Survival of Lassa Virus in Blood and Tissue Culture Media and in a Small Particle Aerosol
Abstract
1. Introduction
2. Results
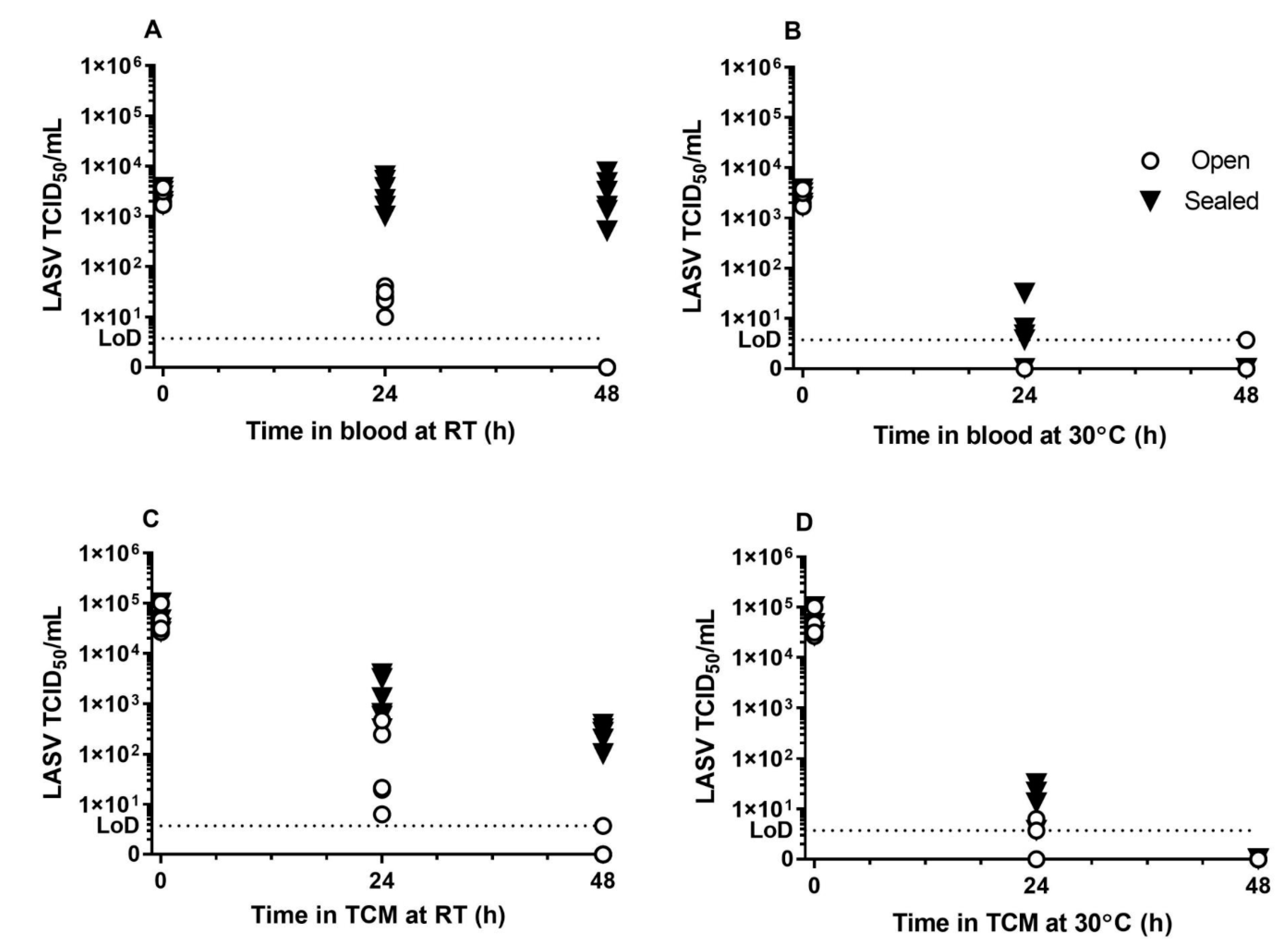
2.1. Survival of Lassa Virus in Blood and Tissue Culture Media
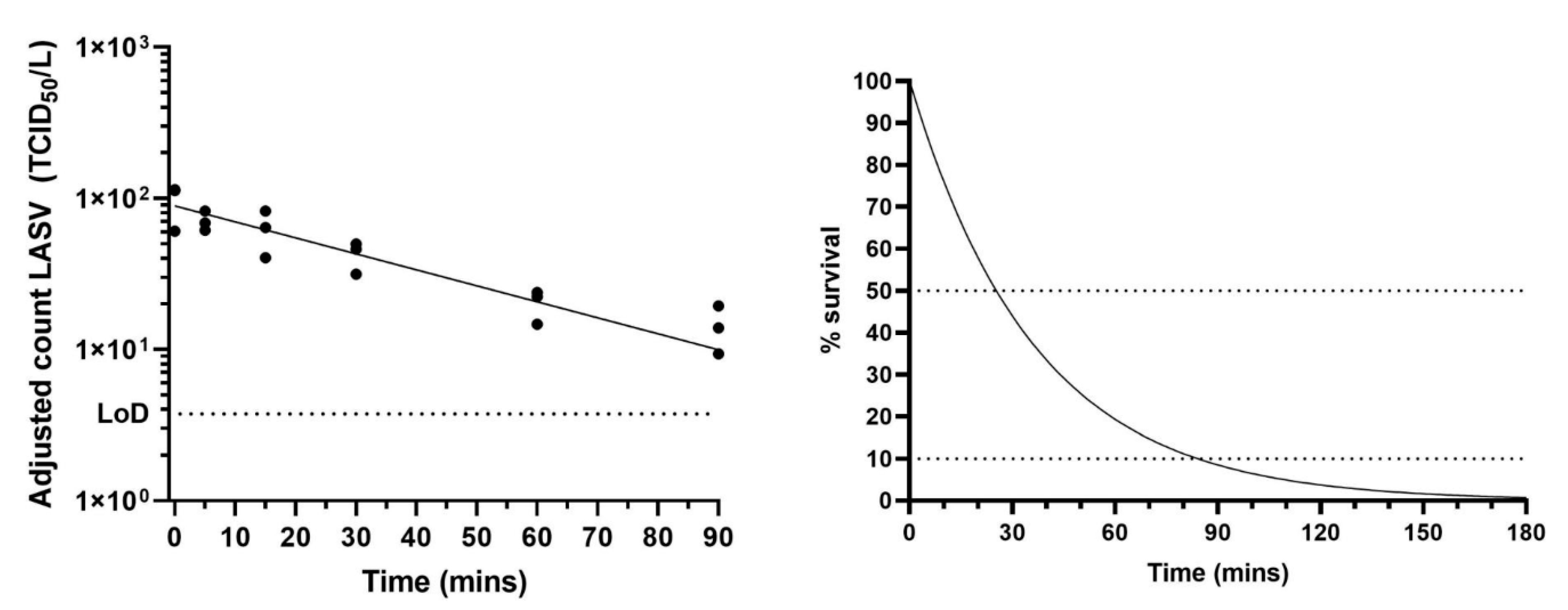
2.2. Survival of Lassa Virus in a Small Particle Aerosol
3. Discussion
4. Materials and Methods
4.1. Virus Growth and Enumeration
4.2. Liquid Survival Studies
4.3. Viral Survival Studies Within Aerosols Using the Rotating GOLDBERG Drum
Author Contributions
Funding
Conflicts of Interest
Disclaimer
References
- Asogun, D.A.; Günther, S.; Akpede, G.O.; Ihekweazu, C.; Zumla, A. Lassa fever: Epidemiology, clinical features, diagnosis, management and prevention. Infect. Dis. Clin. N. Am. 2019, 33, 933–951. [Google Scholar] [CrossRef] [PubMed]
- Delahoy, M.J.; Wodnik, B.; McAliley, L.; Penakalapati, G.; Swarthout, J.; Freeman, M.C.; Levy, K. Pathogens transmitted in animal feces in low- and middle-income countries. Int. J. Hyg. Environ. Health 2018, 221, 661–676. [Google Scholar] [CrossRef]
- Monath, T.P. A short history of Lassa fever: The first 10–15 years after discovery. Curr. Opin. Virol. 2019, 37, 77–83. [Google Scholar] [CrossRef] [PubMed]
- WHO. Essential medicines and health products. Available online: https://www.who.int/medicines/ebola-treatment/WHO-list-of-top-emerging-diseases/en/ (accessed on 8 July 2020).
- WHO Emergencies Preparedness, Response. Lassa Fever. Available online: https://www.who.int/csr/don/20-april-2018-lassa-fever-nigeria/en/ (accessed on 8 July 2020).
- Fisher-Hoch, S.P.; Tomori, O.; Nasidi, A.; Perez-Oronoz, G.I.; Fakile, Y.; Hutwagner, L.; McCormick, J.B. Review of cases of nosocomial Lassa fever in Nigeria: The high price of poor medical practice. BMJ 1995, 311, 857–859. [Google Scholar] [CrossRef] [PubMed]
- Kofman, A.; Choi, M.J.; Rollin, P.E. Lassa fever in travelers from West Africa, 1969–2016. Emerg. Infect. Dis. 2019, 25, 245–248. [Google Scholar] [CrossRef]
- Judson, S.D.; Munster, V.J. Nosocomial transmission of emerging viruses via aerosol-generating medical procedures. Viruses 2019, 11, 940. [Google Scholar] [CrossRef]
- Smither, S.J.; Eastaugh, L.S.; Findlay, J.S.; O’Brien, L.M.; Thom, R.; Lever, M.S. Survival and persistence of Nipah virus in blood and tissue culture media. Emerg. Microbes Infect. 2019, 8, 1760–1762. [Google Scholar]
- Piercy, T.J.; Smither, S.J.; Steward, J.A.; Eastaugh, L.; Lever, M.S. The survival of filoviruses in liquids, on solid substrates and in a dynamic aerosol. J. Appl. Microbiol. 2010, 109, 1531–1539. [Google Scholar] [CrossRef]
- Sagripanti, J.L.; Rom, A.M.; Holland, L.E. Persistence in darkness of virulent alphaviruses, Ebola virus, and Lassa virus deposited on solid surfaces. Arch. Virol. 2010, 155, 2035–2039. [Google Scholar] [CrossRef]
- Hardestam, J.; Simon, M.; Hedlund, K.O.; Vaheri, A.; Klingström, J.; Lundkvist, A. Ex vivo stability of the rodent-borne Hantaan virus in comparison to that of arthropod-borne members of the Bunyaviridae family. Appl. Environ. Microbiol. 2007, 73, 2547–2551. [Google Scholar] [CrossRef]
- Carrion, R., Jr.; Brasky, K.; Mansfield, K.; Johnson, C.; Gonzales, M.; Ticer, A.; Lukashevich, I.; Tardif, S.; Patterson, J. Lassa virus infection in experimentally infected marmosets: Liver pathology and immunophenotypic alterations in target tissues. J. Virol. 2007, 81, 6482–6490. [Google Scholar] [CrossRef] [PubMed]
- Downs, I.L.; Shaia, C.I.; Zeng, X.; Johnson, J.C.; Hensley, L.; Saunders, D.L.; Rossi, F.; Cashman, K.A.; Esham, H.L.; Gregory, M.K.; et al. Natural history of aerosol induced lassa fever in non-human primates. Viruses 2020, 12, 593. [Google Scholar] [CrossRef] [PubMed]
- McCormick, J.B.; King, I.J.; Webb, P.A.; Scribner, C.L.; Craven, R.B.; Johnson, K.M.; Elliott, L.H.; Belmont-Williams, R. Lassa fever. Effective therapy with ribavirin. N. Engl. J. Med. 1986, 314, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Happi, A.N.; Happi, C.T.; Schoepp, R.J. Lassa fever diagnostics: Past, present, and future. Curr. Opin. Virol. 2019, 37, 132–138. [Google Scholar] [CrossRef] [PubMed]
- Boisen, M.L.; Uyigue, E.; Aiyepada, J.; Siddle, K.; Oestereich, L.; Nelson, D.K.S.; Bush, D.; Rowland, M.M.; Heinrich, M.L.; Eromon, P.; et al. Field evaluation of a Pan-Lassa rapid diagnostic test during the 2018 Nigerian Lassa fever outbreak. Sci. Rep. 2020, 10, 8724. [Google Scholar] [CrossRef] [PubMed]
- Climate Data. Available online: https://en.climate-data.org/africa/ (accessed on 12 August 2020).
- Stephenson, E.H.; Larson, E.W.; Dominik, J.W. Effect of environmental factors on aerosol-induced Lassa virus infection. J. Med. Virol. 1984, 14, 295–303. [Google Scholar] [CrossRef]
- Sinclair, R.; Boone, S.A.; Greenberg, D.; Keim, P.; Gerba, C.P. Persistence of category a select agents in the environment. Appl. Environ. Microbiol. 2008, 74, 555–563. [Google Scholar] [CrossRef]
- Papineni, R.S.; Rosenthal, F.S. The size distribution of droplets in the exhaled breath of healthy human subjects. J. Aerosol. Med. 1997, 10, 105–116. [Google Scholar] [CrossRef]
- Asadi, S.; Wexler, A.S.; Cappa, C.D.; Barreda, S.; Bouvier, M.N.; Ristenpart, W.D. Effect of voicing and articulation manner on aerosol particle emission during human speech. PLoS ONE 2020, 15, e0227699. [Google Scholar] [CrossRef]
- Schuit, M.; Gardner, S.; Wood, S.; Bower, K.; Williams, G.; Freeburger, D.; Dabisch, P. The influence of simulated sunlight on the inactivation of influenza virus in aerosols. J. Infect. Dis. 2020, 221, 372–378. [Google Scholar] [CrossRef]
- van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I.; et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef] [PubMed]
- Smither, S.J.; Eastaugh, L.S.; Findlay, J.S.; Lever, M.S. Experimental aerosol survival of SARS-CoV-2 in artificial saliva and tissue culture media at medium and high humidity. Emerg. Microbes Infect. 2020, 9, 1415–1417. [Google Scholar] [CrossRef] [PubMed]
- Vasickova, P.; Pavlik, I.; Verani, M.; Carducci, A. Issues concerning survival of viruses on surfaces. Food Environ. Virol. 2010, 2, 24–34. [Google Scholar] [CrossRef]
- Grundy, D.J.; Bowen, E.T.; Lloyd, G. Isolated case of Lassa fever in Zaria, Northern Nigeria. Lancet 1980, 2, 649–650. [Google Scholar] [CrossRef]
- Reed, L.J.; Muench, H. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 1938, 27, 493–497. [Google Scholar]
| Substrate | Temperature | Open | Sealed |
|---|---|---|---|
| TCM | 19–22 °C | 0.250 | 0.149 |
| 30 °C | 0.411 | 0.325 | |
| Blood | 19–22 °C | 0.194 | ND |
| 30 °C | ND | 0.224 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Smither, S.J.; Eastaugh, L.S.; Findlay, J.S.; O’Brien, L.M.; Lever, M.S. Survival of Lassa Virus in Blood and Tissue Culture Media and in a Small Particle Aerosol. Pathogens 2020, 9, 680. https://doi.org/10.3390/pathogens9090680
Smither SJ, Eastaugh LS, Findlay JS, O’Brien LM, Lever MS. Survival of Lassa Virus in Blood and Tissue Culture Media and in a Small Particle Aerosol. Pathogens. 2020; 9(9):680. https://doi.org/10.3390/pathogens9090680
Chicago/Turabian StyleSmither, Sophie J, Lin S Eastaugh, James S Findlay, Lyn M O’Brien, and Mark S Lever. 2020. "Survival of Lassa Virus in Blood and Tissue Culture Media and in a Small Particle Aerosol" Pathogens 9, no. 9: 680. https://doi.org/10.3390/pathogens9090680
APA StyleSmither, S. J., Eastaugh, L. S., Findlay, J. S., O’Brien, L. M., & Lever, M. S. (2020). Survival of Lassa Virus in Blood and Tissue Culture Media and in a Small Particle Aerosol. Pathogens, 9(9), 680. https://doi.org/10.3390/pathogens9090680




