COVID-19 Transmission Potential and Non-Pharmaceutical Interventions in Maine During the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources
2.2. Unit of Analysis
2.3. Data Cleaning and Deconvolution
2.4. Rt Estimation
2.5. Statistical Software
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CARES | Coronavirus Aid, Relief, and Economic Security |
| CDC | Centers for Disease Control and Prevention |
| COVID-19 | Coronavirus Disease 2019 |
| CSSE | Center for Systems Science and Engineering |
| CrI | Credible Interval |
| DACF | Department of Agriculture, Conservation, and Forestry |
| DHHS | Department of Health and Human Services |
| DOF | Degree of Freedom |
| MEMA | Maine Emergency Management Agency |
| NPI | Non-Pharmaceutical Intervention |
| OPTIONS | Overdose Prevention Through Intensive Outreach, Naloxone, and Safety |
| PPE | Personal Protective Equipment |
| Rt | Time-Varying Reproduction Number |
| SARS-CoV-2 | Severe Acute Respiratory Syndrome Coronavirus 2 |
| SD | Standard Deviation |
| VRBO | Vacation Rentals by Owner |
References
- Acter, T.; Uddin, N.; Das, J.; Akhter, A.; Choudhury, T.R.; Kim, S. Evolution of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) as coronavirus disease 2019 (COVID-19) pandemic: A global health emergency. Sci. Total Environ. 2020, 730, 138996. [Google Scholar] [CrossRef]
- Bialek, S.; Bowen, V.; Chow, N.; Curns, A.; Gierke, R.; Hall, A.; Hughes, M.; Pilishvili, T.; Ritchey, M.; Roguski, K.; et al. Geographic Differences in COVID-19 Cases, Deaths, and Incidence—United States, February 12–April 7, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 465–471. [Google Scholar] [CrossRef]
- Johns Hopkins University Coronavirus Resource Center. COVID-19 United States Cases by County. Available online: https://coronavirus.jhu.edu/us-map (accessed on 25 May 2025).
- Maine Center for Disease Control and Prevention. Define Rural Health and Primary Care. Available online: https://web.archive.org/web/20241218093039/https://www.maine.gov/dhhs/mecdc/public-health-systems/rhpc/rural-health.shtml (accessed on 1 January 2025).
- U.S. Census Bureau. QuickFacts: Maine. Available online: https://web.archive.org/web/20240615070406/https://www.census.gov/quickfacts/ME (accessed on 1 January 2025).
- Letourneau, L.M.; Korsen, N.; Osgood, J.; Swartz, S. Rural communities improving quality through collaboration: The MaineHealth story. J. Healthc. Qual. 2006, 28, 15–27. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.W.S.; Li, Y. Spreading of COVID-19: Density matters. PLoS ONE 2020, 15, e0242398. [Google Scholar] [CrossRef]
- State of Maine Department of Health and Human Services. Transforming Rural Health. Available online: https://www.maine.gov/dhhs/initiatives/transforming-rural-health (accessed on 1 January 2025).
- U.S. Census Bureau. New Estimates Highlight Differences in Growth Between the U.S. Hispanic and Non-Hispanic Populations. Available online: https://www.census.gov/newsroom/press-releases/2024/population-estimates-characteristics.html (accessed on 1 January 2025).
- Singhal, S.; Kumar, P.; Singh, S.; Saha, S.; Dey, A.B. Clinical features and outcomes of COVID-19 in older adults: A systematic review and meta-analysis. BMC Geriatr. 2021, 21, 321. [Google Scholar] [CrossRef]
- Maine Center for Disease Control and Prevention. Public Health Districts. Available online: https://www.maine.gov/dhhs/mecdc/public-health-systems/lphd/index.shtml (accessed on 1 January 2025).
- State of Maine Department of Health and Human Services. DHHS Has Historic Opportunity to Address COVID-19 Health Disparities with $32 Million in Federal Funding. Available online: https://www.maine.gov/dhhs/blog/dhhs-has-historic-opportunity-address-covid-19-health-disparities-32-million-federal-funding-2021-11-04 (accessed on 1 January 2025).
- State of Maine Department of Health and Human Services. DHHS Progress on Addressing Health Disparities in Maine. Available online: https://www.maine.gov/dhhs/blog/dhhs-progress-addressing-health-disparities-maine-2023-05-31 (accessed on 1 January 2025).
- Cowling, B.J.; Ali, S.T.; Ng, T.W.Y.; Tsang, T.K.; Li, J.C.M.; Fong, M.W.; Liao, Q.; Kwan, M.Y.W.; Lee, S.L.; Chiu, S.S.; et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: An observational study. Lancet Public Health 2020, 5, e279–e288. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Wang, W.; Wong, W.K.; Zhu, W. Effectiveness of non-pharmaceutical interventions for COVID-19 in USA. Sci. Rep. 2024, 14, 21387. [Google Scholar] [CrossRef] [PubMed]
- Nagata, S.; Takahashi, Y.; Adachi, H.M.; Johnson, G.D.; Nakaya, T. Local effects of non-pharmaceutical interventions on mitigation of COVID-19 spread through decreased human mobilities in Japan: A prefecture-level mediation analysis. Sci. Rep. 2024, 14, 26996. [Google Scholar] [CrossRef]
- Yang, W.; Shaff, J.; Shaman, J. Effectiveness of non-pharmaceutical interventions to contain COVID-19: A case study of the 2020 spring pandemic wave in New York City. J. R. Soc. Interface 2021, 18, 20200822. [Google Scholar] [CrossRef]
- Center for Systems Science and Engineering, Johns Hopkins University. COVID-19 Unified Dataset. Available online: https://github.com/CSSEGISandData/COVID-19_Unified-Dataset/blob/master/COVID-19.rds (accessed on 1 July 2024).
- Badr, H.S.; Zaitchik, B.F.; Kerr, G.H.; Nguyen, N.-L.H.; Chen, Y.T.; Hinson, P.; Colston, J.M.; Kosek, M.N.; Dong, E.; Du, H.; et al. Unified real-time environmental-epidemiological data for multiscale modeling of the COVID-19 pandemic. Sci. Data 2023, 10, 367. [Google Scholar] [CrossRef]
- American Community Survey, U.S. Census Bureau. 2020 Maine Demographic and Housing Estimates. Available online: https://data.census.gov/table/ACSDP5Y2020.DP05 (accessed on 1 January 2025).
- American Community Survey, U.S. Census Bureau. 2022 Maine Demographic and Housing Estimates. Available online: https://data.census.gov/table/ACSDP5Y2022.DP05 (accessed on 1 January 2025).
- Miller, A.; Hannah, L.; Foti, N.; Futoma, J. Package ‘incidental’: Implements Empirical Bayes Incidence Curves. Available online: https://cran.r-project.org/web/packages/incidental/incidental.pdf (accessed on 1 January 2025).
- Division of Viral Diseases, National Center for Immunization and Respiratory Diseases. Estimated COVID-19 Burden. Available online: https://stacks.cdc.gov/view/cdc/117147 (accessed on 1 January 2025).
- Ogwara, C.A.; Ronberg, J.W.; Cox, S.M.; Wagner, B.M.; Stotts, J.W.; Chowell, G.; Spaulding, A.C.; Fung, I.C. Impact of public health policy and mobility change on transmission potential of severe acute respiratory syndrome coronavirus 2 in Rhode Island, March 2020–November 2021. Pathog. Glob. Health 2024, 118, 65–79. [Google Scholar] [CrossRef]
- U.S. Centers for Disease Control and Prevention. Estimated COVID-19 Burden. Available online: https://archive.cdc.gov/#/details?url=https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/burden.html (accessed on 10 August 2025).
- Cori, A.; Ferguson, N.M.; Fraser, C.; Cauchemez, S. A new framework and software to estimate time-varying reproduction numbers during epidemics. Am. J. Epidemiol. 2013, 178, 1505–1512. [Google Scholar] [CrossRef]
- Park, S.W.; Sun, K.; Abbott, S.; Sender, R.; Bar-on, Y.M.; Weitz, J.S.; Funk, S.; Grenfell, B.T.; Backer, J.A.; Wallinga, J.; et al. Inferring the differences in incubation-period and generation-interval distributions of the Delta and Omicron variants of SARS-CoV-2. Proc. Natl. Acad. Sci. USA 2023, 120, e2221887120. [Google Scholar] [CrossRef]
- Ofori, S.K.; Ogwara, C.A.; Kwon, S.; Hua, X.; Martin, K.M.; Mallhi, A.K.; Twum, F.; Chowell, G.; Fung, I.C. SARS-CoV-2 transmission potential and rural-urban disease burden disparities across Alabama, Louisiana, and Mississippi, March 2020–May 2021. Ann. Epidemiol. 2022, 71, 1–8. [Google Scholar] [CrossRef]
- You, C.; Deng, Y.; Hu, W.; Sun, J.; Lin, Q.; Zhou, F.; Pang, C.H.; Zhang, Y.; Chen, Z.; Zhou, X.H. Estimation of the time-varying reproduction number of COVID-19 outbreak in China. Int. J. Hyg. Environ. Health 2020, 228, 113555. [Google Scholar] [CrossRef] [PubMed]
- State of Maine Office of Governor Janet T. Mills. Governor Mills Issues Stay Healthy at Home Mandate. Available online: https://www.maine.gov/governor/mills/news/governor-mills-issues-stay-healthy-home-mandate-2020-03-31 (accessed on 15 December 2024).
- State of Maine Office of Governor Janet T. Mills. Governor Mills Extends Maine’s Stay at Home Order. Available online: https://www.maine.gov/governor/mills/news/governor-mills-extends-maines-stay-home-order-2020-04-30 (accessed on 15 December 2024).
- State of Maine Office of Governor Janet T. Mills. Governor Mills Issues Executive Order Allowing for Easing of Restrictions as Restarting Maine Plan Progresses. Available online: https://www.maine.gov/governor/mills/news/governor-mills-issues-executive-order-allowing-easing-restrictions-restarting-maine-plan (accessed on 15 December 2024).
- State of Maine Office of Governor Janet T. Mills. To Fight COVID-19, Governor Mills Strengthens Enforcement of Face Covering Requirement as Maine Reopens. Available online: https://www.maine.gov/governor/mills/news/fight-covid-19-governor-mills-strengthens-enforcement-face-covering-requirement-maine-reopens (accessed on 15 December 2024).
- Maine Public. What You Need to Know as Schools Reopen in Maine. Available online: https://www.mainepublic.org/maine/2020-09-08/what-you-need-to-know-as-schools-reopen-in-maine (accessed on 1 January 2025).
- State of Maine Office of Governor Janet T. Mills. Mills Administration Announces Maine to Enter Stage 4 of Reopening. Available online: https://www.maine.gov/governor/mills/news/mills-administration-announces-maine-enter-stage-4-reopening-2020-10-06 (accessed on 15 December 2024).
- State of Maine Office of Governor Janet T. Mills. Following Record COVID-19 Cases, Governor Mills Announces New Face Covering Executive Order. Available online: https://www.maine.gov/governor/mills/news/following-record-covid-19-cases-governor-mills-announces-new-face-covering-executive-order (accessed on 15 December 2024).
- Gostic, K.M.; McGough, L.; Baskerville, E.B.; Abbott, S.; Joshi, K.; Tedijanto, C.; Kahn, R.; Niehus, R.; Hay, J.A.; De Salazar, P.M.; et al. Practical considerations for measuring the effective reproductive number, Rt. PLoS Comput. Biol. 2020, 16, e1008409. [Google Scholar] [CrossRef]
- Tang, J.W.; Caniza, M.A.; Dinn, M.; Dwyer, D.E.; Heraud, J.-M.; Jennings, L.C.; Kok, J.; Kwok, K.O.; Li, Y.; Loh, T.P.; et al. An exploration of the political, social, economic and cultural factors affecting how different global regions initially reacted to the COVID-19 pandemic. Interface Focus 2022, 12, 20210079. [Google Scholar] [CrossRef] [PubMed]
- Petherick, A.; Goldszmidt, R.; Andrade, E.B.; Furst, R.; Hale, T.; Pott, A.; Wood, A. A worldwide assessment of changes in adherence to COVID-19 protective behaviours and hypothesized pandemic fatigue. Nat. Hum. Behav. 2021, 5, 1145–1160. [Google Scholar] [CrossRef]
- Pan, W.K.; Fernández, D.; Tyrovolas, S.; Iago, G.-V.; Dasgupta, R.R.; Zaitchik, B.F.; Lantos, P.M.; Woods, C.W. Heterogeneity in the effectiveness of non-pharmaceutical interventions during the first SARS-CoV-2 wave in the United States. Front. Public Health 2021, 9, 754696. [Google Scholar] [CrossRef]
- Chen, C.; Wang, Y.; Kaur, G.; Adiga, A.; Espinoza, B.; Venkatramanan, S.; Warren, A.; Lewis, B.; Crow, J.; Singh, R.; et al. Wastewater-based epidemiology for COVID-19 surveillance and beyond: A survey. Epidemics 2024, 49, 100793. [Google Scholar] [CrossRef]
- Ali, S.T.; Wang, L.; Lau, E.H.Y.; Xu, X.K.; Du, Z.; Wu, Y.; Leung, G.M.; Cowling, B.J. Serial interval of SARS-CoV-2 was shortened over time by nonpharmaceutical interventions. Science 2020, 369, 1106–1109. [Google Scholar] [CrossRef]
- Google LLC. Google COVID-19 Community Mobility Reports. Available online: https://www.google.com/covid19/mobility/ (accessed on 10 August 2025).
- Ofori, S.K.; Schwind, J.S.; Sullivan, K.L.; Cowling, B.J.; Chowell, G.; Fung, I.C. Transmission dynamics of COVID-19 in Ghana and the impact of public health interventions. Am. J. Trop. Med. Hyg. 2022, 107, 175–179. [Google Scholar] [CrossRef]
- Peng, L.; Ainslie, K.E.C.; Huang, X.; Cowling, B.J.; Wu, P.; Tsang, T.K. Evaluating the association between COVID-19 transmission and mobility in omicron outbreaks in China. Commun. Med. 2025, 5, 188. [Google Scholar] [CrossRef] [PubMed]
- Hale, T.; Angrist, N.; Goldszmidt, R.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S.; Cameron-Blake, E.; Hallas, L.; Majumdar, S.; et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat. Hum. Behav. 2021, 5, 529–538. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Morgenstern, C.; Kelly, J.; Lowe, R.; Munday, J.; Villabona-Arenas, C.J.; Gibbs, H.; Pearson, C.A.B.; Prem, K.; Leclerc, Q.J.; et al. The impact of non-pharmaceutical interventions on SARS-CoV-2 transmission across 130 countries and territories. BMC Med. 2021, 19, 40. [Google Scholar] [CrossRef] [PubMed]
- Tsang, T.K.; Sullivan, S.G.; Huang, X.; Wang, C.; Peng, L.; Yang, B.; Cowling, B.J. Intensity of public health and social measures are associated with effectiveness of SARS-CoV-2 vaccine in test-negative study. medRxiv 2025. [Google Scholar] [CrossRef]



| Label | Date | Policy Measure | Details |
|---|---|---|---|
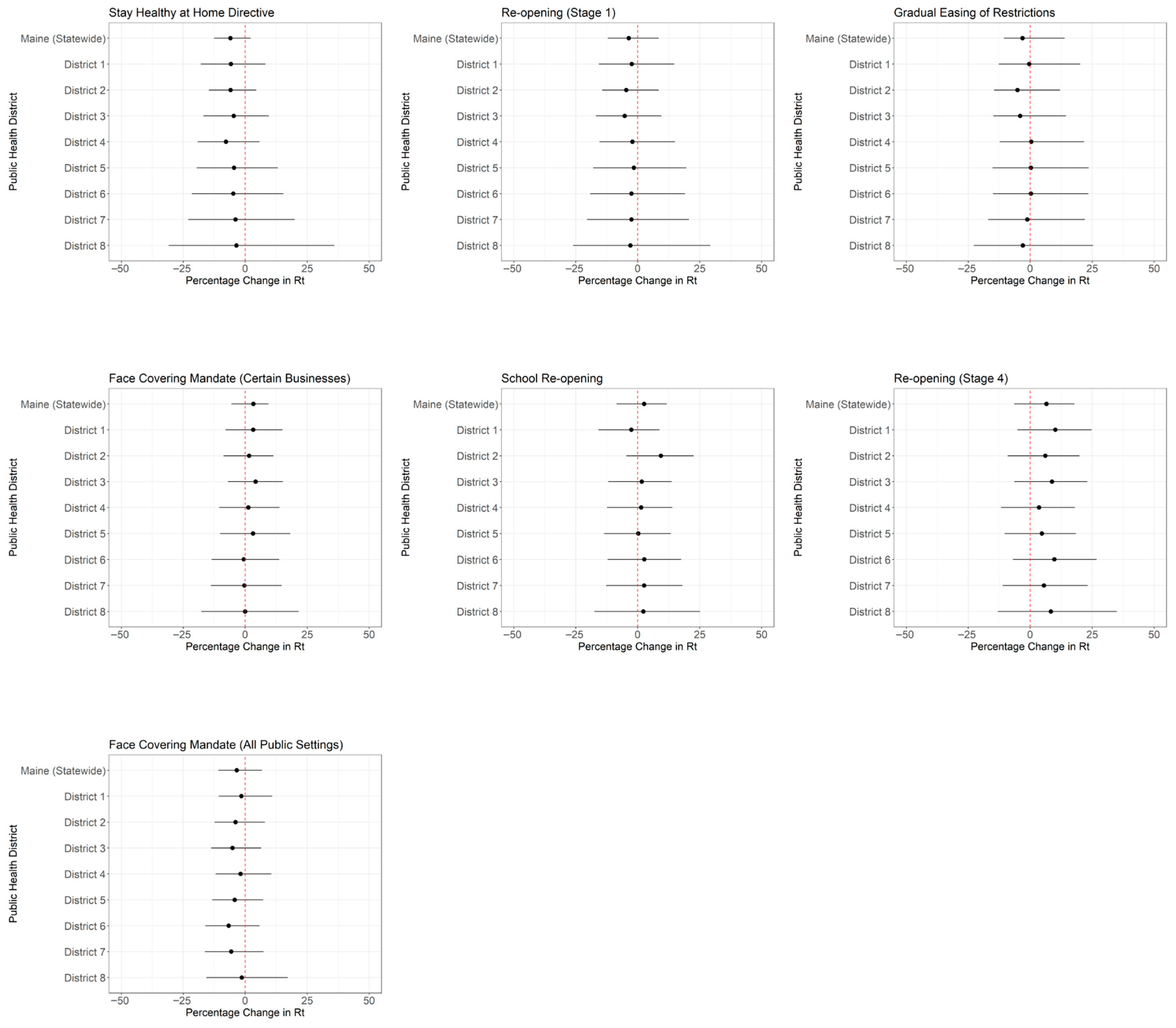
| A | 2 April 2020 | Stay Healthy at Home Directive | Governor Mills issued a series of substantial new mandates to protect public health and safety in the face of COVID-19, including a Stay Healthy at Home directive that required people living in Maine to stay at home at all times, except for essential jobs or essential personal reasons such as obtaining food, medicine, health care, or other necessary purposes [30]. |
| B | 1 May 2020 | Re-opening (Stage 1) | Governor Mills issued a new Stay Safer at Home Executive Order. The order continued to direct Maine residents to stay at home, with established exceptions for permitted activities such as occasional grocery shopping or exercising. It also allowed residents to visit businesses or participate in activities deemed safe to open under Stage 1 of the reopening plan presented on 28 April. These included barber shops and hair salons, auto dealerships, and drive-in, stay-in-your-vehicle religious services that followed COVID-19 Prevention Checklists. The order was effective immediately and extended through 31 May 2020, subject to change [31]. |
| C | 31 May 2020 | Gradual Easing of Restrictions | Governor Mills signed an Executive Order allowing for the gradual easing of restrictions implemented under previous orders as the state continued to reopen under the Restarting Maine’s Economy plan. As of this date, Maine had reopened its economy on par with, or to a greater extent than, most other New England states [32]. |
| D | 8 July 2020 | Face Covering Mandate (Certain Businesses) | Governor Mills issued an Executive Order requiring large retail businesses, restaurants, outdoor bars, tasting rooms, and lodging establishments in Maine’s more populous cities and coastal counties to enforce the state’s face covering requirement. Governor Mills also extended the State of Civil Emergency for thirty days through 6 August 2020 [33]. |
| E | 8 September 2020 | School Re-opening | Students in Maine returned to in-person classes for the first time since schools were closed due to the pandemic [34]. |
| F | 13 October 2020 | Re-opening (Stage 4) | The Mills Administration announced that Maine would move into Stage 4 of the Plan to Restart Maine’s Economy beginning Tuesday, 13 October 2020. Stage 4 increased limits on indoor seating to 50% of permitted occupancy, or 100 people (whichever was less) and maintained critical public health measures outlined in COVID-19 Prevention Checklists, such as enhanced cleaning practices and physical distancing. The state’s face covering mandate was further strengthened, requiring a broader range of entities, such as private schools and municipal buildings, to ensure that employees and individuals in their facilities adhered to this requirement. The order also expanded enforcement statewide, rather than limiting it to coastal counties and more populous cities [35]. |
| G | 4 November 2020 | Face Covering Mandate (All Public Settings) | Governor Mills announced an Executive Order requiring Maine residents to wear face coverings in public settings, regardless of the ability to maintain physical distance [36]. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, I.S.-T.; Ofori, S.K.; Babatunde, D.A.; Akowuah, E.A.; Kwok, K.O.; Chowell, G.; Fung, I.C.-H. COVID-19 Transmission Potential and Non-Pharmaceutical Interventions in Maine During the COVID-19 Pandemic. Pathogens 2025, 14, 893. https://doi.org/10.3390/pathogens14090893
Lee IS-T, Ofori SK, Babatunde DA, Akowuah EA, Kwok KO, Chowell G, Fung IC-H. COVID-19 Transmission Potential and Non-Pharmaceutical Interventions in Maine During the COVID-19 Pandemic. Pathogens. 2025; 14(9):893. https://doi.org/10.3390/pathogens14090893
Chicago/Turabian StyleLee, Ina Sze-Ting, Sylvia K. Ofori, Doyinsola A. Babatunde, Emmanuel A. Akowuah, Kin On Kwok, Gerardo Chowell, and Isaac Chun-Hai Fung. 2025. "COVID-19 Transmission Potential and Non-Pharmaceutical Interventions in Maine During the COVID-19 Pandemic" Pathogens 14, no. 9: 893. https://doi.org/10.3390/pathogens14090893
APA StyleLee, I. S.-T., Ofori, S. K., Babatunde, D. A., Akowuah, E. A., Kwok, K. O., Chowell, G., & Fung, I. C.-H. (2025). COVID-19 Transmission Potential and Non-Pharmaceutical Interventions in Maine During the COVID-19 Pandemic. Pathogens, 14(9), 893. https://doi.org/10.3390/pathogens14090893







