Group A Streptococcus Pili—Roles in Pathogenesis and Potential for Vaccine Development
Abstract
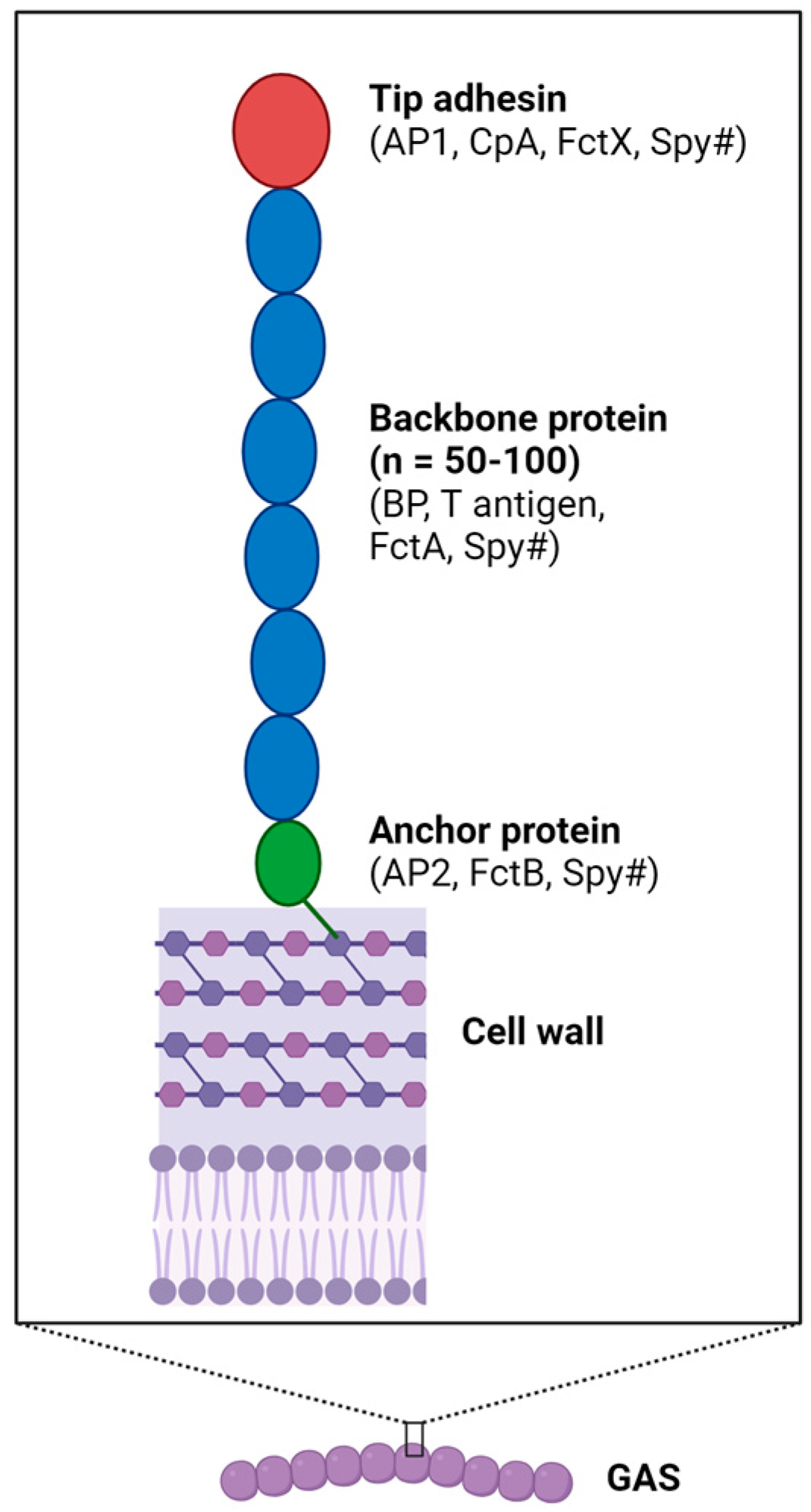
1. Introduction
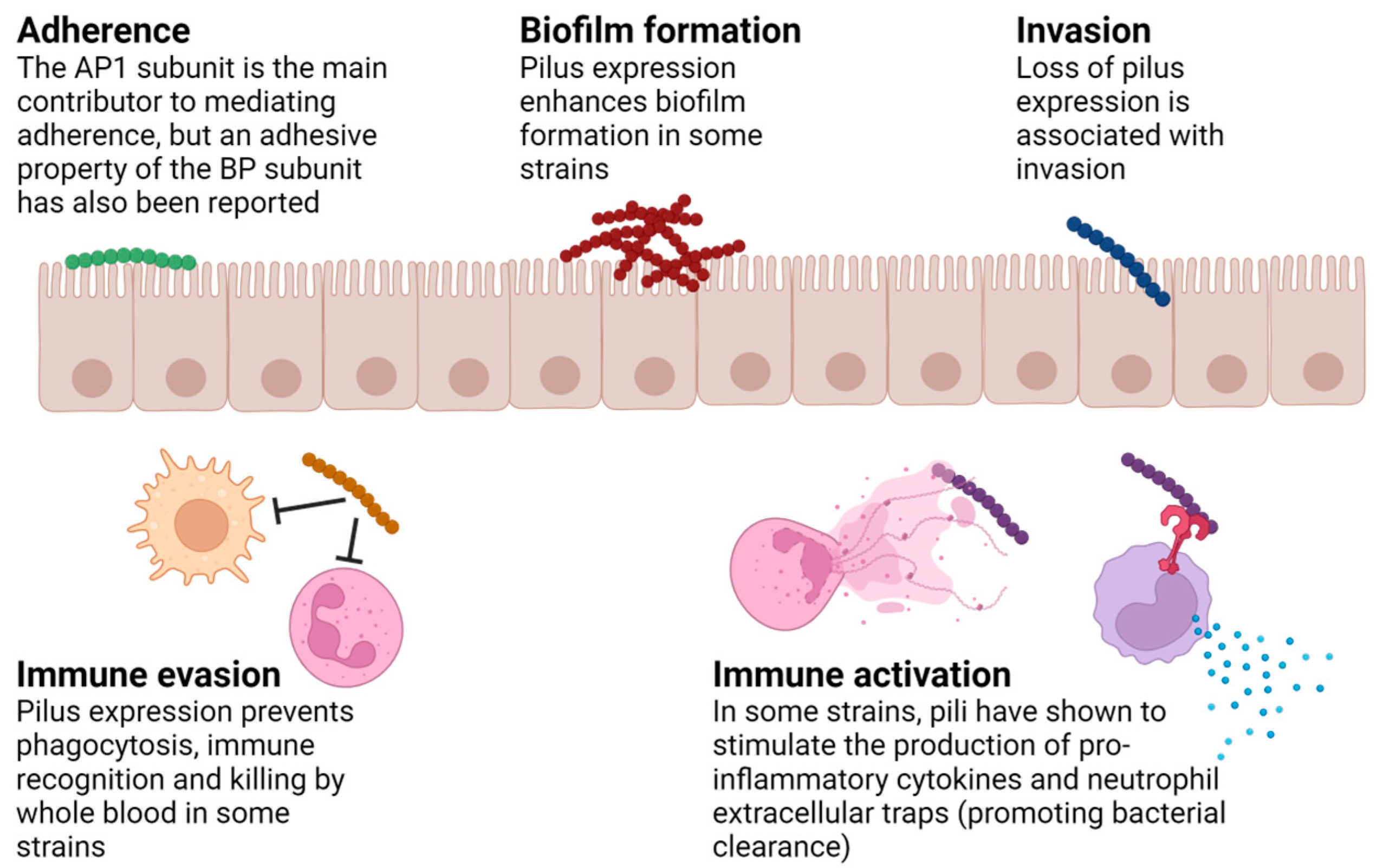
2. Roles in Pathogenesis
2.1. Adhesion
2.2. Biofilm Formation
2.3. Virulence
2.4. Immune Activation or Evasion
3. Experimental Systems for Functional Characterization
4. Potentials in Vaccine Development
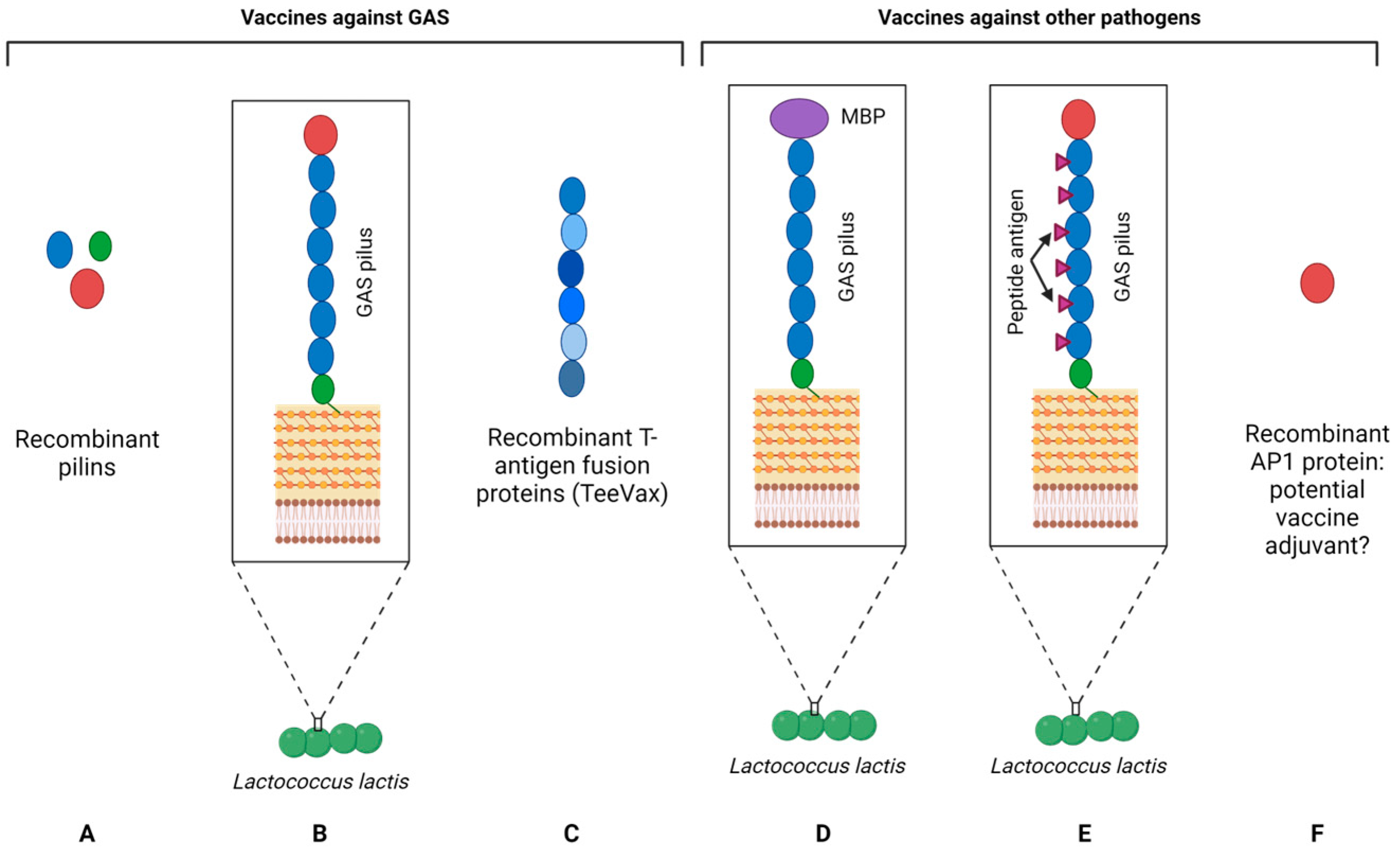
4.1. Pilus-Based GAS Vaccines
4.2. GAS Pili as a Vaccine Carrier
5. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Mora, M.; Bensi, G.; Capo, S.; Falugi, F.; Zingaretti, C.; Manetti, A.G.; Maggi, T.; Taddei, A.R.; Grandi, G.; Telford, J.L. Group A Streptococcus produce pilus-like structures containing protective antigens and Lancefield T antigens. Proc. Natl. Acad. Sci. USA 2005, 102, 15641–15646. [Google Scholar] [CrossRef]
- Sela, S.; Aviv, A.; Tovi, A.; Burstein, I.; Caparon, M.G.; Hanski, E. Protein F: An adhesin of Streptococcus pyogenes binds fibronectin via two distinct domains. Mol. Microbiol. 1993, 10, 1049–1055. [Google Scholar] [CrossRef]
- Talay, S.R.; Valentin-Weigand, P.; Timmis, K.N.; Chhatwal, G.S. Domain structure and conserved epitopes of Sfb protein, the fibronectin-binding adhesin of Streptococcus pyogenes. Mol. Microbiol. 1994, 13, 531–539. [Google Scholar] [CrossRef]
- Jaffe, J.; Natanson-Yaron, S.; Caparon, M.G.; Hanski, E. Protein F2, a novel fibronectin-binding protein from Streptococcus pyogenes, possesses two binding domains. Mol. Microbiol. 1996, 21, 373–384. [Google Scholar] [CrossRef]
- Rocha, C.L.; Fischetti, V.A. Identification and characterization of a novel fibronectin-binding protein on the surface of group A streptococci. Infect. Immun. 1999, 67, 2720–2728. [Google Scholar] [CrossRef] [PubMed]
- Kreikemeyer, B.; Nakata, M.; Oehmcke, S.; Gschwendtner, C.; Normann, J.; Podbielski, A. Streptococcus pyogenes collagen type I-binding Cpa surface protein. Expression profile, binding characteristics, biological functions, and potential clinical impact. J. Biol. Chem. 2005, 280, 33228–33239. [Google Scholar] [CrossRef] [PubMed]
- Schneewind, O.; Jones, K.F.; Fischetti, V.A. Sequence and structural characteristics of the trypsin-resistant T6 surface protein of group A streptococci. J. Bacteriol. 1990, 172, 3310–3317. [Google Scholar] [CrossRef] [PubMed]
- Kratovac, Z.; Manoharan, A.; Luo, F.; Lizano, S.; Bessen, D.E. Population genetics and linkage analysis of loci within the FCT region of Streptococcus pyogenes. J. Bacteriol. 2007, 189, 1299–1310. [Google Scholar] [CrossRef]
- Falugi, F.; Zingaretti, C.; Pinto, V.; Mariani, M.; Amodeo, L.; Manetti, A.G.; Capo, S.; Musser, J.M.; Orefici, G.; Margarit, I.; et al. Sequence variation in group A Streptococcus pili and association of pilus backbone types with lancefield T serotypes. J. Infect. Dis. 2008, 198, 1834–1841. [Google Scholar] [CrossRef] [PubMed]
- Koller, T.; Manetti, A.G.O.; Kreikemeyer, B.; Lembke, C.; Margarit, I.; Grandi, G.; Podbielski, A. Typing of the pilus-protein-encoding FCT region and biofilm formation as novel parameters in epidemiological investigations of Streptococcus pyogenes isolates from various infection sites. J. Med. Microbiol. 2010, 59 Pt 4, 442–452. [Google Scholar] [CrossRef][Green Version]
- Steemson, J.D.; Moreland, N.J.; Williamson, D.; Morgan, J.; Carter, P.E.; Proft, T. Survey of the bp/tee genes from clinical group A Streptococcus isolates in New Zealand—Implications for vaccine development. J. Med. Microbiol. 2014, 63 Pt 12, 1670–1678. [Google Scholar] [CrossRef] [PubMed]
- Linke, C.; Young, P.G.; Kang, H.J.; Bunker, R.D.; Middleditch, M.J.; Caradoc-Davies, T.T.; Proft, T.; Baker, E.N. Crystal structure of the minor pilin FctB reveals determinants of Group A streptococcal pilus anchoring. J. Biol. Chem. 2010, 285, 20381–20389. [Google Scholar] [CrossRef] [PubMed]
- Nakata, M.; Koller, T.; Moritz, K.; Ribardo, D.; Jonas, L.; McIver, K.S.; Sumitomo, T.; Terao, Y.; Kawabata, S.; Podbielski, A.; et al. Mode of expression and functional characterization of FCT-3 pilus region-encoded proteins in Streptococcus pyogenes serotype M49. Infect. Immun. 2009, 77, 32–44. [Google Scholar] [CrossRef] [PubMed]
- Lacey, J.A.; Bennett, J.; James, T.B.; Hines, B.S.; Chen, T.; Lee, D.; Sika-Paotonu, D.; Anderson, A.; Harwood, M.; Tong, S.Y.C.; et al. A worldwide population of Streptococcus pyogenes strains circulating among school-aged children in Auckland, New Zealand: A genomic epidemiology analysis. Lancet Reg. Health West. Pac. 2024, 42, 100964. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.J.; Coulibaly, F.; Clow, F.; Proft, T.; Baker, E.N. Stabilizing isopeptide bonds revealed in gram-positive bacterial pilus structure. Science 2007, 318, 1625–1628. [Google Scholar] [CrossRef] [PubMed]
- Smith, W.D.; Pointon, J.A.; Abbot, E.; Kang, H.J.; Baker, E.N.; Hirst, B.H.; Wilson, J.A.; Banfield, M.J.; Kehoe, M.A. Roles of minor pilin subunits Spy0125 and Spy0130 in the serotype M1 Streptococcus pyogenes strain SF370. J. Bacteriol. 2010, 192, 4651–4659. [Google Scholar] [CrossRef]
- Ton-That, H.; Liu, G.; Mazmanian, S.K.; Faull, K.F.; Schneewind, O. Purification and characterization of sortase, the transpeptidase that cleaves surface proteins of Staphylococcus aureus at the LPXTG motif. Proc. Natl. Acad. Sci. USA 1999, 96, 12424–12429. [Google Scholar] [CrossRef]
- Mazmanian, S.K.; Liu, G.; Ton-That, H.; Schneewind, O. Staphylococcus aureus sortase, an enzyme that anchors surface proteins to the cell wall. Science 1999, 285, 760–763. [Google Scholar] [CrossRef]
- Nakata, M.; Kimura, K.R.; Sumitomo, T.; Wada, S.; Sugauchi, A.; Oiki, E.; Higashino, M.; Kreikemeyer, B.; Podbielski, A.; Okahashi, N.; et al. Assembly mechanism of FCT region type 1 pili in serotype M6 Streptococcus pyogenes. J. Biol. Chem. 2011, 286, 37566–37577. [Google Scholar] [CrossRef]
- Young, P.G.; Moreland, N.J.; Loh, J.M.; Bell, A.; Atatoa Carr, P.; Proft, T.; Baker, E.N. Structural conservation, variability, and immunogenicity of the T6 backbone pilin of serotype M6 Streptococcus pyogenes. Infect. Immun. 2014, 82, 2949–2957. [Google Scholar] [CrossRef]
- Lizano, S.; Luo, F.; Bessen, D.E. Role of streptococcal T antigens in superficial skin infection. J. Bacteriol. 2007, 189, 1426–1434. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tsai, J.C.; Loh, J.M.; Clow, F.; Lorenz, N.; Proft, T. The Group A Streptococcus serotype M2 pilus plays a role in host cell adhesion and immune evasion. Mol. Microbiol. 2017, 103, 282–298. [Google Scholar] [CrossRef]
- Nakata, M.; Sumitomo, T.; Patenge, N.; Kreikemeyer, B.; Kawabata, S. Thermosensitive pilus production by FCT type 3 Streptococcus pyogenes controlled by Nra regulator translational efficiency. Mol. Microbiol. 2020, 113, 173–189. [Google Scholar] [CrossRef] [PubMed]
- Luo, F.; Lizano, S.; Bessen, D.E. Heterogeneity in the polarity of Nra regulatory effects on streptococcal pilus gene transcription and virulence. Infect. Immun. 2008, 76, 2490–2497. [Google Scholar] [CrossRef][Green Version]
- Granok, A.B.; Parsonage, D.; Ross, R.P.; Caparon, M.G. The RofA binding site in Streptococcus pyogenes is utilized in multiple transcriptional pathways. J. Bacteriol. 2000, 182, 1529–1540. [Google Scholar] [CrossRef] [PubMed]
- Fogg, G.C.; Gibson, C.M.; Caparon, M.G. The identification of rofA, a positive-acting regulatory component of prtF expression: Use of an m gamma delta-based shuttle mutagenesis strategy in Streptococcus pyogenes. Mol. Microbiol. 1994, 11, 671–684. [Google Scholar] [CrossRef]
- Calfee, G.; Danger, J.L.; Jain, I.; Miller, E.W.; Sarkar, P.; Tjaden, B.; Kreikemeyer, B.; Sumby, P. Identification and Characterization of Serotype-Specific Variation in Group A Streptococcus Pilus Expression. Infect. Immun. 2018, 86, e00792-17. [Google Scholar] [CrossRef]
- Lizano, S.; Luo, F.; Tengra, F.K.; Bessen, D.E. Impact of orthologous gene replacement on the circuitry governing pilus gene transcription in streptococci. PLoS ONE 2008, 3, e3450. [Google Scholar] [CrossRef]
- Kreikemeyer, B.; Nakata, M.; Koller, T.; Hildisch, H.; Kourakos, V.; Standar, K.; Kawabata, S.; Glocker, M.O.; Podbielski, A. The Streptococcus pyogenes serotype M49 Nra-Ralp3 transcriptional regulatory network and its control of virulence factor expression from the novel eno ralp3 epf sagA pathogenicity region. Infect. Immun. 2007, 75, 5698–5710. [Google Scholar] [CrossRef]
- Podbielski, A.; Woischnik, M.; Leonard, B.A.; Schmidt, K.H. Characterization of nra, a global negative regulator gene in group A streptococci. Mol. Microbiol. 1999, 31, 1051–1064. [Google Scholar] [CrossRef]
- Nakata, M.; Podbielski, A.; Kreikemeyer, B. MsmR, a specific positive regulator of the Streptococcus pyogenes FCT pathogenicity region and cytolysin-mediated translocation system genes. Mol. Microbiol. 2005, 57, 786–803. [Google Scholar] [CrossRef] [PubMed]
- Roberts, S.A.; Churchward, G.G.; Scott, J.R. Unraveling the regulatory network in Streptococcus pyogenes: The global response regulator CovR represses rivR directly. J. Bacteriol. 2007, 189, 1459–1463. [Google Scholar] [CrossRef][Green Version]
- Liu, Z.; Trevino, J.; Ramirez-Pena, E.; Sumby, P. The small regulatory RNA FasX controls pilus expression and adherence in the human bacterial pathogen group A Streptococcus. Mol. Microbiol. 2012, 86, 140–154. [Google Scholar] [CrossRef] [PubMed]
- Kreikemeyer, B.; Gamez, G.; Margarit, I.; Giard, J.C.; Hammerschmidt, S.; Hartke, A.; Podbielski, A. Genomic organization, structure, regulation and pathogenic role of pilus constituents in major pathogenic Streptococci and Enterococci. Int. J. Med. Microbiol. 2011, 301, 240–251. [Google Scholar] [CrossRef] [PubMed]
- Flores, A.R.; Olsen, R.J.; Cantu, C.; Pallister, K.B.; Guerra, F.E.; Voyich, J.M.; Musser, J.M. Increased Pilus Production Conferred by a Naturally Occurring Mutation Alters Host-Pathogen Interaction in Favor of Carriage in Streptococcus pyogenes. Infect. Immun. 2017, 85, e00949-16. [Google Scholar] [CrossRef] [PubMed]
- Manetti, A.G.; Koller, T.; Becherelli, M.; Buccato, S.; Kreikemeyer, B.; Podbielski, A.; Grandi, G.; Margarit, I. Environmental acidification drives S. pyogenes pilus expression and microcolony formation on epithelial cells in a FCT-dependent manner. PLoS ONE 2010, 5, e13864. [Google Scholar] [CrossRef] [PubMed]
- Kimura, K.R.; Nakata, M.; Sumitomo, T.; Kreikemeyer, B.; Podbielski, A.; Terao, Y.; Kawabata, S. Involvement of T6 pili in biofilm formation by serotype M6 Streptococcus pyogenes. J. Bacteriol. 2012, 194, 804–812. [Google Scholar] [CrossRef]
- Abbot, E.L.; Smith, W.D.; Siou, G.P.; Chiriboga, C.; Smith, R.J.; Wilson, J.A.; Hirst, B.H.; Kehoe, M.A. Pili mediate specific adhesion of Streptococcus pyogenes to human tonsil and skin. Cell. Microbiol. 2007, 9, 1822–1833. [Google Scholar] [CrossRef]
- Crotty Alexander, L.E.; Maisey, H.C.; Timmer, A.M.; Rooijakkers, S.H.; Gallo, R.L.; von Kockritz-Blickwede, M.; Nizet, V. M1T1 group A streptococcal pili promote epithelial colonization but diminish systemic virulence through neutrophil extracellular entrapment. J. Mol. Med. 2010, 88, 371–381. [Google Scholar] [CrossRef]
- Manetti, A.G.; Zingaretti, C.; Falugi, F.; Capo, S.; Bombaci, M.; Bagnoli, F.; Gambellini, G.; Bensi, G.; Mora, M.; Edwards, A.M.; et al. Streptococcus pyogenes pili promote pharyngeal cell adhesion and biofilm formation. Mol. Microbiol. 2007, 64, 968–983. [Google Scholar] [CrossRef]
- Takahashi, R.; Radcliff, F.J.; Proft, T.; Tsai, C.J. Pilus proteins from Streptococcus pyogenes stimulate innate immune responses through Toll-like receptor 2. Immunol. Cell Biol. 2022, 100, 174–185. [Google Scholar] [CrossRef] [PubMed]
- Edwards, A.M.; Manetti, A.G.; Falugi, F.; Zingaretti, C.; Capo, S.; Buccato, S.; Bensi, G.; Telford, J.L.; Margarit, I.; Grandi, G. Scavenger receptor gp340 aggregates group A streptococci by binding pili. Mol. Microbiol. 2008, 68, 1378–1394. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.H.; Li, S.H.; Yang, Y.C.; Hsu, S.H.; Nizet, V.; Chang, Y.C. T4 Pili Promote Colonization and Immune Evasion Phenotypes of Nonencapsulated M4 Streptococcus pyogenes. mBio 2020, 11, 10.1128. [Google Scholar] [CrossRef]
- Bessen, D.E.; Kalia, A. Genomic localization of a T serotype locus to a recombinatorial zone encoding extracellular matrix-binding proteins in Streptococcus pyogenes. Infect. Immun. 2002, 70, 1159–1167. [Google Scholar] [CrossRef][Green Version]
- Siemens, N.; Chakrakodi, B.; Shambat, S.M.; Morgan, M.; Bergsten, H.; Hyldegaard, O.; Skrede, S.; Arnell, P.; Madsen, M.B.; Johansson, L.; et al. Biofilm in group A streptococcal necrotizing soft tissue infections. JCI Insight 2016, 1, e87882. [Google Scholar] [CrossRef]
- Vyas, H.K.N.; Proctor, E.J.; McArthur, J.; Gorman, J.; Sanderson-Smith, M. Current Understanding of Group A Streptococcal Biofilms. Curr. Drug Targets 2019, 20, 982–993. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, T.; Terao, Y.; Okuni, H.; Ninomiya, K.; Sakata, H.; Ikebe, K.; Maeda, Y.; Kawabata, S. Biofilm formation or internalization into epithelial cells enable Streptococcus pyogenes to evade antibiotic eradication in patients with pharyngitis. Microb. Pathog. 2011, 51, 58–68. [Google Scholar] [CrossRef]
- Becherelli, M.; Manetti, A.G.; Buccato, S.; Viciani, E.; Ciucchi, L.; Mollica, G.; Grandi, G.; Margarit, I. The ancillary protein 1 of Streptococcus pyogenes FCT-1 pili mediates cell adhesion and biofilm formation through heterophilic as well as homophilic interactions. Mol. Microbiol. 2012, 83, 1035–1047. [Google Scholar] [CrossRef]
- Rouchon, C.N.; Ly, A.T.; Noto, J.P.; Luo, F.; Lizano, S.; Bessen, D.E. Incremental Contributions of FbaA and Other Impetigo-Associated Surface Proteins to Fitness and Virulence of a Classical Group A Streptococcal Skin Strain. Infect. Immun. 2017, 85, e00374-17. [Google Scholar] [CrossRef]
- Takahashi, R.; J-Khemlani, A.H.; Loh, J.M.; Radcliff, F.J.; Proft, T.; Tsai, C.J. Different Group A Streptococcus pili lead to varying proinflammatory cytokine responses and virulence. Immunol. Cell Biol. 2023, 102, 21–33. [Google Scholar] [CrossRef]
- Herwald, H.; Cramer, H.; Morgelin, M.; Russell, W.; Sollenberg, U.; Norrby-Teglund, A.; Flodgaard, H.; Lindbom, L.; Bjorck, L. M protein, a classical bacterial virulence determinant, forms complexes with fibrinogen that induce vascular leakage. Cell 2004, 116, 367–379. [Google Scholar] [CrossRef]
- Smeesters, P.R.; McMillan, D.J.; Sriprakash, K.S. The streptococcal M protein: A highly versatile molecule. Trends Microbiol. 2010, 18, 275–282. [Google Scholar] [CrossRef]
- Gabay, C.; Kushner, I. Acute-phase proteins and other systemic responses to inflammation. N. Engl. J. Med. 1999, 340, 448–454. [Google Scholar] [CrossRef]
- Lancefield, R.C. Differentiation of group A streptococci with a common R antigen into three serological types, with special reference to the bactericidal test. J. Exp. Med. 1957, 106, 525–544. [Google Scholar] [CrossRef] [PubMed]
- Maxted, W.R. The indirect bactericidal test as a means of identifying antibody to the M antigen of Streptococcus pyogenes. Br. J. Exp. Pathol. 1956, 37, 415–422. [Google Scholar]
- Zhu, L.; Charbonneau, A.R.L.; Waller, A.S.; Olsen, R.J.; Beres, S.B.; Musser, J.M. Novel Genes Required for the Fitness of Streptococcus pyogenes in Human Saliva. mSphere 2017, 2, e00460-17. [Google Scholar] [CrossRef]
- Alam, F.M.; Turner, C.E.; Smith, K.; Wiles, S.; Sriskandan, S. Inactivation of the CovR/S virulence regulator impairs infection in an improved murine model of Streptococcus pyogenes naso-pharyngeal infection. PLoS ONE 2013, 8, e61655. [Google Scholar] [CrossRef]
- Watson, M.E., Jr.; Neely, M.N.; Caparon, M.G. Animal Models of Streptococcus pyogenes Infection. In Streptococcus pyogenes: Basic Biology to Clinical Manifestations; Ferretti, J.J., Stevens, D.L., Fischetti, V.A., Eds.; University of Oklahoma Health Sciences Center: Oklahoma City, OK, USA, 2016. [Google Scholar]
- Loh, J.M.S.; Lorenz, N.; Tsai, C.J.; Khemlani, A.H.J.; Proft, T. Mucosal vaccination with pili from Group A Streptococcus expressed on Lactococcus lactis generates protective immune responses. Sci. Rep. 2017, 7, 7174. [Google Scholar] [CrossRef] [PubMed]
- Rivera-Hernandez, T.; Walker, M.J. Humanized Plasminogen Mouse Model to Study Group A Streptococcus Invasive Disease. Methods Mol. Biol. 2020, 2136, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Loh, J.M.; Adenwalla, N.; Wiles, S.; Proft, T. Galleria mellonella larvae as an infection model for group A streptococcus. Virulence 2013, 4, 419–428. [Google Scholar] [CrossRef]
- Tsai, C.J.; Loh, J.M.; Proft, T. Galleria mellonella infection models for the study of bacterial diseases and for antimicrobial drug testing. Virulence 2016, 7, 214–229. [Google Scholar] [CrossRef]
- Reglinski, M. Lancefield Whole Blood Killing Assay to Evaluate Vaccine Efficacy. Methods Mol. Biol. 2020, 2136, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Salehi, S.; Hohn, C.M.; Penfound, T.A.; Dale, J.B. Development of an Opsonophagocytic Killing Assay Using HL-60 Cells for Detection of Functional Antibodies against Streptococcus pyogenes. mSphere 2018, 3, e00617-18. [Google Scholar] [CrossRef] [PubMed]
- McGregor, R.; Jones, S.; Jeremy, R.M.; Goldblatt, D.; Moreland, N.J. An Opsonophagocytic Killing Assay for the Evaluation of Group A Streptococcus Vaccine Antisera. Methods Mol. Biol. 2020, 2136, 323–335. [Google Scholar] [CrossRef] [PubMed]
- Jones, S.; Moreland, N.J.; Zancolli, M.; Raynes, J.; Loh, J.M.S.; Smeesters, P.R.; Sriskandan, S.; Carapetis, J.R.; Fraser, J.D.; Goldblatt, D. Development of an opsonophagocytic killing assay for group A Streptococcus. Vaccine 2018, 36, 3756–3763. [Google Scholar] [CrossRef]
- Raynes, J.M.; Young, P.G.; Lorenz, N.; Loh, J.M.S.; McGregor, R.; Baker, E.N.; Proft, T.; Moreland, N.J. Identification of an immunodominant region on a group A Streptococcus T-antigen reveals temperature-dependent motion in pili. Virulence 2023, 14, 2180228. [Google Scholar] [CrossRef] [PubMed]
- Ralph, A.P.; Carapetis, J.R. Group a streptococcal diseases and their global burden. Curr. Top. Microbiol. Immunol. 2013, 368, 1–27. [Google Scholar] [CrossRef] [PubMed]
- Carapetis, J.R.; Steer, A.C.; Mulholland, E.K.; Weber, M. The global burden of group A streptococcal diseases. Lancet Infect. Dis. 2005, 5, 685–694. [Google Scholar] [CrossRef] [PubMed]
- Bowen, A.C.; Mahe, A.; Hay, R.J.; Andrews, R.M.; Steer, A.C.; Tong, S.Y.; Carapetis, J.R. The Global Epidemiology of Impetigo: A Systematic Review of the Population Prevalence of Impetigo and Pyoderma. PLoS ONE 2015, 10, e0136789. [Google Scholar] [CrossRef]
- Watkins, D.A.; Johnson, C.O.; Colquhoun, S.M.; Karthikeyan, G.; Beaton, A.; Bukhman, G.; Forouzanfar, M.H.; Longenecker, C.T.; Mayosi, B.M.; Mensah, G.A.; et al. Global, Regional, and National Burden of Rheumatic Heart Disease, 1990–2015. N. Engl. J. Med. 2017, 377, 713–722. [Google Scholar] [CrossRef]
- Liang, Y.; Yu, D.; Lu, Q.; Zheng, Y.; Yang, Y. The rise and fall of acute rheumatic fever and rheumatic heart disease: A mini review. Front. Cardiovasc. Med. 2023, 10, 1183606. [Google Scholar] [CrossRef] [PubMed]
- Bennett, J.; Zhang, J.; Leung, W.; Jack, S.; Oliver, J.; Webb, R.; Wilson, N.; Sika-Paotonu, D.; Harwood, M.; Baker, M.G. Rising Ethnic Inequalities in Acute Rheumatic Fever and Rheumatic Heart Disease, New Zealand, 2000–2018. Emerg. Infect. Dis. 2021, 27, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Wyber, R.; Noonan, K.; Halkon, C.; Enkel, S.; Cannon, J.; Haynes, E.; Mitchell, A.G.; Bessarab, D.C.; Katzenellenbogen, J.M.; Bond-Smith, D.; et al. Ending rheumatic heart disease in Australia: The evidence for a new approach. Med. J. Aust. 2020, 213 (Suppl. S10), S3–S31. [Google Scholar] [CrossRef]
- Pastural, E.; McNeil, S.A.; MacKinnon-Cameron, D.; Ye, L.; Langley, J.M.; Stewart, R.; Martin, L.H.; Hurley, G.J.; Salehi, S.; Penfound, T.A.; et al. Safety and immunogenicity of a 30-valent M protein-based group a streptococcal vaccine in healthy adult volunteers: A randomized, controlled phase I study. Vaccine 2020, 38, 1384–1392. [Google Scholar] [CrossRef] [PubMed]
- Sekuloski, S.; Batzloff, M.R.; Griffin, P.; Parsonage, W.; Elliott, S.; Hartas, J.; O’Rourke, P.; Marquart, L.; Pandey, M.; Rubin, F.A.; et al. Evaluation of safety and immunogenicity of a group A Streptococcus vaccine candidate (MJ8VAX) in a randomized clinical trial. PLoS ONE 2018, 13, e0198658. [Google Scholar] [CrossRef] [PubMed]
- McNeil, S.A.; Halperin, S.A.; Langley, J.M.; Smith, B.; Warren, A.; Sharratt, G.P.; Baxendale, D.M.; Reddish, M.A.; Hu, M.C.; Stroop, S.D.; et al. Safety and immunogenicity of 26-valent group a Streptococcus vaccine in healthy adult volunteers. Clin. Infect. Dis. 2005, 41, 1114–1122. [Google Scholar] [CrossRef] [PubMed]
- Kotloff, K.L.; Corretti, M.; Palmer, K.; Campbell, J.D.; Reddish, M.A.; Hu, M.C.; Wasserman, S.S.; Dale, J.B. Safety and immunogenicity of a recombinant multivalent group a streptococcal vaccine in healthy adults: Phase 1 trial. JAMA 2004, 292, 709–715. [Google Scholar] [CrossRef]
- Massell, B.F.; Honikman, L.H.; Amezcua, J. Rheumatic fever following streptococcal vaccination. Report of three cases. JAMA 1969, 207, 1115–1119. [Google Scholar] [CrossRef]
- Dale, J.B.; Beachey, E.H. Epitopes of streptococcal M proteins shared with cardiac myosin. J. Exp. Med. 1985, 162, 583–591. [Google Scholar] [CrossRef]
- Young, P.G.; Raynes, J.M.; Loh, J.M.; Proft, T.; Baker, E.N.; Moreland, N.J. Group A Streptococcus T Antigens Have a Highly Conserved Structure Concealed under a Heterogeneous Surface That Has Implications for Vaccine Design. Infect. Immun. 2019, 87, e00205-19. [Google Scholar] [CrossRef]
- AH, J.K.; Pilapitiya, D.; Tsai, C.J.; Proft, T.; Loh, J.M.S. Expanding strain coverage of a group A Streptococcus pilus-expressing Lactococcus lactis mucosal vaccine. Immunol. Cell Biol. 2023, 101, 545–555. [Google Scholar] [CrossRef]
- Loh, J.M.S.; Rivera-Hernandez, T.; McGregor, R.; Khemlani, A.H.J.; Tay, M.L.; Cork, A.J.; Raynes, J.M.; Moreland, N.J.; Walker, M.J.; Proft, T. A multivalent T-antigen-based vaccine for Group A Streptococcus. Sci. Rep. 2021, 11, 4353. [Google Scholar] [CrossRef]
- Quigley, B.R.; Hatkoff, M.; Thanassi, D.G.; Ouattara, M.; Eichenbaum, Z.; Scott, J.R. A foreign protein incorporated on the Tip of T3 pili in Lactococcus lactis elicits systemic and mucosal immunity. Infect. Immun. 2010, 78, 1294–1303. [Google Scholar] [CrossRef]
- Chamcha, V.; Jones, A.; Quigley, B.R.; Scott, J.R.; Amara, R.R. Oral Immunization with a Recombinant Lactococcus lactis-Expressing HIV-1 Antigen on Group A Streptococcus Pilus Induces Strong Mucosal Immunity in the Gut. J. Immunol. 2015, 195, 5025–5034. [Google Scholar] [CrossRef]
- Wagachchi, D.; Tsai, J.C.; Chalmers, C.; Blanchett, S.; Loh, J.M.S.; Proft, T. PilVax—A novel peptide delivery platform for the development of mucosal vaccines. Sci. Rep. 2018, 8, 2555. [Google Scholar] [CrossRef] [PubMed]
- Blanchett, S.; Tsai, C.J.; Sandford, S.; Loh, J.M.; Huang, L.; Kirman, J.R.; Proft, T. Intranasal immunization with Ag85B peptide 25 displayed on Lactococcus lactis using the PilVax platform induces antigen-specific B- and T-cell responses. Immunol. Cell Biol. 2021, 99, 767–781. [Google Scholar] [CrossRef] [PubMed]
- Clow, F.; Peterken, K.; Pearson, V.; Proft, T.; Radcliff, F.J. PilVax, a novel Lactococcus lactis-based mucosal vaccine platform, stimulates systemic and mucosal immune responses to Staphylococcus aureus. Immunol. Cell Biol. 2020, 98, 369–381. [Google Scholar] [CrossRef] [PubMed]
- Bah, S.Y.; Keeley, A.J.; Armitage, E.P.; Khalid, H.; Chaudhuri, R.R.; Senghore, E.; Manneh, J.; Tilley, L.; Marks, M.; Darboe, S.; et al. Genomic Characterization of Skin and Soft Tissue Streptococcus pyogenes Isolates from a Low-Income and a High-Income Setting. mSphere 2023, 8, e0046922. [Google Scholar] [CrossRef] [PubMed]
- Danger, J.L.; Cao, T.N.; Cao, T.H.; Sarkar, P.; Trevino, J.; Pflughoeft, K.J.; Sumby, P. The small regulatory RNA FasX enhances group A Streptococcus virulence and inhibits pilus expression via serotype-specific targets. Mol. Microbiol. 2015, 96, 249–262. [Google Scholar] [CrossRef] [PubMed]
- Roshika, R.; Jain, I.; Glenaldo, T.; Sickler, T.; Musser, J.M.; Sumby, P. Characterization of M-Type-Specific Pilus Expression in Group A Streptococcus. J. Bacteriol. 2022, 204, e0027022. [Google Scholar] [CrossRef] [PubMed]
- Courtney, H.S.; Ofek, I.; Hasty, D.L. M protein mediated adhesion of M type 24 Streptococcus pyogenes stimulates release of interleukin-6 by HEp-2 tissue culture cells. FEMS Microbiol. Lett. 1997, 151, 65–70. [Google Scholar] [CrossRef]
- Bartelt, M.A.; Duncan, J.L. Adherence of group A streptococci to human epithelial cells. Infect. Immun. 1978, 20, 200–208. [Google Scholar] [CrossRef]
- Schrager, H.M.; Alberti, S.; Cywes, C.; Dougherty, G.J.; Wessels, M.R. Hyaluronic acid capsule modulates M protein-mediated adherence and acts as a ligand for attachment of group A Streptococcus to CD44 on human keratinocytes. J. Clin. Investig. 1998, 101, 1708–1716. [Google Scholar] [CrossRef]
- Keeble, A.H.; Howarth, M. Power to the protein: Enhancing and combining activities using the Spy toolbox. Chem. Sci. 2020, 11, 7281–7291. [Google Scholar] [CrossRef] [PubMed]
- Kwon, H.; Young, P.G.; Squire, C.J.; Baker, E.N. Engineering a Lys-Asn isopeptide bond into an immunoglobulin-like protein domain enhances its stability. Sci. Rep. 2017, 7, 42753. [Google Scholar] [CrossRef] [PubMed]
- Van Braeckel-Budimir, N.; Haijema, B.J.; Leenhouts, K. Bacterium-like particles for efficient immune stimulation of existing vaccines and new subunit vaccines in mucosal applications. Front. Immunol. 2013, 4, 282. [Google Scholar] [CrossRef] [PubMed]
- Guilherme, L.; Kalil, J.; Cunningham, M. Molecular mimicry in the autoimmune pathogenesis of rheumatic heart disease. Autoimmunity 2006, 39, 31–39. [Google Scholar] [CrossRef] [PubMed]
| FCT Type | Stages of Infection | Determination of Characteristics | References |
|---|---|---|---|
| FCT-1 | Adhesion | AP1 deletion reduces binding to epithelial cells | |
| Biofilm formation | Loss of biofilm formation in BP and AP1 deletion mutants | [37] | |
| Virulence | AP1 deletion decreases GAS virulence in humanized mouse impetigo model | ||
| FCT-2 | Adhesion | Reduced binding to epithelial cells with AP1 deletion and with addition of anti-AP1 sera | [16,38,39,40,41] |
| Biofilm formation | Loss of biofilm formation in BP and AP1 deletion mutants | ||
| Immune stimulation | AP1 and BP activate TLR2 and induce pro-inflammatory cytokine release | ||
| FCT-3 | Adhesion | Pilus deletion reduces binding to host proteins | |
| Virulence | AP1 or BP deletion decreases GAS virulence in human-skin-engrafted mouse model | [21,27,31] | |
| FCT-4 | Adhesion | Pilus expressed on L. lactis binds to host proteins | [42] |
| Biofilm formation | pH-dependent increase in pilus expression levels linked to biofilm formation | ||
| FCT-5 | Adhesion | Reduced binding to epithelial cells following BP deletion | [43] |
| Biofilm formation | Loss of biofilm formation in BP deletion mutant | ||
| Virulence | BP deletion decreases GAS virulence in systemic mouse infection model | ||
| Immune evasion | BP mediates haptoglobin binding, which promotes reduced susceptibility to antimicrobial peptides | ||
| FCT-6 | Adhesion | BP mediates adherence to and invasion of epithelial cells and directly binds to fibrinogen | [22] |
| Immune evasion | BP binds to monocyte, interferes with blood clot formation, and reduces macrophage uptake and killing | ||
| Virulence | Expression of pili provides resistance in whole-blood killing assay and a Galleria mellonella infection model |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsai, C.J.-Y.; Takahashi, R.; Loh, J.M.-S.; Proft, T. Group A Streptococcus Pili—Roles in Pathogenesis and Potential for Vaccine Development. Microorganisms 2024, 12, 555. https://doi.org/10.3390/microorganisms12030555
Tsai CJ-Y, Takahashi R, Loh JM-S, Proft T. Group A Streptococcus Pili—Roles in Pathogenesis and Potential for Vaccine Development. Microorganisms. 2024; 12(3):555. https://doi.org/10.3390/microorganisms12030555
Chicago/Turabian StyleTsai, Catherine Jia-Yun, Risa Takahashi, Jacelyn Mei-San Loh, and Thomas Proft. 2024. "Group A Streptococcus Pili—Roles in Pathogenesis and Potential for Vaccine Development" Microorganisms 12, no. 3: 555. https://doi.org/10.3390/microorganisms12030555
APA StyleTsai, C. J.-Y., Takahashi, R., Loh, J. M.-S., & Proft, T. (2024). Group A Streptococcus Pili—Roles in Pathogenesis and Potential for Vaccine Development. Microorganisms, 12(3), 555. https://doi.org/10.3390/microorganisms12030555







