Neuroangiostrongyliasis: Updated Provisional Guidelines for Diagnosis and Case Definitions
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alicata, J.E. Biology and distribution of the rat lungworm, Angiostrongylus cantonensis, and its relationship to eosinophilic meningoencephalitis and other neurological disorders of man and animals. Adv. Parasitol. 1965, 3, 223–248. [Google Scholar] [PubMed]
- Graeff-Teixeira, C.; Silva, A.C.A.; Yoshimura, K. Update on eosinophilic meningoencephalitis and its clinical relevance. Clin. Microbiol. Rev. 2009, 22, 322–348. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.P.; Lai, D.H.; Zhu, X.Q.; Chen, X.G.; Lun, Z.R. Human angiostrongyliasis. Lancet Infect. Dis. 2008, 8, 621–630. [Google Scholar] [CrossRef]
- Howe, K.; Kaluna, L.; Lozano, A.; Torres Fischer, B.; Tagami, Y.; McHugh, R.; Jarvi, S. Water transmission potential of Angiostrongylus cantonensis: Larval viability and effectiveness of rainwater catchment sediment filters. PLoS ONE 2019, 14, e0209813. [Google Scholar] [CrossRef]
- Jarvi, S.I.; Eamsobhana, P.; Quarta, S.; Howe, K.; Jacquier, S.; Hanlon, A.; Snook, K.; McHugh, R.; Tman, Z.; Miyamura, J.; et al. Estimating Human Exposure to Rat Lungworm (Angiostrongylus cantonensis) on Hawai’i Island: A Pilot Study. Am. J. Trop. Med. Hyg. 2020, 102, 69–77. [Google Scholar] [CrossRef]
- Punyagupta, S.; Juttijudata, P.; Bunnag, T. Eosinophilic meningitis in Thailand. Clinical studies of 484 typical cases probably caused by Angiostrongylus cantonensis. Am. J. Trop. Med. Hyg. 1975, 24, 921–931. [Google Scholar] [CrossRef]
- Eamsobhana, P.; Yong, H.S. Immunological diagnosis of human angiostrongyliasis due to Angiostrongylus cantonensis (Nematoda: Angiostrongylidae). Int. J. Infect. Dis. 2009, 13, 425–431. [Google Scholar] [CrossRef]
- Qvarnstrom, Y.; Xayavong, M.; Silva, A.C.A.; Park, S.Y.; Whelen, A.C.; Calimlim, P.S.; Silva, A.J. Real-time polymerase chain reaction detection of Angiostrongylus cantonensis DNA in cerebrospinal fluid from patients with eosinophilic meningitis. Am. J. Trop. Med. Hyg. 2016, 94, 176. [Google Scholar] [CrossRef]
- Somboonpatarakun, C.; Intapan, P.M.; Sadaow, L.; Rodpai, R.; San pool, O.; Maleewong, W. Development of an immunochromato graphic device to detect antibodies for rapid diagnosis of human angiostrongyliasis. Parasitology 2020, 147, 194–198. [Google Scholar] [CrossRef]
- Sears, W.J.; Qvarnstrom, Y.; Dahlstrom, E.; Snook, K.; Kaluna, L.; Baláž, V.; Feckova, B.; Šlapeta, J.; Modry, D.; Jarvi, S.; et al. AcanR3990 qPCR: A Novel, Highly Sensitive, Bioinformatically-Informed Assay to Detect Angiostrongylus cantonensis Infections. Clin. Infect. Dis. 2021, 73, e1594–e1600. [Google Scholar] [CrossRef]
- Kliks, M.M.; Palumbo, N.E. Eosinophilic meningitis beyond the Pacific basin: The global dispersal of a peridomestic zoonosis caused by Angiostrongylus cantonensis, the nematode lungworm of rats. Soc. Sci. Med. 1992, 34, 199–212. [Google Scholar] [CrossRef] [PubMed]
- Johnston, D.I.; Dixon, M.C.; Elm, J.L., Jr.; Calimlim, P.S.; Sciulli, R.H.; Park, S.Y. Review of cases of angiostrongyliasis in Hawaii, 2007–2017. Am. J. Trop. Med. Hyg. 2019, 101, 608. [Google Scholar] [CrossRef] [PubMed]
- Khamsai, S.; Chotmongkol, V.; Tiamkao, S.; Maleewong, W.; Limpawattana, P.; Boonsawat, W.; Sawanyawisuth, K. Eosinophilic meningitis epidemiological data from a national database in Thailand’s Department of Disease Control: A pragmatic, retrospective analytical study. Orphanet J. Rare Dis. 2022, 17, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Sawanyawisuth, K.; Sawanyawisuth, K. Treatment of angiostrongyliasis. Trans. R. Soc. Trop. Med. Hyg. 2008, 102, 990–996. [Google Scholar] [CrossRef]
- Sawanyawisuth, K.; Kitthaweesin, K.; Limpawattana, P.; Intapan, P.; Tiamkao, S.; Jitpimolmard, S.; Chotmongkol, V. Intraocular angiostrongyliasis: Clinical findings, treatments and outcomes. Trans. R. Soc. Trop. Med. Hyg. 2007, 101, 497–501. [Google Scholar] [CrossRef] [PubMed]
- Chotmongkol, V.; Sawanyawisuth, K. Clinical manifestations and outcome of patients with severe eosinophilic meningoencephalitis presumably caused by Angiostrongylus cantonensis. Southeast Asian J. Trop. Med. Public Health 2002, 45, 30–61. [Google Scholar]
- Lv, S.; Zhang, Y.; Chen, S.-R.; Wang, L.-B.; Fang, W.; Chen, F.; Jiang, J.-Y.; Li, Y.-L.; Du, Z.-W.; Zhou, X.-N. Human Angiostrongyliasis Outbreak in Dali, China. PLoS Negl. Trop. Dis. 2009, 3, e520. [Google Scholar] [CrossRef]
- Ansdell, V.; Kramer, K.J.; McMillan, J.K.; Gosnell, W.L.; Murphy, G.S.; Meyer, B.C.; Blalock, E.U.; Yates, J.; Leteif, L.; Smith, O.A.; et al. Guidelines for the diagnosis and treatment of neuroangiostrongyliasis: Updated recommendations. Parasitology 2021, 148, 227–233. [Google Scholar] [CrossRef]
- Dechet, A.M.; Parsons, M.; Rambaran, M.; Mohamed-Rambaran, P.; Florendo-Cumbermack, A.; Persaud, S.; Baboolal, S.; Ari, M.D.; Shadomy, S.V.; Zaki, S.R.; et al. Leptospirosis Outbreak following Severe Flooding: A Rapid Assessment and Mass Prophylaxis Campaign; Guyana, January–February 2005. PLoS ONE 2012, 7, e39672. [Google Scholar] [CrossRef]
- OPAS/WHO. Modulos de Principios de Epidemiología para el Control de Enfermedades. In Modulo 4: Vigilancia em Salud Publica; Organização Pan-Americana da Saúde: Brasília, Brazil, 2010; 52p. [Google Scholar]
- Colt, S.; Garcia-Casal, M.N.; Peña-Rosas, J.P.; Finkelstein, J.L.; Rayco-Solon, P.; Weise, Z.C.; Mehta, S. Transmission of Zika virus through breast milk and other breastfeeding-related bodily-fluids: A systematic review. PLoS Negl. Trop. Dis. 2017, 11, e0005528. [Google Scholar] [CrossRef]
- WHO. Yellow fever surveillance and outbreak response: Revision of case definitions, October 2010. Wkly. Epidemiol. Rec. 2010, 47, 19. [Google Scholar]
- WHO. Surveillance, Case Investigation and Contact Tracing for Mpox (Monkeypox): Interim Guidance, 22 December 2022. WHO/MPX/Surveillance/2022.4. Available online: https://www.who.int/publications/i/item/WHO-MPX-Surveillance-2022.4 (accessed on 26 January 2023).
- Jarvi, S.I.; Nakayama, K.; Eamsobhana, P.; Kaluna, L.; Shepherd, L.; Tagami, Y. Immunodiagnostic detection of Angiostrongylus cantonensis exposure on Hawai’i Island using isogeographical 31 kDa antigen. Am. J. Trop. Med. Hyg. 2023, in press. [Google Scholar]
- Khamsai, S.; Chindaprasirt, J.; Chotmongkol, V.; Tiamkao, S.; Limpawattana, P.; Senthong, V.; Sawanyawisuth, K. Clinical features of eosinophilic meningitis caused by Angiostrongylus cantonensis in Thailand: A systematic review. Asia-Pac. J. Sci. Technol. 2020, 25, APST-25-02-09. Available online: https://so01.tci-thaijo.org/index.php/APST/article/view/240510 (accessed on 20 March 2023).
- Jacob, J.; Steel, A.; Howe, K.; Jarvi, S.I. Management of Rat Lungworm Disease (Neuroangiostrongyliasis) Using Anthelmintics: Recent Updates and Recommendations. Pathogens 2023, 12, 23. [Google Scholar] [CrossRef] [PubMed]
- Sonakul, D. Pathological findings in four cases of human angiostrongyliasis. Southeast Asian J. Trop. Med. Public Health 1978, 9, 220–227. [Google Scholar] [PubMed]
- Cooke-Yarborough, C.M.; Kornberg, A.J.; Hogg, G.G.; Spratt, D.M.; Forsyth, J.R. A fatal case of angiostrongyliasis in an 11-month-old infant. Med. J. Aust. 1999, 170, 541–543. [Google Scholar] [CrossRef]
- Prociv, P.; Carlisle, M.S. The spread of Angiostrongylus cantonensis in Australia. Southeast Asian J. Trop. Med. Public Health 2001, 32, 126–128. [Google Scholar]
- Sawanyawisuth, K.; Chindaprasirt, J.; Senthong, V.; Limpawattana, P.; Auvichayapat, N.; Tassniyom, S.; Chotmongkol, V.; Maleewong, W.; Intapan, P.M. Clinical manifestations of Eosinophilic meningitis due to infection with Angiostrongylus cantonensis in children. Korean J. Parasitol. 2013, 51, 735–738. [Google Scholar] [CrossRef]
- Sawanyawisuth, K.; Pugkhem, A.; Mitchai, J.; Intapan, P.M.; Anunnatsiri, S.; Limpawattana, P.; Chotmongkol, V. Abdominal angiostrongyliasis caused by Angiostrongylus cantonensis: A possible cause of eosinophilic infiltration in human digestive tract. Pathol. Res. Pract. 2010, 206, 102–104. [Google Scholar] [CrossRef]
- Yii, C.Y. Clinical observations on eosinophilic meningitis and meningoencephalitis caused by Angiostrongylus cantonensis inTaiwan. Am. J. Trop. Med. Hyg. 1976, 25, 233–249. [Google Scholar] [CrossRef]
- Cross, J.H. Clinical manifestations and laboratory diagnosis of eosinophilic meningitis syndrome associated with angiostrongyliasis. Southeast Asian J. Trop. Med. Public Health 1978, 9, 161–170. [Google Scholar] [PubMed]
- Sawanyawisuth, K.; Sawanyawisuth, K.; Senthong, V.; Limpawattana, P.; Phichaphop, A.; Intapan, P.M.; Maleewong, W.; Tiamkao, S.; Jitpimolmard, S.; Chotmongkol, V. How can clinicians ensure the diagnosis of meningitic angiostrongyliasis? Vector-Borne Zoonotic Dis. 2012, 12, 73–75. [Google Scholar] [CrossRef] [PubMed]
- Jacob, J.; Steel, A.; Kaluna, L.; Hess, S.; Leinbach, I.; Antaky, C.; Sugihara, R.; Hamilton, L.; Follett, P.; Howe, K.; et al. In vivo efficacy of pyrantel pamoate as a post-exposure prophylactic for rat lungworm (Angiostrongylus cantonensis). Int. J. Parasitol. Drugs Drug Resist. 2022, 19, 1–5. [Google Scholar] [CrossRef]
- Cognato, B.B.; Handali, S.; Morassutti, A.L.; Silva, A.J.; Graeff-Teixeira, C. Heterologous expression of three antigenic proteins from Angiostrongylus cantonensis: ES-7, Lec-5, and 14-3-3 in mammalian cells. Mol. Biochem. Parasitol. 2018, 221, 32–35. [Google Scholar] [CrossRef] [PubMed]
- Morassutti, A.L.; Levert, K.; Perelygin, A.; Silva, A.J.; Wilkins, P.; Graeff-Teixeira, C. The 31-kDa antigen of Angiostrongylus cantonensis comprises distinct antigenic glycoproteins. Vector-Borne Zoonotic Dis. 2012, 12, 961–968. [Google Scholar] [CrossRef] [PubMed]
- Murphy, G.S.; Johnson, S. Clinical aspects of eosinophilic meningitis and meningoencephalitis caused by Angiostrongylus cantonensis, the rat lungworm. Hawaii J. Med. Public Health 2013, 72, 35. [Google Scholar]
- Sawanyawisuth, K.; Limpawattana, P.; Busaracome, P.; Ninpaitoon, B.; Chotmongkol, V.; Intapan, P.M.; Tanawirattananit, S. A 1-week course of corticosteroids in the treatment of eosinophilic meningitis. Am. J. Med. 2004, 117, 802–803. [Google Scholar] [CrossRef]
- Ansdell, V.; Wattanagoon, Y. Angiostrongylus cantonensis in travelers: Clinical manifestations, diagnosis, and treatment. Curr. Opin. Infect. Dis. 2018, 31, 399–408. [Google Scholar] [CrossRef]
- Khamsai, S.; Sawanyawisuth, K.; Senthong, V.; Limpawattana, P.; Chindaprasirt, J.; Intapan, P.M.; Ngamjarus, C. Corticosteroid treatment reduces headache in eosinophilic meningitis: A systematic review. Drug Target Insights 2021, 15, 1. [Google Scholar] [CrossRef]
- Jacob, J.; Steel, A.; Lin, Z.; Berger, F.; Zöeller, K.; Jarvi, S.I. Clinical Efficacy and Safety of Albendazole and Other Benzimidazole Anthelmintics for Rat Lungworm Disease (Neuroangiostrongyliasis): A Systematic Analysis of Clinical Reports and Animal Studies. Clin. Infect. Dis. 2022, 74, 1293–1302. [Google Scholar] [CrossRef]
| Type of Exposure | Vectors/ Transmission Areas |
|---|---|
| Ingestion of raw, undercooked and/or inadequately washed foods | Mollusks: snails, slugs |
| Salads | |
| Juices Fruits Planarians | |
| Freshwater shrimp Crabs | |
| Frogs | |
| Lizards | |
| Water contaminated with larvae | |
| Touching, handling | Mollusks, snails, or slugs |
| Residence or recent travel | Endemic areas |
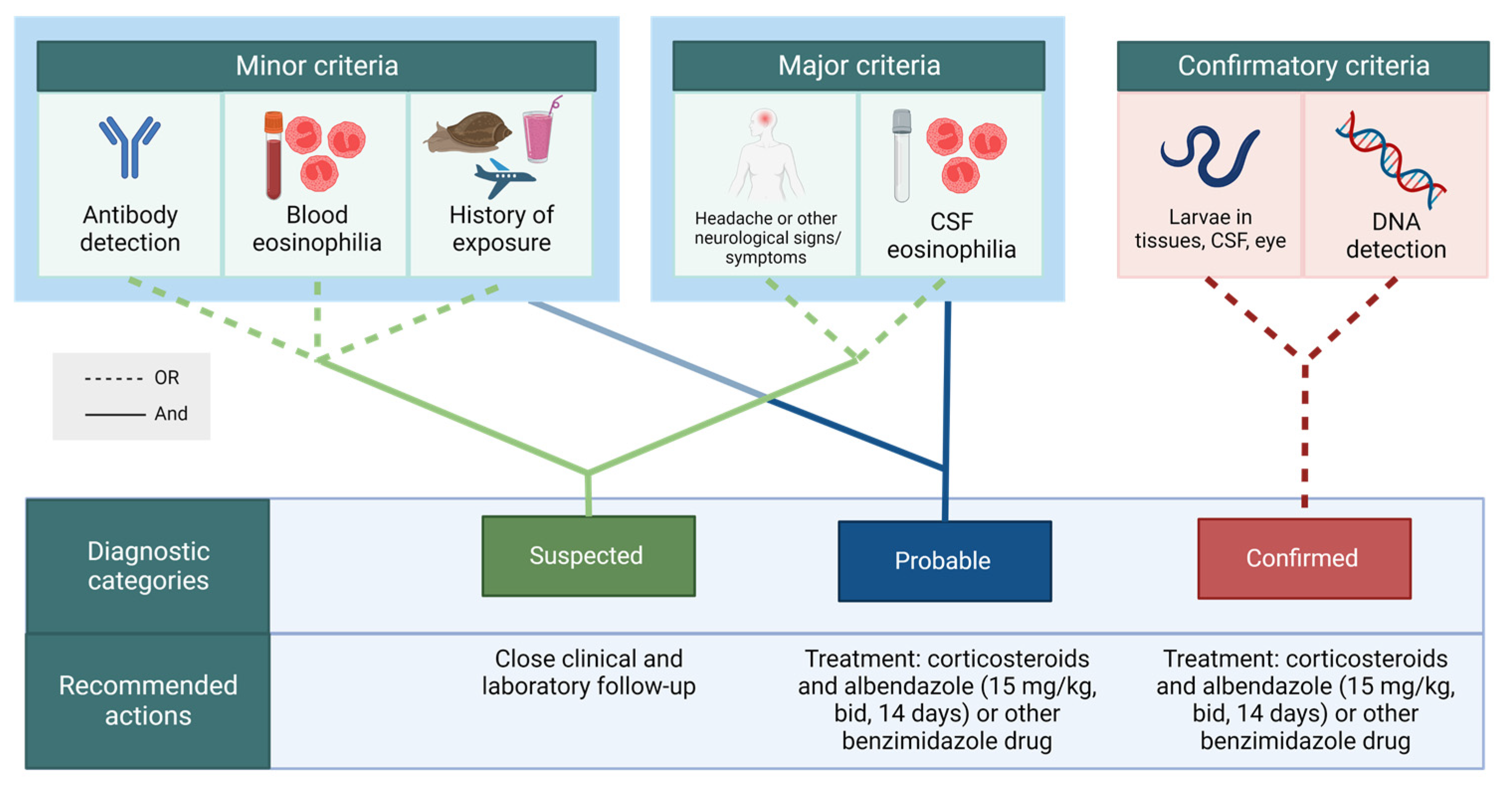
| Criteria Category | Criteria | |
|---|---|---|
| Minor | a. Exposure history b. Serology (antibody detection) c. Blood eosinophilia | |
| Major | a. CSF 1 eosinophilia b. Headache, other neurological signs or symptoms, and other obvious etiologies ruled out. | |
| Confirmatory | a. Larvae in tissues, CSF, or eye b. DNA detection 2 | |
| Diagnosis Categories | Criteria | Recommended Actions |
|---|---|---|
| Suspected | ||
| Close clinical and laboratory follow up | |
| Probable | ||
| 3 Treatment: corticosteroids and albendazole (15 mg/kg, bid, 14 days) | |
| Confirmed | ||
| 3 Treatment: corticosteroids and albendazole (15 mg/kg, bid, 14 days) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Graeff-Teixeira, C.; Sawanyawisuth, K.; Lv, S.; Sears, W.; Rodríguez, Z.G.; Álvarez, H.H.; Arias, P.C.; Schultz, L.K.W.; Rojas, A.; Jacob, J.; et al. Neuroangiostrongyliasis: Updated Provisional Guidelines for Diagnosis and Case Definitions. Pathogens 2023, 12, 624. https://doi.org/10.3390/pathogens12040624
Graeff-Teixeira C, Sawanyawisuth K, Lv S, Sears W, Rodríguez ZG, Álvarez HH, Arias PC, Schultz LKW, Rojas A, Jacob J, et al. Neuroangiostrongyliasis: Updated Provisional Guidelines for Diagnosis and Case Definitions. Pathogens. 2023; 12(4):624. https://doi.org/10.3390/pathogens12040624
Chicago/Turabian StyleGraeff-Teixeira, Carlos, Kittisak Sawanyawisuth, Shan Lv, William Sears, Zhaily González Rodríguez, Hilda Hernández Álvarez, Pedro Casanova Arias, Leticia Karolini Walger Schultz, Alicia Rojas, John Jacob, and et al. 2023. "Neuroangiostrongyliasis: Updated Provisional Guidelines for Diagnosis and Case Definitions" Pathogens 12, no. 4: 624. https://doi.org/10.3390/pathogens12040624
APA StyleGraeff-Teixeira, C., Sawanyawisuth, K., Lv, S., Sears, W., Rodríguez, Z. G., Álvarez, H. H., Arias, P. C., Schultz, L. K. W., Rojas, A., Jacob, J., Jarvi, S., & Kramer, K., on behalf of International Network on Angiostrongyliasis—INA. (2023). Neuroangiostrongyliasis: Updated Provisional Guidelines for Diagnosis and Case Definitions. Pathogens, 12(4), 624. https://doi.org/10.3390/pathogens12040624