Integrating Statistical and Machine-Learning Approaches for Salmonella enterica Surveillance in Northwestern Italy: A One Health Data-Driven Framework
Abstract
1. Introduction
- (1)
- Which temporal, spatial, and food-chain factors have influenced Salmonella contamination in food matrices from Piedmont during the 2013–2023 surveillance period?
- (2)
- To what extent did environmental factors—particularly temperature and relative humidity—modulate this risk within the regional context?
- (3)
- Can integrating official surveillance and climatic data through both inferential and ML frameworks enhance contamination-risk prediction and guide targeted prevention strategies?
2. Materials and Methods
2.1. Data Sources and Data Management
2.2. Datasets and Variable Recoding
2.2.1. Exploratory Data Processing
2.2.2. Modelling and Prediction Phase Using Machine Learning (ML)
2.3. Statistical Analyses
2.3.1. Exploratory and Inferential Analysis
2.3.2. Predictive Modelling Using Extreme Gradient Boosting (XGBoost)
- (a)
- Learning, testing, and validation strategy
- (b)
- Hyperparameter optimisation and final model
- (c)
- Model calibration
- (d)
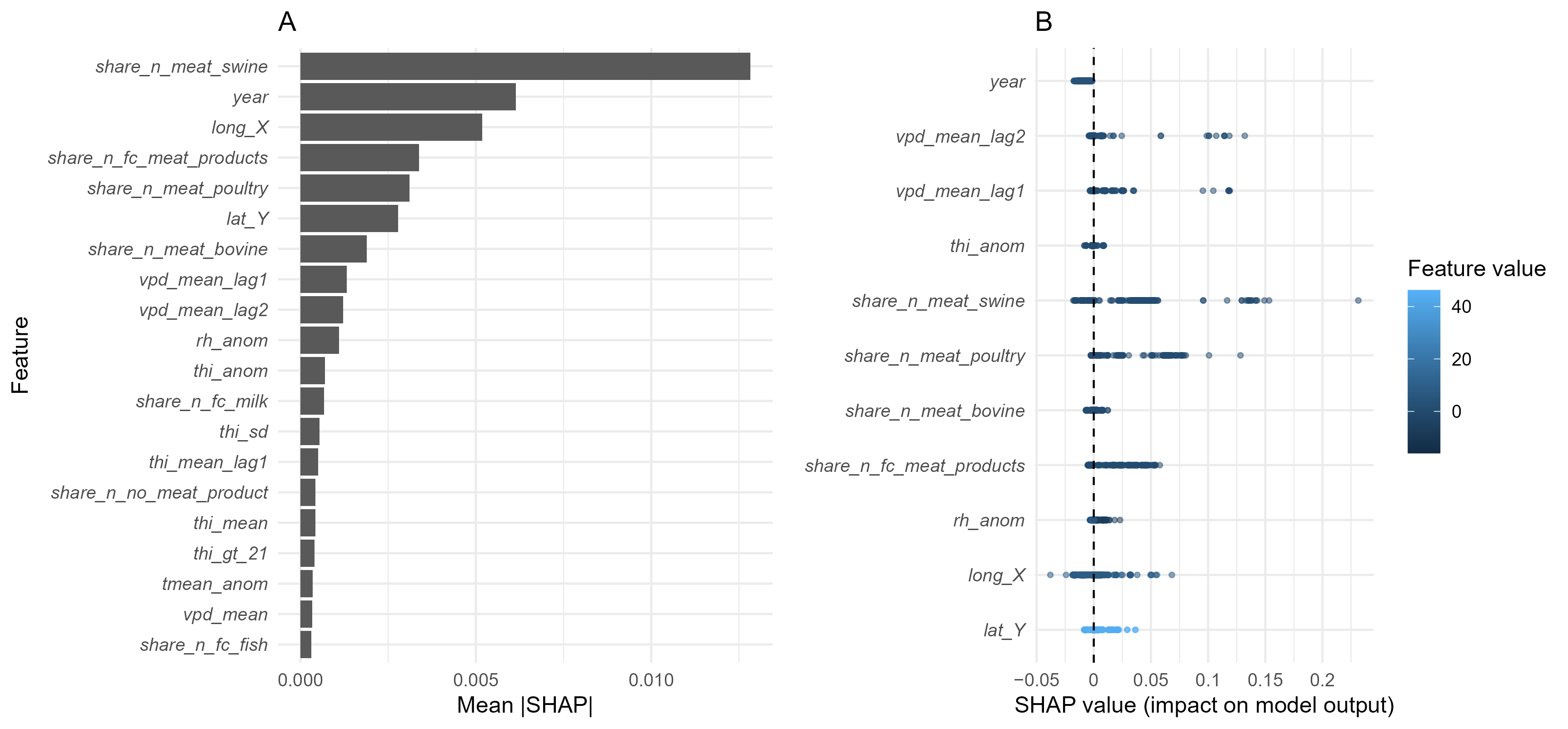
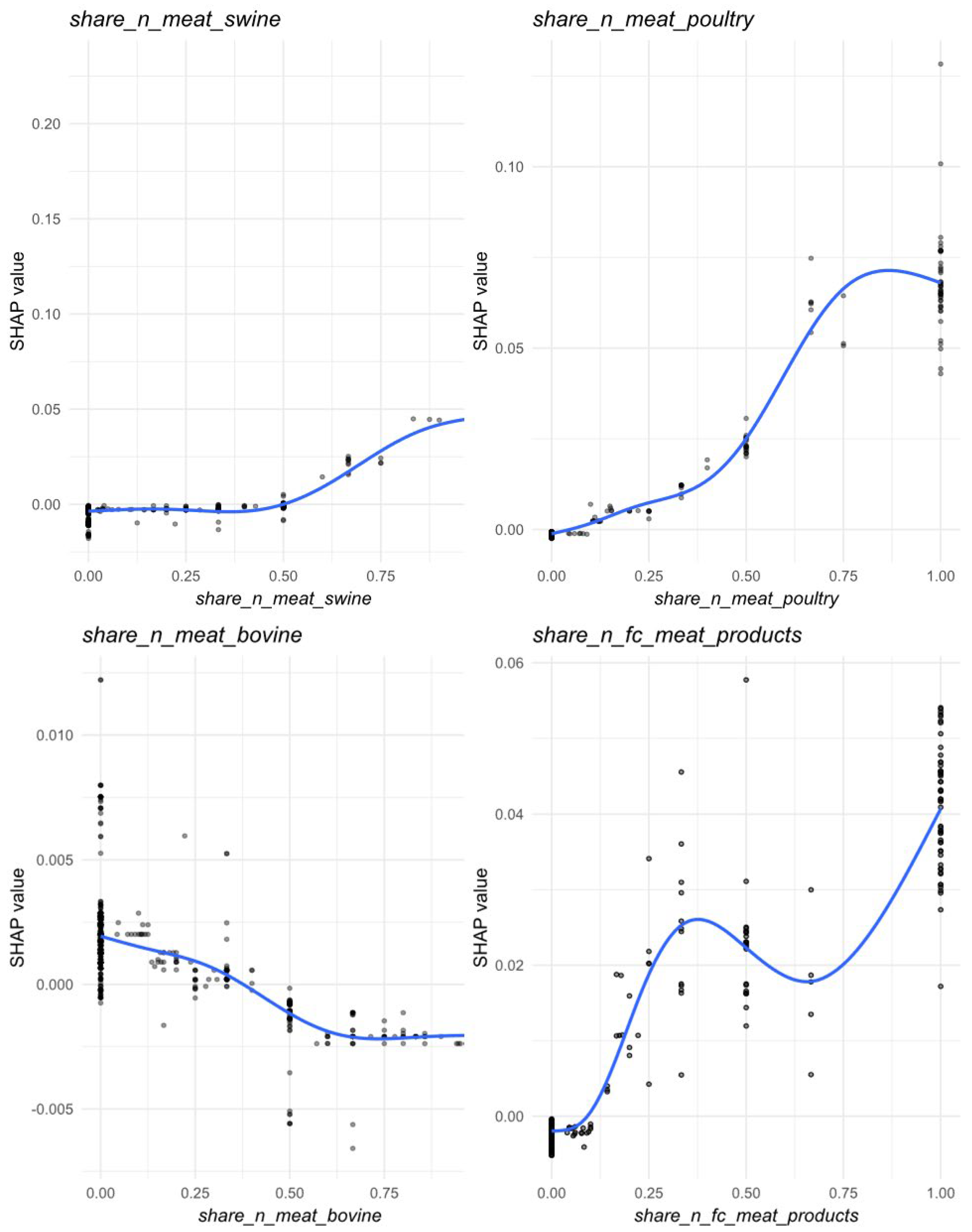
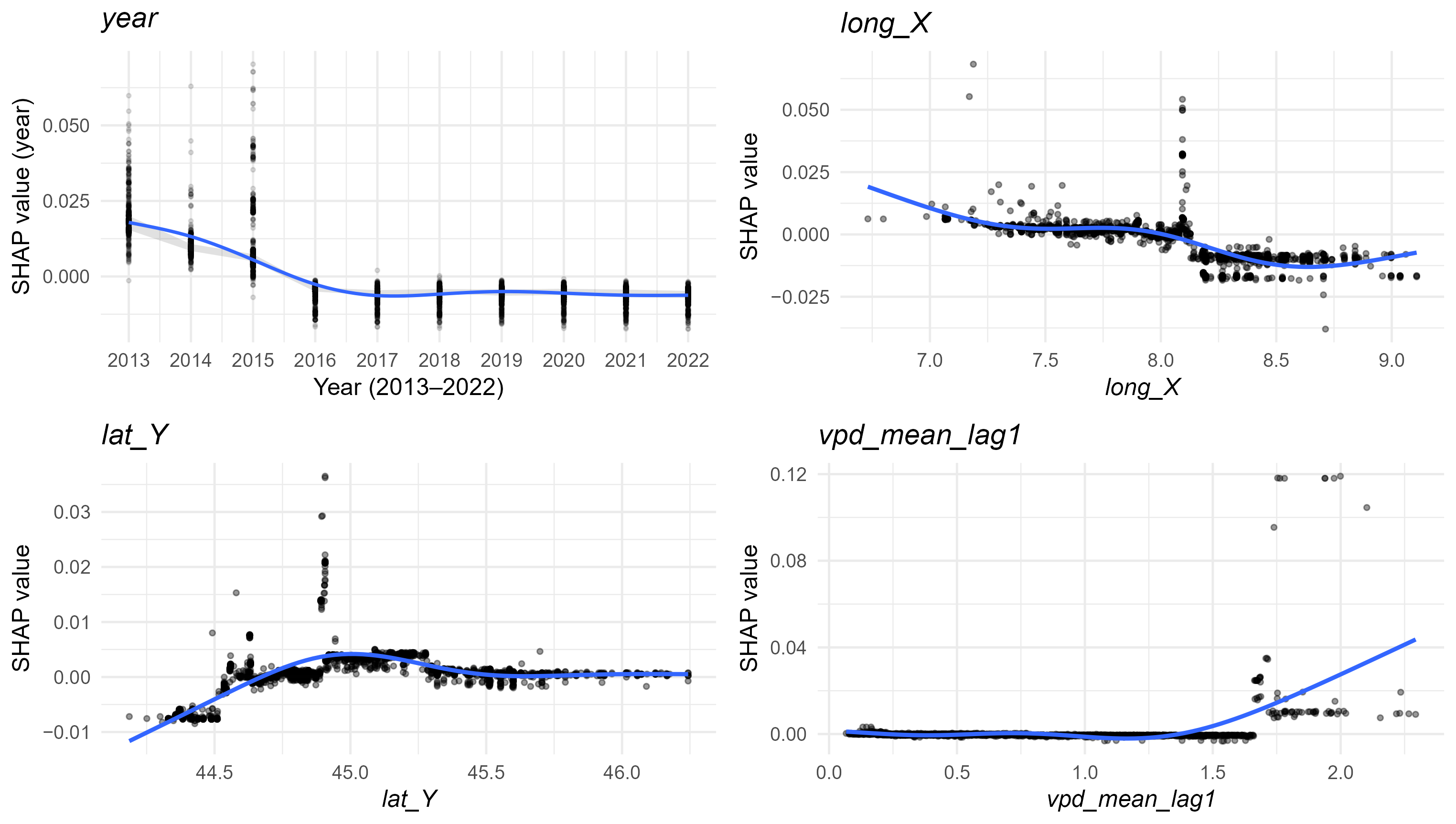
- Model interpretation
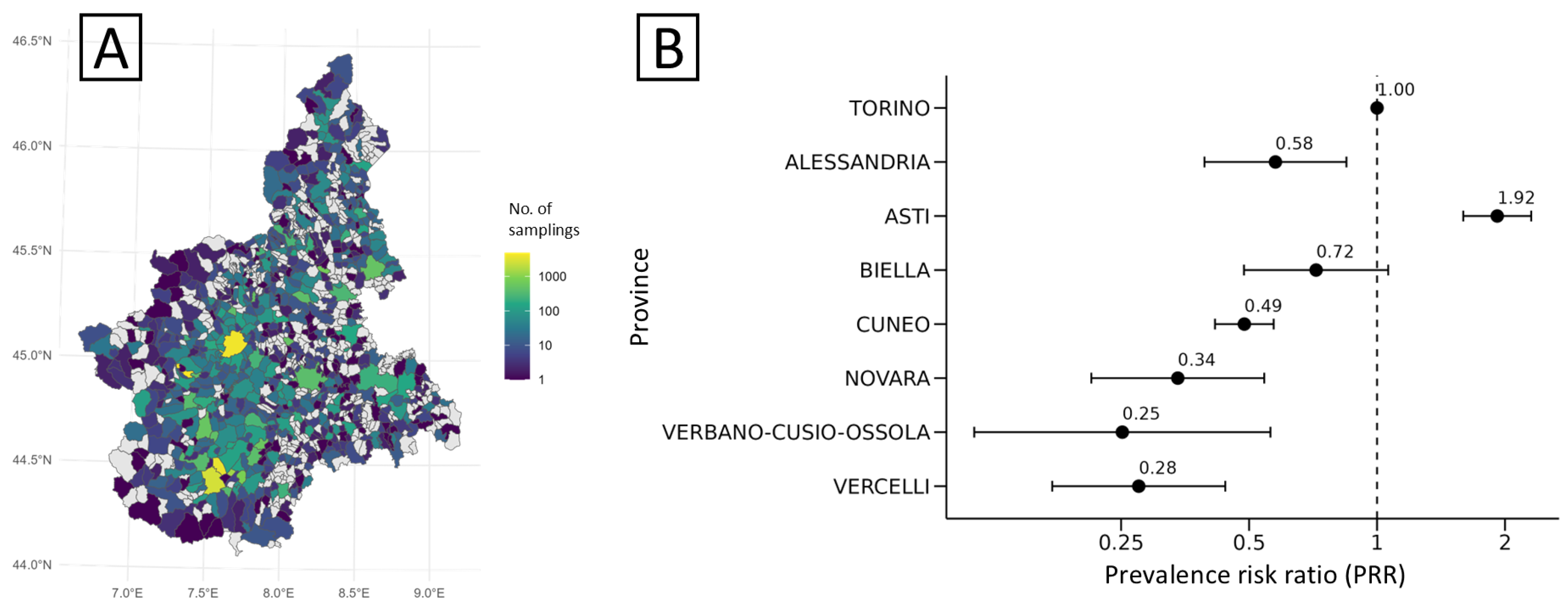
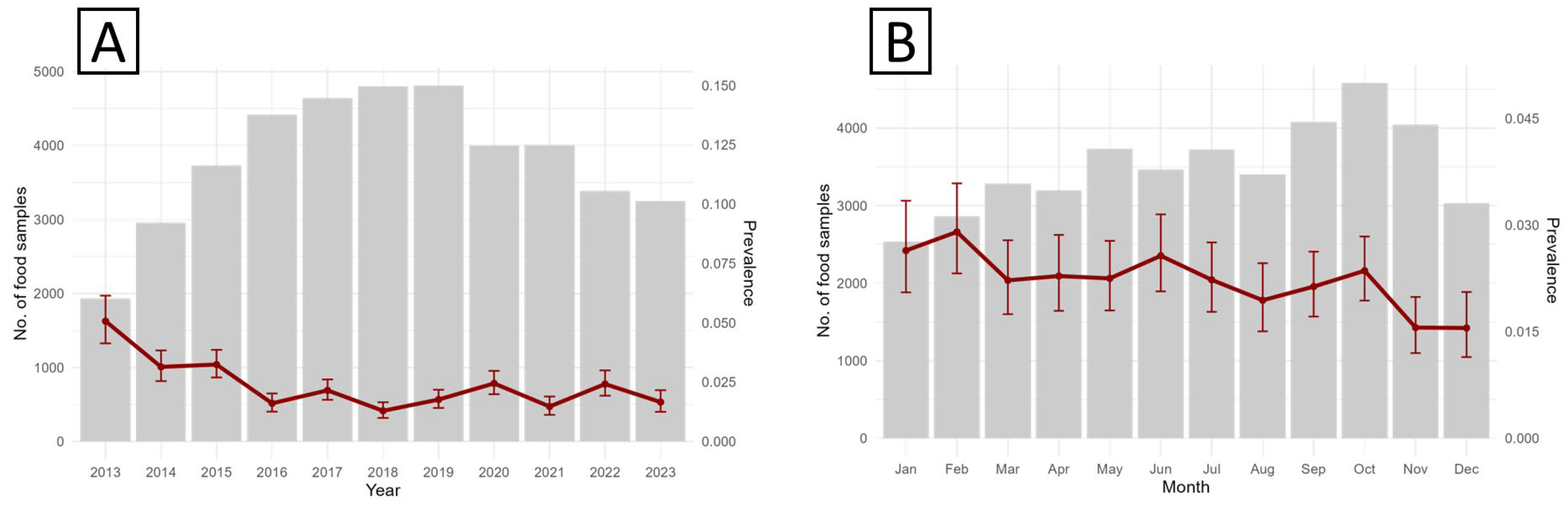
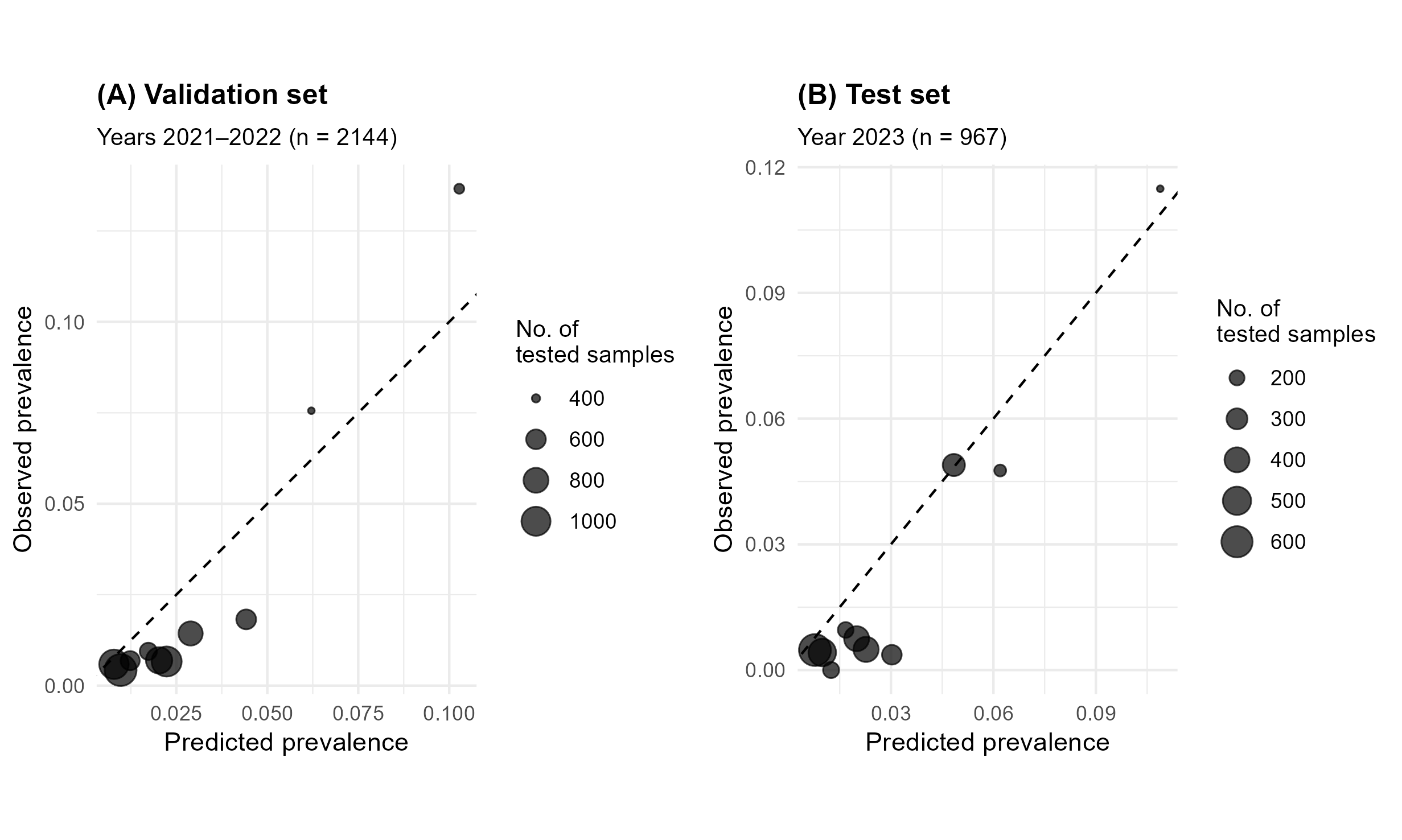
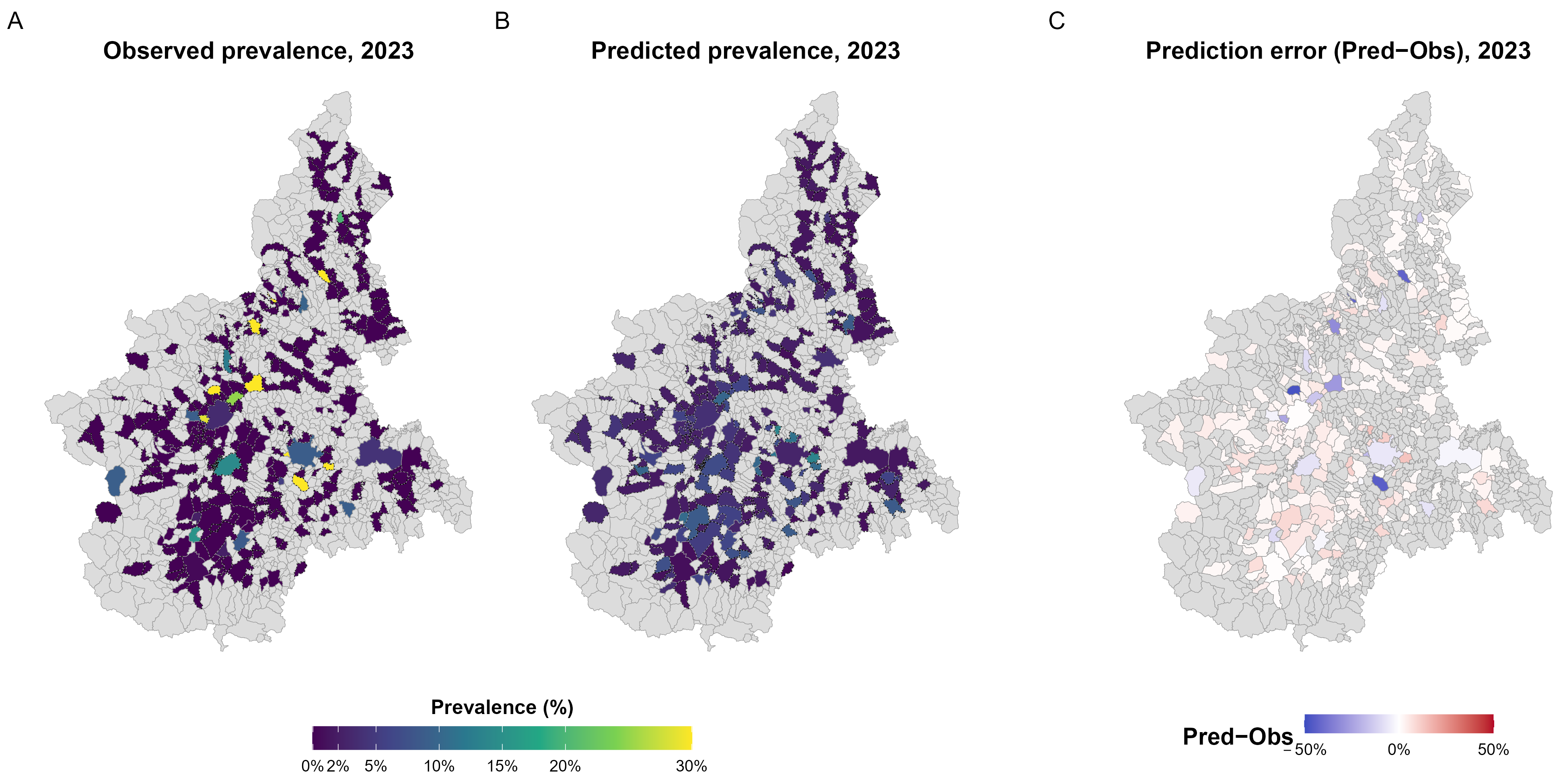
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Majowicz, S.E.; Musto, J.; Scallan, E.; Angulo, F.J.; Kirk, M.; O’Brien, S.J.; Jones, T.F.; Fazil, A.; Hoekstra, R.M.; International Collaboration on Enteric Disease ‘Burden of Illness’ Studies. The global burden of nontyphoidal Salmonella gastroenteritis. Clin. Infect. Dis. 2010, 50, 882–889. [Google Scholar] [CrossRef]
- Sanni, A.O.; Onyango, J.; Rota, A.F.; Mikecz, O.; Usman, A.; PicaCiamarra, U.; Fasina, F.O. Underestimated economic and social burdens of non-Typhoidal Salmonella infections: The One Health perspective from Nigeria. One Health 2023, 16, 100546. [Google Scholar] [CrossRef]
- World Health Organization. Estimating the Burden of Foodborne Diseases. Available online: https://www.who.int/activities/estimating-the-burden-of-foodborne-diseases (accessed on 1 November 2025).
- Silva, C.; Calva, E.; Maloy, S. One Health and Food-Borne Disease: Salmonella Transmission between Humans, Animals, and Plants. Microbiol. Spectr. 2014, 2, 137–148. [Google Scholar] [CrossRef]
- Liu, H.; Whitehouse, C.A.; Li, B. Presence and Persistence of Salmonella in Water: The Impact on Microbial Quality of Water and Food Safety. Front. Public Health 2018, 6, 159. [Google Scholar] [CrossRef] [PubMed]
- Rocha, A.D.L.; Ferrari, R.G.; Pereira, W.E.; Lima, L.A.; Givisiez, P.E.N.; Moreno-Switt, A.I.; Toro, M.; Delgado-Suárez, E.J.; Meng, J.; Oliveira, C.J.B. Revisiting the Biological Behavior of Salmonella enterica in Hydric Resources: A Meta-Analysis Study Addressing the Critical Role of Environmental Water on Food Safety and Public Health. Front. Microbiol. 2022, 13, 802625. [Google Scholar] [CrossRef]
- Hilbert, F.; Smulders, F.J.M.; Chopra-Dewasthaly, R.; Paulsen, P. Salmonella in the wildlife-human interface. Food Res. Int. 2012, 45, 603–608. [Google Scholar] [CrossRef]
- Wigley, P. Salmonella and Salmonellosis in Wild Birds. Animals 2024, 14, 3533. [Google Scholar] [CrossRef]
- European Food Safety Authority (EFSA); European Centre for Disease Prevention and Control (ECDC). The European Union One Health 2019 Zoonoses Report. EFSA J. 2021, 19, e06406. [Google Scholar] [CrossRef]
- European Food Safety Authority (EFSA); European Centre for Disease Prevention and Control (ECDC). The European Union One Health 2023 Zoonoses report. EFSA J. 2024, 22, e9106. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control (ECDC). Assessing the Potential Impacts of Climate Change on Food- and Waterborne Diseases in Europe; ECDC: Stockholm, Sweden, 2012. [Google Scholar] [CrossRef]
- Akil, L.; Ahmad, H.A.; Reddy, R.S. Effects of climate change on Salmonella infections. Foodborne Pathog. Dis. 2014, 11, 974–980. [Google Scholar] [CrossRef] [PubMed]
- Morgado, M.E.; Jiang, C.; Zambrana, J.; Upperman, C.R.; Mitchell, C.; Boyle, M.; Sapkota, A.R.; Sapkota, A. Climate change, extreme events, and increased risk of salmonellosis: Foodborne diseases active surveillance network (FoodNet), 2004–2014. Environ. Health 2021, 20, 105. [Google Scholar] [CrossRef]
- Kovats, R.S.; Edwards, S.J.; Hajat, S.; Armstrong, B.G.; Ebi, K.L.; Menne, B. The effect of temperature on food poisoning: A time-series analysis of salmonellosis in ten European countries. Epidemiol. Infect. 2004, 132, 443–453. [Google Scholar] [CrossRef]
- World Health Organization. Climate Change: Linking Health and Food Safety; WHO: Geneva, Switzerland, 2018; Available online: https://cdn.who.int/media/docs/default-source/food-safety/climate-change.pdf (accessed on 9 November 2025).
- Rupasinghe, R.; Chomel, B.B.; Martínez-López, B. Climate change and zoonoses: A review of the current status, knowledge gaps, and future trends. Acta Trop. 2022, 226, 106225. [Google Scholar] [CrossRef] [PubMed]
- Salmonella: Enter-Vet. Available online: https://www.izsvenezie.it/temi/malattie-patogeni/salmonella/enter-vet/ (accessed on 9 November 2025).
- Enter-Net Italia: Enteric Pathogen Network. Available online: https://enternet.iss.it/ (accessed on 9 November 2025).
- Zinsstag, J.; Schelling, E.; Waltner-Toews, D.; Tanner, M. From “one medicine” to “one health” and systemic approaches to health and well-being. Prev. Vet. Med. 2011, 101, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Iannetti, S.; Malizia, E.; Sorgente, A.; Ricci, A.; Cibin, V.; Colangeli, P. The Integrated Management System for Salmonella Control Plan in Italy. J. Health Med. Informat. 2015, 6, 4. [Google Scholar] [CrossRef]
- Filippetti, S.; Bonetta, S.; Pignata, C.; Zaccaria, T.; Bondi, A.; Marro, S.; Sattanino, G.; Griglio, B.; Carraro, E. Integrated surveillance of foodborne diseases: The organization of the Piemonte region (Italy). Popul. Med. 2023, 5, A1926. [Google Scholar] [CrossRef]
- Nzietchueng, S.; Kitua, A.; Nyatanyi, T.; Rwego, I.B. Facilitating implementation of the one health approach: A definition of a one health intervention. One Health 2023, 16, 100491. [Google Scholar] [CrossRef]
- Tast Lahti, E.; Karamehmedovic, N.; Riedel, H.; Blom, L.; Boel, J.; Delibato, E.; Denis, M.; van Essen-Zandbergen, A.; Garcia-Fernandez, A.; Hendriksen, R.; et al. One Health surveillance—A cross-sectoral detection, characterization, and notification of foodborne pathogens. Front. Public Health 2023, 11, 1129083. [Google Scholar] [CrossRef]
- Arredondo-Rivera, M.; Barois, Z.; Monti, G.E.; Steketee, J.; Daburon, A. Bridging Food Systems and One Health: A key to preventing future pandemics? One Health 2024, 18, 100727. [Google Scholar] [CrossRef] [PubMed]
- One Health High-Level Expert Panel (OHHLEP); Hayman, D.T.S.; Adisasmito, W.B.; Almuhairi, S.; Behravesh, C.B.; Bilivogui, P.; Bukachi, S.A.; Casas, N.; Becerra, N.C.; Charron, D.F.; et al. Developing One Health surveillance systems. One Health 2023, 17, 100617. [Google Scholar] [CrossRef]
- Food and Agriculture Organization of the United Nations (FAO); United Nations Environment Programme (UNEP); World Health Organisation (WHO); World Organisation for Animal Health (WOAH). One Health Joint Plan of Action (2022–2026). Working Together for the Health of Humans, Animals, Plants and the Environment; FAO: Rome, Italy; UNEP: Nairobi, Kenya; WHO: Geneva, Switzerland; WOAH: Paris, France, 2022. [Google Scholar] [CrossRef]
- Kim, J.H.; Koo, J.Y.; Kim, J.S.; Om, A.S. Role of Artificial Intelligence (AI) and Machine Learning (ML) in Food Safety and Quality Improvement. Food Suppl. Biomater. Health 2025, 5, e11. [Google Scholar] [CrossRef]
- Hamidy, S.M.; Erik, A.; Kuvvetli, Y.; Gökşen, G. Chapter 31: Artificial intelligence and machine learning for food safety and traceability. In Artificial Intelligence in Food Science, Transforming Food and Bioprocess Development; Academic Press: Cambridge, MA, USA, 2025; pp. 589–609. [Google Scholar] [CrossRef]
- Hartman, J. Predictive Models for Food Code Violations. Food Prot. Trends 2020, 40, 56–65. [Google Scholar]
- Wang, X.; Bouzembrak, Y.; Lansink, A.O.; van der Fels-Klerx, H.J. Application of machine learning to the monitoring and prediction of food safety: A review. Compr. Rev. Food Sci. Food Saf. 2022, 21, 416–434. [Google Scholar] [CrossRef]
- Sari, O.F.; Bader-El-Den, M.; Leadley, C.; Esmeli, R.; Mohasseb, A.; Ince, V. AI-driven food safety risk prediction: A transformer-based approach with RASFF database. Br. Food J. 2025, 127, 3427–3445. [Google Scholar] [CrossRef]
- Gottschald, M. Advancing food safety through digital traceability, interoperability, harmonized data and collaborative partnerships. J. Consum. Prot. Food Saf. 2024, 19, 257–258. [Google Scholar] [CrossRef]
- European Food Safety Authority (EFSA). Programming Document 2024–2026. In Science, Safe food, Sustainability; Publications Office of the European Union: Luxembourg, 2024. [Google Scholar] [CrossRef]
- European Commission Joint Research Centre; Tóth, K.; Acs, S.; Aschberger, K.; Barbero Vignola, G.; Bopp, S.; Caivano, A.; Catarino, R.; Dominguez Torreiro, M.; Druon, J.; et al. EU Food System Monitoring Framework, From Concepts to Indicators; Publications Office of the European Union: Luxembourg, 2024; p. JRC137971. [Google Scholar] [CrossRef]
- European Parliament. Regulation (EU) 2022/868 of the European Parliament and of the Council of 30 May 2022 on European data governance and amending Regulation (EU) 2018/1724. Off. J. Eur. Union 2022, 152, 1–44. [Google Scholar]
- European Food Safety Authority (EFSA). EFSA Strategy 2027 Mid-Term Review; Publications Office of the European Union: Luxembourg, 2025. [Google Scholar]
- Wheeler, N.E. Tracing outbreaks with machine learning. Nat. Rev. Microbiol. 2019, 17, 269. [Google Scholar] [CrossRef]
- Wang, H.; Cui, W.; Guo, Y.; Du, Y.; Zhou, Y. Machine Learning Prediction of Foodborne Disease Pathogens: Algorithm Development and Validation Study. JMIR Med. Inform. 2021, 9, e24924. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Cui, W.; Wang, H.; Du, Y.; Zhou, Y. High-Efficiency Machine Learning Method for Identifying Foodborne Disease Outbreaks and Confounding Factors. Foodborne Pathog. Dis. 2021, 18, 590–598. [Google Scholar] [CrossRef]
- Tao, D.; Zhang, D.; Hu, R.; Rundensteiner, E.; Feng, H. Crowdsourcing and machine learning approaches for extracting entities indicating potential foodborne outbreaks from social media. Sci. Rep. 2021, 11, 21678. [Google Scholar] [CrossRef] [PubMed]
- Liu, N.; Bouzembrak, Y.; van den Bulk, L.M.; Gavai, A.; van den Heuvel, L.J.; Marvin, H.J.P. Automated food safety early warning system in the dairy supply chain using machine learning. Food Control 2022, 136, 108872. [Google Scholar] [CrossRef]
- Zacher, B.; Czogiel, I. Supervised learning using routine surveillance data improves outbreak detection of Salmonella and Campylobacter infections in Germany. PLoS ONE 2022, 17, e0267510. [Google Scholar] [CrossRef]
- Nogales, A.; Díaz-Morón, R.; García-Tejedor, A. A comparison of neural and non-neural machine learning models for food safety risk prediction with European Union RASFF data. Food Control 2022, 134, 108697. [Google Scholar] [CrossRef]
- Zhong, J.; Sun, L.; Zuo, E.; Chen, C.; Chen, C.; Jiang, H.; Li, H.; Lv, X. An ensemble of AHP-EW and AE-RNN for food safety risk early warning. PLoS ONE 2023, 18, e0284144. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Vozmediano, A.; Maurella, C.; Ceballos, L.A.; Crescio, E.; Meo, R.; Martelli, W.; Pitti, M.; Lombardi, D.; Meloni, D.; Pasqualini, C.; et al. Machine learning approach as an early warning system to prevent foodborne Salmonella outbreaks in northwestern Italy. Vet. Res. 2024, 55, 72. [Google Scholar] [CrossRef] [PubMed]
- Salaris, S.; Ocagli, H.; Casamento, A.; Lanera, C.; Gregori, D. Foodborne Event Detection Based on Social Media Mining: A Systematic Review. Foods 2025, 14, 239. [Google Scholar] [CrossRef]
- Constenla-Villoslada, S.; Liu, Y.; McBride, L.; Ouma, C.; Mutanda, N.; Barrett, C.B. High-frequency monitoring enables machine learning-based forecasting of acute child malnutrition for early warning. Proc. Natl. Acad. Sci. USA 2025, 122, e2416161122. [Google Scholar] [CrossRef]
- Qin, K.; Dai, X.; Wu, L.; Gao, M. Spatiotemporal analysis and risk prediction of foodborne diseases based on meteorological risk factors: A case study of Wuxi city, China. BMC Infect. Dis. 2025, 25, 1206. [Google Scholar] [CrossRef]
- Sodagari, H.R.; Ghasemi, M.; Varga, C.; Habib, I. Machine Learning Prediction of Multidrug Resistance in Swine-Derived Campylobacter spp. Using United States Antimicrobial Resistance Surveillance Data (2013–2023). Vet. Sci. 2025, 12, 937. [Google Scholar] [CrossRef] [PubMed]
- Banicod, R.J.S.; Tabassum, N.; Jo, D.M.; Javaid, A.; Kim, Y.M.; Khan, F. Integration of Artificial Intelligence in Biosensors for Enhanced Detection of Foodborne Pathogens. Biosensors 2025, 15, 690. [Google Scholar] [CrossRef]
- ISO 6579:2002; Microbiology of food and animal feeding stuffs: Horizontal method for the detection of Salmonella spp. International Organization for Standardization: Geneva, Switzerland, 2002.
- ISO 6579-1:2017; Microbiology of the food chain: Horizontal method for the detection, enumeration and serotyping of Salmonella. International Organization for Standardization: Geneva, Switzerland, 2017.
- Copernicus Climate Change Service (2020): Agrometeorological Indicators from 1979 to Present Derived from Reanalysis. Copernicus Climate Change Service (C3S) Climate Data Store (CDS). Available online. Available online: https://cds.climate.copernicus.eu/datasets/sis-agrometeorological-indicators?tab=overview (accessed on 2 November 2025).
- Istituto Nazionale di Statistica. Sistema Informativo Territoriale delle Unità Amministrative e Statistiche (SITUAS). Available online: https://situas.istat.it/ (accessed on 2 November 2025).
- Kelly, C.; Bond, T. (Eds.) A Guide to Environmental Research on Animals; National Academy of Sciences: Washington, DC, USA, 1971; pp. 7–92. [Google Scholar]
- Deblais, L.; Helmy, Y.A.; Testen, A.; Vrisman, C.; Jimenez Madrid, A.M.; Kathayat, D.; Miller, S.A.; Rajashekara, G. Specific Environmental Temperature and Relative Humidity Conditions and Grafting Affect the Persistence and Dissemination of Salmonella enterica subsp. enterica Serotype Typhimurium in Tomato Plant Tissues. Appl. Environ. Microbiol. 2019, 85, e00403-19. [Google Scholar] [CrossRef] [PubMed]
- Bashir, A.; Lambert, P.A.; Stedman, Y.; Hilton, A.C. Combined Effect of Temperature and Relative Humidity on the Survival of Salmonella Isolates on Stainless Steel Coupons. Int. J. Environ. Res. Public. Health 2022, 19, 909. [Google Scholar] [CrossRef]
- Monteith, J.L.; Unsworth, M.H. Principles of Environmental Physics, 4th ed.; Elsevier Ltd.: London, UK, 2014. [Google Scholar] [CrossRef]
- Chen, T.; Guestrin, C. XGBoost: A scalable Tree Boosting System. arXiv 2016, arXiv:1603.02754. [Google Scholar] [CrossRef]
- Lundberg, S.; Lee, S.-I. A unified approach to interpreting model predictions. arXiv 2017, arXiv:1705.07874. [Google Scholar] [CrossRef]
- Chen, T.; He, T.; Benesty, M.; Khotilovich, V.; Tang, Y.; Cho, H.; Chen, K.; Mitchell, R.; Cano, I.; Zhou, T.; et al. xgboost: Extreme Gradient Boosting. R package version 3.2.0.0. 2025. Available online: https://github.com/dmlc/xgboost (accessed on 8 November 2025).
- Zanotti, M. On the retraining frequency of global forecasting models. arXiv 2025, arXiv:2505.00356v2. [Google Scholar]
- Khoshvaght, H.; Permala, R.R.; Razmjou, A.; Khiadani, M. A critical review on selecting performance evaluation metrics for supervised machine learning models in wastewater quality prediction. J. Environ. Chem. Eng. 2025, 13, 119675. [Google Scholar] [CrossRef]
- Chai, T.; Draxler, R.R. Root mean square error (RMSE) or mean absolute error (MAE)?—Arguments against avoiding RMSE in the literature. Geosci. Model. Dev. 2014, 7, 1247–1250. [Google Scholar] [CrossRef]
- Van Calster, B.; McLernon, D.J.; van Smeden, M.; Wynants, L.; Steyerberge, E.W. Calibration: The Achilles heel of predictive analytics. BMC Med. 2019, 17, 230. [Google Scholar] [CrossRef]
- Shaji, S.; Selvaraj, R.K.; Shanmugasundaram, R. Salmonella Infection in Poultry: A Review on the Pathogen and Control Strategies. Microorganisms 2023, 11, 2814. [Google Scholar] [CrossRef]
- Bonardi, S. Salmonella in the pork production chain and its impact on human health in the European Union. Epidemiol. Infect. 2017, 145, 1513–1526. [Google Scholar] [CrossRef]
- Zeng, H.; De Reu, K.; Gabriël, S.; Mattheus, W.; De Zutter, L.; Rasschaert, G. Salmonella prevalence and persistence in industrialized poultry slaughterhouses. Poult. Sci. 2021, 100, 100991. [Google Scholar] [CrossRef]
- Klaharn, K.; Pichpol, D.; Meeyam, T.; Harintharanon, T.; Lohaanukul, P.; Punyapornwithaya, V. Bacterial contamination of chicken meat in slaughterhouses and the associated risk factors: A nationwide study in Thailand. PLoS ONE 2022, 17, e0269416. [Google Scholar] [CrossRef]
- Brito, B.L.A.; Machado, R.A.; Jesus, J.L.B.; Reis, F.Y.T.; Zanon, I.P.; Casas, M.R.T.; Silva, R.O.S.; Figueiredo, H.C.P.; Figueiredo, T.C.; Souza, M.R.; et al. Microbiological Quality and Presence of Salmonella spp. in Broiler Carcasses with and Without Visible Gastrointestinal Contamination During Industrial Processing. Microorganisms 2025, 13, 1124. [Google Scholar] [CrossRef]
- Rosamilia, A.; Galletti, G.; Casadei, G.; Dell’Orfano, G.; Ferrari, M.; Carlantonio, E.D.; Vergani, F.; Riceputi, N.; Zanchini, F.; Bardasi, L.; et al. Assessment of process hygiene criteria in poultry slaughterhouses: A comparative analysis of own-checks and official controls in Northeast Italy (2021–2023). Poult. Sci. 2025, 104, 105465. [Google Scholar] [CrossRef] [PubMed]
- Sun, T.; Liu, Y.; Qin, X.; Aspridou, Z.; Zheng, J.; Wang, X.; Li, Z.; Dong, Q. The Prevalence and Epidemiology of Salmonella in Retail Raw Poultry Meat in China: A Systematic Review and Meta-Analysis. Foods 2021, 10, 2757. [Google Scholar] [CrossRef] [PubMed]
- Sirsat, S.A.; Kim, K.; Gibson, K.E.; Crandall, P.G.; Ricke, S.C.; Neal, J.A. Tracking microbial contamination in retail environments using fluorescent powder—A retail delicatessen environment example. JoVE 2014, 85, 51402. [Google Scholar] [CrossRef]
- Innes, G.K.; Patton, A.N.; Nachman, K.E.; Casey, J.A.; Stapleton, S.; Abraham, A.G.; Price, L.B.; Tartof, S.Y.; Davis, M.F. Distance and destination of retail meat alter multidrug resistant contamination in the United States food system. Sci. Rep. 2023, 13, 21024. [Google Scholar] [CrossRef]
- Cota, J.B.; Langkabel, N.; Barco, L.; Olsen, A.; Bonardi, S.; Vieira-Pinto, M.; Roasto, M.; Huneau-Salaün, A.; Sandberg, M.; Alvseike, O.; et al. Comparison of European surveillance and control programs for Salmonella in broiler and Turkey chains. Food Control 2024, 165, 110656. [Google Scholar] [CrossRef]
- Bianchi, D.M.; Barzanti, P.; Adriano, D.; Martucci, F.; Pitti, M.; Ferraris, C.; Floris, I.; La Brasca, R.; Ligotti, C.; Morello, S.; et al. Food Safety Monitoring of Salmonella spp. in Northern Italy 2019–2021. Pathogens 2023, 12, 963. [Google Scholar] [CrossRef]
- Tamba, M.; Pallante, I.; Petrini, S.; Feliziani, F.; Iscaro, C.; Arrigoni, N.; Di Sabatino, D.; Barberio, A.; Cibin, V.; Santi, A.; et al. Overview of Control Programs for Twenty-Four Infectious Cattle Diseases in Italy. Front. Vet. Sci. 2021, 8, 665607. [Google Scholar] [CrossRef]
- European Food Safety Authority (EFSA); European Centre for Disease Prevention and Control (ECDC). The European Union One Health 2021 Zoonoses Report. EFSA J. 2022, 20, e07666. [Google Scholar] [CrossRef]
- European Food Safety Authority (EFSA); European Centre for Disease Prevention and Control (ECDC). The European Union summary report on trends and sources of zoonoses, zoonotic agents and food-borne outbreaks in 2017. EFSA J. 2018, 16, 5500. [Google Scholar] [CrossRef]
- Chanamé Pinedo, L.; Mughini-Gras, L.; Franz, E.; Hald, T.; Pires, S.M. Sources and trends of human salmonellosis in Europe, 2015-2019: An analysis of outbreak data. Int. J. Food Microbiol. 2022, 379, 109850. [Google Scholar] [CrossRef]
- European Food Safety Authority (EFSA) Salmonella. Available online: https://www.efsa.europa.eu/en/topics/topic/salmonella (accessed on 3 November 2025).
- Neelawala, R.N.; Edison, L.K.; Kariyawasam, S. Pre-Harvest Non-Typhoidal Salmonella Control Strategies in Commercial Layer Chickens. Animals 2024, 14, 3578. [Google Scholar] [CrossRef] [PubMed]
- Carvajal, A.; Kramer, M.; Argüello, H. Salmonella Control in Swine: A Thoughtful Discussion of the Pre- and Post-Harvest Control Approaches in Industrialized Countries. Animals 2024, 14, 1035. [Google Scholar] [CrossRef]
- Dietrich, J.; Hammerl, J.A.; Johne, A.; Kappenstein, O.; Loeffler, C.; Nöckler, K.; Rosner, B.; Spielmeyer, A.; Szabo, I.; Richter, M.H. Impact of climate change on foodborne infections and intoxications. J. Health Monit. 2023, 8, 78–92. [Google Scholar] [CrossRef] [PubMed]
- Awad, D.A.; Masoud, H.A.; Hamad, A. Climate changes and food-borne pathogens: The impact on human health and mitigation strategy. Clim. Chang. 2024, 177, 92. [Google Scholar] [CrossRef]
- Billah, M.M.; Rahman, M.S. Salmonella in the environment: A review on ecology, antimicrobial resistance, seafood contaminations and human health implications. J. Hazard. Mater. Adv. 2024, 13, 100407. [Google Scholar] [CrossRef]
- Lal, A.; Ikeda, T.; French, N.; Baker, M.G.; Hales, S. Climate variability, weather and enteric disease incidence in New Zealand: Time series analysis. PLoS ONE 2013, 8, e83484. [Google Scholar] [CrossRef]
- Weisent, J.; Seaver, W.; Odoi, A.; Rohrbach, B. The importance of climatic factors and outliers in predicting regional monthly campylobacteriosis risk in Georgia, USA. Int. J. Biometeorol. 2014, 58, 1865–1878. [Google Scholar] [CrossRef] [PubMed]
- Manchal, N.; Young, M.K.; Castellanos, M.E.; Leggat, P.; Adegboye, O. A systematic review and meta-analysis of ambient temperature and precipitation with infections from five food-borne bacterial pathogens. Epidemiol. Infect. 2024, 152, e98, Erratum in Epidemiol. Infect. 2024, 152, e164. [Google Scholar] [CrossRef]
- Jin, C.; Qi, X.; Wang, J.; Chen, L.; Chen, J.; Yin, H. Identifying Key Drivers of Foodborne Diseases in Zhejiang, China: A Machine Learning Approach. Foods 2025, 14, 2857. [Google Scholar] [CrossRef] [PubMed]
- Onyeaka, H.; Akinsemolu, A.; Miri, T.; Darlington Nnaji, N.; Emeka, C.; Tamasiga, P.; Pang, G.; Al-sharify, Z. Advancing food security: The role of machine learning in pathogen detection. Appl. Food Res. 2024, 4, 100532. [Google Scholar] [CrossRef]
- Sadilek, A.; Caty, S.; DiPrete, L.; Mansour, R.; Schenk, T., Jr.; Bergtholdt, M.; Jha, A.; Ramaswami, P.; Gabrilovich, E. Machine-learned epidemiology: Real-time detection of foodborne illness at scale. npj Digital Med. 2018, 1, 36. [Google Scholar] [CrossRef]
- May, S.; Bigelow, C. Modeling nonlinear dose-response relationships in epidemiologic studies: Statistical approaches and practical challenges. Dose Response 2006, 3, 474–490. [Google Scholar] [CrossRef]
- Russo, S.; Bonassi, S. Prospects and Pitfalls of Machine Learning in Nutritional Epidemiology. Nutrients 2022, 14, 1705. [Google Scholar] [CrossRef]
- Rajula, H.S.R.; Verlato, G.; Manchia, M.; Antonucci, N.; Fanos, V. Comparison of Conventional Statistical Methods with Machine Learning in Medicine: Diagnosis, Drug Development, and Treatment. Medicina 2020, 56, 455. [Google Scholar] [CrossRef]
- Siddique, A.; Gupta, A.; Sawyer, J.T.; Huang, T.S.; Morey, A. Big data analytics in food industry: A state-of-the-art literature review. npj Sci. Food 2025, 9, 36. [Google Scholar] [CrossRef]
- Arrighi, L.; Alves de Moraes, I.; Zullich, M.; Simonato, M.; Fernandes Barbin, D.; Barbon Junior, S. Explainable Artificial Intelligence techniques for interpretation of food datasets: A review. arXiv 2025, arXiv:2504.10527. [Google Scholar]
- Ranasinghe, N.; Ramanan, A.; Fernando, S.; Hameed, P.N.; Herath, D.; Malepathirana, T.; Suganthan, P.; Niranjan, M.; Halgamuge, S. Interpretability and accessibility of machine learning in selected food processing, agriculture and health applications. J. Natl. Sci. Found. Sri Lanka 2022, 50, 263–276. [Google Scholar] [CrossRef]
- Dimitrakopoulou, M.E.; Garre, A. AI’s Intelligence for Improving Food Safety: Only as Strong as the Data that Feeds It. Curr. Food Sci. Technol. Rep. 2025, 3, 15. [Google Scholar] [CrossRef]
- Linardatos, P.; Papastefanopoulos, V.; Kotsiantis, S. Explainable AI: A Review of Machine Learning Interpretability Methods. Entropy 2020, 23, 18. [Google Scholar] [CrossRef]
- Bian, W.; Hou, H.; Chen, J.; Zhou, B.; Xia, J.; Xie, S.; Liu, T. Evaluating the Spatial Risk of Bacterial Foodborne Diseases Using Vulnerability Assessment and Geographically Weighted Logistic Regression. Remote Sens. 2022, 14, 3613. [Google Scholar] [CrossRef]
- European Food Safety Authority (EFSA); Jijón, A.F.; Costa, R.; Nicova, K.; Furnari, G. Review of the Use of GIS in Public Health and Food Safety. EFSA J. 2022, 19, EN-7639. [Google Scholar] [CrossRef]

| Variable | Description | Definition |
|---|---|---|
| year | Centred year | Sampling year centred on 2018. It ranges from –5 (2013) to +5 (2023). |
| month_sine, month_cosine | Cyclic month encoding | Sine and cosine transformations of month to represent annual periodicity. |
| long_X, lat_Y | Geographic coordinates | Longitude and latitude of the sampling municipality centroid. |
| share_production, share_retail | Sampling-phase composition | Proportion of samples collected in production vs. distribution/retail. |
| share_n_meat_species | Meat-type composition | Proportion of meat samples belonging to each species category (swine, poultry, bovine, game, other, none). One variable per species. |
| share_n_fc_food_cat | Food-category composition | Proportion of samples in each processed food category (e.g., cured meats, vegetables, fruit, bakery, etc.). One variable per category. |
| *_anom | Climatic anomalies | Difference between monthly observed values and 2013–2020 climatological means * One variable per parameter: t_mean, thi_mean, vpd_mean. |
| thi_mean | Mean THI | Monthly mean Temperature-Humidity Index (°C) derived from temperature and humidity. |
| thi_sd | THI variability | Standard deviation of THI (°C) during the sampling month. |
| vpd_mean | Mean VPD | Monthly mean Vapour Pressure Deficit (kPa). |
| thi/vpd_mean_lag1, thi/vpd_mean_lag2 | Lagged climatic means | Monthly means of THI or VPD lagged by one or two months relative to sampling. |
| thi_gt_percentile | THI exceedance days | Number of days exceeding the 75th, 90th, and 95th percentiles of the long-term THI distribution. One variable per percentile. |
| Parameter | Description | Distribution | Range/Values |
|---|---|---|---|
| max_depth | Maximum tree depth | Discrete | {3, 4, 5, 6, 7, 8} |
| eta | Learning rate | Log-uniform | [0.02, 0.20] |
| min_child_weight | Minimum child node weight | Discrete | {1, 3, 5, 10} |
| subsample | Subsample ratio | Uniform | [0.60, 0.90] |
| colsample_bytree | Column subsampling per tree | Uniform | [0.60, 0.90] |
| gamma | Minimum loss reduction per split | Uniform | [0.60, 0.90] |
| No. Tested Samples | No. of Positives | Prevalence (%) [95% IC] | PRR [95%IC] | p | |
|---|---|---|---|---|---|
| Food category | |||||
| Beverages | 174 | 0 | 0 [0–2.1] | - | - |
| Meat | 28,779 | 602 | 2.09 [1.93–2.26] | 1 (Ref.) | - |
| Cereals, seeds, and flours | 593 | 6 | 1.01 [0.37–2.19] | 0.29 [0.12–0.71] | <0.01 |
| Fruit | 169 | 5 | 2.96 [0.97–6.77] | 0.92 [0.38–2.22] | |
| Milk and dairy products | 3170 | 75 | 2.37 [1.87–2.96] | 0.79 [0.47–1.31] | |
| Pasta | 190 | 3 | 1.58 [0.33–4.54] | 0.36 [0.15–0.83] | <0.05 |
| Fish products | 1115 | 19 | 1.70 [1.03–2.65] | 0.45 [0.22–0.90] | <0.05 |
| Food preparations | 676 | 2 | 0.30 [0.04–1.06] | 0.08 [0.02–0.30] | <0.001 |
| Meat products | 1426 | 120 | 8.42 [7.03–9.98] | 1.99 [1.25–3.19] | <0.01 |
| Bakery and pastry products | 476 | 7 | 1.47 [0.59–3.01] | 0.40 [0.14–1.11] | |
| Ready-to-eat products | 3059 | 48 | 1.57 [1.16–2.08] | 0.34 [0.22–0.53] | <0.001 |
| Sauces | 175 | 7 | 4.0 [1.62–8.07] | 0.76 [0.35–1.65] | |
| Eggs and egg products | 1148 | 18 | 1.57 [0.93–2.47] | 0.91 [0.37–2.25] | |
| Vegetables | 795 | 11 | 1.38 [0.69–2.46] | 0.30 [0.17–0.55] | <0.001 |
| Origin of meat products | |||||
| Bovine | 22,869 | 221 | 0.97 [0.84–1.10] | 1 (Ref.) | |
| Poultry | 1139 | 134 | 11.8 [9.95–13.8] | 8.85 [4.37–18.0] | <0.001 |
| Swine | 4311 | 308 | 7.14 [6.39–7.95] | 7.75 [2.82–21.3] | <0.001 |
| Game | 894 | 3 | 0.34 [0.07–7.95] | 0.37 [0.12–1.19] | |
| Mixed or unidentified | 1130 | 62 | 5.80 [4.48–7.38] | 3.21 [1.25–8.27] | <0.05 |
| Other meats | 339 | 4 | 1.18 [0.32–3.0] | 0.84 [0.36–1.96] | |
| Productive phase | |||||
| Production | 29,791 | 560 | 1.88 [1.73–2.04] | 1 (Ref.) | |
| Distribution/retail | 12,154 | 363 | 2.99 [2.69–3.30] | 1.88 [1.13–3.13] | <0.05 |
| Model performance | |||||||
|---|---|---|---|---|---|---|---|
| Set | RMSE | MAE | wRMSE | wMAE | R2 | QAE50 | QAE90 |
| Training (2013–2020) | 0.140 | 0.054 | 0.093 | 0.037 | 0.094 | 0.024 | 0.076 |
| Validation (2021–2022) | 0.120 | 0.048 | 0.091 | 0.036 | 0.031 | 0.021 | 0.071 |
| Test (2023) | 0.134 | 0.052 | 0.087 | 0.033 | 0.009 | 0.021 | 0.069 |
| Model calibration | |||||||
| Set | Intercept (α) (95% IC) | Slope (β) (95% IC) | wECE | Max. Absolute Gap | |||
| Validation (2021–2022) | −0.33 (−0.50–−0.16) | 1.42 (1.23–1.61) | 0.012 | 0.034 | |||
| Test (2023) | −0.46 (−0.73–−0.19) | 1.28 (0.99–1.58) | 0.01 | 0.027 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garcia-Vozmediano, A.; Romano, A.; Begovoeva, M.; Pitti, M.; Crescio, E.; Brenda, A.; Di Roberto, M.; Gioia, A.; Giraldo, A.; Massone, E.; et al. Integrating Statistical and Machine-Learning Approaches for Salmonella enterica Surveillance in Northwestern Italy: A One Health Data-Driven Framework. Microorganisms 2025, 13, 2773. https://doi.org/10.3390/microorganisms13122773
Garcia-Vozmediano A, Romano A, Begovoeva M, Pitti M, Crescio E, Brenda A, Di Roberto M, Gioia A, Giraldo A, Massone E, et al. Integrating Statistical and Machine-Learning Approaches for Salmonella enterica Surveillance in Northwestern Italy: A One Health Data-Driven Framework. Microorganisms. 2025; 13(12):2773. https://doi.org/10.3390/microorganisms13122773
Chicago/Turabian StyleGarcia-Vozmediano, Aitor, Angelo Romano, Mattia Begovoeva, Monica Pitti, Elisabetta Crescio, Aldo Brenda, Michela Di Roberto, Anna Gioia, Adriana Giraldo, Eva Massone, and et al. 2025. "Integrating Statistical and Machine-Learning Approaches for Salmonella enterica Surveillance in Northwestern Italy: A One Health Data-Driven Framework" Microorganisms 13, no. 12: 2773. https://doi.org/10.3390/microorganisms13122773
APA StyleGarcia-Vozmediano, A., Romano, A., Begovoeva, M., Pitti, M., Crescio, E., Brenda, A., Di Roberto, M., Gioia, A., Giraldo, A., Massone, E., Lanzarini, M. N., Raggio, A., De Vita, E., Ru, G., & Maurella, C. (2025). Integrating Statistical and Machine-Learning Approaches for Salmonella enterica Surveillance in Northwestern Italy: A One Health Data-Driven Framework. Microorganisms, 13(12), 2773. https://doi.org/10.3390/microorganisms13122773







