Rapid and Sensitive Multiplex Assay for the Detection of B. anthracis Spores from Environmental Samples
Abstract
1. Introduction
2. Results
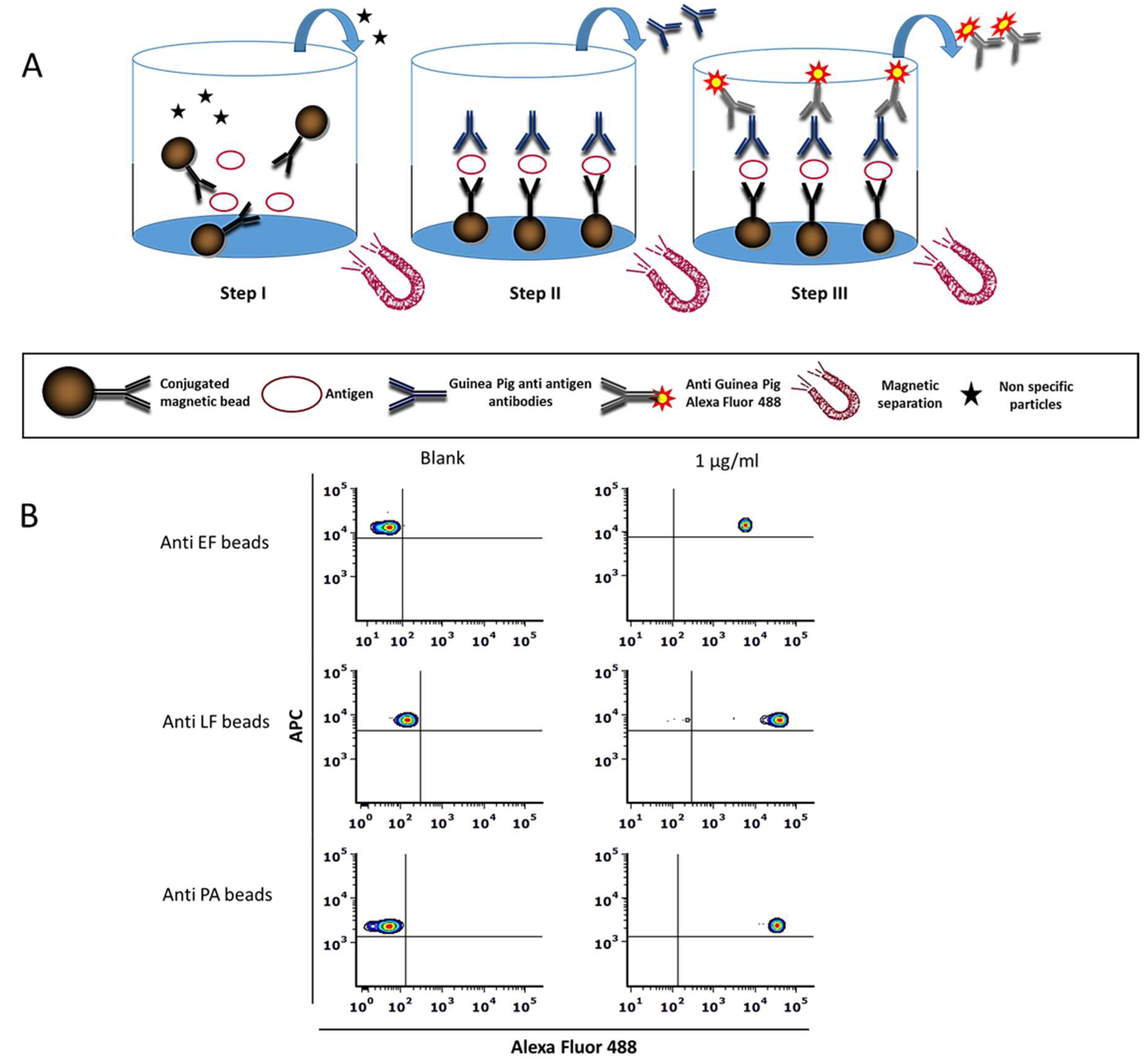
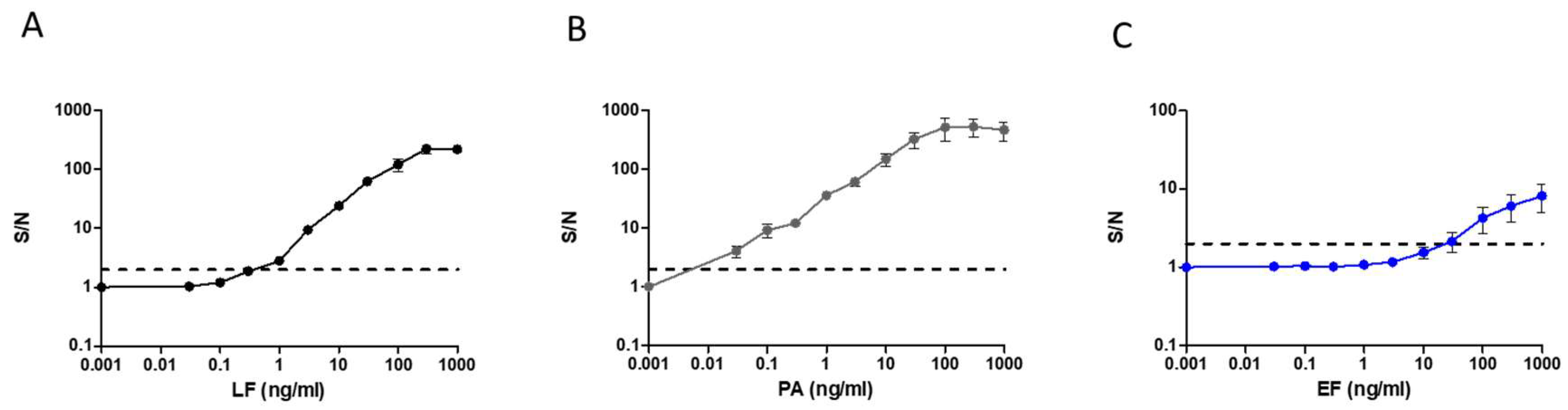
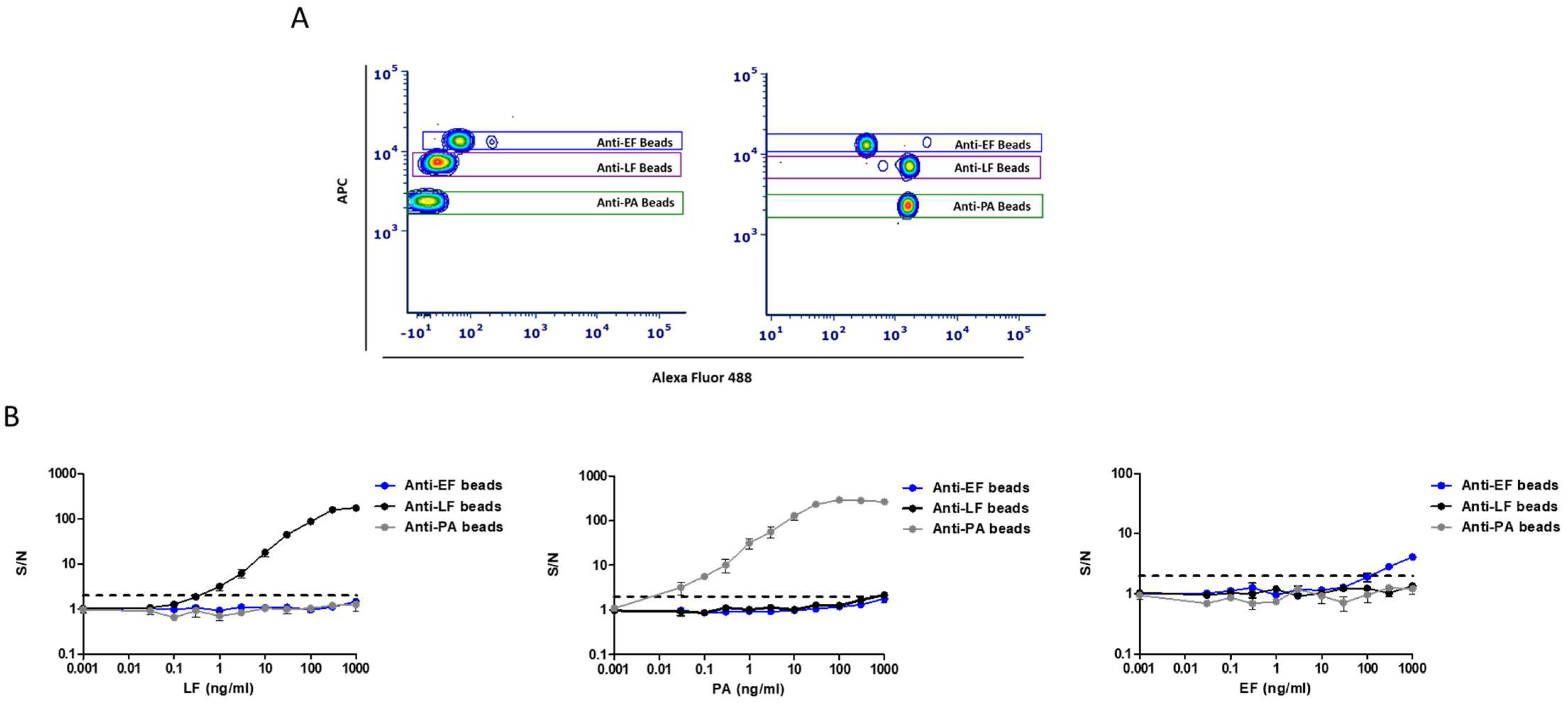
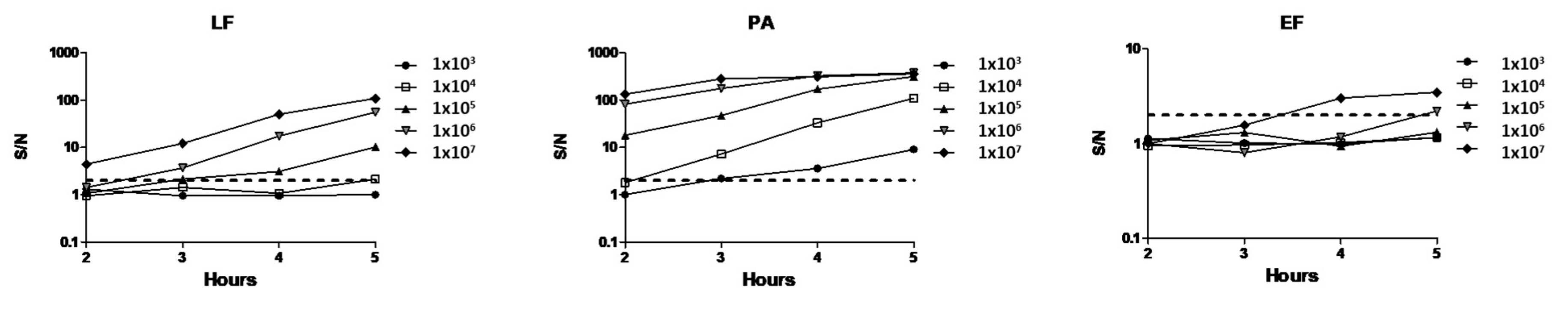
2.1. Development of a Magnetic Bead Immunoassay Based Flow Cytometry Method for the Detection of Anthrax Virulence Factors
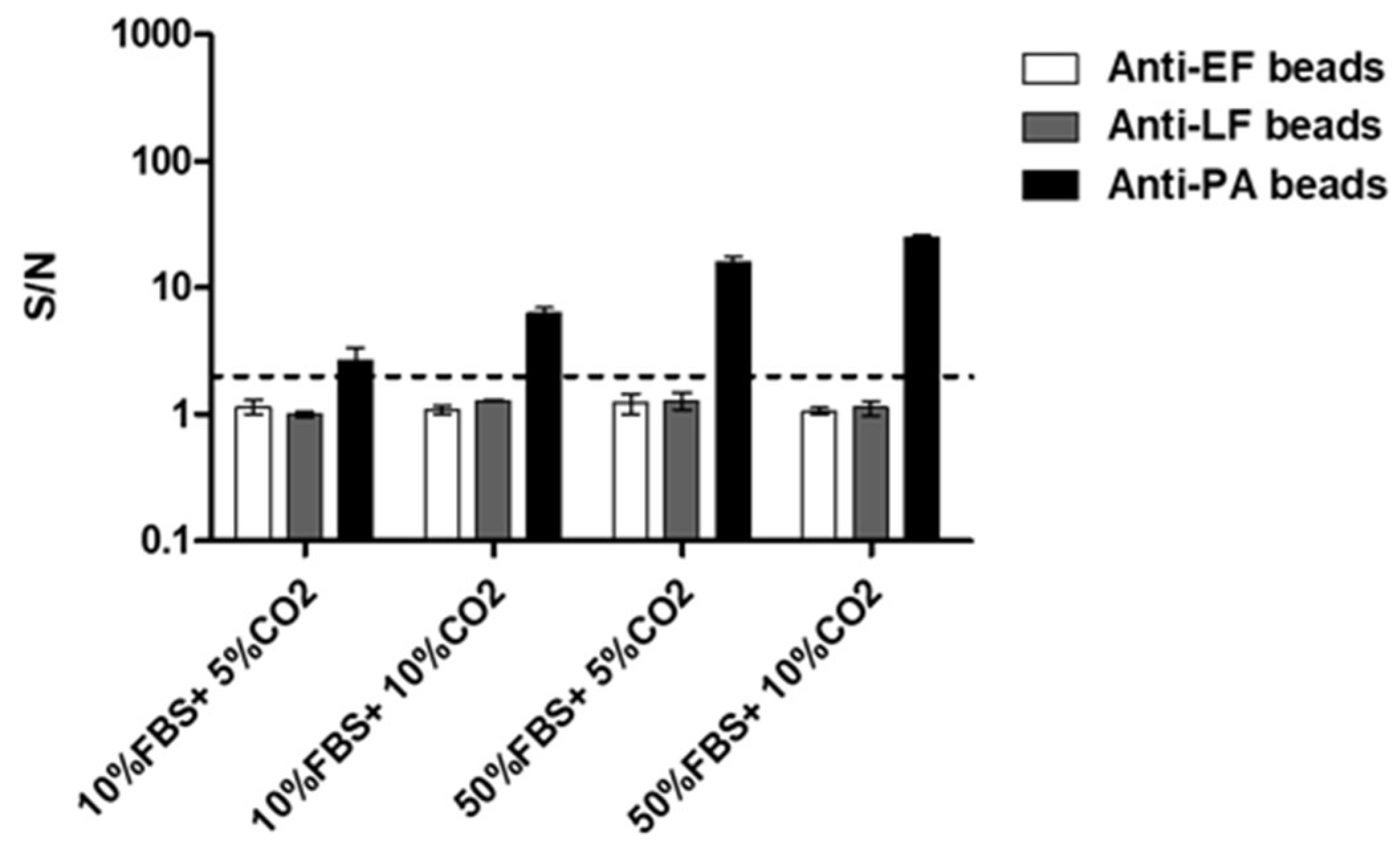
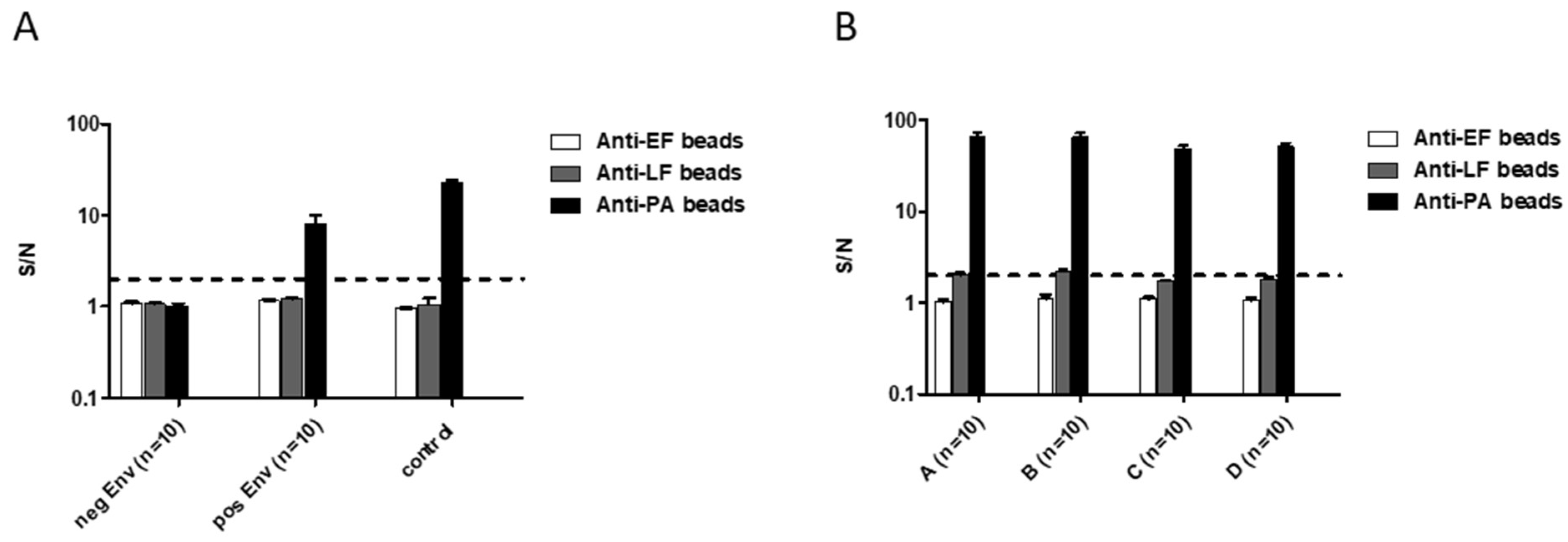
2.2. Applying the New Multiplex Assay for B. anthracis Spore Detection
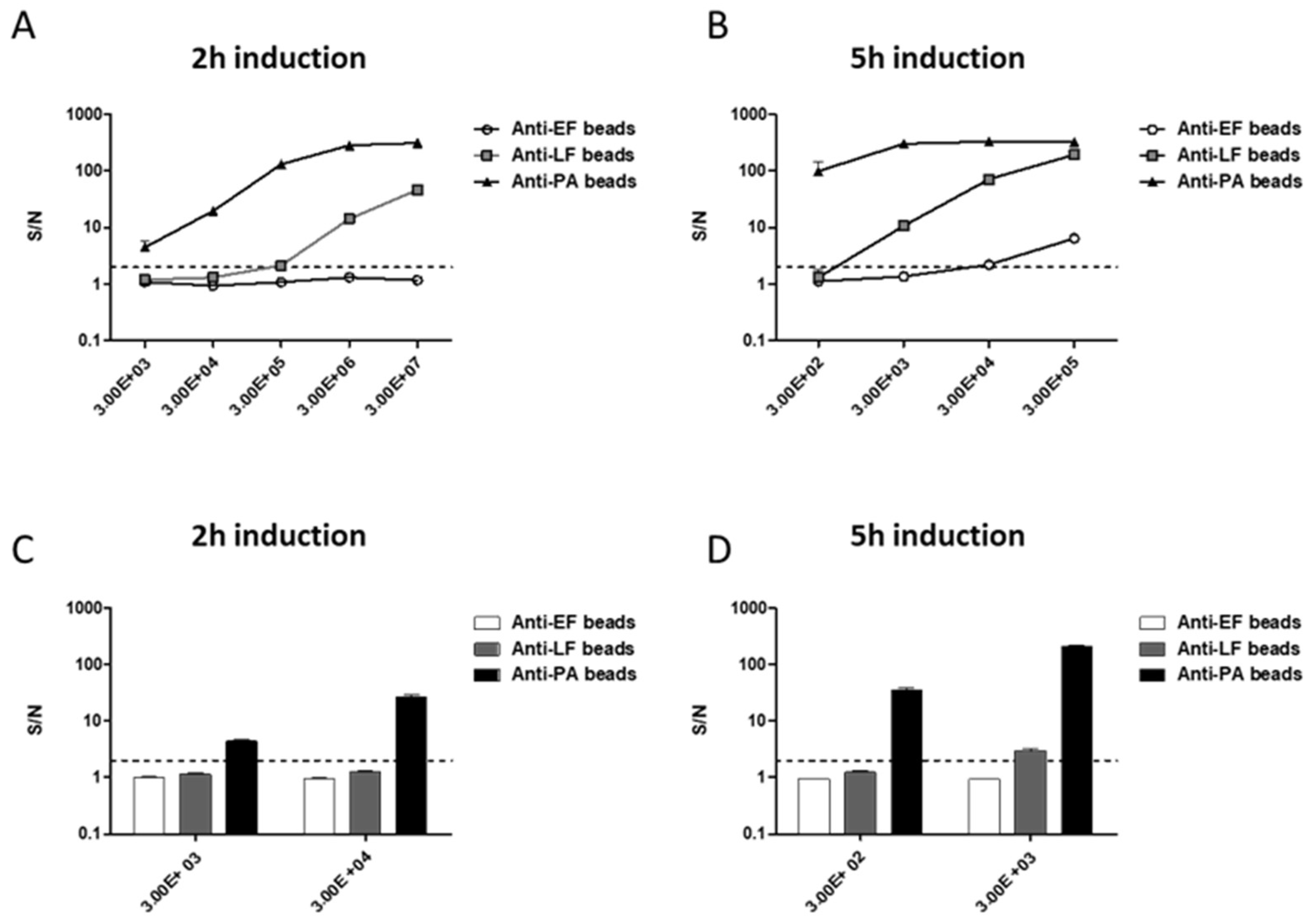
2.3. Assay Validation Using Fully Virulent B. anthracis Vollum Strain Spores
3. Discussion
4. Materials and Methods
4.1. B. anthracis Strains
4.2. Antibodies and Proteins
4.3. Preparation of Coupled Magnetic Beads
4.4. Magnetic Bead Based Detection Assays
4.5. Environmental Sample Collection, Preparation, and Toxin Biosynthesis Process
4.6. Signal Analysis
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Dixon, T.C.; Meselson, M.; Guillemin, J.; Hanna, P.C. Anthrax. N. Engl. J. Med. 1999, 341, 815–826. [Google Scholar] [CrossRef] [PubMed]
- WHO. Anthrax in Humans and Animals; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Tier1. Available online: www.selectagents.gov/ohp-app1.html (accessed on 2 December 2019).
- Brachman, P.C. Inhalation Anthrax. Ann. N. Y. Acad. Sci. 1980, 353, 11. [Google Scholar] [CrossRef] [PubMed]
- Jernigan, D.B.; Raghunathan, P.L.; Bell, B.P.; Brechner, R.; Bresnitz, E.A.; Butler, J.C.; Cetron, M.; Cohen, M.; Doyle, T.; Fischer, M.; et al. Investigation of bioterrorism-related anthrax, United States, 2001: Epidemiologic findings. Emerg. Infect. Dis. 2002, 8, 1019–1028. [Google Scholar] [CrossRef] [PubMed]
- LRN. Available online: https://www.asm.org/Articles/Policiy/Laboratory-Response-Network-LRN-Sentinel-Level-C (accessed on 3 December 2019).
- Israeli, O.; Cohen-Gihon, I.; Zvi, A.; Lazar, S.; Shifman, O.; Levy, H.; Tidhar, A.; Beth-Din, A. Rapid identification of unknown pathogens in environmental samples using a high-throughput sequencing-based approach. Heliyon 2019, 5, e01793. [Google Scholar] [CrossRef]
- Ryu, C.; Lee, K.; Yoo, C.; Seong, W.K.; Oh, H.B. Sensitive and rapid quantitative detection of anthrax spores isolated from soil samples by real-time PCR. Microbiol. Immunol. 2003, 47, 693–699. [Google Scholar] [CrossRef]
- Be, N.A.; Thissen, J.B.; Gardner, S.N.; McLoughlin, K.S.; Fofanov, V.Y.; Koshinsky, H.; Ellingson, S.R.; Brettin, T.S.; Jackson, P.J.; Jaing, C.J. Detection of Bacillus anthracis DNA in complex soil and air samples using next-generation sequencing. PLoS ONE 2013, 8, e73455. [Google Scholar] [CrossRef]
- Irenge, L.M.; Gala, J.L. Rapid detection methods for Bacillus anthracis in environmental samples: A review. Appl. Microbiol. Biotechnol. 2012, 93, 1411–1422. [Google Scholar] [CrossRef]
- King, D.; Luna, V.; Cannons, A.; Cattani, J.; Amuso, P. Performance assessment of three commercial assays for direct detection of Bacillus anthracis spores. J. Clin. Microbiol. 2003, 41, 3454–3455. [Google Scholar] [CrossRef]
- Whitman, W.B.; Coleman, D.C.; Wiebe, W.J. Prokaryotes: The unseen majority. Proc. Natl. Acad. Sci. USA 1998, 95, 6578–6583. [Google Scholar] [CrossRef]
- Dang, J.L.; Heroux, K.; Kearney, J.; Arasteh, A.; Gostomski, M.; Emanuel, P.A. Bacillus spore inactivation methods affect detection assays. Appl. Environ. Microbiol. 2001, 67, 3665–3670. [Google Scholar] [CrossRef]
- Zahavy, E.; Fisher, M.; Bromberg, A.; Olshevsky, U. Detection of frequency resonance energy transfer pair on double-labeled microsphere and Bacillus anthracis spores by flow cytometry. Appl. Environ. Microbiol. 2003, 69, 2330–2339. [Google Scholar] [CrossRef] [PubMed]
- Hang, J.; Sundaram, A.K.; Zhu, P.; Shelton, D.R.; Karns, J.S.; Martin, P.A.; Li, S.; Amstutz, P.; Tang, C.M. Development of a rapid and sensitive immunoassay for detection and subsequent recovery of Bacillus anthracis spores in environmental samples. J. Microbiol. Methods 2008, 73, 242–246. [Google Scholar] [CrossRef] [PubMed]
- Tamborrini, M.; Holzer, M.; Seeberger, P.H.; Schurch, N.; Pluschke, G. Anthrax spore detection by a luminex assay based on monoclonal antibodies that recognize anthrose-containing oligosaccharides. Clin. Vaccine Immunol. 2010, 17, 1446–1451. [Google Scholar] [CrossRef] [PubMed]
- Yu, H. Comparative studies of magnetic particle-based solid phase fluorogenic and electrochemiluminescent immunoassay. J. Immunol. Methods 1998, 218, 1–8. [Google Scholar] [CrossRef]
- Kuehn, A.; Kovac, P.; Saksena, R.; Bannert, N.; Klee, S.R.; Ranisch, H.; Grunow, R. Development of antibodies against anthrose tetrasaccharide for specific detection of Bacillus anthracis spores. Clin. Vaccine Immunol. 2009, 16, 1728–1737. [Google Scholar] [CrossRef]
- Sastry, K.S.; Tuteja, U.; Santhosh, P.K.; Lalitha, M.K.; Batra, H.V. Identification of Bacillus anthracis by a simple protective antigen-specific mAb dot-ELISA. J. Med. Microbiol. 2003, 52, 47–49. [Google Scholar] [CrossRef][Green Version]
- Cheun, H.I.; Makino, S.I.; Watarai, M.; Erdenebaatar, J.; Kawamoto, K.; Uchida, I. Rapid and effective detection of anthrax spores in soil by PCR. J. Appl. Microbiol. 2003, 95, 728–733. [Google Scholar] [CrossRef]
- Letant, S.E.; Kane, S.R.; Murphy, G.A.; Alfaro, T.M.; Hodges, L.R.; Rose, L.J.; Raber, E. Most-probable-number rapid viability PCR method to detect viable spores of Bacillus anthracis in swab samples. J. Microbiol. Methods 2010, 81, 200–202. [Google Scholar] [CrossRef][Green Version]
- Kane, S.R.; Letant, S.E.; Murphy, G.A.; Alfaro, T.M.; Krauter, P.W.; Mahnke, R.; Legler, T.C.; Raber, E. Rapid, high-throughput, culture-based PCR methods to analyze samples for viable spores of Bacillus anthracis and its surrogates. J. Microbiol. Methods 2009, 76, 278–284. [Google Scholar] [CrossRef]
- Kobiler, D.; Weiss, S.; Levy, H.; Fisher, M.; Mechaly, A.; Pass, A.; Altboum, Z. Protective antigen as a correlative marker for anthrax in animal models. Infect. Immun. 2006, 74, 5871–5876. [Google Scholar] [CrossRef]
- Cote, C.K.; Rossi, C.A.; Kang, A.S.; Morrow, P.R.; Lee, J.S.; Welkos, S.L. The detection of protective antigen (PA) associated with spores of Bacillus anthracis and the effects of anti-PA antibodies on spore germination and macrophage interactions. Microb. Pathog. 2005, 38, 209–225. [Google Scholar] [CrossRef] [PubMed]
- Levy, H.; Glinert, I.; Weiss, S.; Sittner, A.; Schlomovitz, J.; Altboum, Z.; Kobiler, D. Toxin-independent virulence of Bacillus anthracis in rabbits. PLoS ONE 2014, 9, e84947. [Google Scholar] [CrossRef] [PubMed]
- Glinert, I.; Bar-David, E.; Sittner, A.; Weiss, S.; Schlomovitz, J.; Ben-Shmuel, A.; Mechaly, A.; Altboum, Z.; Kobiler, D.; Levy, H. Revisiting the Concept of Targeting Only Bacillus anthracis Toxins as a Treatment for Anthrax. Antimicrob. Agents Chemother. 2016, 60, 4878–4885. [Google Scholar] [CrossRef] [PubMed]
- Levy, H.; Weiss, S.; Altboum, Z.; Schlomovitz, J.; Glinert, I.; Sittner, A.; Shafferman, A.; Kobiler, D. Differential contribution of Bacillus anthracis toxins to pathogenicity in two animal models. Infect. Immun. 2012, 80, 2623–2631. [Google Scholar] [CrossRef]
- Levy, H.; Glinert, I.; Weiss, S.; Bar-David, E.; Sittner, A.; Schlomovitz, J.; Altboum, Z.; Kobiler, D. The central nervous system as target of Bacillus anthracis toxin independent virulence in rabbits and guinea pigs. PLoS ONE 2014, 9, e112319. [Google Scholar] [CrossRef]
- Cohen-Gihon, I.; Israeli, O.; Beth-Din, A.; Levy, H.; Cohen, O.; Shafferman, A.; Zvi, A.; Chitlaru, T. Whole-Genome Sequencing of the Nonproteolytic Bacillus anthracis V770-NP1-R Strain Reveals Multiple Mutations in Peptidase Loci. Genome. Announc. 2014, 2. [Google Scholar] [CrossRef]
- Helgason, E.; Okstad, O.A.; Caugant, D.A.; Johansen, H.A.; Fouet, A.; Mock, M.; Hegna, I.; Kolsto, A.B. Bacillus anthracis, Bacillus cereus, and Bacillus thuringiensis—One species on the basis of genetic evidence. Appl. Environ. Microbiol. 2000, 66, 2627–2630. [Google Scholar] [CrossRef]
- Ash, C.; Farrow, J.A.; Dorsch, M.; Stackebrandt, E.; Collins, M.D. Comparative analysis of Bacillus anthracis, Bacillus cereus, and related species on the basis of reverse transcriptase sequencing of 16S rRNA. Int. J. Syst. Bacteriol. 1991, 41, 343–346. [Google Scholar] [CrossRef]
- Brezillon, C.; Haustant, M.; Dupke, S.; Corre, J.P.; Lander, A.; Franz, T.; Monot, M.; Couture-Tosi, E.; Jouvion, G.; Leendertz, F.H.; et al. Capsules, toxins and AtxA as virulence factors of emerging Bacillus cereus biovar anthracis. PLoS Negl. Trop. Dis. 2015, 9, e0003455. [Google Scholar] [CrossRef]
- Tengelsen, L.; Hudson, R.; Barnes, S.; Hahn, C. Coordinated response to reports of possible anthrax contamination, Idaho, 2001. Emerg. Infect. Dis. 2002, 8, 1093–1095. [Google Scholar] [CrossRef]
- Lim, D.V.; Simpson, J.M.; Kearns, E.A.; Kramer, M.F. Current and developing technologies for monitoring agents of bioterrorism and biowarfare. Clin. Microbiol. Rev. 2005, 18, 583–607. [Google Scholar] [CrossRef] [PubMed]
- Sharp, N.J.; Molineux, I.J.; Page, M.A.; Schofield, D.A. Rapid Detection of Viable Bacillus anthracis Spores in Environmental Samples by Using Engineered Reporter Phages. Appl. Environ. Microbiol. 2016, 82, 2380–2387. [Google Scholar] [CrossRef] [PubMed]
- Ramage, J.G.; Prentice, K.W.; DePalma, L.; Venkateswaran, K.S.; Chivukula, S.; Chapman, C.; Bell, M.; Datta, S.; Singh, A.; Hoffmaster, A.; et al. Comprehensive Laboratory Evaluation of a Highly Specific Lateral Flow Assay for the Presumptive Identification of Bacillus anthracis Spores in Suspicious White Powders and Environmental Samples. Health Secur. 2016, 14, 351–365. [Google Scholar] [CrossRef]
- Tamborrini, M.; Oberli, M.A.; Werz, D.B.; Schurch, N.; Frey, J.; Seeberger, P.H.; Pluschke, G. Immuno-detection of anthrose containing tetrasaccharide in the exosporium of Bacillus anthracis and Bacillus cereus strains. J. Appl. Microbiol. 2009, 106, 1618–1628. [Google Scholar] [CrossRef] [PubMed]
- Vignali, D.A. Multiplexed particle-based flow cytometric assays. J. Immunol. Methods 2000, 243, 243–255. [Google Scholar] [CrossRef]
- Mechaly, A.; Vitner, E.; Levy, H.; Weiss, S.; Bar-David, E.; Gur, D.; Koren, M.; Cohen, H.; Cohen, O.; Mamroud, E.; et al. Simultaneous Immunodetection of Anthrax, Plague, and Tularemia from Blood Cultures by Use of Multiplexed Suspension Arrays. J. Clin. Microbiol. 2018, 56. [Google Scholar] [CrossRef]
- Rosenfeld, R.; Marcus, H.; Ben-Arie, E.; Lachmi, B.E.; Mechaly, A.; Reuveny, S.; Gat, O.; Mazor, O.; Ordentlich, A. Isolation and chimerization of a highly neutralizing antibody conferring passive protection against lethal Bacillus anthracis infection. PLoS ONE 2009, 4, e6351. [Google Scholar] [CrossRef]
- Reuveny, S.; White, M.D.; Adar, Y.Y.; Kafri, Y.; Altboum, Z.; Gozes, Y.; Kobiler, D.; Shafferman, A.; Velan, B. Search for correlates of protective immunity conferred by anthrax vaccine. Infect. Immun. 2001, 69, 2888–2893. [Google Scholar] [CrossRef]
- ICH. ICH Harmonised Tripartite Guideline. Validation of Analytical Procedures: Text and Methodology; ICH: Geneva, Switzerland, November 1996. [Google Scholar]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Makdasi, E.; Laskar, O.; Glinert, I.; Alcalay, R.; Mechaly, A.; Levy, H. Rapid and Sensitive Multiplex Assay for the Detection of B. anthracis Spores from Environmental Samples. Pathogens 2020, 9, 164. https://doi.org/10.3390/pathogens9030164
Makdasi E, Laskar O, Glinert I, Alcalay R, Mechaly A, Levy H. Rapid and Sensitive Multiplex Assay for the Detection of B. anthracis Spores from Environmental Samples. Pathogens. 2020; 9(3):164. https://doi.org/10.3390/pathogens9030164
Chicago/Turabian StyleMakdasi, Efi, Orly Laskar, Itai Glinert, Ron Alcalay, Adva Mechaly, and Haim Levy. 2020. "Rapid and Sensitive Multiplex Assay for the Detection of B. anthracis Spores from Environmental Samples" Pathogens 9, no. 3: 164. https://doi.org/10.3390/pathogens9030164
APA StyleMakdasi, E., Laskar, O., Glinert, I., Alcalay, R., Mechaly, A., & Levy, H. (2020). Rapid and Sensitive Multiplex Assay for the Detection of B. anthracis Spores from Environmental Samples. Pathogens, 9(3), 164. https://doi.org/10.3390/pathogens9030164




