A Practical Framework for ASFV Disinfectant Evaluation: Differentiating Cytopathic Effects from Cytotoxicity via Integrated Analytical Methods
Abstract
1. Introduction
2. Materials and Methods
2.1. Cells and Virus
2.2. Preparation of Disinfectant Solutions
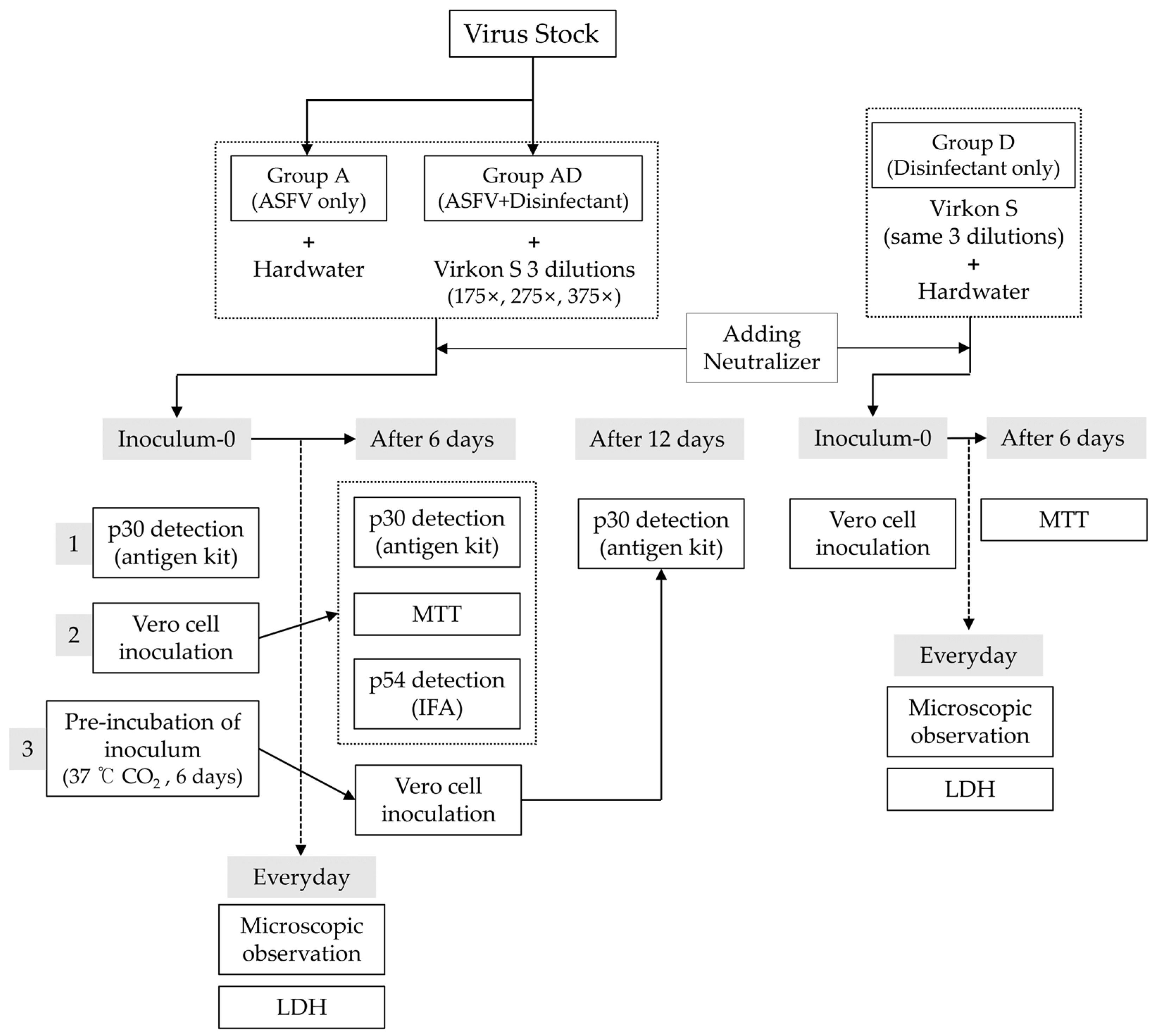
2.3. Experimental Design
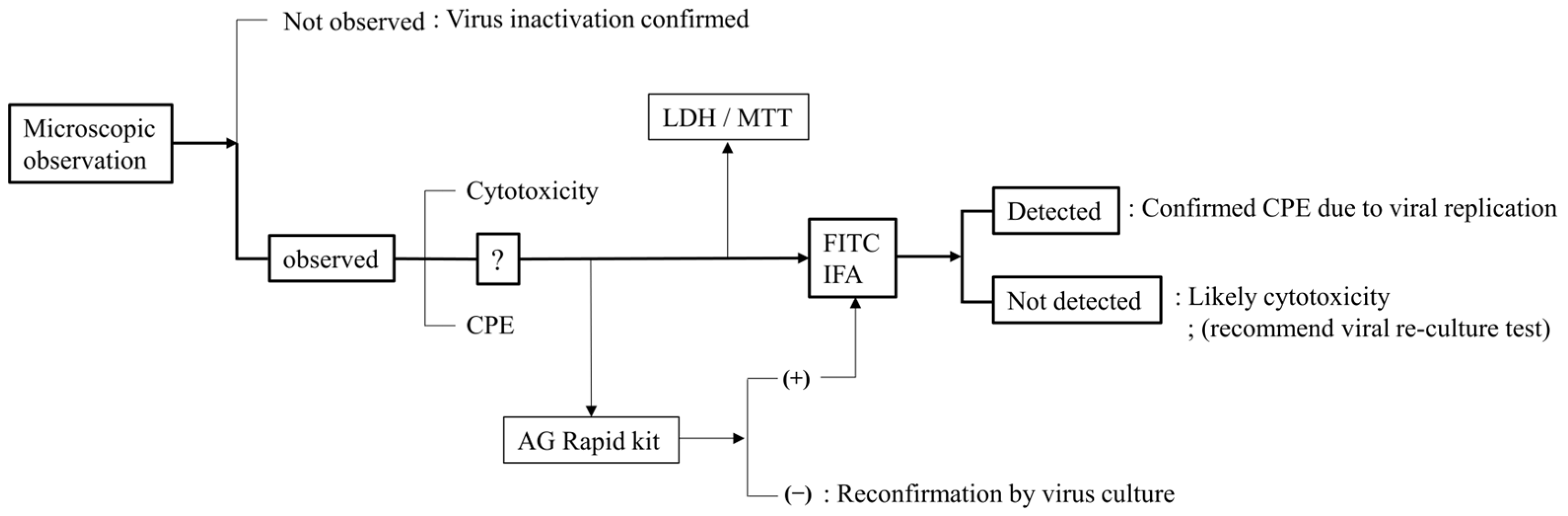
2.4. Virucidal Efficacy Test and Microscopic Observation
2.5. Viral Antigen Detection
2.5.1. Lateral Flow Immunoassay (AG Rapid Kit—p30 Detection)
2.5.2. FITC Immunofluorescence (p54 Detection) and DAPI
2.6. Cytotoxicity and Viability Assays
2.6.1. LDH Release Assay
2.6.2. MTT Assay
2.7. Statistical Analysis
3. Results
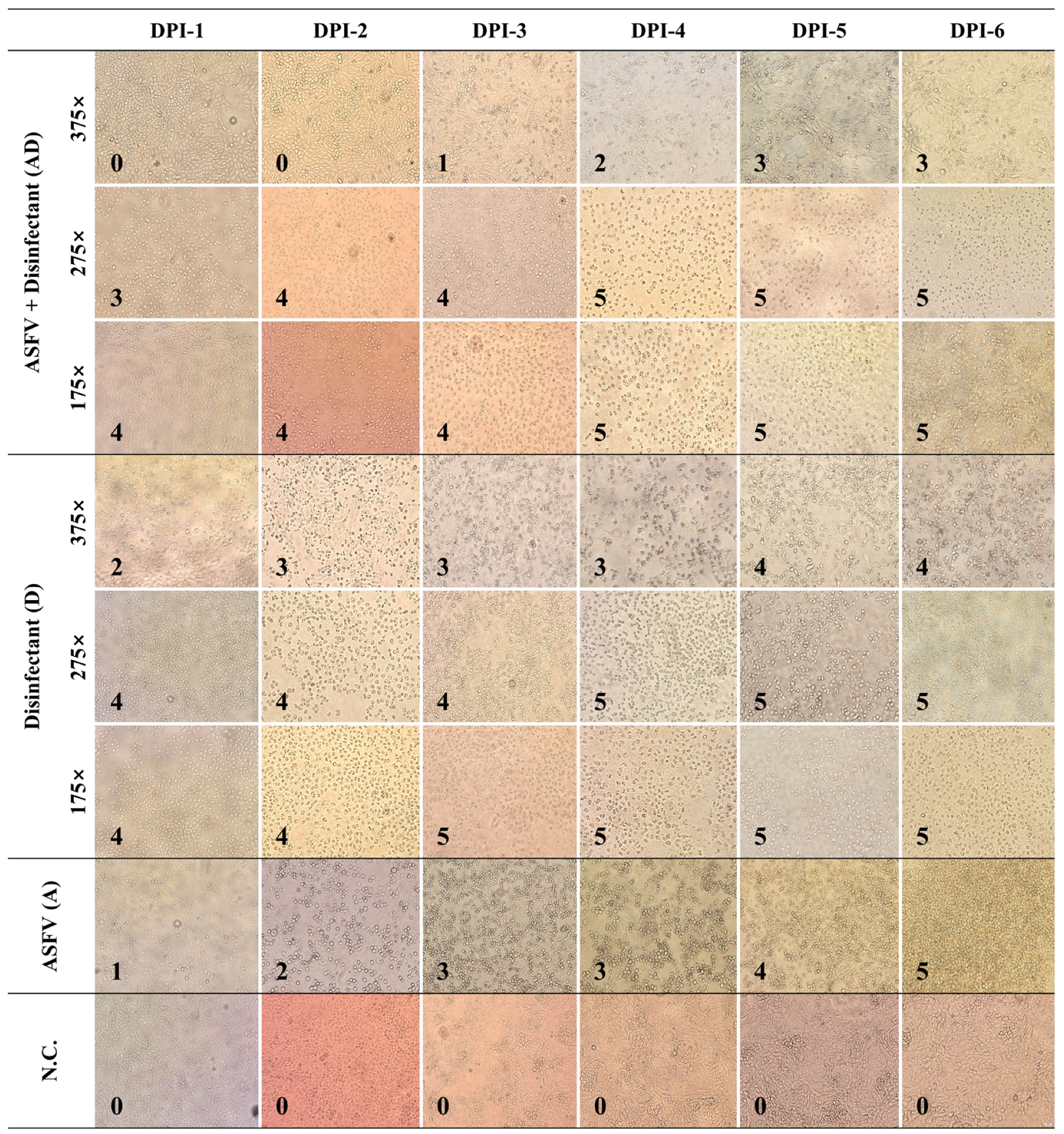
3.1. Cell Damage over Time
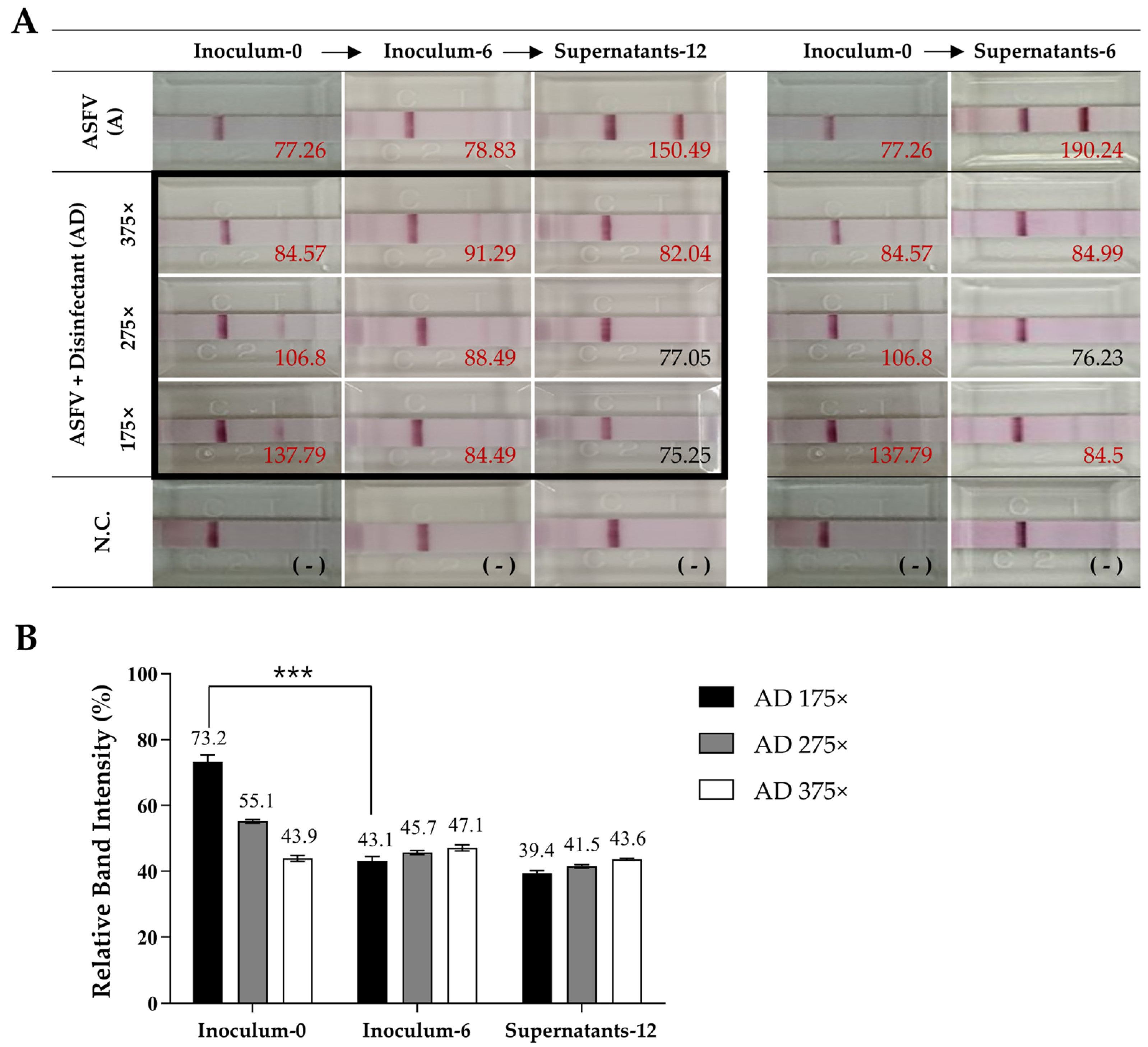
3.2. Antigen Detection Using AG Rapid Kit over Time
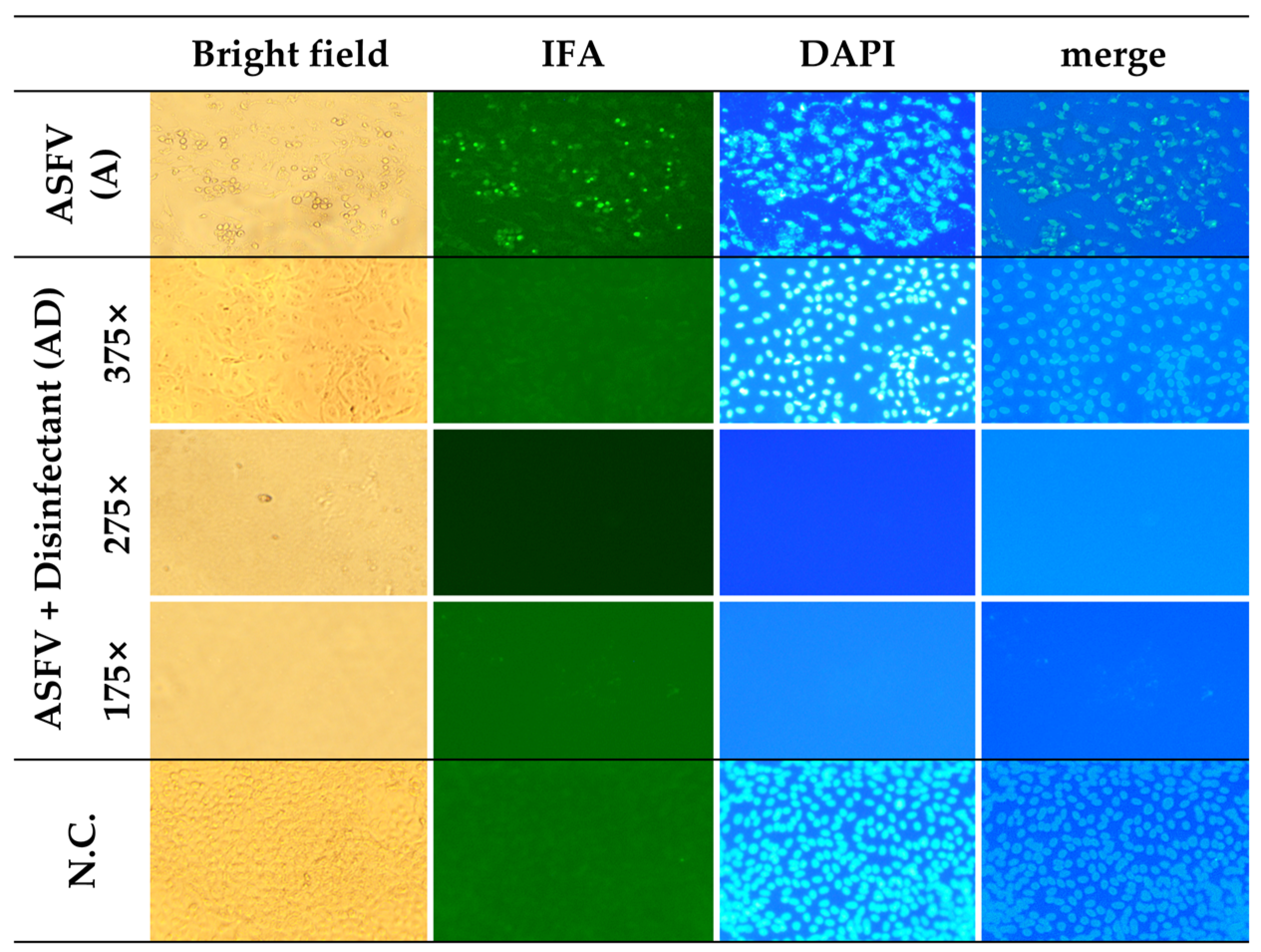
3.3. Detection of ASFV Antigen (FITC) and Nuclei Integrity (DAPI) at DPI-6
3.4. Cytotoxicity Analysis Based on LDH Release and MTT Assay
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| A | ASFV-only group |
| AD | ASFV + disinfectant group |
| AIV | Avian influenza virus |
| ANOVA | Analysis of variance |
| APQA | Animal and Plant Quarantine Agency |
| ASFV | African swine fever virus |
| CPE | Cytopathic effect |
| CV | Coefficient of variation |
| D | Disinfectant-only group |
| DAPI | 4′,6-Diamidino-2-Phenylindole |
| DPI | Days post infection or inoculation |
| DNA | Deoxyribonucleic acid |
| EM | Electron microscopy |
| FBS | Fetal bovine serum |
| FITC | Fluorescein isothiocyanate |
| FMDV | Foot-and-mouth disease virus |
| IFA | Immunofluorescence assay |
| kbp | Kilobase pair |
| KVCC | Korea Veterinary Culture Collection |
| LDH | Lactate dehydrogenase |
| MTT | 3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide |
| PAMs | Porcine alveolar macrophages |
| PEDV | Porcine epidemic diarrhea virus |
| SD | Standard deviation |
| TCID | Tissue culture infectious dose |
| WSL | Wild boar lung or wild swine lung |
References
- Dixon, L.K.; Stahl, K.; Jori, F.; Vial, L.; Pfeiffer, D.U. African Swine Fever Epidemiology and Control. Annu. Rev. Anim. Biosci. 2020, 8, 221–246. [Google Scholar] [CrossRef]
- Sauter-Louis, C.; Conraths, F.J.; Probst, C.; Blohm, U.; Schulz, K.; Sehl, J.; Fischer, M.; Forth, J.H.; Zani, L.; Depner, K.; et al. African Swine Fever in Wild Boar in Europe—A Review. Viruses 2021, 13, 1717. [Google Scholar] [CrossRef] [PubMed]
- Ceruti, A.; Kobialka, R.M.; El Wahed, A.A.; Truyen, U. African Swine Fever: A One Health Perspective and Global Challenges. Animals 2025, 15, 928. [Google Scholar] [CrossRef]
- Li, Z.; Chen, W.; Qiu, W.; Li, Y.; Fan, J.; Wu, K.; Li, X.; Zhao, M.; Ding, H.; Fan, S. African swine fever virus: A review. Life 2022, 12, 1255. [Google Scholar] [CrossRef] [PubMed]
- Dixon, L.; Sun, H.; Roberts, H. African swine fever. Antivir. Res. 2019, 165, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Gaudreault, N.N.; Madden, D.W.; Wilson, W.C.; Trujillo, J.D.; Richt, J.A. African Swine Fever Virus: An Emerging DNA Arbovirus. Front. Vet. Sci. 2020, 7, 215. [Google Scholar] [CrossRef]
- Blome, S.; Franzke, K.; Beer, M. African swine fever—A review of current knowledge. Virus Res. 2020, 287, 198099. [Google Scholar] [CrossRef]
- Wang, G.; Xie, M.; Wu, W.; Chen, Z. Structures and Functional Diversities of ASFV Proteins. Viruses 2021, 13, 2124. [Google Scholar] [CrossRef]
- Dolata, K.M.; Pei, G.; Netherton, C.L.; Karger, A. Functional Landscape of African Swine Fever Virus–Host and Virus–Virus Protein Interactions. Viruses 2023, 15, 1634. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, Y.; Zhang, K.; Deng, D.; Peng, K.; Zheng, W.; Chen, N.; Liu, P.; Shang, S.; Li, R.; et al. Characterization of three African swine fever viruses from different clinical settings revealed a potential attenuation mechanism. Anim. Dis. 2024, 4, 24. [Google Scholar] [CrossRef]
- Simões, M.; Martins, C.; Ferreira, F. Localization of ASFV DNA replication and morphological study of subnuclear compartments during viral infection. Microsc. Microanal. 2013, 19, 13–14. [Google Scholar] [CrossRef]
- Juszkiewicz, M.; Walczak, M.; Mazur-Panasiuk, N.; Woźniakowski, G. Effectiveness of Chemical Compounds Used against African Swine Fever Virus in Commercial Available Disinfectants. Pathogens 2020, 9, 878. [Google Scholar] [CrossRef]
- Beato, M.S.; D’errico, F.; Iscaro, C.; Petrini, S.; Giammarioli, M.; Feliziani, F. Disinfectants against African Swine Fever: An Updated Review. Viruses 2022, 14, 1384. [Google Scholar] [CrossRef]
- Frost, L.; Tully, M.; Dixon, L.; Hicks, H.M.; Bennett, J.; Stokes, I.; Marsella, L.; Gubbins, S.; Batten, C. Evaluation of the Efficacy of Commercial Disinfectants against African Swine Fever Virus. Pathogens 2023, 12, 855. [Google Scholar] [CrossRef] [PubMed]
- Lee, G.-H.; Park, S.-H.; Song, B.-M.; Kim, D.-M.; Han, H.-J.; Park, J.-Y.; Jo, Y.-W.; Hwang, M.-Y.; Sim, K.-T.; Kang, S.-M.; et al. Comparative efficacy evaluation of disinfectants against severe acute respiratory syndrome coronavirus-2. J. Hosp. Infect. 2022, 131, 12–22. [Google Scholar] [CrossRef]
- Chiu, S.; Skura, B.; Petric, M.; McIntyre, L.; Gamage, B.; Isaac-Renton, J. Efficacy of common disinfectant/cleaning agents in inactivating murine norovirus and feline calicivirus as surrogate viruses for human norovirus. Am. J. Infect. Control. 2015, 43, 1208–1212. [Google Scholar] [CrossRef]
- Gordon, V.; Parry, S.; Bellamy, K.; Osborne, R. Assessment of chemical disinfectants against human immunodeficiency virus: Overcoming the problem of cytotoxicity and the evaluation of selected actives. J. Virol. Methods 1993, 45, 247–257. [Google Scholar] [CrossRef] [PubMed]
- Juszkiewicz, M.; Walczak, M.; Woźniakowski, G.; Pejsak, Z.; Podgórska, K. The Influence of the Temperature on Effectiveness of Selected Disinfectants Against African Swine Fever Virus (ASFV). Viruses 2025, 17, 156. [Google Scholar] [CrossRef]
- Rhee, C.H.; Her, M.; Jeong, W. Modified Vaccinia Virus Ankara as a Potential Biosafety Level 2 Surrogate for African Swine Fever Virus in Disinfectant Efficacy Tests. Pathogens 2022, 11, 320. [Google Scholar] [CrossRef]
- Sugiura, K.; Yamamoto, M.; Motomura, S.; Negishi, T.; Shinkawa, S.; Oishi, K. Creation of the animal products safety division in the ministry of agriculture, forestry and fisheries of Japan. Vet Ital. 2007, 43, 55–64. [Google Scholar]
- Bieker, J.M. Chemical Inactivation of Viruses; Kansas State University: Manhattan, KS, USA, 2006. [Google Scholar]
- Wales, A.D.; Davies, R.H. Disinfection to control African swine fever virus: A UK perspective. J. Med. Microbiol. 2021, 70, 001410. [Google Scholar] [CrossRef] [PubMed]
- Ekström, J.-O.; Tolf, C.; Edman, K.-A.; Lindberg, A.M. Physicochemical Properties of the Ljungan Virus Prototype Virion in Different Environments: Inactivated by Heat but Resistant to Acidic pH, Detergents and Non-Physiological Environments Such as Virkon®-Containing Solutions. Microbiol. Immunol. 2007, 51, 841–850. [Google Scholar] [CrossRef]
- Gabbert, L.R.; Neilan, J.G.; Rasmussen, M. Recovery and chemical disinfection of foot-and-mouth disease and African swine fever viruses from porous concrete surfaces. J. Appl. Microbiol. 2020, 129, 1092–1101. [Google Scholar] [CrossRef]
- De Benedictis, P.; Beato, M.S.; Capua, I. Inactivation of Avian Influenza Viruses by Chemical Agents and Physical Conditions: A Review. Zoonoses Public Health 2007, 54, 51–68. [Google Scholar] [CrossRef]
- Meloni, D.; Franzoni, G.; Oggiano, A. Cell Lines for the Development of African Swine Fever Virus Vaccine Candidates: An Update. Vaccines 2022, 10, 707. [Google Scholar] [CrossRef] [PubMed]
- Krug, P.W.; Holinka, L.G.; O’Donnell, V.; Reese, B.; Sanford, B.; Fernandez-Sainz, I.; Gladue, D.P.; Arzt, J.; Rodriguez, L.; Risatti, G.R.; et al. The Progressive Adaptation of a Georgian Isolate of African Swine Fever Virus to Vero Cells Leads to a Gradual Attenuation of Virulence in Swine Corresponding to Major Modifications of the Viral Genome. J. Virol. 2015, 89, 2324–2332. [Google Scholar] [CrossRef]
- Rodríguez, J.M.; Salas, M.L. African swine fever virus transcription. Virus Res. 2013, 173, 15–28. [Google Scholar] [CrossRef] [PubMed]
- Sun, E.; Zhang, Z.; Wang, Z.; He, X.; Zhang, X.; Wang, L.; Wang, W.; Huang, L.; Xi, F.; Huangfu, H.; et al. Emergence and prevalence of naturally occurring lower virulent African swine fever viruses in domestic pigs in China in 2020. Sci. China Life Sci. 2021, 64, 752–765. [Google Scholar] [CrossRef]
- Hulseberg, C.E.; Fénéant, L.; Szymańska-de Wijs, K.M.; Kessler, N.P.; Nelson, E.A.; Shoemaker, C.J.; Schmaljohn, C.S.; Polyak, S.J.; White, J.M. Arbidol and Other Low-Molecular-Weight Drugs That Inhibit Lassa and Ebola Viruses Downloaded from. J. Virol. 2019, 93, e02185-18. [Google Scholar] [CrossRef]
- Rodríguez, J.M.; García-Escudero, R.; Salas, M.L.; Andrés, G. African Swine Fever Virus Structural Protein p54 Is Essential for the Recruitment of Envelope Precursors to Assembly Sites. J. Virol. 2004, 78, 4299–4313. [Google Scholar] [CrossRef]
- Vu, T.T.H.; Le, V.P.; Jeong, D.G.; Yeom, M.; Oh, J.; Kang, B.; Park, S.-K.; Song, D. Establishment of a p30-based lateral flow assay for African swine fever virus detection. J. Virol. Methods 2023, 322, 114823. [Google Scholar] [CrossRef]
- Alonso, C.; Miskin, J.; Hernáez, B.; Fernandez-Zapatero, P.; Soto, L.; Cantó, C.; Rodríguez-Crespo, I.; Dixon, L.; Escribano, J.M. African Swine Fever Virus Protein p54 Interacts with the Microtubular Motor Complex through Direct Binding to Light-Chain Dynein. J. Virol. 2001, 75, 9819–9827. [Google Scholar] [CrossRef]
- Chen, Y.; Guo, Y.; Chang, H.; Song, Z.; Wei, Z.; Huang, Z.; Zheng, Z.; Zhang, G.; Sun, Y. Brequinar inhibits African swine fever virus replication in vitro by activating ferroptosis. Virol. J. 2023, 20, 242. [Google Scholar] [CrossRef] [PubMed]
- Bossche, S.V.D.; Vandeplassche, E.; Ostyn, L.; Coenye, T.; Crabbé, A. Bacterial Interference with Lactate Dehydrogenase Assay Leads to an Underestimation of Cytotoxicity. Front. Cell. Infect. Microbiol. 2020, 10, 494. [Google Scholar] [CrossRef]
- Fotakis, G.; Timbrell, J.A. In vitro cytotoxicity assays: Comparison of LDH, neutral red, MTT and protein assay in hepatoma cell lines following exposure to cadmium chloride. Toxicol. Lett. 2006, 160, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Stockert, J.C.; Blázquez-Castro, A.; Cañete, M.; Horobin, R.W.; Villanueva, Á. MTT assay for cell viability: Intracellular localization of the formazan product is in lipid droplets. Acta Histochem. 2012, 114, 785–796. [Google Scholar] [CrossRef]
- Tanneberger, F.; El Wahed, A.A.; Fischer, M.; Blome, S.; Truyen, U. The Efficacy of Disinfection on Modified Vaccinia Ankara and African Swine Fever Virus in Various Forest Soil Types. Viruses 2021, 13, 2173. [Google Scholar] [CrossRef]
- Kowalczyk, A.; Guzik, K.; Slezak, K.; Dziedzic, J.; Rokita, H. Heat shock protein and heat shock factor 1 expression and localization in vaccinia virus infected human monocyte derived macrophages. J. Inflamm. 2005, 2, 12. [Google Scholar] [CrossRef]
- Liberti, R.; Colabella, C.; Anzalone, L.; Severi, G.; Paolo, A.; Casciari, C.; Casano, A.; Giammarioli, M.; Cagiola, M.; Feliziani, F.; et al. Expression of a recombinant ASFV P30 protein and production of monoclonal antibodies. Open Vet. J. 2023, 13, 358–364. [Google Scholar] [CrossRef]
- Duan, X.; Ru, Y.; Yang, W.; Ren, J.; Hao, R.; Qin, X.; Li, D.; Zheng, H. Research progress on the proteins involved in African swine fever virus infection and replication. Front. Immunol. 2022, 13, 947180. [Google Scholar] [CrossRef]
- Zheng, W.; Xi, J.; Zi, Y.; Wang, J.; Chi, Y.; Chen, M.; Zou, Q.; Tang, C.; Zhou, X. Stability of African swine fever virus genome under different environmental conditions. Vet. World 2023, 16, 2374–2381. [Google Scholar] [CrossRef] [PubMed]
- Hernáez, B.; Guerra, M.; Salas, M.L.; Andrés, G. African Swine Fever Virus Undergoes Outer Envelope Disruption, Capsid Disassembly and Inner Envelope Fusion before Core Release from Multivesicular Endosomes. PLoS Pathog. 2016, 12, e1005595. [Google Scholar] [CrossRef] [PubMed]

| Group | Mean (%) ± SD for Each Day | Total | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| DPI-1 | DPI-2 | DPI-3 | DPI-4 | DPI-5 | DPI-6 | Mean (%) | SD | CV (%) | |||
| ASFV (A) | 28.8 ± 1.7 | 30.3 ± 0.2 | 31 ± 1.3 | 41.9 ± 2.1 | 83.2 ± 6.6 | 86.3 ± 2 | 50.2 | 26.5 | 52.7 | ||
| Disinfectant (D) | 375× | 9.3 ± 0.5 | 16.7 ± 0.4 | 20.2 ± 1.5 | 30 ± 2.0 | 50.1 ± 5.4 | 70.3 ± 6.0 | 32.9 | 24.5 | 74.6 | |
| 275× | 29.1 ± 1.4 | 30 ± 3.3 | 37.2 ± 1.2 | 29.1 ± 2.2 | 37.2 ± 4.6 | 64.9 ± 1.5 | 37.6 | 12.4 | 33.1 | ||
| 175× | 48.3 ± 0.7 | 39.7 ± 0.7 | 26.1 ± 1.3 | 40.4 ± 0.9 | 61.7 ± 12.2 | 49.6 ± 4.5 | 44.6 | 11.1 | 24.9 | ||
| ASFV + Disinfectant (AD) | 375× | 6.4 ± 0.6 | 11.8 ± 0.4 | 13.6 ± 0.1 | 24.3 ± 0.3 | 46.6 ± 0.9 | 75.8 ± 3.1 | 29.4 | 27.3 | 92.9 | |
| 275× | 45.1 ± 0.6 | 41.0 ± 0.4 | 40.1 ± 0.6 | 43.8 ± 0.8 | 61.3 ± 3.1 | 69.7 ± 1.5 | 50.8 | 12.1 | 23.7 | ||
| 175× | 45.4 ± 3.1 | 44.1 ± 1.9 | 39.9 ± 2.1 | 45.0 ± 1.8 | 61.6 ± 2.3 | 72.8 ± 2.1 | 51.5 | 12.4 | 24.0 | ||
| Damage Scores (DPI 1~6) | Rapid Kit (p30), %(DPI 0, 6, 12) | FITC (p54) | LDH Cytotoxicity, % (DPI 1~6) | MTT Viability, % (DPI 6) | ||
|---|---|---|---|---|---|---|
| ASFV (A) | 1/2/3/3/4/5 | 40.5/41.4/79 | Pos | 28.8/30.3/31.0/41.9/83.2/86.3 | 35.9 | |
| ASFV + Disinfectant (AD) | 175× | 4/4/4/5/5/5 | 73.2/43.1/39.4 | Neg | 45.4/44.1/40.0/45.0/61.6/72.8 | 15.2 |
| 275× | 3/4/4/5/5/5 | 55.1/45.7/41.5 | Neg | 45.1/41.0/40.1/43.8/61.3/69.7 | 12.9 | |
| 375× | 0/0/1/2/3/3 | 43.9/47.1/43.6 | Neg | 6.4/11.8/13.6/24.3/46.6/75.8 | 56.9 | |
| Disinfectant (D) | 175× | 4/4/5/5/5/5 | - | - | 48.3/39.7/26.1/40.4/61.7/49.6 | 13.4 |
| 275× | 4/4/4/5/5/5 | - | - | 29.1/30.0/37.2/29.2/37.2/64.9 | 13.4 | |
| 375× | 2/3/3/3/4/4 | - | - | 9.3/16.7/20.2/30.7/50.1/70.3 | 14.6 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, S.; Shin, K.-S.; Kim, S.-J.; Joo, Y.Y.; Han, B.; Park, S.-H.; Ku, H.-O.; Jeong, W.; Park, C.-K. A Practical Framework for ASFV Disinfectant Evaluation: Differentiating Cytopathic Effects from Cytotoxicity via Integrated Analytical Methods. Pathogens 2025, 14, 451. https://doi.org/10.3390/pathogens14050451
Song S, Shin K-S, Kim S-J, Joo YY, Han B, Park S-H, Ku H-O, Jeong W, Park C-K. A Practical Framework for ASFV Disinfectant Evaluation: Differentiating Cytopathic Effects from Cytotoxicity via Integrated Analytical Methods. Pathogens. 2025; 14(5):451. https://doi.org/10.3390/pathogens14050451
Chicago/Turabian StyleSong, Sok, Kyu-Sik Shin, Su-Jeong Kim, Yong Yi Joo, Bokhee Han, So-Hee Park, Hyun-Ok Ku, Wooseog Jeong, and Choi-Kyu Park. 2025. "A Practical Framework for ASFV Disinfectant Evaluation: Differentiating Cytopathic Effects from Cytotoxicity via Integrated Analytical Methods" Pathogens 14, no. 5: 451. https://doi.org/10.3390/pathogens14050451
APA StyleSong, S., Shin, K.-S., Kim, S.-J., Joo, Y. Y., Han, B., Park, S.-H., Ku, H.-O., Jeong, W., & Park, C.-K. (2025). A Practical Framework for ASFV Disinfectant Evaluation: Differentiating Cytopathic Effects from Cytotoxicity via Integrated Analytical Methods. Pathogens, 14(5), 451. https://doi.org/10.3390/pathogens14050451







