The Prevalence of Chlamydia trachomatis and Three Other Non-Viral Sexually Transmitted Infections among Pregnant Women in Pemba Island Tanzania
Abstract
1. Introduction
2. Methods
2.1. Sample Collection and Design
2.2. DNA Isolation and Real-Time PCR
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Study Population
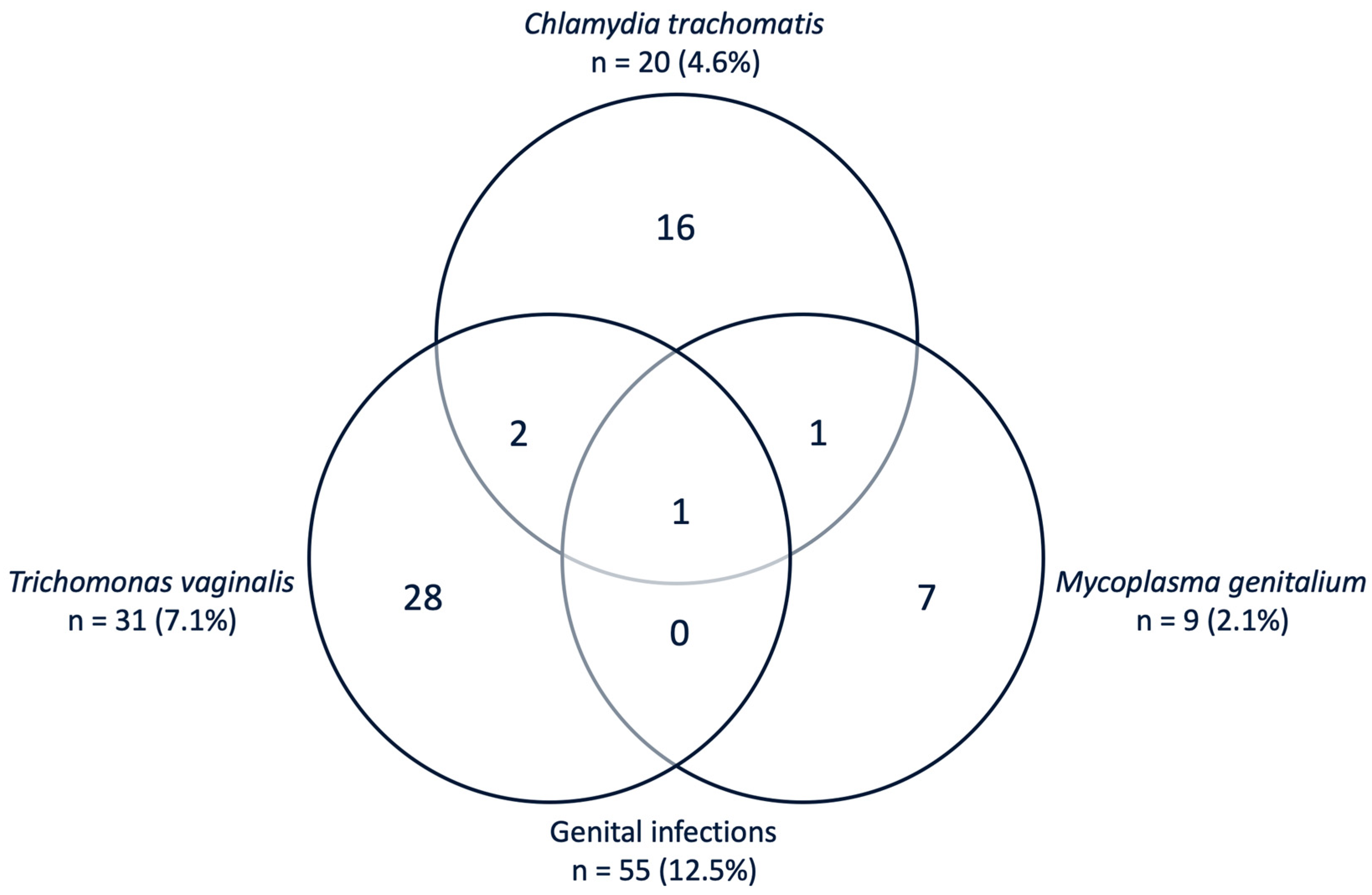
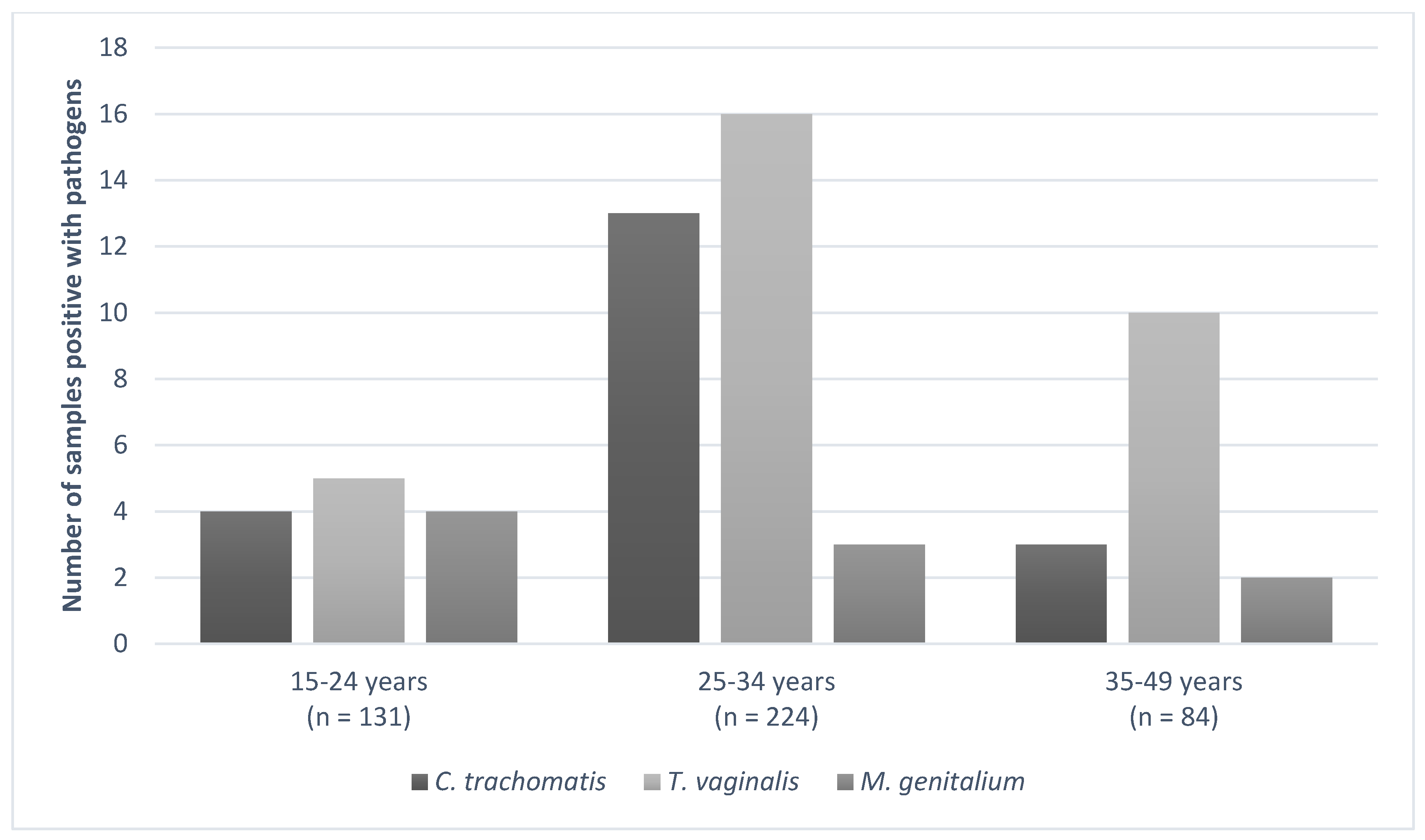
3.2. Genital Infections Prevalence
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Rowley, J.; Vander Hoorn, S.; Korenromp, E.; Low, N.; Unemo, M.; Abi-Raddad, L.J.; Chico, R.M.; Smolak, A.; Newman, L.; Gottlieb, S.; et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: Global prevalence and incidence estimates. Bull. World Health Org. 2019, 97, 548–562. [Google Scholar] [CrossRef]
- World Health Organization. Report on Global Sexually Transmitted Infection Surveillance, 2018; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- World Health Organization. Global Health Sector Strategy on Sexually Transmitted Infections 2016–Towards Ending STIs; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- World Health Organization. Global Incidence and Prevalence of Selected Curable Sexually Transmitted Infections-2008; WHO: Geneva, Switzerland, 2012. [Google Scholar]
- McGregor, J.A.; French, J.I.; Seo, K. Premature rupture of membranes and bacterial vaginosis. Am. J. Obstet. Gynecol. 1993, 169, 463–466. [Google Scholar] [CrossRef]
- Adachi, K.; Nielsen-Saines, K.; Klausner, J.D. Chlamydia trachomatis Infection in Pregnancy: The Global Challenge of Preventing Adverse Pregnancy and Infant Outcomes in Sub-Saharan Africa and Asia. Biomed. Res. Int. 2016, 2016, 9315757. [Google Scholar] [CrossRef]
- Oakeshott, P.; Hay, P.; Taylor-Robinson, D.; Hay, S.; Dohn, B.; Kerry, S.; Jensen, J.S. Prevalence of Mycoplasma genitalium in early pregnancy and relationship between its presence and pregnancy outcome. BJOG Int. J. Obstet. Gynaecol. 2004, 111, 1464–1467. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guidelines for the Treatment of Chlamydia Trachomatis; WHO: Geneva, Switzerland, 2016; ISBN 9789241549714. [Google Scholar]
- Nusbaum, M.; Wallace, R.; Slatt, L.M.; Kondrad, E.C. Sexually transmitted infections and increased risk of co-infection with human immunodeficiency virus. J. Am. Osteopath. Assoc. 2004, 104, 527–535. [Google Scholar] [PubMed]
- Watson-Jones, D.; Weiss, H.A.; Changalucha, J.M.; Todd, J.; Gumodoka, B.; Bulmer, J.; Balira, R.; Ross, D.; Mugeye, K.; Hayes, R.; et al. Adverse birth outcomes in United Republic of Tanzania—Impact and prevention of maternal risk factors. Bull. World Health Organ. 2007, 85, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Donders, G.G.G.; Desmyter, J.; De Wet, D.H.; Van Assche, F.A. The association of gonorrhoea and syphilis with premature birth and low birthweight. Genitourin. Med. 1993, 69, 98–101. [Google Scholar] [CrossRef] [PubMed]
- Gravett, M.G.; Nelson, H.P.; Derouen, T.; Critchlow, C.; Eschenbach, D.A.; Holmes, K.K. Independent Associations of Bacterial Vaginosis and Chlamydia trachomatis Infection With Adverse Pregnancy Outcome. JAMA J. Am. Med. Assoc. 1986, 256, 1899–1903. [Google Scholar] [CrossRef]
- Cotch, M.F.; Pastorek, J.G.; Nugent, R.P.; Hillier, S.L.; Gibbs, R.S.; Martin, D.H.; Eschenbach, D.A.; Edelman, R.; Carey, J.C.; Regan, J.A.; et al. Trichomonas vaginalis associated with low birth weight and preterm delivery. The Vaginal Infections and Prematurity Study Group. Sex. Transm. Dis. 1997, 24, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Heumann, C.L.; Quilter, L.A.S.; Eastment, M.C.; Heffron, R.; Hawes, S.E. Adverse birth outcomes and maternal Neisseria gonorrhoeae infection: A population-based cohort study in Washington State. Sex. Transm. Dis. 2017, 44, 266–271. [Google Scholar] [CrossRef]
- Martius, J.; Krohn, M.A.; Millier, S.L.; Stamm, W.E.; Holmes, K.K.; Eschenbach, D.A. Relationships of vaginal lactobacillus species, cervical chlamydia trachomatis, and bacterial vaginosis to preterm birth. Obstet. Gynecol. 1988, 71, 89–95. [Google Scholar] [PubMed]
- Torrone, E.A.; Morrison, C.S.; Chen, P.L.; Kwok, C.; Francis, S.C.; Hayes, R.J.; Looker, K.J.; McCormack, S.; McGrath, N.; van de Wijgert, J.H.H.M.; et al. Prevalence of sexually transmitted infections and bacterial vaginosis among women in sub-Saharan Africa: An individual participant data meta-analysis of 18 HIV prevention studies. PLoS Med. 2018, 15, e1002511. [Google Scholar] [CrossRef] [PubMed]
- Davey, D.L.J.; Shull, H.I.; Billings, J.D.; Wang, D.; Adachi, K.; Klausner, J.D. Prevalence of curable sexually transmitted infections in pregnant women in low- and middle-income countries from 2010 to 2015: A systematic review. Sex. Transm. Dis. 2016, 43, 450–458. [Google Scholar] [CrossRef] [PubMed]
- Kapiga, S.H.; Sam, N.E.; Mlay, J.; Aboud, S.; Ballard, R.C.; Shao, J.F.; Larsen, U. The epidemiology of HIV-1 infection in northern Tanzania: Results from a community-based study. AIDS Care Psychol. Socio-Med Asp. AIDS/HIV 2006, 18, 379–387. [Google Scholar] [CrossRef]
- Thriemer, K.; Ley, B.; Ame, S.; von Seidlein, L.; Pak, G.D.; Chang, N.Y.; Hashim, R.; Schmied, W.H.; Busch, C.J.-L.; Nixon, S.; et al. The Burden of Invasive Bacterial Infections in Pemba, Zanzibar. PLoS ONE 2012, 7, e30350. [Google Scholar] [CrossRef]
- Alliance for Maternal and Newborn Health Improvement; Baqui, A.H.; Khanam, R.; Rahman, M.S.; Ahmed, A.; Rahman, H.H.; Moin, M.I.; Ahmed, S.; Jehan, F.; Nisar, I.; et al. Understanding biological mechanisms underlying adverse birth outcomes in developing countries: Protocol for a prospective cohort (AMANHI bio-banking) study. J. Glob. Health 2017, 7, 021201. [Google Scholar] [CrossRef]
- Dols, J.A.M.; Molenaar, D.; van der Helm, J.J.; Caspers, M.P.M.; Angelino-Bart, A.K.; Schuren, F.H.J.; Speksnijder, A.G.C.L.; Westerhoff, H.V.; Richardus, J.H.; Boon, M.E.; et al. Molecular assessment of bacterial vaginosis by Lactobacillus abundance and species diversity. BMC Infect. Dis. 2016, 180, 1–8. [Google Scholar] [CrossRef]
- de Waaij, D.J.; Ouburg, S.; Dubbink, J.H.; Peters, R.P.H.; Morré, S.A. Evaluation of Prestoplus assay and LightMix kit Trichomonas vaginalis assay for detection of Trichomonas vaginalis in dry vaginal swabs. J. Microbiol. Methods 2016, 127, 102–104. [Google Scholar] [CrossRef][Green Version]
- de Waaij, D.J.; Dubbink, J.H.; Peters, R.P.H.; Ouburg, S.; Morré, S.A. Comparison of GMT presto assay and Roche cobas® 4800 CT/NG assay for detection of Chlamydia trachomatis and Neisseria gonorrhoeae in dry swabs. J. Microbiol. Methods 2015, 118, 70–74. [Google Scholar] [CrossRef]
- Müller, E.E.; Venter, J.M.E.; Magooa, M.P.; Morrison, C.; Lewis, D.A.; Mavedzenge, S.N. Development of a rotor-gene real-time PCR assay for the detection and quantification of Mycoplasma genitalium. J. Microbiol. Methods 2012, 88, 311–315. [Google Scholar] [CrossRef]
- Daniel, W. Biostatistics: A Foundation for Analysis in the Health Sciences; John Wiley & Sons: New York, NY, USA, 1999; pp. 120–159. [Google Scholar]
- Ahmed, I.; Ali, S.M.; Amenga-Etego, S.; Ariff, S.; Bahl, R.; Baqui, A.H.; Begum, N.; Bhandari, N.; Bhatia, K.; Bhutta, Z.A.; et al. Population-based rates, timing, and causes of maternal deaths, stillbirths, and neonatal deaths in south Asia and sub-Saharan Africa: A multi-country prospective cohort study. Lancet Glob. Health 2018, 6, e1297–e1308. [Google Scholar] [CrossRef]
- Aboud, S.; Msamanga, G.; Read, J.S.; Mwatha, A.; Chen, Y.Q.; Potter, D.; Valentine, M.; Sharma, U.; Hoffmann, I.; Taha, T.E.; et al. Genital tract infections among HIV-infected pregnant women in Malawi, Tanzania and Zambia. Int. J. STD AIDS 2008, 19, 824–832. [Google Scholar] [CrossRef] [PubMed]
- Chiduo, M.; Theilgaard, Z.P.; Bakari, V.; Mtatifikolo, F.; Flanholc, L.; Gerstoft, J.; Christiansen, C.B.; Phd, L.; Katzenstein, T.L. Prevalence of sexually transmitted infections among women attending antenatal clinics in Tanga, north eastern Tanzania. Int. J. STD AIDS 2012, 23, 325–329. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization; United Nations; Unicef. Epidemiological Fact Sheets on HIV/AIDS and Sexually Transmitted Infections. Available online: http://data.unaids.org/publications/fact-sheets01/tanzania_en.pdf (accessed on 31 March 2020).
- Hokororo, A.; Kihunrwa, A.; Hoekstra, P.; Kalluvya, S.E.; Changalucha, J.M.; Fitzgerald, D.W.; Downs, J.A. High prevalence of sexually transmitted infections in pregnant adolescent girls in Tanzania: A multi-community cross-sectional study. Sex. Transm. Infect. 2015, 91, 473–478. [Google Scholar] [CrossRef] [PubMed]
- McCleary-Sills, J.; Douglas, Z.; Rwehumbiza, A.; Hamisi, A.; Mabala, R. Gendered norms, sexual exploitation and adolescent pregnancy in rural Tanzania. Reprod. Health Matters 2013, 21, 97–105. [Google Scholar] [CrossRef]
- Chacko, M.R.; Lovchik, J.C. Chiamydia trachomatis Infection in Sexually Active Adolescents: Prevalence and Risk Factors. Pediatrics 1984, 73, 836–840. [Google Scholar]
- Chen, X.-S.; Yin, Y.-P.; Chen, L.-P.; Thuy, N.T.T.; Zhang, G.-Y.; Shi, M.-Q.; Hu, L.-H.; Yu, Y.-H. Sexually Transmitted Infections Among Pregnant Women Attending an Antenatal Clinic in Fuzhou, China. Sex. Transm. Dis. 2006, 33, 296–301. [Google Scholar] [CrossRef]
- Slurink, I.A.; National Institute for Public Health and the Environment (RIVM); Netherlands Institute for Health Services Research (Nivel); Stichting HIV Monitoring (SHM) (HIV Monitoring Foundation). Sexually Transmitted Infections in The Netherlands in 2018; RIVM: Bilthoven, The Netherlands, 2019. [Google Scholar]
- Williams, C.L.; Harrison, L.L.; Llata, E.; Smith, R.A.; Meites, E. Sexually Transmitted Diseases Among Pregnant Women: 5 States, United States, 2009. Matern. Child Healthj. 2018, 22, 538–545. [Google Scholar] [CrossRef]
- Teasdale, C.A.; Abrams, E.J.; Chiasson, M.A.; Justman, J.; Blanchard, K.; Jones, H.E. Incidence of sexually transmitted infections during pregnancy. PLoS ONE 2018, 13, e0197696. [Google Scholar] [CrossRef]
- Adamczyk, A.; Hayes, B.E. Religion and Sexual Behaviors: Understanding the Influence of Islamic Cultures and Religious Affiliation for Explaining Sex Outside of Marriage. Am. Sociol. Rev. 2012, 77, 723–746. [Google Scholar] [CrossRef]
- Kakaire, O.; Byamugisha, J.K.; Tumwesigye, N.M.; Gamzell-Danielsson, K. Prevalence and Factors Associated with Sexually Transmitted Infections among HIV Positive Women Opting for Intrauterine Contraception. PLoS ONE 2015, 10, e0122400. [Google Scholar] [CrossRef] [PubMed]
- Lovett, A.; Duncan, J.A. Human immune response and the natural history of neisseria gonorrhoeae infection. Front. Immunol. 2019, 9, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Van Der Pol, B. Trichomonas vaginalis Infection: The Most Prevalent Nonviral Sexually Transmitted Infection Receives the Least Public Health Attention. Clin. Infect. Dis. 2007, 44, 23–25. [Google Scholar] [CrossRef] [PubMed]
- Sheffield, J.S.; Andrews, W.W.; Klebanoff, M.A.; MacPherson, C.; Carey, J.C.; Ernest, J.M.; Wapner, R.J.; Trout, W.; Moawad, A.; Miodovnik, M.; et al. Spontaneous resolution of asymptomatic Chlamydia trachomatis in pregnancy. Obstet. Gynecol. 2005, 105, 557–562. [Google Scholar] [CrossRef] [PubMed]
- Bowden, F.J.; Garnett, G.P. Trichomonas vaginalis epidemiology: Parameterising and analysing a model of treatment interventions. Sex. Trans. Inf. 2000, 76, 248–256. [Google Scholar] [CrossRef]
- Morré, S.A.; Van den Brule, A.J.C.; Rozendaal, L.; Boeke, A.J.P.; Voorhorst, F.J.; De Blok, S.; Meijer, C.J.L.M. The natural course of asymptomatic Chlamydia trachomatis infections: 45% Clearance and no development of clinical PID after one-year follow-up. Proc. Int. J. STD AIDS 2002, 13, 12–18. [Google Scholar] [CrossRef]
- Masha, S.C.; Cools, P.; Descheemaeker, P.; Reynders, M.; Sanders, E.J.; Vaneechoutte, M. Urogenital pathogens, associated with Trichomonas vaginalis, among pregnant women in Kilifi, Kenya: A nested case-control study. BMC Infect. Dis. 2018, 18, 549. [Google Scholar] [CrossRef]
- Leonard, C.A.; Schoborg, R.V.; Low, N.; Unemo, M.; Borel, N. Pathogenic Interplay Between Chlamydia trachomatis and Neisseria gonorrhoeae that Influences Management and Control Efforts—More Questions than Answers? Curr. Clin. Microbiol. Rep. 2019, 6, 182–191. [Google Scholar] [CrossRef]
- Reekie, J.; Donovan, B.; Guy, R.; Hocking, J.S.; Kaldor, J.M.; Mak, D.; Preen, D.; Ward, J.; Liu, B.; Chlamydia and Reproductive Health Outcome. Risk of ectopic pregnancy and tubal infertility following gonorrhea and chlamydia infections. Clin. Infect. Dis. 2019, 69, 1621–1623. [Google Scholar] [CrossRef]
- Malogajski, J.; Brankovic, I.; Stephan, P.V.; Ambrosino, E.; Van Agtmael, M.A.; Brand, A.; Ouburg, S.; Servaas, A.M. Translational potential into health care of basic genomic and genetic findings for human immunodeficiency virus, Chlamydia trachomatis, and human. BioMed Res. Int. 2013, 2013, 1–10. [Google Scholar] [CrossRef]
- Janssen, K.J.H.; Dirks, J.A.M.C.; Dukers-Muijrers, N.H.T.M.; Hoebe, C.J.P.A.; Wolffs, P.F.G. Review of Chlamydia trachomatis viability methods: Assessing the clinical diagnostic impact of NAAT positive results. Expert Rev. Mol. Diagn. 2018, 18, 739–747. [Google Scholar] [CrossRef]
- Berg, E.; Benson, D.M.; Haraszkiewicz, P.; Grieb, J.; McDonald, J. High Prevalence of Sexually Transmitted Diseases in Women with Urinary Infections. Acad. Emerg. Med. 1996, 3, 1030–1034. [Google Scholar] [CrossRef] [PubMed]
- Annang, L.; Walsemann, K.M.; Maitra, D.; Kerr, J.C. Does education matter? Examining racial differences in the association between education and STI diagnosis among black and white young adult females in the U.S. Public Health Rep. 2010, 125, 110–121. [Google Scholar] [CrossRef] [PubMed]
- Halpern, C.T.; Joyner, K.; Udry, J.R.; Suchindran, C. Smart teens don’t have sex (or kiss much either). J. Adolesc. Health 2000, 26, 213–225. [Google Scholar] [CrossRef]
- Abdul, R.; Gerritsen, A.A.M.; Mwangome, M.; Geubbels, E. Prevalence of self-reported symptoms of sexually transmitted infections, knowledge and sexual behaviour among youth in semi-rural Tanzania in the period of adolescent friendly health services strategy implementation. BMC Infect. Dis. 2018, 18, 1–10. [Google Scholar] [CrossRef]
- Wilson Chialepeh, N.; Sathiyasusuman, A. Associated Risk Factors of STIs and Multiple Sexual Relationships among Youths in Malawi. PLoS ONE 2015, 10, e0134286. [Google Scholar]
- Ministry of Health, Community Development, Gender, Elderly and Children—MoHCDGEC/Tanzania Mainland; Ministry of Health—MoH/Zanzibar; National Bureau of Statistics—NBS/Tanzania; Office of Chief Government Statistician—OCGS/Zanzibar and ICF. Tanzania Demographic and Health Survey and Malaria Indicator Survey (TDHS-MIS) 2015–16; NBS: Dar es Salaam, Africa, 2016.
- Wiesenfeld, H.; Manhart, L. Mycoplasma genitalium in women: Current knowledge and research priorities for this recently emerged pathogen. J. Infect. Dis. 2017, S389–S395. [Google Scholar] [CrossRef]
- Mullick, S.; Watson-Jones, D.; Beksinska, M.; Mabey, D. Sexually transmitted infections in pregnancy: Prevalence, impact on pregnancy outcomes, and approach to treatment in developing countries. Sex. Transm. Infect. 2005, 81, 294–302. [Google Scholar] [CrossRef] [PubMed]
- Thomas, P.P.M.; Allam, R.R.; Ambrosino, E.; Malogajski, J.; Lal, J.A.; Morré, S.A.; Peters, R.P.H. An Integrated Care Model With Implementation Roadmap to Improve Chlamydia trachomatis Management and Control in India. Front. Public Health 2018, 6, 321. [Google Scholar] [CrossRef]
- Lal, J.A.; Malogajski, J.; Verweij, S.P.; de Boer, P.; Ambrosino, E.; Brand, A.; Ouburg, S.; Morré, S.A. Chlamydia trachomatis Infections and Subfertility: Opportunities to Translate Host Pathogen Genomic Data into Public Health. Public Health Genom. 2013, 16, 50–61. [Google Scholar] [CrossRef]
| No (%) or Mean (Range) | |
|---|---|
| Mean maternal age (n = 439) | 28.3 (16–48) year |
| Mean gravidity (n = 434) | 4.6 (1–16) |
| Mean parity (n = 374) | 3.6 (0–10) |
| Number of first pregnancy (n = 374) | 60 (16.0%) |
| History with stillbirth (n = 374) | 30 (8.0%) |
| History with PROM (n = 371) | 18 (4.9%) |
| History with preterm delivery (n = 371) | 26 (7.0%) |
| Previously diagnosed with HIV/AIDS * (n= 430) | 1 (0.23%) |
| Number of years attended in school (n = 434) | 2.1 ± 1.7 (1–5) (Mean ± SD (range)) n = 127 (29.3 %) one year n = 241 (55.5 %) two years n = 13 (3.0 %) three years n = 3 (0.7 %) four years n = 50 (11.5%) five years |
| Smoking (n = 431) | 0 (0%) |
| Ethnicity (n = 439) | 100% Shirazi (Zanzibar Africans) |
| Religion | |
| - Islam | 433 (99.8%) |
| - Christian | 1 (0.2%) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Juliana, N.C.A.; Deb, S.; Ouburg, S.; Chauhan, A.; Pleijster, J.; Ali, S.M.; Morré, S.A.; Sazawal, S.; Ambrosino, E. The Prevalence of Chlamydia trachomatis and Three Other Non-Viral Sexually Transmitted Infections among Pregnant Women in Pemba Island Tanzania. Pathogens 2020, 9, 625. https://doi.org/10.3390/pathogens9080625
Juliana NCA, Deb S, Ouburg S, Chauhan A, Pleijster J, Ali SM, Morré SA, Sazawal S, Ambrosino E. The Prevalence of Chlamydia trachomatis and Three Other Non-Viral Sexually Transmitted Infections among Pregnant Women in Pemba Island Tanzania. Pathogens. 2020; 9(8):625. https://doi.org/10.3390/pathogens9080625
Chicago/Turabian StyleJuliana, Naomi C.A., Saikat Deb, Sander Ouburg, Aishwarya Chauhan, Jolein Pleijster, Said M. Ali, Servaas A. Morré, Sunil Sazawal, and Elena Ambrosino. 2020. "The Prevalence of Chlamydia trachomatis and Three Other Non-Viral Sexually Transmitted Infections among Pregnant Women in Pemba Island Tanzania" Pathogens 9, no. 8: 625. https://doi.org/10.3390/pathogens9080625
APA StyleJuliana, N. C. A., Deb, S., Ouburg, S., Chauhan, A., Pleijster, J., Ali, S. M., Morré, S. A., Sazawal, S., & Ambrosino, E. (2020). The Prevalence of Chlamydia trachomatis and Three Other Non-Viral Sexually Transmitted Infections among Pregnant Women in Pemba Island Tanzania. Pathogens, 9(8), 625. https://doi.org/10.3390/pathogens9080625







