Increased Measured GFR and Proteinuria in Children with Previous Infection by SARS-CoV-2: Should We Be Concerned?
Abstract
:1. Introduction
2. Materials and Methods
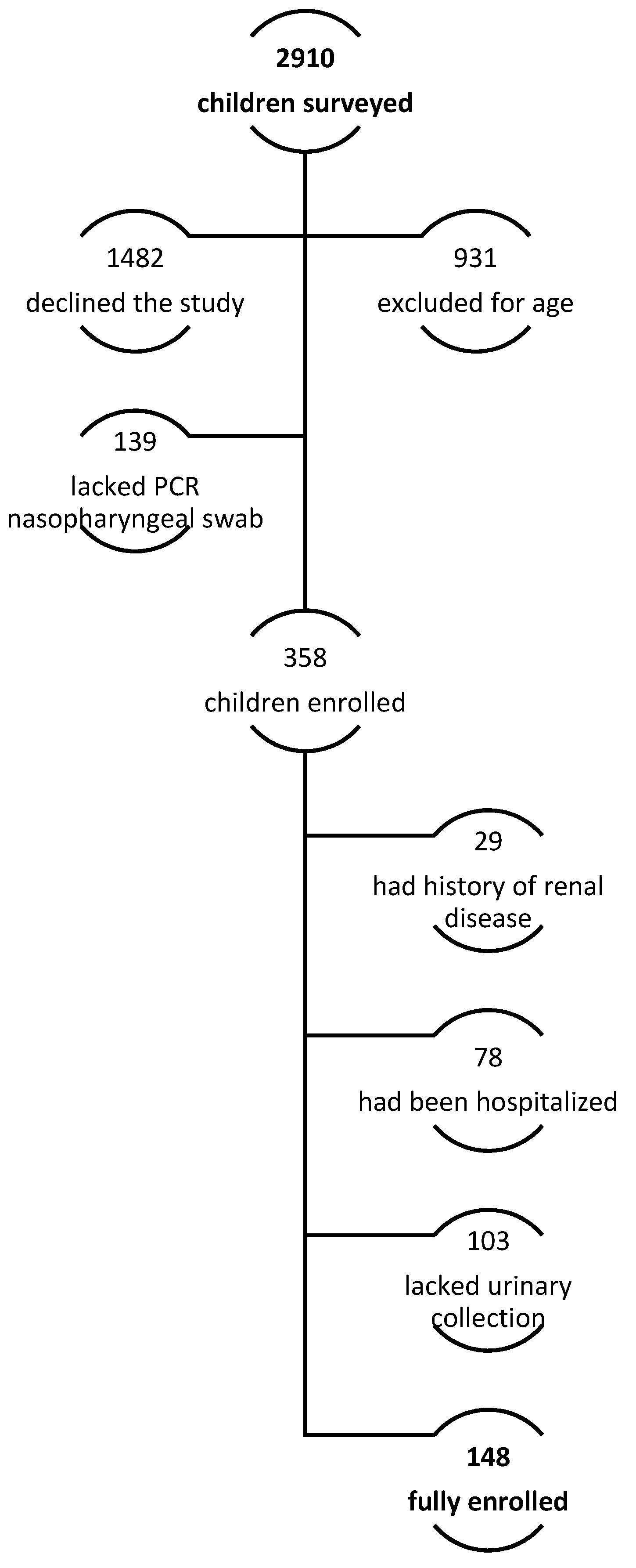
2.1. Patients
- -
- Diagnosis of SARS-CoV-2 infection made by molecular swab according to regulations at the time of diagnosis; all patients with positive antigenic swab had been confirmed with Polymerase Chain Reaction (PCR) nasopharyngeal swab for SARS-CoV-2. The procedure was performed as follows, according to Fazio et al. instructions [11]: the child was positioned seated, with the head tilted 30–45° upward and toward the operator, in order to have a direct view of the oropharynx. The swab was inserted in the inferomedial angle of the nostril, next to the nasal septum, proceeding along a plane parallel to the hard palate, and with the swab’s end pointed laterally, away from the nasal septum and toward the inferior turbinate. The swab was inserted for at least 9 cm to reach the right target.
- -
- Age at first evaluation between 3 and 18 years;
- -
- Paucisymptomatic infection: rhinitis, fever (>38.5 °C) lasting up to 72 h, cough, asthenia, myalgias, arthralgias, low-grade fever (<38.5 °C lasting up to 6 days);
- -
- Complete evaluation at our post-COVID-19 outpatient clinic of the Unit of Pediatrics of S. Maria Goretti Hospital.
- -
- Evaluation performed at least 2 weeks after a swab resulted negative for SARS-CoV-2.
- -
- Personal and family history of renal disease, based on clinical judgment, in particular: proteinuria and/or hematuria, solitary kidney functioning, urinary tract abnormalities, vesicoureteral reflux, glomerulonephritis (both acute and chronic), nephrotic syndrome.
- -
- Personal history of diseases linked to kidney diseases, such as obesity, genetic syndromes (i.e., Down syndrome), diabetes, etc.
- -
- Lack of parenting consent.
- -
- Vaccination for SARS-CoV-2.
- -
- Under or overcollection of urine. All children and parents had been instructed by trained nurses to ensure proper urine collection verbally and through an explanatory illustrated leaflet. When the children delivered their urine containers to the hospital, trained nurses conducted an additional interview aimed at ascertaining that the collection had been conducted properly. An assay on the urinary excretion of creatinine provided an additional approach to assessing the appropriateness of urine collection [12].
2.2. Study Protocol
- -
- Evaluation of both proteinuria/m2/day (Glenbio Ltd., Cork, Ireland) (n.v. < 100 mg/m2/day) and presence of microhematuria by urine cytofluorometry (n.v. < 10 Red Blood Cells/μL).
- -
- Evaluation of full abdominal ultrasound.
- -
- group A: from 1 to 14 days
- -
- group B: from 15 to 26 days
- -
- group C: greater than 27 days
- -
- early (assessed within 3 months of infection)
- -
- late (assessed more than 3 months after infection).
- -
- Age-matching with our SARS-CoV-2 cohort
- -
- Sex-matching with our SARS-CoV-2 cohort
- -
- Blood and urine analysis performed before year 2020: Glomerular filtration rate (GFR) as creatinine clearance (GFRCr). We considered as normal the range reported by Heilbron et al. [15], Fractional excretion of sodium (FENa), tubular reabsorption of phosphate (TRP), calcium–creatinine urine ratio (CaU/CrU). We considered normal values: FENa < 1%, TRP > 85%, CaU/CrU < 0.8 mg/mg in infants < 6 months, <0.6 mg/mg between 6 and 12 months and <0.2 in older children [16]. Evaluation of both proteinuria/m2/day (n.v. < 100 mg/m2/day) and presence of microhematuria by urine cytofluorometry (n.v. < 10 Red Blood Cells/μL).
- -
- Personal and family history of renal disease, based on clinical judgment, in particular: proteinuria and/or hematuria, solitary kidney functioning, urinary tract abnormalities, vesicoureteral reflux, glomerulonephritis (both acute and chronic), and nephrotic syndrome.
- -
- Personal history of diseases linked to kidney diseases, such as obesity, genetic syndromes (i.e., Down syndrome), diabetes, etc.
2.3. Statistical Analysis
3. Results
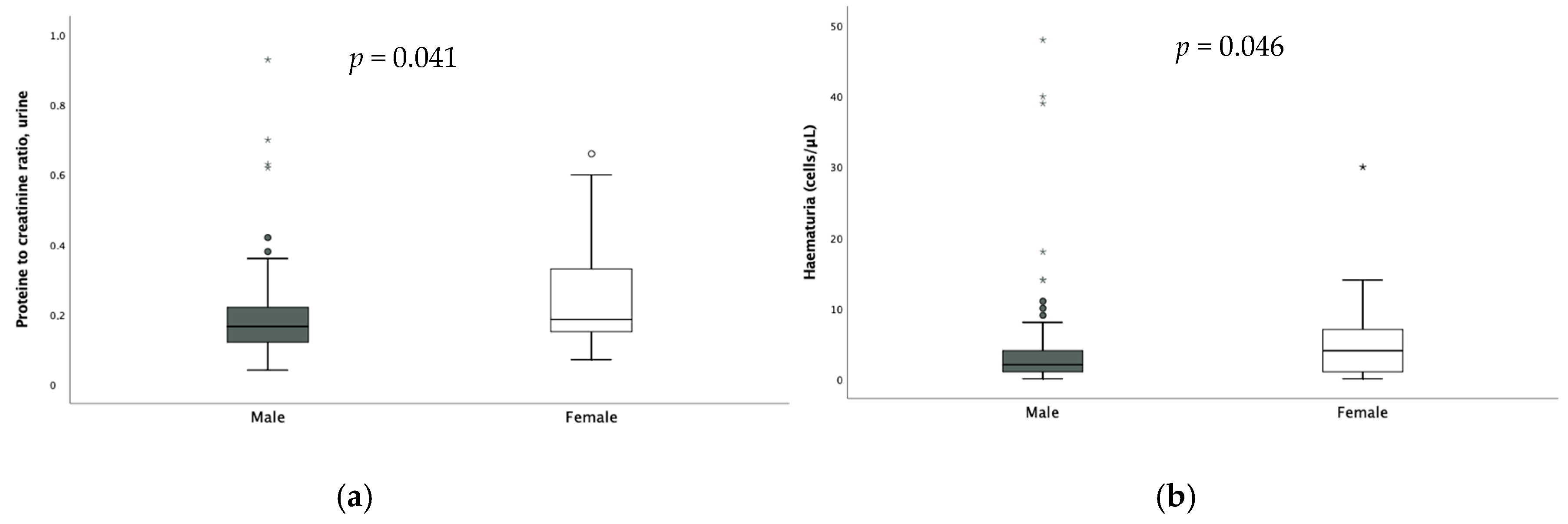
3.1. SARS-CoV-2 Population
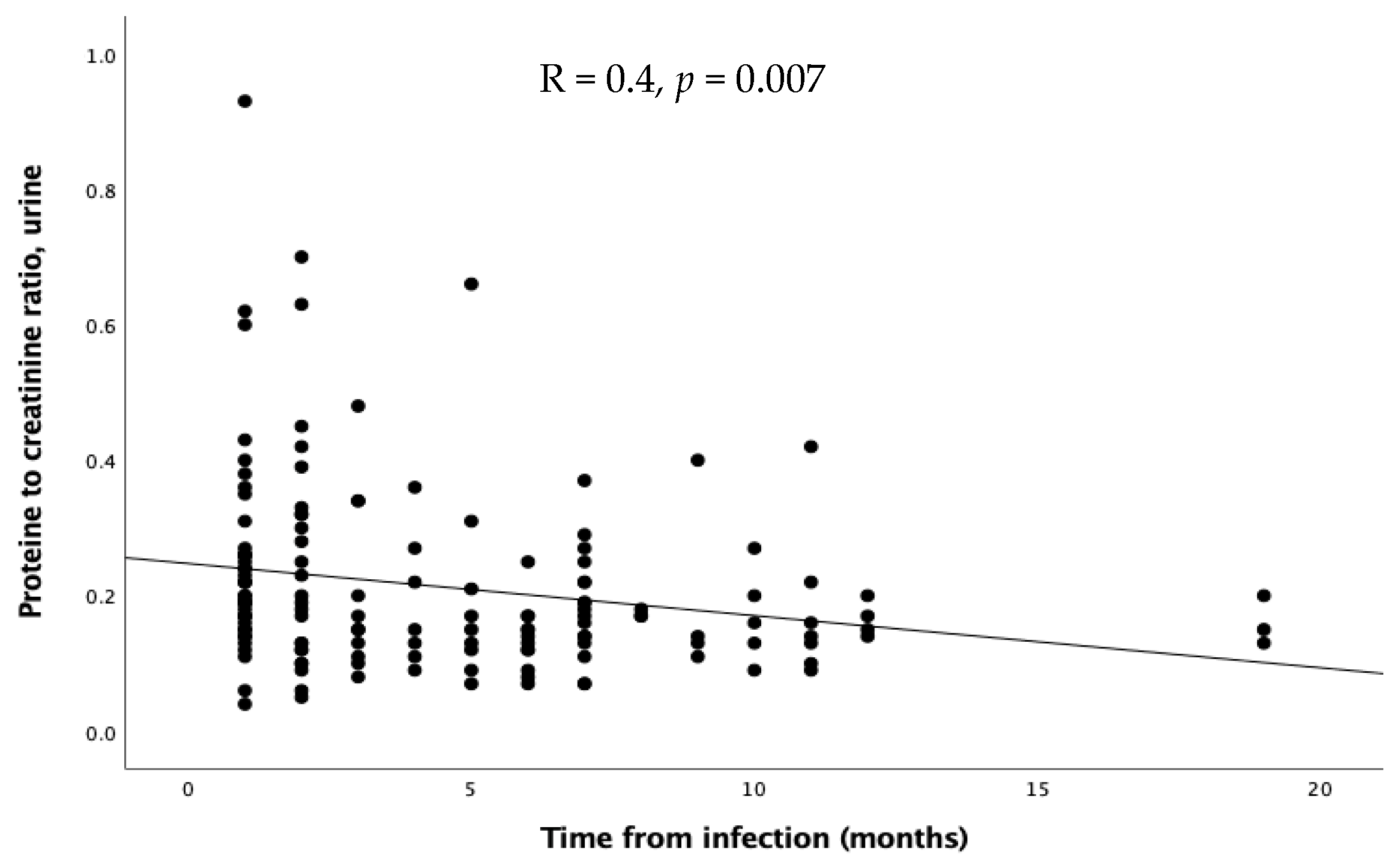
3.2. Analysis According to Time of Evaluation and Duration of Infection
3.3. Comparison Between SARS-CoV-2 Patients and Healthy Controls
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Lazzerini, M.; Sforzi, I.; Trapani, S.; Biban, P.; Silvagni, D.; Villa, G.; Tibaldi, J.; Bertacca, L.; Felici, E.; Perricone, G.; et al. Characteristics and risk factors for SARS-CoV-2 in children tested in the early phase of the pandemic: A cross-sectional study, Italy, 23 February to 24 May 2020. Eurosurveillance 2021, 26, 2001248. [Google Scholar] [CrossRef]
- Seth, S.; Rashid, F.; Khera, K. An overview of the COVID-19 complications in paediatric population: A pandemic dilemma. Int. J. Clin. Pract. 2021, 75, e14494. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.H.L.; Shenoy, M.; Kalra, P.A.; Chinnadurai, R. Intrinsic Kidney Pathology Following COVID-19 Infection in Children and Adolescents: A Systematic Review. Children 2021, 9, 3. [Google Scholar] [CrossRef] [PubMed]
- Meneghel, A.; Masenello, V.; Alfier, F.; Giampetruzzi, S.; Sembenini, C.; Martini, G.; Tirelli, F.; Meneghesso, D.; Zulian, F. Renal Involvement in Multisystem Inflammatory Syndrome in Children: Not Only Acute Kidney Injury. Children 2023, 10, 1661. [Google Scholar] [CrossRef]
- Basu, R.K.; Bjornstad, E.C.; Gist, K.M.; Starr, M.; Khandhar, P.; Chanchlani, R.; Kelli, A. Acute kidney injury in critically Ill children and young adults with suspected SARS-CoV2 infection. Pediatr. Res. 2022, 91, 1787–1796. [Google Scholar] [CrossRef]
- Stewart, D.J.; Mudalige, N.L.; Johnson, M.; Shroff, R.; du Pré, P.; Stojanovic, J. Acute kidney injury in paediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS) is not associated with progression to chronic kidney disease. Arch. Dis. Child. 2022, 107, e21. [Google Scholar] [CrossRef]
- Deep, A.; Upadhyay, G.; du Pré, P.; Lillie, J.; Pan, D.; Mudalige, N.; Kanthimathinathan, H.K.; Johnson, M.; Riphagen, S.; Dwarakanathan, B.; et al. Acute Kidney Injury in Pediatric Inflammatory Multisystem Syndrome Temporally Associated With Severe Acute Respiratory Syndrome Coronavirus-2 Pandemic: Experience From PICUs Across United Kingdom. Crit. Care Med. 2020, 48, 1809–1818. [Google Scholar] [CrossRef] [PubMed]
- Bjornstad, E.C.; Krallman, K.A.; Askenazi, D.; Zappitelli, M.; Goldstein, S.L.; Basu, R.K. Preliminary Assessment of Acute Kidney Injury in Critically Ill Children Associated with SARS-CoV-2 Infection: A Multicenter Cross-Sectional Analysis. Clin. J. Am. Soc. Nephrol. 2021, 16, 446–448. [Google Scholar] [CrossRef]
- Twichell, S.; Ashoor, I.; Boynton, S.; Dharnidharka, V.; Kizilbash, S.; Erez, D.L.; Smith, J. COVID-19 disease among children and young adults enrolled in the North American Pediatric Renal Trials and Collaborative Studies registry. Pediatr. Nephrol. 2023, 39, 1459–1468. [Google Scholar] [CrossRef]
- Saygili, S.; Canpolat, N.; Cicek, R.Y.; Agbas, A.; Yilmaz, E.K.; Sakalli, A.A.K.; Aygun, D.; Akkoc, G.; Demirbas, K.C.; Konukoglu, D.; et al. Clinical and subclinical acute kidney injury in children with mild-to-moderate COVID-19. Pediatr. Res. 2023, 93, 654–660. [Google Scholar] [CrossRef]
- Fazio, E.; Abousiam, M.; Caselli, A.; Accorona, R.; Nebiaj, A.; Ermoli, I.; Erckert, B.; Calabrese, L.; Gazzini, L. Proper Procedures for Performing Nasopharyngeal and Oropharyngeal Swabs for COVID-19. ATS Sch. 2020, 1, 495–497. [Google Scholar] [CrossRef] [PubMed]
- Lubrano, R.; Travasso, E.; Raggi, C.; Guido, G.; Masciangelo, R.; Elli, M. Blood pressure load, proteinuria and renal function in pre-hypertensive children. Pediatr. Nephrol. 2009, 24, 823–831. [Google Scholar] [CrossRef]
- WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: Length/Height-For-Age, Weight-For-Age, Weight-For-Length, Weight-Forheight and Body Mass Index-For-Age: Methods and Development; WHO: Geneva, Switzerland, 2006. [Google Scholar]
- Marcellino, A.; Bloise, S.; Fraternali, R.; Pirone, C.; Brandino, G.; Testa, A.; Filippi, L.; Lubrano, R. Evaluation of Renal Function and Scars in Children With Primary Vesicoureteral Reflux. Urology 2022, 168, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Heilbron, D.C.; Holliday, M.A.; Al-Dahwi, A.; Kogan, B.A. Expressing glomerular filtration rate in children. Pediatr. Nephrol. 1991, 5, 5–11. [Google Scholar] [CrossRef]
- Kruse, K.; Kracht, U.; Kruse, U. Reference values for urinary calcium excretion and screening for hypercalciuria in children and adolescents. Eur. J. Pediatr. 1984, 143, 25–31. [Google Scholar] [CrossRef]
- Adebayo, O.C.; Nkoy, A.B.; van den Heuvel, L.P.; Labarque, V.; Levtchenko, E.; Delanaye, P.; Pottel, H. Glomerular hyperfiltration: Part 2-clinical significance in children. Pediatr. Nephrol. 2023, 38, 2529–2547. [Google Scholar] [CrossRef]
- Levey, A.S.; Coresh, J.; Tighiouart, H.; Greene, T.; Inker, L.A. Measured and estimated glomerular filtration rate: Current status and future directions. Nat. Rev. Nephrol. 2020, 16, 51–64. [Google Scholar] [CrossRef]
- Stevens, L.A.; Coresh, J.; Greene, T.; Levey, A.S. Assessing kidney function--measured and estimated glomerular filtration rate. N. Engl. J. Med. 2006, 354, 2473–2483. [Google Scholar] [CrossRef] [PubMed]
- Pierce, C.B.; Muñoz, A.; Ng, D.K.; Warady, B.A.; Furth, S.L.; Schwartz, G.J. Age- and sex-dependent clinical equations to estimate glomerular filtration rates in children and young adults with chronic kidney disease. Kidney Int. 2021, 99, 948–956. [Google Scholar] [CrossRef]
- Serafinelli, J.; Mastrangelo, A.; Morello, W.; Cerioni, V.F.; Salim, A.; Nebuloni, M.; Montini, G. Kidney involvement and histological findings in two pediatric COVID-19 patients. Pediatr. Nephrol. 2021, 36, 3789–3793. [Google Scholar] [CrossRef]
- Stewart, D.J.; Hartley, J.C.; Johnson, M.; Marks, S.D.; du Pré, P.; Stojanovic, J. Renal dysfunction in hospitalised children with COVID-19. Lancet Child Adolesc. Health 2020, 4, e28–e29. [Google Scholar] [CrossRef] [PubMed]
- Alvarado, A.; Franceschi, G.; Resplandor, E.; Sumba, J.; Orta, N. COVID-19 associated with onset nephrotic syndrome in a pediatric patient: Coincidence or related conditions? Pediatr. Nephrol. 2021, 36, 205–207. [Google Scholar] [CrossRef]
- Shah, S.A.; Carter, H.P. New-Onset Nephrotic Syndrome in a Child Associated With COVID-19 Infection. Front. Pediatr. 2020, 8, 471. [Google Scholar] [CrossRef] [PubMed]
- Morreale, A.; Casciana, M.L. Onset of nephrotic syndrome concomitant to SARS-CoV-2 infection in a 3-year-old child. Pediatr. Nephrol. 2022, 37, 225. [Google Scholar] [CrossRef]
- Morgan, K.M.; Imani, P.D. Case report: A 5-year-old with new onset nephrotic syndrome in the setting of COVID-19 infection. BMC Nephrol. 2021, 22, 323. [Google Scholar] [CrossRef] [PubMed]
- Basalely, A.; Brathwaite, K.; Duong, M.D.; Liu, D.; Mazo, A.; Xie, Y.; Del Rio, M.; Goilav, B.; Hayde, N.; Kaskel, F.J.; et al. COVID-19 in Children With Kidney Disease: A Report of 2 Cases. Kidney Med. 2021, 3, 120–123. [Google Scholar] [CrossRef]
- Enya, T.; Morimoto, Y.; Oshima, R.; Miyazaki, K.; Miyazawa, T.; Okada, M.; Sugimoto, K. Nephrotic syndrome relapse in a boy with COVID-19. CEN Case Rep. 2021, 10, 431–434. [Google Scholar] [CrossRef]
- Basiratnia, M.; Derakhshan, D.; Yeganeh, B.S.; Derakhshan, A. Acute necrotizing glomerulonephritis associated with COVID-19 infection: Report of two pediatric cases. Pediatr. Nephrol. 2021, 36, 1019–1023. [Google Scholar] [CrossRef]
- Fireizen, Y.; Shahriary, C.; Imperial, M.E.; Randhawa, I.; Nianiaris, N.; Ovunc, B. Pediatric P-ANCA vasculitis following COVID-19. Pediatr. Pulmonol. 2021, 56, 3422–3424. [Google Scholar] [CrossRef]
- Isoldi, S.; Mallardo, S.; Marcellino, A.; Bloise, S.; Dilillo, A.; Iorfida, D.; Testa, A.; Del Giudice, E.; Martucci, V.; Sanseviero, M.; et al. The comprehensive clinic, laboratory, and instrumental evaluation of children with COVID-19, A 6-months prospective study. J. Med. Virol. 2021, 93, 3122–3132. [Google Scholar] [CrossRef]
- Dike, A.I.; Okechukwu, A.A.; Ocheke, I.; Airede, K.I. Asymptomatic Proteinuria and Haematuria in Healthy Public Primary School Children in Abuja, Nigeria. West Afr. J. Med. 2021, 38, 8–14. [Google Scholar] [PubMed]
- Chen, M.-C.; Wang, J.-H.; Chu, C.-H.; Cheng, C.-F. Differential prevalence of hematuria and proteinuria with socio-demographic factors among school children in Hualien, Taiwan. Pediatr. Neonatol. 2018, 59, 360–367. [Google Scholar] [CrossRef] [PubMed]
- Jafar, T.H.; Chaturvedi, N.; Hatcher, J.; Khan, I.; Rabbani, A.; Khan, A.Q.; Portman, R.; Schmid, C.H.; Levey, A.S. Proteinuria in South Asian children: Prevalence and determinants. Pediatr. Nephrol. 2005, 20, 1458–1465. [Google Scholar] [CrossRef]
- Hothan, K.A.; Alasmari, B.A.; Alkhelaiwi, O.K.; Althagafi, K.M.; Alkhaldi, A.A.; Alfityani, A.K.; Aladawi, M.M.; Sharief, S.N.; El Desoky, S.; Kari, J.A. Prevalence of hypertension, obesity, hematuria and proteinuria amongst healthy adolescents living in Western Saudi Arabia. Saudi Med. J. 2016, 37, 1120–1126. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, M.; Roy, D.; Lingeswaran, M.; Tomo, S.; Mittal, A.; Varma, P.P. Urinary Screening in Asymptomatic Indian Children: A Cross Sectional Epidemiological Study. EJIFCC 2022, 33, 242–251. [Google Scholar]
- Larkins, N.; Teixeira-Pinto, A.; Craig, J. The population-based prevalence of albuminuria in children. Pediatr. Nephrol. 2017, 32, 2303–2309. [Google Scholar] [CrossRef]
- Diao, B.; Wang, C.; Wang, R.; Feng, Z.; Zhang, J.; Yang, H.; Tan, Y.; Wang, H.; Wang, C.; Liu, L.; et al. Human kidney is a target for novel severe acute respiratory syndrome coronavirus 2 infection. Nat. Commun. 2021, 12, 2506. [Google Scholar] [CrossRef]
- Martinez-Rojas, M.A.; Vega-Vega, O.; Bobadilla, N.A. Is the kidney a target of SARS-CoV-2? Am. J. Physiol. Renal Physiol. 2020, 318, F1454–F1462. [Google Scholar] [CrossRef]
- Khairwa, A.; Jat, K.R. Autopsy findings of COVID-19 in children: A systematic review and meta-analysis. Forensic Sci. Med. Pathol. 2022, 18, 516–529. [Google Scholar] [CrossRef]
- Park, H.S.; Kim, S.; Lee, C.S.; Byeon, S.H.; Kim, S.S.; Lee, S.W.; Kim, Y.J. Retinal vascular occlusion risks during the COVID-19 pandemic and after SARS-CoV-2 infection. Sci. Rep. 2023, 13, 16851. [Google Scholar] [CrossRef]
- Hamming, I.; Timens, W.; Bulthuis, M.L.C.; Lely, A.T.; Navis, G.J.; van Goor, H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J. Pathol. 2004, 203, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Cristiani, L.; Mancino, E.; Matera, L.; Nenna, R.; Pierangeli, A.; Scagnolari, C.; Midulla, F. Will children reveal their secret? The coronavirus dilemma. Eur. Respir. J. 2020, 55, 2000749. [Google Scholar] [CrossRef]
- Puelles, V.G.; Lütgehetmann, M.; Lindenmeyer, M.T.; Sperhake, J.P.; Wong, M.N.; Allweiss, L.; Chilla, S.; Heinemann, A.; Wanner, N.; Liu, S.; et al. Multiorgan and Renal Tropism of SARS-CoV-2. N. Engl. J. Med. 2020, 383, 590–592. [Google Scholar] [CrossRef] [PubMed]
- Su, H.; Yang, M.; Wan, C.; Yi, L.-X.; Tang, F.; Zhu, H.-Y.; Yi, F.; Yang, H.C.; Fogo, A.B.; Nie, X.; et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020, 98, 219–227. [Google Scholar] [CrossRef]
- Sharma, P.; Uppal, N.N.; Wanchoo, R.; Shah, H.H.; Yang, Y.; Parikh, R.; Khanin, Y.; Madireddy, V.; Larsen, C.P.; Jhaveri, K.D.; et al. COVID-19-Associated Kidney Injury: A Case Series of Kidney Biopsy Findings. J. Am. Soc. Nephrol. 2020, 31, 1948–1958. [Google Scholar] [CrossRef]
- Al Rumaihi, K.; Khalafalla, K.; Arafa, M.; Nair, A.; Al Bishawi, A.; Fino, A.; Sirtaj, F.; Ella, M.K.; ElBardisi, H.; Khattab, M.A.; et al. COVID-19 and renal involvement: A prospective cohort study assessing the impact of mild SARS-CoV-2 infection on the kidney function of young healthy males. Int. Urol. Nephrol. 2023, 55, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Chen, I.-W.; Chang, L.-C.; Ho, C.-N.; Wu, J.-Y.; Tsai, Y.-W.; Lin, C.-M.; Chang, Y.J.; Hung, K.C. Association between COVID-19 and the development of chronic kidney disease in patients without initial acute kidney injury. Sci. Rep. 2025, 15, 10924. [Google Scholar] [CrossRef]
- Brenner, B.M. Nephron adaptation to renal injury or ablation. Am. J. Physiol. 1985, 249 Pt 2, F324–F337. [Google Scholar] [CrossRef]
- Anderson, S.; Brenner, B.M. The role of intraglomerular pressure in the initiation and progression of renal disease. J. Hypertens. Suppl. 1986, 4, S236–S238. [Google Scholar]
- Neuringer, J.R.; Brenner, B.M. Hemodynamic theory of progressive renal disease: A 10-year update in brief review. Am. J. Kidney Dis. 1993, 22, 98–104. [Google Scholar] [CrossRef]
- Neuringer, J.R.; Brenner, B.M. Glomerular hypertension: Cause and consequence of renal injury. J. Hypertens. Suppl. 1992, 10, S91–S97. [Google Scholar] [CrossRef] [PubMed]
- Ye, Q.; Wang, B.; Mao, J. The pathogenesis and treatment of the ‘Cytokine Storm’ in COVID-19. J. Infect. 2020, 80, 607–613. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.; Lee, J.; Lee, J.H. Kidney involvement in children during the SARS-CoV-2 Omicron variant pandemic. BMC Pediatr. 2023, 23, 491. [Google Scholar] [CrossRef]
- Chagnac, A.; Zingerman, B.; Rozen-Zvi, B.; Herman-Edelstein, M. Consequences of Glomerular Hyperfiltration: The Role of Physical Forces in the Pathogenesis of Chronic Kidney Disease in Diabetes and Obesity. Nephron 2019, 143, 38–42. [Google Scholar] [CrossRef]
- Morello, W.; Vianello, F.A.; Proverbio, E.; Peruzzi, L.; Pasini, A.; Montini, G. COVID-19 and idiopathic nephrotic syndrome in children: Systematic review of the literature and recommendations from a highly affected area. Pediatr. Nephrol. 2022, 37, 757–764. [Google Scholar] [CrossRef]
- Lubrano, R.; Villani, A.; Berrettini, S.; Caione, P.; Chiara, A.; Costantino, A.; Formigari, R.; Franzoni, E.; Gattinara, G.C.; Giustardi, A.; et al. Point of view of the Italians pediatric scientific societies about the pediatric care during the COVID-19 lockdown: What has changed and future prospects for restarting. Ital. J. Pediatr. 2020, 46, 142. [Google Scholar] [CrossRef]
- Borrego-Moreno, J.C.; Cárdenas-de Luna, M.J.; Márquez-Castillo, J.C.; Reyes-Ruiz, J.M.; Osuna-Ramos, J.F.; León-Juárez, M.; Del Ángel, R.M.; Rodríguez-Carlos, A.; Rivas-Santiago, B.; Farfan-Morales, C.N.; et al. Acute Kidney Injury in the Context of COVID-19: An Analysis in Hospitalized Mexican Patients. Infect. Dis. Rep. 2024, 16, 458–471. [Google Scholar] [CrossRef]
- Wu, H.H.L.; Shenoy, M.; Kalra, P.A.; Chinnadurai, R. Intrinsic Kidney Pathology in Children and Adolescents Following COVID-19 Vaccination: A Systematic Review. Children 2022, 9, 1467. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Lauber, C.; Hänzelmann, S.; Schunk, S.; Petersen, E.L.; Alabdo, A.; Lindenmeyer, M.; Hausmann, F.; Kuta, P.; Renné, T.; Twerenbold, R.; et al. Kidney outcome after mild to moderate COVID-19. Nephrol. Dial. Transplant. 2023, 38, 2031–2040. [Google Scholar] [CrossRef]
- Baek, H.S.; Cho, M.H. Kidney complications associated with COVID-19 infection and vaccination in children and adolescents: A brief review. Clin. Exp. Pediatr. 2023, 66, 424–431. [Google Scholar] [CrossRef]
- Rai, V. COVID-19 and Kidney: The Importance of Follow-Up and Long-Term Screening. Life 2023, 13, 2137. [Google Scholar] [CrossRef]

| Demographics | ||
|---|---|---|
| Male | N (%) | 90 (60.8%) |
| Female | N (%) | 58 (39.2%) |
| Age (years) | mean ± SD | 10.1 ± 4.2 |
| Weight (percentile) | median (IQR) | 60.0 (49.8) |
| Height (percentile) | median (IQR) | 43.5 (52.8) |
| BMI (percentile) | median (IQR) | 71.5 (48.8) |
| Renal Function | ||
| GFR (ml/min/1.73 m2) | median (IQR) | 132.3 (71.5) |
| Creatinine (blood, mg/dL) | median (IQR) | 0.55 (0.15) |
| Creatinine (urine, mg/dL) | median (IQR) | 92.8 (63.4) |
| FENa (%) | median (IQR) | 0.5 (0.3) |
| TRP (%) | median (IQR) | 90.0 (3.8) |
| Proteinuria (mg/m2/day) | median (IQR) | 107.0 (59.8) |
| PrU/CrU | median (IQR) | 0.17 (0.12) |
| CaU/CrU | median (IQR) | 0.09 (0.11) |
| Hematuria (cells/μL) | median (IQR) | 2.5 (4.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marcellino, A.; Bloise, S.; Pirone, C.; Brandino, G.; Barberi, A.; Del Giudice, E.; Martucci, V.; Sanseviero, M.; Ventriglia, F.; Lubrano, R. Increased Measured GFR and Proteinuria in Children with Previous Infection by SARS-CoV-2: Should We Be Concerned? Microorganisms 2025, 13, 1008. https://doi.org/10.3390/microorganisms13051008
Marcellino A, Bloise S, Pirone C, Brandino G, Barberi A, Del Giudice E, Martucci V, Sanseviero M, Ventriglia F, Lubrano R. Increased Measured GFR and Proteinuria in Children with Previous Infection by SARS-CoV-2: Should We Be Concerned? Microorganisms. 2025; 13(5):1008. https://doi.org/10.3390/microorganisms13051008
Chicago/Turabian StyleMarcellino, Alessia, Silvia Bloise, Carmelo Pirone, Giulia Brandino, Antonio Barberi, Emanuela Del Giudice, Vanessa Martucci, Mariateresa Sanseviero, Flavia Ventriglia, and Riccardo Lubrano. 2025. "Increased Measured GFR and Proteinuria in Children with Previous Infection by SARS-CoV-2: Should We Be Concerned?" Microorganisms 13, no. 5: 1008. https://doi.org/10.3390/microorganisms13051008
APA StyleMarcellino, A., Bloise, S., Pirone, C., Brandino, G., Barberi, A., Del Giudice, E., Martucci, V., Sanseviero, M., Ventriglia, F., & Lubrano, R. (2025). Increased Measured GFR and Proteinuria in Children with Previous Infection by SARS-CoV-2: Should We Be Concerned? Microorganisms, 13(5), 1008. https://doi.org/10.3390/microorganisms13051008






