; Davaro, R. Kidney actinomycosis, a rare diagnosis that can mimic renal cell carcinoma: A case report and review of the literature. Infect. Dis. Clin. Pract. 2012, 20, 362–364. [Google Scholar] [CrossRef]
- Lin, C.D.; Tai, H.C.; Wang, C.C.; Yu, C.T.; Chang, S.J.; Hsieh, C.H.; Shei-Dei Yang, S. Renal actinomycosis-An unusual cause of a renal abscess. Urol. Sci. 2012, 23, 129–132. [Google Scholar] [CrossRef]
- Pourmand, M.R.; Dehghani, S.; Hadjati, M.; Kosari, F.; Pourmand, G. Renal Actinomycosis in Presence of Renal Stones in a Patient with End Stage Renal Disease. J. Med. Bacteriol. 2012, 1, 62–65. [Google Scholar]
- Herbland, A.; Leloup, M.; Levrat, Q.; Guillaume, F.; Verrier, V.; Bouillard, P.; Landois, T.; Ouaki, C.F.; Lesieur, O. Fulminant course of unilateral emphysematous pyelonephritis revealing a renal actinomycosis caused by Actinomyces meyeri, an unknown cause of septic shock. J. Intensive Care 2014, 2, 42. [Google Scholar] [CrossRef]
- Agrawal, P.; Vaiphei, K. Renal actinomycosis. BMJ Case Rep. 2014, 2014, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Smid, M.C.; Bhardwaj, N.R.; Di Giovanni, L.M.; Eggener, S.; Della Torre, M. Renal hemorrhagic actinomycotic abscess in pregnancy. Infect. Dis. Rep. 2014, 6, 1–2. [Google Scholar] [CrossRef]
- Gulwani, H.V. Xanthogranulomatous pyelonephritis with colesional actinomycosis in a 63-year-old man. Indian J. Urol. 2015, 31, 144–145. [Google Scholar] [CrossRef]
- Niknejad, N.; Moradi, B.; Niknezhad, N.; Safaei, M.; Nili, F. Renal actinomycosis, a rare diagnosis which can clinically mimic a malignancy, case report and review of the literature. Arch. Pediatr. Infect. Dis. 2018, 6, 4–8. [Google Scholar] [CrossRef]
- Diab, C.; Almarzouq, A.; Ajise, O.; Barkati, S.; Tchervenkov, J.; Andonian, S. Renal actinomycosis presenting as uro-cutaneous fistula. Urol. Case Rep. 2020, 28, 101054. [Google Scholar] [CrossRef]
- Heo, S.H.; Shin, S.S.; Kim, J.W.; Lim, H.S.; Seon, H.J.; Jung, S.I.; Jeong, Y.Y.; Kang, H.K. Imaging of actinomycosis in various organs: A comprehensive review. Radiographics 2014, 34, 19–33. [Google Scholar] [CrossRef]
- Shanbhogue, K.P.; Ramani, N.; Surabhi, V.R.; Balasubramanya, R.; Prasad, S.R. Tumefactive Nonneoplastic Proliferative Pseudotumors of the Kidneys and Urinary Tract: CT and MRI Findings with Histopathologic Correlation. Radiographics 2023, 43, e230071. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.K.; Denton, K.J.; Minervini, A.; Oxley, J.; Khastigir, J.; Timoney, A.G.; Keeley, F.X., Jr. Correlation of upper-tract cytology, retrograde pyelography, ureteroscopic appearance, and ureteroscopic biopsy with histologic examination of upper-tract transitional cell carcinoma. J. Endourol. 2008, 22, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Scotland, K.B.; Kleinmann, N.; Cason, D.; Ehdaie, B. Ureteroscopic biopsy of upper tract urothelial carcinoma: A systematic review. J Endourol. 2013, 27, 560–567. [Google Scholar] [CrossRef]
- Roupret, M.; Seisen, T.; Birtle, A.J.; Capoun, O.; Compérat, E.M.; Dominguez-Escrig, J.; Andersson, I.G.; Liedberg, F.; Mariappan, P.; Mostafid, A.H.; et al. European Association of Urology Guidelines on Upper Urinary Tract Urothelial Carcinoma: 2023 Update. Eur. Urol. 2023, 84, 49–64. [Google Scholar] [CrossRef]
- Sullivan, D.C.; Chapman, S.W. Bacteria that masquerade as fungi: Actinomycosis/nocardia. Proc. Am. Thorac. Soc. 2010, 7, 216–221. [Google Scholar] [CrossRef]
- Kolbert, C.P.; Persing, D.H. Ribosomal DNA sequencing as a tool for identification of bacterial pathogens. Curr. Opin. Microbiol. 1999, 2, 299–305. [Google Scholar] [CrossRef]
- Lane, D.J. 16S/23S rRNA sequencing. In Nucleic Acid Techniques in Bacterial Systematics; Stackebrandt, E., Goodfellow, M., Eds.; John Wiley & Sons: Chichester, UK, 1991; pp. 115–175. [Google Scholar]
- Wade, W.G.; Könönen, E. Propionibacterium, Lactobacillus, Actinomyces, and other non-spore-forming anaerobic gram-positive rods. In Manual of Clinical Microbiology, 10th ed.; Versalovic, J., Carroll, K.C., Funke, G., Jorgensen, J.H., Landry, M.L., Warnock, D.W., Eds.; ASM Press: Washington, DC, USA, 2011; pp. 817–833. [Google Scholar]
- Smith, A.J.; Hall, V.; Thakker, B.; Gemmell, C.G. Antimicrobial susceptibility testing of Actinomyces species with 12 antimicrobial agents. J. Antimicrob. Chemother. 2005, 56, 407–409. [Google Scholar] [CrossRef]
- Goldstein, E.J.C.; Citron, D.M.; Merriam, C.V.; Warren, Y.A.; Tyrrell, K.L.; Fernandez, H.T.; Bryskier, A. Comparative in vitro activities of XRP 2868, pristinamycin, quinupristin-dalfopristin, vancomycin, daptomycin, linezolid, clarithromycin, telithromycin, clindamycin, and ampicillin against anaerobic gram-positive species, actinomycetes, and lactobacilli. Antimicrob. Agents Chemother. 2005, 49, 408–413. [Google Scholar] [CrossRef]


| Gender | Age (Years) | Clinical Presentation | Imaging Findings | Diagnostic Method | Species | Risk Factors | Treatment | Outcome | Reference |
|---|---|---|---|---|---|---|---|---|---|
| Female | 19 | Renal tumor with duodenal fistula | US: Extensive tumor mass affecting the right kidney | Histopathology | Not identified | DM | Radical nephrectomy | Alive | [6] |
| Male | 45 | Renal tumor | US: 7-cm solid mass in the upper pole of the right kidney with less echogenicity than the renal cortex and with a multinodular internal pattern + poorly delimited subcutaneous lesion at the thoracic level CT: enlarged right kidney or with heterogeneous contrast enhancement and edema in the fascia, renal hilum, muscles, retroperitoneum and pleura | Histopathology | Not identified | None | IV penicillin for two months and then orally for at least 4 months | Alive | [7] |
| Male | 41 | Renal tumor | US: heterogeneous left renal mass that bulges around the contour and compromises the renal sinus and parenchyma. CT: Tissue mass infiltrating the left kidney with contrast enhancement + enlarged psoas muscle or with multiple ring-shaped enhancements + small focal hypodensity in the liver | Histopathology | Not identified | DM | Abscess drainage and a high dose of oral penicillin | Alive | [8] |
| Male | 52 | Renal tumor | US: left-sided renal mass CT: 4 cm mass in the upper pole region of the left kidney with an irregularly shaped radiolucent middle area | Histopathology | Not identified | None | Nephrectomy and oral amoxicillin for 3 months | Alive | [9] |
| Male | 16 | Renal tumor | CT: renal mass in the upper right pole + mass in the left lobe of the liver + multiple pulmonary nodules | Histopathology + Positive abscess culture | Actinomyces israelii + Actinobacillus actinomycetemycomitans | None | IV penicillin for two weeks, followed by oral doxycycline for 6 months | Alive | [10] |
| Male | 68 | Renal tumor | US: Hypoechoic solid mass of the right kidney CT: Enlarged right kidney with a mass with little enhancement with contrast medium MRI: Renal tumor of hypo to isointense (T1) and hypointense (T2) | Histopathology | Not identified | Oral infections | Nephrectomy | Alive | [11] |
| Male | 64 | Renal tumor | CT: heterogeneous mass with enhancement in the right flank containing air-fluid levels and an inflammatory reaction affecting the right colon and psoas muscle | Histopathology | Not identified | IV penicillin for 8 weeks followed by doxycycline + oral ciprofloxacin for 4 months | Alive | [12] | |
| Male | 66 | Right ureter tumor | US: grade II ureteric opyelo-calicectasis of the right kidney CT: Hydronephrotic atrophy of the right kidney, with no intraureteral endoluminal images visible | Histopathology | Not identified | DM | Right radical nephroureterectomy | Alive | [13] |
| Male | 41 | Renal tumor | CT: large mass compatible with a large locally advanced left hypernephroma, with invasion of the left psoas and descending colon | Histopathology | Not identified | None | Nephrectomy | Alive | [14] |
| Female | 25 | Renal tumor | CT: Right renal solid mass that enhances with contrast with central liquefaction areas and invades the liver, alveolar infiltrates | Histopathology | Not identified | Pregnancy | Nephrectomy and oral penicillin for 2 months | Alive | [15] |
| Female | 27 | Renal tumor with retroperitoneal bleeding | US and CT: Right renal mass with retroperitoneal bleeding | Histopathology | Not identified | None | Nephrectomy | Alive | [16] |
| Male | 39 | Chronic kidney infection | CT: Enlargement of the left kidney due to an infiltrative process with enhancement + wall of the descending colon with increased thickness and enhancement + sinus tracts extending from the colon to the left iliopsoas muscle and the muscles of the abdominal wall | Histopathology | Not identified | None | Nephrectomy + segmental resection of the descending colon Oral penicillin for 6 months | Alive | [17] |
| Female | 50 | Kidney cyst | US: 8 × 8 cm left renal mass with a central fluid portion and a thick surrounding wall CT: Enlarged left kidney with a well-delineated 5 × 9 cm cystic lesion of homogeneous content of 0–3 HU surrounded by a thickened outer wall without contrast enhancement. | Positive culture of purulent discharge | Actinomyces israelii | None | Nephrectomy and oral amoxicillin for 3 months | Alive | [18] |
| Female | 42 | Septic shock caused by Emphysematous pyelonephritis | CT: striation of perirenal fat, calculus at the right ureteropelvic junction with formation of air and subcapsular fluid in the right kidney, mild right pleural effusion | Histopathology | Not identified | DM Kidney stones | Nephrectomy and oral penicillin | Alive | [19] |
| Male | 55 | Renal tumor | US: Heterogeneous mass in the upper pole of the left kidney CT: Mass in the upper pole of the left kidney with thickening of the renal fascia MRI: Hypointense mass on T1 and T2 | Histopathology | Not identified | None | Nephrectomy and oral penicillin for 8 weeks | Alive | [20] |
| Female | 80 | Renal tumor | MRI: central hyperintense lesion with a surrounding isointense mass on T2-weighted images, suggestive of central necrotizing tumor CT: exophytic renal mass with extension contiguous to the diaphragm, pleural space and lower right lobe | Positive culture of purulent fluid | Actinomyces gerencseriae | Renal carcinoma | Oral penicillin G for 3 weeks and then amoxicillin for 6 months. | Alive | [21] |
| Female | 59 | Pyonephrosis | US: cystic renal mass with an irregular solid border CT: enlarged right kidney infiltrated with multiple cystic lesions with hypodense content | Positive blood culture + Histopathology | Not identified | DM ESRD | Nephrectomy and Penicillin for 4 weeks | Alive | [22] |
| Male | 56 | Asymptomatic | US: multiple stones in both kidneys | Histopathology | Not identified | Nephrolithiasis with ureteral catheterization | Right nephrectomy and doxycycline for 4 weeks | Alive | [23] |
| Female | 75 | Septic shock caused by Emphysematous pyelonephritis | CT: pyonephrosis of the right kidney, pneumaturia in the collecting system, cyst in the lower pole, dilated pelvicalyceal cavities CT: persistent posterior abscess of the right kidney with infiltration of the perinephric space | Positive urine culture | Actimomyces meyeri | None | Open stenting of the right ureter with drainage of Pyuria + percutaneous drainage of the abscess Amoxicillin for 3 months | Alive | [24] |
| Male | 52 | Septic shock with bilateral necrotizing papillitis | US: loss of corticomedullary differentiation and increased renal echogenicity. CT: enlarged kidneys with reduced nephrogenic density and compact pyelocaliceal system. | Histopathology | Not identified | DM | Cefotaxime and azithromycin, empirically | Deceased | [25] |
| Female | 20 | Renal tumor | US: Hemorrhagic mass in the right renal subcapsular area extending to the right diaphragm MRI: Heterogeneous mass in the right kidney extending to the edge of the liver and mild hydronephrosis, splenomegaly | Histopathology | Not identified | Pregnancy | Resection of retroperitoneal mass + partial nephretomy IV piperacillin /Tazobactam and subsequently amoxicillin/clavulanate for 6 months | Alive | [26] |
| Male | 63 | Xanthogranulomatous pyelonephritis | CT: Diffuse Xanthogranulomatous pyelonephritis in the left kidney with extension of inflammation to the pararenal tissues | Histopathology | Not identified | None | Not available | Not available | [27] |
| Male | 8 | Renal tumor + Xanthogranulomatous pyelonephritis | US: solid cystic mass with extension to perinephric adipose tissue CT: enlargement of the right kidney with thickening of Gerota’s fascia and heterogeneous mass with cystic component in the upper pole of the right kidney | Histopathology | Not identified | None | Right nephrectomy and amoxicillin for 4 months | Alive | [28] |
| Male | 36 | Xanthogranulomatous pyelonephritis | CT: left Xanthogranulomatous pyelonephritis with a staghorn calculus and a urocutaneous fistula | Histopathology and + Positive culture of purulent discharge | Actinomyces odontolyticus Proteus mirabilis | Kidney stones | Radical left nephrectomy IV ertapenem for 6 weeks | Alive | [29] |
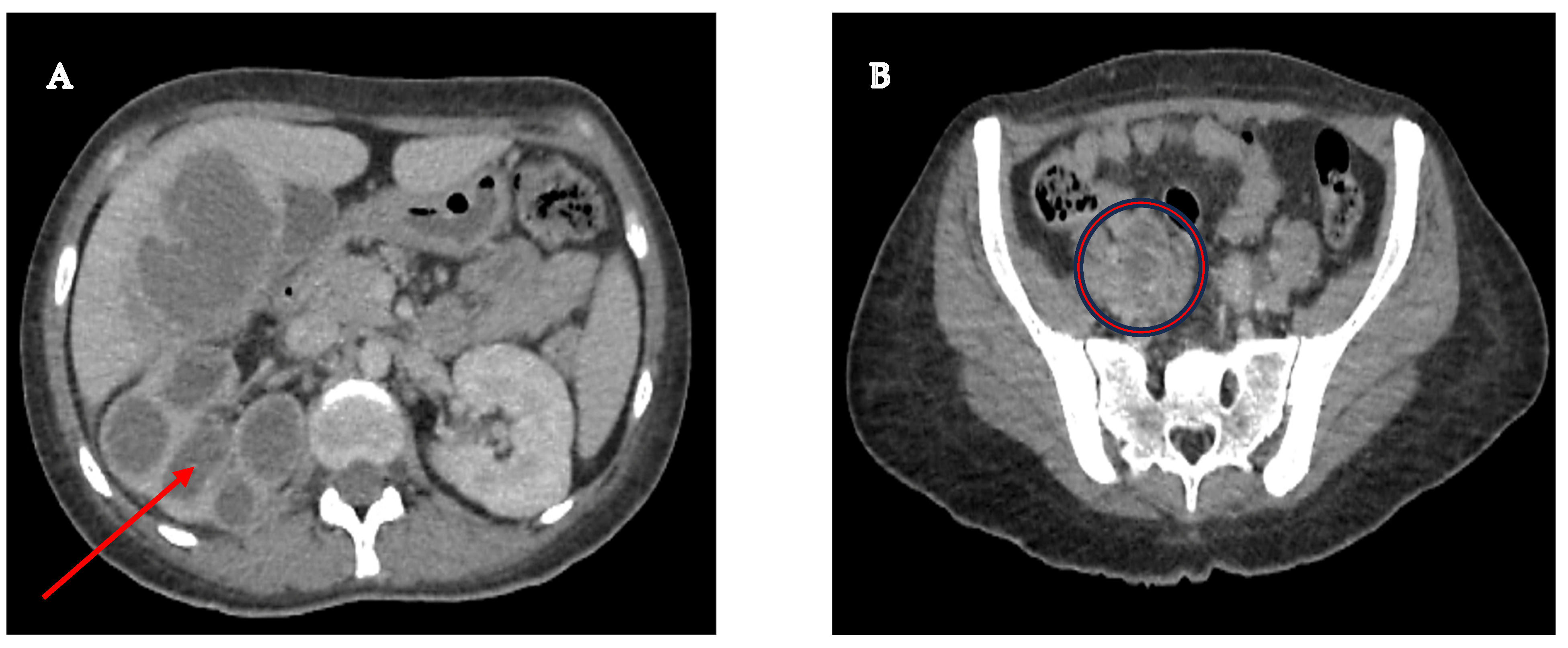
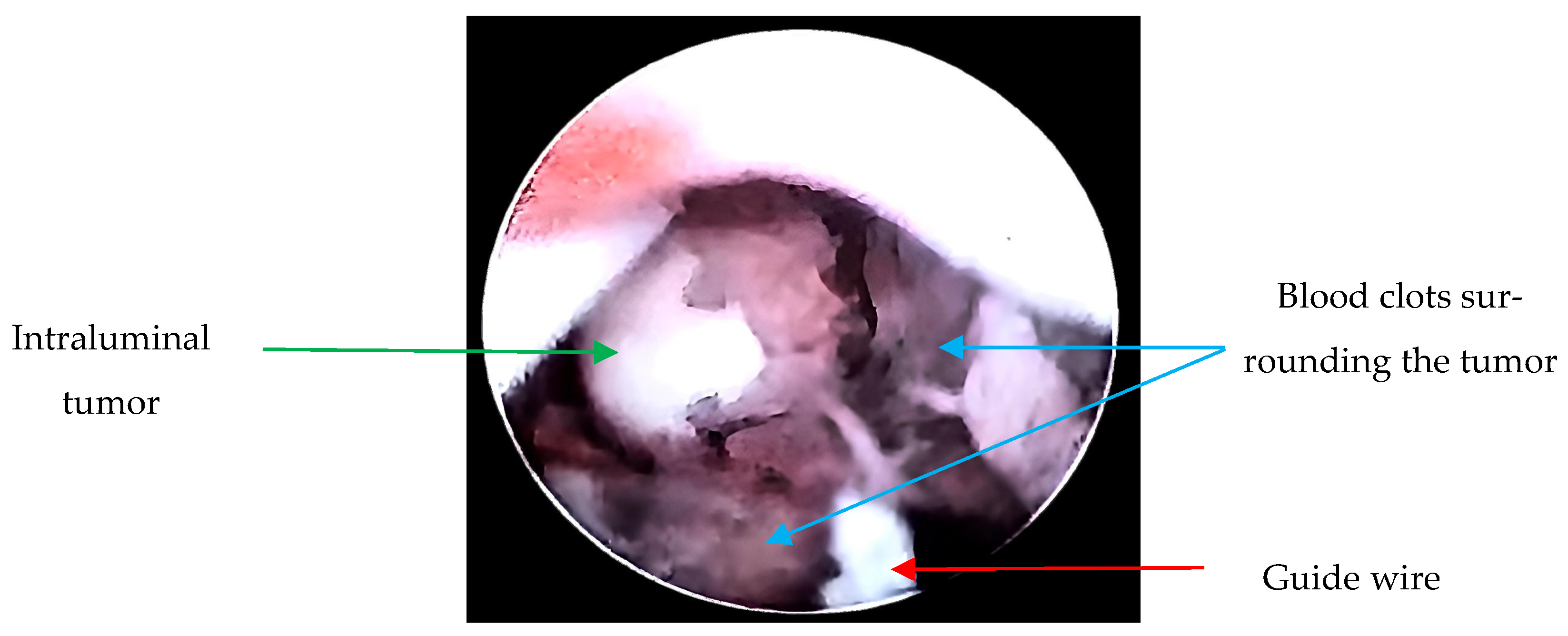
| Female | 33 | Right ureter tumor | CT: Right kidney with decreased cortical thickness associated with ureterohydronephrosis + Pelvic tumor with apparent origin in the lumen of the right ureter with infiltration into the distal third + liver lesion with liquid and solid components | Histopathology | Not identified | DM | Nephrectomy and Amoxicillin for 6 months | Alive | ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Meza-Meneses, P.A.; Becerra, R.P.; Sainz, G.G.; Ortiz, L.T.; Correa, A.M.; Soriano, A.R.P.; Santiago González, R.M.A.; Corral, A.D.; Valdez, O.V.; Morales, G.A.; et al. Uncommon Urinary Actinomycosis Mimicking Upper Urinary Tract Urothelial Tumor: Case Report and Literature Review. Microorganisms 2025, 13, 1033. https://doi.org/10.3390/microorganisms13051033
Meza-Meneses PA, Becerra RP, Sainz GG, Ortiz LT, Correa AM, Soriano ARP, Santiago González RMA, Corral AD, Valdez OV, Morales GA, et al. Uncommon Urinary Actinomycosis Mimicking Upper Urinary Tract Urothelial Tumor: Case Report and Literature Review. Microorganisms. 2025; 13(5):1033. https://doi.org/10.3390/microorganisms13051033
Chicago/Turabian StyleMeza-Meneses, Patricia A., Rodrigo Pérez Becerra, Gerardo Garza Sainz, Luis Trujillo Ortiz, Adrián Martinez Correa, Alan Rodrigo Pérez Soriano, Ruben Miguel Angel Santiago González, Aarón Delgado Corral, Omar Vieyra Valdez, Genaro Argüelles Morales, and et al. 2025. "Uncommon Urinary Actinomycosis Mimicking Upper Urinary Tract Urothelial Tumor: Case Report and Literature Review" Microorganisms 13, no. 5: 1033. https://doi.org/10.3390/microorganisms13051033
APA StyleMeza-Meneses, P. A., Becerra, R. P., Sainz, G. G., Ortiz, L. T., Correa, A. M., Soriano, A. R. P., Santiago González, R. M. A., Corral, A. D., Valdez, O. V., Morales, G. A., Díaz, M. A. T., Luna, A. S., Castro-Fuentes, C. A., & Osornio Sánchez, V. (2025). Uncommon Urinary Actinomycosis Mimicking Upper Urinary Tract Urothelial Tumor: Case Report and Literature Review. Microorganisms, 13(5), 1033. https://doi.org/10.3390/microorganisms13051033







