Silver Nanoparticles: Review of Antiviral Properties, Mechanism of Action and Applications
Abstract
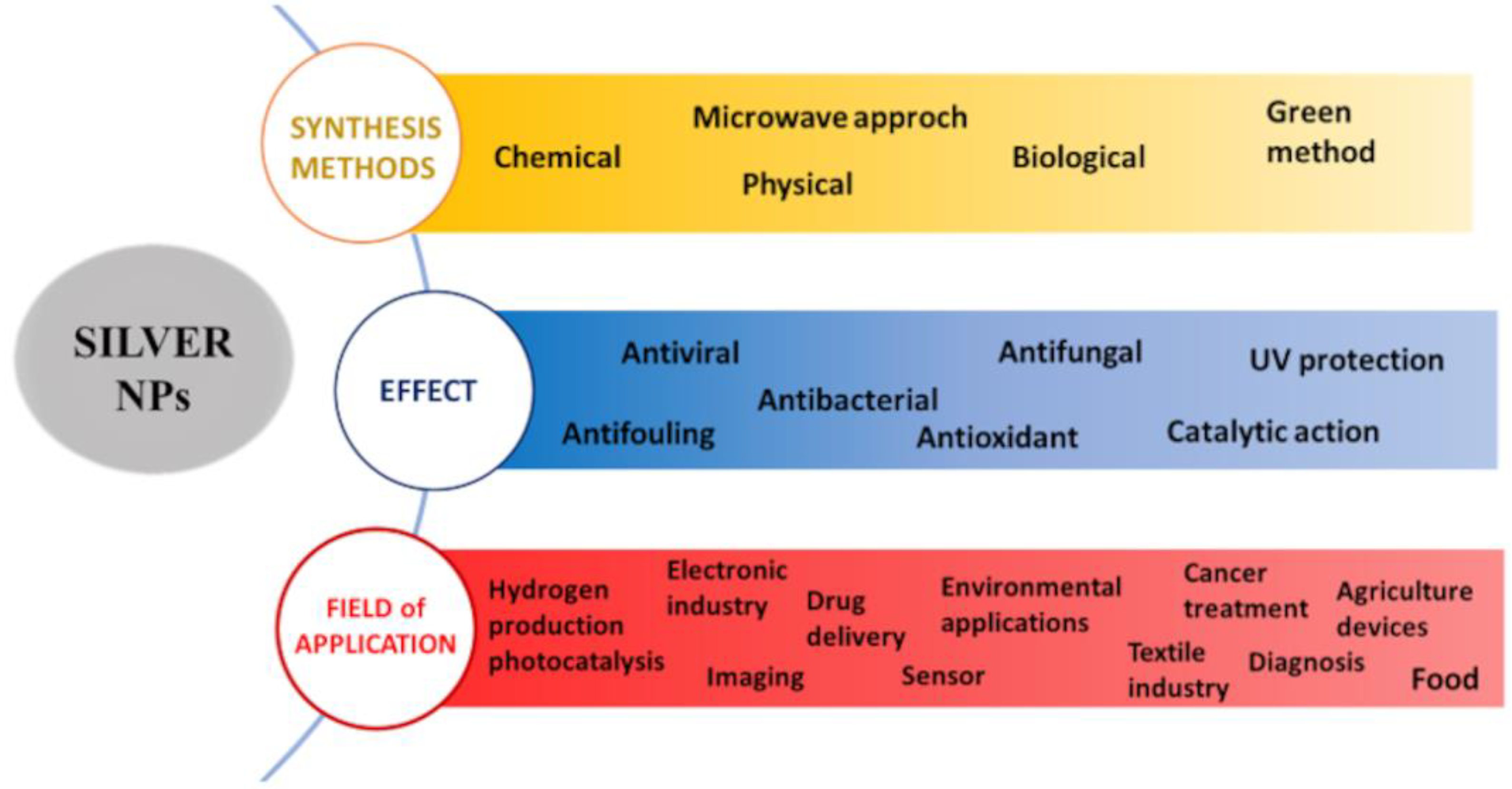
1. Introduction
2. Wide-Spectrum Antiviral Activity of AgNPs
2.1. In Vitro and In Vivo Evidence of AgNP Antiviral Efficacy
2.2. Antiviral Mechanisms of Action of AgNPs
2.2.1. Virucidal Activity of AgNPs
2.2.2. AgNP Inhibition of the Early Steps of Viral Replication
2.2.3. AgNP Inhibition of the Late Steps of Viral Replication
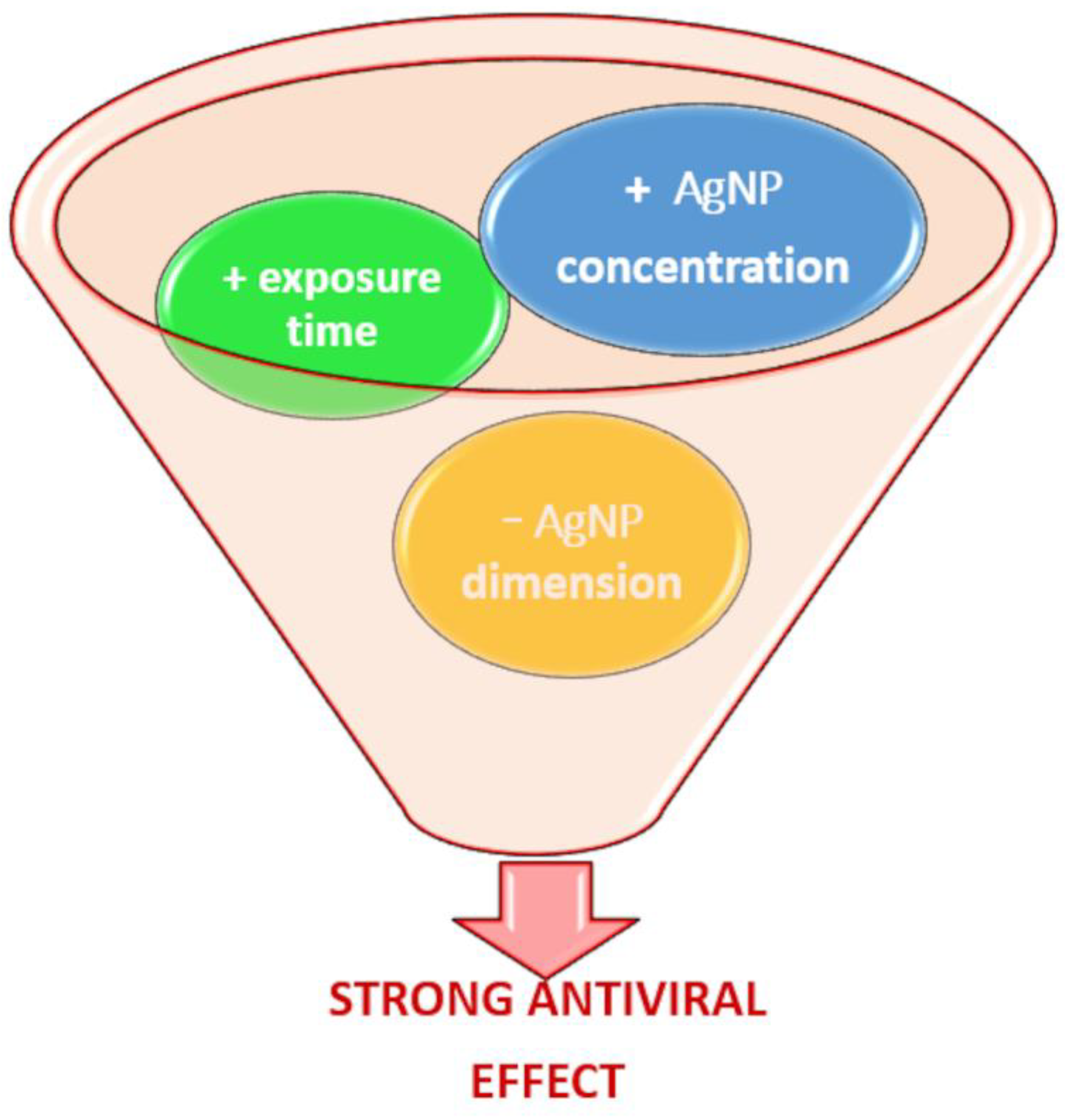
2.3. AgNP Factors Influencing Virucidal Activity
2.3.1. Impact of Size and Concentration on AgNP Antiviral Activity
2.3.2. Impact of AgNP Functionalization on Antiviral Activity
2.3.3. Impact of AgNP Shape on Antiviral Activity
3. Application Fields of AgNPs
3.1. Application in the Human Health Sector
3.2. Veterinary Applications of AgNPs
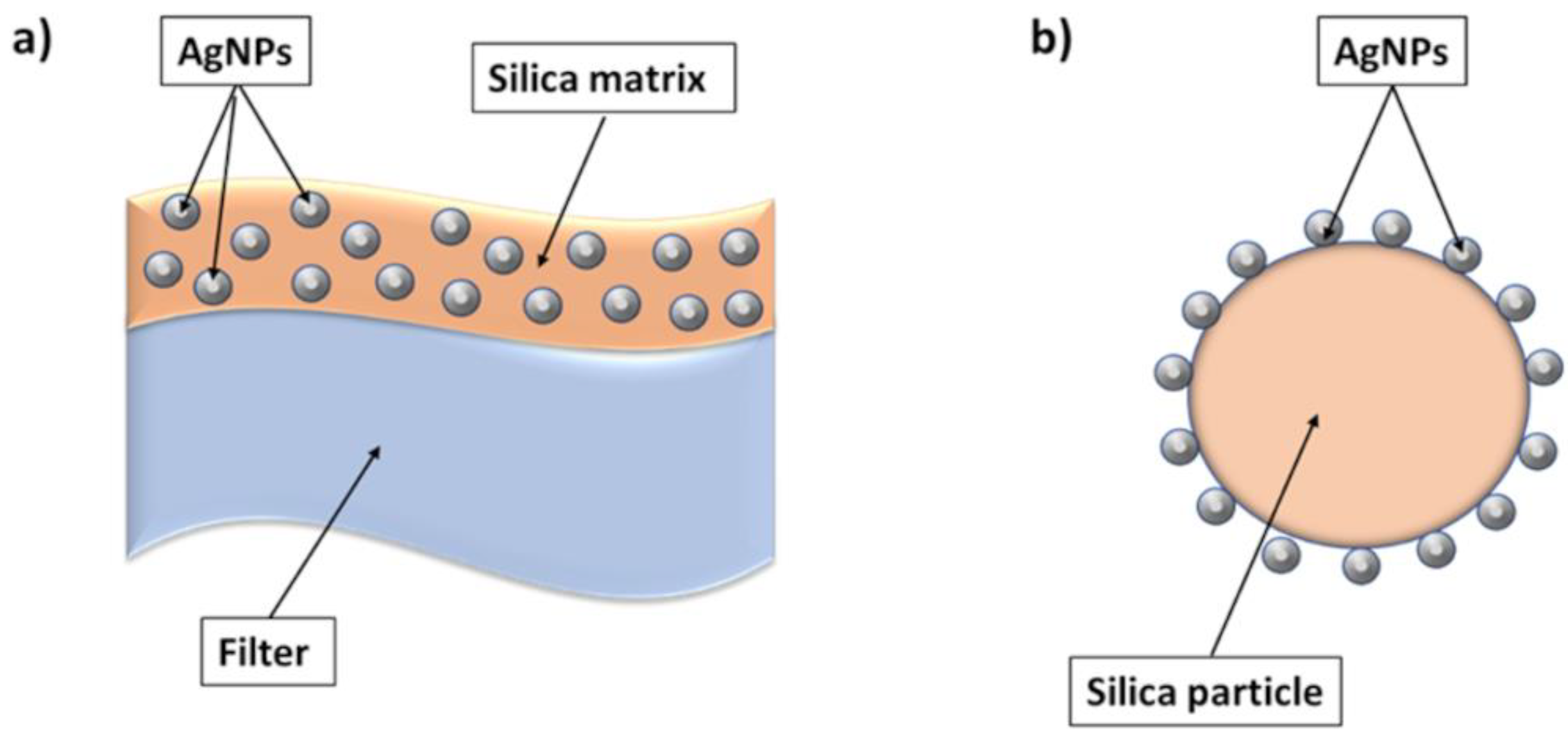
3.3. Applications of AgNPs in Water and Air Filtration Systems
3.3.1. Water Treatment
3.3.2. Air Filtration Systems
3.4. Applications of AgNPs in the Food Industry
3.5. Applications of AgNPs in the Textile Industry
4. Notes about Limitations of AgNPs
5. Conclusions and Future Perspective
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Morens, D.M.; Fauci, A.S. Emerging Pandemic Diseases: How We Got to COVID-19. Cell 2020, 182, 1077–1092. [Google Scholar] [CrossRef] [PubMed]
- Morens, D.M.; Folkers, G.K.; Fauci, A.S. The Challenge of Emerging and Re-Emerging Infectious Diseases. Nature 2004, 430, 242–249. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, B.C.; Lopes Barbosa, M.G.; Silva Olak, A.P.; Belebecha Terezo, N.; Nishi, L.; Watanabe, M.A.; Marinello, P.; Zendrini Rechenchoski, D.; Dejato Rocha, S.P.; Faccin-Galhardi, L.C. Antiviral Therapies: Advances and Perspectives. Fundam. Clin. Pharmacol. 2021, 35, 305–320. [Google Scholar] [CrossRef] [PubMed]
- Mao, H.H.; Chao, S. Advances in Vaccines. Curr. Appl. Pharm. Biotechnol. 2019, 171, 155–188. [Google Scholar]
- Jorge de Souza, T.A.; Rosa Souza, L.R.; Franchi, L.P. Silver Nanoparticles: An Integrated View of Green Synthesis Methods, Transformation in the Environment, and Toxicity. Ecotoxicol. Environ. Saf. 2019, 171, 691–700. [Google Scholar] [CrossRef] [PubMed]
- Yaqoob, A.A.; Umar, K.; Ibrahim, M.N.M. Silver Nanoparticles: Various Methods of Synthesis, Size Affecting Factors and Their Potential Applications—A Review. Appl. Nanosci. 2020, 10, 1369–1378. [Google Scholar] [CrossRef]
- Crisan, C.M.; Mocan, T.; Manolea, M.; Lasca, L.I.; Tăbăran, F.-A.; Mocan, L. Review on Silver Nanoparticles as a Novel Class of Antibacterial Solutions. Appl. Sci. 2021, 11, 1120. [Google Scholar] [CrossRef]
- Rajeshkumar, S.; Bharath, L.V. Mechanism of Plant-Mediated Synthesis of Silver Nanoparticles–A Review on Biomolecules Involved, Characterisation and Antibacterial Activity. Chem. Biol. Interact. 2017, 273, 219–227. [Google Scholar] [CrossRef]
- Siddiqi, K.S.; Husen, A.; Rao, R.A.K. A Review on Biosynthesis of Silver Nanoparticles and Their Biocidal Properties. J. Nanobiotechnol. 2018, 16, 14. [Google Scholar] [CrossRef]
- Qing, Y.; Cheng, L.; Li, R.; Liu, G.; Zhang, Y.; Tang, X.; Wang, J.; Liu, H.; Qin, Y. Potential Antibacterial Mechanism of Silver Nanoparticles and the Optimization of Orthopedic Implants by Advanced Modification Technologies. Int. J. Nanomed. 2018, 13, 3311–3327. [Google Scholar] [CrossRef]
- Jung, W.K.; Koo, H.C.; Kim, K.W.; Shin, S.; Kim, S.H.; Park, Y.H. Antibacterial Activity and Mechanism of Action of the Silver Ion in Staphylococcus Aureus and Escherichia Coli. Appl. Environ. Microbiol. 2008, 74, 2171–2178. [Google Scholar] [CrossRef] [PubMed]
- Durán, N.; Durán, M.; de Jesus, M.B.; Seabra, A.B.; Fávaro, W.J.; Nakazato, G. Silver Nanoparticles: A New View on Mechanistic Aspects on Antimicrobial Activity. Nanomed. Nanotechnol. Biol. Med. 2016, 12, 789–799. [Google Scholar] [CrossRef] [PubMed]
- Jin, J.-C.; Wu, X.-J.; Xu, J.; Wang, B.-B.; Jiang, F.-L.; Liu, Y. Ultrasmall Silver Nanoclusters: Highly Efficient Antibacterial Activity and Their Mechanisms. Biomater. Sci. 2017, 5, 247–257. [Google Scholar] [CrossRef] [PubMed]
- Elechiguerra, J.L.; Burt, J.L.; Morones, J.R.; Camacho-Bragado, A.; Gao, X.; Lara, H.H.; Yacaman, M.J. Interaction of Silver Nanoparticles with HIV-1. J. Nanobiotechnol. 2005, 3, 6. [Google Scholar] [CrossRef] [PubMed]
- Fatima, M.; Zaidi, N.-S.S.; Amraiz, D.; Afzal, F. In Vitro Antiviral Activity of Cinnamomum Cassia and Its Nanoparticles Against H7N3 Influenza A Virus. J. Microbiol. Biotechnol. 2016, 26, 151–159. [Google Scholar] [CrossRef]
- Li, Y.; Lin, Z.; Zhao, M.; Xu, T.; Wang, C.; Hua, L.; Wang, H.; Xia, H.; Zhu, B. Silver Nanoparticle Based Codelivery of Oseltamivir to Inhibit the Activity of the H1N1 Influenza Virus through ROS-Mediated Signaling Pathways. ACS Appl. Mater. Interfaces 2016, 8, 24385–24393. [Google Scholar] [CrossRef]
- Park, S.; Ko, Y.-S.; Lee, S.J.; Lee, C.; Woo, K.; Ko, G. Inactivation of Influenza A Virus via Exposure to Silver Nanoparticle-Decorated Silica Hybrid Composites. Environ. Sci. Pollut. Res. 2018, 25, 27021–27030. [Google Scholar] [CrossRef]
- Sreekanth, T.V.M.; Nagajyothi, P.C.; Muthuraman, P.; Enkhtaivan, G.; Vattikuti, S.V.P.; Tettey, C.O.; Kim, D.H.; Shim, J.; Yoo, K. Ultra-Sonication-Assisted Silver Nanoparticles Using Panax Ginseng Root Extract and Their Anti-Cancer and Antiviral Activities. J. Photochem. Photobiol. B Biol. 2018, 188, 6–11. [Google Scholar] [CrossRef]
- Xiang, D.; Chen, Q.; Pang, L.; Zheng, C. Inhibitory Effects of Silver Nanoparticles on H1N1 Influenza A Virus in Vitro. J. Virol. Methods 2011, 178, 137–142. [Google Scholar] [CrossRef]
- Xiang, D.; Zheng, C.; Zheng, Y.; Li, X.; Yin, J.; O’Conner, M.; Marappan, M.; Miao, Y.; Xiang, B.; Duan, W.; et al. Inhibition of A/Human/Hubei/3/2005 (H3N2) Influenza Virus Infection by Silver Nanoparticles in Vitro and in Vivo. Int. J. Nanomed. 2013, 8, 4103. [Google Scholar] [CrossRef]
- Mori, Y.; Ono, T.; Miyahira, Y.; Nguyen, V.Q.; Matsui, T.; Ishihara, M. Antiviral Activity of Silver Nanoparticle/Chitosan Composites against H1N1 Influenza A Virus. Nanoscale Res. Lett. 2013, 8, 93. [Google Scholar] [CrossRef] [PubMed]
- Galdiero, S.; Rai, M.; Gade, A.; Falanga, A.; Incoronato, N.; Russo, L.; Galdiero, M.; Gaikwad, S.; Ingle, A. Antiviral Activity of Mycosynthesized Silver Nanoparticles against Herpes Simplex Virus and Human Parainfluenza Virus Type 3. Int. J. Nanomed. 2013, 8, 4303. [Google Scholar] [CrossRef] [PubMed]
- Haggag, E.; Elshamy, A.; Rabeh, M.; Gabr, N.; Salem, M.; Youssif, K.; Samir, A.; Bin Muhsinah, A.; Alsayari, A.; Abdelmohsen, U.R. Antiviral Potential of Green Synthesized Silver Nanoparticles of Lampranthus coccineus and Malephora lutea. Int. J. Nanomed. 2019, 14, 6217–6229. [Google Scholar] [CrossRef] [PubMed]
- Orlowski, P.; Tomaszewska, E.; Gniadek, M.; Baska, P.; Nowakowska, J.; Sokolowska, J.; Nowak, Z.; Donten, M.; Celichowski, G.; Grobelny, J.; et al. Tannic Acid Modified Silver Nanoparticles Show Antiviral Activity in Herpes Simplex Virus Type 2 Infection. PLoS ONE 2014, 9, e104113. [Google Scholar] [CrossRef]
- Szymańska, E.; Orłowski, P.; Winnicka, K.; Tomaszewska, E.; Bąska, P.; Celichowski, G.; Grobelny, J.; Basa, A.; Krzyżowska, M. Multifunctional Tannic Acid/Silver Nanoparticle-Based Mucoadhesive Hydrogel for Improved Local Treatment of HSV Infection: In Vitro and In Vivo Studies. Int. J. Mol. Sci. 2018, 19, 387. [Google Scholar] [CrossRef]
- Baram-Pinto, D.; Shukla, S.; Perkas, N.; Gedanken, A.; Sarid, R. Inhibition of Herpes Simplex Virus Type 1 Infection by Silver Nanoparticles Capped with Mercaptoethane Sulfonate. Bioconjugate Chem. 2009, 20, 1497–1502. [Google Scholar] [CrossRef]
- Bekele, A.Z.; Gokulan, K.; Williams, K.M.; Khare, S. Dose and Size-Dependent Antiviral Effects of Silver Nanoparticles on Feline Calicivirus, a Human Norovirus Surrogate. Foodborne Pathog. Dis. 2016, 13, 239–244. [Google Scholar] [CrossRef]
- Sinclair, T.R.; van den Hengel, S.K.; Raza, B.G.; Rutjes, S.A.; de Roda Husman, A.M.; Peijnenburg, W.J.G.M.; Roesink, H.D.W.; de Vos, W.M. Surface Chemistry-Dependent Antiviral Activity of Silver Nanoparticles. Nanotechnology 2021, 32, 365101. [Google Scholar] [CrossRef]
- El-Mohamady, R.S.; Ghattas, T.A.; Zawrah, M.F.; Abd El-Hafeiz, Y.G.M. Inhibitory Effect of Silver Nanoparticles on Bovine Herpesvirus-1. Int. J. Vet. Sci. Med. 2018, 6, 296–300. [Google Scholar] [CrossRef]
- Lv, X.; Wang, P.; Bai, R.; Cong, Y.; Suo, S.; Ren, X.; Chen, C. Inhibitory Effect of Silver Nanomaterials on Transmissible Virus-Induced Host Cell Infections. Biomaterials 2014, 35, 4195–4203. [Google Scholar] [CrossRef]
- Amooaghaie, R.; Saeri, M.R.; Azizi, M. Synthesis, Characterization and Biocompatibility of Silver Nanoparticles Synthesized from Nigella Sativa Leaf Extract in Comparison with Chemical Silver Nanoparticles. Ecotoxicol. Environ. Saf. 2015, 120, 400–408. [Google Scholar] [CrossRef] [PubMed]
- Sharmin, S.; Rahaman, M.M.; Sarkar, C.; Atolani, O.; Islam, M.T.; Adeyemi, O.S. Nanoparticles as Antimicrobial and Antiviral Agents: A Literature-Based Perspective Study. Heliyon 2021, 7, e06456. [Google Scholar] [CrossRef] [PubMed]
- Vargas-Hernandez, M.; Macias-Bobadilla, I.; Guevara-Gonzalez, R.G.; Rico-Garcia, E.; Ocampo-Velazquez, R.V.; Avila-Juarez, L.; Torres-Pacheco, I. Nanoparticles as Potential Antivirals in Agriculture. Agriculture 2020, 10, 444. [Google Scholar] [CrossRef]
- Chen, L.; Liang, J. An Overview of Functional Nanoparticles as Novel Emerging Antiviral Therapeutic Agents. Mater. Sci. Eng. C 2020, 112, 110924. [Google Scholar] [CrossRef]
- Valdez-Salas, B.; Beltran-Partida, E.; Cheng, N.; Salvador-Carlos, J.; Valdez-Salas, E.A.; Curiel-Alvarez, M.; Ibarra-Wiley, R. Promotion of Surgical Masks Antimicrobial Activity by Disinfection and Impregnation with Disinfectant Silver Nanoparticles. Int. J. Nanomed. 2021, 16, 2689–2702. [Google Scholar] [CrossRef]
- Jeremiah, S.S.; Miyakawa, K.; Morita, T.; Yamaoka, Y.; Ryo, A. Potent Antiviral Effect of Silver Nanoparticles on SARS-CoV-2. Biochem. Biophys. Res. Commun. 2020, 533, 195–200. [Google Scholar] [CrossRef]
- Almanza-Reyes, H.; Moreno, S.; Plascencia-López, I.; Alvarado-Vera, M.; Patrón-Romero, L.; Borrego, B.; Reyes-Escamilla, A.; Valencia-Manzo, D.; Brun, A.; Pestryakov, A.; et al. Evaluation of Silver Nanoparticles for the Prevention of SARS-CoV-2 Infection in Health Workers: In Vitro and In Vivo. PLoS ONE 2021, 16, e0256401. [Google Scholar] [CrossRef]
- Karagoz, S.; Kiremitler, N.B.; Sarp, G.; Pekdemir, S.; Salem, S.; Goksu, A.G.; Onses, M.S.; Sozdutmaz, I.; Sahmetlioglu, E.; Ozkara, E.S.; et al. Antibacterial, Antiviral, and Self-Cleaning Mats with Sensing Capabilities Based on Electrospun Nanofibers Decorated with ZnO Nanorods and Ag Nanoparticles for Protective Clothing Applications. ACS Appl. Mater. Interfaces 2021, 13, 5678–5690. [Google Scholar] [CrossRef]
- Hamouda, T.; Ibrahim, H.M.; Kafafy, H.H.; Mashaly, H.M.; Mohamed, N.H.; Aly, N.M. Preparation of Cellulose-Based Wipes Treated with Antimicrobial and Antiviral Silver Nanoparticles as Novel Effective High-Performance Coronavirus Fighter. Int. J. Biol. Macromol. 2021, 181, 990–1002. [Google Scholar] [CrossRef]
- Chen, Y.-N.; Hsueh, Y.-H.; Hsieh, C.-T.; Tzou, D.-Y.; Chang, P.-L. Antiviral Activity of Graphene–Silver Nanocomposites against Non-Enveloped and Enveloped Viruses. Int. J. Environ. Res. Public Health 2016, 13, 430. [Google Scholar] [CrossRef]
- Ju, Y.; Han, T.; Yin, J.; Li, Q.; Chen, Z.; Wei, Z.; Zhang, Y.; Dong, L. Bumpy Structured Nanofibrous Membrane as a Highly Efficient Air Filter with Antibacterial and Antiviral Property. Sci. Total Environ. 2021, 777, 145768. [Google Scholar] [CrossRef] [PubMed]
- Huy, T.Q.; Hien Thanh, N.T.; Thuy, N.T.; Chung, P.V.; Hung, P.N.; Le, A.-T.; Hong Hanh, N.T. Cytotoxicity and Antiviral Activity of Electrochemical–Synthesized Silver Nanoparticles against Poliovirus. J. Virol. Methods 2017, 241, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Lv, X.; Wang, H.; Su, A.; Chu, Y. A Novel Approach for Sericin-Conjugated Silver Nanoparticle Synthesis and Their Potential as Microbicide Candidates. J. Microbiol. Biotechnol. 2018, 28, 1367–1375. [Google Scholar] [CrossRef] [PubMed]
- Orłowski, P.; Kowalczyk, A.; Tomaszewska, E.; Ranoszek-Soliwoda, K.; Węgrzyn, A.; Grzesiak, J.; Celichowski, G.; Grobelny, J.; Eriksson, K.; Krzyzowska, M. Antiviral Activity of Tannic Acid Modified Silver Nanoparticles: Potential to Activate Immune Response in Herpes Genitalis. Viruses 2018, 10, 524. [Google Scholar] [CrossRef]
- Morris, D.; Ansar, M.; Speshock, J.; Ivanciuc, T.; Qu, Y.; Casola, A.; Garofalo, R. Antiviral and Immunomodulatory Activity of Silver Nanoparticles in Experimental RSV Infection. Viruses 2019, 11, 732. [Google Scholar] [CrossRef]
- Yang, X.X.; Li, C.M.; Huang, C.Z. Curcumin Modified Silver Nanoparticles for Highly Efficient Inhibition of Respiratory Syncytial Virus Infection. Nanoscale 2016, 8, 3040–3048. [Google Scholar] [CrossRef]
- Khandelwal, N.; Kaur, G.; Chaubey, K.K.; Singh, P.; Sharma, S.; Tiwari, A.; Singh, S.V.; Kumar, N. Silver Nanoparticles Impair Peste Des Petits Ruminants Virus Replication. Virus Res. 2014, 190, 1–7. [Google Scholar] [CrossRef]
- Sharma, V.; Kaushik, S.; Pandit, P.; Dhull, D.; Yadav, J.P.; Kaushik, S. Green Synthesis of Silver Nanoparticles from Medicinal Plants and Evaluation of Their Antiviral Potential against Chikungunya Virus. Appl. Microbiol. Biotechnol. 2019, 103, 881–891. [Google Scholar] [CrossRef]
- Sharma, Y.; Kawatra, A.; Sharma, V.; Dhull, D.; Kaushik, S.; Yadav, J.P.; Kaushik, S. In-Vitro and in-Silico Evaluation of the Anti-Chikungunya Potential of Psidium Guajava Leaf Extract and Their Synthesized Silver Nanoparticles. Virus Dis. 2021, 32, 260–265. [Google Scholar] [CrossRef]
- Shady, N.H.; Khattab, A.R.; Ahmed, S.; Liu, M.; Quinn, R.J.; Fouad, M.A.; Kamel, M.S.; Muhsinah, A.B.; Krischke, M.; Mueller, M.J.; et al. Hepatitis C Virus NS3 Protease and Helicase Inhibitors from Red Sea Sponge (Amphimedon) Species in Green Synthesized Silver Nanoparticles Assisted by in Silico Modeling and Metabolic Profiling. Int. J. Nanomed. 2020, 15, 3377–3389. [Google Scholar] [CrossRef]
- Murugan, K.; Aruna, P.; Panneerselvam, C.; Madhiyazhagan, P.; Paulpandi, M.; Subramaniam, J.; Rajaganesh, R.; Wei, H.; Alsalhi, M.S.; Devanesan, S.; et al. Fighting Arboviral Diseases: Low Toxicity on Mammalian Cells, Dengue Growth Inhibition (In Vitro), and Mosquitocidal Activity of Centroceras Clavulatum-Synthesized Silver Nanoparticles. Parasitol. Res. 2016, 115, 651–662. [Google Scholar] [CrossRef] [PubMed]
- Murugan, K.; Dinesh, D.; Paulpandi, M.; Althbyani, A.D.M.; Subramaniam, J.; Madhiyazhagan, P.; Wang, L.; Suresh, U.; Kumar, P.M.; Mohan, J.; et al. Nanoparticles in the Fight against Mosquito-Borne Diseases: Bioactivity of Bruguiera cylindrica-Synthesized Nanoparticles against Dengue Virus DEN-2 (In Vitro) and Its Mosquito Vector Aedes aegypti (Diptera: Culicidae). Parasitol. Res. 2015, 114, 4349–4361. [Google Scholar] [CrossRef] [PubMed]
- Sujitha, V.; Murugan, K.; Paulpandi, M.; Panneerselvam, C.; Suresh, U.; Roni, M.; Nicoletti, M.; Higuchi, A.; Madhiyazhagan, P.; Subramaniam, J.; et al. Green-Synthesized Silver Nanoparticles as a Novel Control Tool against Dengue Virus (DEN-2) and Its Primary Vector Aedes aegypti. Parasitol. Res. 2015, 114, 3315–3325. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Lin, Z.; Lui, V.C.H.; Wong, K.K.Y.; Tam, P.K.H.; Lee, P.; Lok, C.N.; Lamb, J.R.; Chen, Y.; Xia, H. Silver Nanoparticle Treatment Ameliorates Biliary Atresia Syndrome in Rhesus Rotavirus Inoculated Mice. Nanomed. Nanotechnol. Biol. Med. 2017, 13, 1041–1050. [Google Scholar] [CrossRef]
- Shimabuku, Q.L.; Arakawa, F.S.; Fernandes Silva, M.; Ferri Coldebella, P.; Ueda-Nakamura, T.; Fagundes-Klen, M.R.; Bergamasco, R. Water Treatment with Exceptional Virus Inactivation Using Activated Carbon Modified with Silver (Ag) and Copper Oxide (CuO) Nanoparticles. Environ. Technol. 2017, 38, 2058–2069. [Google Scholar] [CrossRef]
- Borrego, B.; Lorenzo, G.; Mota-Morales, J.D.; Almanza-Reyes, H.; Mateos, F.; López-Gil, E.; de la Losa, N.; Burmistrov, V.A.; Pestryakov, A.N.; Brun, A.; et al. Potential Application of Silver Nanoparticles to Control the Infectivity of Rift Valley Fever Virus In Vitro and In Vivo. Nanomed. Nanotechnol. Biol. Med. 2016, 12, 1185–1192. [Google Scholar] [CrossRef]
- Castro-Mayorga, J.L.; Randazzo, W.; Fabra, M.J.; Lagaron, J.M.; Aznar, R.; Sánchez, G. Antiviral Properties of Silver Nanoparticles against Norovirus Surrogates and Their Efficacy in Coated Polyhydroxyalkanoates Systems. LWT-Food Sci. Technol. 2017, 79, 503–510. [Google Scholar] [CrossRef]
- Trefry, J.C.; Wooley, D. Silver Nanoparticles Inhibit Vaccinia Virus Infection by Preventing Viral Entry through a Macropinocytosis-Dependent Mechanism. J. Biomed. Nanotechnol. 2013, 9, 1624–1635. [Google Scholar] [CrossRef]
- Chen, N.; Zheng, Y.; Yin, J.; Li, X.; Zheng, C. Inhibitory Effects of Silver Nanoparticles against Adenovirus Type 3 in Vitro. J. Virol. Methods 2013, 193, 470–477. [Google Scholar] [CrossRef]
- Lu, L.; Sun, R.W.-Y.; Chen, R.; Hui, C.-K.; Ho, C.-M.; Luk, J.M.; Lau, G.K.; Che, C.-M. Silver Nanoparticles Inhibit Hepatitis B Virus Replication. Antivir. Ther. 2008, 13, 253–262. [Google Scholar] [CrossRef]
- García-Serradilla, M.; Risco, C. Light and Electron Microscopy Imaging Unveils New Aspects of the Antiviral Capacity of Silver Nanoparticles in Bunyavirus-Infected Cells. Virus Res. 2021, 302, 198444. [Google Scholar] [CrossRef] [PubMed]
- Pangestika, R.; Ernawati, R. Antiviral Activity Effect of Silver Nanoparticles (Agnps) Solution Against the Growth of Infectious Bursal Disease Virus on Embryonated Chicken Eggs with Elisa Test. KnE Life Sci. 2017, 3, 536. [Google Scholar] [CrossRef]
- Balagna, C.; Francese, R.; Perero, S.; Lembo, D.; Ferraris, M. Nanostructured Composite Coating Endowed with Antiviral Activity against Human Respiratory Viruses Deposited on Fibre-Based Air Filters. Surf. Coat. Technol. 2021, 409, 126873. [Google Scholar] [CrossRef]
- Salem, S.S.; Fouda, A. Green Synthesis of Metallic Nanoparticles and Their Prospective Biotechnological Applications: An Overview. Biol. Trace Elem. Res. 2021, 199, 344–370. [Google Scholar] [CrossRef]
- Galdiero, S.; Falanga, A.; Vitiello, M.; Cantisani, M.; Marra, V.; Galdiero, M. Silver Nanoparticles as Potential Antiviral Agents. Molecules 2011, 16, 8894–8918. [Google Scholar] [CrossRef] [PubMed]
- Ciriminna, R.; Albo, Y.; Pagliaro, M. New Antivirals and Antibacterials Based on Silver Nanoparticles. Chem. Med. Chem. 2020, 15, 1619–1623. [Google Scholar] [CrossRef] [PubMed]
- Hu, R.L.; Li, S.R.; Kong, F.J.; Hou, R.J.; Guan, X.L.; Guo, F. Inhibition Effect of Silver Nanoparticles on Herpes Simplex Virus 2. Genet. Mol. Res. 2014, 13, 7022–7028. [Google Scholar] [CrossRef]
- Burdușel, A.-C.; Gherasim, O.; Grumezescu, A.M.; Mogoantă, L.; Ficai, A.; Andronescu, E. Biomedical Applications of Silver Nanoparticles: An Up-to-Date Overview. Nanomaterials 2018, 8, 681. [Google Scholar] [CrossRef]
- Kirubaharan, C.J.; Kalpana, D.; Lee, Y.S.; Kim, A.R.; Yoo, D.J.; Nahm, K.S.; Kumar, G.G. Biomediated Silver Nanoparticles for the Highly Selective Copper(II) Ion Sensor Applications. Ind. Eng. Chem. Res. 2012, 51, 7441–7446. [Google Scholar] [CrossRef]
- Kale, S.K.; Parishwad, G.V.; Patil, A.S.N.H.A.S. Emerging Agriculture Applications of Silver Nanoparticles. ES Food Agrofor. 2021, 3, 17–22. [Google Scholar] [CrossRef]
- Microban Silver Antimicrobial Technology. Microban. Available online: https://www.microban.com/antimicrobial-solutions/technologies/microban-silver-technology (accessed on 16 February 2022).
- Tecnologia SilverShield® Con Argento Antibatterico. Microban. Available online: https://www.microban.com/it/odor-control/technologies/silvershield (accessed on 16 February 2022).
- Abbigliamento Intimo Tecnico in Argento. Available online: https://www.silverskin.it/?gclid=EAIaIQobChMIlvH7yO2D9gIVIJBoCR2l_g-rEAAYASAAEgKoJ_D_BwE (accessed on 16 February 2022).
- ICOSAN DEFEND AG-Pittura Igienizzante Con Ioni D’argento | Colorificio Postumia. Available online: https://www.colorificiopostumia.it/prodotto/icosan-defend-ag-pittura-igienizzante-con-ioni-dargento (accessed on 16 February 2022).
- Face Mask FFP2 with Silver ANTI-COVID19. Available online: https://www.nanosilver.eu/Face-mask-FFP2-with-silver-ANTI-COVID19 (accessed on 16 February 2022).
- Hodek, J.; Zajícová, V.; Lovětinská-Šlamborová, I.; Stibor, I.; Müllerová, J.; Weber, J. Protective Hybrid Coating Containing Silver, Copper and Zinc Cations Effective against Human Immunodeficiency Virus and Other Enveloped Viruses. BMC Microbiol. 2016, 16, 56. [Google Scholar] [CrossRef] [PubMed]
- Fayaz, A.M.; Ao, Z.; Girilal, M.; Chen, L.; Xiao, X.; Kalaichelvan, P.T.; Yao, X. Inactivation of Microbial Infectiousness by Silver Nanoparticles-Coated Condom: A New Approach to Inhibit HIV-and HSV-Transmitted Infection. Int. J. Nanomed. 2012, 7, 5007. [Google Scholar]
- Balagna, C.; Perero, S.; Percivalle, E.; Nepita, E.V.; Ferraris, M. Virucidal Effect against Coronavirus SARS-CoV-2 of a Silver Nanocluster/Silica Composite Sputtered Coating. Open Ceram. 2020, 1, 100006. [Google Scholar] [CrossRef]
- Bogdanchikova, N.; Vazquez-Munoz, R.; Huerta-Saquero, A.; Pena-Jasso, A.; Aguilar-Uzcanga, G.; Picos-Díaz, P.; Pestryakov, A.; Burmistrov, V.; Martynyuk, O.; Vazquez Gomez, R.; et al. Silver Nanoparticles Composition for Treatment of Distemper in Dogs. Int. J. Nanotechnol. 2016, 13, 227. [Google Scholar] [CrossRef]
- Camacho-Jiménez, L.; Álvarez-Sánchez, A.R.; Mejía-Ruíz, C.H. Silver Nanoparticles (AgNPs) as Antimicrobials in Marine Shrimp Farming: A Review. Aquac. Rep. 2020, 18, 100512. [Google Scholar] [CrossRef]
- Juarez-Moreno, K.; Mejía-Ruiz, C.H.; Díaz, F.; Reyna-Verdugo, H.; Re, A.D.; Vazquez-Felix, E.F.; Sánchez-Castrejón, E.; Mota-Morales, J.D.; Pestryakov, A.; Bogdanchikova, N. Effect of Silver Nanoparticles on the Metabolic Rate, Hematological Response, and Survival of Juvenile White Shrimp Litopenaeus vannamei. Chemosphere 2017, 169, 716–724. [Google Scholar] [CrossRef]
- Mehmood, Y.; Farooq, U.; Yousaf, H.; Riaz, H.; Mahmood, R.K.; Nawaz, A.; Abid, Z.; Gondal, M.; Malik, N.S.; Barkat, K.; et al. Antiviral Activity of Green Silver Nanoparticles Produced Using Aqueous Buds Extract of Syzygium aromaticum. Pak. J. Pharm. Sci. 2020, 33, 839–845. [Google Scholar]
- De Gusseme, B.; Sintubin, L.; Baert, L.; Thibo, E.; Hennebel, T.; Vermeulen, G.; Uyttendaele, M.; Verstraete, W.; Boon, N. Biogenic Silver for Disinfection of Water Contaminated with Viruses. Appl. Environ. Microbiol. 2010, 76, 1082–1087. [Google Scholar] [CrossRef]
- Liga, M.V.; Bryant, E.L.; Colvin, V.L.; Li, Q. Virus Inactivation by Silver Doped Titanium Dioxide Nanoparticles for Drinking Water Treatment. Water Res. 2011, 45, 535–544. [Google Scholar] [CrossRef]
- Nangmenyi, G.; Li, X.; Mehrabi, S.; Mintz, E.; Economy, J. Silver-Modified Iron Oxide Nanoparticle Impregnated Fiberglass for Disinfection of Bacteria and Viruses in Water. Mater. Lett. 2011, 65, 1191–1193. [Google Scholar] [CrossRef]
- Park, S.; Park, H.H.; Kim, S.Y.; Kim, S.J.; Woo, K.; Ko, G. Antiviral Properties of Silver Nanoparticles on a Magnetic Hybrid Colloid. Appl. Environ. Microbiol. 2014, 80, 2343–2350. [Google Scholar] [CrossRef]
- Bharti, S.; Mukherji, S.; Mukherji, S. Antiviral Application of Colloidal and Immobilized Silver Nanoparticles. Nanotechnology 2021, 32, 205102. [Google Scholar] [CrossRef]
- Joe, Y.H.; Park, D.H.; Hwang, J. Evaluation of Ag Nanoparticle Coated Air Filter against Aerosolized Virus: Anti-Viral Efficiency with Dust Loading. J. Hazard. Mater. 2016, 301, 547–553. [Google Scholar] [CrossRef]
- Wang, I.-J.; Chen, Y.-C.; Su, C.; Tsai, M.-H.; Shen, W.-T.; Bai, C.-H.; Yu, K.-P. Effectiveness of the Nanosilver/TiO 2-Chitosan Antiviral Filter on the Removal of Viral Aerosols. J. Aerosol Med. Pulm. Drug Deliv. 2021, 34, 293–302. [Google Scholar] [CrossRef] [PubMed]
- Pelet, T.; Wallach, D.F.H. Composition for Inactivating an Enveloped Virus. U.S. Patent 9526700B2, 27 December 2016. [Google Scholar]
- Shao, W.; Liu, X.; Min, H.; Dong, G.; Feng, Q.; Zuo, S. Preparation, Characterization, and Antibacterial Activity of Silver Nanoparticle-Decorated Graphene Oxide Nanocomposite. ACS Appl. Mater. Interfaces 2015, 7, 6966–6973. [Google Scholar] [CrossRef]
- Baron, M.D.; Parida, S.; Oura, C.A.L. Peste Des Petits Ruminants: A Suitable Candidate for Eradication? Vet. Rec. 2011, 169, 16–21. [Google Scholar] [CrossRef]
- Khalid, M.; Khalid, N.; Ahmed, I.; Hanif, R.; Ismail, M.; Janjua, H.A. Comparative Studies of Three Novel Freshwater Microalgae Strains for Synthesis of Silver Nanoparticles: Insights of Characterization, Antibacterial, Cytotoxicity and Antiviral Activities. J. Appl. Phycol. 2017, 29, 1851–1863. [Google Scholar] [CrossRef]
- Abbaszadegan, M.; Lechevallier, M.; Gerba, C. Occurrence of Viruses in US Groundwaters. J. Am. Water Works Assoc. 2003, 95, 107–120. [Google Scholar] [CrossRef]
- Hamza, I.A.; Jurzik, L.; Stang, A.; Sure, K.; Überla, K.; Wilhelm, M. Detection of Human Viruses in Rivers of a Densly-Populated Area in Germany Using a Virus Adsorption Elution Method Optimized for PCR Analyses. Water Res. 2009, 43, 2657–2668. [Google Scholar] [CrossRef]
- Wong, M.; Kumar, L.; Jenkins, T.M.; Xagoraraki, I.; Phanikumar, M.S.; Rose, J.B. Evaluation of Public Health Risks at Recreational Beaches in Lake Michigan via Detection of Enteric Viruses and a Human-Specific Bacteriological Marker. Water Res. 2009, 43, 1137–1149. [Google Scholar] [CrossRef] [PubMed]
- Yates, M.V.; Malley, J.; Rochelle, P.; Hoffman, R. Effect of Adenovirus Resistance on UV Disinfection Requirements: A Report on the State of Adenovirus Science. J. Am. Water Work. Assoc. 2006, 98, 93–106. [Google Scholar] [CrossRef]
- Liberti, L.; Notarnicola, M.; Petruzzelli, D. Advanced Treatment for Municipal Wastewater Reuse in Agriculture. UV Disinfection: Parasite Removal and by-Product Formation. Desalination 2003, 152, 315–324. [Google Scholar] [CrossRef]
- Sobsey, M.D.; Fuji, T.; Shields, P.A. Inactivation of Hepatitis A Virus and Model Viruses in Water by Free Chlorine and Monochloramine. Water Sci. Technol. 1988, 20, 385–391. [Google Scholar] [CrossRef]
- Tree, J.A.; Adams, M.R.; Lees, D.N. Chlorination of Indicator Bacteria and Viruses in Primary Sewage Effluent. Appl. Environ. Microbiol. 2003, 69, 2038–2043. [Google Scholar] [CrossRef]
- Möritz, M.; Peters, H.; Nipko, B.; Rüden, H. Capability of Air Filters to Retain Airborne Bacteria and Molds in Heating, Ventilating and Air-Conditioning (HVAC) Systems. Int. J. Hyg. Environ. Health 2001, 203, 401–409. [Google Scholar] [CrossRef]
- Ferraris, M.; Balagna, C.; Perero, S. Method for the Application of an Antiviral Coating to a Substrate and Relative Coating. WO2019/082001, 2 May 2019. [Google Scholar]
- Balagna, C.; Irfan, M.; Perero, S.; Miola, M.; Maina, G.; Crosera, M.; Santella, D.; Simone, A.; Ferraris, M. Antibacterial Nanostructured Composite Coating on High Performance VectranTM Fabric for Aerospace Structures. Surf. Coat. Technol. 2019, 373, 47–55. [Google Scholar] [CrossRef]
- Irfan, M.; Perero, S.; Miola, M.; Maina, G.; Ferri, A.; Ferraris, M.; Balagna, C. Antimicrobial Functionalization of Cotton Fabric with Silver Nanoclusters/Silica Composite Coating via RF Co-Sputtering Technique. Cellulose 2017, 24, 2331–2345. [Google Scholar] [CrossRef]
- Balagna, C.; Perero, S.; Bosco, F.; Mollea, C.; Irfan, M.; Ferraris, M. Antipathogen Nanostructured Coating for Air Filters. Appl. Surf. Sci. 2020, 508, 145283. [Google Scholar] [CrossRef]
- Joe, Y.H.; Woo, K.; Hwang, J. Fabrication of an Anti-Viral Air Filter with SiO2–Ag Nanoparticles and Performance Evaluation in a Continuous Airflow Condition. J. Hazard. Mater. 2014, 280, 356–363. [Google Scholar] [CrossRef]
- Carbone, M.; Donia, D.T.; Sabbatella, G.; Antiochia, R. Silver Nanoparticles in Polymeric Matrices for Fresh Food Packaging. J. King Saud Univ. Sci. 2016, 28, 273–279. [Google Scholar] [CrossRef]
- World Health Organization. WHO Estimates of the Global Burden of Foodborne Diseases: Foodborne Disease Burden Epidemiology Reference Group 2007–2015; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Wei, L.; Lu, J.; Xu, H.; Patel, A.; Chen, Z.-S.; Chen, G. Silver Nanoparticles: Synthesis, Properties, and Therapeutic Applications. Drug Discov. Today 2015, 20, 595–601. [Google Scholar] [CrossRef] [PubMed]
- Pratsinis, A.; Hervella, P.; Leroux, J.-C.; Pratsinis, S.E.; Sotiriou, G.A. Toxicity of Silver Nanoparticles in Macrophages. Small 2013, 9, 2576–2584. [Google Scholar] [CrossRef] [PubMed]
- Soares, T.; Ribeiro, D.; Proença, C.; Chisté, R.C.; Fernandes, E.; Freitas, M. Size-Dependent Cytotoxicity of Silver Nanoparticles in Human Neutrophils Assessed by Multiple Analytical Approaches. Life Sci. 2016, 145, 247–254. [Google Scholar] [CrossRef]
- Zhang, Y.; Fan, W.; Sun, Y.; Chen, W.; Zhang, Y. Application of Antiviral Materials in Textiles: A Review. Nanotechnol. Rev. 2021, 10, 1092–1115. [Google Scholar] [CrossRef]
- VIROFORMULATM: Wear a Better Future Now. Thomas Mason. Available online: https://www.thomasmason.co.uk/en/news/viroformula-wear-a-better-future-now/ (accessed on 16 February 2022).
- HeiQ Viroblock. HeiQ Materials AG. Available online: https://www.heiq.com/products/functional-textile-technologies/heiq-viroblock/ (accessed on 16 February 2022).
- Zhang, T.; Wang, L.; Chen, Q.; Chen, C. Cytotoxic Potential of Silver Nanoparticles. Yonsei Med. J. 2014, 55, 283–291. [Google Scholar] [CrossRef]
- Hadrup, N.; Sharma, A.K.; Loeschner, K.; Jacobsen, N.R. Pulmonary Toxicity of Silver Vapours, Nanoparticles and Fine Dusts: A Review. Regul. Toxicol. Pharmacol. 2020, 115, 104690. [Google Scholar] [CrossRef]
- Mathur, P.; Jha, S.; Ramteke, S.; Jain, N.K. Pharmaceutical Aspects of Silver Nanoparticles. Artif. Cells Nanomed. Biotechnol. 2018, 46, 115–126. [Google Scholar] [CrossRef]
- Hyun, J.-S.; Lee, B.S.; Ryu, H.Y.; Sung, J.H.; Chung, K.H.; Yu, I.J. Effects of Repeated Silver Nanoparticles Exposure on the Histological Structure and Mucins of Nasal Respiratory Mucosa in Rats. Toxicol. Lett. 2008, 182, 24–28. [Google Scholar] [CrossRef]
- Rahman, M.F.; Wang, J.; Patterson, T.A.; Saini, U.T.; Robinson, B.L.; Newport, G.D.; Murdock, R.C.; Schlager, J.J.; Hussain, S.M.; Ali, S.F. Expression of Genes Related to Oxidative Stress in the Mouse Brain after Exposure to Silver-25 Nanoparticles. Toxicol. Lett. 2009, 187, 15–21. [Google Scholar] [CrossRef]
- Luther, E.M.; Koehler, Y.; Diendorf, J.; Epple, M.; Dringen, R. Accumulation of Silver Nanoparticles by Cultured Primary Brain Astrocytes. Nanotechnology 2011, 22, 375101. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Wu, Y.; Wang, C.; Li, H.C.; Wang, T.; Liao, C.Y.; Cui, L.; Zhou, Q.F.; Yan, B.; Jiang, G.B. Impact of Silver Nanoparticles on Human Cells: Effect of Particle Size. Nanotoxicology 2010, 4, 319–330. [Google Scholar] [CrossRef] [PubMed]
- Stoehr, L.C.; Gonzalez, E.; Stampfl, A.; Casals, E.; Duschl, A.; Puntes, V.; Oostingh, G.J. Shape Matters: Effects of Silver Nanospheres and Wires on Human Alveolar Epithelial Cells. Part. Fibre Toxicol. 2011, 8, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Ahamed, M.; Karns, M.; Goodson, M.; Rowe, J.; Hussain, S.M.; Schlager, J.J.; Hong, Y. DNA Damage Response to Different Surface Chemistry of Silver Nanoparticles in Mammalian Cells. Toxicol. Appl. Pharmacol. 2008, 233, 404–410. [Google Scholar] [CrossRef] [PubMed]

| Virus (and Family) | In Vitro/In Vivo Study | AgNPs Synthesis/Methods | Mechanism of Action | Main Features of and Factors Influencing the Antiviral Activity | Ref. |
|---|---|---|---|---|---|
| Influenza virus A (IFVA) (Orthomyxoviridae family) | In vitro | AgNPs dispersed into a chitosan matrix | Probable alteration or inactivation of the viral particle | Shape: spherical | [21] |
| Size: 3.5, 6.5, and 12.9 nm. Stronger antiviral effect with smaller AgNPs | |||||
| Concentration: 73, 62 and 77 µg/mL. ↑C.→↑A.e. | |||||
| Modification/functionalization: chitosan matrix without any antiviral effect, but used only for avoiding NP diffusion into the environment | |||||
| Exposure time: / | |||||
| In vitro | New disinfectant formulation combining surfactants and AgNPs | / | Shape: spherical | [35] | |
| Size: 13.2 ± 4 nm | |||||
| Concentration: / | |||||
| Modification/functionalization: / | |||||
| Exposure time: / | |||||
| In vitro | AgNPs from Panax ginseng root extract | / | Shape: quasi-spherical | [18] | |
| Size: range 5–15 nm | |||||
| Concentration: 0.005, 0.01, 0.015, 0.02, 0.025 M. ↑C.→↑A.e. | |||||
| Modification/functionalization: / | |||||
| Exposure time: / | |||||
| In vitro | AgNP–decorated silica hybrid composite | Damaging of the viral protein HA and NA | Shape: / | [17] | |
| Size: 30 nm | |||||
| Concentration: 1 × 108, 1 × 109, 5 × 109, 1 × 1010 particles/mL. ↑C.→↑A.e. | |||||
| Modification/functionalization: / | |||||
| Exposure time: 1, 2 3, 6 and 24 h. ↑E.t.→↑A.e | |||||
| In vitro | Oseltamivir-modified AgNPs (Ag@OTV) | Induction of morphologic abnormalities in the viral particle. Inhibition of HA and NA activity. Ag@OTV inhibited the accumulation of ROS by the H1N1 virus | Shape: / | [16] | |
| Size: 2–3 nm | |||||
| Concentration: / | |||||
| Modification/functionalization: Oseltamivir modification. Improvement of antiviral effect and reduction of toxicity towards cells | |||||
| Exposure time: / | |||||
| In vitro and in vivo | AgNPs via oxidation-reduction reaction | Destruction of morphologic viral structure | Shape: spherical | [20] | |
| Size: 9.5 ± 0.8 nm | |||||
| Concentration: 12, 5, 25, 50 µg/mL. ↑C.→↑A.e. | |||||
| Modification/functionalization: / | |||||
| Exposure time: 30, 60 and 120 min. Alteration of viral morphological structure with higher exposure time | |||||
| In vitro | AgNPs (unspecified synthesis) | / | Shape: / | [19] | |
| Size: range 5–20 nm | |||||
| Concentration: 6, 25, 12, 5, 25, 50, 100, 200 µg/mL. Better antiviral effect with AgNP concentration of 50 µg/mL | |||||
| Modification/functionalization: / | |||||
| Exposure time: 72 and 96 h. ↑E.t.→↑A.e. | |||||
| Transmissible gastroenteritis virus (TGEV) (Coronaviridae family) | In vitro | AgNPs, Ag nanowires, Ag colloids (unspecified synthesis) | / | Shape: Nanowires, spherical nanoparticles and colloids | [30] |
| Size: NPs less than 20 nm, nanowire diameter of 60 nm and 400 nm, colloids about 10 nm | |||||
| Concentration: 3.125, 6.25 and 12.5 µg/mL. ↑C.→↑A.e. | |||||
| Modification/functionalization: Polyvinylpyrrolidone (PVP) as capping agent. Higher antiviral effect with nanowires and nanoparticles; the presence of PVP coating in Ag colloids decreases their antiviral activity | |||||
| Exposure time: / | |||||
| Severe acute respiratory syndrome coronavirus virus 2 (SARS-CoV-2) (Coronaviridae family) | In vitro | AgNPs (commercial) | Inhibition of extracellular viral particles | Shape: / | [36] |
| Size: 2, 15, 50, 80, 100 nm. Stronger antiviral effect with 2 and 15 nm dimension | |||||
| Concentration: 0, 1, 0.5, 1, 2, 5 and 10 ppm. Higher concentration could become cytotoxic | |||||
| Modification/functionalization: / | |||||
| Exposure time: / | |||||
| In vitro and in a prospectiverandomized study of 231 participants | AgNPs (ArgovitTM) | / | Shape: spherical | [37] | |
| Size: 35 ± 15 nm | |||||
| Concentration: / | |||||
| Modification/functionalization: / | |||||
| Exposure time: 24, 48 and 72 h | |||||
| Bovine coronavirus (BCoV) (Coronaviridae family) | In vitro | poly(methyl methacrylate) (PMMA) nanofibers decorated with ZnO nanorods and AgNPs (PMMA/ZnO−Ag NFs) | / | Shape: / | [38] |
| Size: 510 ± 122 nm | |||||
| Concentration: / | |||||
| Modification/functionalization: System of poly(methylmethacrylate) (PMMA) nanofibers with ZnO nanorods and AgNPs | |||||
| Exposure time: 1 h and 24 h. ↑E.t.→↑A.e. | |||||
| Middle East respiratory syndrome coronavirus (MERS-CoV) and severe acute respiratory syndrome coronavirus (SARS-CoV) (Coronaviridae family) | In vitro | AgNPs prepared with different methods | / | Shape: spherical | [39] |
| Size: 7.1 ± 2.4 nm | |||||
| Concentration: 3.13–100 ppm. Stronger antiviral activity at a concentration of AgNPs 3.13 ppm. Higher concentrations are toxic | |||||
| Modification/functionalization: / | |||||
| Exposure time: 24, 48 and 72 h. ↑E.t.→↑A.e. | |||||
| Feline coronavirus (FCoV) (Coronaviridae family) | In vitro | AgNP-anchored Graphene Oxide (GO-Ag) | / | Shape: spherical | [40] |
| Size: 5–25 nm | |||||
| Concentration: 0.1, 1, 10, 100 mg/mL. Higher antiviral activity with higher AgNP concentration | |||||
| Modification/functionalization: AgNPs attached on graphene oxide. GO acts as stabilizing and supporting agent | |||||
| Exposure time: / | |||||
| Porcine deltacoronavirus (PDCoV) (Coronaviridae family) | In vitro | PP nonwoven substrate with a layer of PA6 electrospun nanofiber, impregnated with AgNPs | / | Shape: / | [41] |
| Size: / | |||||
| Concentration: / | |||||
| Modification/functionalization: PA6 nanofiber impregnated with AgNPs | |||||
| Exposure time: 15, 30 and 60 min. ↑E.t.→↑A.e. | |||||
| Poliovirus (Picornaviridae family) | In vitro | AgNPs synthesized via electrochemical method | / | Shape: / | [42] |
| Size: 7.1 ± 2.4 nm | |||||
| Concentration: 3.13–100 ppm. Stronger antiviral activity at AgNP concentration of 3.13 ppm. Higher concentrations are toxic | |||||
| Modification/functionalization: / | |||||
| Exposure time: 24, 48 and 72 h. ↑E.t.→↑A.e. | |||||
| Hepatitis A virus (HAV) and Coxakievirus B4 (CoxB4) (Picornaviridae family) | In vitro | AgNP synthesis using Lampranthus coccineus and Malephora lutea aqueous and hexane extracts | / | Shape: spherical | [23] |
| Size: range between 10.12–27.89 nm for L. coccineus and 8.91–14.48 nm for M. Iutea | |||||
| Concentration: / | |||||
| Modification/functionalization: / | |||||
| Exposure time: / | |||||
| Human immunodeficiency virus (HIV) (Retroviridaefamily) | In vitro | AgNPs into foamy carbon (1–10 nm) AgNPs coated by poly (N-vinyl-2-pyrrolidone) (PVP) AgNPs modified by bovine serum albumin (BSA) | The physical interaction of AgNPs with the viral particle probably inhibits virus binding to the host cell | Shape: / | [14] |
| Size: 16.19 ± 8.68 nm, 6.53 ± 2.41 nm, 3.12 ± 2.00 nm, depending on the preparation method | |||||
| Concentration: / | |||||
| Modification/functionalization: AgNP-coated foamy carbon, PVP-coated AgNPs, BSA- functionalized AgNPs. Reduction of antiviral effect for the presence of PVP and BSA | |||||
| Exposure time: / | |||||
| In vitro | AgNPs synthesized with sericin | / | Shape: / | [43] | |
| Size: 3.78 ± 1.14 nm (at optimized sericin concentration) | |||||
| Concentration: / | |||||
| Modification/functionalization: / | |||||
| Exposure time: / | |||||
| Herpes simplex virus type 1 or 2 (HSV-1, HSV-2) (Herpesviridae family) | In vitro | AgNPs capped with mercaptoethane sulfonate group (Ag–MES) | Suggested inhibition of virus binding to cell | Shape: / | [26] |
| Size: 4 ± 1 nm | |||||
| Concentration: 200, 400 and 800 µg/mL. ↑C.→↑A.e. (infection is blocked at a concentration of 400 µg/mL) | |||||
| Modification/functionalization: mercaptoethane (MES) sulfonate group. MES, which decorated AgNPs, acts as a multivalent inhibitor since it mimics HS group on the membrane of host cell, inhibiting the virus | |||||
| Exposure time: / | |||||
| In vitro and in vivo | Tannic Acid (TA)- Modified AgNPs | TA-AgNPs bind the virus, blocking cell infection; TA-AgNPs elicited B cells’ activation and plasma cells’ homing | Shape: / | [44] | |
| Size: 33 nm | |||||
| Concentration: / | |||||
| Modification/functionalization: Tannic acid as additional adjuvant for enhancing antiviral properties | |||||
| Exposure time: / | |||||
| In vitro and in vivo | Tannic acid-modified AgNPs block virus attachment and entry by direct interaction | Shape: / | [24] | ||
| Size: 13 ± 5 nm, 33 ± 7 nm, 46 ± 9 nm and 10 ± 5 nm. Higher antiviral activity with 33 nm nanoparticles | |||||
| Concentration: 0.5, 1, 2.5 µg/mL. The effect of the concentration depends on AgNPs’ size | |||||
| Modification/functionalization: Tannic acid as additional adjuvant for enhancing antiviral properties | |||||
| Exposure time: 60 min | |||||
| In vitro | AgNP synthesis using Lampranthus coccineus and Malephora lutea aqueous and hexane extracts | Probable binding of AgNPs to viral envelope glycoproteins, preventing viral penetration into the host cell | Shape: spherical | [23] | |
| Size: range between 10.12–27.89 nm for L. coccineus and 8.91–14.48 nm for M. Iutea | |||||
| Concentration: / | |||||
| Modification/functionalization: / | |||||
| Exposure time: / | |||||
| In vitro and in vivo | Tannic Acid–AgNPs into Carbopol 974P gel | Inhibition of viral attachment, penetration and cell-to-cell transmission; Direct interaction of NPs with viral envelope or its proteins | Shape: / | [25] | |
| Size: 33 ±13 nm | |||||
| Concentration: 25 or 50 ppm | |||||
| Modification/functionalization: Tannic acid as additional adjuvant for enhancing antiviral properties. Presence of Carbopol 974P hydrogels | |||||
| Exposure time: 24 h | |||||
| In vitro | AgNPs synthesized from different types of fungi | / | Shape: spherical | [22] | |
| Size: range between 4 and 31 nm. Smaller size, higher inhibition of virus infectivity | |||||
| Concentration: 0.1, 0.5, 1, 5 and 10 µg/mL. ↑C.→↑A.e., depending on fungal species | |||||
| Modification/functionalization: / | |||||
| Exposure time: / | |||||
| Respiratory syncytial virus (RSV) (Paramyxoviridae family) | In vitro and in vivo | PVP-coated AgNPs (commercial) | AgNP-treated and RSV-infected mice showed reductions in pro-inflammatory cytokines and chemokines | Shape: spherical | [45] |
| Size: range 8–12 nm | |||||
| Concentration: 0, 10, 25, 50 µg/mL. ↑C.→↑A.e. | |||||
| Modification/functionalization: PVP coating | |||||
| Exposure time: / | |||||
| In vitro | Curcumin-modified silver nanoparticles (cAgNPs) | Direct virus inactivation | Shape: / | [46] | |
| Size: 11.95 ± 0.23 nm | |||||
| Concentration: 0.008, 0.015, 0.03, 0.06, 0.12, 0.24 nM. Higher virus titer reduction with concentration between 0.008 and 0.06 nM. | |||||
| Modification/functionalization: AgNPs modified by curcumin | |||||
| Exposure time: 1 h | |||||
| Peste des petits ruminants virus (PPRV) (Paramyxoviridae family) | In vitro | AgNP synthesis from silver nitrate using extract of the Argemone maxicana leaf as reducing agent | Inhibition of virus entry | Shape: / | [47] |
| Size: 20 nm | |||||
| Concentration: range 1.23–900 µg/mL. ↑C.→↑A.e. | |||||
| Modification/functionalization: / | |||||
| Exposure time: 90 min | |||||
| Parainfluenza virus (HPVI) (Paramyxoviridae family) | In vitro | AgNP synthesis from different types of fungi | / | Shape: spherical | [22] |
| Size: range between 4 and 31 nm. Smaller size, higher inhibition of virus infectivity | |||||
| Concentration: 0.1, 0.5, 1, 5 and 10 µg/mL. ↑C.→↑A.e., depending on fungal species | |||||
| Modification/functionalization: / | |||||
| Exposure time: / | |||||
| Bovine parainfluenza virus 3 (BPIV3) (Paramyxoviridae family) | In vitro | Poly(methyl methacrylate) (PMMA) nanofibers decorated with ZnO nanorods and Ag nanoparticles (PMMA/ZnO−Ag NFs) | / | Shape: / | [38] |
| Size: 510 ± 122 nm | |||||
| Concentration: / | |||||
| Modification/functionalization: System of poly(methylmethacrylate) (PMMA) nanofibers with ZnO nanorods and AgNPs | |||||
| Exposure time: 1 h and 24 h. Higher antiviral activity with higher exposure time | |||||
| Chikungunya virus (CHIKV) (Togaviridae family) | In vitro | AgNP synthesis via plants with bioactive phytoconstituents linked to them | / | Shape: spherical | [48] |
| Size: range 50–120 nm depending on the plant | |||||
| Concentration: / | |||||
| Modification/functionalization: / | |||||
| Exposure time: / | |||||
| In vitro | AgNP synthesis using P. guajava leaves extract | / | Shape: / | [49] | |
| Size: 75–99 nm | |||||
| Concentration: / | |||||
| Surface functionalization: / | |||||
| Exposure time: / | |||||
| Hepatitis C virus (HCV) (Flaviviridae family) | In vitro | AgNPs from total extract and petroleum ether fraction of Amphimedon | Anti–HCV NS3 helicase and protease activity | Shape: spherical | [50] |
| Size: 8.22–14.30 nm and 8.22–9.97 nm | |||||
| Concentration: / | |||||
| Modification/functionalization: / | |||||
| Exposure time: / | |||||
| Dengue virus (DENV) (Flaviviridae family) | In vitro | AgNP synthesis using Centroceras clavulatum aqueous extract | / | Shape: spheric and cubic | [51] |
| Size: 35–65 nm | |||||
| Concentration: 6.25, 12.5, 25 and 50 µg/mL. ↑C.→↑A.e. | |||||
| Modification/functionalization: / | |||||
| Exposure time: 48 h | |||||
| In vitro | B. cylindrica-synthesized AgNPs | / | Shape: spherical | [52] | |
| Size: 30–70 nm | |||||
| Concentration: 10, 20 and 30 µg/mL. ↑C.→↑A.e. | |||||
| Modification/functionalization: / | |||||
| Exposure time: 24 h | |||||
| In vitro | M. oleifera-synthesized AgNPs | / | Shape: spherical | [53] | |
| Size: 100 nm | |||||
| Concentration: / | |||||
| Modification/functionalization: / | |||||
| Exposure time: / | |||||
| Resus rotavirus (RRV) (Reoviridae family) | In vitro | AgNP synthesis using NaBH4 into AgNO3 solution containing sodium citrate | In vivo upregulation of TGF-β | Shape: / | [54] |
| Size: 10 ± 5 nm | |||||
| Concentration: 0, 1, 5, 10 and 20 µg/mL. ↑C.→↑A.e. | |||||
| Modification/functionalization: / | |||||
| Exposure time: / | |||||
| T4 bacteriophage (Myoviridae family) | In vitro | Granular activated carbon (GAC) modified with silver and/or copper oxide nanoparticles | Suggested inactivation of the viral particle | Shape: / | [55] |
| Size: 25–40 nm | |||||
| Concentration: 0.5% and 1% w/w | |||||
| Modification/functionalization: Presence of GAC as second element | |||||
| Exposure time: / | |||||
| Rift Valley fever virus (RVFV) (Phenuiviridae family) | In vitro and in vivo | AgNPs functionalized with PVP (ArgovitTM) | / | Shape: spherical | [56] |
| Size: 35 ± 15 nm | |||||
| Concentration: 1.5–12 µg/mL. ↑C.→↑A.e. | |||||
| Modification/functionalization: poly(vinylpyrrolidone) (PVP) | |||||
| Exposure time: / | |||||
| Feline calicivirus (FCV) (Calicidiviridae family) | In vitro | AgNPs | Alteration of the viral capsid protein | Shape: spherical | [27] |
| Size: 10, 75, 110 nm. Stronger effect with smaller dimension | |||||
| Concentration: 25, 50, 100 µg/mL. ↑C.→↑A.e. | |||||
| Modification/functionalization: / | |||||
| Exposure time: 15 min, 30 min, 1 h, 2 h, 4 h | |||||
| Murine norovirus (MNV) and Feline Calicivirus (FCV) (Calicidiviridae family) | In vitro | Ag nitrate, AgNPs, poly (3- hydroxybutyrate-co-3 mol%-3-hydroxyvalerate) (PHBV3) coated with PHBV18/AgNP fiber | Virucidal activity of the AgNP film | Shape: / | [57] |
| Size: AgNPs 7 ± 3 nm; PHBV18/AgNP fibers 1.1 ± 0.40 µm | |||||
| Concentration: For AgNPs 0, 2.1, 10.5 and 21 mg/L. ↑C.→↑A.e. | |||||
| Modification/functionalization: PHBV18/AgNP fibers electrospun on PHBV3 | |||||
| Exposure time: 0, 30, 75 and 150 days: for Ag nitrate, ↑E.t.→↑A.e., until 75 days, with 150 days antiviral activity was reduced. For AgNPs, higher antiviral activity with higher exposure time. For PHBV3/PHBV18/Ag NPs: 24 h | |||||
| Vaccinia virus (VACV) (Poxvirus family) | In vitro | AgNPs (commercial) | Inhibition of viral entry through a macropinocytosis-dependent mechanism | Shape: / | [58] |
| Size: 25 nm ± 10 nm | |||||
| Concentration: 32 µg/mL | |||||
| Modification/functionalization: / | |||||
| Exposure time: 1 h | |||||
| Adenovirus (ADV) (Adenoviridae family) | In vitro | AgNPs by chemical redox method using tannic acid | Damaging of the viral structure | Shape: spherical | [59] |
| Size: 10, 75, 110 nm. Stronger effect with smaller dimension | |||||
| Concentration: 25, 50, 100 µg/mL. ↑C.→↑A.e. | |||||
| Modification/functionalization: / | |||||
| Exposure time: 48 and 96 h. | |||||
| Hepatitis B virus (HBV) (Hepadnaviridae family) | In vitro | AgNPs synthesized in HEPES buffer from silver nitrate | AgNPs binding to HBV double-stranded DNA or to the viral particle | Shape: / | [60] |
| Size: 10, 50, 800 nm. Good antiviral effect of AgNPs of 10 and 50 nm. AgNPs of 800 nm induce cytotoxic effect | |||||
| Concentration: 5–50 µM (for AgNPs of 10 and 50 nm). ↑C.→↑A.e. | |||||
| Modification/functionalization: / | |||||
| Exposure time: 0–96 h. ↑E.t.→↑A.e. | |||||
| Bunyamwera virus (BUNV) (Peribunyaviridae family) | In vitro | AgNPs (commercial) | Alteration of virus morphology and alteration of replication organelles (RO) | Shape: / | [61] |
| Size: 10 nm | |||||
| Concentration: 1.5, 2.4, 6, 12 and 24 µg/mL. ↑C.→↑A.e. | |||||
| Modification/functionalization: / | |||||
| Exposure time: 10 h | |||||
| Infectious bursal disease virus (IBDV) (Birnaviridae family) | In vitro | AgNP-anchored Graphene Oxide (GO-Ag) | / | Shape: spherical | [40] |
| Size: 5–25 nm | |||||
| Concentration: 0.1, 1, 10, 100 mg/mL. ↑C.→↑A.e. | |||||
| Modification/functionalization: AgNPs attached on graphene oxide. GO acts as stabilizing and supporting agent | |||||
| Exposure time: / | |||||
| In vitro | AgNPs | / | Shape: / | [62] | |
| Size: range 50–59 nm | |||||
| Concentration: 0, 10, 20, 50 ppm. Higher antiviral effect with a dosage of 20 ppm | |||||
| Modification/functionalization: / | |||||
| Exposure time: / |
| Virucidal Activity | Inhibition of the Early Steps of Replication (Binding Inhibition, Entry Inhibition) | Inhibition of the Late Steps of Replication (Viral Replication Inhibition or Viral Enzyme Inhibition) | |
|---|---|---|---|
| Virus | IFV-A, SARS-CoV-2, RSV, FCV, ADV, BUNV, MNV, T4 bacteriophage | HIV, HSV-1, HSV-2, PPRV, VACV | HCV, HBV |
| Field | Description of Application | System | Tested Virus | Study Level | Ref. |
|---|---|---|---|---|---|
| Health sector | Potential therapeutic use | AgNPs | IFVA (H3N2) | Laboratory study | [20] |
| Potential therapeutic use | Tannic acid-modified AgNPs (TA-AgNP) | HSV-2 | Laboratory study | [24] | |
| Potential therapeutic use | TA-AgNPs into Carbopol 974P gel | HSV-1 and HSV-2 | Laboratory study | [25] | |
| Potential therapeutic use | TA-AgNPs | HSV-2 | Laboratory study | [44] | |
| Potential therapeutic use | AgNPs | RSV | Laboratory study | [45] | |
| Potential therapeutic use | AgNPs functionalized with PVP (ArgovitTM) | RVFV | Prototype | [56] | |
| Prevention | AgNPs (ArgovitTM) | SARS-CoV-2 | Prototype | [37] | |
| Coating for surfaces | Protective hybrid coatings with AgNPs realized by means of sol gel | HIV-1, DENV, HSV-1, IFVA, CoxB3 | Prototype | [76] | |
| Coating for condoms for the prevention of sexually transmitted viruses | AgNP coating by immersion | HIV, HSV-1, HSV-2 | Prototype | [77] | |
| Surgical mask doped with AgNPs by immersion | AgNPs obtained by electrochemical method and incorporating an aqueous solution | IFVA (H5N1) | Prototype | [35] | |
| Co-sputtered disposable mask | Silver nanoclusters/silica composite coating by co-sputtering method | SARS-CoV-2 | Prototype | [78] | |
| Part of respiratory and surgical masks | Graphene–silver nanocomposite | FCoV, IBDV | Prototype | [40] | |
| Veterinary sector | Potential therapeutic use | AgNPs synthesized by chemical reduction method | IBDV | Laboratory study | [62] |
| Potential therapeutic use | Biologically synthesized AgNPs | PPRV | Laboratory study | [47] | |
| Potential therapeutic use | AgNPs | RVFV | Laboratory study | [56] | |
| Potential therapeutic use | AgNPs | CVD | Laboratory study | [79] | |
| Potential therapeutic use | AgNPs | WSSV | Laboratory study | [80,81] | |
| Potential therapeutic use | AgNPs from aqueous extracts of clove | NDV | Laboratory study | [82] | |
| Water and air filtration systems | Water treatment | AgNPs produced via Lactobacillus fermentum (Biogenic Ag0) | UZ1 (bacteriophage), MNV-1 | Prototype | [83] |
| Water treatment under UV radiation | AgNPs via photochemical reduction of silver nitrate on Aeroxide TiO2 P25 and Anatase TiO2 | MS2 (bacteriophage) | Laboratory study | [84] | |
| Water treatment | Fe2O3/Ag NPs coating on fiber glass | MS2 (bacteriophage) | Laboratory study | [85] | |
| Water treatment | AgNP-doped and Ag/Cu NP-doped activated carbon by impregnation | T4 (bacteriophage) | Laboratory study | [55] | |
| Water treatment | Magnetic hybrid colloid-AgNPs | MNV, ɸX174, AdV2 | Laboratory study | [86] | |
| Water treatment | Colloidal and immobilized Ag nanoparticles on a glass substrate | MS2 and T4 (bacteriophages) | Laboratory study | [87] | |
| Air filtration | PP nonwoven substrate with a layer of PA6 electrospun nanofiber, impregnated with AgNPs | PDCoV | Prototype | [41] | |
| Air filtration | Silver nanoclusters/silica composite coating on air filter | IFVA, RSV | Laboratory study | [63] | |
| Air filtration | Silver nanoparticle-coated silica particle | IFVA, MS2 (bacteriophage) | Laboratory study/Prototype | [17,63,88] | |
| Air filtration | Nano-Ag0/titania-chitosan | MS2 (bacteriophage) | Laboratory study | [89] | |
| Food packaging | Packaging | Polymeric film–AgNPs | FCV and Murine Norovirus (MNV) | Prototype | [57] |
| Textile industry | Antiviral clothing | AgNPs and phospholipid vesicles in the Viroblock/ViroFormulaTM | FluVA, SARS-Cov 2 | Commercial product | [90] |
| Antiviral clothing | Electrospun nanofibers with ZnO Nanorods and Ag NPs | BCV, Bovine Parainfluenza Virus Type 3 (BPIV3) | Laboratory study | [37] | |
| Disinfectant for polyester/viscose spunlace wipes for use in surface disinfection | AgNPs prepared by reducing agent or aqueous solution of PVA in the presence of glucose or photochemical reaction | MERS-CoV | Prototype | [39] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luceri, A.; Francese, R.; Lembo, D.; Ferraris, M.; Balagna, C. Silver Nanoparticles: Review of Antiviral Properties, Mechanism of Action and Applications. Microorganisms 2023, 11, 629. https://doi.org/10.3390/microorganisms11030629
Luceri A, Francese R, Lembo D, Ferraris M, Balagna C. Silver Nanoparticles: Review of Antiviral Properties, Mechanism of Action and Applications. Microorganisms. 2023; 11(3):629. https://doi.org/10.3390/microorganisms11030629
Chicago/Turabian StyleLuceri, Angelica, Rachele Francese, David Lembo, Monica Ferraris, and Cristina Balagna. 2023. "Silver Nanoparticles: Review of Antiviral Properties, Mechanism of Action and Applications" Microorganisms 11, no. 3: 629. https://doi.org/10.3390/microorganisms11030629
APA StyleLuceri, A., Francese, R., Lembo, D., Ferraris, M., & Balagna, C. (2023). Silver Nanoparticles: Review of Antiviral Properties, Mechanism of Action and Applications. Microorganisms, 11(3), 629. https://doi.org/10.3390/microorganisms11030629





