Liver Stiffness Evaluation in Chronic Hepatitis C Patients with Cirrhosis before and after Direct-Acting Antivirals
Abstract
1. Introduction
2. Clinical Assessment of Liver Cirrhosis
3. The Advancement and Revolution in the HCV Treatment
4. Longitudinal Evaluation of Liver Stiffness in HCV-Related Cirrhosis before and after DAA Treatment
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ye, F.; Zhai, M.; Long, J.; Gong, Y.; Ren, C.; Zhang, D.; Lin, X.; Liu, S. The burden of liver cirrhosis in mortality: Results from the global burden of disease study. Front Public Health 2022, 10, 909455. [Google Scholar] [CrossRef]
- IHME, Global Burden of Disease (2024)—With Minor Processing by Our World in Data. “Deaths from Liver Disease” [Dataset]. IHME, Global Burden of Disease, “Global Burden of Disease—Deaths and DALYs” [Original Data]. Available online: https://ourworldindata.org/grapher/deaths-from-liver-disease (accessed on 29 June 2024).
- Romanelli, R.G.; Stasi, C. Recent Advancements in Diagnosis and Therapy of Liver Cirrhosis. Curr. Drug Targets 2016, 17, 1804–1817. [Google Scholar] [CrossRef]
- D’Amico, G.; Garcia-Tsao, G.; Pagliaro, L. Natural history and prognostic indicators of survival in cirrhosis: A systematic review of 118 studies. J. Hepatol. 2006, 44, 217–231. [Google Scholar] [CrossRef]
- Child, C.G.; Turcotte, J.G. Surgery and portal hypertension. Major Probl. Clin. Surg. 1964, 1, 1–85. [Google Scholar]
- Kamath, P.S.; Kim, W.R.; Advanced Liver Disease Study Group. The model for end-stage liver disease (MELD). Hepatology 2007, 45, 797–805. [Google Scholar] [CrossRef]
- Kim, W.R.; Mannalithara, A.; Heimbach, J.K.; Kamath, P.S.; Asrani, S.K.; Biggins, S.W.; Wood, N.L.; Gentry, S.E.; Kwong, A.J. MELD 3.0: The Model for End-Stage Liver Disease Updated for the Modern Era. Gastroenterology 2021, 161, 1887–1895.e4. [Google Scholar] [CrossRef]
- Stewart, C.A.; Malinchoc, M.; Kim, W.R.; Kamath, P.S. Hepatic encephalopathy as a predictor of survival in patients with end-stage liver disease. Liver Transplant. 2007, 13, 1366–1371. [Google Scholar] [CrossRef]
- Elshaarawy, O.; Allam, N.; Abdelsameea, E.; Gomaa, A.; Waked, I. Platelet-albumin-bilirubin score—A predictor of outcome of acute variceal bleeding in patients with cirrhosis. World J. Hepatol. 2020, 12, 99–107. [Google Scholar] [CrossRef]
- Stasi, C.; Milani, S. Evolving strategies for liver fibrosis staging: Non-invasive assessment. World J. Gastroenterol. 2017, 23, 191–196. [Google Scholar] [CrossRef]
- European Association for the Study of the Liver; Pawlotsky, J.-M.; Negro, F.; Aghemo, A.; Berenguer, M.; Dalgard, O.; Dusheiko, G.; Marra, F.; Puoti, M.; Wedemeyer, H. EASL recommendations on treatment of hepatitis C: Final update of the series. J. Hepatol. 2020, 73, 1170–1218, Erratum in J. Hepatol. 2023, 78, 452. [Google Scholar] [CrossRef]
- Tsochatzis, E.A.; Gurusamy, K.S.; Ntaoula, S.; Cholongitas, E.; Davidson, B.R.; Burroughs, A.K. Elastography for the diagnosis of severity of fibrosis in chronic liver disease: A meta-analysis of diagnostic accuracy. J. Hepatol. 2011, 54, 650–659. [Google Scholar] [CrossRef]
- Taylor, K.J.; Riely, C.A.; Hammers, L.; Flax, S.; Weltin, G.; Garcia-Tsao, G.; Conn, H.O.; Kuc, R.; Barwick, K.W. Quantitative US attenuation in normal liver and in patients with diffuse liver disease: Importance of fat. Radiology 1986, 160, 65–71. [Google Scholar] [CrossRef]
- Claudon, M.; Dietrich, C.F.; Choi, B.I.; Cosgrove, D.O.; Kudo, M.; Nolsøe, C.P.; Piscaglia, F.; Wilson, S.R.; Barr, R.G.; Chammas, M.C.; et al. Guidelines and good clinical practice recommendations for Contrast Enhanced Ultrasound (CEUS) in the liver—Update 2012: A WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultrasound Med. Biol. 2013, 39, 187–210. [Google Scholar] [CrossRef]
- Marot, A.; Trépo, E.; Doerig, C.; Schoepfer, A.; Moreno, C.; Deltenre, P. Liver stiffness and platelet count for identifying patients with compensated liver disease at low risk of variceal bleeding. Liver Int. 2017, 37, 707–716. [Google Scholar] [CrossRef]
- Dietrich, C.F.; Bamber, J.; Berzigotti, A.; Bota, S.; Cantisani, V.; Castera, L.; Cosgrove, D.; Ferraioli, G.; Friedrich-Rust, M.; Gilja, O.H.; et al. EFSUMB Guidelines and Recommendations on the Clinical Use of Liver Ultrasound Elastography, Update 2017 (Short Version). Ultraschall. Med. 2017, 38, 377–394. [Google Scholar] [CrossRef]
- Marcellin, P.; Cheinquer, H.; Curescu, M.; Dusheiko, G.M.; Ferenci, P.; Horban, A.; Jensen, D.; Lengyel, G.; Mangia, A.; Ouzan, D.; et al. High Sustained Virologic Response Rates in Rapid Virologic Response Patients in the Large Real-World PROPHESYS Cohort Confirm Results from Randomized Clinical Trials. Hepatology 2012, 65, 2039–2050. [Google Scholar] [CrossRef]
- World Health Organization. Guidelines for the Screening Care and Treatment of Persons with Hepatitis C Infection. 2014. Available online: http://apps.who.int/iris/bitstream/10665/111747/1/9789241548755_eng.pdf?.ua=1&ua=1 (accessed on 1 April 2014).
- European Association for the Study of the Liver. EASL Recommendations on Treatment of Hepatitis C 2015. J. Hepatol. 2015, 63, 199–236. [Google Scholar] [CrossRef]
- Flisiak, R.; Janczewska, E.; Wawrzynowicz-Syczewska, M.; Jaroszewicz, J.; Zarębska-Michaluk, D.; Nazzal, K.; Bolewska, B.; Bialkowska, J.; Berak, H.; Fleischer-Stępniewska, K.; et al. Real-world effectiveness and safety of ombitasvir/paritaprevir/ritonavir ± dasabuvir ± ribavirin in hepatitis C: AMBER study. Aliment. Pharmacol. Ther. 2016, 44, 946–956. [Google Scholar] [CrossRef]
- Lampertico, P.; Carrión, J.A.; Curry, M.; Turnes, J.; Cornberg, M.; Negro, F.; Brown, A.; Persico, M.; Wick, N.; Porcalla, A.; et al. Real-world effectiveness and safety of glecaprevir/pibrentasvir for the treatment of patients with chronic HCV infection: A meta-analysis. J. Hepatol. 2020, 72, 1112–1121. [Google Scholar] [CrossRef]
- Manns, M.P.; Burra, P.; Sargent, J.; Horton, R.; Karlsen, T.H. The Lancet-EASL Commission on liver diseases in Europe: Overcoming unmet needs, stigma, and inequities. Lancet 2018, 392, 621–622. [Google Scholar] [CrossRef]
- World Health Organization. Global Health Sector Strategy on Viral Hepatitis 2016–2021. Towards Ending Viral Hepatitis. 2016. Available online: https://www.who.int/publications/i/item/WHO-HIV-2016.06 (accessed on 8 July 2024).
- World Health Organization. WHO Publishes Updated Guidance on Hepatitis C Infection—With New Recommendations on Treatment of Adolescents and Children, Simplified Service Delivery and Diagnostics. 2022. Available online: https://www.who.int/news/item/24-06-2022-WHO-publishes-updated-guidance-on-hepatitis-C-infection (accessed on 24 June 2024).
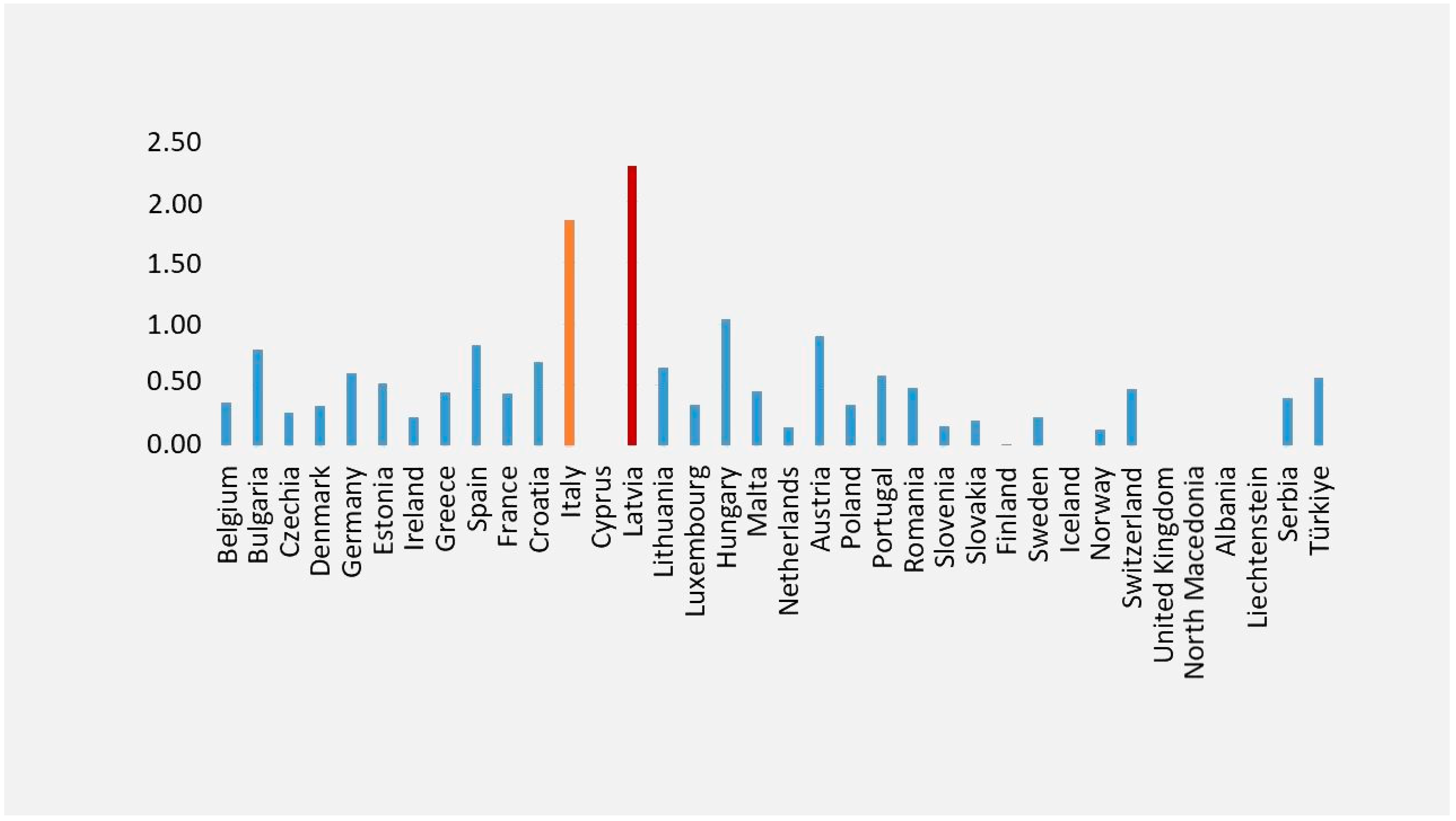
- EUROSTAT. Standardised Death Rate Due to Tuberculosis, HIV and Hepatitis by Type of Disease. Available online: https://ec.europa.eu/eurostat/databrowser/view/sdg_03_41__custom_11318007/default/bar?lang=en (accessed on 25 April 2024).
- GBD 2017 Cirrhosis Collaborators. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 2020, 5, 245–266. [Google Scholar] [CrossRef]
- Fedeli, U.; Grande, E.; Grippo, F.; Frova, L. Mortality associated with hepatitis C and hepatitis B virus infection: A nationwide study on multiple causes of death data. World J. Gastroenterol. 2017, 23, 1866–1871. [Google Scholar] [CrossRef]
- Stasi, C.; Piluso, A.; Arena, U.; Salomoni, E.; Montalto, P.; Monti, M.; Boldrini, B.; Corti, G.; Marra, F.; Laffi, G.; et al. Evaluation of the prognostic value of liver stiffness in patients with hepatitis C virus treated with triple or dual antiviral therapy: A prospective pilot study. World J Gastroenterol. 2015, 21, 3013–3019. [Google Scholar] [CrossRef]
- Stasi, C.; Sadalla, S.; Carradori, E.; Monti, M.; Petraccia, L.; Madia, F.; Gragnani, L.; Zignego, A.L. Longitudinal evaluation of liver stiffness and outcomes in patients with chronic hepatitis C before and after short- and long-term IFN-free antiviral treatment. Curr. Med. Res. Opin. 2020, 36, 245–249. [Google Scholar] [CrossRef]
- Hamoir, C.; Horsmans, Y.; Stärkel, P.; Dahlqvist, G.; Negrin Dastis, S.; Lanthier, N. Risk of hepatocellular carcinoma and fibrosis evolution in hepatitis C patients with severe fibrosis or cirrhosis treated with direct acting antiviral agents. Acta Gastroenterol. Belg. 2021, 84, 25–32. [Google Scholar] [CrossRef]
- Sultanik, P.; Kramer, L.; Soudan, D.; Bouam, S.; Meritet, J.F.; Vallet-Pichard, A.; Fontaine, H.; Bousquet, L.; Boueyre, E.; Corouge, M.; et al. The relationship between liver stiffness measurement and outcome in patients with chronic hepatitis C and cirrhosis: A retrospective longitudinal hospital study. Aliment. Pharmacol. Ther. 2016, 44, 505–513. [Google Scholar] [CrossRef]
- Sirinawasatien, A.; Supawan, P. Sustained virological response in chronic hepatitis C patients by direct-acting antiviral treatment significantly reduces liver stiffness over 24 weeks posttreatment. Medicine 2024, 103, e38096. [Google Scholar] [CrossRef]
- Berenguer, J.; Aldámiz-Echevarría, T.; Hontañón, V.; Fanciulli, C.; Quereda, C.; Busca, C.; Domínguez, L.; Hernández, C.; Vergas, J.; Gaspar, G.; et al. Clinical outcomes and prognostic factors after HCV clearance with DAA in HIV/HCV-coinfected patients with advanced fibrosis/cirrhosis. Hepatology, 2024; ahead of print. [Google Scholar] [CrossRef]
- Semmler, G.; Lens, S.; Meyer, E.L.; Baiges, A.; Alvardo-Tapias, E.; Llop, E.; Tellez, L.; Schwabl, P.; Mauro, E.; Escudé, L.; et al. Non-invasive tests for clinically significant portal hypertension after HCV cure. J. Hepatol. 2022, 77, 1573–1585. [Google Scholar] [CrossRef]
- Nicoletti, A.; Ainora, M.E.; Cintoni, M.; Garcovich, M.; Funaro, B.; Pecere, S.; De Siena, M.; Santopaolo, F.; Ponziani, F.R.; Riccardi, L.; et al. Dynamics of liver stiffness predicts complications in patients with HCV related cirrhosis treated with direct-acting antivirals. Dig. Liver Dis. 2023, 55, 1472–1479. [Google Scholar] [CrossRef]
- Czarnecka, P.; Czarnecka, K.; Tronina, O.; Bączkowska, T.; Wyczałkowska-Tomasik, A.; Durlik, M.; Czerwinska, K. Evaluation of Long-Term Outcomes of Direct Acting Antiviral Agents in Chronic Kidney Disease Subjects: A Single Center Cohort Study. J. Clin. Med. 2023, 12, 3513. [Google Scholar] [CrossRef]
- Rabell-Bernal, A.; López-Valle, R.; Morales-Santiago, A.; Toro, D.H. The Impact of a Sustained Virologic Response to Hepatitis C Virus Treatment on Liver Stiffness in the Puerto Rico Veterans Attending Liver Clinics in the Veterans Affairs Caribbean Healthcare System. P. R. Health Sci. J. 2022, 41, 123–127. [Google Scholar]
- Armandi, A.; Rosso, C.; Troshina, G.; Pérez Diaz Del Campo, N.; Marinoni, C.; Nicolosi, A.; Caviglia, G.P.; Saracco, G.M.; Bugianesi, E.; Ciancio, A. Changes in Liver Stiffness and Markers of Liver Synthesis and Portal Hypertension following Hepatitis C Virus Eradication in Cirrhotic Individuals. Biology 2022, 11, 1160. [Google Scholar] [CrossRef]
- Mezina, A.; Krishnan, A.; Woreta, T.A.; Rubenstein, K.B.; Watson, E.; Chen, P.H.; Rodriguez-Watson, C. Longitudinal assessment of liver stiffness by transient elastography for chronic hepatitis C patients. World J. Clin. Cases 2022, 10, 5566–5576. [Google Scholar] [CrossRef]
- Alswat, K.; Al-Sohaibani, F.; Khathlan, A.; Bashmail, A.; Alanazi, M.; Kurdi, A.; Almakadma, A.H.; Al-Hamoudi, W. Hepatic fibrosis changes in patients with chronic hepatitis C infection who respond to direct-acting antivirals. Ann. Saudi Med. 2022, 42, 89–95. [Google Scholar] [CrossRef]
- Davidov, Y.; Kleinbaum, Y.; Inbar, Y.; Cohen-Ezra, O.; Veitsman, E.; Weiss, P.; Likhter, M.; Berdichevski, T.; Katsherginsky, S.; Hassid, A.; et al. Noninvasive Assessment of Fibrosis Regression after Direct-acting Antiviral Treatment in Hepatitis C Virus Patients. Isr. Med. Assoc. J. 2021, 23, 794–800. [Google Scholar]
- Knop, V.; Hoppe, D.; Vermehren, J.; Troetschler, S.; Herrmann, E.; Vermehren, A.; Friedrich-Rust, M.; Sarrazin, C.; Trebicka, J.; Zeuzem, S.; et al. Non-invasive assessment of fibrosis regression and portal hypertension in patients with advanced chronic hepatitis C virus (HCV)-associated liver disease and sustained virologic response (SVR): 3 years follow-up of a prospective longitudinal study. J. Viral Hepat. 2021, 28, 1604–1613. [Google Scholar] [CrossRef]
- Ferreira, J.; Bicho, M.; Serejo, F. Effects of HCV Clearance with Direct-Acting Antivirals (DAAs) on Liver Stiffness, Liver Fibrosis Stage and Metabolic/Cellular Parameters. Viruses 2024, 16, 371. [Google Scholar] [CrossRef]
- Medrano, L.M.; Berenguer, J.; Salgüero, S.; González-García, J.; Díez, C.; Hontañón, V.; Garcia-Broncano, P.; Ibañez-Samaniego, L.; Bellón, J.M.; Jiménez-Sousa, M.A.; et al. Successful HCV Therapy Reduces Liver Disease Severity and Inflammation Biomarkers in HIV/HCV-Coinfected Patients With Advanced Cirrhosis: A Cohort Study. Front. Med. 2021, 8, 615342. [Google Scholar] [CrossRef]
- Rodprasert, N.; Hongboontry, T.; Cherdchoochart, C.; Chaiteerakij, R. Association between Liver Stiffness and Liver-Related Events in HCV-Infected Patients after Successful Treatment with Direct-Acting Antivirals. Medicina 2024, 59, 602. [Google Scholar] [CrossRef]
- Pons, M.; Rodríguez-Tajes, S.; Esteban, J.I.; Mariño, Z.; Vargas, V.; Lens, S.; Buti, M.; Augustin, S.; Forns, X.; Mínguez, B.; et al. Non-invasive prediction of liver-related events in patients with HCV-associated compensated advanced chronic liver disease after oral antivirals. J. Hepatol. 2020, 72, 472–480. [Google Scholar] [CrossRef]
- John, B.V.; Dang, Y.; Kaplan, D.E.; Jou, J.H.; Taddei, T.H.; Spector, S.A.; Martin, P.; Bastaich, D.R.; Chao, H.H.; Dahman, B. Liver Stiffness Measurement and Risk Prediction of Hepatocellular Carcinoma After HCV Eradication in Veterans with Cirrhosis. Clin. Gastroenterol. Hepatol. 2023, 22, 778–788. [Google Scholar] [CrossRef]
- Ciancio, A.; Ribaldone, D.G.; Spertino, M.; Risso, A.; Ferrarotti, D.; Caviglia, G.P.; Carucci, P.; Gaia, S.; Rolle, E.; Sacco, M.; et al. Who Should Not Be Surveilled for HCC Development after Successful Therapy with DAAS in Advanced Chronic Hepatitis C? Results of a Long-Term Prospective Study. Biomedicines 2023, 11, 166. [Google Scholar] [CrossRef]
- Nakai, M.; Yamamoto, Y.; Baba, M.; Suda, G.; Kubo, A.; Tokuchi, Y.; Kitagataya, T.; Yamada, R.; Shigesawa, T.; Suzuki, K.; et al. Prediction of hepatocellular carcinoma using age and liver stiffness on transient elastography after hepatitis C virus eradication. Sci. Rep. 2022, 12, 1449. [Google Scholar] [CrossRef]
- Ravaioli, F.; Conti, F.; Brillanti, S.; Andreone, P.; Mazzella, G.; Buonfiglioli, F.; Serio, I.; Verrucchi, G.; Bacchi Reggiani, M.L.; Colli, A.; et al. Hepatocellular carcinoma risk assessment by the measurement of liver stiffness variations in HCV cirrhotics treated with direct acting antivirals. Dig. Liver Dis. 2018, 50, 573–579. [Google Scholar] [CrossRef] [PubMed]
- Stasi, C.; Brillanti, S. Liver Stiffness Values to Predict Occurrence and Recurrence of Hepatocellular Carcinoma. Life 2024, 14, 342. [Google Scholar] [CrossRef]
| Study Design | Cirrhotic Patients (F4) | DAA | Follow-Up | Country | Baseline LSV | Outcomes | References |
|---|---|---|---|---|---|---|---|
| Prospective cohort study | 110, of whom 66 were cirrhotic patients | Cirrhosis was treated with SOF + LDV plus weight-based RBV (SOF + LDV + RBV) for 12 weeks | Over 24 weeks | Thailand | Median: 15.05 (8.76–23.68) kPa Cirrhosis (LSV ≥ 13.5 kPa), n (%) | Median: 9.60 (6.50–14.40) kPa at 24 weeks 52% of patients experienced a reduction of >30% in LSV over 24 weeks | Sirinawasatien et al., 2024 [32] |
| Multicenter retrospective study | 384 advanced fibrosis; 761 compensated cirrhosis; 155 decompensated cirrhosis | Sofosbuvir/Ledipasvir or Sofosbuvir and Daclatasvir or Ombitasvir/Paritaprevir/Ritonavir and Dasabuvir or other direct-acting antivirals, different % in advanced/compensated and decompensated cirrhosis | 40.9 (34.5–45.1) months | Spain | 15.8 kPa | Incidence rate of events per 100 PY (95% CI) 2.35 (1.62–3.41) in advanced fibrosis 2.26 (1.73–2.94) in compensated cirrhosis 1.22 (0.55–2.72) in decompensated cirrhosis | Berenguer et al., 2024 [33] |
| Prospective | 229 | Sofosbuvir + Ribavirin (16.2%); Simeprevir/Sofosbuvir ± Ribavirin (17.5%); Sofosbuvir/Velpatasvir ± Ribavirin (11.4%); Daclatasvir/Sofosbuvir ± Ribavirin (10.0%); Elbasvir/Grazoprevir (3.5%); Ledipasvir/Sofosbuvir ± Ribavirin (20.1%); Paritaprevir/Ritonavir/Ombitasvir/Dasabuvir ± Ribavirin (20.1); Glecaprevir/Pibrentasvir (1.2%) | 24 weeks 48 weeks | Italy | 18.1 (±6.6) kPa | 13.6 (±6.1) kPa at 24 weeks 12.5 (±6.1) kPa at 48 weeks | Nicoletti et al., 2024 [35] |
| Observational, cohort single-center study | 57 HCV chronic kidney disease, of whom 6 in F3, 5 in F4 | Ombitasvir/Parytaprevir/Rytonavir (23.7%) Ledipasvir/Sofosbuvir (52.5%) Glecaprevir/Pibrentasvir (5.1%) Elbasvir/Grazoprevir (18.6%) RBV (76.2%) | 4 years after EOT | Poland | F3 (9.5–12.4 kPa) F4 (≥12.5 kPa) | Advanced fibrosis (F3–F4) patients was reduced from 19.83% (n = 11) to 12.3% (n = 7) 1 advanced fibrosis patient progressed to cirrhosis (baseline = 12.4 kPa; 4 years after EOT = 13.6 kPa) | Czarnecka et al., 2023 [36] |
| Prospective | Out of 43 total patients, 15 had F4, 25 had advanced fibrosis (F3–F4) | Sofosbuvir + Velpatasvir (9.3%) Sofosbuvir + Ledipasvir (37.2%) Glecaprevir + Pibrentasvir (18.6%) Paritaprevir + Ritonavir + ombitasvir + Dasabuvir (2.3%) Sofosbuvir + Velpatasvir + Voxilaprevir (4.7%) Elbasvir + Grazoprevir (27.9%) | 6 to 9 months after reaching SVR | Spain | F4 (from 14 kPa and up) F3 (from 9 to 14 kPa) | Decreased fibrosis stage in 20.9% (n = 9) of F4 patients, in 7.0% (n = 3) of F3 patients | Rabell-Bernal et al., 2022 [37] |
| Retrospective | 373 cirrhotic patients with successful HCV eradication | Sofosbuvir/Ledipasvir (+/− Ribavirin) (53.6%) Sofosbuvir (+/− Ribavirin) (13.9%) Paritaprevir/Ritonavir/Ombitasvir + Dasabuvir (+/− Ribavirin) (11.3%) Sofosbuvir + Daclatasvir (+/− Ribavirin) (7.5%) Sofosbuvir/Velpatasvir (+/− Ribavirin) (5.9%) Sofosbuvir + Simeprevir (+/− Ribavirin) (4.0%) Paritaprevir/Ritonavir/Ombitasvir (+/− Ribavirin) (2.7%) Sofosbuvir + Velpatasvir + Voxilaprevir (+/− Ribavirin) (0.5%) Elbasvir/Grazoprevir (+/− Ribavirin) (0.3%) Glecaprevir + Pibrentasvir (+/− Ribavirin) 1 (0.3%) | 6 months | Italy | 19.3 kPa (14.7–27) | 11.6 (7.7–16.8 kPa) | Armandi et al., 2022 [38] |
| Longitudinal retrospective study | Patients with cirrhosis (kPa ≥ 12, n = 119); non-cirrhotic patients (kPa < 12, n = 651) | DAA treatment | Median of 11.7 months | United States | kPa ≥ 12 | No significant changes in LSV over time | Mezina et al., 2022 [39] |
| Retrospective cohort study | 172 HCV treatment responders, 102 Advanced fibrosis (F3, F4) | DAA treatment | Mean follow-up was 141 (57.9) weeks | Saudi Arabia | 21.10 (11.35) | 13.84 (8.47) | Alswat et al., 2022 [40] |
| Retrospective/prospective observational single center study | 133 SVR patients, of whom 82 cirrhosis with Child–Pugh score A | DAA treatment | 6, 12, 18, 24 months after EOT | Israel | 15.1 kPa (range 10.5–100) using shear wave elastography | 13.4 kPa (range 5.5–51) 6 months after EOT 11.4 kPa (range 6.1–35.8) 12 months after EOT 12.6 kPa (range 5.4–36) 18 months after EOT 11.5 kPa (range 5.2–16.4) 24 months after EOT | Davidov et al., 2021 [41] |
| Prospective | 54 achieved SVR 41 in FU | Daclatasvir + Sofosbuvir ± Ribavirin (66.7%), Sofosbuvir +Ledipasvir ± Ribavirin (22.2%), Simeprevir + Sofosbuvir ± Ribavirin (9.3%), Ombitasvir/Paritaprevir/Ritonavir + Dasabuvir (1.8%) | EOT 24 weeks after EOT 1, 2 and 3 years post-treatment | Germany | 32.4 (9.1–75) | 21.3 (6.7–73.5) kPa at EOT 16 (4.1–75) kPa 3 years | Knop et al., 2021 [42] |
| Prospective | 82 patients in F1/F2, 50 in F3/F4 | Sofosbuvir/Velpatasvir | LSV after DAA treatment | Portugal | Out of 50 patients in F3/F4, 22.4% obtained statistically significant in t in liver fibrosis stage | Ferreira J et al. [43] | |
| Multicenter observational study | 50 HIV-infected patients with advanced HCV-related cirrhosis. | Sofosbuvir + Ledipasvir (40%), Sofosbuvir + Daclatasvir (28%), Sofosbuvir + Daclatasvir + Simeprevir (6%), Sofosbuvir + Simeprevir (20%), Ombitasvir + Paritaprevir + Ritonavir + Dasabuvir (6%) | 48 weeks after DAAs treatment | Spain, United States | Significant decreases in severity scores of liver disease (LSV, HVPG, and CTP) and plasma biomarkers | Medrano et al. [44] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stasi, C.; Brillanti, S. Liver Stiffness Evaluation in Chronic Hepatitis C Patients with Cirrhosis before and after Direct-Acting Antivirals. Microorganisms 2024, 12, 1418. https://doi.org/10.3390/microorganisms12071418
Stasi C, Brillanti S. Liver Stiffness Evaluation in Chronic Hepatitis C Patients with Cirrhosis before and after Direct-Acting Antivirals. Microorganisms. 2024; 12(7):1418. https://doi.org/10.3390/microorganisms12071418
Chicago/Turabian StyleStasi, Cristina, and Stefano Brillanti. 2024. "Liver Stiffness Evaluation in Chronic Hepatitis C Patients with Cirrhosis before and after Direct-Acting Antivirals" Microorganisms 12, no. 7: 1418. https://doi.org/10.3390/microorganisms12071418
APA StyleStasi, C., & Brillanti, S. (2024). Liver Stiffness Evaluation in Chronic Hepatitis C Patients with Cirrhosis before and after Direct-Acting Antivirals. Microorganisms, 12(7), 1418. https://doi.org/10.3390/microorganisms12071418







