Acute Calculous Cholecystitis Caused by Streptococcus gallolyticus subspecies pasteurianus: A Case Report
Abstract
:1. Introduction
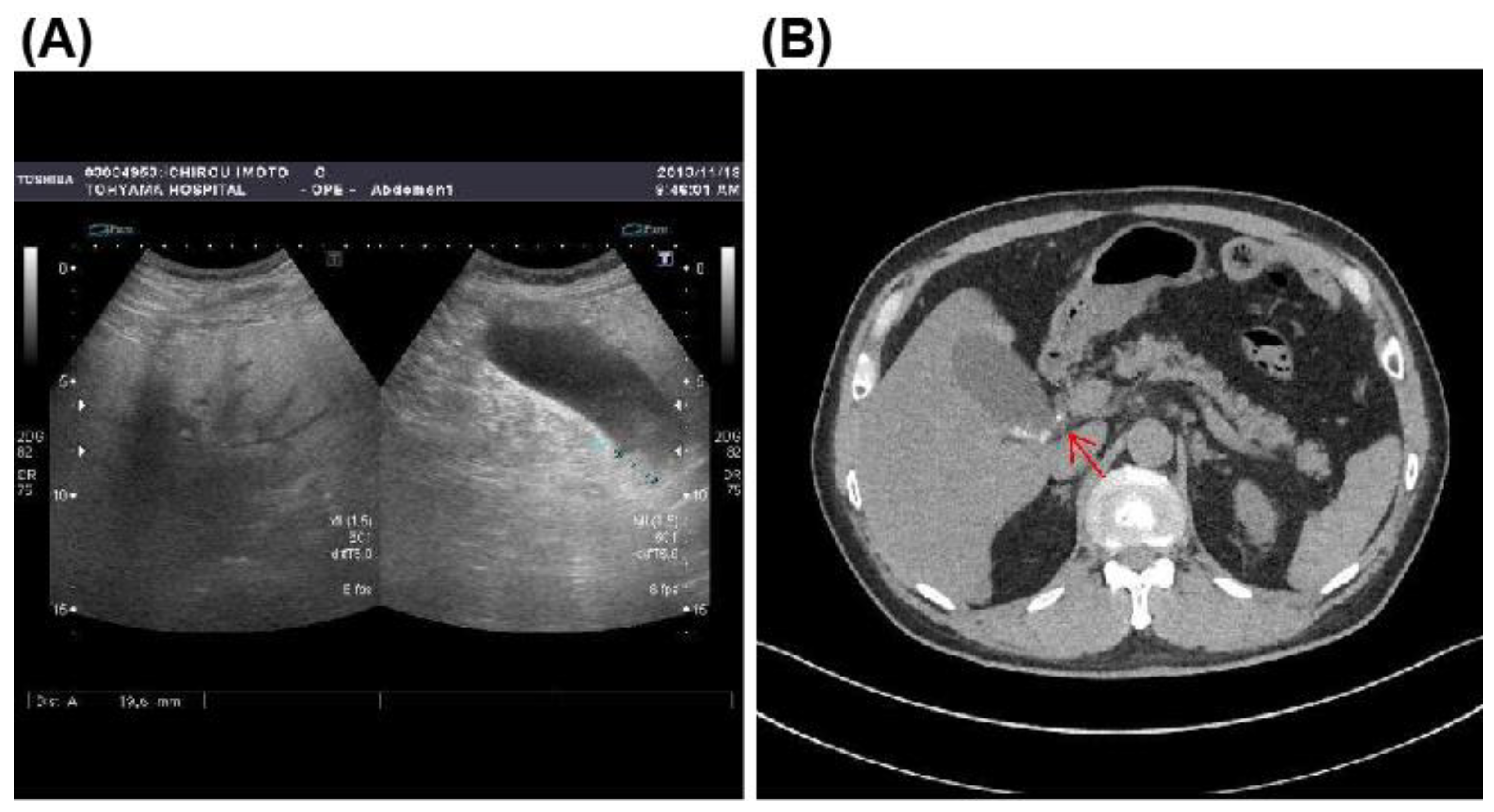
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Coykendall, A.L. Classification and identification of the viridans streptococci. Clin. Microbiol. Rev. 1989, 2, 315–328. [Google Scholar] [CrossRef] [PubMed]
- Schlegel, L.; Grimont, F.; Ageron, E.; Grimont, P.A.D.; Bouvet, A. Reappraisal of the taxonomy of the Streptococcus bovis/Streptococcus equinus complex and related species: Description of Streptococcus gallolyticus subsp. gallolyticus subsp. nov., S. gallolyticus subsp. macedonicus subsp. nov. and S. gallolyticus subsp. pasteurianus subsp. nov. Int. J. Syst. Evol. Microbiol. 2003, 53 Pt 3, 631–645. [Google Scholar] [CrossRef] [PubMed]
- Boleij, A.; van Gelder, M.M.; Swinkels, D.W.; Tjalsma, H. Clinical Importance of Streptococcus gallolyticus infection among colorectal cancer patients: Systematic review and meta-analysis. Clin. Infect. Dis. 2011, 53, 870–878. [Google Scholar] [CrossRef] [PubMed]
- Gavin, P.J.; Thomson, R.B., Jr.; Horng, S.J.; Yogev, R. Neonatal sepsis caused by Streptococcus bovis variant (biotype II/2): Report of a case and review. J. Clin. Microbiol. 2003, 41, 3433–3435. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Madani, R.; Mukhtar, H. Streptococcus bovis endocarditis, a silent sign for colonic tumour. Colorectal Dis. 2010, 12, 164–171. [Google Scholar] [CrossRef]
- Klatte, J.M.; Clarridge, J.E., 3rd; Bratcher, D.; Selvarangan, R. A longitudinal case series description of meningitis due to Streptococcus gallolyticus subsp. pasteurianus in infants. J. Clin. Microbiol. 2012, 50, 57–60. [Google Scholar] [CrossRef]
- Corredoira, J.; Alonso, M.P.; Garcia-Garrote, F.; Garcia-Pais, M.J.; Coira, A.; Rabunal, R.; Gonzalez-Ramirez, A.; Pita, J.; Matesanz, M.; Velasco, D.; et al. Streptococcus bovis group and biliary tract infections: An analysis of 51 cases. Clin. Microbiol. Infect. 2014, 20, 405–409. [Google Scholar] [CrossRef]
- Okamoto, K.; Suzuki, K.; Takada, T.; Strasberg, S.M.; Asbun, H.J.; Endo, I.; Iwashita, Y.; Hibi, T.; Pitt, H.A.; Umezawa, A.; et al. Tokyo Guidelines 2018: Flowchart for the management of acute cholecystitis. J. Hepatobiliary Pancreat. Sci. 2018, 25, 55–72. [Google Scholar] [CrossRef]
- Marziali, I.; Cicconi, S.; Marilungo, F.; Benedetti, M.; Ciano, P.; Pagano, P.; D’Emidio, F.; Guercioni, G.; Catarci, M. Role of percutaneous cholecystostomy in all-comers with acute cholecystitis according to current guidelines in a general surgical unit. Updates Surg. 2021, 73, 473–480. [Google Scholar] [CrossRef]
- Pompilio, A.; Di Bonaventura, G.; Gherardi, G. An Overview on Streptococcus bovis/Streptococcus equinus Complex Isolates: Identification to the Species/Subspecies Level and Antibiotic Resistance. Int. J. Mol. Sci. 2019, 20, 480. [Google Scholar] [CrossRef] [Green Version]
- Klein, R.S.; Recco, R.A.; Catalano, M.T.; Edberg, S.C.; Casey, J.I.; Steigbigel, N.H. Association of Streptococcus bovis with carcinoma of the colon. N. Engl. J. Med. 1977, 297, 800–802. [Google Scholar] [CrossRef] [PubMed]
- Corredoira, J.; Miguez, E.; Mateo, L.M.; Fernandez-Rodriguez, R.; Garcia-Rodriguez, J.F.; Perez-Gonzalez, A.; Sanjurjo, A.; Pulian, M.V.; Rabuñal, R.; GESBOGA. Correlation between Streptococcus bovis bacteremia and density of cows in Galicia, northwest of Spain. Infection 2019, 47, 399–407. [Google Scholar] [CrossRef] [PubMed]
- Jans, C.; Kaindi, D.W.; Bock, D.; Njage, P.M.; Kouame-Sina, S.M.; Bonfoh, B.; Lacroix, C.; Meile, L. Prevalence and comparison of Streptococcus infantarius subsp. infantarius and Streptococcus gallolyticus subsp. macedonicus in raw and fermented dairy products from East and West Africa. Int. J. Food Microbiol. 2013, 167, 186–195. [Google Scholar] [CrossRef] [PubMed]
- Facklam, R.R.; Moody, M.D. Presumptive identification of group D streptococci: The bile-esculin test. Appl. Microbiol. 1970, 20, 245–250. [Google Scholar] [CrossRef]
- Lee, R.A.; Woo, P.C.Y.; To, A.P.C.; Lau, S.K.P.; Wong, S.S.Y.; Yuen, K.Y. Geographical difference of disease association in Streptococcus bovis bacteraemia. J. Med. Microbiol. 2003, 52 Pt 10, 903–908. [Google Scholar] [CrossRef]
- Ruoff, K.L.; Miller, S.I.; Garner, C.V.; Ferraro, M.J.; Calderwood, S.B. Bacteremia with Streptococcus bovis and Streptococcus salivarius: Clinical correlates of more accurate identification of isolates. J. Clin. Microbiol. 1989, 27, 305–308. [Google Scholar] [CrossRef]
- Corredoira, J.C.; Alonso, M.P.; Garcia, J.F.; Casariego, E.; Coira, A.; Rodriguez, A.; Pita, J.; Louzao, C.; Pombo, B.; Lopez, M.J.; et al. Clinical characteristics and significance of Streptococcus salivarius bacteremia and Streptococcus bovis bacteremia: A prospective 16-year study. Eur. J. Clin. Microbiol. Infect. Dis. 2005, 24, 250–255. [Google Scholar] [CrossRef]
- Kimura, Y.; Takada, T.; Kawarada, Y.; Nimura, Y.; Hirata, K.; Sekimoto, M.; Yoshida, M.; Mayumi, T.; Wada, K.; Miura, F.; et al. Definitions, pathophysiology, and epidemiology of acute cholangitis and cholecystitis: Tokyo Guidelines. J. Hepatobiliary Pancreat. Surg. 2007, 14, 15–26. [Google Scholar] [CrossRef]
- Kaufman, H.S.; Magnuson, T.H.; Lillemoe, K.D.; Frasca, P.; Pitt, H.A. The role of bacteria in gallbladder and common duct stone formation. Ann. Surg. 1989, 209, 584–591; discussion 591–592. [Google Scholar] [CrossRef]
- Bae, W.K.; Moon, Y.S.; Kim, J.H.; Lee, S.H.; Kim, N.H.; Kim, K.A.; Lee, J.S.; Um, T.H.; Cho, C.R. Microbiologic study of the bile culture and antimicrobial susceptibility in patients with biliary tract infection. Korean J. Gastroenterol. 2008, 51, 248–254. [Google Scholar]
- Stewart, L.; Oesterle, A.L.; Erdan, I.; Griffiss, J.M.; Way, L.W. Pathogenesis of pigment gallstones in Western societies: The central role of bacteria. J. Gastrointest. Surg. 2002, 6, 891–903; discussion 903–904. [Google Scholar] [CrossRef]
- Vitek, L.; Carey, M.C. New pathophysiological concepts underlying pathogenesis of pigment gallstones. Clin. Res. Hepatol. Gastroenterol. 2012, 36, 122–129. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Peripheral Blood | Normal Range | Biochemistry | Normal Range | ||
|---|---|---|---|---|---|
| White blood cells | 9800/μL | 3900–9800 | Total protein | 7.7 g/dL | 6.5–8.5 |
| Neutrophils | 81.9% | 27.0–70.0 | Albumin | 4.7 g/dL | 4.1–5.3 |
| Eosinophils | 0.5% | 0.0–10.0 | Total bilirubin | 0.80 mg/dL | 0.2–1.3 |
| Basophils | 0.3% | 0.0–3.0 | AST | 37 IU/L | 10–35 |
| Lymphocytes | 15.0% | 19.0–59.0 | ALT | 54 IU/L | 10–35 |
| Monocytes | 1.8% | 0.0–12.0 | Lactate dehydrogenase | 174 IU/L | 110–225 |
| Red blood cells | 488 × 104/μL | 427–570 | Alkaline phosphatase | 222 IU/L | 110–340 |
| Hemoglobin | 15.6 g/dL | 13.5–17.6 | γ-GTP | 30 IU/L | 8–60 |
| Hematocrit | 44.5% | 39.8–51.8 | Cholinesterase | 424 IU/L | 214–466 |
| MCV | 91.3 fl | 82.7–101.6 | Amylase | 153 IU/L | 38–137 |
| MCH | 31.9 pg | 28.0–34.6 | Total cholesterol | 233 mg/dL | 150–219 |
| MCHC | 35.0% | 31.6–36.6 | HDL-C | 69 mg/dL | 40–96 |
| Platelets | 19.5 × 104/μL | 13.1–36.2 | LDL-C | 143 mg/dL | 70–139 |
| Coagulation> | Triglycerides | 177 mg/dL | 50–150 | ||
| APTT | 24.3 s | 27.0–38.5 | CRP | 0.139 mg/dL | 0.000–0.299 |
| PT | 107% | 70–140 | Blood urea nitrogen | 9.8 mg/dL | 9.0–22.0 |
| PT-INR | 0.95 | 0.85–1.15 | Creatinine | 0.64 mg/L | 0.50–1.10 |
| FDP | 3.2 μg/mL | 0–5.0 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shigemori, T.; Hiasa, A.; Inoue, Y.; Oka, S.; Yasuma, T.; Nishiwaki, R.; Sugimasa, N.; Hamaguchi, T.; Noji, M.; Takeuchi, K.; et al. Acute Calculous Cholecystitis Caused by Streptococcus gallolyticus subspecies pasteurianus: A Case Report. Microorganisms 2022, 10, 1929. https://doi.org/10.3390/microorganisms10101929
Shigemori T, Hiasa A, Inoue Y, Oka S, Yasuma T, Nishiwaki R, Sugimasa N, Hamaguchi T, Noji M, Takeuchi K, et al. Acute Calculous Cholecystitis Caused by Streptococcus gallolyticus subspecies pasteurianus: A Case Report. Microorganisms. 2022; 10(10):1929. https://doi.org/10.3390/microorganisms10101929
Chicago/Turabian StyleShigemori, Tsunehiko, Atsunori Hiasa, Yasuhiro Inoue, Satoko Oka, Taro Yasuma, Ryo Nishiwaki, Natsuko Sugimasa, Tetsuya Hamaguchi, Midori Noji, Kenji Takeuchi, and et al. 2022. "Acute Calculous Cholecystitis Caused by Streptococcus gallolyticus subspecies pasteurianus: A Case Report" Microorganisms 10, no. 10: 1929. https://doi.org/10.3390/microorganisms10101929
APA StyleShigemori, T., Hiasa, A., Inoue, Y., Oka, S., Yasuma, T., Nishiwaki, R., Sugimasa, N., Hamaguchi, T., Noji, M., Takeuchi, K., Ito, Y., Katoh, T., Gabazza, E. C., & Imoto, I. (2022). Acute Calculous Cholecystitis Caused by Streptococcus gallolyticus subspecies pasteurianus: A Case Report. Microorganisms, 10(10), 1929. https://doi.org/10.3390/microorganisms10101929







