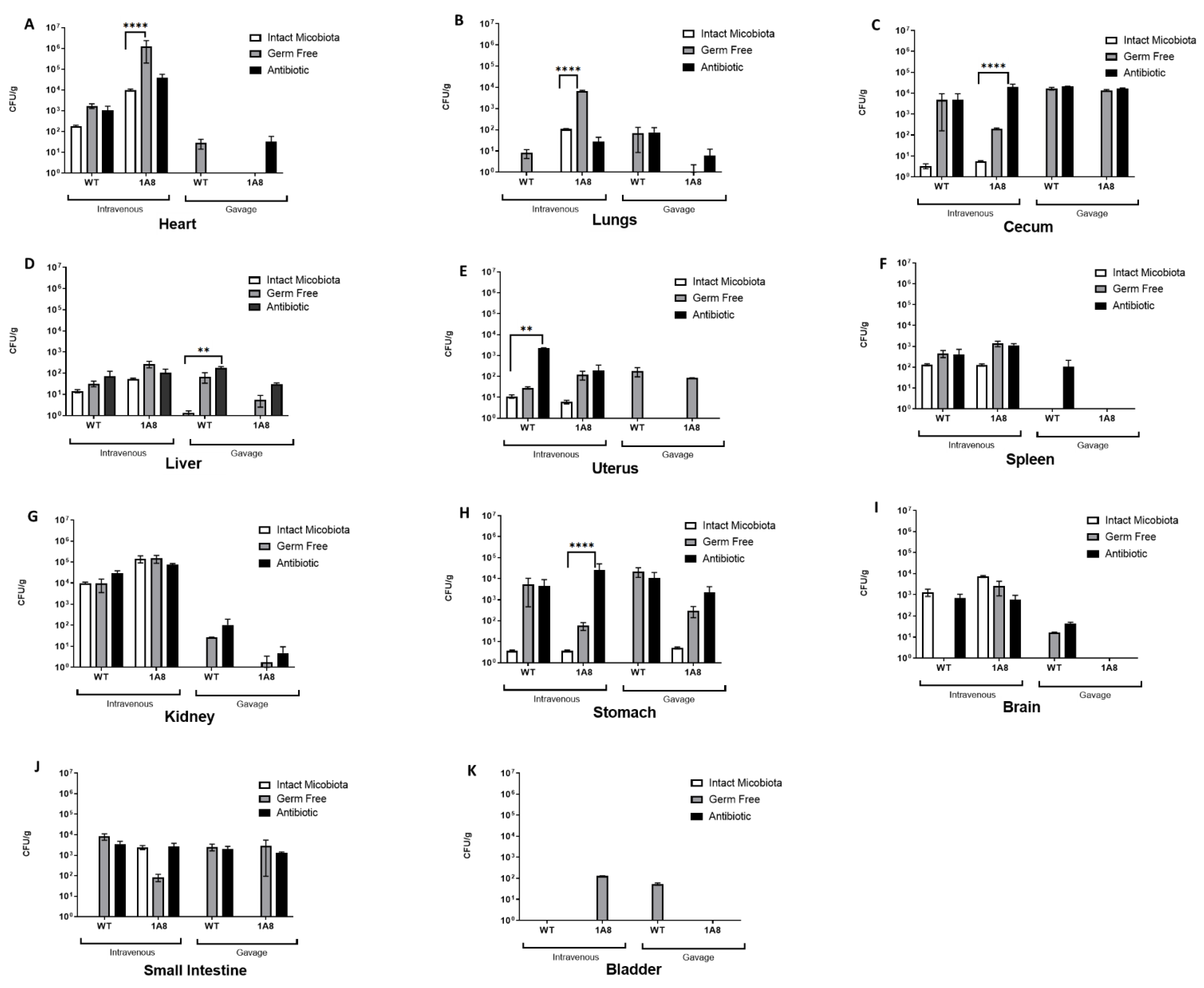
Depletion of the Microbiota Has a Modest but Important Impact on the Fungal Burden of the Heart and Lungs during Early Systemic Candida auris Infection in Neutropenic Mice
Abstract
:1. Introduction
2. Materials and Methods
2.1. Animal Use Ethics Statement
2.2. Animals and Microbiota Depletion
2.3. Neutrophil Depletion and Infection with C. auris
2.4. Fecal Pellet and Urine Collection
2.5. Tissue Collection for CFU Counts and Histology
2.6. Histopathology and Immunohistochemistry
2.7. Fecal DNA Purification, PCR, and 16S rDNA Sequencing
2.8. 16S rDNA Sequencing Analysis
2.9. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lockhart, S.R. Candida auris and multidrug resistance: Defining the new normal. Fungal Genet. Biol. 2019, 131, 103243. [Google Scholar] [CrossRef] [PubMed]
- Azar, M.M.; Turbett, S.E.; Fishman, J.A.; Pierce, V.M. Donor-Derived Transmission of Candida auris During Lung Transplantation. Clin. Infect. Dis. 2017, 65, 1040–1042. [Google Scholar] [CrossRef] [PubMed]
- Du, H.; Bing, J.; Hu, T.; Ennis, C.L.; Nobile, C.J.; Huang, G. Candida auris: Epidemiology, biology, antifungal resistance, and virulence. PLoS Pathog 2020, 16, e1008921. [Google Scholar] [CrossRef] [PubMed]
- Leach, L.; Zhu, Y.; Chaturvedi, S. Development and Validation of a Real-Time PCR Assay for Rapid Detection of Candida auris from Surveillance Samples. J. Clin. Microbiol. 2018, 56, e01223-17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bao, J.R.; Master, R.N.; Azad, K.N.; Schwab, D.A.; Clark, R.B.; Jones, R.S.; Moore, E.C.; Shier, K.L. Rapid, Accurate Identification of Candida auris by Using a Novel Matrix-Assisted Laser Desorption Ionization-Time of Flight Mass Spectrometry (MALDI-TOF MS) Database (Library). J. Clin. Microbiol. 2018, 56, e01700-17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Carolis, E.; Marchionni, F.; La Rosa, M.; Meis, J.F.; Chowdhary, A.; Posteraro, B.; Sanguinetti, M. Are We Ready for Nosocomial Candida auris Infections? Rapid Identification and Antifungal Resistance Detection Using MALDI-TOF Mass Spectrometry May Be the Answer. Front. Cell. Infect. Microbiol. 2021, 11, 645049. [Google Scholar] [CrossRef]
- Fasciana, T.; Cortegiani, A.; Ippolito, M.; Giarratano, A.; Di Quattro, O.; Lipari, D.; Graceffa, D.; Giammanco, A. Candida auris: An Overview of How to Screen, Detect, Test and Control This Emerging Pathogen. Antibiotics (Basel) 2020, 9, 778. [Google Scholar] [CrossRef]
- Pandya, N.; Cag, Y.; Pandak, N.; Pekok, A.U.; Poojary, A.; Ayoade, F.; Fasciana, T.; Giammanco, A.; Caskurlu, H.; Rajani, D.P.; et al. International Multicentre Study of Candida auris Infections. J. Fungi (Basel) 2021, 7, 878. [Google Scholar] [CrossRef]
- Casadevall, A.; Kontoyiannis, D.P.; Robert, V. Environmental Candida auris and the Global Warming Emergence Hypothesis. mBio 2021, 12, e00360-21. [Google Scholar] [CrossRef]
- Forsberg, K.; Woodworth, K.; Walters, M.; Berkow, E.L.; Jackson, B.; Chiller, T.; Vallabhaneni, S. Candida auris: The recent emergence of a multidrug-resistant fungal pathogen. Med. Mycol. 2019, 57, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Cortegiani, A.; Misseri, G.; Fasciana, T.; Giammanco, A.; Giarratano, A.; Chowdhary, A. Epidemiology, clinical characteristics, resistance, and treatment of infections by Candida auris. J. Intensive Care 2018, 6, 69. [Google Scholar] [CrossRef] [PubMed]
- Jackson, B.R.; Chow, N.; Forsberg, K.; Litvintseva, A.P.; Lockhart, S.R.; Welsh, R.; Vallabhaneni, S.; Chiller, T. On the Origins of a Species: What Might Explain the Rise of Candida auris? J. Fungi (Basel) 2019, 5, 58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lynch, S.V.; Pedersen, O. The Human Intestinal Microbiome in Health and Disease. N. Engl. J. Med. 2016, 375, 2369–2379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fan, Y.; Pedersen, O. Gut microbiota in human metabolic health and disease. Nat. Rev. Microbiol. 2021, 19, 55–71. [Google Scholar] [CrossRef]
- Iliev, I.D.; Funari, V.A.; Taylor, K.D.; Nguyen, Q.; Reyes, C.N.; Strom, S.P.; Brown, J.; Becker, C.A.; Fleshner, P.R.; Dubinsky, M.; et al. Interactions between commensal fungi and the C-type lectin receptor Dectin-1 influence colitis. Science 2012, 336, 1314–1317. [Google Scholar] [CrossRef] [Green Version]
- Moyes, D.L.; Naglik, J.R. The mycobiome: Influencing IBD severity. Cell Host Microbe 2012, 11, 551–552. [Google Scholar] [CrossRef] [Green Version]
- Proctor, D.M.; Dangana, T.; Sexton, D.J.; Fukuda, C.; Yelin, R.D.; Stanley, M.; Bell, P.B.; Baskaran, S.; Deming, C.; Chen, Q.; et al. Integrated genomic, epidemiologic investigation of Candida auris skin colonization in a skilled nursing facility. Nat. Med. 2021, 27, 1401–1409. [Google Scholar] [CrossRef]
- Torres, S.R.; Pichowicz, A.; Torres-Velez, F.; Song, R.; Singh, N.; Lasek-Nesselquist, E.; De Jesus, M. Impact of Candida auris Infection in a Neutropenic Murine Model. Antimicrob. Agents Chemother. 2020, 64, e01625-19. [Google Scholar] [CrossRef]
- Kilburn, S.; Innes, G.; Quinn, M.; Southwick, K.; Ostrowsky, B.; Greenko, J.A.; Lutterloh, E.; Greeley, R.; Magleby, R.; Chaturvedi, V.; et al. Antifungal Resistance Trends of Candida auris Clinical Isolates, New York-New Jersey, 2016–2020. Antimicrob. Agents Chemother. 2022, aac0224221. [Google Scholar] [CrossRef]
- Pathirana, R.U.; Friedman, J.; Norris, H.L.; Salvatori, O.; McCall, A.D.; Kay, J.; Edgerton, M. Fluconazole-Resistant Candida auris Is Susceptible to Salivary Histatin 5 Killing and to Intrinsic Host Defenses. Antimicrob. Agents Chemother. 2018, 62, e01872-17. [Google Scholar] [CrossRef] [Green Version]
- Al-Ghalith, G.A.; Montassier, E.; Ward, H.N.; Knights, D. NINJA-OPS: Fast Accurate Marker Gene Alignment Using Concatenated Ribosomes. PLoS Comput. Biol. 2016, 12, e1004658. [Google Scholar] [CrossRef] [PubMed]
- Langmead, B.; Salzberg, S.L. Fast gapped-read alignment with Bowtie 2. Nat. Methods 2012, 9, 357–359. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McDonald, D.; Price, M.N.; Goodrich, J.; Nawrocki, E.P.; DeSantis, T.Z.; Probst, A.; Andersen, G.L.; Knight, R.; Hugenholtz, P. An improved Greengenes taxonomy with explicit ranks for ecological and evolutionary analyses of bacteria and archaea. ISME J. 2012, 6, 610–618. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, R.H.; Larsson, K.H.; Taylor, A.F.S.; Bengtsson-Palme, J.; Jeppesen, T.S.; Schigel, D.; Kennedy, P.; Picard, K.; Glockner, F.O.; Tedersoo, L.; et al. The UNITE database for molecular identification of fungi: Handling dark taxa and parallel taxonomic classifications. Nucleic Acids Res. 2019, 47, D259–D264. [Google Scholar] [CrossRef] [PubMed]
- Caporaso, J.G.; Kuczynski, J.; Stombaugh, J.; Bittinger, K.; Bushman, F.D.; Costello, E.K.; Fierer, N.; Pena, A.G.; Goodrich, J.K.; Gordon, J.I.; et al. QIIME allows analysis of high-throughput community sequencing data. Nat. Methods 2010, 7, 335–336. [Google Scholar] [CrossRef] [Green Version]
- Love, M.I.; Huber, W.; Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014, 15, 550. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morales-Lopez, S.E.; Parra-Giraldo, C.M.; Ceballos-Garzon, A.; Martinez, H.P.; Rodriguez, G.J.; Alvarez-Moreno, C.A.; Rodriguez, J.Y. Invasive Infections with Multidrug-Resistant Yeast Candida auris, Colombia. Emerg. Infect. Dis. 2017, 23, 162–164. [Google Scholar] [CrossRef] [Green Version]
- Parra-Giraldo, C.M.; Valderrama, S.L.; Cortes-Fraile, G.; Garzon, J.R.; Ariza, B.E.; Morio, F.; Linares-Linares, M.Y.; Ceballos-Garzon, A.; de la Hoz, A.; Hernandez, C.; et al. First report of sporadic cases of Candida auris in Colombia. Int. J. Infect. Dis. 2018, 69, 63–67. [Google Scholar] [CrossRef] [Green Version]
- Emara, M.; Ahmad, S.; Khan, Z.; Joseph, L.; Al-Obaid, I.; Purohit, P.; Bafna, R. Candida auris candidemia in Kuwait, 2014. Emerg. Infect. Dis. 2015, 21, 1091–1092. [Google Scholar] [CrossRef] [Green Version]
- Ruiz-Gaitan, A.; Moret, A.M.; Tasias-Pitarch, M.; Aleixandre-Lopez, A.I.; Martinez-Morel, H.; Calabuig, E.; Salavert-Lleti, M.; Ramirez, P.; Lopez-Hontangas, J.L.; Hagen, F.; et al. An outbreak due to Candida auris with prolonged colonisation and candidaemia in a tertiary care European hospital. Mycoses 2018, 61, 498–505. [Google Scholar] [CrossRef] [Green Version]
- Adams, E.; Quinn, M.; Tsay, S.; Poirot, E.; Chaturvedi, S.; Southwick, K.; Greenko, J.; Fernandez, R.; Kallen, A.; Vallabhaneni, S.; et al. Candida auris in Healthcare Facilities, New York, USA, 2013–2017. Emerg. Infect. Dis. 2018, 24, 1816–1824. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Forgacs, L.; Borman, A.M.; Prepost, E.; Toth, Z.; Kardos, G.; Kovacs, R.; Szekely, A.; Nagy, F.; Kovacs, I.; Majoros, L. Comparison of in vivo pathogenicity of four Candida auris clades in a neutropenic bloodstream infection murine model. Emerg. Microbes Infect. 2020, 9, 1160–1169. [Google Scholar] [CrossRef] [PubMed]
- López-Vilella, R.; Ruiz Gaitán, A.C.; Gimeno Costa, J.R.; Vicente Guillén, R.; Pemán García, J.; Sánchez-Lázaro, I.; Almenar Bonet, L. Candida auris and Heart Transplantation. Preoperative Attitude. OBM Transplant. 2019, 3. [Google Scholar] [CrossRef] [Green Version]

| Sample | Liver | Kidney | Spleen | Heart | Uterus | Lung | Urinary Bl | Brain | Stomach | Small Intestine | Large Intestine | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HE | IHC | HE | IHC | HE | IHC | HE | IHC | HE | IHC | HE | IHC | HE | IHC | HE | IHC | HE | IHC | HE | IHC | HE | IHC | |
| Control | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | NA | NA | NA | NA |
| Control | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | NA | NA | NA | NA |
| Control | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| i.v. | ++ | ++ | + | + | - | ++ | ++ | ++ | - | - | - | - | NA | NA | + | + | - | + | NA | NA | NA | NA |
| i.v. | + | ++ | - | + | - | + | + | ++ | - | - | - | - | - | - | - | - | - | + | NA | NA | NA | NA |
| i.v. | + | ++ | + | + | - | + | + | + | - | - | - | - | - | - | - | + | - | + | - | + | - | + |
| i.v + 1A8 | + | +++ | +++ | +++ | - | ++ | ++++ | ++++ | - | + | - | ++ | + | + | + | + | + | + | NA | NA | NA | NA |
| i.v + 1A8 | + | +++ | +++ | +++ | - | ++ | ++++ | ++++ | - | - | - | + | - | - | - | + | + | + | NA | NA | NA | NA |
| i.v + 1A8 | + | +++ | +++ | +++ | - | ++ | ++++ | ++++ | - | § | - | + | - | - | - | + | - | + | ++ | + | - | + |
| Gavage | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | + | NA | NA | NA | NA |
| Gavage | - | - | - | - | - | - | - | - | - | - | - | + | - | - | - | - | - | + | NA | NA | NA | NA |
| Gavage | - | - | - | - | - | - | - | - | - | - | - | - | NA | NA | - | - | - | + | - | + | - | + |
| Gavage + 1A8 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | NA | NA | NA | NA |
| Gavage + 1A8 | EMH | - | - | - | - | - | - | - | - | - | - | ++ | - | - | - | - | - | - | NA | NA | NA | NA |
| Gavage + 1A8 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | + | - | + |
| Sample | Liver | Kidney | Heart | Brain | Stomach | Spleen | Lung | Uterus | Urinary Bladder | Small Intestine | Cecum/Large Intestine | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HE | IHC | HE | IHC | HE | IHC | HE | IHC | HE | IHC | HE | IHC | HE | IHC | HE | IHC | HE | IHC | HE | IHC | HE | IHC | |
| Control | - | - | - | - | - | - | - | - | - | - | - | - | - | - | NT | NT | NT | NT | NT | NT | NT | NT |
| Control | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | NT | NT | NT | NT | NT | NT |
| Control | - | - | - | - | NT | NT | - | - | - | - | NT | NT | - | - | NT | NT | NT | NT | - | - | - | - |
| i.v. | + | - | ++ | + | + | + | - | - | - | - | - | - | - | - | NT | NT | - | + | NT | NT | NT | NT |
| i.v. | - | - | ++ | + | + | + | - | - | - | - | - | + | Au | - | - | - | - | - | NT | NT | NT | NT |
| i.v. | - | - | NT | NT | + | ++ | - | - | - | - | - | - | Au | - | NT | NT | NT | NT | - | - | - | + |
| i.v + 1A8 | + | + | + | ++ | +++ | +++ | - | + | - | - | - | + | - | + | - | - | - | - | NT | NT | NT | NT |
| i.v + 1A8 | + | + | +++ | +++ | +++ | +++ | - | - | - | + | - | + | - | - | NT | NT | - | - | NT | NT | NT | NT |
| i.v + 1A8 | + | + | +++ | +++ | +++ | +++ | + | ++ | - | - | - | + | - | + | - | - | - | - | - | - | - | + |
| Gavage | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | NT | NT | NT | NT |
| Gavage | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | NT | NT | NT | NT |
| Gavage | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | + | - | + |
| Gavage + 1A8 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | NT | NT | NT | NT | NT | NT |
| Gavage + 1A8 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | NT | NT | NT | NT |
| Gavage + 1A8 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | + | - | + |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pichowicz, A.M.; Torres, S.R.; Torres-Velez, F.J.; Longyear, A.D.; Singh, N.; Lasek-Nesselquist, E.; De Jesus, M. Depletion of the Microbiota Has a Modest but Important Impact on the Fungal Burden of the Heart and Lungs during Early Systemic Candida auris Infection in Neutropenic Mice. Microorganisms 2022, 10, 330. https://doi.org/10.3390/microorganisms10020330
Pichowicz AM, Torres SR, Torres-Velez FJ, Longyear AD, Singh N, Lasek-Nesselquist E, De Jesus M. Depletion of the Microbiota Has a Modest but Important Impact on the Fungal Burden of the Heart and Lungs during Early Systemic Candida auris Infection in Neutropenic Mice. Microorganisms. 2022; 10(2):330. https://doi.org/10.3390/microorganisms10020330
Chicago/Turabian StylePichowicz, Amber M., Steven R. Torres, Fernando J. Torres-Velez, Adina D. Longyear, Navjot Singh, Erica Lasek-Nesselquist, and Magdia De Jesus. 2022. "Depletion of the Microbiota Has a Modest but Important Impact on the Fungal Burden of the Heart and Lungs during Early Systemic Candida auris Infection in Neutropenic Mice" Microorganisms 10, no. 2: 330. https://doi.org/10.3390/microorganisms10020330
APA StylePichowicz, A. M., Torres, S. R., Torres-Velez, F. J., Longyear, A. D., Singh, N., Lasek-Nesselquist, E., & De Jesus, M. (2022). Depletion of the Microbiota Has a Modest but Important Impact on the Fungal Burden of the Heart and Lungs during Early Systemic Candida auris Infection in Neutropenic Mice. Microorganisms, 10(2), 330. https://doi.org/10.3390/microorganisms10020330





