Feral Swine as Indirect Indicators of Environmental Anthrax Contamination and Potential Mechanical Vectors of Infectious Spores
Abstract
1. Introduction
2. Materials and Methods
2.1. Animals
2.2. Spore Preparation
2.3. Animal Challenge
2.4. Sampling and Clinical Observation
2.5. Serology
2.6. Nasal Swab Processing
2.7. DNA Extraction and PCR
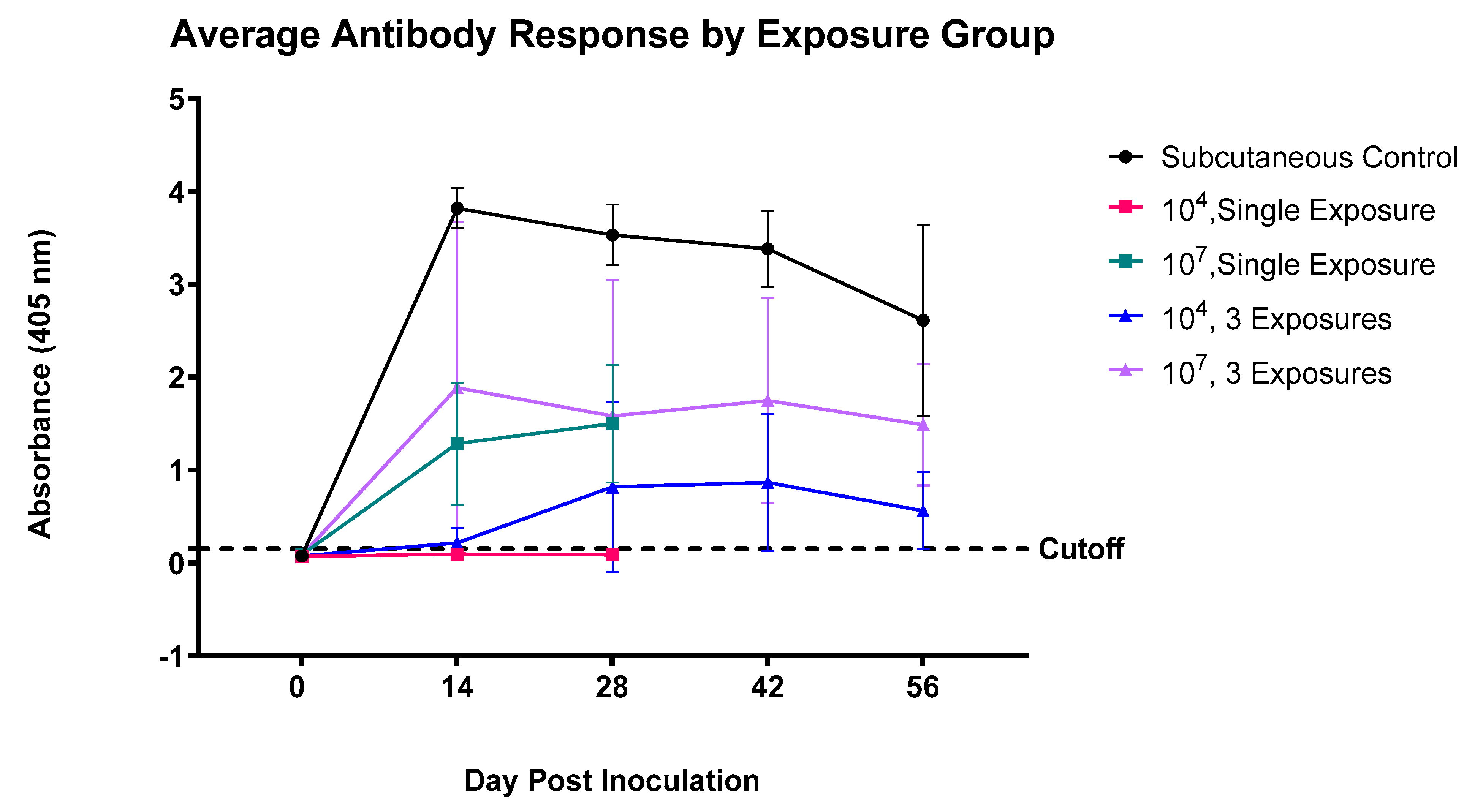
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bengis, R.G. Anthrax in free-ranging wildlife. In Fowler’s Zoo and Wild Animal Medicine Current Therapy; Miller, R.E., Fowler, M.E., Eds.; Elsevier Health Sciences: St. Louis, MI, USA, 2012; pp. 98–107. [Google Scholar]
- Ebedes, H. Anthrax epizo tics in Etosha National Park. Madoqua 1977, 1977, 99–118. [Google Scholar]
- Turnbull, P.C.B.; Doganay, M.; Lindeque, P.M.; Aygen, B.; McLaughlin, J. Serology and anthrax in humans, livestock and Etosha National Park wildlife. Epidemiol. Infect. 1992, 108, 299–313. [Google Scholar] [CrossRef] [PubMed]
- Bagamian, K.H.; Alexander, K.A.; Hadfield, T.L.; Blackburn, J.K. Ante-and postmortem diagnostic techniques for anthrax: Rethinking pathogen exposure and the geographic extent of the disease in wildlife. J. Wildl. Dis. 2013, 49, 786–801. [Google Scholar] [CrossRef] [PubMed]
- Mukarati, N.L.; Ndumnego, O.; Van Heerden, H.; Ndhlovu, D.N.; Matope, G.; Caron, A.; Garine-Wichatitsky, M.; Pfukenyi, D.M. A serological survey of anthrax in domestic dogs in Zimbabwe: A potential tool for anthrax surveillance. Epidemiol. Infect. 2018, 146, 1526–1532. [Google Scholar] [CrossRef] [PubMed]
- Walker, M.A.; Uribasterra, M.; Asher, V.; Getz, W.M.; Ryan, S.J.; Ponciano, J.M.; Blackburn, J.K. Anthrax surveillance and the limited overlap between obligate scavengers and endemic anthrax zones in the United States. Vector Borne Zoonotic Dis. 2021, 21, 675–684. [Google Scholar] [CrossRef]
- Blackburn, J.K.; Curtis, A.; Hadfield, T.L.; O’Shea, B.; Mitchell, M.A.; Hugh-Jones, M.E. Confirmation of Bacillus anthracis from flesh-eating flies collected during a West Texas anthrax season. J. Wildl. Dis. 2010, 46, 918–922. [Google Scholar] [CrossRef]
- Braack, L.E.; De Vos, V. Feeding habits and flight range of blow-flies (Chrysomyia spp.) in relation to anthrax transmission in the Kruger National Park, South Africa. Onderstepoort J. Vet. Res. 1990, 57, 141–142. [Google Scholar]
- Hugh-Jones, M.E.; De Vos, V. Anthrax and wildlife. Rev. Sci. Tech. 2002, 21, 359–384. [Google Scholar] [CrossRef]
- Dragon, D.C.; Elkin, B.T.; Nishi, J.S.; Ellsworth, T.R. A review of anthrax in Canada and implications for research on the disease in northern bison. J. Appl. Microbiol. 1999, 87, 208–213. [Google Scholar] [CrossRef]
- Barandongo, Z.R.; Mfune, J.K.; Turner, W.C. Dust-bathing behaviors of African herbivores and the potential risk of inhalational anthrax. J. Wildl. Dis. 2018, 54, 34–44. [Google Scholar] [CrossRef]
- Turnbull, P.C.B. Anthrax in Humans and Animals, 4th ed.; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Glinert, I.; Weiss, S.; Sittner, A.; Bar-David, E.; Ben-Shmuel, A.; Schlomovitz, J.; Kobiler, D.; Levy, H. Infection with a nonencapsulated Bacillus anthracis strain in rabbits-the role of bacterial adhesion and the potential for a safe live attenuated vaccine. Toxins 2018, 10, 506. [Google Scholar] [CrossRef]
- Ascenzi, P.; Visca, P.; Ippolito, G.; Spallarossa, A.; Bolognesi, M.; Montecucco, C. Anthrax toxin: A tripartite lethal combination. FEBS Lett. 2002, 531, 384–388. [Google Scholar] [CrossRef] [PubMed]
- Friebe, S.; Van der Goot, F.G.; Bürgi, J. The ins and outs of anthrax toxin. Toxins 2016, 8, 69. [Google Scholar] [CrossRef] [PubMed]
- Dragon, D.C.; Rennie, R.P. The ecology of anthrax spores: Tough but not invincible. Can. Vet. J. 1995, 36, 295. [Google Scholar] [PubMed]
- Spickler, A.R. Anthrax. Available online: http://www.cfsph.iastate.edu/DiseaseInfo/factsheets.php (accessed on 1 January 2023).
- Halvorson, H.O. Two generations of spore research: From father to son. Microbiologia 1997, 13, 131–148. [Google Scholar]
- Norris, M.H.; Zincke, D.; Leiser, O.P.; Kreuzer, H.; Hadfied, T.L.; Blackburn, J.K. Laboratory strains of Bacillus anthracis lose their ability to rapidly grow and sporulate compared to wildlife outbreak strains. PLoS ONE 2020, 15, e0228270. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.L.; DeVos, V.; Bryden, H.; Price, L.B.; Hugh-Jones, M.E.; Keim, P. Bacillus anthracis diversity in Kruger National Park. J. Clin. Microbiol. 2000, 38, 3780–3784. [Google Scholar] [CrossRef] [PubMed]
- Stallknecht, D.E. Impediments to wildlife disease surveillance, research, and diagnostics. In Wildlife and Emerging Zoonotic Diseases: The Biology, Circumstances and Consequences of Cross-Species Transmission; Childs, J.E., Mackenzie, J.S., Richt, J.A., Eds.; Springer: Berlin/Heidelberg, Germany, 2007; pp. 445–461. [Google Scholar]
- Bellan, S.E.; Gimenez, O.; Choquet, R.; Getz, W.M. A hierarchical distance sampling approach to estimating mortality rates from opportunistic carcass surveillance data. Methods Ecol. Evol. 2013, 4, 361–369. [Google Scholar] [CrossRef]
- Yang, A.; Mullins, J.C.; Van Ert, M.; Bowen, R.A.; Hadfield, T.L.; Blackburn, J.K. Predicting the geographic distribution of the Bacillus anthracis A1. a/Western North American sub-lineage for the continental United States: New outbreaks, new genotypes, and new climate data. Am. J. Trop. Med. Hyg. 2020, 102, 392–402. [Google Scholar] [CrossRef]
- Blackburn, J.K.; Hadfield, T.L.; Curtis, A.J.; Hugh-Jones, M.E. Spatial and temporal patterns of anthrax in white-tailed deer, Odocoileus virginianus, and hematophagous flies in west Texas during the summertime anthrax risk period. Ann. Am. Assoc. Geogr. 2014, 104, 939–958. [Google Scholar] [CrossRef]
- Blackburn, J.K.; McNyset, K.M.; Curtis, A.; Hugh-Jones, M.E. Modeling the geographic distribution of Bacillus anthracis, the causative agent of anthrax disease, for the contiguous United States using predictive ecologic niche modeling. Am. J. Trop. Med. Hyg. 2007, 77, 1103–1110. [Google Scholar] [CrossRef] [PubMed]
- Dragon, D.C.; Rennie, R.P.; Elkin, B.T. Detection of anthrax spores in endemic regions of northern Canada. J. Appl. Microbiol. 2001, 91, 435–441. [Google Scholar] [CrossRef] [PubMed]
- Saggese, M.D.; Noseda, R.P.; Uhart, M.M.; Deem, S.L.; Ferreyra, H.; Romano, M.C.; Ferreyra-Armas, M.C.; Hugh-Jones, M. First detection of Bacillus anthracis in feces of free-ranging raptors from central Argentina. J. Wildl. Dis. 2007, 43, 136–141. [Google Scholar] [CrossRef] [PubMed]
- Goossens, P.L. Animal models of human anthrax: The quest for the holy grail. Mol. Aspects Med. 2009, 30, 467–480. [Google Scholar] [CrossRef] [PubMed]
- Maison, R.M.; Pierce, C.F.; Ragan, I.K.; Brown, V.R.; Bodenchuk, M.J.; Bowen, R.A.; Bosco-Lauth, A.M. Potential use for serosurveillance of feral swine to map risk for anthrax exposure, Texas, USA. J. Emerg. Infect. Dis. 2021, 27, 3103–3110. [Google Scholar] [CrossRef]
- Bagamian, K.H.; Skrypnyk, A.; Rodina, Y.; Bezymennyi, M.; Nevolko, O.; Skrypnyk, V.; Blackburn, J.K. Serological anthrax surveillance in wild boar (Sus scrofa) in Ukraine. Vector Borne Zoonotic Dis. 2014, 14, 618–620. [Google Scholar] [CrossRef]
- USDA APHIS. History of Feral Swine in the Americas. Available online: https://www.aphis.usda.gov/aphis/ourfocus/wildlifedamage/operational-activities/feral-swine/sa-fs-history (accessed on 15 January 2023).
- Graves, H.B. Behavior and ecology of wild and feral swine (Sus scrofa). J. Anim. Sci. 1984, 58, 482–492. [Google Scholar] [CrossRef]
- USDA-WS. Wildlife Services’ Comprehensive Feral Swine Disease Surveillance Procedures Manual, Fiscal Year 2020. In Procedure Manual for Comprehensive Feral Swine Disease Surveillance; United States Department of Agriculture, National Wildlife Research Center: Fort Collins, CO, USA, 2020. [Google Scholar]
- Lyons, C.R.; Lovchik, J.; Hutt, J.; Lipscomb, M.F.; Wang, E.; Heninger, S.; Berliba, L.; Garrison, K. Murine model of pulmonary anthrax: Kinetics of dissemination, histopathology, and mouse strain susceptibility. Infect. Immun. 2004, 72, 4801–4809. [Google Scholar] [CrossRef]
- Leighton, T.J.; Doi, R.H. The stability of messenger, ribonucleic acid during sporulation in Bacillus subtilis. J. Biol. Chem. 1971, 246, 3189–3195. [Google Scholar] [CrossRef]
- Janeway, C.A.; Travers, P.; Walport, M.; Shlomchik, M.J. Principles of Inate and Adaptive Immunity. In Immunobiology: The Immune System in Health and Disease, 5th ed.; Garland Science: New York, NY, USA, 2001. [Google Scholar]
- Snyder, J.W.; Shapiro, D.S.; Gilchrist, M.J.; Wyant, R.S.; Popovic, T.; Ezzell, J.W.; Morse, S.A. Basic Diagnostic Testing Protocols for Level A Laboratories for the Presumptive Identification of Bacillus Anthracis; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2002. [Google Scholar]
- Knisely, R.F. Selective medium for Bacillus anthracis. J. Bacteriol. 1966, 92, 784–786. [Google Scholar] [CrossRef]
- Ogawa, H.; Fujikura, D.; Ohnuma, M.; Ohnishi, N.; Hang’ombe, B.M.; Mimuro, H.; Ezaki, T.; Mweene, A.S.; Higashi, H. A novel multiplex PCR discriminates Bacillus anthracis and its genetically related strains from other Bacillus cereus group species. PLoS ONE 2015, 10, e0122004. [Google Scholar] [CrossRef] [PubMed]
- Lozano, G.L.; Holt, J.; Ravel, J.; Rasko, D.A.; Thomas, M.G.; Handelsman, J. Draft genome sequence of biocontrol agent Bacillus cereus UW85. Genome Announc. 2016, 4, e00910-16. [Google Scholar] [CrossRef] [PubMed]
- Fasanella, A.; Losito, S.; Trotta, T.; Adone, R.; Massa, S.; Ciuchini, F.; Chiocco, D. Detection of anthrax vaccine virulence factors by polymerase chain reaction. Vaccine 2001, 19, 4214–4218. [Google Scholar] [CrossRef] [PubMed]
- Zincke, D.; Norris, M.H.; Kurmanov, B.; Hadfield, T.L.; Blackburn, J.K. Nucleotide polymorphism assay for the identification of west African group Bacillus anthracis: A lineage lacking anthrose. BMC Microbiol. 2020, 20, 1–12. [Google Scholar] [CrossRef]
- CDC. Anthrax Sterne, General Information. Available online: https://www.cdc.gov/nczved/divisions/dfbmd/diseases/anthrax_sterne/ (accessed on 20 January 2023).
- Strom, B.L.; Durch, J.S.; Zwanziger, L.L.; Joellenbeck, L.M. The Anthrax Vaccine: Is It Safe? Does it Work? National Academy Press: Washington, DC, USA, 2002. [Google Scholar]
- Bengis, R.G.; Rean, J. Anthrax as an example of the one health concept. Rev. Sci. Tech. 2014, 33, 593–604. [Google Scholar] [CrossRef]
- Fasanella, A.; Galante, D.; Garofolo, G.; Jones, M.H. Anthrax undervalued zoonosis. Vet. Microbiol. 2010, 140, 318–331. [Google Scholar] [CrossRef]
- Massei, G.; Genov, P.V. The environmental impact of wild boar. Galemys 2004, 16, 135–145. [Google Scholar]
- Krishna Rao, N.S.; Mohiyudekn, S. Tabanus flies as transmitters of anthrax-a field experience. Indian Vet. J. 1958, 38, 348–353. [Google Scholar]
- Turell, M.J.; Knudson, G.B. Mechanical transmission of Bacillus anthracis by stable flies (Stomoxys calcitrans) and mosquitos (Aedes aegypti and Aedes taeniorhynchus). Infect. Immun. 1987, 55, 1859–1861. [Google Scholar] [CrossRef]
- Rollins, D. Impacts of Feral Swine on Wildlife. In Proceedings of the First National Feral Swine Conference, Fort Worth, TX, USA, 2–3 June 1999. [Google Scholar]
- Eckert, K.D.; Keiter, D.A.; Beasley, J.C. Animal visitation to wild pig (Sus scrofa) wallow and implications for disease transmission. J. Wildl. Dis. 2019, 55, 488–493. [Google Scholar] [CrossRef]
- Chitlaru, T.; Gat, O.; Grosfeld, H.; Inbar, I.; Gozlan, Y.; Shafferman, A. Identification of in vivo-expressed immunogenic proteins by serological proteome analysis of the Bacillus anthracis secretome. Infect. Immun. 2007, 75, 2841–2852. [Google Scholar] [CrossRef] [PubMed]
- Morner, T.; Obendorf, D.L.; Artois, M.; Woodford, M.H. Surveillance and monitoring of wildlife diseases. Rev. Sci. Tech. 2002, 21, 67–76. [Google Scholar] [CrossRef] [PubMed]
| Animal ID | Sex | Times Exposed | Inoculum Dose (CFU/mL) | Route of Inoculation 1 | Animal Room |
|---|---|---|---|---|---|
| 7634 | F | 1 | 104 | i.n | 1 |
| 7635 | F | 1 | 104 | i.n | 1 |
| 7637 | F | 1 | 104 | i.n | 1 |
| 7618 | F | 1 | 107 | i.n | 1 |
| 7641 | F | 1 | 107 | i.n | 1 |
| 7636 | M | 1 | 107 | i.n | 1 |
| 7619 | F | 1 | 104 | s.c | 1 |
| 7621 | F | 1 | 104 | s.c | 1 |
| 7633 | M | 1 | 104 | s.c | 1 |
| 3915 | F | 3 | 104 | i.n | 2 |
| 3911 | M | 3 | 104 | i.n | 2 |
| 3920 | M | 3 | 104 | i.n | 2 |
| 3913 | F | 3 | 107 | i.n | 2 |
| 3912 | M | 3 | 107 | i.n | 2 |
| 3919 | M | 3 | 107 | i.n | 2 |
| Species | Strain [Reference] | Plasmid Content | |
|---|---|---|---|
| pag | cap | ||
| Bacillus cereus | UW85 [40] | − | − |
| Bacillus anthracis | Sterne 34F2 [41] | + | − |
| Bacillus anthracis | 1075.4 [42] | + | + |
| Animal ID | Inoculum Dose (CFU/mL) | Times Exposed | Nasal Swab Culture 1 +/−, (CFU/mL) | |||
|---|---|---|---|---|---|---|
| D14 | D28 | D42 | D56 | |||
| 7634 | 104 | 1 | − | + (10) | NA | NA |
| 7635 | 104 | 1 | − | − | NA | NA |
| 7637 | 104 | 1 | − | − | NA | NA |
| 7618 | 107 | 1 | + (80) | − | NA | NA |
| 7641 | 107 | 1 | − | + (10) | NA | NA |
| 7636 | 107 | 1 | − | + (20) | NA | NA |
| 3915 | 104 | 3 | + (220) | + (50) | + (50) | − |
| 3911 | 104 | 3 | + (TN) | + (60) | + (10) | + (30) |
| 3920 | 104 | 3 | + (390) | + (110) | − | − |
| 3913 | 107 | 3 | + (670) | + (180) | + (20) | − |
| 3912 | 107 | 3 | + (270) | + (20) | + (80) | − |
| 3919 | 107 | 3 | + (110) | + (160) | + (50) | + (10) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maison, R.M.; Priore, M.R.; Brown, V.R.; Bodenchuk, M.J.; Borlee, B.R.; Bowen, R.A.; Bosco-Lauth, A.M. Feral Swine as Indirect Indicators of Environmental Anthrax Contamination and Potential Mechanical Vectors of Infectious Spores. Pathogens 2023, 12, 622. https://doi.org/10.3390/pathogens12040622
Maison RM, Priore MR, Brown VR, Bodenchuk MJ, Borlee BR, Bowen RA, Bosco-Lauth AM. Feral Swine as Indirect Indicators of Environmental Anthrax Contamination and Potential Mechanical Vectors of Infectious Spores. Pathogens. 2023; 12(4):622. https://doi.org/10.3390/pathogens12040622
Chicago/Turabian StyleMaison, Rachel M., Maggie R. Priore, Vienna R. Brown, Michael J. Bodenchuk, Bradley R. Borlee, Richard A. Bowen, and Angela M. Bosco-Lauth. 2023. "Feral Swine as Indirect Indicators of Environmental Anthrax Contamination and Potential Mechanical Vectors of Infectious Spores" Pathogens 12, no. 4: 622. https://doi.org/10.3390/pathogens12040622
APA StyleMaison, R. M., Priore, M. R., Brown, V. R., Bodenchuk, M. J., Borlee, B. R., Bowen, R. A., & Bosco-Lauth, A. M. (2023). Feral Swine as Indirect Indicators of Environmental Anthrax Contamination and Potential Mechanical Vectors of Infectious Spores. Pathogens, 12(4), 622. https://doi.org/10.3390/pathogens12040622









