Epidemiology of Zoonotic Coxiella burnetii in The Republic of Guinea
Abstract
1. Introduction
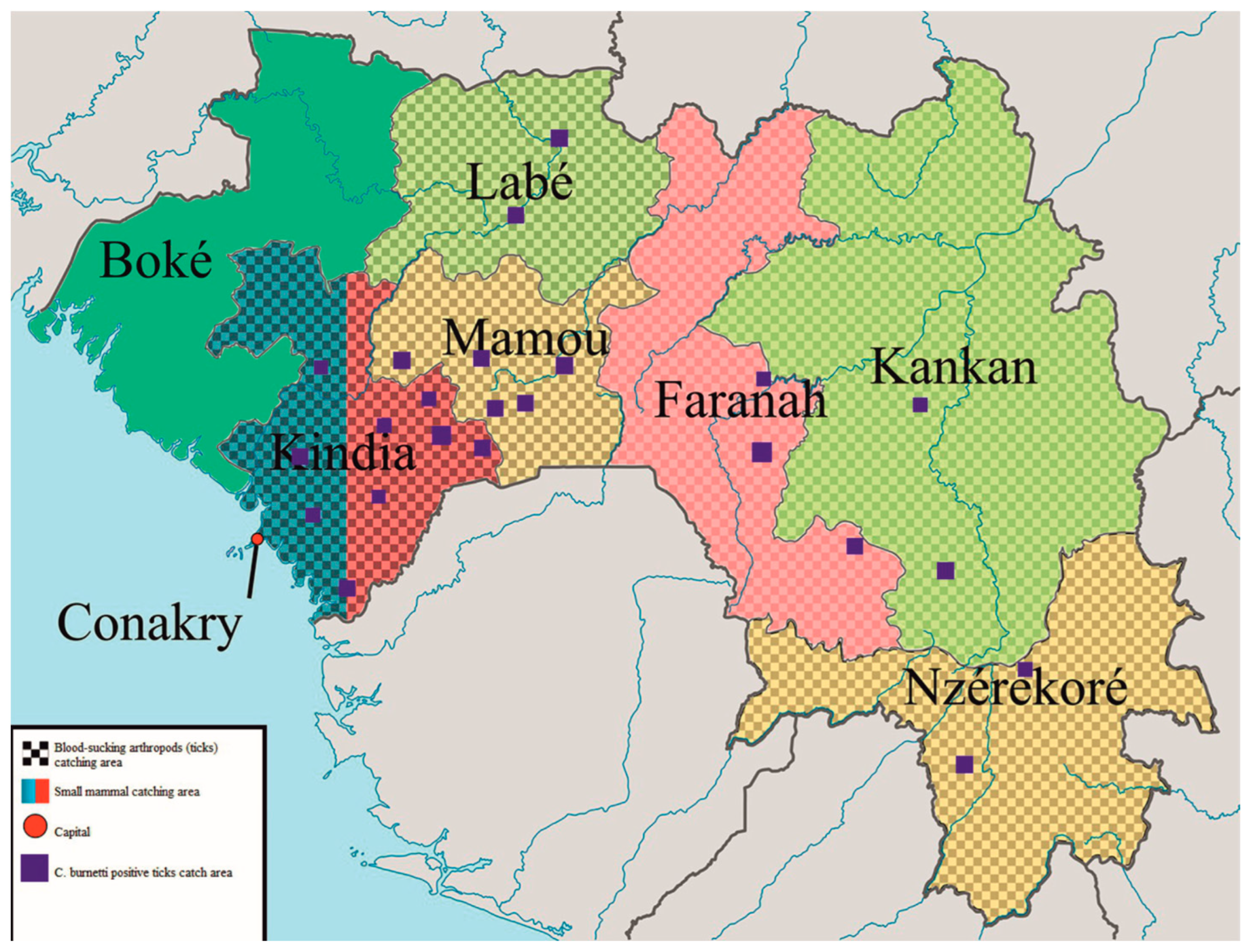
2. Materials and Methods
3. Results
3.1. Coxiella Burnetii DNA Prevalence in Small Mammal Tissue
3.2. Coxiella burnetii DNA Prevalence in Ticks Collected from Cattle
3.3. Abundance of Ticks in Investigated Cattle
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sykes, J.E.; Norris, J.M. Coxiellosis and Q Fever. In Canine and Feline Infectious Diseases; Elsevier Inc.: Amsterdam, The Netherlands, 2014; pp. 320–325. [Google Scholar]
- Wilson, K.H.; Blitchington, R.; Shah, P.; McDonald, G.; Gilmore, R.D.; Mallavia, L.P. Probe directed at a segment of Rickettsia rickettsii rRNA amplified with polymerase chain reaction. J. Clin. Microbiol. 1989, 27, 2692–2696. [Google Scholar] [CrossRef]
- Stein, A.; Saunders, N.; Taylor, A.; Raoult, D. Phylogenic homogeneity of Coxiella burnetii strains as determinated by 16S ribosomal RNA sequencing. FEMS Microbiol. Lett. 1993, 113, 339–344. [Google Scholar] [CrossRef]
- Brann, K.R.; Fullerton, M.S.; Voth, D.E. Coxiella burnetii Requires Host Eukaryotic Initiation Factor 2α Activity for Efficient Intracellular Replication. Infect. Immun. 2020, 88, e00096-20. [Google Scholar] [CrossRef]
- Ullah, Q.; Jamil, T.; Saqib, M.; Iqbal, M.; Neubauer, H. Q Fever—A Neglected Zoonosis. Microorganisms 2022, 10, 1530. [Google Scholar] [CrossRef]
- Gürtler, L.; Bauerfeind, U.; Blümel, J.; Burger, R.; Drosten, C.; Gröner, A.; Heiden, M.; Hildebrandt, M.; Jansen, B.; Offergeld, R.; et al. Coxiella burnetii—Pathogenic Agent of Q (Query) Fever. Transfus. Med. Hemother. Off. Organ Der Dtsch. Fur Transfus. Und Immunhamatol. 2014, 41, 60–72. [Google Scholar]
- Mediannikov, O.; Fenollar, F.; Socolovschi, C.; Diatta, G.; Bassene, H.; Molez, J.F.; Sokhna, C.; Trape, J.F.; Raoult, D. Coxiella burnetii in humans and ticks in rural Senegal. PLoS Negl. Trop. Dis. 2010, 4, e654. [Google Scholar] [CrossRef]
- Valkovska, L.; Mališevs, A.; Kovaļenko, K.; Bērziņš, A.; Grantiņa-Ieviņa, L. Coxiella burnetii DNA in Milk, Milk Products, and Fermented Dairy Products. J. Vet. Res. 2021, 65, 441–447. [Google Scholar] [CrossRef]
- Shapiro, A.; Bosward, K.; Mathews, K.; Vincent, G.; Stenos, J.; Tadepalli, M.; Norris, J. Molecular detection of Coxiella burnetii in raw meat intended for pet consumption. Zoonoses Public Health 2020, 67, 443–452. [Google Scholar] [CrossRef] [PubMed]
- Sireci, G.; Badami, G.D.; Di Liberto, D.; Blanda, V.; Grippi, F.; Di Paola, L.; Guercio, A.; de la Fuente, J.; Torina, A. Recent Advances on the Innate Immune Response to Coxiella burnetii. Front. Cell. Infect. Microbiol. 2021, 11, 754455. [Google Scholar] [CrossRef]
- Malov, V.A.; Ponomarev, S.V.; Tarasevich, I.V.; Kubensky, E.N.; Gorobchenko, A.N.; Pantyukhina, A.N.; Nemilostiva, E.A.; Bogdanova, M.V.; Makhmutov, Y.I. Description of a case of severe Q fever. Ter. Arkhiv 2015, 87, 84–91. [Google Scholar] [CrossRef]
- Melenotte, C.; Protopopescu, C.; Million, M.; Edouard, S.; Carrieri, M.P.; Eldin, C.; Angelakis, E.; Djossou, F.; Bardin, N.; Fournier, P.-E.; et al. Clinical Features and Complications of Coxiella burnetiid Infections From the French National Reference Center for Q Fever. JAMA Netw. Open 2018, 1, e181580. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, S.Y.; Mølbak, K.; Henriksen, T.B.; Krogfelt, K.A.; Larsen, C.S.; Villumsen, S. Adverse pregnancy outcomes and Coxiella burnetii antibodies in pregnant women, Denmark. Emerg. Infect. Dis. 2014, 20, 925–931. [Google Scholar] [CrossRef] [PubMed]
- Maurin, M.; Raoult, D. Q fever. Clin. Microbiol. Rev. 1999, 12, 518–553. [Google Scholar] [CrossRef] [PubMed]
- Celina, S.S.; Cerný, J. Coxiella burnetii in ticks, livestock, pets and wildlife: A mini-review. Front. Vet. Sci. 2022, 9, 1068129. [Google Scholar] [CrossRef]
- Mori, M.; Roest, H.-J. Farming, Q fever and public health: Agricultural practices and beyond. Arch. Public Health 2018, 76, 2. [Google Scholar] [CrossRef]
- Dijkstra, F.; Van Der Hoek, W.; Wijers, N.; Schimmer, B.; Rietveld, A.; Wijkmans, C.J.; Vellema, P.; Schneeberger, P.M. The 2007–2010 Q fever epidemic in the Netherlands: Characteristics of notified acute Q fever patients and the association with dairy goat farming. FEMS Immunol. Med. Microbiol. 2012, 64, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Whelan, J.; Schimmer, B.; Schneeberger, P.; Meekelenkamp, J.; Van Der Hoek, W.; Holle, M.R.R.V.B. Q Fever among Culling Workers, the Netherlands, 2009–2010. Emerg. Infect. Dis. 2011, 17, 1719–1723. [Google Scholar] [CrossRef]
- Rodríguez-Alonso, B.; Almeida, H.; Alonso-Sardón, M.; López-Bernus, A.; Pardo-Lledias, J.; Velasco-Tirado, V.; Carranza-Rodríguez, C.; Pérez-Arellano, J.L.; Belhassen-García, M. Epidemiological scenario of Q fever hospitalized patients in the Spanish Health System: What’s new. Int. J. Infect. Dis. 2020, 90, 226–233. [Google Scholar] [CrossRef]
- Clark, N.J.; Magalhães, R.J.S. Airborne geographical dispersal of Q fever from livestock holdings to human communities: A systematic review and critical appraisal of evidence. BMC Infect. Dis. 2018, 18, 218. [Google Scholar] [CrossRef]
- Dedkov, V.G.; Magassouba, N.; Stukolova, O.A.; Savina, V.A.; Camara, J.; Soropogui, B.; Safonova, M.V.; Semizhon, P.; Platonov, A.E. Differential Laboratory Diagnosis of Acute Fever in Guinea: Preparedness for the Threat of Hemorrhagic Fevers. Int. J. Environ. Res. Public Health 2021, 18, 6022. [Google Scholar] [CrossRef]
- World Health Organization. 2020. Available online: https://apps.who.int/gho/data/node.main.688 (accessed on 26 April 2023).
- Liu, L.; Xu, B.; Fu, Y.; Li, M.; Yang, Y.; Hou, Y.; Wang, S.; Hu, M.; Guo, T.; Jiang, C.; et al. Coxiella burnetii in rodents on Heixiazi Island at the Sino-Russian border. Am. J. Trop. Med. Hyg. 2013, 88, 770–773. [Google Scholar]
- Walker, A.R.; Bouattour, A.; Camicas, J.-L.; Estrada-Peña, A. Ticks of Domestic Animals in Africa: A Guide to Identification of Species; Bioscience Reports: Edinburgh, UK, 2003; p. 221. [Google Scholar]
- Goheen, J.R.; Palmer, T.M.; Charles, G.K.; Helgen, K.M.; Kinyua, S.N.; MacLean, J.E.; Turner, B.L.; Young, H.S.; Pringle, R.M. Piecewise Disassembly of a Large-Herbivore Community across a Rainfall Gradient: The UHURU Experiment. PLoS ONE 2013, 8, e55192. [Google Scholar] [CrossRef]
- Duron, O.; Sidi-Boumedine, K.; Rousset, E.; Moutailler, S.; Jourdain, E. The importance of ticks in Q fever transmission: What has (and has not) been demonstrated? Trends Parasitol. 2015, 31, 536–552. [Google Scholar] [CrossRef]
- Eklund, C.M.; Parker, R.R.; Lackman, D.B.; Ecklund, C.M.; Lockman, D.B. A Case of Q Fever Probably Contracted by Exposure to Ticks in Nature. Public Health Rep. 1947, 62, 1413–1416. [Google Scholar] [CrossRef] [PubMed]
- Pascual-Velasco, F.; Carrascosa-Porras, M.; Martínez-Bernal, M.A.; Jado-García, I. Fiebre Q tras picadura de garrapatas. Enferm. Infecc. Microbiol. Clín. 2007, 25, 360. [Google Scholar] [CrossRef]
- Dubourg, G.; Socolovschi, C.; Del Giudice, P.; Fournier, P.E.; Raoult, D. Scalp eschar and neck lymphadenopathy after tick bite: An emerging syndrome with multiple causes. Eur. J. Clin. Microbiol. Infect. Dis. 2014, 33, 1449–1456. [Google Scholar] [CrossRef]
- Beaman, M.H.; Hung, J. Pericarditis associated with tick-borne Q fever. Aust. N. Z. J. Med. 1989, 19, 254–256. [Google Scholar] [CrossRef] [PubMed]
- Nett, R.J.; Book, E.; Anderson, A.D. Q Fever with Unusual Exposure History: A Classic Presentation of a Commonly Misdiagnosed Disease. Case Rep. Infect. Dis. 2012, 2012, 916142. [Google Scholar] [CrossRef]
- Buaro, M.E. Seroepidemiological and epizootological studies of tick-borne rickettsioses in the Republic of Guinea. Pest Manag. 2013, 1, 22–28. [Google Scholar]
- Chief State Sanitary Physician of the Russian Federation Resolution. Safety of Work with Microorganisms of Risk (Hazard) Groups 1 and 2; Sanitary Rules 1.3.3118-13; Chief state sanitary physician of the Russian Federation resolution: Moscow, Russia, 2014. [Google Scholar]
- Panferova, Y.A.; Freilikhman, O.A.; Tokarevich, N.K.; Karpenko, S.F.; Galimzyanov, K.M. Comparison of diagnostic effectiveness of methods of detection of Coxiella burnetii in blood of patients with Q fever based on amplification of 16s rRNA gene fragments (standard PCR) and groel gene (realtime PCR). J. Microbiol. Epidemiol. Immunobiol. 2016, 93, 70–74. [Google Scholar]
- Freilikhman, O.A.; Tokarevich, N.K.; Panferova, Y.A. Kit for Detection of cu Fever Pathogen in Biological Material by Real-Time Polymerase Chain Reaction (PCR-PV). RU2525059C2, 19 July 2012. [Google Scholar]
- AmpliSence Coxiella burnetii-FL. Detection of the Causative Agent of Q Fever (Coxiella burnetii). Available online: https://www.amplisens.ru/upload/iblock/352/Coxiella%20burnetii-FL.pdf (accessed on 28 April 2023).
- Dedu, I. Ecological Encyclopedic Dictionary. In Ecological Encyclopedic Dictionary; Main Editorial Board of the Moldavian Soviet Encyclopedia (ITU): G. Asaki, Moldavia, 1989. [Google Scholar]
- Centers of the State Sanitary and Epidemiological Surveillance of the Russian Federation. Collecting, Recording and Preparing for Laboratory Examination of Blood-Sicking Arthropod Vectors of Natural Focal Pathogens; Methodological Guidelines 3.1.1027-01; Centers of the State Sanitary and Epidemiological Surveillance of the Russian Federation: Moscow, Russia, 2019. [Google Scholar]
- Naydenova, E.V.; Kalivogui, S.; Kartashov, M.Y.; Boyko, A.V.; Boumbaly, S.; Safronov, V.A.; Zakharov, K.S.; Nassour, A.A.; Drame, F.; Konstantinov, O.K.; et al. New data on the level of immune stratum against Q fever agent in population of the of Republic of Guinea. Russ. J. Infect. Immun. 2021, 11, 165–170. [Google Scholar] [CrossRef]
- Panferova, Y.A. Coxiella burnetii pathogenicity molecular basis. Russ. J. Infect. Immun. Infektsiyaiimmun. 2016, 6, 7–24. [Google Scholar] [CrossRef]
- Körner, S.; Makert, G.R.; Mertens-Scholz, K.; Henning, K.; Pfeffer, M.; Starke, A.; Nijhof, A.M.; Ulbert, S. Uptake and fecal excretion of Coxiella burnetii by Ixodes ricinus and Dermacentor marginatus ticks. Parasites Vectors 2020, 13, 75. [Google Scholar] [CrossRef]
- Almeida, A.P.; Marcili, A.; Leite, R.C.; Nieri-Bastos, F.A.; Domingues, L.N.; Martins, J.R.; Labruna, M.B. Coxiella symbiont in the tick Ornithodoros rostratus (Acari: Argasidae). Ticks Tick-Borne Dis. 2012, 3, 203–206. [Google Scholar] [CrossRef]
- Duron, O.; Jourdain, E.; McCoy, K.D. Diversity and global distribution of the Coxiella intracellular bacterium in seabird ticks. Ticks Tick-Borne Dis. 2014, 5, 557–563. [Google Scholar] [CrossRef]
- Bayer, W.; Maina, J.A. Seasonal pattern of tick load in Bunaji cattle in the subhumid zone of Nigeria. Vet. Parasitol. 1984, 15, 301–307. [Google Scholar] [CrossRef]
- Duron, O.; Noël, V.; McCoy, K.D.; Bonazzi, M.; Sidi-Boumedine, K.; Morel, O.; Vavre, F.; Zenner, L.; Jourdain, E.; Durand, P.; et al. The Recent Evolution of a Maternally-Inherited Endosymbiont of Ticks Led to the Emergence of the Q Fever Pathogen, Coxiella burnetii. PLoS Pathog. 2015, 11, e1004892. [Google Scholar] [CrossRef]
- Smith, T.A.; Driscoll, T.; Gillespie, J.J.; Raghavan, R. A Coxiella-Like Endosymbiont Is a Potential Vitamin Source for the Lone Star Tick. Genome Biol. Evol. 2015, 7, 831–838. [Google Scholar] [CrossRef]
- Spyridaki, I.; Psaroulaki, A.; Vranakis, I.; Tselentis, Y.; Gikas, A. Bacteriostatic and Bactericidal Activities of Tigecycline against Coxiella burnetii and Comparison with Those of Six Other Antibiotics. Antimicrob. Agents Chemother. 2009, 53, 2690–2692. [Google Scholar] [CrossRef]
- Troupin, C.; Ellis, I.; Doukouré, B.; Camara, A.; Keita, M.; Kagbadouno, M.; Bart, J.-M.; Diallo, R.; Lacôte, S.; Marianneau, P.; et al. Seroprevalence of brucellosis, Q fever and Rift Valley fever in domestic ruminants in Guinea in 2017–2019. BMC Vet Res. 2022, 18, 64. [Google Scholar] [CrossRef]
- Balashov, Y.S.; Daiter, A.B. Bloodsucking arthropods and rickettsiae. Sci. Leningr. 1973, 251. [Google Scholar]
- Körner, S.; Makert, G.R.; Ulbert, S.; Pfeffer, M.; Mertens-Scholz, K. The Prevalence of Coxiella burnetii in Hard Ticks in Europe and Their Role in Q Fever Transmission Revisited—A Systematic Review. Front. Vet. Sci. 2021, 8, 655715. [Google Scholar] [CrossRef] [PubMed]
- Ni, J.; Lin, H.; Xu, X.; Ren, Q.; Aizezi, M.; Luo, J.; Luo, Y.; Ma, Z.; Chen, Z.; Tan, Y.; et al. Coxiella burnetii is widespread in ticks (Ixodidae) in the Xinjiang areas of China. BMC Vet. Res. 2020, 16, 317. [Google Scholar] [CrossRef]
- González, J.; González, M.G.; Valcárcel, F.; Sánchez, M.; Martín-Hernández, R.; Tercero, J.M.; Olmeda, A.S. Prevalence of Coxiella burnetii (Legionellales: Coxiellaceae) Infection among Wildlife Species and the Tick Hyalomma lusitanicum (Acari: Ixodidae) in a Meso-Mediterranean Ecosystem. J. Med. Entomol. 2020, 57, 551–556. [Google Scholar] [CrossRef]
- Mancini, F.; Di Luca, M.; Toma, L.; Vescio, F.; Bianchi, R.; Khoury, C.; Marini, L.; Rezza, G.; Ciervo, A. Prevalence of tick-borne pathogens in an urban park in Rome, Italy. Ann. Agric. Environ. Med. 2014, 21, 723–727. [Google Scholar] [CrossRef] [PubMed]
- Yessinou, R.E.; Katja, M.-S.; Heinrich, N.; Farougou, S. Prevalence of Coxiella-infections in ticks—Review and meta-analysis. Ticks Tick-Borne Dis. 2022, 13, 101926. [Google Scholar] [CrossRef] [PubMed]
- Pilloux, L.; Baumgartner, A.; Jaton, K.; Lienhard, R.; Ackermann-Gäumann, R.; Beuret, C.; Greub, G. Prevalence of Anaplasma phagocytophilum and Coxiella burnetii in Ixodes ricinus ticks in Switzerland: An underestimated epidemiologic risk. New Microbes New Infect. 2018, 27, 22–26. [Google Scholar] [CrossRef]
- Knap, N.; Žele, D.; Biškup, U.G.; Avšič-Županc, T.; Vengušt, G. The prevalence of Coxiella burnetii in ticks and animals in Slovenia. BMC Vet. Res. 2019, 15, 368. [Google Scholar] [CrossRef]
- Sprong, H.; Fonville, M.; van Leeuwen, A.D.; Devillers, E.; Ibañez-Justicia, A.; Stroo, A.; Hansford, K.; Cull, B.; Medlock, J.; Heyman, P.; et al. Detection of pathogens in Dermacentor reticulatus in northwestern Europe: Evaluation of a high-throughput array. Heliyon 2019, 5, e01270. [Google Scholar] [CrossRef]
- Reeves, W.K.; Loftis, A.D.; Sanders, F.; Spinks, M.D.; Wills, W.; Denison, A.M.; Dasch, G.A. Borrelia, Coxiella, and Rickettsia in Carios capensis (Acari: Argasidae) from a brown pelican (Pelecanus occidentalis) rookery in South Carolina, USA. Exp. Appl. Acarol. 2006, 39, 321–329. [Google Scholar] [CrossRef]
- Buysse, M.; Plantard, O.; McCoy, K.D.; Duron, O.; Menard, C. Tissue localization of Coxiella-like endosymbionts in three European tick species through fluorescence in situ hybridization. Ticks Tick-Borne Dis. 2019, 10, 798–804. [Google Scholar] [CrossRef]
- Gottlieb, Y.; Lalzar, I.; Klasson, L. Distinctive Genome Reduction Rates Revealed by Genomic Analyses of Two Coxiella-Like Endosymbionts in Ticks. Genome Biol. Evol. 2015, 7, 1779–1796. [Google Scholar] [CrossRef]
- Klee, S.R.; Tyczka, J.; Ellerbrok, H.; Franz, T.; Linke, S.; Baljer, G.; Appel, B. Highly sensitive real-time PCR for specific detection and quantification of Coxiella burnetii. BMC Microbiol. 2006, 6, 2. [Google Scholar] [CrossRef]
- Brennan, R.E.; Samuel, J.E. Evaluation of Coxiella burnetii Antibiotic Susceptibilities by Real-Time PCR Assay. J. Clin. Microbiol. 2003, 41, 1869–1874. [Google Scholar] [CrossRef]
- Stein, A.; Raoult, D. Detection of Coxiella burnetii by DNA amplification using polymerase chain reaction. J. Clin. Microbiol. 1992, 30, 2462–2466. [Google Scholar] [CrossRef]
- Duron, O. The IS1111 insertion sequence used for detection of Coxiella burnetii is widespread in Coxiella-like endosymbionts of ticks. FEMS Microbiol. Lett. 2015, 362, fnv132. [Google Scholar] [CrossRef]
- Jourdain, E.; Duron, O.; Barry, S.; González-Acuña, D.; Sidi-Boumedine, K. Molecular methods routinely used to detect Coxiella burnetii in ticks cross-react with Coxiella-like bacteria. Infect. Ecol. Epidemiol. 2015, 5, 29230. [Google Scholar] [CrossRef]
- Babayani, N.D.; Makati, A. Predictive Analytics of Cattle Host and Environmental and Micro-Climate Factors for Tick Distribution and Abundance at the Livestock–Wildlife Interface in the Lower Okavango Delta of Botswana. Front. Vet. Sci. 2021, 8, 698395. [Google Scholar] [CrossRef]
- Marufu, M.C.; Chimonyo, M.; Mapiye, C.; Dzama, K. Tick loads in cattle raised on sweet and sour rangelands in the low-input farming areas of South Africa. Trop. Anim. Health Prod. 2011, 43, 307–313. [Google Scholar] [CrossRef]
- Faccini, J.L.H.; De Almeida, T.K.; Sousa, I.C.; Costa, L.M., Jr.; Luz, H.R. Temperature effects on the non-parasitic phase of Amblyomma parvum (Acari:Ixodidae) Syst. Appl. Acar. 2021, 1168–1176. [Google Scholar]
- Mapholi, N.O.; Banga, C.; Dzama, K.; Matika, O.; Riggio, V.; Nyangiwe, N.; Maiwashe, A. Prevalence and tick loads in Nguni cattle reared in different environmental conditions across four provinces of South Africa. Vet. World 2022, 15, 1943–1953. [Google Scholar] [CrossRef]
- Okwuonu, E.S.; Andong, F.A.; Ugwuanyi, I.K. Association of ticks with seasons, age, and cattle color of North-Western region of Nigeria. Sci. Afr. 2021, 12, e00832. [Google Scholar] [CrossRef]
- Chepkwony, R.; van Bommel, S.; van Langevelde, F. Interactive effects of biological, human and environmental factors on tick loads in Boran cattle in tropical drylands. Parasit Vectors 2021, 14, 188. [Google Scholar] [CrossRef] [PubMed]
- Russia Federal Service for Supervision in the field of consumer rights protection and human well-being (hereinafter—Rospotrebnadzor). Prevention of Coxiellosis (Q Fever); Sanitary Rules 3.1.7.2811-10; Russia Federal Service for Supervision in the field of consumer rights protection and human well-being (hereinafter—Rospotrebnadzor): Moscow, Russia, 2010. [Google Scholar]
- Titcomb, G.; Allan, B.F.; Ainsworth, T.; Henson, L.; Hedlund, T.; Pringle, R.M.; Palmer, T.; Njoroge, L.; Campana, M.; Fleischer, R.C.; et al. Interacting effects of wildlife loss and climate on ticks and tick-borne disease. Proc. R. Soc. B Biol. Sci. 2017, 284, 20170475. [Google Scholar] [CrossRef]
- Dantas-Torres, F.; Lia, R.P.; Capelli, G.; Otranto, D. Efficiency of flagging and dragging for tick collection. Exp. Appl. Acarol. 2013, 61, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Randolph, S.E. Climate, satellite imagery and the seasonal abundance of the tick Rhipicephalus appendiculatus in southern Africa: A new perspective. Med. Vet. EÈntomol. 1993, 7, 243–258. [Google Scholar] [CrossRef]
- Cumming, G.S. Comparing Climate and Vegetation as Limiting Factors for Species Ranges of African Ticks. Ecology 2002, 83, 255–268. [Google Scholar] [CrossRef]
- Camberlin, P.; Philippon, N. The East African March–May rainy season: Associated atmospheric dynamics and predictability over the 1968–1997 period. J. Clim. 2002, 15, 1002–1019. [Google Scholar] [CrossRef]
| Small Mammals Species | Number of Small Mammals | PI (%) |
|---|---|---|
| Mastomys natalensis | 1 | 1.3 |
| Mastomys erythroleucus | 7 | 8.2 |
| Gerbilliscus guineae | 1 | 25 |
| Rattus rattus | 1 | 1.3 |
| Mus musculus | 1 | 1.3 |
| Total: | 11 |
| Biotype | Setting Up the Trap (Times) | % Traps in Biotype | Number of Traps | % Traps in Biotypes/Total Traps | Small Mammals Captured (n) |
|---|---|---|---|---|---|
| Savannah | 22 | 35.4 | 993 | 51.8 | 86 |
| Neer water | 1 | 1.6 | 7 | 0.4 | 0 |
| Agrocenoses | 5 | 8.1 | 199 | 10.4 | 16 |
| Houses | 25 | 40.3 | 600 | 31.3 | 143 |
| Stores/warehouses | 7 | 11.3 | 47 | 2,4 | 10 |
| Coniferous forest | 2 | 3.2 | 70 | 3.6 | 2 |
| Total: | 62 | 1916 | 250 |
| Cattle (n) | Cattle Positive for Ticks | Number of Ticks | Yearly AI |
|---|---|---|---|
| Total during the period of study | |||
| 303 | 220 | 695 | 2.3 |
| AI by season | |||
| Dry season | |||
| 266 | 183 | 563 | 2.1 |
| Rainy season | |||
| 37 | 37 | 132 | 3.5 |
| Species | Total | PI | Rainy Season | Dry Deason | ||||
|---|---|---|---|---|---|---|---|---|
| Total | PI | % Positive | Total | PI | % Positive | |||
| Amblyomma ariegatum | 544 | 78.27 | 76 | 57.57 | 42.1 | 468 | 83.12 | 16.0 |
| Haemophysalis leachi | 2 | 0.28 | 0 | 0 | 0.0 | 2 | 0.35 | 50.0 |
| Hyalomma truncatum | 26 | 3.74 | 1 | 0.75 | 100.0 | 25 | 4.44 | 20.0 |
| Rhipicephalu annulatus | 38 | 5.46 | 0 | 0 | 0,0 | 38 | 6.74 | 26.3 |
| Rhipicephalus decoloratus | 62 | 8.92 | 48 | 36.36 | 52.1 | 14 | 2.48 | 28.6 |
| Rhipicephalus geigyi | 7 | 1.00 | 7 | 5.30 | 57.1 | 0 | 0 | 0.0 |
| Rhipicephalus sanguineus | 16 | 2.30 | 0 | 0 | 0.0 | 16 | 2.84 | 25.0 |
| Total positive | 695 | 132 | 563 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ohlopkova, O.V.; Yakovlev, S.A.; Emmanuel, K.; Kabanov, A.A.; Odnoshevsky, D.A.; Kartashov, M.Y.; Moshkin, A.D.; Tuchkov, I.V.; Nosov, N.Y.; Kritsky, A.A.; et al. Epidemiology of Zoonotic Coxiella burnetii in The Republic of Guinea. Microorganisms 2023, 11, 1433. https://doi.org/10.3390/microorganisms11061433
Ohlopkova OV, Yakovlev SA, Emmanuel K, Kabanov AA, Odnoshevsky DA, Kartashov MY, Moshkin AD, Tuchkov IV, Nosov NY, Kritsky AA, et al. Epidemiology of Zoonotic Coxiella burnetii in The Republic of Guinea. Microorganisms. 2023; 11(6):1433. https://doi.org/10.3390/microorganisms11061433
Chicago/Turabian StyleOhlopkova, Olesia V., Sergey A. Yakovlev, Kabwe Emmanuel, Alexey A. Kabanov, Dmitry A. Odnoshevsky, Mikhail Yu. Kartashov, Alexey D. Moshkin, Igor V. Tuchkov, Nikita Yu. Nosov, Andrey A. Kritsky, and et al. 2023. "Epidemiology of Zoonotic Coxiella burnetii in The Republic of Guinea" Microorganisms 11, no. 6: 1433. https://doi.org/10.3390/microorganisms11061433
APA StyleOhlopkova, O. V., Yakovlev, S. A., Emmanuel, K., Kabanov, A. A., Odnoshevsky, D. A., Kartashov, M. Y., Moshkin, A. D., Tuchkov, I. V., Nosov, N. Y., Kritsky, A. A., Agalakova, M. A., Davidyuk, Y. N., Khaiboullina, S. F., Morzunov, S. P., N’Fally, M., Bumbali, S., Camara, M. F., Boiro, M. Y., Agafonov, A. P., ... Maksyutov, R. A. (2023). Epidemiology of Zoonotic Coxiella burnetii in The Republic of Guinea. Microorganisms, 11(6), 1433. https://doi.org/10.3390/microorganisms11061433








