An Umbrella Review of E-Cigarettes’ Impact on Oral Microbiota and Biofilm Buildup
Abstract
1. Introduction
2. Materials and Methods
2.1. Reporting Format
2.2. Population, Exposure, Comparison, Outcome (PECO)
- Population: E-cigarette users, traditional cigarette smokers, and non-smokers.
- Exposure: E-cigarettes or ENDS.
- Comparison: Non-smokers vs. traditional cigarette smokers.
- Outcome: Biofilm buildup or plaque index and composition of the oral microbiota.
2.3. Eligibility Criteria
- Inclusion Criteria: Systematic reviews, with or without meta-analyses, that examine the effects of e-cigarette use on the buildup of oral biofilms (e.g., plaque index) and/or the composition of the oral microbiota in e-cigarette smokers, traditional cigarette smokers, and non-smokers. No language restrictions were applied.
- Exclusion Criteria: Studies that are not systematic reviews or meta-analyses, studies that do not focus on e-cigarette use, studies that do not address oral health outcomes, commentary papers, and studies involving non-human populations.
2.4. Information Sources and Search Strategy
2.5. Study Screening and Data Extraction Procedures
2.6. Quality Assessment
3. Results
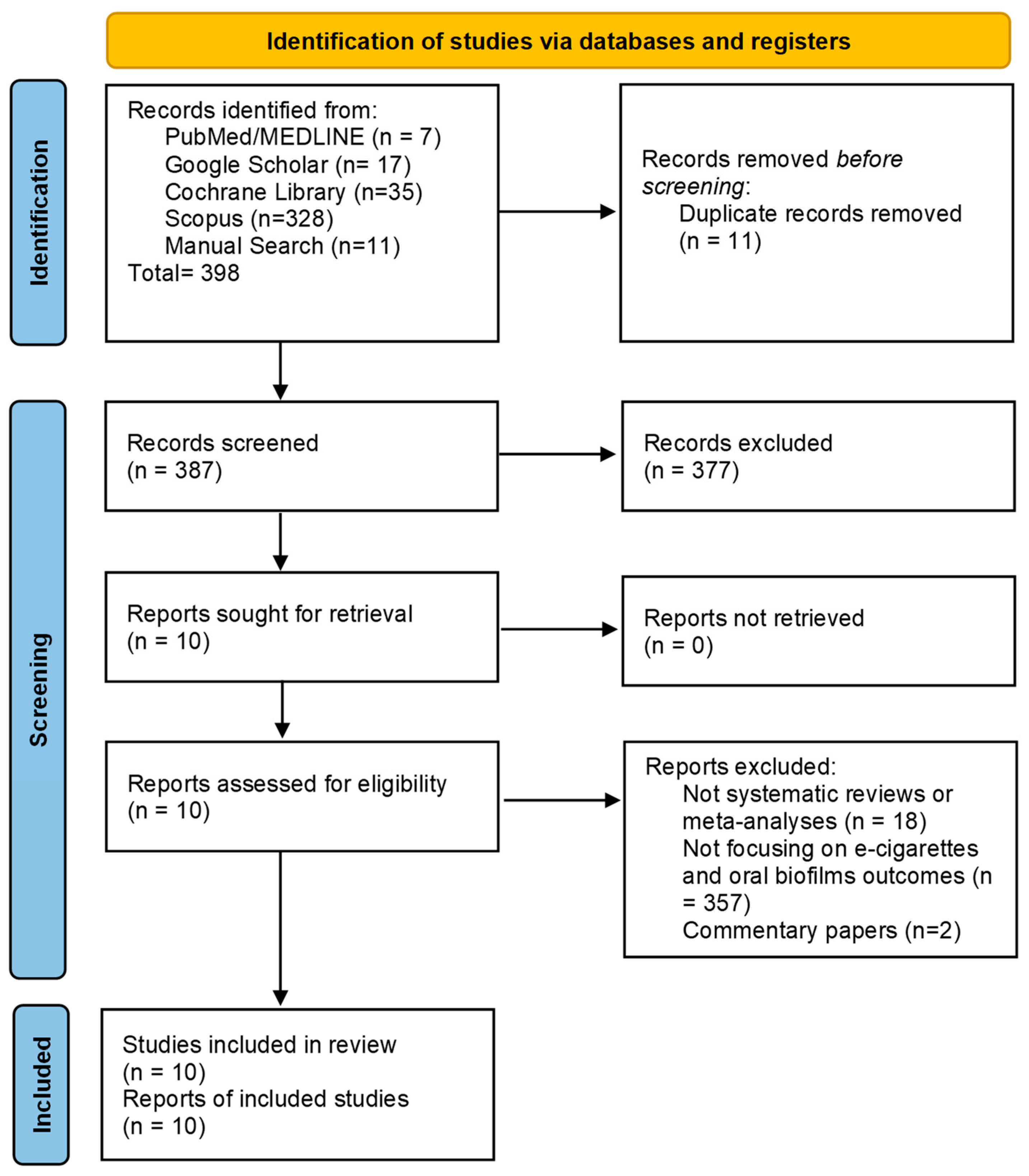
3.1. Overview of the Screening Process
3.2. Characteristics of the Included Studies
3.3. Quality Assessment Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ENDS | Electronic nicotine delivery system |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| AMSTAR | A MeaSurement Tool to Assess Systematic Reviews |
References
- Kumar, P.S.; Clark, P.; Brinkman, M.C.; Saxena, D. Novel Nicotine Delivery Systems. Adv. Dent. Res. 2019, 30, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Albadrani, M.S.; Tobaiqi, M.A.; Muaddi, M.A.; Eltahir, H.M.; Abdoh, E.S.; Aljohani, A.M.; Albadawi, E.A.; Alzaman, N.S.; Abouzied, M.M.; Fadlalmola, H.A. A global prevalence of electronic nicotine delivery systems (ENDS) use among students: A systematic review and meta-analysis of 4,189,145 subjects. BMC Public Health 2024, 24, 3311. [Google Scholar] [CrossRef] [PubMed]
- CDC. E-Cigarette Use Among Youth. Available online: https://www.cdc.gov/tobacco/e-cigarettes/youth.html (accessed on 28 March 2025).
- Cui, Z.; Wang, P.; Gao, W. Microbial dysbiosis in periodontitis and peri-implantitis: Pathogenesis, immune responses, and therapeutic. Front. Cell. Infect. Microbiol. 2025, 15, 1517154. [Google Scholar] [CrossRef] [PubMed]
- Hajishengallis, G.; Lamont, R.J.; Koo, H. Oral polymicrobial communities: Assembly, function, and impact on diseases. Cell Host Microbe 2023, 31, 528–538. [Google Scholar] [CrossRef]
- Lamont, R.J.; Koo, H.; Hajishengallis, G. The oral microbiota: Dynamic communities and host interactions. Nat. Rev. Microbiol. 2018, 16, 745–759. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, R.; Botelho, J.; Machado, V.; Mascarenhas, P.; Alcoforado, G.; Mendes, J.J.; Chambrone, L. Predictors of tooth loss during long-term periodontal maintenance: An updated systematic review. J. Clin. Periodontol. 2021, 48, 1019–1036. [Google Scholar] [CrossRef]
- Socransky, S.S.; Haffajee, A.D. Periodontal microbial ecology. Periodontology 2000 2005, 38, 135–187. [Google Scholar] [CrossRef]
- Chapple, I.L.C.; Mealey, B.L.; Van Dyke, T.E.; Bartold, P.M.; Dommisch, H.; Eickholz, P.; Geisinger, M.L.; Genco, R.J.; Glogauer, M.; Goldstein, M.; et al. Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: Consensus report of workgroup 1 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Periodontol. 2018, 89, S74–S84. [Google Scholar] [CrossRef]
- Belibasakis, G.N.; Manoil, D. Microbial Community-Driven Etiopathogenesis of Peri-Implantitis. J. Dent. Res. 2021, 100, 21–28. [Google Scholar] [CrossRef]
- Costa, F.O.; Lages, E.J.; Cota, L.O.; Lorentz, T.C.; Soares, R.V.; Cortelli, J.R. Tooth loss in individuals under periodontal maintenance therapy: 5-year prospective study. J. Periodontal. Res. 2014, 49, 121–128. [Google Scholar] [CrossRef]
- Ebersole, J.; Samburova, V.; Son, Y.; Cappelli, D.; Demopoulos, C.; Capurro, A.; Pinto, A.; Chrzan, B.; Kingsley, K.; Howard, K.; et al. Harmful chemicals emitted from electronic cigarettes and potential deleterious effects in the oral cavity. Tob. Induc. Dis. 2020, 18, 41. [Google Scholar] [CrossRef] [PubMed]
- Ganesan, S.M.; Dabdoub, S.M.; Nagaraja, H.N.; Scott, M.L.; Pamulapati, S.; Berman, M.L.; Shields, P.G.; Wewers, M.E.; Kumar, P.S. Adverse effects of electronic cigarettes on the disease-naive oral microbiome. Sci. Adv. 2020, 6, eaaz0108. [Google Scholar] [CrossRef] [PubMed]
- Thomas, C.; Minty, M.; Vinel, A.; Canceill, T.; Loubières, P.; Burcelin, R.; Kaddech, M.; Blasco-Baque, V.; Laurencin-Dalicieux, S. Oral Microbiota: A Major Player in the Diagnosis of Systemic Diseases. Diagnostics 2021, 11, 1376. [Google Scholar] [CrossRef] [PubMed]
- Ptasiewicz, M.; Grywalska, E.; Mertowska, P.; Korona-Głowniak, I.; Poniewierska-Baran, A.; Niedźwiedzka-Rystwej, P.; Chałas, R. Armed to the Teeth-The Oral Mucosa Immunity System and Microbiota. Int. J. Mol. Sci. 2022, 23, 882. [Google Scholar] [CrossRef]
- Alves, C.H.; Russi, K.L.; Rocha, N.C.; Bastos, F.; Darrieux, M.; Parisotto, T.M.; Girardello, R. Host-microbiome interactions regarding peri-implantitis and dental implant loss. J. Transl. Med. 2022, 20, 425. [Google Scholar] [CrossRef]
- Persson, G.R.; Renvert, S. Cluster of bacteria associated with peri-implantitis. Clin. Implant. Dent. Relat. Res. 2014, 16, 783–793. [Google Scholar] [CrossRef]
- Gaur, S.; Agnihotri, R. The Role of Electronic Cigarettes in Dental Caries: A Scoping Review. Scientifica 2023, 2023, 9980011. [Google Scholar] [CrossRef]
- Fagan, P.; Pokhrel, P.; Herzog, T.A.; Moolchan, E.T.; Cassel, K.D.; Franke, A.A.; Li, X.; Pagano, I.; Trinidad, D.R.; Sakuma, K.K.; et al. Sugar and Aldehyde Content in Flavored Electronic Cigarette Liquids. Nicotine Tob. Res. 2018, 20, 985–992. [Google Scholar] [CrossRef]
- Ng, E.; Tay, J.R.H.; Mattheos, N.; Bostanci, N.; Belibasakis, G.N.; Seneviratne, C.J. A Mapping Review of the Pathogenesis of Peri-Implantitis: The Biofilm-Mediated Inflammation and Bone Dysregulation (BIND) Hypothesis. Cells 2024, 13, 315. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef] [PubMed]
- Tattar, R.; Jackson, J.; Holliday, R. The impact of e-cigarette use on periodontal health: A systematic review and meta-analysis. Evid. Based Dent. 2025, 1–7. [Google Scholar] [CrossRef]
- Shabil, M.; Khatib, M.N.; Ballal, S.; Bansal, P.; Tomar, B.S.; Ashraf, A.; Kumar, M.R.; Sinha, A.; Rawat, P.; Gaidhane, A.M.; et al. The impact of electronic cigarette use on periodontitis and periodontal outcomes: A systematic review and meta-analysis. BMC Oral Health 2024, 24, 1197. [Google Scholar] [CrossRef]
- Vámos, O.; Komora, P.; Gede, N.; Hegyi, P.; Kelemen, K.; Varga, G.; Mikulás, K.; Kerémi, B.; Kispélyi, B. The Effect of Nicotine-Containing Products on Peri-Implant Tissues: A Systematic Review and Network Meta-Analysis. Nicotine Tob. Res. 2024, 26, 1276–1285. [Google Scholar] [CrossRef] [PubMed]
- Zięba, S.; Zalewska, A.; Żukowski, P.; Maciejczyk, M. Can smoking alter salivary homeostasis? A systematic review on the effects of traditional and electronic cigarettes on qualitative and quantitative saliva parameters. Dent. Med. Probl. 2024, 61, 129–144. [Google Scholar] [CrossRef] [PubMed]
- Youssef, M.; Marzouk, T.; Abdelsalam, H.; Malmstrom, H.; Barmak, A.B.; Fraser, D.; Tsigarida, A. The effect of electronic cigarette use on peri-implant conditions in men: A systematic review and meta-analysis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2023, 135, 492–500. [Google Scholar] [CrossRef]
- Camoni, N.; Conti, G.; Esteves-Oliveira, M.; Carvalho, T.S.; Roccuzzo, A.; Cagetti, M.G.; Campus, G. Electronic Cigarettes, Heated Tobacco Products, and Oral Health: A Systematic Review and Meta-Analysis. Appl. Sci. 2023, 13, 9654. [Google Scholar] [CrossRef]
- Thiem, D.G.E.; Donkiewicz, P.; Rejaey, R.; Wiesmann-Imilowski, N.; Deschner, J.; Al-Nawas, B.; Kämmerer, P.W. The impact of electronic and conventional cigarettes on periodontal health-a systematic review and meta-analysis. Clin. Oral Investig. 2023, 27, 4911–4928. [Google Scholar] [CrossRef]
- Figueredo, C.A.; Abdelhay, N.; Figueredo, C.M.; Catunda, R.; Gibson, M.P. The impact of vaping on periodontitis: A systematic review. Clin. Exp. Dent. Res. 2021, 7, 376–384. [Google Scholar] [CrossRef]
- Yang, I.; Shelly, S.; Rodriguez, J. The oral health impact of electronic cigarette use: A systematic review. Crit. Rev. Toxicol. 2020, 50, 97–127. [Google Scholar] [CrossRef]
- Ralho, A.; Coelho, A.; Ribeiro, M.; Paula, A.; Amaro, I.; Sousa, J.; Marto, C.; Ferreira, M.; Carrilho, E. Effects of Electronic Cigarettes on Oral Cavity: A Systematic Review. J. Evid. Based Dent. Pract. 2019, 19, 101318. [Google Scholar] [CrossRef] [PubMed]
- Koo, H.; Yamada, K.M. Dynamic cell-matrix interactions modulate microbial biofilm and tissue 3D microenvironments. Curr. Opin. Cell Biol. 2016, 42, 102–112. [Google Scholar] [CrossRef] [PubMed]
- Marsh, P.D. Dental plaque as a biofilm and a microbial community-implications for health and disease. BMC Oral Health 2006, 6 (Suppl. 1), S14. [Google Scholar] [CrossRef] [PubMed]
- Murakami, S.; Mealey, B.L.; Mariotti, A.; Chapple, I.L.C. Dental plaque-induced gingival conditions. J. Periodontol. 2018, 89 (Suppl. 1), S17–S27. [Google Scholar] [CrossRef]
- Xu, F.; Pushalkar, S.; Lin, Z.; Thomas, S.C.; Persaud, J.K.; Sierra, M.A.; Vardhan, M.; Vasconcelos, R.; Akapo, A.; Guo, Y.; et al. Electronic cigarette use enriches periodontal pathogens. Mol. Oral Microbiol. 2022, 37, 63–76. [Google Scholar] [CrossRef]
- Corrêa, M.G.; Pimentel, S.P.; Ribeiro, F.V.; Cirano, F.R.; Casati, M.Z. Host response and peri-implantitis. Braz. Oral Res. 2019, 33, e066. [Google Scholar] [CrossRef]
| Authors/Year | Type of Study | No. of Included Studies | Population | Risk of Bias and Quality Assessment Methods | Source of Funding | Outcomes Related to Plaque Accumulation and Microbial Diversity Changes in E-Cigarette Users | Conclusions |
|---|---|---|---|---|---|---|---|
| Tattar et al., 2025 [23] | Systematic review and meta-analysis | 40 | E-cigarette smokers, traditional cigarette smokers and non-smokers. | NOS, ROBINS-I, and RoB-2 | National Institute of Health and Care Research (NIHR). | Five studies in this review investigated microbiome changes and found that e-cigarette use is associated with alterations in the oral microbiome, with specific microbial shifts tied to oral health risks. | There is evidence that e-cigaretts use has some impact on periodontal parameters compared to non-smokers/former smokers. Tobacco smokers had consistently worst outcomes. Caution is needed due to methodological issues, such as reliance on self-reporting and confounding factors like smoking status and history of the patient. |
| Shabil et al., 2024 [24] | Systematic review and meta-analysis | 12 | E-cigarette users and non-users. | NOS | This study received no funding. | There is a significant difference in plaque index between e-cigarette users and non-users, with e-cigarette users exhibiting an increased plaque index. | Further long-term observational studies are needed to better understand the potential risks e-cigarettes pose to periodontal health. The studies showed considerable heterogeneity. |
| Vámos et al., 2024 [25] | Systematic review and network meta-analysis | 39 | E-cigarette users, waterpipe users, traditional cigarette smokers, and non-smokers possesing dental implants. | QUIPS | Centre for Translational Medicine, Semmelweis University. | E-cigarette smokers showed significantly higher plaque indexes compared to non-smokers. | Most nicotine-containing product users presented worse clinico-radiographic and immunological peri-implant parameters compared to non-smokers. The analysis revealed no significant heterogeneity across the studies. |
| Zięba et al., 2024 [26] | Systematic review | 65 | E-cigarette and traditional cigarette users. | Quality Assessment Tool guidelines issued by the National Heart, Lung and Blood Institute (NHLBI) within the U.S. National Institutes of Health (NIH). | None declared. | E-cigarette use can increase the levels of cariogenic bacteria, such as Streptococcus mutans and Lactobacilli, in saliva. Nicotine in e-cigarettes is believed to contribute to this by promoting the adhesion of bacteria to the tooth biofilm and stimulating the synthesis of extracellular polysaccharides, which thickens the biofilm. This process may increase the risk of dental caries, as the activity of these bacteria leads to higher levels of lactic acid production. | While some studies show a correlation between e-cigarette use and increased bacterial counts, more research is needed to fully understand the extent of e-cigarettes’ impact on oral health. |
| Youssef et al., 2023 [27] | Systematic review and meta-analysis | 4 | Only male e-cigarette users and non-smokers possessing implant-supported prostheses. | Joanna Briggs Institute critical appraisal tool | Did not declare. | E-cigarette users had significantly higher plaque index compared to never smokers. | E-cigarettes may have a negative effect on the clinical, radiographic, and pro-inflammatory profile of dental implants. Further studies, including longitudinal investigations in diverse patient populations, are required to confirm these outcomes.The studies showed moderate but nonsignificant heterogeneity |
| Camoni et al., 2023 [28] | Systematic review and meta-analysis | 84 | E- cigarette and heated tobacco smokers or human cells/oral bacteria exposed to ENDS. | ROBIN-I and RoB-2 | This study received no funding. | A meta-analyses combining data from 6 studies on self-perceived gingivitis and found an association between e-cigarette use and self-reported gingivitis. They also noted that flavored e-liquids from e-cigarettes are detrimental to the enamel, similar to what is caused by gelatinous sweets or acidic drinks. | E-cigarettes have a potential detrimental effect on periodontal and peri-implant parameters, and laboratory tests confirmed the presence of carcinogenic and inflammatory biomarkers. Flavored e-liquids may be a caries risk factor. |
| Thiem et al., 2023 [29] | Systematic review and meta-analysis | 16 | E-cigarette smokers, traditional cigarette smokers and non-smokers. | NOS and GRADE | Open Access funding enabled and organized by Projekt DEAL. | The plaque index was significantly higher in cigarette smokers compared to e-cigarette users and non-smokers in six studies. One study showing no difference between e-cigarette users and non-smokers, and another study showed increased plaque in e-cigarette users compared to non-smokers. | E-cigarette use may be considered a healthier alternative to cigarette smoking in terms of periodontal health; however, harmful effects of e-cigarettes use on periodontal health have also been observed. |
| Figueredo et al., 2021 [30] | Systematic review | 8 | Individuals using e-cigarettes for at least one year prior to the study, including both non-smokers and those who did not use any form of tobacco. | Joanna Briggs Institute critical appraisal tool | Did not declare. | Plaque index results are consistently increased across studies with the use of e-cigarettes. | While there is insufficient evidence to fully characterize vaping’s impact on periodontitis, available results suggest a negative effect, highlighting the need for further longitudinal clinical studies. |
| Yang et al., 2020 [31] | Systematic review | 98 | E-cigarette users, conventional cigarette smokers and non-smokers using e-ciagaretts for at least one year. | Effective Public Health Practice Project (EPHPP) Quality Assessment Tool | This study received no funding. | E-cigarette users, especially long-term users, were more likely to develop periodontal and gingival disease compared to non-users. They also experienced worse peri-implant parameters than non-users, although better than conventional smokers, along with increased dental issues like cracked teeth, toothache, and worsened dental caries. Daily e-cigarette use was linked to poorer oral health, including tooth loss, and flavored aerosols contributed to decreased enamel hardness and discoloration. | This review suggests that e-cigarette use may reduce negative oral symptoms in conventional smokers but may cause discomfort, lesions, and dental damage in non-smokers. Further research is needed, particularly regarding long-term clinical outcomes, age, and flavored e-cigarette products. |
| Ralho et al., 2019 [32] | Systematic review | 8 | Non-smokers, ex-smokers, conventional cigarette smokers, or other types of smokers. | ROBINS-I | This study received no funding. | E-cigarette users did not show significant differences in plaque index compared to non-smokers, except in one study where e-cigarette users exhibited a higher plaque index; however, another study found that e-cigarette users, waterpipe smokers, and cigarette smokers had a higher prevalence of Candida spp. compared to non-smokers. | The results suggest that e-cigarettes are less harmful than conventional cigarettes; however, they also indicate that e-cigarette users may be more susceptible to developing alterations in oral biological tissues compared to ex-smokers or non-smokers. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Panariello, B.; Dias Panariello, F.; Misir, A.; Barboza, E.P. An Umbrella Review of E-Cigarettes’ Impact on Oral Microbiota and Biofilm Buildup. Pathogens 2025, 14, 578. https://doi.org/10.3390/pathogens14060578
Panariello B, Dias Panariello F, Misir A, Barboza EP. An Umbrella Review of E-Cigarettes’ Impact on Oral Microbiota and Biofilm Buildup. Pathogens. 2025; 14(6):578. https://doi.org/10.3390/pathogens14060578
Chicago/Turabian StylePanariello, Beatriz, Fabrízio Dias Panariello, Ashminie Misir, and Eliane Porto Barboza. 2025. "An Umbrella Review of E-Cigarettes’ Impact on Oral Microbiota and Biofilm Buildup" Pathogens 14, no. 6: 578. https://doi.org/10.3390/pathogens14060578
APA StylePanariello, B., Dias Panariello, F., Misir, A., & Barboza, E. P. (2025). An Umbrella Review of E-Cigarettes’ Impact on Oral Microbiota and Biofilm Buildup. Pathogens, 14(6), 578. https://doi.org/10.3390/pathogens14060578





