Abstract
Neurocysticercosis (NCC) is a common parasitic disease of the central nervous system (CNS) in low- and middle-income countries. The infection is pleomorphic, caused by the larval form of the cestode, Taenia solium, and part of the heterogeneity of its clinical presentations is associated with the localization of the parasite within the CNS. Changes in the current epidemiological trends of NCC indicate that extra-parenchymal NCC is proportionally becoming more frequent. Extraparenchymal NCC is commonly accompanied by raised intracranial hypertension due to hydrocephalus, which is an emergency requiring cyst extirpation by surgical intervention to relieve the symptoms. Although less frequent, parenchymal cysts may also reach giant sizes requiring urgent surgical treatment. Finally, there is an advancement in the comprehension of the association between NCC and epilepsy—and patients with drug-resistant seizures are candidates for surgical treatment. In this narrative review, we summarize the present state of knowledge to update the current trends in the role of surgery in the treatment of NCC.
1. Introduction
Neurocysticercosis (NCC) is the most common parasitic disease of the central nervous system (CNS) in many developing countries, including regions of Latin America, sub-Saharan Africa, and southeast Asia [1,2,3]. It is caused by the ingestion of eggs from the adult tapeworm, Taenia solium, and is highly associated with poor sanitary conditions. Migratory flows and trips to endemic regions contribute to new cases in Europe and the United States [4,5,6].
After the larvae hatch from the eggs, they enter the systemic circulation and reach the CNS, where they can lodge in the brain parenchyma or in the cerebrospinal fluid (CSF) compartments (brain ventricles or the subarachnoid space). The parenchymal form of the disease (P-NCC) is the most common and it manifests in headaches, seizures, focal neurological deficits, or behavioral changes. P-NCC is highly responsive to medical treatment, and albendazole and praziquantel are commonly used cysticides, with the proven benefit of effectively destroying cysts. Apart from massive infections, P-NCC has a relatively benign course with an achievable cure [7,8]. However, as will be discussed in this review, surgery may be of utility particularly in cases of large cysts that produce important mass effect and in patients with NCC who have drug-resistant epilepsy.
Extraparenchymal NCC (EP-NCC) is associated with higher rates of morbidity and mortality [9,10,11]. In the CSF compartments, it causes meningitis, vasculitis (and, thereby, stroke), and raised intracranial pressure due to hydrocephalus. In addition, EP-NCC is less responsive to medical treatment: the concentration of albendazole sulfoxide varies widely among individuals and the CSF itself is a low-cellular compartment, allowing the parasites to be somehow hidden from the hosts’ immune surveillance [12,13,14].
For medical treatment, two anthelmintics have proved effective since the 1980s: albendazole and praziquantel. Their efficacy is similar, both being significantly more active in parenchymal disease than in extraparenchymal disease. Treatment is administered for 8 to 15 days, and the doses used are generally 15–30 mg/kg/day for albendazole and 50 mg/kg/day for praziquantel. It should be combined with corticoids, mainly in cases of extraparenchymal localization, to avoid inflammatory complications. The current NCC treatment guidelines are based on high-quality evidence-based recommendations for P-NCC. However, for EP-NCC, the strong recommendations are based on low-quality evidence [15]. Therefore, many questions remain relevant to the treatment of EP-NCC. In addition, EP-NCC is associated with conditions that may require surgical treatment, such as raised intracranial pressure (ICP) due to hydrocephalus. Based on the authors’ background, in this review, we analyze the relevance of NCC for both, clinicians and surgeons, the clinical presentations of the disease, and the different surgical modalities that can be employed for the treatment of hydrocephalus, cyst excision, and epilepsy.
2. Recent Evidence Regarding Epidemiological Trends in NCC
The heterogeneity of NCC is related to several factors such as the host’s immune system, genetic differences of the parasite across different geographical sites, and the number and localization of the cysts within the CNS [16,17].
Recently, we proposed that differences in infection pressure (the risk of a person ingesting T. solium eggs) could play a role in the disease’s heterogeneity as well [18]. Briefly, although it is difficult to assess the exact time between infection and the onset of symptoms, studies investigating NCC among people who travel from non-endemic countries to endemic regions (British soldiers on duty in India) or people from endemic countries who migrated to non-endemic countries (mainly Latins who migrated to United States), have allowed us to estimate that P-NCC has a latent period of 2–5 years, whereas EP-NCC may vary from 10 to 20 years [19,20]. Furthermore, patients with EP-NCC are older than those with P-NCC [11,21,22], which is probably related to a longer preclinical phase of EP-NCC [23]. Accordingly, the ratio of P-NCC cases to EP-NCC is declining in countries with decreasing disease incidence, such as Brazil, Mexico, and South Korea, although in countries with a still high endemicity of NCC, the proportion of EP-NCC is lower [18].
3. Pathophysiology of NCC
In the brain parenchyma, the cysts can initially remain undetected by the immune system. This phase corresponds to the vesicular appearance of cysts on brain imaging (clear fluid). The natural evolution of parenchymal cysts is degeneration accompanied by perilesional inflammation. The clear fluid is replaced by a jellylike material and the host organizes a granuloma to isolate the cysts, which finally calcify. This transition may be asymptomatic or may manifest in symptoms—most frequently, seizures—depending on the number and location of the cysts [24]. However, the inflammation is restricted to the brain parenchyma.
The evolution of cysts in the CSF compartments (the brain ventricles and the subarachnoid space) is different. Inflammation may take a longer time to occur because the CSF is a privileged site for the parasite [25,26]. Indeed, the low cellularity of the CSF and the blood-CSF barrier enable the cysts to remain relatively hidden from the host’s immune surveillance. In addition, the large space of the subarachnoid cisterns allows their growth without triggering an immune response. All these factors explain why patients with subarachnoid NCC have a long latent period from infection to the onset of symptoms.
Once the immune system recognizes the cysts’ antigens and activates to destroy the cysts, inflammatory reactions are initiated triggering the symptoms. Inflammation in the CSF compartments may damage the cranial nerves and the adjacent vessels (leading to vasculitis and, therefore, ischemic attacks), and disturb the CSF flow (either by fibrosis in the subarachnoid cisterns or ependymitis within the ventricles), leading to hydrocephalus. In addition, the cysts themselves may obstruct the CSF flow in the narrow spaces of the ventricles and manifest in hydrocephalus even in the absence of inflammation. Finally, hydrocephalus leads to an increase in ICP, with a high risk of death [27,28,29].
Inflammation and mechanical obstruction are the two mechanisms underlying hydrocephalus in NCC. Inflammation within the basal subarachnoid space impairs the normal CSF flow, resulting in the accumulation of CSF in the ventricles [30].
Recent advances in the understanding of the CSF dynamics, including the glymphatic system and a possible new meningeal layer, have questioned the classic understanding of the flow of CSF from the ventricles, passing through the subarachnoid space, to be absorbed in the arachnoid granulations juxtaposed to the venous sinuses [31,32]. Irrespective of the explanations, it is widely established that subarachnoid NCC causes arachnoiditis [28], which, in turn, impairs the CSF dynamics (either by blocking the classically described flow, or, possibly, by changing the vascular permeability to CSF exchanges).
Therefore, surgical intervention in NCC may target the treatment of hydrocephalus or the mechanical excision of cysts. The treatment of NCC-related epilepsy is also noteworthy and will be discussed later.
4. Treatment of Hydrocephalus in NCC
Hydrocephalus in NCC can have a chronic or acute presentation. The chronic presentation is less frequent and generally resembles normal pressure hydrocephalus, including apraxic gait, cognitive deficits, and urinary incontinence. In contrast, acute hydrocephalus is a life-threatening condition that requires emergency care [30]. Additionally, treating hydrocephalus needs to be prioritized over cyst management.
Conventionally, hydrocephalus is treated by ventricle-peritoneal (VP) shunts or endoscopic third ventriculostomy. The same options can be used for NCC-associated hydrocephalus.
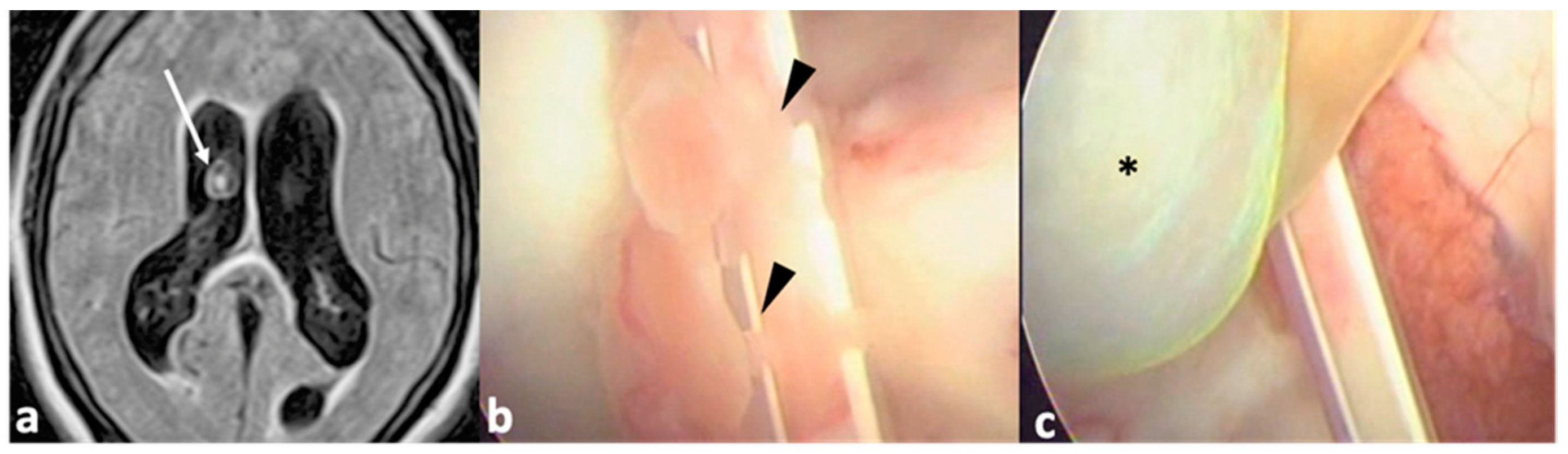
Studies on VP shunts for hydrocephalus in NCC have highly heterogeneous results. With respect to symptom resolution, rates of success vary from 20 to 90% [33,34], and the need for further surgical procedures varies from 10 to 100% [33,35]. Specifically, regarding shunt malfunction, the reported rates are approximately 50%, with a mean of 1.5 to 3 procedures per patient [36,37]. This variability can be explained by the differences in diagnostic tools used in each study. For example, older studies did not have the availability of magnetic resonance imaging (MRI), and the diagnosis was based on computed tomography (CT), which has a low sensitivity for the detection of EP-NCC [38,39]. A more recent case series was published with better outcomes, and it is possible that advances in neuroimaging played a role in this improvement [40]. Therefore, in the past, simply placing a VP shunt was insufficient to prevent the possible complications associated with the maintenance of viable cysts within the ventricles or subarachnoid space (Figure 1), such as inflammation and obstruction of the ventricles in locations other than the one in which the catheter was placed. This led to some authors advocating the use of postoperative anthelminthic drugs to promote higher longevity of the shunt [37,41]; though this association has not been demonstrated in recent studies [38]. Nonetheless, VP shunts have a high intrinsic risk of infection and malfunction, and the scenario is not different for NCC, especially because in NCC, inflammation within the CSF may persist irrespective of the shunt.

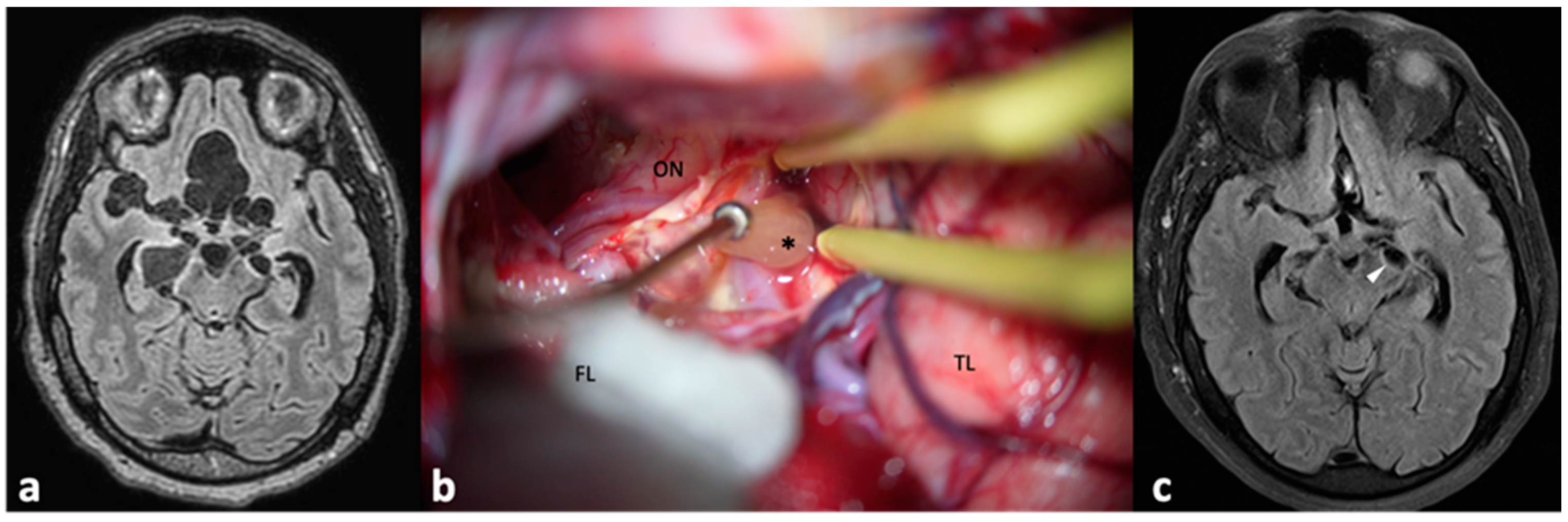
Figure 1.
Patient with hydrocephalus secondary to NCC. She was first managed by a VP shunt, which developed a malfunction a few months after insertion. A magnetic resonance imaging (a) showed a cyst (arrow) within the right ventricle. A new surgery (b) was performed for endoscopic removal of the cyst. During ventricle examination, choroid scars were identified near the previous catheter (arrowheads), which were the cause of the shunt malfunction. Finally, the cyst (c), * was successfully removed.
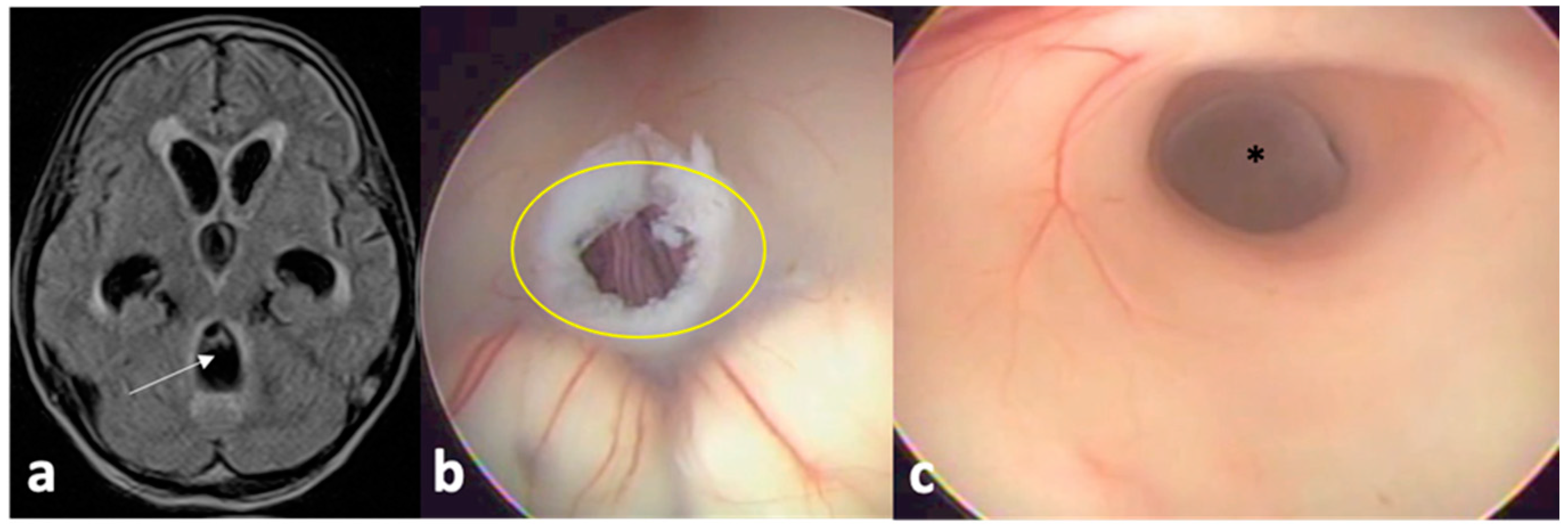
The introduction of endoscopic tools in neurosurgery benefited the management of hydrocephalus and NCC as well. With endoscopy, it is possible to perform the endoscopic third ventriculostomy (ETV, a communication of the third ventricle directly to the subarachnoid space), creating a bypass for the CSF flow, as well as to mechanically remove cysts inside the ventricles (Figure 2) [42,43]. Reports on ETV for hydrocephalus in NCC indicated significant improvement in symptom resolution (70–95%) and non-requirement of further surgical procedures (0–30%) [44,45,46]. In cases with significant inflammatory reactions, there is a risk of ETV failure due to the closure of the ostomy—and a subsequent VP shunt may be required. However, if neuro-endoscopy is used to remove ventricular cysts, third ventriculostomy should be attempted.
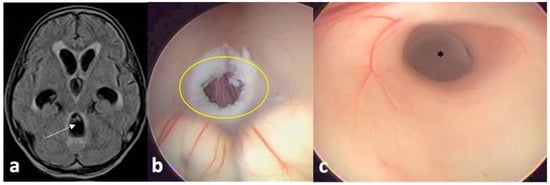
Figure 2.
MRI of a patient with hydrocephalus (a) secondary to a cysticercus occupying the fourth ventricle towards the Sylvius aqueduct. He underwent a conventional endoscopic third ventriculostomy (b) with communication of the third ventricle to the subarachnoid space; after rotating the endoscope, the cyst (*) could be identified within the aqueduct (c) with posterior mechanical removal.
Concomitantly, the introduction of volumetric MRI allowed for good visualization of cysts within the CSF compartments [38,47]. Thus, nowadays it is possible to determine the location of the cysts, and whether they can be endoscopically removed at the same operative time as the treatment of hydrocephalus. However, it is important to highlight that endoscopic management is not possible in all hospitals, especially in endemic countries, and therefore, efforts to improve VP shunt management must continue [48]. In addition, more robust evidence comparing VP shunt and neuro-endoscopy for NCC may help policy makers to update the required technologies. A systematic review comparing the techniques is in progress and shall bring useful data (PROSPERO database CRD42021264290).
5. Surgical Removal of Cysts
EP-NCC, unlike P-NCC, responds less positively to medical treatment. This fact may be related to the wide individual variation of albendazole metabolites in the CSF, the higher volume of parasites, the nature of the immune response in this compartment, and the use of corticosteroids to prevent complications during anthelminthic treatment [11,12,13,49]. The anthelminthic treatment may trigger the secretion of various antigens from the cysts, eliciting inflammatory responses that determine the symptoms and can be fatal [8,28]. Therefore, corticosteroids are of critical relevance for the treatment of inflammation [50]. However, the control of inflammation is also beneficial to the parasite, because the parasites may use corticosteroid metabolites for their own reproductive process, as shown with T. crassiceps (a T. solium analogue) in vitro, and probably also because of the immunosuppression associated with their use [51,52,53]. Consequently, many cycles and higher doses of anthelminthics may be necessary to effectively destroy intraventricular and subarachnoid cysts [54].
Another relevant issue is the mass effect that cysts may cause on the adjacent tissues such as cranial nerves, spinal roots, the spinal cord itself, and the narrow points of the CSF flow. The inflammatory reactions that may be triggered upon anthelminthic treatment can either initiate or deteriorate the previous compressive effect. For cranial nerves, there have been reported cases of visual loss, trigeminal pain, and facial nerve dysfunctions secondary to the compressive effects of cisternal cysts [55,56,57,58]. Cysts in the subarachnoid space of the spine can compress the spinal roots and the spinal cord. These cases can present with severe pain or progressive limb palsy [59,60]. Especially in cases of spinal cysts with spinal cord compression, there may be an urgent need for symptom relief and function restoration. In these cases, surgical removal of cysts is sometimes of primary importance, even though recovery may be limited due to inflammatory injury to the spinal cord or arachnoid adhesions [61].
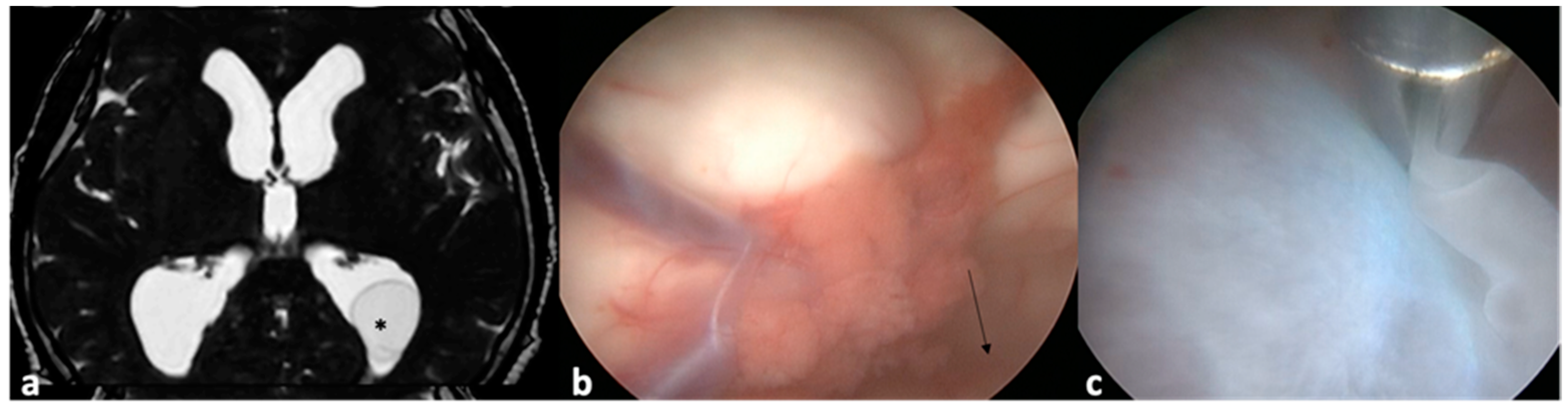
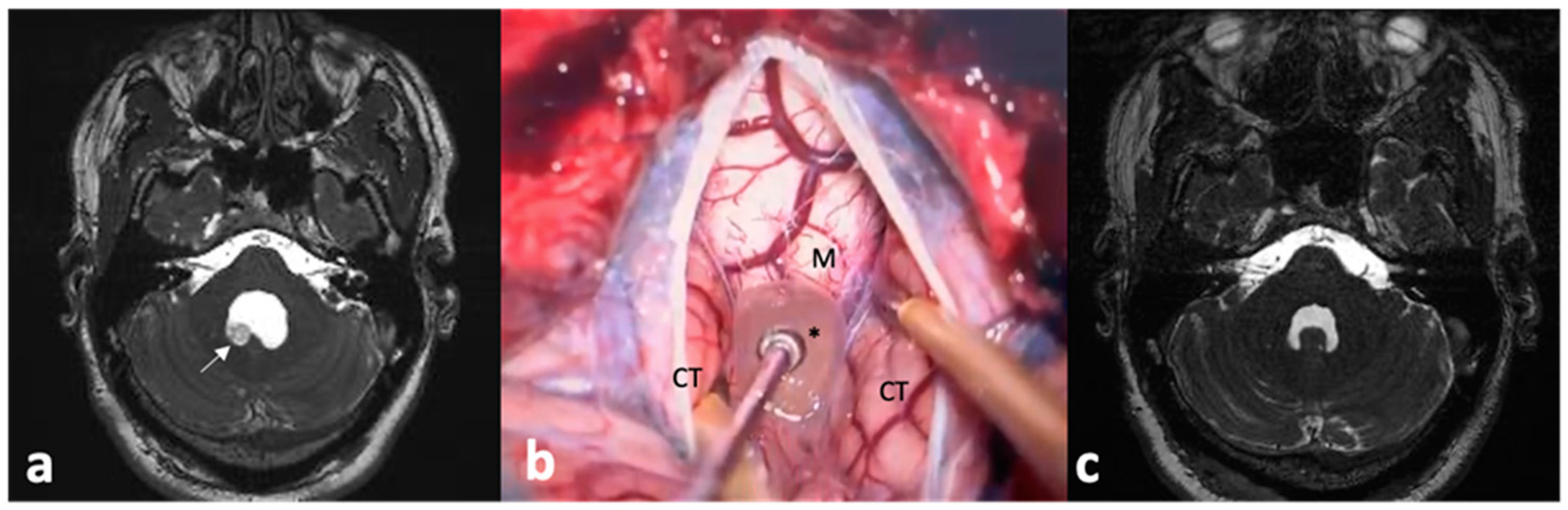
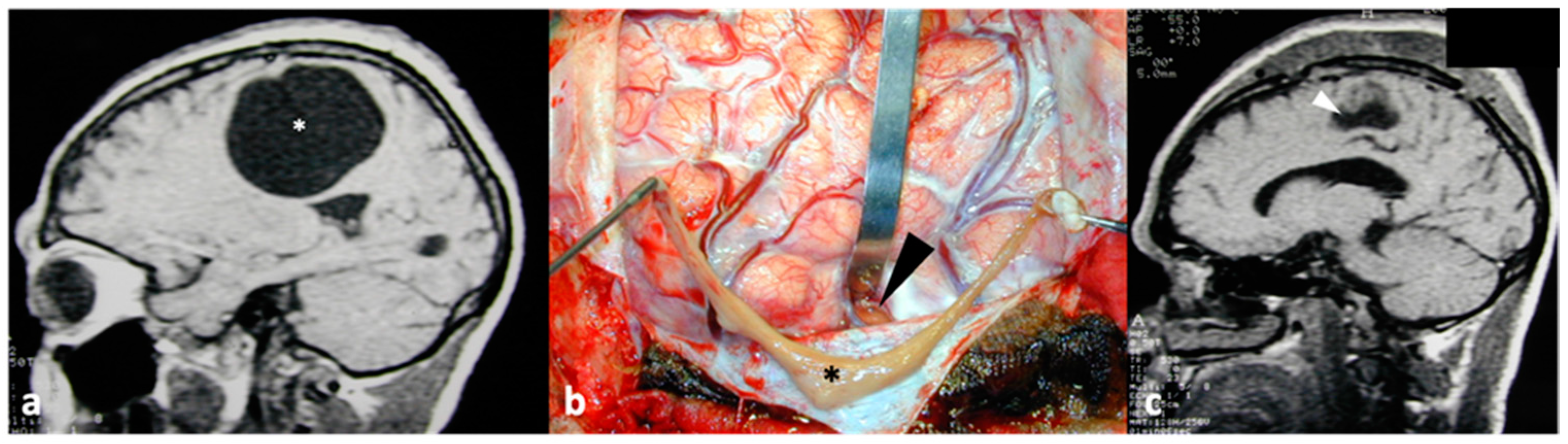
Intraventricular cysts can cause acute or progressive obstruction of CSF flow, leading to hydrocephalus [30]. As discussed earlier, hydrocephalus can be managed either by VP shunt or ETV. Endoscopic surgery has the advantage of being capable of treating hydrocephalus together with removing cysts [62]. Cysts lodged in the third and lateral ventricles can be managed by rigid endoscopes. Even when cysts cannot be directly visualized, continuous irrigation of the ventricle cavities can move cysts to the operative field for further removal (Figure 3) [63]. For cysts in the fourth ventricle, flexible endoscopes are an interesting option, even though they have lower availability and reduced image quality. Recently, rigid endoscopes using irrigation and pressure differences across the ventricles have been used to successfully remove fourth ventricle cysts [64,65]. Nevertheless, posterior fossa craniotomy followed by a telovelar approach is a relatively simple and effective route for fourth ventricle cysts [66] (Figure 4).

Figure 3.
In this MRI, a cyst (*) can be visualized within the occipital horn of the left lateral ventricle (a). The endoscope was introduced through a conventional burr-hole in the Kocher point until the lateral ventricle (b) and slightly turned posteriorly (arrow) towards the ventricular atrium. After continuous saline irrigation, the cyst moved from the occipital horn to the operative field and could be held with surgical forceps (c).
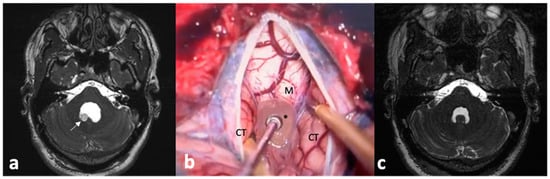
Figure 4.
(a) This MRI shows a cyst with a scolex (arrow) within the fourth ventricle. This cyst was removed by means of suboccipital craniotomy (b) with dissection of the cerebellar tonsils (CT) to expose the fourth ventricle, allowing for the removal of the cyst (*), M: medulla oblongata. Postoperative imaging (c) showed no residual lesion and recovery of the normal shape of the fourth ventricle.
Cisternal subarachnoid cysts can also be reached by means of simple pterional craniotomy with Sylvian fissure dissection (Figure 5). However, a key parameter prior to surgery indication is the assessment of adjacent inflammation. Contrast-enhancement of structures adjacent to the cysts is a signal of inflammation, and the surgical manipulation of these structures may cause significant damage to cranial nerves, vessels (with increased risk of postoperative ischemic lesions), and the brain parenchyma itself [66]. Therefore, the indication of surgical removal of subarachnoid cysts should be based on: (1) good preoperative imaging to discard inflammation surrounding the cysts, (2) adequate microsurgical armamentarium: a surgical microscope with depth of view control, micro scissors, microdissectors, and bipolar forceps, and (3) expertise in microsurgical skills and anatomical knowledge [67,68,69]. The lack of adequate preoperative workup and surgical tools and skills may add risk for the surgical treatment. Minimally invasive approaches with mini-craniotomy, stereotactic surgery, and endonasal endoscopic surgery can also be used with good results and few complications [70].
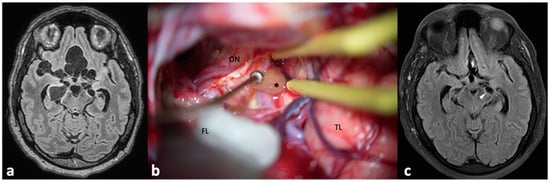
Figure 5.
Preoperative magnetic resonance imaging of a patient with multiple subarachnoid cysts (a) within several cisterns. Most of the cysts were successfully and uneventfully removed by means of a conventional pterional approach (b), ON: optic nerve, FL: frontal lobe, covered by cotton compress, TL: temporal lobe, *: a cyst in the carotid–oculomotor cistern. (c) Postoperative imaging showed a residual cyst (arrowhead, contralateral to the approach side) that was treated with albendazole.
Furthermore, the main advantage of surgical removal of the cysts is that their complete removal (even though it is not always possible) eliminates the need for postoperative cysticidal treatment and, sometimes, the need for permanent ventricle-peritoneal shunts for hydrocephalus [71]. The elimination of anthelminthic treatment has the advantage of reducing the risk of inflammation, and therefore, the need for corticosteroids, which have substantial side effects.
Another frequently mentioned concern in the surgical management of NCC is the risk of severe inflammation throughout the CNS in case of cyst rupture during surgery. Postoperative neurological deterioration has been attributed to ruptured cysts that would have released several antigenic components, causing subtle inflammation, dissemination of disease, or anaphylactic reaction [72,73]. However, there is currently a paucity of evidence supporting this hypothesis, and several authors’ experiences with surgical care of neurocysticercosis report no complications following cyst rupture. Considerable saline irrigation is suggested to avoid possible complications associated with cyst rupture [74,75,76].
Finally, it is relevant to mention that some parenchymal cysts may require surgical removal, particularly giant cysts with significant mass effects leading to raised intracranial pressure [77,78]. Patients with giant cysts may be admitted to emergency departments with signs of rapid neurological deterioration and, in these cases, surgical removal is more advisable than anthelminthic treatment, which could deteriorate symptoms (due to inflammation) and take several days to reduce the cyst size (Figure 6).
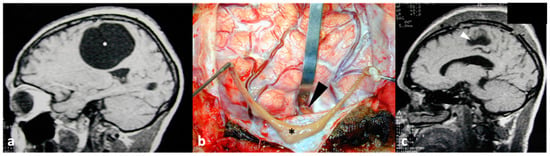
Figure 6.
Preoperative magnetic resonance imaging showing a giant parenchymal cysticercus ((a), *). The cyst (*) was entirely removed through minimum brain damage with a small corticectomy ((b), arrowhead). Postoperative imaging (c) showed only an area of encephalomalacia (arrowhead).
6. Surgical Treatment of NCC-Related Epilepsy
The association between NCC and epilepsy has been debated for many years [79,80]. It is typical to refer to NCC as the primary cause of late-onset epilepsy in endemic areas. However, more recent data on the etiology of first acute symptomatic seizures have shown that this may not be the case [81], even though, for NCC, seizures are the most common symptom [82]. Nonetheless, the findings of both, epilepsy and NCC, are not uncommon [83] and further research is needed to determine whether the association is casual or causal.
For surgical purposes, two conditions need to be discussed. First, it has been shown that even calcified cysts may have antigenic remnants that can eventually cause inflammation and trigger seizures [28,84,85]. In addition, the surrounding perilesional edema, gliosis, as well as neuronal and axonal damage may also be epileptogenic foci [86,87,88,89]. Generally, these cases are successfully managed medically with anti-epileptic drugs. For refractory cases, surgical indication is challenging and relies on clear electroencephalographic and neuroimaging evidence that the calcified cyst is the causative lesion for anti-epileptic drug resistance [90,91]. Importantly, intraoperative identification of calcified cysts may be difficult, especially if deeply seated. For lesionectomy in such cases, neuronavigation, focused ultrasound, intraoperative MRI, and electrocorticography are important tools for safer resection with better seizure outcomes [92,93,94].
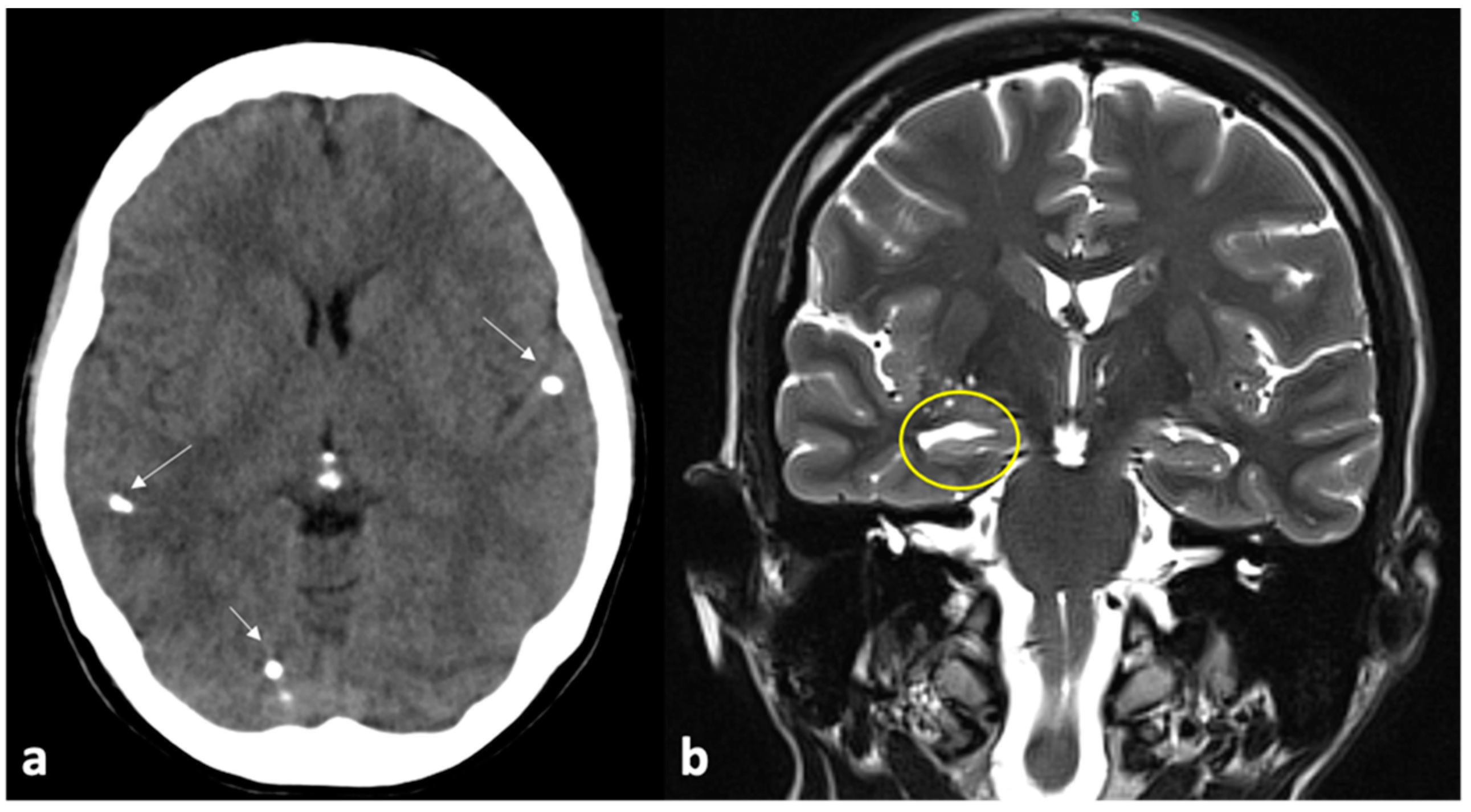
The second scenario is mesial temporal lobe epilepsy and hippocampus sclerosis (Figure 7). Debate persists whether the nature of this association is causal or casual. Many studies have investigated the relationship between NCC and hippocampus sclerosis and there are doubts whether hippocampus sclerosis results from recurrent seizures from local or distant focus or from chronic recurrent inflammation [95,96,97]. For example, status epilepticus from a distant lesion could lead to hippocampus injury; NCC can induce gliosis surrounding the hippocampus causing damage to it; antibodies against NCC could have a cross-reaction against hippocampal cells; the hippocampus being a highly sensitive structure of the brain, can be damaged secondary to systemic conditions (such as febrile seizures) [98,99,100,101]. Several hypotheses exist on the pathophysiologic mechanisms underlying NCC and mesial temporal lobe epilepsy [102]. Irrespective of the precise mechanisms, patients with temporal lobe epilepsy due to hippocampus sclerosis clearly benefit from surgical treatment [103]. The surgical procedure may vary from selective amygdalohippocampectomy (AH) to a combination of AH and anterior temporal lobectomy [104]. Moreover, for AH, there is disagreement regarding transsylvian or transcortical approaches [105]. According to the authors’ experience, there are significant disparities between selective AH and anterior temporal lobectomy in terms of seizure and cognitive results. [106,107,108]. However, for selective AH, there are differences with regard to postoperative visual defects, which are higher for transcortical rather than for transsylvian approaches [109]. Specifically for NCC and hippocampus sclerosis, there is a lack of studies comparing the techniques and approaches. Nonetheless, it appears reasonable that in cases of calcified lesions close but outside the hippocampus, a more extensive resection would be recommended.
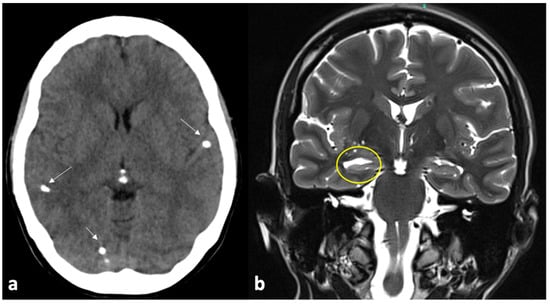
Figure 7.
This is the case of a patient with epilepsy who presented with multiple calcified lesions (arrows) on computed tomography (a). Magnetic resonance imaging showed sclerosis of the right hippocampus, clearly seen by means of an enlarged temporal horn ((b), yellow circle). After anterior temporal lobectomy and amygdalohippocampectomy, the patient had significant improvement in seizures.
7. Concluding Remarks
Despite the decrease in NCC globally, it remains a neglected disease with enormous consequences for patients and governments [110,111,112,113,114]. The accurate identification of NCC and its differential diagnosis remains important, especially in non-endemic and decreasing endemicity contexts [115]. In this regard, the role of neurosurgery in disease management remains relevant.
If hydrocephalus is present, endoscopic procedures have the advantage of treating hydrocephalus and removing intraventricular cysts. Attention should be paid to the identification of cysts attached to the ventricle walls; in these circumstances, extensive cyst removal may be detrimental and result in deficits. In addition, even after treatment for cysts (either by surgical removal or anthelminthic drugs) and third ventriculostomy, hydrocephalus may occur at a later stage, and a VP shunt may have to be performed. The surgical removal of the subarachnoid is feasible and may dismiss the use of postoperative anthelminthic drugs if all cysts are removed. However, for subarachnoid cysts surgery, it is mandatory to verify that there are no signals of active inflammation. As for endoscopic procedures, cysts attached to vascular or neural structures should not be removed. Research is needed to clarify the relationship between NCC and epilepsy. Irrespective of the precise pathophysiologic mechanisms, calcified cysts will rarely demand lesionectomy, whereas hippocampus sclerosis causing mesial temporal lobe epilepsy benefits from surgical treatment.
Author Contributions
P.T.H.F.: conceptualization, data management, funding acquisition, writing—draft. L.F.N.: writing—review and editing. A.F.: writing—review and editing. M.A.Z.: conceptualization, data management, writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP—22/03042-5). Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brasil (CAPES)—Finance Code 001.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Carpio, A.; Romo, M.L.; Parkhouse, R.M.; Short, B.; Dua, T. Parasitic Diseases of the Central Nervous System: Lessons for Clinicians and Policy Makers. Expert Rev. Neurother. 2016, 16, 401–414. [Google Scholar] [CrossRef]
- Ta, R.; Blond, B.N. The Prevalence of and Contributors to Neurocysticercosis in Endemic Regions. J. Neurol. Sci. 2022, 441, 120393. [Google Scholar] [CrossRef]
- Rodríguez-Rivas, R.; Flisser, A.; Norcia, L.F.; Hamamoto Filho, P.T.; Bonilla-Aldana, D.K.; Rodriguez-Morales, A.J.; Carpio, A.; Romo, M.L.; Fleury, A. Neurocysticercosis in Latin America: Current Epidemiological Situation Based on Official Statistics from Four Countries. PLoS Negl. Trop. Dis. 2022, 16, e0010652. [Google Scholar] [CrossRef] [PubMed]
- Abraham, A.; Schmidt, V.; Kaminski, M.; Stelzle, D.; De Meijere, R.; Bustos, J.; Sahu, P.S.; Garcia, H.H.; Bobić, B.; Cretu, C.; et al. Epidemiology and Surveillance of Human (Neuro)Cysticercosis in Europe: Is Enhanced Surveillance Required? Trop. Med. Int. Health 2020, 25, 566–578. [Google Scholar] [CrossRef] [PubMed]
- O’Neal, S.E.; Flecker, R.H. Hospitalization Frequency and Charges for Neurocysticercosis, United States, 2003–2012. Emerg. Infect. Dis. 2015, 21, 969–976. [Google Scholar] [CrossRef] [PubMed]
- Stelzle, D.; Abraham, A.; Kaminski, M.; Schmidt, V.; De Meijere, R.; Bustos, J.A.; Garcia, H.H.; Sahu, P.S.; Bobić, B.; Cretu, C.; et al. Clinical Characteristics and Management of Neurocysticercosis Patients: A Retrospective Assessment of Case Reports from Europe. J. Travel Med. 2023, 30, taac102. [Google Scholar] [CrossRef] [PubMed]
- Gonzales, I.; Rivera, J.T.; Garcia, H.H.; Cysticercosis Working Group in Peru. Pathogenesis of Taenia solium Taeniasis and Cysticercosis. Parasite Immunol. 2016, 38, 136–146. [Google Scholar] [CrossRef] [PubMed]
- Carpio, A.; Fleury, A.; Romo, M.L.; Abraham, R. Neurocysticercosis: The Good, the Bad, and the Missing. Expert Rev. Neurother. 2018, 18, 289–301. [Google Scholar] [CrossRef]
- Fleury, A.; Carrillo-Mezo, R.; Flisser, A.; Sciutto, E.; Corona, T. Subarachnoid Basal Neurocysticercosis: A Focus on the Most Severe Form of the Disease. Expert Rev. Anti. Infect. Ther. 2011, 9, 123–133. [Google Scholar] [CrossRef]
- Abanto, J.; Blanco, D.; Saavedra, H.; Gonzales, I.; Siu, D.; Pretell, E.J.; Bustos, J.A.; Garcia, H.H.; Cysticercosis Working Group in Peru. Mortality in Parenchymal and Subarachnoid Neurocysticercosis. Am. J. Trop. Med. Hyg. 2021, 105, 176–180. [Google Scholar] [CrossRef]
- Marcin Sierra, M.; Arroyo, M.; Cadena Torres, M.; Ramírez Cruz, N.; García Hernández, F.; Taboada, D.; Galicia Martínez, Á.; Govezensky, T.; Sciutto, E.; Toledo, A.; et al. Extraparenchymal Neurocysticercosis: Demographic, Clinicoradiological, and Inflammatory Features. PLoS Negl. Trop. Dis. 2017, 11, e0005646. [Google Scholar] [CrossRef] [PubMed]
- Osorio, R.; Carrillo-Mezo, R.; Romo, M.L.; Toledo, A.; Matus, C.; González-Hernández, I.; Jung, H.; Fleury, A. Factors Associated with Cysticidal Treatment Response in Extraparenchymal Neurocysticercosis. J. Clin. Pharmacol. 2019, 59, 548–556. [Google Scholar] [CrossRef] [PubMed]
- Takayanagui, O.M. Therapy for Neurocysticercosis. Expert Rev. Neurother. 2004, 4, 129–139. [Google Scholar] [CrossRef] [PubMed]
- González-Hernández, I.; Ruiz-Olmedo, M.I.; Cárdenas, G.; Jung-Cook, H. A Simple LC-MS/MS Method to Determine Plasma and Cerebrospinal Fluid Levels of Albendazole Metabolites (Albendazole Sulfoxide and Albendazole Sulfone) in Patients with Neurocysticercosis. Biomed. Chromatogr. 2012, 26, 267–272. [Google Scholar] [CrossRef] [PubMed]
- White, A.C., Jr.; Coyle, C.M.; Rajshekhar, V.; Singh, G.; Hauser, W.A.; Mohanty, A.; Garcia, H.H.; Nash, T.E. Diagnosis and Treatment of Neurocysticercosis: 2017 Clinical Practice Guidelines by the Infectious Diseases Society of America (IDSA) and the American Society of Tropical Medicine and Hygiene (ASTMH). Clin. Infect. Dis. 2018, 66, 1159–1163. [Google Scholar] [CrossRef] [PubMed]
- Fleury, A.; Escobar, A.; Fragoso, G.; Sciutto, E.; Larralde, C. Clinical Heterogeneity of Human Neurocysticercosis Results from Complex Interactions Among Parasite, Host and Environmental Factors. Trans. R. Soc. Trop. Med. Hyg. 2010, 104, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Ito, A.; Budke, C.M. Genetic Diversity of Taenia solium and Its Relation to Clinical Presentation of Cysticercosis. Yale J. Biol. Med. 2021, 94, 343–349. [Google Scholar] [PubMed]
- Hamamoto Filho, P.T.; Singh, G.; Winkler, A.S.; Carpio, A.; Fleury, A. Could Differences in Infection Pressure Be Involved in Cysticercosis Heterogeneity? Trends Parasitol. 2020, 36, 826–834. [Google Scholar] [CrossRef]
- Serpa, J.A.; Graviss, E.A.; Kass, J.S.; White, A.C., Jr. Neurocysticercosis in Houston, Texas: An Update. Medicine 2011, 90, 81–86. [Google Scholar] [CrossRef]
- Singh, G.; Sander, J.W. Historical Perspective: The British Contribution to the Understanding of Neurocysticercosis. J. Hist. Neurosci. 2019, 28, 332–344. [Google Scholar] [CrossRef]
- Nash, T.E.; O’Connell, E.M. Subarachnoid Neurocysticercosis: Emerging Concepts and Treatment. Curr. Opin. Infect. Dis. 2020, 33, 339–346. [Google Scholar] [CrossRef]
- Nateros, F.; Saenz, E.; Saavedra, H.; Gonzales, I.; Pretell, E.J.; Perez, E.; Castillo, Y.; Bustos, J.A.; Garcia, H.H.; Cysticercosis Working Group in Peru. Older Age in Subarachnoid Neurocysticercosis Reflects a Long Prepatent Period. Am. J. Trop. Med. Hyg. 2023, 108, 1188–1191. [Google Scholar] [CrossRef]
- Tellez-Arellano, C.A.; Kuschick-Fehér, J.; Romero-Gonzalez, F.G.; Fleury, A. Neurocysticercosis: The Duration of Its Preclinical Phase Relies on the Parasite Location. Trop. Med. Int. Health 2024. ahead of print. [Google Scholar] [CrossRef]
- Takayanagui, O.M.; Haes, T.M. Update on the Diagnosis and Management of Neurocysticercosis. Arq. Neuropsiquiatr. 2022, 80 (Suppl. S1), 296–306. [Google Scholar] [CrossRef]
- Muldoon, L.L.; Alvarez, J.I.; Begley, D.J.; Boado, R.J.; Del Zoppo, G.J.; Doolittle, N.D.; Engelhardt, B.; Hallenbeck, J.M.; Lonser, R.R.; Ohlfest, J.R.; et al. Immunologic Privilege in the Central Nervous System and the Blood-Brain Barrier. J. Cereb. Blood Flow Metab. 2013, 33, 13–21. [Google Scholar] [CrossRef]
- Engelhardt, B.; Ransohoff, R.M. Capture, Crawl, Cross: The T Cell Code to Breach the Blood-Brain Barriers. Trends Immunol. 2012, 33, 579–589. [Google Scholar] [CrossRef] [PubMed]
- White, A.C., Jr. Neurocysticercosis: Updates on Epidemiology, Pathogenesis, Diagnosis, and Management. Annu. Rev. Med. 2000, 51, 187–206. [Google Scholar] [CrossRef] [PubMed]
- Hamamoto Filho, P.T.; Fragoso, G.; Sciutto, E.; Fleury, A. Inflammation in Neurocysticercosis: Clinical Relevance and Impact on Treatment Decisions. Expert Rev. Anti. Infect. Ther. 2021, 19, 1503–1518. [Google Scholar] [CrossRef] [PubMed]
- Prodjinotho, U.F.; Lema, J.; Lacorcia, M.; Schmidt, V.; Vejzagic, N.; Sikasunge, C.; Ngowi, B.; Winkler, A.S.; Prazeres da Costa, C. Hosts. Host Immune Responses during Taenia Solium Neurocysticercosis Infection and Treatment. PLoS Negl. Trop. Dis. 2020, 14, e0008005. [Google Scholar] [CrossRef] [PubMed]
- Hamamoto Filho, P.T.; Zanini, M.A.; Fleury, A. Hydrocephalus in Neurocysticercosis: Challenges for Clinical Practice and Basic Research Perspectives. World Neurosurg. 2019, 126, 264–271. [Google Scholar] [CrossRef] [PubMed]
- Jessen, N.A.; Munk, A.S.; Lundgaard, I.; Nedergaard, M. The Glymphatic System: A Beginner’s Guide. Neurochem. Res. 2015, 40, 2583–2599. [Google Scholar] [CrossRef]
- Møllgård, K.; Beinlich, F.R.M.; Kusk, P.; Miyakoshi, L.M.; Delle, C.; Plá, V.; Hauglund, N.L.; Esmail, T.; Rasmussen, M.K.; Gomolka, R.S.; et al. A Mesothelium Divides the Subarachnoid Space into Functional Compartments. Science 2023, 379, 84–88. [Google Scholar] [CrossRef]
- Sotelo, J.; Rubalcava, M.A.; Gomez-Llata, S. A New Shunt for Hydrocephalus That Relies on CSF Production Rather Than on Ventricular Pressure: Initial Clinical Experiences. Surg. Neurol. 1995, 43, 324–331; discussion 331. [Google Scholar] [CrossRef] [PubMed]
- Bazan, R.; Hamamoto Filho, P.T.; Luvizutto, G.J.; Nunes, H.R.C.; Odashima, N.S.; Dos Santos, A.C.; Elias Júnior, J.; Zanini, M.A.; Fleury, A.; Takayanagui, O.M. Clinical Symptoms, Imaging Features and Cyst Distribution in the Cerebrospinal Fluid Compartments in Patients with Extraparenchymal Neurocysticercosis. PLoS Negl. Trop. Dis. 2016, 10, e0005115. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, L.; Almeida-Pinto, J.; Stocker, A.; Sampaio-Silva, M. Active Neurocysticercosis, Parenchymal and Extraparenchymal: A Study of 38 Patients. J. Neurol. 1993, 241, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Colli, B.O.; Carlotti, C.G., Jr.; Assirati, J.A., Jr.; Machado, H.R.; Valença, M.; Amato, M.C. Surgical Treatment of Cerebral Cysticercosis: Long-Term Results and Prognostic Factors. Neurosurg. Focus 2002, 12, e3. [Google Scholar] [CrossRef]
- Agapejev, S.; Pouza, A.F.; Bazan, R.; Faleiros, A.T. Clinical and Evolutive Aspects of Hydrocephalus in Neurocysticercosis. Arq. Neuropsiquiatr. 2007, 65, 674–680. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Carrillo Mezo, R.; Lara García, J.; Arroyo, M.; Fleury, A. Relevance of 3D Magnetic Resonance Imaging Sequences in Diagnosing Basal Subarachnoid Neurocysticercosis. Acta Trop. 2015, 152, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Citow, J.S.; Johnson, J.P.; McBride, D.Q.; Ammirati, M. Imaging Features and Surgery-Related Outcomes in Intraventricular Neurocysticercosis. Neurosurg. Focus 2002, 12, e6. [Google Scholar] [CrossRef] [PubMed]
- Cruz, L.; Pacheco, E.; Soto, W.; Cong, R.; Suastegui, R.; Moreno-Jimenez, S.; Fleury, A. Neurocysticercosis and Hydrocephalus: The Value of Ventriculoperitoneal Shunting in Its Management. Trans. R. Soc. Trop. Med. Hyg. 2023, 117, 773–779. [Google Scholar] [CrossRef]
- Kelley, R.; Duong, D.H.; Locke, G.E. Characteristics of Ventricular Shunt Malfunctions Among Patients with Neurocysticercosis. Neurosurgery 2002, 50, 757–761; discussion 761. [Google Scholar] [CrossRef]
- Husain, M.; Jha, D.K.; Rastogi, M.; Husain, N.; Gupta, R.K. Neuro-endoscopic Management of Intraventricular Neurocysticercosis (NCC). Acta Neurochir. 2007, 149, 341–346. [Google Scholar] [CrossRef]
- Torres-Corzo, J.G.; Tapia-Pérez, J.H.; Vecchia, R.R.; Chalita-Williams, J.C.; Sánchez-Aguilar, M.; Sánchez-Rodríguez, J.J. Endoscopic Management of Hydrocephalus Due to Neurocysticercosis. Clin. Neurol. Neurosurg. 2010, 112, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Proaño, J.V.; Torres-Corzo, J.; Rodríguez-Della Vecchia, R.; Guizar-Sahagun, G.; Rangel-Castilla, L. Intraventricular and Subarachnoid Basal Cisterns Neurocysticercosis: A Comparative Study Between Traditional Treatment Versus Neuroendoscopic Surgery. Child’s Nerv. Syst. 2009, 25, 1467–1475. [Google Scholar] [CrossRef] [PubMed]
- Goel, R.K.; Ahmad, F.U.; Vellimana, A.K.; Suri, A.; Chandra, P.S.; Kumar, R.; Sharma, B.S.; Mahapatra, A.K. Endoscopic Management of Intraventricular Neurocysticercosis. J. Clin. Neurosci. 2008, 15, 1096–1101. [Google Scholar] [CrossRef] [PubMed]
- Zhenye, L.; Chuzhong, L.; Xuyi, Z.; Songbai, G.; Peng, Z.; Jiwei, B.; Lei, C.; Xinsheng, W. Ventriculoscopic Approach for Intraventricular Neurocysticercosis: A Single Neurosurgical Center’s Experience. World Neurosurg. 2017, 107, 853–859. [Google Scholar] [CrossRef]
- do Amaral, L.L.; Ferreira, R.M.; da Rocha, A.J.; Ferreira, N.P. Neurocysticercosis: Evaluation with Advanced Magnetic Resonance Techniques and Atypical Forms. Top. Magn. Reson. Imaging 2005, 16, 127–144. [Google Scholar] [CrossRef] [PubMed]
- Enslin, J.M.N.; Thango, N.S.; Figaji, A.; Fieggen, G.A. Hydrocephalus in Low and Middle-Income Countries—Progress and Challenges. Neurol. India 2021, 69, S292–S297. [Google Scholar] [CrossRef] [PubMed]
- Cárdenas, G.; Carrillo-Mezo, R.; Jung, H.; Sciutto, E.; Hernandez, J.L.; Fleury, A. Subarachnoidal Neurocysticercosis Non-responsive to Cysticidal Drugs: A Case Series. BMC Neurol. 2010, 10, 16. [Google Scholar] [CrossRef] [PubMed]
- Hamamoto Filho, P.T.; Rodríguez-Rivas, R.; Fleury, A. Neurocysticercosis: A Review into Treatment Options, Indications, and Their Efficacy. Res. Rep. Trop. Med. 2022, 13, 67–79. [Google Scholar] [CrossRef]
- Toledo, A.; Osorio, R.; Matus, C.; Martinez Lopez, Y.; Ramirez Cruz, N.; Sciutto, E.; Fragoso, G.; Arauz, A.; Carrillo-Mezo, R.; Fleury, A. Human Extraparenchymal Neurocysticercosis: The Control of Inflammation Favors the Host…But Also the Parasite. Front. Immunol. 2018, 9, 2652. [Google Scholar] [CrossRef]
- Adalid-Peralta, L.; Rosas, G.; Arce-Sillas, A.; Bobes, R.J.; Cárdenas, G.; Hernández, M.; Trejo, C.; Meneses, G.; Hernández, B.; Estrada, K.; et al. Effect of Transforming Growth Factor-β upon Taenia solium and Taenia crassiceps Cysticerci. Sci. Rep. 2017, 7, 12345. [Google Scholar] [CrossRef]
- Romano, M.C.; Jiménez, P.; Miranda-Brito, C.; Valdez, R.A. Parasites and Steroid Hormones: Corticosteroid and Sex Steroid Synthesis, Their Role in the Parasite Physiology and Development. Front. Neurosci. 2015, 9, 224. [Google Scholar] [CrossRef] [PubMed]
- Nash, T.E.; O’Connell, E.M.; Hammoud, D.A.; Wetzler, L.; Ware, J.M.; Mahanty, S. Natural History of Treated Subarachnoid Neurocysticercosis. Am. J. Trop. Med. Hyg. 2020, 102, 78–89. [Google Scholar] [CrossRef]
- Cuellar-Hernandez, J.J.; Valadez-Rodriguez, A.; Olivas-Campos, R.; Tabera-Tarello, P.; Juan-Orta, D.S.; Segura-López, R.; Fleury, A. Intrasellar Cysticercosis Cyst Treated with a Transciliary Supraorbital Keyhole Approach—A Case Report. Surg. Neurol. Int. 2020, 11, 436. [Google Scholar] [CrossRef]
- Burgos-Sosa, E.; Bergna-Vazquez, P.; Mendizabal-Guerra, R.; Ayala-Arcipreste, A. Microsurgical and Endoscopic-Assisted Supraorbital Keyhole Approach for Intra-suprasellar Cysticercosis. Surg. Neurol. Int. 2023, 14, 328. [Google Scholar] [CrossRef] [PubMed]
- Hamamoto Filho, P.T.; Poliseli, G.B.; Oliveira, V.A.; Vital, R.B.; Ferreira Lima, M.M.; Bazan, R.; Zanini, M.A. Unusual Painful Trigeminal Neuropathy Caused by Racemose Neurocysticercosis. Pain Med. 2016, 17, 992–994. [Google Scholar] [CrossRef][Green Version]
- Yang, S.Y.; Vásquez, C.M.; Cysticercosis Working Group in Peru. Hemifacial Spasm Secondary to Arachnoiditis Due to Neurocysticercosis: Clinical Image. World Neurosurg. 2020, 143, 180–182. [Google Scholar] [CrossRef] [PubMed]
- Cárdenas, G.; Guevara-Silva, E.; Romero, F.; Ugalde, Y.; Bonnet, C.; Fleury, A.; Sciutto, E.; Nunes, C.M.; Soto-Hernández, J.L.; Shankar, S.K.; et al. Spinal Taenia solium Cysticercosis in Mexican and Indian Patients: A Comparison of 30-Year Experience in Two Neurological Referral Centers and Review of Literature. Eur. Spine J. 2016, 25, 1073–1081. [Google Scholar] [CrossRef]
- Colli, B.O.; Valença, M.M.; Carlotti, C.G., Jr.; Machado, H.R.; Assirati, J.A., Jr. Spinal Cord Cysticercosis: Neurosurgical Aspects. Neurosurg. Focus 2002, 12, e9. [Google Scholar] [CrossRef]
- Alsina, G.A.; Johnson, J.P.; McBride, D.Q.; Rhoten, P.R.; Mehringer, C.M.; Stokes, J.K. Spinal Neurocysticercosis. Neurosurg. Focus 2002, 12, e8. [Google Scholar] [CrossRef]
- Kaif, M.; Husain, M.; Ojha, B.K. Endoscopic Management of Intraventricular Neurocysticercosis. Turk. Neurosurg. 2019, 29, 59–65. [Google Scholar]
- Zymberg, S.T. Neurocysticercosis. World Neurosurg. 2013, 79, S24.e5–S24.e8. [Google Scholar] [CrossRef]
- Sharma, B.S.; Sawarkar, D.P.; Verma, S.K. Endoscopic Management of Fourth Ventricle Neurocysticercosis: Description of the New Technique in a Case Series of 5 Cases and Review of the Literature. World Neurosurg. 2019, 122, e647–e654. [Google Scholar] [CrossRef]
- Singh, S.; Marutirao, R.; Deora, H.; Das, K.K.; Bhaisora, K.S.; Sardhara, J.; Parab, A.; Mehrotra, A.; Srivastava, A.K.; Jaiswal, S.; et al. Endoscopic Route for Excision of Intraventricular Neurocysticercosis: Light At the End of the Tunnel. World Neurosurg. 2019, 125, e74–e81. [Google Scholar] [CrossRef] [PubMed]
- Nash, T.E.; Ware, J.M.; Mahanty, S. Intraventricular Neurocysticercosis: Experience and Long-Term Outcome from a Tertiary Referral Center in The United States. Am. J. Trop. Med. Hyg. 2018, 98, 1755–1762. [Google Scholar] [CrossRef]
- Ribas, G.C. The Cerebral Sulci and Gyri. Neurosurg. Focus 2010, 28, E2. [Google Scholar] [CrossRef] [PubMed]
- Tayebi Meybodi, A.; Borba Moreira, L.; Gandhi, S.; Preul, M.C.; Lawton, M.T. Sylvian Fissure Splitting Revisited: Applied Arachnoidal Anatomy and Proposition of a Live Practice Model. J. Clin. Neurosci. 2019, 61, 235–242. [Google Scholar] [CrossRef]
- Ribas, E.C.; da Róz, L.M.; Wen, H.T. Sylvian Fissure: Anatomical and a Clinical Correlations. In Brain Anatomy and Neurosurgical Approaches; Figueiredo, E.G., Rabelo, N.N., Welling, L.C., Eds.; Springer: Cham, Switzerland, 2023. [Google Scholar]
- Lines-Aguilar, W.W.; García, H.H.; Medina, J.E.; Saavedra, L.J.; Vela, E.; Lozano, M.; Vargas, J.; Cuya, C.; Heredia, D.; Apaza-Tintaya, A.; et al. Multimodal Minimally Invasive Surgery in the Treatment of Neurocysticercosis. Interdiscip. Neurosurg. Adv. Tech. Case Manag. 2024, 36, 101872. [Google Scholar] [CrossRef]
- Paiva, A.L.C.; Araujo, J.L.V.; Ferraz, V.R.; Lovato, R.M.; Pedrozo, C.A.G.; Aguiar, G.B.; Veiga, J.C.E. Surgical Treatment of Neurocysticercosis. Retrospective Cohort Study and an Illustrative Case Report. Sao Paulo Med. J. 2017, 135, 146–149. [Google Scholar] [CrossRef] [PubMed]
- Madrazo, I.; García-Rentería, J.A.; Sandoval, M.; López Vega, F.J. Intraventricular Cysticercosis. Neurosurgery 1983, 12, 148–152. [Google Scholar] [CrossRef]
- Colli, B.O.; Martelli, N.; Assirati, J.A., Jr.; Machado, H.R.; de Vergueiro Forjaz, S. Results of Surgical Treatment of Neurocysticercosis in 69 Cases. J. Neurosurg. 1986, 65, 309–315. [Google Scholar] [CrossRef]
- Gravori, T.; Steineke, T.; Bergsneider, M. Endoscopic Removal of Cisternal Neurocysticercal Cysts. Technical Note. Technical note. Neurosurg. Focus 2002, 12, e7. [Google Scholar] [CrossRef] [PubMed]
- Rangel-Castilla, L.; Serpa, J.A.; Gopinath, S.P.; Graviss, E.A.; Diaz-Marchan, P.; White, A.C., Jr. Contemporary Neurosurgical Approaches to Neurocysticercosis. Am. J. Trop. Med. Hyg. 2009, 80, 373–378. [Google Scholar] [CrossRef]
- Rajshekhar, V. Surgical Management of Neurocysticercosis. Int. J. Surg. 2010, 8, 100–104. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, P.P.; Gaikwad, S.B.; Garg, A.; Gupta, V.; Mishra, N.K.; Mehta, V.S. Giant Intraparenchymal Neurocysticercosis: Unusual MRI Findings. Neurol. India 2004, 52, 259–260. [Google Scholar]
- Peralta, I.; Ramírez, M.J.E.; Baldoncini, M.; Vicente, D.; Willingham, A.L.; Nurmukhametov, R.; Valdez, S.; Castillo, Y.; Encarnación, D.A.; Soler, I.J.R.; et al. Surgical Nuances of Giant Neurocysticercosis According to Intracranial Location in the Southwest Region of the Dominican Republic, Presentation of Cases, and Literature Review. Surg. Neurol. Int. 2023, 14, 242. [Google Scholar] [CrossRef] [PubMed]
- Carpio, A.; Romo, M.L. The Relationship Between Neurocysticercosis and Epilepsy: An Endless Debate. Arq. Neuropsiquiatr. 2014, 72, 383–390. [Google Scholar] [CrossRef]
- Tellez-Zenteno, J.F.; Hernandez-Ronquillo, L. Epidemiology of Neurocysticercosis and Epilepsy, Is Everything Described? Epilepsy Behav. 2017, 76, 146–150. [Google Scholar] [CrossRef]
- Carpio, A.; Salgado, C.; Di Capua, C.; Fleury, A.; Suastegui, R.; Giagante, B.; Aguilera, L.; Quijada, A.; Nunez, L.; Villanueva, M.; et al. Causes and Prognosis of Adults Experiencing a First Seizure in Adulthood: A Pilot Cohort Study Conducted in Five Countries in Latin America. Epilepsia Open 2024. ahead of print. [Google Scholar] [CrossRef]
- Carabin, H.; Ndimubanzi, P.C.; Budke, C.M.; Nguyen, H.; Qian, Y.; Cowan, L.D.; Stoner, J.A.; Rainwater, E.; Dickey, M. Clinical Manifestations Associated with Neurocysticercosis: A Systematic Review. PLoS Negl. Trop. Dis. 2011, 5, e1152. [Google Scholar] [CrossRef]
- Bruno, E.; Bartoloni, A.; Zammarchi, L.; Strohmeyer, M.; Bartalesi, F.; Bustos, J.A.; Santivañez, S.; García, H.H.; Nicoletti, A.; COHEMI Project Study Group. Epilepsy and Neurocysticercosis in Latin America: A Systematic Review and Meta-analysis. PLoS Negl. Trop. Dis. 2013, 7, e2480. [Google Scholar] [CrossRef]
- Nash, T.E.; Del Brutto, O.H.; Butman, J.A.; Corona, T.; Delgado-Escueta, A.; Duron, R.M.; Evans, C.A.; Gilman, R.H.; Gonzalez, A.E.; Loeb, J.A.; et al. Calcific Neurocysticercosis and Epileptogenesis. Neurology 2004, 62, 1934–1938. [Google Scholar] [CrossRef] [PubMed]
- Herrick, J.A.; Maharathi, B.; Kim, J.S.; Abundis, G.G.; Garg, A.; Gonzales, I.; Saavedra, H.; Bustos, J.A.; Garcia, H.H.; Loeb, J.A.; et al. Inflammation Is a Key Risk Factor for Persistent Seizures in Neurocysticercosis. Ann. Clin. Transl. Neurol. 2018, 5, 630–639. [Google Scholar] [CrossRef] [PubMed]
- de Souza, A.; Nalini, A.; Kovoor, J.M.; Yeshraj, G.; Siddalingaiah, H.S.; Thennarasu, K. Perilesional Gliosis Around Solitary Cerebral Parenchymal Cysticerci and Long-Term Seizure Outcome: A Prospective Study Using Serial Magnetization Transfer Imaging. Epilepsia 2011, 52, 1918–1927. [Google Scholar] [CrossRef] [PubMed]
- Mejia Maza, A.; Carmen-Orozco, R.P.; Carter, E.S.; Dávila-Villacorta, D.G.; Castillo, G.; Morales, J.D.; Mamani, J.; Gavídia, C.M.; Alroy, J.; Sterling, C.R.; et al. Axonal Swellings and Spheroids: A New Insight into the Pathology of Neurocysticercosis. Brain Pathol. 2019, 29, 425–436. [Google Scholar] [CrossRef] [PubMed]
- Nash, T. Edema Surrounding Calcified Intracranial Cysticerci: Clinical Manifestations, Natural History, and Treatment. Pathog. Glob. Health 2012, 106, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Coyle, C.M. New Insights into Calcified Neurocysticercosis: Closing the Knowledge Gap. Clin. Infect. Dis. 2021, 73, e2601–e2603. [Google Scholar] [CrossRef]
- Rathore, C.; Thomas, B.; Kesavadas, C.; Abraham, M.; Radhakrishnan, K. Calcified Neurocysticercosis Lesions and Antiepileptic Drug-Resistant Epilepsy: A Surgically Remediable Syndrome? Epilepsia 2013, 54, 1815–1822. [Google Scholar] [CrossRef]
- Singh, G.; Chowdhary, A.K. Epilepsy Surgery in Context of Neurocysticercosis. Ann. Indian Acad. Neurol. 2014, 17 (Suppl. S1), S65–S68. [Google Scholar] [CrossRef]
- Stone, S.S.; Rutka, J.T. Utility of Neuronavigation and Neuromonitoring in Epilepsy Surgery. Neurosurg. Focus 2008, 25, E17. [Google Scholar] [CrossRef]
- Roessler, K.; Hofmann, A.; Sommer, B.; Grummich, P.; Coras, R.; Kasper, B.S.; Hamer, H.M.; Blumcke, I.; Stefan, H.; Nimsky, C.; et al. Resective Surgery for Medically Refractory Epilepsy Using Intraoperative MRI and Functional Neuronavigation: The Erlangen Experience of 415 Patients. Neurosurg. Focus 2016, 40, E15. [Google Scholar] [CrossRef]
- Terra, V.C.; Volpon, M.; Machado, H.R. Intraoperative Monitoring in Epilepsy Surgery. In Intraoperative Monitoring; Verst, S.M., Barros, M.R., Maldaun, M.V.C., Eds.; Springer: Cham, Switzerland, 2022. [Google Scholar]
- Bianchin, M.M.; Velasco, T.R.; Santos, A.C.; Sakamoto, A.C. On the Relationship Between Neurocysticercosis and Mesial Temporal Lobe Epilepsy Associated with Hippocampal Sclerosis: Coincidence or a Pathogenic Relationship? Pathog. Glob. Health 2012, 106, 280–285. [Google Scholar] [CrossRef]
- Del Brutto, O.H.; Engel, J., Jr.; Eliashiv, D.S.; García, H.H. Update on Cysticercosis Epileptogenesis: The Role of the Hippocampus. Curr. Neurol. Neurosci. Rep. 2016, 16, 1. [Google Scholar] [CrossRef]
- Secchi, T.L.; Brondani, R.; Bragatti, J.A.; Bizzi, J.W.J.; Bianchin, M.M. Evaluating the Association of Calcified Neurocysticercosis and Mesial Temporal Lobe Epilepsy with Hippocampal Sclerosis in a Large Cohort of Patients with Epilepsy. Front. Neurol. 2021, 12, 769356. [Google Scholar] [CrossRef] [PubMed]
- Leite, J.P.; Terra-Bustamante, V.C.; Fernandes, R.M.; Santos, A.C.; Chimelli, L.; Sakamoto, A.C.; Assirati, J.A.; Takayanagui, O.M. Calcified Neurocysticercotic Lesions and Postsurgery Seizure Control in Temporal Lobe Epilepsy. Neurology 2000, 55, 1485–1491. [Google Scholar] [CrossRef] [PubMed]
- Bianchin, M.M.; Velasco, T.R.; Wichert-Ana, L.; Alexandre, V., Jr.; Araujo, D., Jr.; dos Santos, A.C.; Carlotti, C.G., Jr.; Takayanagui, O.M.; Sakamoto, A.C. Characteristics of Mesial Temporal Lobe Epilepsy Associated with Hippocampal Sclerosis plus Neurocysticercosis. Epilepsy Res. 2014, 108, 1889–1895. [Google Scholar] [CrossRef] [PubMed]
- Issa, N.P.; Sedler, M.J.; Del Brutto, V.J.; Darsan, E.; Milla, L.; Montes, J.; Zambrano, M.; Del Brutto, O.H. EEG Patterns in Patients with Calcified Neurocysticercosis with or Without Hippocampal Atrophy. J. Clin. Neurophysiol. 2018, 35, 332–338. [Google Scholar] [CrossRef]
- Espino, P.H.; Couper, R.G.; Burneo, J.G. An Update on Neurocysticercosis-Related Epilepsy. Clin. Neurol. Neurosurg. 2022, 213, 107139. [Google Scholar] [CrossRef]
- Bianchin, M.M.; Velasco, T.R.; Wichert-Ana, L.; Dos Santos, A.C.; Sakamoto, A.C. Understanding the Association of Neurocysticercosis and Mesial Temporal Lobe Epilepsy and Its Impact on the Surgical Treatment of Patients with Drug-Resistant Epilepsy. Epilepsy Behav. 2017, 76, 168–177. [Google Scholar] [CrossRef]
- Bianchin, M.M.; Velasco, T.R.; Coimbra, E.R.; Gargaro, A.C.; Escorsi-Rosset, S.R.; Wichert-Ana, L.; Terra, V.C.; Alexandre, V., Jr.; Araujo, D., Jr.; dos Santos, A.C.; et al. Cognitive and Surgical Outcome in Mesial Temporal Lobe Epilepsy Associated with Hippocampal Sclerosis plus Neurocysticercosis: A Cohort Study. PLoS ONE 2013, 8, e60949. [Google Scholar] [CrossRef]
- Singh, G.; Sander, J.W. Neurocysticercosis as a Probable Risk Factor for Hippocampal Sclerosis. Arq. Neuropsiquiatr. 2018, 76, 783–790. [Google Scholar] [CrossRef]
- Uda, H.; Uda, T.; Tanoue, Y.; Koh, S.; Kawashima, T.; Nakajo, K.; Ohata, K.; Goto, T. Comparison of the Keyhole Trans-middle Temporal Gyrus Approach and Transsylvian Approach for Selective Amygdalohippocampectomy: A Single-Center Experience. J. Clin. Neurosci. 2020, 81, 390–396. [Google Scholar] [CrossRef]
- Hu, W.H.; Zhang, C.; Zhang, K.; Meng, F.G.; Chen, N.; Zhang, J.G. Selective Amygdalohippocampectomy Versus Anterior Temporal Lobectomy in the Management of Mesial Temporal Lobe Epilepsy: A Meta-analysis of Comparative Studies. J. Neurosurg. 2013, 119, 1089–1097. [Google Scholar] [CrossRef]
- Xu, K.; Wang, X.; Guan, Y.; Zhao, M.; Zhou, J.; Zhai, F.; Wang, M.; Li, T.; Luan, G. Comparisons of the Seizure-Free Outcome and Visual Field Deficits Between Anterior Temporal Lobectomy and Selective Amygdalohippocampectomy: A Systematic Review and Meta-analysis. Seizure 2020, 81, 228–235. [Google Scholar] [CrossRef] [PubMed]
- Almeida, L.C.A.; Lobato, V.A.; Santos, M.D.C.V.; Moraes, A.C.; Costa, B.S. Surgical Treatment of Temporal Lobe Epilepsy: Comparative Results of Selective Amygdalohippocampectomy Versus Anterior Temporal Lobectomy from a Referral Center in Brazil. Arq. Neuropsiquiatr. 2023, 81, 647–655. [Google Scholar] [CrossRef] [PubMed]
- Vakharia, V.N.; Diehl, B.; Tisdall, M. Visual Field Defects in Temporal Lobe Epilepsy Surgery. Curr. Opin. Neurol. 2021, 34, 188–196. [Google Scholar] [CrossRef] [PubMed]
- Bhattarai, R.; Budke, C.M.; Carabin, H.; Proaño, J.V.; Flores-Rivera, J.; Corona, T.; Ivanek, R.; Snowden, K.F.; Flisser, A. Estimating the Non-monetary Burden of Neurocysticercosis in Mexico. PLoS Negl. Trop. Dis. 2012, 6, e1521. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.B.; Khatkar, M.S.; Gill, J.P.; Dhand, N.K. Estimation of the Health and Economic Burden of Neurocysticercosis in India. Acta Trop. 2017, 165, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Dupont, F.; Trevisan, C.; Moriku Kaducu, J.; Ovuga, E.; Schmidt, V.; Winkler, A.S.; Devleesschauwer, B. Human Health and Economic Impact of Neurocysticercosis in Uganda. Trop. Med. Int. Health 2022, 27, 99–109. [Google Scholar] [CrossRef]
- Mosley, I.A.; Li, T.; Zhao, X.; Huang, L.; Chen, X.; Liu, Y.; Chen, Z.; Duan, M.; Budke, C.M. Monetary Burden of Neurocysticercosis on a Hospitalized Population in Muli County, China. Acta Trop. 2023, 246, 106984. [Google Scholar] [CrossRef] [PubMed]
- White, A.C. Calcifications and the Global Burden of Neurocysticercosis: Not Just Rocks in Your Head. Clin. Infect. Dis. 2021, 73, e2604–e2606. [Google Scholar] [CrossRef] [PubMed]
- Delgado-García, G.; Méndez-Zurita, V.A.; Bayliss, L.; Flores-Rivera, J.; Fleury, A. Neurocysticercosis: Mimics and Chameleons. Pract. Neurol. 2019, 19, 88–95. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).