Viral Filtration Efficiency of Fabric Masks Compared with Surgical and N95 Masks
Abstract
1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Face Masks
4.2. Conditioning of Face Masks Prior to Testing
4.3. Bacteriophage MS2 Preparation
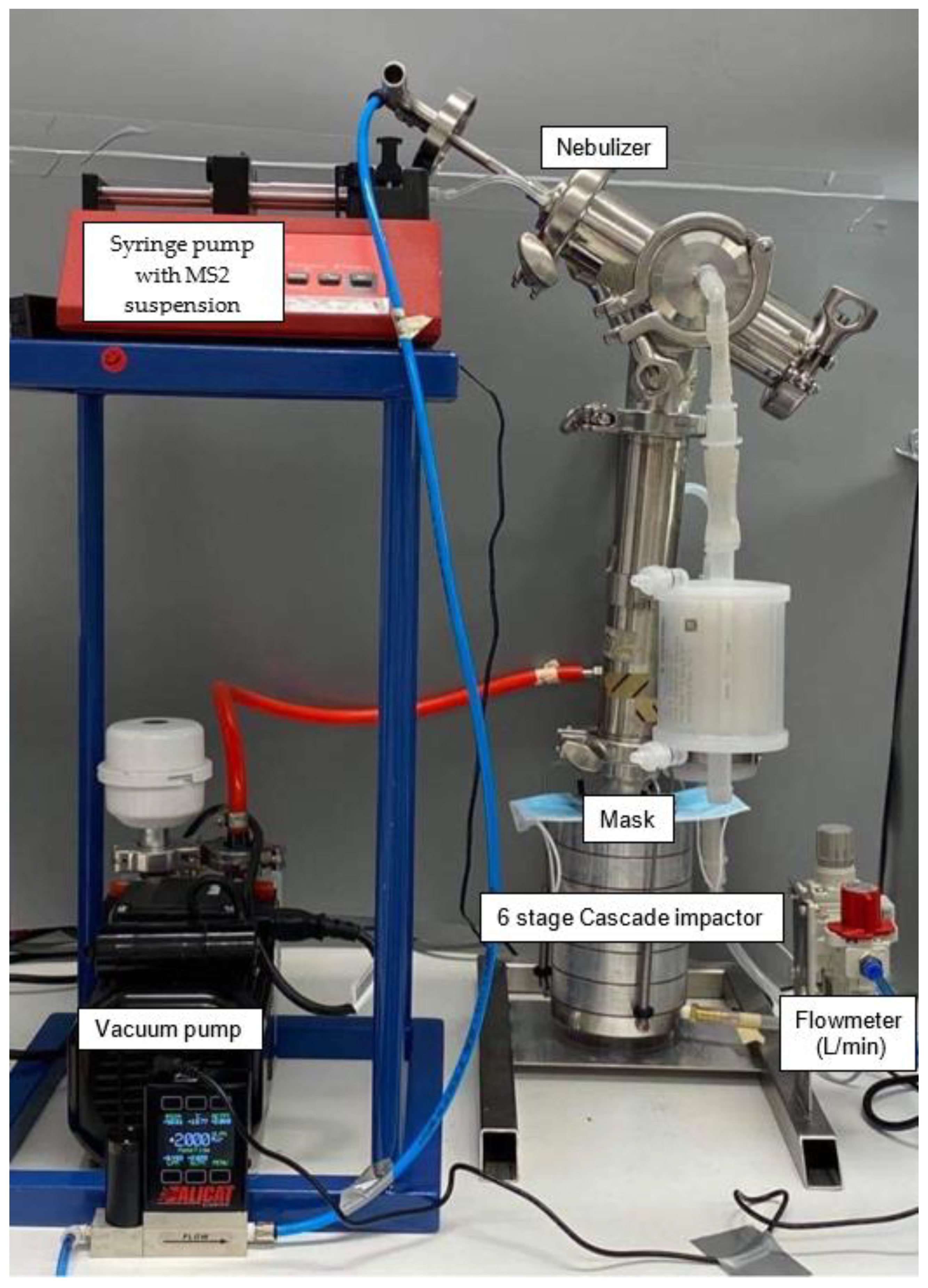
4.4. Viral Filtration Efficiency
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Javid, B.; Weekes, M.P.; Matheson, N.J. Covid-19: Should the public wear face masks? BMJ 2020, 369, m1442. [Google Scholar] [CrossRef] [PubMed]
- Howard, J.; Huang, A.; Li, Z.; Tufekci, Z.; Zdimal, V.; van der Westhuizen, H.-M.; von Delft, A.; Price, A.; Fridman, L.; Tang, L.-H. Face masks against covid-19: An evidence review. Preprints 2020, 2020, 040203. [Google Scholar]
- Eikenberry, S.E.; Mancuso, M.; Iboi, E.; Phan, T.; Eikenberry, K.; Kuang, Y.; Kostelich, E.; Gumel, A.B. To mask or not to mask: Modeling the potential for face mask use by the general public to curtail the covid-19 pandemic. Infect. Dis. Model. 2020, 5, 293–308. [Google Scholar] [CrossRef] [PubMed]
- US Centers for Disease Control and Prevention. Recommendation Regarding the Use of Cloth Face Coverings, Especially in Areas of Significant Community-Based Transmission. Available online: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover.html (accessed on 30 May 2020).
- Cheng, V.C.; Wong, S.-C.; Chuang, V.W.; So, S.Y.; Chen, J.H.; Sridhar, S.; To, K.K.; Chan, J.F.; Hung, I.F.; Ho, P.-L. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (Covid-19) epidemic due to sars-cov-2. J. Infect. 2020, 81, 107–114. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Advice on the Use of Masks in the Context of Covid-19: Interim Guidance, 5 June 2020; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Victorian State Government. Face coverings: Metropolitan Melbourne and Mitchell Shire. Available online: https://www.dhhs.vic.gov.au/face-coverings-covid-19 (accessed on 11 August 2020).
- Moore, H. Woolies customers ‘strongly encouraged’ to wear masks. Australian 2020. Available online: https://www.theaustralian.com.au/breaking-news/woolies-customers-strongly-encouraged-to-wear-masks/news-story/1ea5f63700219630ba6eeae4100e1733 (accessed on 30 August 2020).
- Feng, S.; Shen, C.; Xia, N.; Song, W.; Fan, M.; Cowling, B.J. Rational use of face masks in the Covid-19 pandemic. Lancet Respir. Med. 2020, 8, 434–436. [Google Scholar] [CrossRef]
- Brosseau, L.; Sietsema, M. Commentary: Masks-for-All for Covid-19 Not Based on Sound Data. Available online: https://www.cidrap.umn.edu/news-perspective/2020/04/commentary-masks-all-covid-19-not-based-sound-data (accessed on 8 May 2020).
- World Health Organization. Rational Use of Personal Protective Equipment for Coronavirus Disease (Covid-19): Interim Guidance, 27 February 2020; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Greenhalgh, T.; Schmid, M.B.; Czypionka, T.; Bassler, D.; Gruer, L. Face masks for the public during the Covid-19 crisis. BMJ 2020, 369, 369. [Google Scholar] [CrossRef] [PubMed]
- Victoria State Government. How to Make a Cloth Mask. Instructions for Making a Cloth Face Mask. Available online: https://www.dhhs.vic.gov.au/sites/default/files/documents/202007/Design%20and%20preparation%20of%20cloth%20mask_0.pdf (accessed on 11 August 2020).
- Kwon, J.H.; Burnham, C.-A.D.; Reske, K.A.; Liang, S.Y.; Hink, T.; Wallace, M.A.; Shupe, A.; Seiler, S.; Cass, C.; Fraser, V.J. Assessment of healthcare worker protocol deviations and self-contamination during personal protective equipment donning and doffing. Infect. Control. Hosp. Epidemiol. 2017, 38, 1077. [Google Scholar] [CrossRef] [PubMed]
- Rengasamy, S.; Eimer, B.; Shaffer, R.E. Simple respiratory protection—Evaluation of the filtration performance of cloth masks and common fabric materials against 20–1000 nm size particles. Ann. Occup. Hyg. 2010, 54, 789–798. [Google Scholar] [PubMed]
- Konda, A.; Prakash, A.; Moss, G.A.; Schmoldt, M.; Grant, G.D.; Guha, S. Aerosol filtration efficiency of common fabrics used in respiratory cloth masks. ACS Nano 2020, 14, 6339–6347. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.W.; Nicolle, A.D.; Klettner, C.A.; Pantelic, J.; Wang, L.; Suhaimi, A.B.; Tan, A.Y.; Ong, G.W.; Su, R.; Sekhar, C. Airflow dynamics of human jets: Sneezing and breathing-potential sources of infectious aerosols. PLoS ONE 2013, 8, e59970. [Google Scholar] [CrossRef] [PubMed]
- ASTM International. Astm f2101-19 Standard Test Method for Evaluating the Bacterial Filtration Efficiency (BFE) of Medical Face Mask Materials, Using a Biological Aerosol of Staphylococcus Aureus; ASTM International: West Conshohocken, PA, USA, 2019. [Google Scholar]
- Monteiro, J.M.; Fernandes, P.B.; Vaz, F.; Pereira, A.R.; Tavares, A.C.; Ferreira, M.T.; Pereira, P.M.; Veiga, H.; Kuru, E.; VanNieuwenhze, M.S.; et al. Cell shape dynamics during the staphylococcal cell cycle. Nat. Commun. 2015, 6, 8055. [Google Scholar] [CrossRef] [PubMed]
- Park, W.B.; Kwon, N.J.; Choi, S.J.; Kang, C.K.; Choe, P.G.; Kim, J.Y.; Yun, J.; Lee, G.W.; Seong, M.W.; Kim, N.J.; et al. Virus isolation from the first patient with sars-cov-2 in korea. J. Korean Med. Sci. 2020, 35, e84. [Google Scholar] [CrossRef] [PubMed]
- Mikel, P.; Vasickova, P.; Tesarik, R.; Malenovska, H.; Kulich, P.; Vesely, T.; Kralik, P. Preparation of ms2 phage-like particles and their use as potential process control viruses for detection and quantification of enteric rna viruses in different matrices. Front. Microbiol. 2016, 7, 1911. [Google Scholar] [CrossRef] [PubMed]
- Macher, J.M. Positive-hole correction of multiple-jet impactors for collecting viable microorganisms. Am. Ind. Hyg. Assoc. J. 1989, 50, 561–568. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Lee, G.W.; Chen, C.-M.; Wu, C.-C.; Yu, K.-P. The size and concentration of droplets generated by coughing in human subjects. J. Aerosol Med. 2007, 20, 484–494. [Google Scholar] [CrossRef] [PubMed]
- Labiris, N.R.; Dolovich, M.B. Pulmonary drug delivery, Part I: Physiological factors affecting therapeutic effectiveness of aerosolized medications. Br. J. Clin. Pharmacol. 2003, 56, 588–599. [Google Scholar] [CrossRef] [PubMed]


| Mask | Average Viral Filtration Efficiency for an Average Aerosol Size of 6.0 µm (VFE(6.0 µm)) (%) [Range] | Average Viral Filtration Efficiency Calculated with the Larger Aerosols Excluded to Give an Average Aerosol Size of 2.6 µm (VFE(2.6 µm)) (%) [Range] | Description 1 |
|---|---|---|---|
| N95 | 99.9 [99.8–100] | 99.3 [98.6–99.7] | KN95 (nonmedical device GB2626-2006) |
| Surgical 1 | 99.9 [99.8–100] | 99.5 [98.7–99.5} | Level 1 single use surgical mask (according to AS 4381:2015 Nelson Laboratories, USA, bacterial filtration efficacy (BF) average 98.2%, minimum 97.1% as per ASTMF1862) |
| Surgical 2 | 99.6 [99.3–99.8] | 98.5 [98.3–98.6] | Surgical face mask (99.9% BFE 2) |
| Disposable 1 | 99.9 [99.9–100] | 99.7 [99.7–99.9] | Disposable face mask (nonmedical GB/T32610-2016) |
| Fabric 1 | 54.4 [54.3–54.6] | 65.8 [64.1–67.6] | Three layered masks made of 100% cotton |
| Fabric 2 | 67.3 [54.8–92.1] | 90.9 [86.5–94.3] | Denim face mask—double layer stretchy cotton |
| Fabric 3 | 93.6 [92.1–96.3] | 89.0 [86.1–90.5] | 100% hemp outer layer, poly membrane mid layer, and organic cheesecloth inner layer |
| Fabric 4 | 50.3 [49.7–51.2] | 63.6 [51.8–75.0] | Two layers of 100% Mulberry Silk |
| Fabric 5 | 54.9 [55.4–55.7] | 93.32 [86.9–97.7] | Washable fabric face mask with pocket for filter made from cotton and poplin fabric |
| Fabric 5 + dried baby wipe | 98.5 [97.7–99.6] | 97.6 [97.0–98.5] | Fabric 5 with a dried baby wipe inserted into the pocket |
| Fabric 5 + vacuum cleaner bag | 99.5 [98.9–99.9] | 98.8 [96.9–99.8] | Fabric 5 with a section of a vacuum cleaner bag inserted into the pocket |
| Fabric 6 | 98.6 [97.7–99.6] | 99.1 [98.3–99.7] | Made using the Victorian DHHS design [13]. Two layers of reusable shopping bag (nonwoven polypropylene) and one layer of cotton |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Whiley, H.; Keerthirathne, T.P.; Nisar, M.A.; White, M.A.F.; Ross, K.E. Viral Filtration Efficiency of Fabric Masks Compared with Surgical and N95 Masks. Pathogens 2020, 9, 762. https://doi.org/10.3390/pathogens9090762
Whiley H, Keerthirathne TP, Nisar MA, White MAF, Ross KE. Viral Filtration Efficiency of Fabric Masks Compared with Surgical and N95 Masks. Pathogens. 2020; 9(9):762. https://doi.org/10.3390/pathogens9090762
Chicago/Turabian StyleWhiley, Harriet, Thilini Piushani Keerthirathne, Muhammad Atif Nisar, Mae A. F. White, and Kirstin E. Ross. 2020. "Viral Filtration Efficiency of Fabric Masks Compared with Surgical and N95 Masks" Pathogens 9, no. 9: 762. https://doi.org/10.3390/pathogens9090762
APA StyleWhiley, H., Keerthirathne, T. P., Nisar, M. A., White, M. A. F., & Ross, K. E. (2020). Viral Filtration Efficiency of Fabric Masks Compared with Surgical and N95 Masks. Pathogens, 9(9), 762. https://doi.org/10.3390/pathogens9090762






