The PK/PD Integration and Resistance of Tilmicosin against Mycoplasma hyopneumoniae
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Determination of the Minimum Inhibitory Concentration (MIC)
2.3. Time–Kill Curves
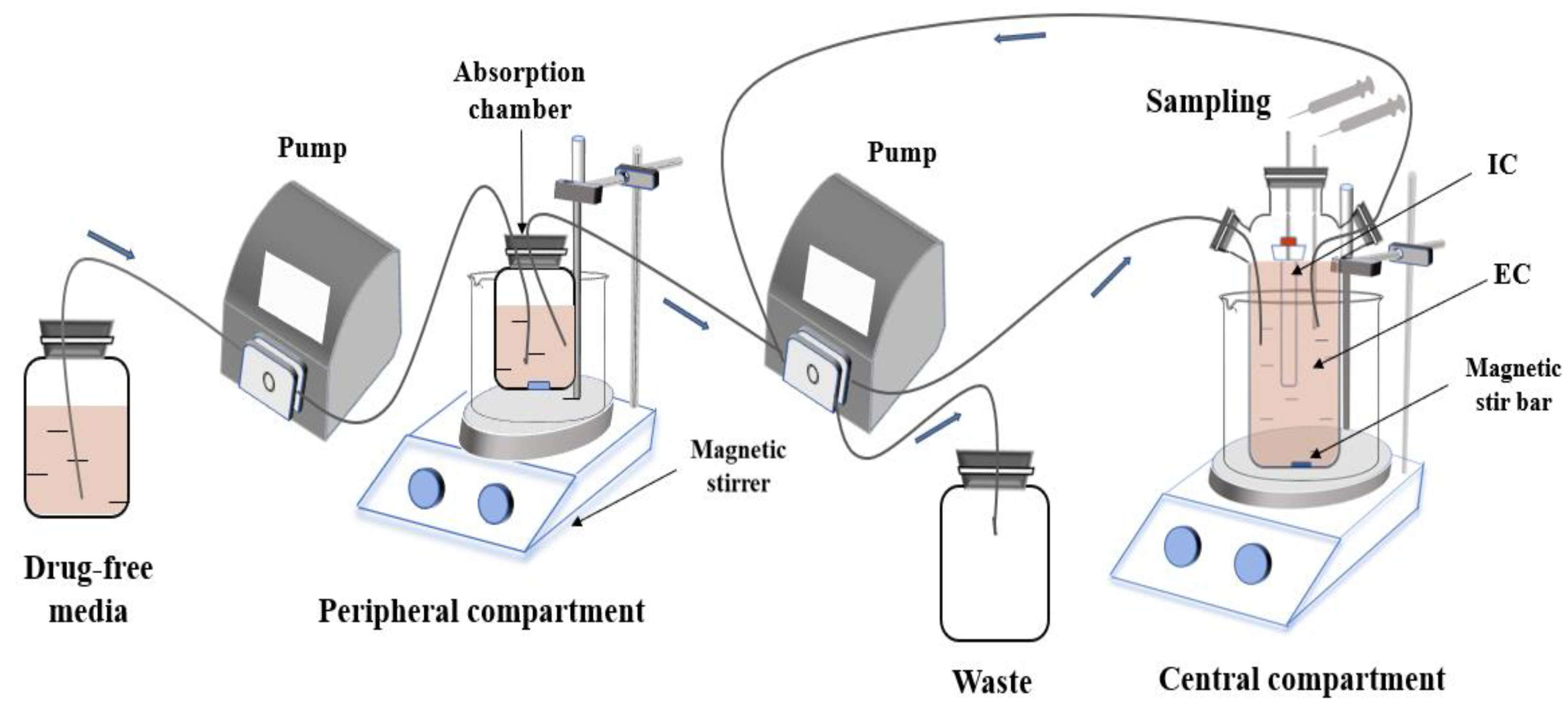
2.4. PK/PD Model In Vitro and Dosing Regimens
2.5. Determination of the Tilmicosin Concentration in the Medium
2.6. Integration and Modeling of PK/PD
2.7. Susceptibility Testing of M. hyopneumoniae and DNA Sequencing
3. Results
3.1. Susceptibility Determination
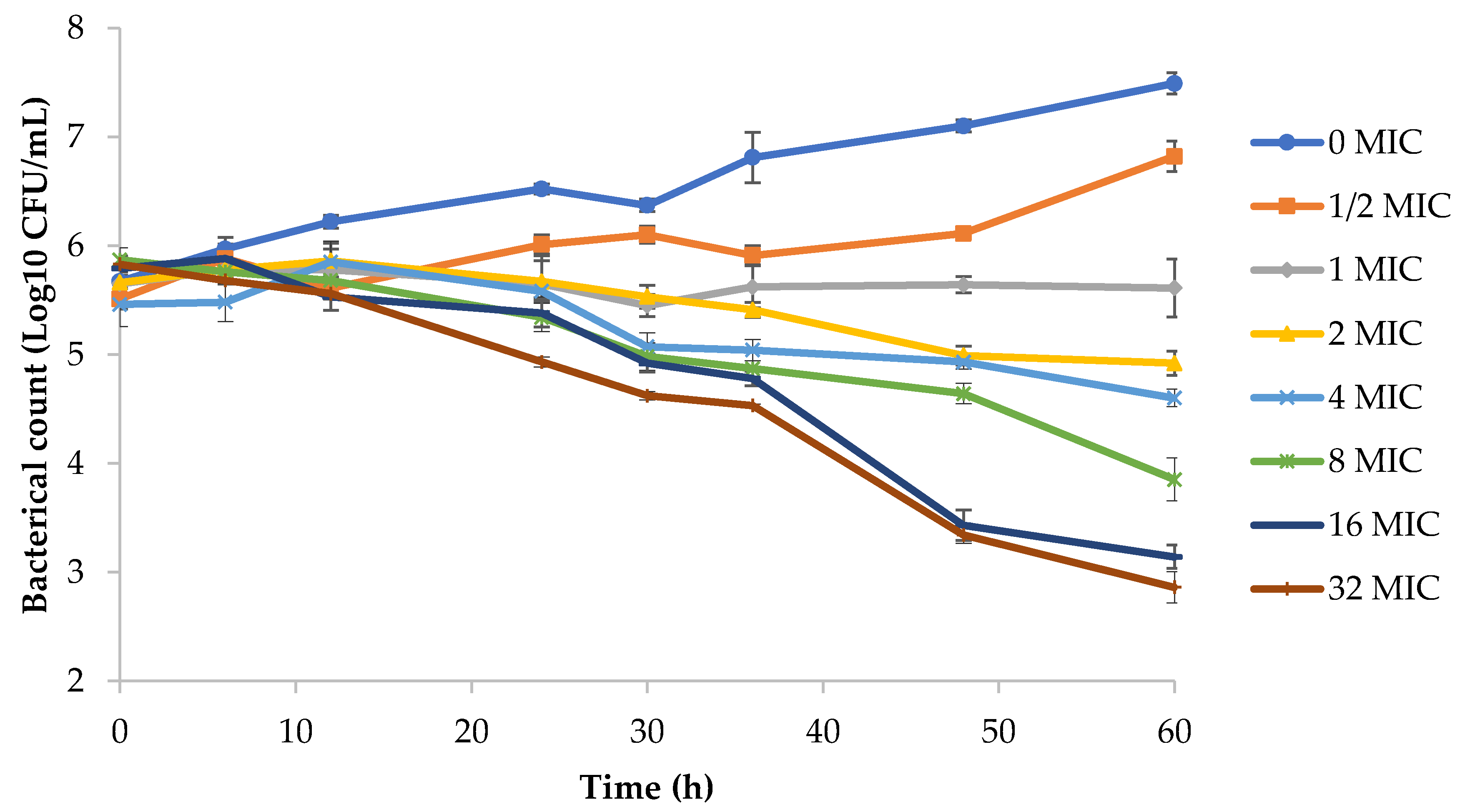
3.2. Analyses of Time–Kill Curves
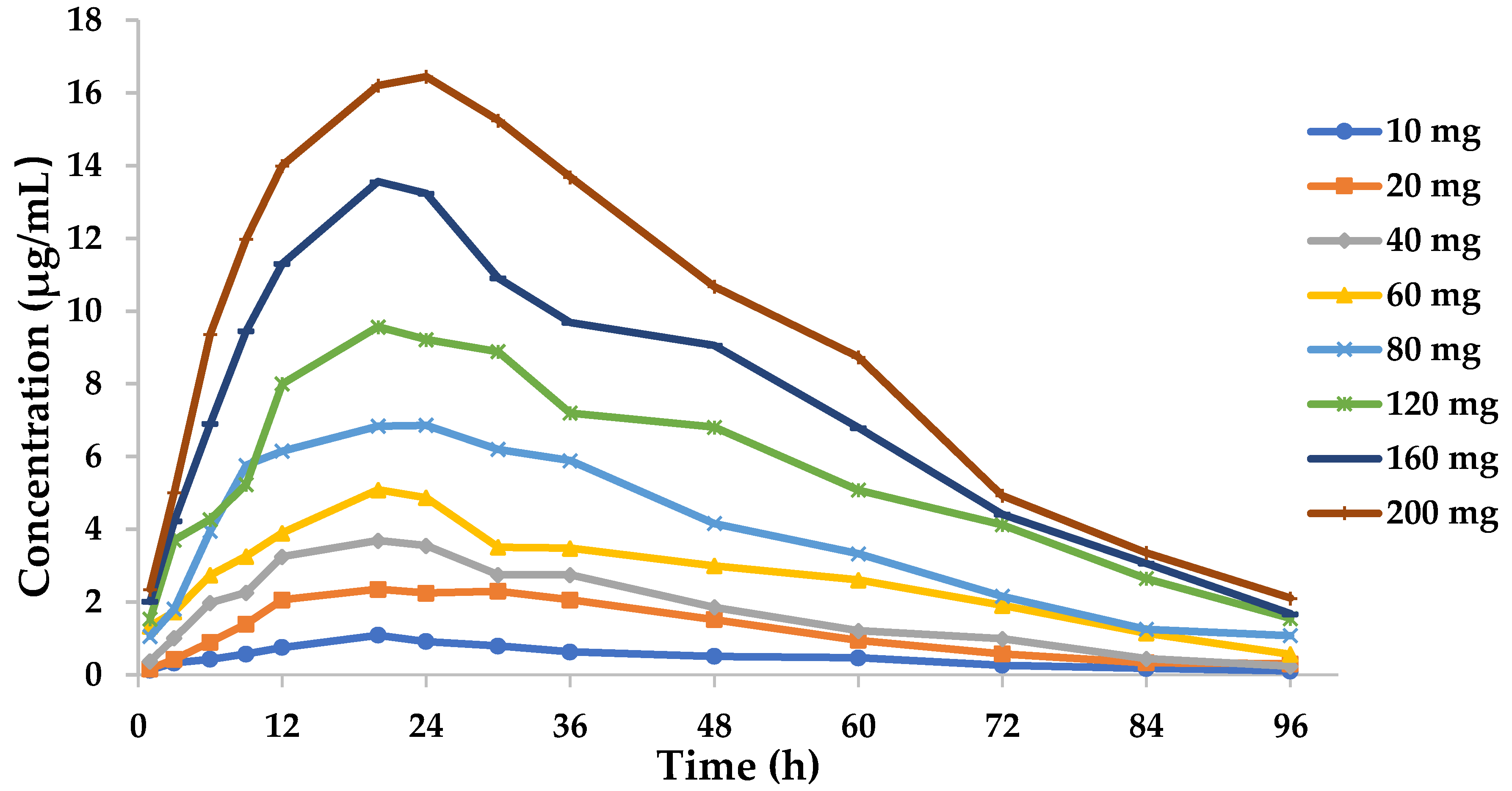
3.3. PK in the In Vitro Dynamic Model
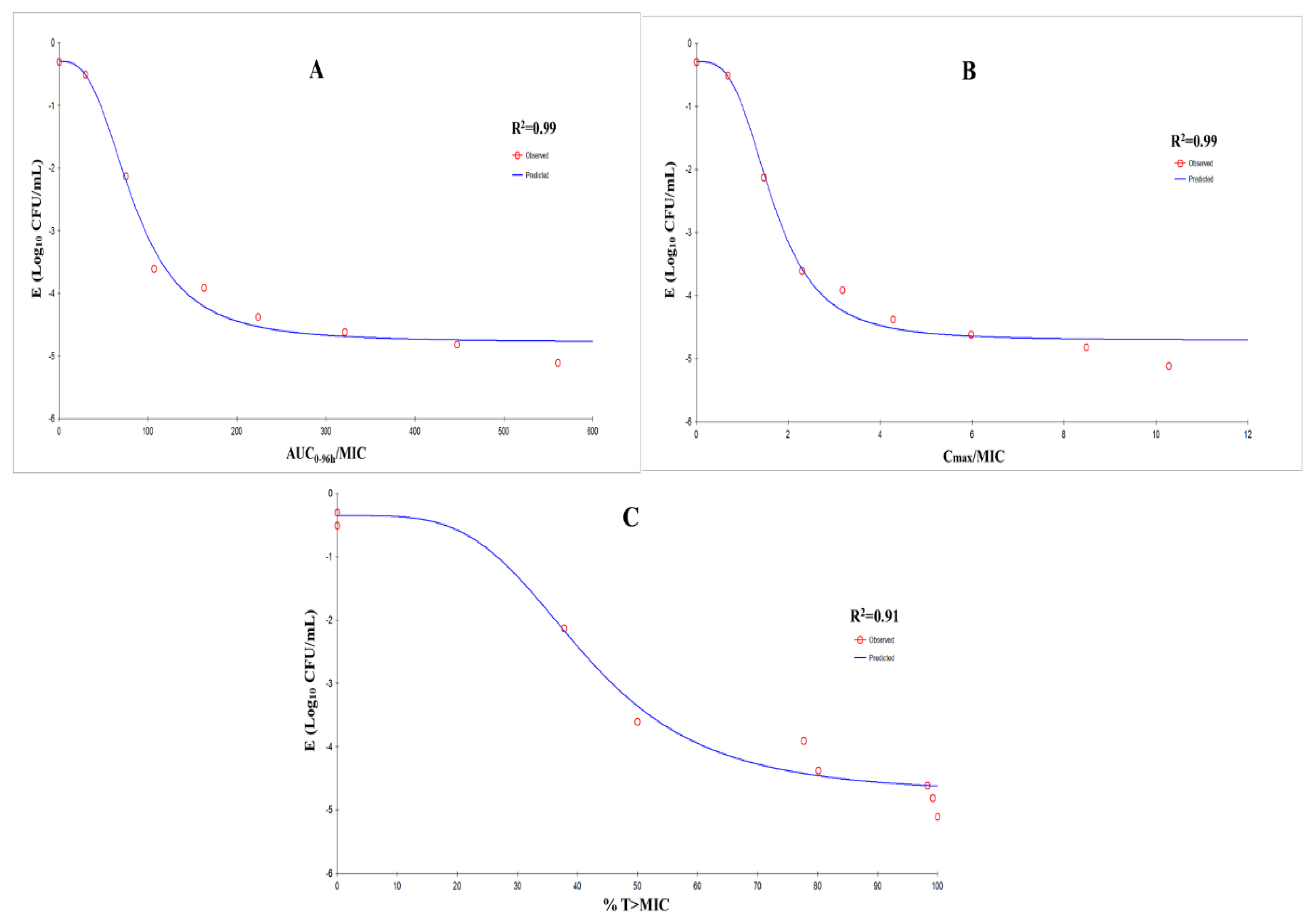
3.4. Modeling and Analyses of PK/PD
3.5. Susceptibility Testing and Mutation Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Maes, D.; Segales, J.; Meyns, T.; Sibila, M.; Pieters, M.; Haesebrouck, F. Control of Mycoplasma hyopneumoniae infections in pigs. Vet. Microbiol. 2008, 126, 297–309. [Google Scholar] [CrossRef] [PubMed]
- Otake, S.; Dee, S.; Corzo, C.; Oliveira, S.; Deen, J. Long-distance airborne transport of infectious PRRSV and Mycoplasma hyopneumoniae from a swine population infected with multiple viral variants. Vet. Microbiol. 2010, 145, 198–208. [Google Scholar] [CrossRef] [PubMed]
- Sibila, M.; Nofrarias, M.; Lopez-Soria, S.; Segales, J.; Riera, P.; Llopart, D.; Calsamiglia, M. Exploratory field study on Mycoplasma hyopneumoniae infection in suckling pigs. Vet. Microbiol. 2007, 121, 352–356. [Google Scholar] [CrossRef] [PubMed]
- Nathues, H.; Doehring, S.; Woeste, H.; Fahrion, A.S.; Doherr, M.G.; Beilage, E.G. Individual risk factors for Mycoplasma hyopneumoniae infections in suckling pigs at the age of weaning. Acta Vet. Scand. 2013, 55, 44. [Google Scholar] [CrossRef] [PubMed]
- van den Bogaard, A.E. The importance of laboratory data for a rational antimicrobial therapy in veterinary practice. Tijdschr. Diergeneeskd. 1988, 113 (Suppl. S1), 91S–92S. [Google Scholar]
- Ziv, G.; Shem-Tov, M.; Glickman, A.; Winkler, M.; Saran, A. Tilmicosin antibacterial activity and pharmacokinetics in cows. J. Vet. Pharmacol. Ther. 1995, 18, 340–345. [Google Scholar] [CrossRef]
- Shen, J.Z.; Li, C.; Jiang, H.Y.; Zhang, S.X.; Guo, P.; Ding, S.Y.; Li, X.W. Pharmacokinetics of tilmicosin after oral administration in swine. Am. J. Vet. Res. 2005, 66, 1071–1074. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Hao, H.H.; Li, J.; Ahmad, I.; Cheng, G.Y.; Chen, D.M.; Tao, Y.F.; Huang, L.L.; Wang, Y.L.; Dai, M.H.; et al. The Epidemiologic and Pharmacodynamic Cutoff Values of Tilmicosin against Haemophilus parasuis. Front. Microbiol. 2016, 7. [Google Scholar] [CrossRef]
- Stakenborg, T.; Vicca, J.; Butaye, P.; Maes, D.; Minion, F.C.; Peeters, J.; De Kruif, A.; Haesebrouck, F. Characterization of in vivo acquired resistance of Mycoplasma hyopneumoniae to macrolides and lincosamides. Microb. Drug Resist. 2005, 11, 290–294. [Google Scholar] [CrossRef]
- Qiu, G.; Rui, Y.P.; Zhang, J.L.; Zhang, L.H.; Huang, S.C.; Wu, Q.X.; Li, K.; Han, Z.Q.; Liu, S.Z.; Li, J.K. Macrolide-Resistance Selection in Tibetan Pigs with a High Load of Mycoplasma hyopneumoniae. Microb. Drug Resist. 2018, 24, 1043–1049. [Google Scholar] [CrossRef] [PubMed]
- Weisblum, B. Erythromycin resistance by ribosome modification. Antimicrob. Agents Chemother. 1995, 39, 577–585. [Google Scholar] [CrossRef] [PubMed]
- Gerchman, I. Characterization of in vivo-acquired resistance to macrolides of Mycoplasma gallisepticum strains isolated from poultry. Vet. Res. 2011, 42, 90. [Google Scholar] [CrossRef] [PubMed]
- Vester, B.; Douthwaite, S. Macrolide resistance conferred by base substitutions in 23S rRNA. Antimicrob. Agents Chemother. 2001, 45, 1. [Google Scholar] [CrossRef] [PubMed]
- Vinks, A.A.; Derendorf, H.; Mouton, J.W. Fundamentals of Antimicrobial Pharmacokinetics and Pharmacodynamics; Springer: Berlin/Heidelberg, Germany, 2014. [Google Scholar]
- Liang, W.; Chen, Y.C.; Cao, Y.R.; Liu, X.F.; Huang, J.; Hu, J.L.; Zhao, M.; Guo, Q.L.; Zhang, S.J.; Wu, X.J.; et al. Pharmacokinetics and Pharmacodynamics of Nemonoxacin against Streptococcus pneumoniae in an In Vitro Infection Model. Antimicrob. Agents Chemother. 2013, 57, 2942–2947. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Andes, D.; Craig, W.A. Pharmacodynamics of the new fluoroquinolone gatifloxacin in murine thigh and lung infection models. Antimicrob. Agents Chemother. 2002, 46, 1665–1670. [Google Scholar] [CrossRef]
- Booker, B.M.; Smith, P.F.; Forrest, A.; Bullock, J.; Kelchlin, P.; Bhavnani, S.M.; Jones, R.N.; Ambrose, P.G. Application of an in vitro infection model and simulation for reevaluation of fluoroquinolone breakpoints for Salmonella enterica serotype Typhi. Antimicrob. Agents Chemother. 2005, 49, 1775–1781. [Google Scholar] [CrossRef]
- Huang, Z.L.; Wu, Y.Z.; Zhou, Z.C.; Xia, X.R.; Gu, X.Y.; Cai, Q.R.; Shen, X.G.; Yang, H.; Ding, H.Z. Pharmacokinetic and Pharmacodynamic Integration and Resistance Analysis of Tilmicosin Against Mycoplasma gallisepticum in an In Vitro Dynamic Model. Front. Pharmacol. 2019, 10, 670. [Google Scholar] [CrossRef]
- Tanner, A.C.; Wu, C.C. Adaptation of the Sensititre broth microdilution technique to antimicrobial susceptibility testing of Mycoplasma gallisepticum. Avian Dis. 1992, 36, 714–717. [Google Scholar] [CrossRef]
- Hannan, P.C.; O’Hanlon, P.J.; Rogers, N.H. In vitro evaluation of various quinolone antibacterial agents against veterinary mycoplasmas and porcine respiratory bacterial pathogens. Res. Vet. Sci. 1989, 46, 202. [Google Scholar] [CrossRef]
- Li, Y.; Feng, B.; Gu, X.; Yang, D.; Zeng, Z.; Zhang, B.; Ding, H. Correlation of PK/PD Indices with Resistance Selection for Cefquinome againstStaphylococcus aureusin anIn VitroModel. Front. Microbiol. 2016, 7, 466. [Google Scholar]
- Marois, C.; Gottschalk, M.; Morvan, H.; Fablet, C.; Madec, F.; Kobisch, M. Experimental infection of SPF pigs with Actinobacillus pleuropneumoniae serotype 9 alone or in association with Mycoplasma hyopneumoniae. Vet. Microbiol. 2009, 135, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Beier, L.S.; Siqueira, F.M.; Schrank, I.S. Evaluation of growth and gene expression of Mycoplasma hyopneumoniae and Mycoplasma hyorhinis in defined medium. Mol. Biol. Rep. 2018, 45, 2469–2479. [Google Scholar] [CrossRef]
- Maes, D.; Sibila, M.; Kuhnert, P.; Segales, J.; Haesebrouck, F.; Pieters, M. Update on Mycoplasma hyopneumoniae infections in pigs: Knowledge gaps for improved disease control. Transbound. Emerg. Dis. 2018, 65 (Suppl. S1), 110–124. [Google Scholar] [CrossRef] [PubMed]
- Tam, V.H.; Schilling, A.N.; Vo, G.; Kabbara, S.; Kwa, A.L.; Wiederhold, N.P.; Lewis, R.E. Pharmacodynamics of polymyxin B against Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 2005, 49, 3624–3630. [Google Scholar] [CrossRef] [PubMed]
- Nan, Z.; Gu, X.; Ye, X.; Xun, W.; Zhang, B.; Zhang, L.; Shen, X.; Jiang, H.; Ding, H. The PK/PD Interactions of Doxycycline againstMycoplasma gallisepticum. Front. Microbiol. 2016, 7. [Google Scholar] [CrossRef]
- Vicca, J.; Stakenborg, T.; Maes, D.; Butaye, P.; Peeters, J.; de Kruif, A.; Haesebrouck, F. In vitro susceptibilities of Mycoplasma hyopneumoniae field isolates. Antimicrob. Agents Chemother. 2004, 48, 4470–4472. [Google Scholar] [CrossRef][Green Version]
- Felde, O.; Kreizinger, Z.; Sulyok, K.M.; Hrivnak, V.; Kiss, K.; Jerzsele, A.; Biksi, I.; Gyuranecz, M. Antibiotic susceptibility testing of Mycoplasma hyopneumoniae field isolates from Central Europe for fifteen antibiotics by microbroth dilution method. PLoS ONE 2018, 13, e0209030. [Google Scholar] [CrossRef]
- Hannan, P.C. Guidelines and recommendations for antimicrobial minimum inhibitory concentration (MIC) testing against veterinary mycoplasma species. International Research Programme on Comparative Mycoplasmology. Vet. Res. 2000, 31, 373–395. [Google Scholar] [CrossRef]
- Whithear, K.G.; Bowtell, D.D.; Ghiocas, E.; Hughes, K.L. Evaluation and use of a micro-broth dilution procedure for testing sensitivity of fermentative avian mycoplasmas to antibiotics. Avian Dis. 1983, 27, 937–949. [Google Scholar] [CrossRef]
- Drlica, K.; Zhao, X. Mutant selection window hypothesis updated. Clin. Infect. Dis. 2007, 44, 681–688. [Google Scholar] [CrossRef]
- Fran Oise, V.B.; Stéphane, C.; Cristina, S.; Hugues, C.; Donatienne, T.; Marie-Paule, M.L.; Tulkens, P.M. Cellular pharmacokinetics and pharmacodynamics of the glycopeptide antibiotic oritavancin (LY333328) in a model of J774 mouse macrophages. Antimicrob. Agents Chemother. 2004, 48, 2853. [Google Scholar]
- Carbon, C. Pharmacodynamics of macrolides, azalides, and streptogramins: Effect on extracellular pathogens. Clin. Infect. Dis. 1998, 27, 28–32. [Google Scholar] [CrossRef] [PubMed]
- Van, B.F.; Tulkens, P.M. Macrolides: Pharmacokinetics and pharmacodynamics. Int. J. Antimicrob. Agents 2001, 18, 17–23. [Google Scholar]
- Tam, V.H.; Kabbara, S.; Vo, G.; Schilling, A.N.; Coyle, E.A. Comparative pharmacodynamics of gentamicin against Staphylococcus aureus and Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 2006, 50, 2626–2631. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.F.; Peng, H.M.; Bu, M.X.; Liu, Y.H.; Sun, J.; Liao, X.P. Pharmacodynamic Evaluation and PK/PD-Based Dose Prediction of Tulathromycin: A Potential New Indication for Streptococcus suis Infection. Front. Pharmacol. 2017, 8, 684. [Google Scholar] [CrossRef]
- Zhao, Y.; Guo, L.L.; Fang, B.; Liu, B. Pharmacokinetic/pharmacodynamic (PK/PD) evaluation of tulathromycin against Haemophilus parasuis in an experimental neutropenic guinea pig model. PLoS ONE 2018, 13, e0209177. [Google Scholar] [CrossRef]
- Toutain, P.L.; Potter, T.; Pelligand, L.; Lacroix, M.; Illambas, J.; Lees, P. Standard PK/PD concepts can be applied to determine a dosage regimen for a macrolide: The case of tulathromycin in the calf. J. Vet. Pharmacol. Ther. 2017, 40, 16–27. [Google Scholar] [CrossRef]
- Zhou, Q.; Zhang, G.; Wang, Q.; Liu, W.; Huang, Y.; Yu, P.; Li, Y.; Ding, H.; Fang, B. Pharmacokinetic/Pharmacodynamic Modeling of Tulathromycin against Pasteurella multocida in a Porcine Tissue Cage Model. Front. Pharmacol. 2017, 8, 392. [Google Scholar] [CrossRef]

| Pharmacokinetic Parameter | Dose Group (mg) | Relative Deviation | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 10 | 20 | 40 | 60 | 80 | 120 | 160 | 200 | |||
| t1/2Ka (h) | 12.7 | 14.3 | 12.6 | 14.3 | 12.1 | 13.1 | 12.4 | 14.6 | 13.3 | 9.28% |
| t1/2Kel (h) | 16.5 | 14.4 | 12.7 | 15.6 | 17.8 | 19.7 | 17.7 | 14.8 | 16.2 | −5.6% |
| Tmax (h) | 20.8 | 20.7 | 18.2 | 21.6 | 21.9 | 23.1 | 21.3 | 21.2 | 21.1 | 1.3% |
| Cmax (μg/mL) | 1.09 | 2.35 | 3.69 | 5.09 | 6.86 | 9.57 | 13.6 | 16.5 | —— | —— |
| AUC (h.mg/L) | 47.2 | 119.6 | 190.4 | 260.5 | 357.9 | 513.9 | 715.4 | 896.6 | —— | —— |
| R2 | 0.963 | 0.986 | 0.939 | 0.963 | 0.918 | 0.975 | 0.988 | 0.997 | —— | —— |
| PK/PD Parameter | Emax (log10 CFU/mL) | EC50 | E0 (log10 CFU/mL) | Hill’s Slope | R2 |
|---|---|---|---|---|---|
| AUC0–96 h/MIC (h) | −0.30 | 91.93 | −5.28 | 1.65 | 0.99 |
| Cmax/MIC | −0.30 | 1.80 | −5.17 | 1.89 | 0.99 |
| Strain | MIC Value of Antibiotics (μg/mL) | |||||||
|---|---|---|---|---|---|---|---|---|
| Tilmicosin | Tylosin | Erythromycin | Tiamulin | Doxycyclin | Enrofloxacin | Amikacin | Lincomycin | |
| Mhp | 1.6 | 0.0625 | 0.64 | 0.08 | 0.0625 | 0.025 | 1.6 | 0.125 |
| M1 | 25.6 | 0.125 | >40.96 | 0.08 | 0.0625 | 0.025 | 1.6 | 0.125 |
| M2 | 819.2 | 8 | >40.96 | 0.08 | 0.0625 | 0.025 | 1.6 | 64 |
| M3 | 1638.4 | 16 | >40.96 | 0.08 | 0.0625 | 0.025 | 1.6 | 256 |
| M4 | 1638.4 | 16 | >40.96 | 0.16 | 0.0625 | 0.025 | 1.6 | 256 |
| Dose (mg) | Strain | MIC (μg/mL) | 23S rRNA | ||
|---|---|---|---|---|---|
| V Region | L4 | L22 | |||
| 0 | Mhp | 1.6 | —— | —— | —— |
| 80 | M3 | 819.2 | A2058G | —— | —— |
| 120 | M4 | 819.2 | A2058G | —— | —— |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, Z.; Hu, Z.; Zheng, H.; Xia, X.; Gu, X.; Shen, X.; Yang, H.; Ding, H. The PK/PD Integration and Resistance of Tilmicosin against Mycoplasma hyopneumoniae. Pathogens 2020, 9, 487. https://doi.org/10.3390/pathogens9060487
Huang Z, Hu Z, Zheng H, Xia X, Gu X, Shen X, Yang H, Ding H. The PK/PD Integration and Resistance of Tilmicosin against Mycoplasma hyopneumoniae. Pathogens. 2020; 9(6):487. https://doi.org/10.3390/pathogens9060487
Chicago/Turabian StyleHuang, Zilong, Zixuan Hu, Haorui Zheng, Xirui Xia, Xiaoyan Gu, Xiangguang Shen, Hong Yang, and Huanzhong Ding. 2020. "The PK/PD Integration and Resistance of Tilmicosin against Mycoplasma hyopneumoniae" Pathogens 9, no. 6: 487. https://doi.org/10.3390/pathogens9060487
APA StyleHuang, Z., Hu, Z., Zheng, H., Xia, X., Gu, X., Shen, X., Yang, H., & Ding, H. (2020). The PK/PD Integration and Resistance of Tilmicosin against Mycoplasma hyopneumoniae. Pathogens, 9(6), 487. https://doi.org/10.3390/pathogens9060487




