HTLV-1 Proviral Load in Vaginal Fluid Correlates with Levels in Peripheral Blood Mononuclear Cells
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Study Design
2.2. Ethical Approval
2.3. Sample Collection
2.4. Sample Analysis
2.5. Statistical Evaluations
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Poiesz, B.J.; Ruscetti, F.W.; Gazdar, A.F.; Bunn, P.A.; Minna, J.D.; Gallo, R.C. Detection and isolation of type C retrovirus particles from fresh and cultured lymphocytes of a patient with cutaneous T-cell lymphoma. Proc. Natl. Acad. Sci. USA 1980, 77, 7415–7419. [Google Scholar] [CrossRef]
- Gessain, A.; Cassar, O. Epidemiological Aspects and World Distribution of HTLV-1 Infection. Front. Microbiol. 2012, 3, 388. [Google Scholar] [CrossRef]
- Dourado, I.; Alcantara, L.C.; Barreto, M.L.; da Gloria Teixeira, M.; Galvão-Castro, B. HTLV-I in the general population of Salvador, Brazil: A city with African ethnic and sociodemographic characteristics. J. Acquir. Immune Defic. Syndr. 2003, 34, 527–531. [Google Scholar] [CrossRef] [PubMed]
- Nunes, D.; Boa-Sorte, N.; Grassi, M.F.; Taylor, G.P.; Teixeira, M.G.; Barreto, M.L.; Dourado, I.; Galvão-Castro, B. HTLV-1 is predominantly sexually transmitted in Salvador, the city with the highest HTLV-1 prevalence in Brazil. PLoS ONE 2017, 12, e0171303. [Google Scholar] [CrossRef] [PubMed]
- Nakano, S.; Ando, Y.; Ichijo, M.; Moriyama, I.; Saito, S.; Sugamura, K.; Hinuma, Y. Search for possible routes of vertical and horizontal transmission of adult T-cell leukemia virus. GANN Jpn. J. Cancer Res. 1984, 75, 1044–1045. [Google Scholar]
- Pereira, C.C.C.; La-Roque, D.G.d.L.; Albuquerque, R.D.S.; Silva, I.C.; Covre, L.D.S.C.; Nobre, A.F.S.; Reis, M.D.N.L.D.; de Assis, I.M.; de Souza, J.D.; de Moraes, S.S.; et al. Human T-lymphotropic virus (HTLV) research in cervical-vaginal discharge samples from women, in Belém, Pará, Brazil. Res. Soc. Dev. 2021, 10, e9410413867. [Google Scholar] [CrossRef]
- Kajiyama, W.; Kashiwagi, S.; Ikematsu, H.; Hayashi, J.; Nomura, H.; Okochi, K. Intrafamilial transmission of adult T cell leukemia virus. J. Infect. Dis. 1986, 154, 851–857. [Google Scholar] [CrossRef]
- Roucoux, D.F.; Wang, B.; Smith, D.; Nass, C.C.; Smith, J.; Hutching, S.T.; Newman, B.; Lee, T.H.; Chafets, D.M.; Murphy, E.L.; et al. A prospective study of sexual transmission of human T lymphotropic virus (HTLV)-I and HTLV-II. J. Infect. Dis. 2005, 191, 1490–1497. [Google Scholar] [CrossRef] [PubMed]
- Murphy, E.L. The clinical epidemiology of human T-lymphotropic virus type II (HTLV-II). JAIDS J. Acquir. Immune Defic. Syndr. 1996, 13, S215–S219. [Google Scholar] [CrossRef]
- Manns, A.; Hisada, M.; La Grenade, L. Human T-lymphotropic virus type I infection. Lancet 1999, 353, 1951–1958. [Google Scholar] [CrossRef]
- Yasunaga, J.-I.; Sakai, T.; Nosaka, K.; Etoh, K.-I.; Tamiya, S.; Koga, S.; Mita, S.; Uchino, M.; Mitsuya, H.; Matsuoka, M. Impaired production of naive T lymphocytes in human T-cell leukemia virus type I-infected individuals: Its implications in the immunodeficient state. Blood 2001, 97, 3177–3183. [Google Scholar] [CrossRef]
- Pique, C.; Jones, K.S. Pathways of cell-cell transmission of HTLV-1. Front. Microbiol. 2012, 3, 378. [Google Scholar] [CrossRef]
- Firmino, A.D.A.; Martins, A.L.L.; Gois, L.L.; Paixão, T.S.; Batista, E.D.S.; Galvão-Castro, B.; Grassi, M.F.R. Evaluation of the cervicovaginal environment in asymptomatic Human T-cell lymphotropic virus type 1 infected women. Braz. J. Infect. Dis. 2019, 23, 27–33. [Google Scholar] [CrossRef]
- Galvão-Castro, B.; Grassi, M.F.R.; Galvão-Castro, A.V.; Nunes, A.; Galvão-Barroso, A.K.; Araújo, T.H.A.; Rathsam-Pinheiro, R.H.; Nunes, C.L.X.; Ribeiro, A.; Lírio, M.; et al. Integrative and Multidisciplinary Care for People Living With Human T-Cell Lymphotropic Virus in Bahia, Brazil: 20 Years of Experience. Front. Med. 2022, 9, 884127. [Google Scholar] [CrossRef] [PubMed]
- Lopes Martins, A.L.; Rios Grassi, M.F.; de Aquino Firmino, A.; Lacerda Araujo, J.P.; Paixao, T.S.; Galvão-Castro, B.; Boa-Sorte, N. Human T-Lymphotropic Virus-1-Associated Myelopathy/Tropical Spastic Paraparesis Is Associated With Sexual Dysfunction in Infected Women of Reproductive Age. Sex. Med. 2018, 6, 324–331. [Google Scholar] [CrossRef]
- De Castro-Costa, C.M.; Araújo, A.Q.; Barreto, M.M.; Takayanagui, O.M.; Sohler, M.P.; Da Silva, E.L.; De Paula, S.M.; Ishak, R.; Ribas, J.G.; Rovirosa, L.C.; et al. Proposal for diagnostic criteria of tropical spastic paraparesis/HTLV-I-associated myelopathy (TSP/HAM). AIDS Res. Hum. Retrovir. 2006, 22, 931–935. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed]
- Dehée, A.; Césaire, R.; Désiré, N.; Lézin, A.; Bourdonné, O.; Béra, O.; Plumelle, Y.; Smadja, D.; Nicolas, J.-C. Quantitation of HTLV-I proviral load by a TaqMan real-time PCR assay. J. Virol. Methods 2002, 102, 37–51. [Google Scholar] [CrossRef] [PubMed]
- Grassi, M.F.; Olavarria, V.N.; Kruschewsky, R.D.A.; Mascarenhas, R.E.; Dourado, I.; Correia, L.C.; De Castro-Costa, C.M.; Galvão-Castro, B. Human T cell lymphotropic virus type 1 (HTLV-1) proviral load of HTLV-associated myelopathy/tropical spastic paraparesis (HAM/TSP) patients according to new diagnostic criteria of HAM/TSP. J. Med. Virol. 2011, 83, 1269–1274. [Google Scholar] [CrossRef]
- Solomon, D.; Davey, D.; Kurman, R.; Moriarty, A.; O’Connor, D.; Prey, M.; Raab, S.; Sherman, M.; Wilbur, D.; Wright, T., Jr.; et al. The 2001 Bethesda System: Terminology for reporting results of cervical cytology. JAMA 2002, 287, 2114–2119. [Google Scholar] [CrossRef] [PubMed]
- Zunt, J.R.; Dezzutti, C.S.; Montano, S.M.; Thomas, K.K.; Alarcón, J.O.; Quijano, E.; Courtois, B.N.; Sánchez, J.L.; Campos, P.; Gotuzzo, E.; et al. Cervical shedding of human T cell lymphotropic virus type I is associated with cervicitis. J. Infect. Dis. 2002, 186, 1669–1672. [Google Scholar] [CrossRef]
- Bélec, L.; Georges-Courbot, M.C.; Georges, A.; Mohamed, A.S.; Londos-Gagliardi, D.; Hallouin, M.C.; Hocini, H.; Guillemain, B. Cervi-covaginal synthesis of IgG antibodies to the immunodominant 175-199 domain of the surface glycoprotein gp46 of human T-cell leukemia virus type I. J. Med. Virol. 1996, 50, 42–49. [Google Scholar] [CrossRef]
- Okayama, A.; Stuver, S.; Matsuoka, M.; Ishizaki, J.; Tanaka, G.; Kubuki, Y.; Mueller, N.; Hsieh, C.-C.; Tachibana, N.; Tsubouchi, H. Role of HTLV-1 proviral DNA load and clonality in the development of adult T-cell leukemia/lymphoma in asymptomatic carriers. Int. J. Cancer 2004, 110, 621–625. [Google Scholar] [CrossRef] [PubMed]
- Santos, S.B.; Oliveira, P.; Luna, T.; Souza, A.; Nascimento, M.; Siqueira, I.; Tanajura, D.; Muniz, A.L.; Glesby, M.J.; Carvalho, E.M. Immunological and viral features in patients with overactive bladder associated with human T-cell lymphotropic virus type 1 infection. J. Med. Virol. 2012, 84, 1809–1817. [Google Scholar] [CrossRef] [PubMed]
- Tanajura, D.; Castro, N.; Oliveira, P.; Neto, A.; Muniz, A.; Carvalho, N.B.; Orge, G.; Santos, S.; Glesby, M.J.; Carvalho, E.M. Neurological Manifestations in Human T-Cell Lymphotropic Virus Type 1 (HTLV-1)-Infected Individuals Without HTLV-1-Associated Myelopathy/Tropical Spastic Paraparesis: A Longitudinal Cohort Study. Clin. Infect. Dis. 2015, 61, 49–56. [Google Scholar] [CrossRef]
- Li, H.C.; Biggar, R.J.; Miley, W.J.; Maloney, E.M.; Cranston, B.; Hanchard, B.; Hisada, M. Provirus load in breast milk and risk of mother-to-child transmission of human T lymphotropic virus type I. J. Infect. Dis. 2004, 190, 1275–1278. [Google Scholar] [CrossRef] [PubMed]
- Rosadas, C.; Woo, T.; Haddow, J.; Rowan, A.; Taylor, G.P. Anti-HTLV-1/2 IgG Antibodies in the Breastmilk of Seropositive Mothers. Microorganisms 2021, 9, 1413. [Google Scholar] [CrossRef]
- Lins, L.; de Carvalho, V.J.; de Almeida Rego, F.F.; Azevedo, R.; Kashima, S.; Gallazi, V.N.; Xavier, M.T.; Galvão-Castro, B.; Alcantara, L.C., Jr. Oral health profile in patients infected with HTLV-1: Clinical findings, proviral load, and molecular analysis from HTLV-1 in saliva. J. Med. Virol. 2012, 84, 1428–1436. [Google Scholar] [CrossRef]
- Lezin, A.; Olindo, S.; Olière, S.; Varrin-Doyer, M.; Marlin, R.; Cabre, P.; Smadja, D.; Cesaire, R. Human T lymphotropic virus type I (HTLV-I) proviral load in cerebrospinal fluid: A new criterion for the diagnosis of HTLV-I-associated myelopathy/tropical spastic paraparesis? J. Infect. Dis. 2005, 191, 1830–1834. [Google Scholar] [CrossRef]
- Mori, S.; Mizoguchi, A.; Kawabata, M.; Fukunaga, H.; Usuku, K.; Maruyama, I.; Osame, M. Bronchoalveolar lymphocytosis correlates with human T lymphotropic virus type I (HTLV-I) proviral DNA load in HTLV-I carriers. Thorax 2005, 60, 138–143. [Google Scholar] [CrossRef] [PubMed]
- Masters, W.H.; Johnson, V.E. (Eds.) Human Sexual Response; Little, Brown and Company: New York, NY, USA, 1966. [Google Scholar]
- Woodard, T.L.; Diamond, M.P. Physiologic measures of sexual function in women: A review. Fertil. Steril. 2009, 92, 19–34. [Google Scholar] [CrossRef] [PubMed]
- Forsberg, J.-G. Cervicovaginal epithelium: Its origin and development. Am. J. Obstet. Gynecol. 1973, 115, 1025–1043. [Google Scholar] [CrossRef] [PubMed]
- Pudney, J.; Quayle, A.J.; Anderson, D.J. Immunological microenvironments in the human vagina and cervix: Mediators of cellular immunity are concentrated in the cervical transformation zone. Biol. Reprod. 2005, 73, 1253–1263. [Google Scholar] [CrossRef] [PubMed]
- Amabebe, E.; Anumba, D.O.C. The Vaginal Microenvironment: The Physiologic Role of Lactobacilli. Front. Med. 2018, 5, 181. [Google Scholar] [CrossRef] [PubMed]
- Schwebke, J.R.; Muzny, C.A.; Josey, W.E. Role of Gardnerella vaginalis in the pathogenesis of bacterial vaginosis: A conceptual model. J. Infect. Dis. 2014, 210, 338–343. [Google Scholar] [CrossRef] [PubMed]
- Coudray, M.S.; Madhivanan, P. Bacterial vaginosis—A brief synopsis of the literature. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 245, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Kinoshita, K.; Amagasaki, T.; Hino, S.; Doi, H.; Yamanouchi, K.; Ban, N.; Momita, S.; Ikeda, S.; Kamihira, S.; Ichimaru, M. Milk-borne transmission of HTLV-I from carrier mothers to their children. Jpn. J. Cancer Res. 1987, 78, 674–680. [Google Scholar]
- Caterino-de-Araujo, A.; de los Santos-Fortuna, E. No evidence of vertical transmission of HTLV-I and HTLV-II in children at high risk for HIV-1 infection from São Paulo, Brazil. J. Trop. Pediatr. 1999, 45, 42–47. [Google Scholar] [CrossRef]
- Kashiwagi, K.; Furusyo, N.; Nakashima, H.; Kubo, N.; Kinukawa, N.; Kashiwagi, S.; Hayashi, J. A decrease in mother-to-child trans-mission of human T lymphotropic virus type I (HTLV-I) in Okinawa, Japan. Am. J. Trop Med. Hyg. 2004, 70, 158–163. [Google Scholar] [CrossRef]
| Variable | |
|---|---|
| Age (years) a | 35.9 ± 7.2 |
| Family income b | 1 (1–2) |
| Educational level (years) b | 9 (5–12) |
| Skin color (%) c | |
| Black | 26 (46.4) |
| Mixed-race | 21 (37.5) |
| White | 9 (16.1) |
| Marital status (%) c | |
| Married/Stable relationship | 41 (73.2) |
| Single | 14 (25) |
| Divorced/Separated | 1 (1.8) |
| Partner age (years) b | 42 (33.5–47.5) |
| Number of lifetime partners b | 4 (3–13.5) |
| Parity b | 1.5 (1–3) |
| Variable | HTLV-1 Asymptomatic (n = 43) | HAM/TSP (n = 13) | p-Value |
|---|---|---|---|
| Cervicovaginal cytopathology n (%) a | |||
| Negative for neoplasia | 42 (97.7) | 12 (92.3) | 0.36 |
| ASC-US b | 1 (2.3) | 0 | 0.58 |
| Unsatisfactory | 0 | 1 (7.7) | 0.07 |
| Vaginal microbiota n (%) a | |||
| Lactobacillus vaginalis | 7 (16.3) | 2 (15.4) | 0.94 |
| Gardnerella vaginalis/Mobiluncus spp. | 9 (20.9) | 2 (15.4) | 0.66 |
| Coccus/Bacillus | 16 (37.2) | 6 (46.1) | 0.56 |
| Candida spp. | 11 (25.6) | 2 (15.4) | 0.44 |
| Unsatisfactory | 0 | 1 (7.7) | 0.07 |
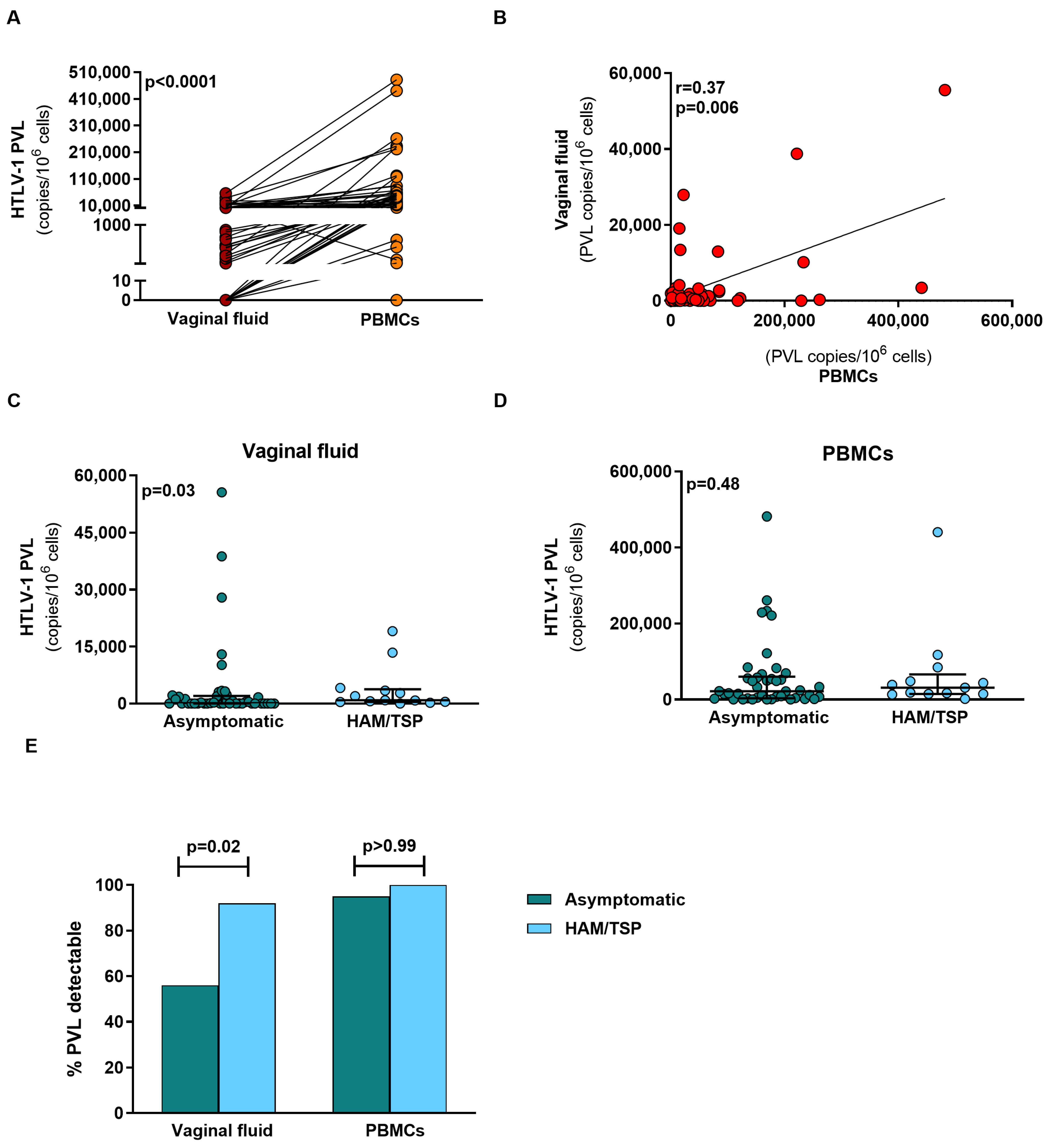
| HTLV-1 PVL in cervicovaginal fluid c,d | 103.1 (0–2000) | 869 (447.9–3760) | 0.03 |
| HTLV-1 PVL in PBMCs c,d | 21,976 (3420–60,036) | 31,080 (14,799–66,420) | 0.48 |
| Variable | PVL Detectable (n = 36) | PVL Undetectable (n = 20) | p-Value |
|---|---|---|---|
| Cervicovaginal cytopathology n (%) a | |||
| Negative for neoplasia | 34 (94.4) | 20 (100) | 0.28 |
| ASC-US b | 1 (2.8) | 0 | 0.45 |
| Unsatisfactory | 1 (2.8) | 0 | 0.45 |
| Vaginal microbiota n (%) a | |||
| Lactobacillus vaginalis | 2 (5.6) | 7 (35) | 0.004 |
| Gardnerella vaginalis/Mobiluncus spp. | 7 (19.4) | 4 (20) | 0.96 |
| Coccus/Bacillus | 20 (55.6) | 2 (10) | 0.001 |
| Candida spp. | 6 (16.6) | 7 (35) | 0.11 |
| Unsatisfactory | 1 (2.8) | 0 | 0.45 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Aquino Firmino, A.; Filho, P.R.T.G.; Martins, A.L.L.; Araújo, T.H.; Gois, L.L.; da Silva Batista, E.; Araújo, J.P.L.; Galvão-Castro, B.; Grassi, M.F.R. HTLV-1 Proviral Load in Vaginal Fluid Correlates with Levels in Peripheral Blood Mononuclear Cells. Pathogens 2023, 12, 682. https://doi.org/10.3390/pathogens12050682
de Aquino Firmino A, Filho PRTG, Martins ALL, Araújo TH, Gois LL, da Silva Batista E, Araújo JPL, Galvão-Castro B, Grassi MFR. HTLV-1 Proviral Load in Vaginal Fluid Correlates with Levels in Peripheral Blood Mononuclear Cells. Pathogens. 2023; 12(5):682. https://doi.org/10.3390/pathogens12050682
Chicago/Turabian Stylede Aquino Firmino, Alisson, Paulo Roberto Tavares Gomes Filho, Adenilda Lima Lopes Martins, Thessika Hialla Araújo, Luana Leandro Gois, Everton da Silva Batista, Jean Paulo Lacerda Araújo, Bernardo Galvão-Castro, and Maria Fernanda Rios Grassi. 2023. "HTLV-1 Proviral Load in Vaginal Fluid Correlates with Levels in Peripheral Blood Mononuclear Cells" Pathogens 12, no. 5: 682. https://doi.org/10.3390/pathogens12050682
APA Stylede Aquino Firmino, A., Filho, P. R. T. G., Martins, A. L. L., Araújo, T. H., Gois, L. L., da Silva Batista, E., Araújo, J. P. L., Galvão-Castro, B., & Grassi, M. F. R. (2023). HTLV-1 Proviral Load in Vaginal Fluid Correlates with Levels in Peripheral Blood Mononuclear Cells. Pathogens, 12(5), 682. https://doi.org/10.3390/pathogens12050682








