Heat Inactivation of Nipah Virus for Downstream Single-Cell RNA Sequencing Does Not Interfere with Sample Quality
Abstract
1. Introduction
2. Materials and Methods
2.1. Biosafety Statement
2.2. Immortalized Cells
2.3. Induced Pluripotent Stem Cell Directed Differentiation of Alveolar Type 2 Cells
2.4. Virus Propagation
2.5. Testing Virus Inactivation by Recovery Agent
2.6. Testing Virus Inactivation Using Heat
2.7. Testing Virus Inactivation following GEM Generation
2.8. Immunofluorescence Analysis
2.9. Limit of Detection Analysis
2.10. Single-Cell RNA Sequencing
2.11. scRNA-seq Data Analysis
3. Results
3.1. Chromium scRNA-seq Workflow and Identification of Potential Steps for Virus Inactivation
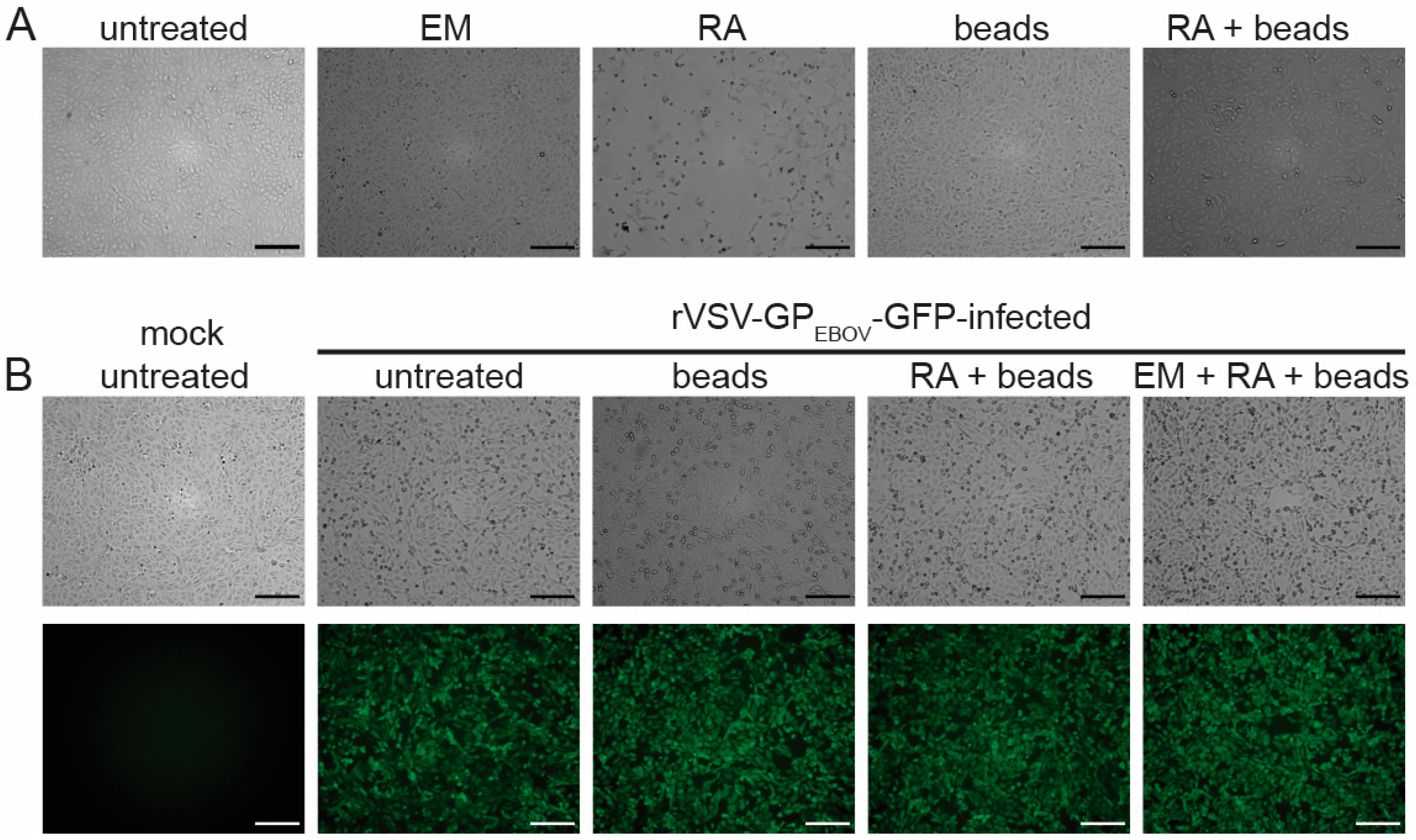
3.2. Neither Emulsion nor Recovery Agent Have Antiviral Activity
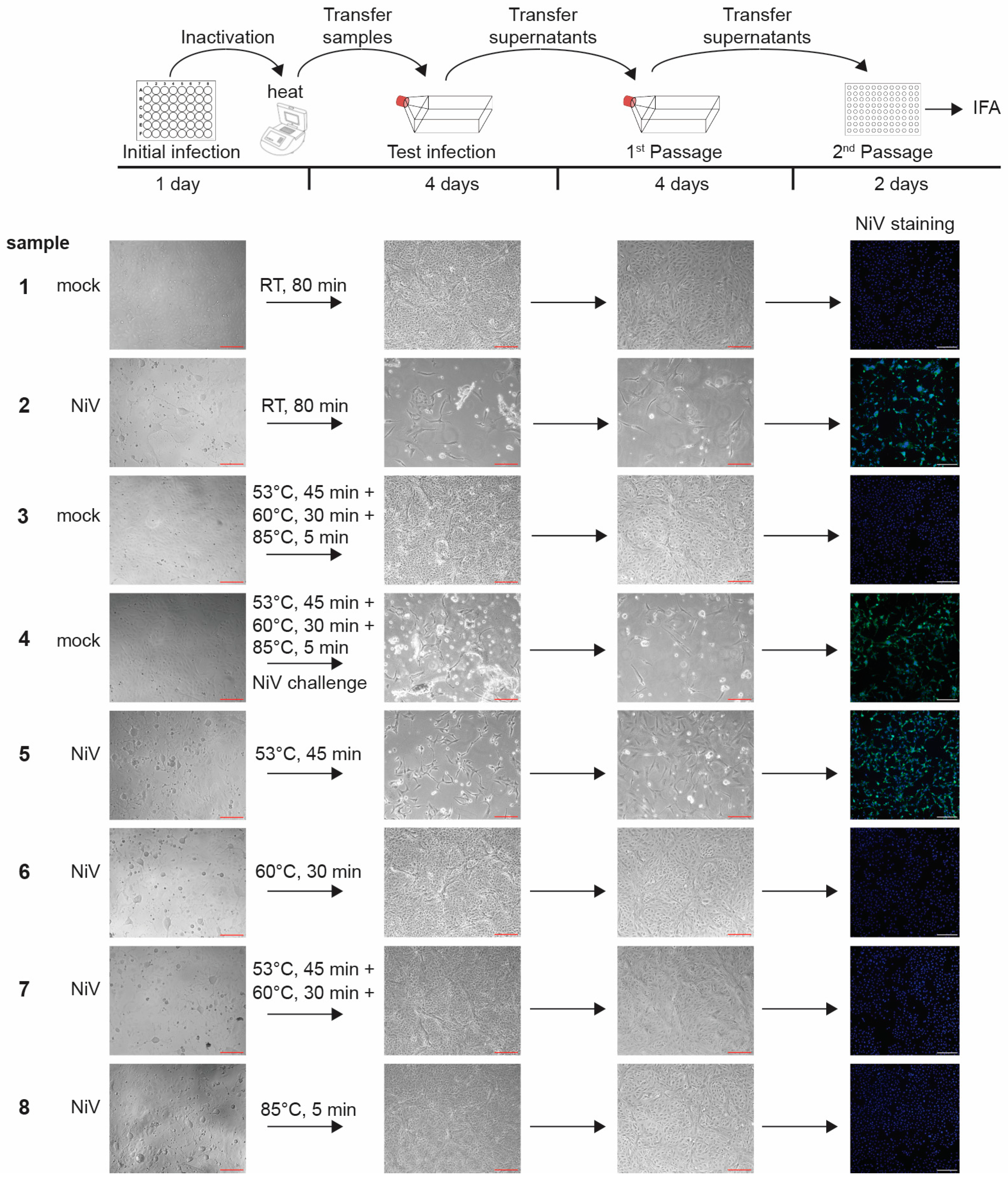
3.3. Inactivation of Nipah Virus-Infected Cells Using Heat
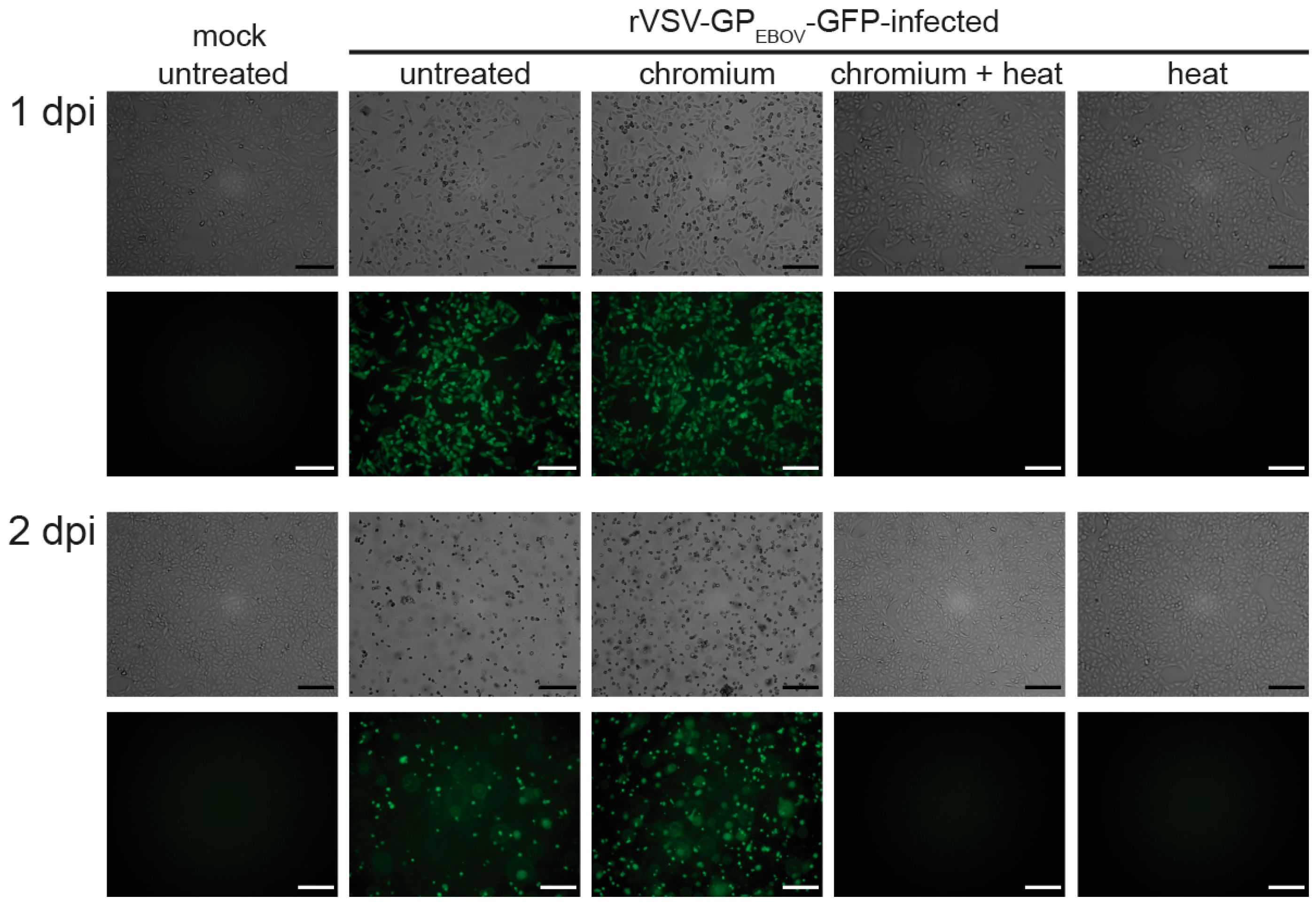
3.4. GEM Formation Does Not Affect Heat Inactivation
3.5. Limit of Detection Analysis for Nipah Virus
3.6. Heat Inactivation Does Not Affect Single-Cell RNA Sequencing Quality
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zou, J.; Li, J.; Zhong, X.; Tang, D.; Fan, X.; Chen, R. Liver in infections: A single-cell and spatial transcriptomics perspective. J. Biomed. Sci. 2023, 30, 53. [Google Scholar] [CrossRef] [PubMed]
- Speranza, E. Understanding virus-host interactions in tissues. Nat. Microbiol. 2023, 8, 1397–1407. [Google Scholar] [CrossRef] [PubMed]
- Ratnasiri, K.; Wilk, A.J.; Lee, M.J.; Khatri, P.; Blish, C.A. Single-cell RNA-seq methods to interrogate virus-host interactions. Semin. Immunopathol. 2023, 45, 71–89. [Google Scholar] [CrossRef] [PubMed]
- CDC; APHIS. Guidance on the Inactivation or Removal of Select Agents and Toxins or Future Use; 7 CFR Part 331, 9 CFR Part 121.3, 42 CFR Part 73.3; Centers for Disease Control and Prevention (CDC), Division of Select Agents and Toxins (DSAT): Atlanta, GA, USA; Animal and Plant Health Inspection Service (APHIS), Division of Agricultural Select Agents and Toxins (DASAT): Riverdale, MD, USA, 2018. [Google Scholar]
- Alles, J.; Karaiskos, N.; Praktiknjo, S.D.; Grosswendt, S.; Wahle, P.; Ruffault, P.L.; Ayoub, S.; Schreyer, L.; Boltengagen, A.; Birchmeier, C.; et al. Cell fixation and preservation for droplet-based single-cell transcriptomics. BMC Biol. 2017, 15, 44. [Google Scholar] [CrossRef] [PubMed]
- Phan, H.V.; van Gent, M.; Drayman, N.; Basu, A.; Gack, M.U.; Tay, S. High-throughput RNA sequencing of paraformaldehyde-fixed single cells. Nat. Commun. 2021, 12, 5636. [Google Scholar] [CrossRef]
- Bageritz, J.; Krausse, N.; Yousefian, S.; Leible, S.; Valentini, E.; Boutros, M. Glyoxal as alternative fixative for single cell RNA sequencing. G3 2023, 13, jkad160. [Google Scholar] [CrossRef]
- Chen, J.; Cheung, F.; Shi, R.; Zhou, H.; Lu, W.; Consortium, C.H.I. PBMC fixation and processing for Chromium single-cell RNA sequencing. J. Transl. Med. 2018, 16, 198. [Google Scholar] [CrossRef]
- Olejnik, J.; Leon, J.; Michelson, D.; Chowdhary, K.; Galvan-Pena, S.; Benoist, C.; Muhlberger, E.; Hume, A.J. Establishment of an Inactivation Method for Ebola Virus and SARS-CoV-2 Suitable for Downstream Sequencing of Low Cell Numbers. Pathogens 2023, 12, 342. [Google Scholar] [CrossRef]
- Reyes, M.; Vickers, D.; Billman, K.; Eisenhaure, T.; Hoover, P.; Browne, E.P.; Rao, D.A.; Hacohen, N.; Blainey, P.C. Multiplexed enrichment and genomic profiling of peripheral blood cells reveal subset-specific immune signatures. Sci. Adv. 2019, 5, eaau9223. [Google Scholar] [CrossRef]
- Lam, V.C.; Folkersen, L.; Aguilar, O.A.; Lanier, L.L. KLF12 Regulates Mouse NK Cell Proliferation. J. Immunol. 2019, 203, 981–989. [Google Scholar] [CrossRef]
- Luo, G.; Gao, Q.; Zhang, S.; Yan, B. Probing infectious disease by single-cell RNA sequencing: Progresses and perspectives. Comput. Struct. Biotechnol. J. 2020, 18, 2962–2971. [Google Scholar] [CrossRef] [PubMed]
- Rato, S.; Golumbeanu, M.; Telenti, A.; Ciuffi, A. Exploring viral infection using single-cell sequencing. Virus Res. 2017, 239, 55–68. [Google Scholar] [CrossRef] [PubMed]
- Olejnik, J.; Hume, A.J.; Ross, S.J.; Scoon, W.A.; Seitz, S.; White, M.R.; Slutzky, B.; Yun, N.E.; Muhlberger, E. Art of the Kill: Designing and Testing Viral Inactivation Procedures for Highly Pathogenic Negative Sense RNA Viruses. Pathogens 2023, 12, 952. [Google Scholar] [CrossRef] [PubMed]
- Scholte, F.E.M.; Kabra, K.B.; Tritsch, S.R.; Montgomery, J.M.; Spiropoulou, C.F.; Mores, C.N.; Harcourt, B.H. Exploring inactivation of SARS-CoV-2, MERS-CoV, Ebola, Lassa, and Nipah viruses on N95 and KN95 respirator material using photoactivated methylene blue to enable reuse. Am. J. Infect. Control 2022, 50, 863–870. [Google Scholar] [CrossRef]
- Kanev, K.; Roelli, P.; Wu, M.; Wurmser, C.; Delorenzi, M.; Pfaffl, M.W.; Zehn, D. Tailoring the resolution of single-cell RNA sequencing for primary cytotoxic T cells. Nat. Commun. 2021, 12, 569. [Google Scholar] [CrossRef]
- Picelli, S. Full-Length Single-Cell RNA Sequencing with Smart-seq2. Methods Mol. Biol. 2019, 1979, 25–44. [Google Scholar] [CrossRef]
- Picelli, S.; Faridani, O.R.; Bjorklund, A.K.; Winberg, G.; Sagasser, S.; Sandberg, R. Full-length RNA-seq from single cells using Smart-seq2. Nat. Protoc. 2014, 9, 171–181. [Google Scholar] [CrossRef]
- Trombetta, J.J.; Gennert, D.; Lu, D.; Satija, R.; Shalek, A.K.; Regev, A. Preparation of Single-Cell RNA-Seq Libraries for Next Generation Sequencing. Curr. Protoc. Mol. Biol. 2014, 107, 4.22.1–4.22.17. [Google Scholar] [CrossRef]
- Immunological Genome Project Ultra-Low-Input RNA-Seq (ULI RNA-Seq). Available online: https://www.immgen.org/Protocols/ImmGenULI_RNAseq_methods.pdf (accessed on 19 November 2022).
- Leon, J.; Michelson, D.A.; Olejnik, J.; Chowdhary, K.; Oh, H.S.; Hume, A.J.; Galvan-Pena, S.; Zhu, Y.; Chen, F.; Vijaykumar, B.; et al. A virus-specific monocyte inflammatory phenotype is induced by SARS-CoV-2 at the immune-epithelial interface. Proc. Natl. Acad. Sci. USA 2022, 119, e2116853118. [Google Scholar] [CrossRef]
- Hume, A.J.; Heiden, B.; Olejnik, J.; Suder, E.L.; Ross, S.; Scoon, W.A.; Bullitt, E.; Ericsson, M.; White, M.R.; Turcinovic, J.; et al. Recombinant Lloviu virus as a tool to study viral replication and host responses. PLoS Pathog. 2022, 18, e1010268. [Google Scholar] [CrossRef]
- Jacob, A.; Morley, M.; Hawkins, F.; McCauley, K.B.; Jean, J.C.; Heins, H.; Na, C.L.; Weaver, T.E.; Vedaie, M.; Hurley, K.; et al. Differentiation of Human Pluripotent Stem Cells into Functional Lung Alveolar Epithelial Cells. Cell Stem Cell 2017, 21, 472–488.e10. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Hume, A.J.; Abo, K.M.; Werder, R.B.; Villacorta-Martin, C.; Alysandratos, K.D.; Beermann, M.L.; Simone-Roach, C.; Lindstrom-Vautrin, J.; Olejnik, J.; et al. SARS-CoV-2 Infection of Pluripotent Stem Cell-Derived Human Lung Alveolar Type 2 Cells Elicits a Rapid Epithelial-Intrinsic Inflammatory Response. Cell Stem Cell 2020, 27, 962–973.e7. [Google Scholar] [CrossRef] [PubMed]
- Hekman, R.M.; Hume, A.J.; Goel, R.K.; Abo, K.M.; Huang, J.; Blum, B.C.; Werder, R.B.; Suder, E.L.; Paul, I.; Phanse, S.; et al. Actionable Cytopathogenic Host Responses of Human Alveolar Type 2 Cells to SARS-CoV-2. Mol. Cell 2020, 80, 1104–1122.e9. [Google Scholar] [CrossRef] [PubMed]
- Jacob, A.; Vedaie, M.; Roberts, D.A.; Thomas, D.C.; Villacorta-Martin, C.; Alysandratos, K.D.; Hawkins, F.; Kotton, D.N. Derivation of self-renewing lung alveolar epithelial type II cells from human pluripotent stem cells. Nat. Protoc. 2019, 14, 3303–3332. [Google Scholar] [CrossRef] [PubMed]
- Hurley, K.; Ding, J.; Villacorta-Martin, C.; Herriges, M.J.; Jacob, A.; Vedaie, M.; Alysandratos, K.D.; Sun, Y.L.; Lin, C.; Werder, R.B.; et al. Reconstructed Single-Cell Fate Trajectories Define Lineage Plasticity Windows during Differentiation of Human PSC-Derived Distal Lung Progenitors. Cell Stem Cell 2020, 26, 593–608.e8. [Google Scholar] [CrossRef]
- Hume, A.J.; Ames, J.; Rennick, L.J.; Duprex, W.P.; Marzi, A.; Tonkiss, J.; Muhlberger, E. Inactivation of RNA Viruses by Gamma Irradiation: A Study on Mitigating Factors. Viruses 2016, 8, 204. [Google Scholar] [CrossRef] [PubMed]
- Lei, C.; Yang, J.; Hu, J.; Sun, X. On the Calculation of TCID50 for Quantitation of Virus Infectivity. Virol. Sin. 2021, 36, 141–144. [Google Scholar] [CrossRef]
- Stuart, T.; Butler, A.; Hoffman, P.; Hafemeister, C.; Papalexi, E.; Mauck, W.M., 3rd; Hao, Y.; Stoeckius, M.; Smibert, P.; Satija, R. Comprehensive Integration of Single-Cell Data. Cell 2019, 177, 1888–1902.e21. [Google Scholar] [CrossRef]
- Hafemeister, C.; Satija, R. Normalization and variance stabilization of single-cell RNA-seq data using regularized negative binomial regression. Genome Biol. 2019, 20, 296. [Google Scholar] [CrossRef]
- McInnes, L.; Healy, J.; Melville, J. UMAP: Uniform Manifold Approximation and Projection for Dimension Reduction. arXiv 2020, arXiv:1802.03426. [Google Scholar] [CrossRef]
- Blondel, V.D.; Guillaume, J.-L.; Lambiotte, R.; Lefebvre, E. Fast unfolding of communities in large networks. J. Stat. Mech. Theory Exp. 2008, 2008, P10008. [Google Scholar] [CrossRef]
- Tirosh, I.; Izar, B.; Prakadan, S.M.; Wadsworth, M.H., 2nd; Treacy, D.; Trombetta, J.J.; Rotem, A.; Rodman, C.; Lian, C.; Murphy, G.; et al. Dissecting the multicellular ecosystem of metastatic melanoma by single-cell RNA-seq. Science 2016, 352, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Finak, G.; McDavid, A.; Yajima, M.; Deng, J.; Gersuk, V.; Shalek, A.K.; Slichter, C.K.; Miller, H.W.; McElrath, M.J.; Prlic, M.; et al. MAST: A flexible statistical framework for assessing transcriptional changes and characterizing heterogeneity in single-cell RNA sequencing data. Genome Biol. 2015, 16, 278. [Google Scholar] [CrossRef] [PubMed]
- Osborn, R.M.; Leach, J.; Zanche, M.; Ashton, J.M.; Chu, C.; Thakar, J.; Dewhurst, S.; Rosenberger, S.; Pavelka, M.; Pryhuber, G.S.; et al. Preparation of noninfectious scRNAseq samples from SARS-CoV-2-infected epithelial cells. PLoS ONE 2023, 18, e0281898. [Google Scholar] [CrossRef]
- Welch, S.R.; Davies, K.A.; Buczkowski, H.; Hettiarachchi, N.; Green, N.; Arnold, U.; Jones, M.; Hannah, M.J.; Evans, R.; Burton, C.; et al. Analysis of Inactivation of SARS-CoV-2 by Specimen Transport Media, Nucleic Acid Extraction Reagents, Detergents, and Fixatives. J. Clin. Microbiol. 2020, 58, e01713-20. [Google Scholar] [CrossRef]
- Kenney, D.J.; O’Connell, A.K.; Turcinovic, J.; Montanaro, P.; Hekman, R.M.; Tamura, T.; Berneshawi, A.R.; Cafiero, T.R.; Al Abdullatif, S.; Blum, B.; et al. Humanized mice reveal a macrophage-enriched gene signature defining human lung tissue protection during SARS-CoV-2 infection. Cell Rep. 2022, 39, 110714. [Google Scholar] [CrossRef]
- Wang, X.; Yu, L.; Wu, A.R. The effect of methanol fixation on single-cell RNA sequencing data. BMC Genom. 2021, 22, 420. [Google Scholar] [CrossRef]
- Vallejo, A.F.; Harvey, K.; Wang, T.; Wise, K.; Butler, L.M.; Polo, J.; Plummer, J.; Swarbrick, A.; Martelotto, L.G. snPATHO-seq: Unlocking the FFPE archives for single nucleus RNA profiling. bioRxiv 2022. [Google Scholar] [CrossRef]
- Chung, H.; Melnikov, A.; McCabe, C.; Drokhlyansky, E.; Wittenberghe, N.V.; Magee, E.M.; Waldman, J.; Spira, A.; Chen, F.; Mazzilli, S.; et al. SnFFPE-Seq: Towards scalable single nucleus RNA-Seq of formalin-fixed paraffin-embedded (FFPE) tissue. bioRxiv 2022. [Google Scholar] [CrossRef]
- Attar, M.; Sharma, E.; Li, S.; Bryer, C.; Cubitt, L.; Broxholme, J.; Lockstone, H.; Kinchen, J.; Simmons, A.; Piazza, P.; et al. A practical solution for preserving single cells for RNA sequencing. Sci. Rep. 2018, 8, 2151. [Google Scholar] [CrossRef]
- Xu, Z.; Zhang, T.; Chen, H.; Zhu, Y.; Lv, Y.; Zhang, S.; Chen, J.; Chen, H.; Yang, L.; Jiang, W.; et al. High-throughput single nucleus total RNA sequencing of formalin-fixed paraffin-embedded tissues by snRandom-seq. Nat. Commun. 2023, 14, 2734. [Google Scholar] [CrossRef] [PubMed]
- Haddock, E.; Feldmann, F.; Feldmann, H. Effective Chemical Inactivation of Ebola Virus. Emerg. Infect. Dis. 2016, 22, 1292–1294. [Google Scholar] [CrossRef] [PubMed]
- Feldmann, F.; Shupert, W.L.; Haddock, E.; Twardoski, B.; Feldmann, H. Gamma Irradiation as an Effective Method for Inactivation of Emerging Viral Pathogens. Am. J. Trop. Med. Hyg. 2019, 100, 1275–1277. [Google Scholar] [CrossRef] [PubMed]
- Alfson, K.J.; Griffiths, A. Development and Testing of a Method for Validating Chemical Inactivation of Ebola Virus. Viruses 2018, 10, 126. [Google Scholar] [CrossRef] [PubMed]
- Boytz, R.; Seitz, S.; Gaudiano, E.; Patten, J.J.; Keiser, P.T.; Connor, J.H.; Sharpe, A.H.; Davey, R.A. Inactivation of Ebola Virus and SARS-CoV-2 in Cell Culture Supernatants and Cell Pellets by Gamma Irradiation. Viruses 2022, 15, 43. [Google Scholar] [CrossRef] [PubMed]
- Widerspick, L.; Vazquez, C.A.; Niemetz, L.; Heung, M.; Olal, C.; Bencsik, A.; Henkel, C.; Pfister, A.; Brunetti, J.E.; Kucinskaite-Kodze, I.; et al. Inactivation Methods for Experimental Nipah Virus Infection. Viruses 2022, 14, 1052. [Google Scholar] [CrossRef]
- Smither, S.J.; Weller, S.A.; Phelps, A.; Eastaugh, L.; Ngugi, S.; O’Brien, L.M.; Steward, J.; Lonsdale, S.G.; Lever, M.S. Buffer AVL Alone Does Not Inactivate Ebola Virus in a Representative Clinical Sample Type. J. Clin. Microbiol. 2015, 53, 3148–3154. [Google Scholar] [CrossRef]
- Sturdevant, G.L.; Meade-White, K.D.; Best, S.M.; Speranza, E. Preservation of scRNA-Seq libraries using existing BSL-4 inactivation protocols. Pathogens, 2024; submitted. [Google Scholar]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hume, A.J.; Olejnik, J.; White, M.R.; Huang, J.; Turcinovic, J.; Heiden, B.; Bawa, P.S.; Williams, C.J.; Gorham, N.G.; Alekseyev, Y.O.; et al. Heat Inactivation of Nipah Virus for Downstream Single-Cell RNA Sequencing Does Not Interfere with Sample Quality. Pathogens 2024, 13, 62. https://doi.org/10.3390/pathogens13010062
Hume AJ, Olejnik J, White MR, Huang J, Turcinovic J, Heiden B, Bawa PS, Williams CJ, Gorham NG, Alekseyev YO, et al. Heat Inactivation of Nipah Virus for Downstream Single-Cell RNA Sequencing Does Not Interfere with Sample Quality. Pathogens. 2024; 13(1):62. https://doi.org/10.3390/pathogens13010062
Chicago/Turabian StyleHume, Adam J., Judith Olejnik, Mitchell R. White, Jessie Huang, Jacquelyn Turcinovic, Baylee Heiden, Pushpinder S. Bawa, Christopher J. Williams, Nickolas G. Gorham, Yuriy O. Alekseyev, and et al. 2024. "Heat Inactivation of Nipah Virus for Downstream Single-Cell RNA Sequencing Does Not Interfere with Sample Quality" Pathogens 13, no. 1: 62. https://doi.org/10.3390/pathogens13010062
APA StyleHume, A. J., Olejnik, J., White, M. R., Huang, J., Turcinovic, J., Heiden, B., Bawa, P. S., Williams, C. J., Gorham, N. G., Alekseyev, Y. O., Connor, J. H., Kotton, D. N., & Mühlberger, E. (2024). Heat Inactivation of Nipah Virus for Downstream Single-Cell RNA Sequencing Does Not Interfere with Sample Quality. Pathogens, 13(1), 62. https://doi.org/10.3390/pathogens13010062









