Clinical Evaluation of a Multiplex PCR Assay for Simultaneous Detection of 18 Respiratory Pathogens in Patients with Acute Respiratory Infections
Abstract
1. Introduction
2. Materials and Methods
2.1. Specimen Collection
2.2. Extraction and Purification of RNA/DNA
2.3. Detection of SARS-CoV-2 and 17 Other Respiratory Pathogens Using Real-Time Quantitative PCR
2.4. Detection of 18 Respiratory Pathogens (MPA Assay)
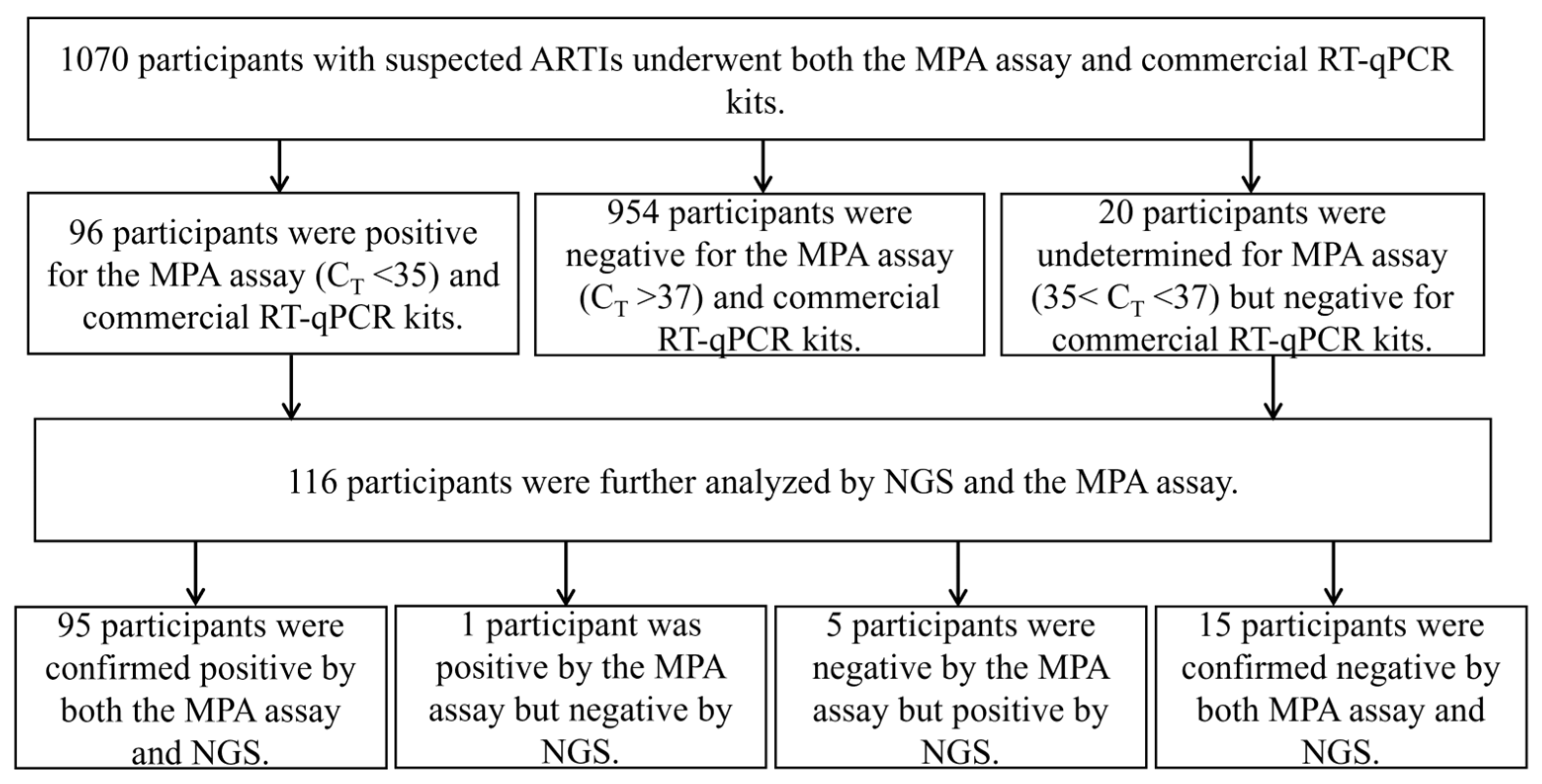
2.5. Validation of the MPA Assay Using NGS
2.6. Statistical Analysis
2.7. Ethics Statement
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liu, L.; Oza, S.; Hogan, D.; Chu, Y.; Perin, J.; Zhu, J.; Lawn, J.E.; Cousens, S.; Mathers, C.; Black, R.E. Global, regional, and national causes of under-5 mortality in 2000–15: An updated systematic analysis with implications for the Sustainable Development Goals. Lancet 2016, 388, 3027–3035. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. Weekly Epidemiological Update on COVID-19. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---30-november-2022 (accessed on 30 November 2022).
- Liu, R.; Han, H.; Liu, F.; Lv, Z.; Wu, K.; Liu, Y.; Feng, Y.; Zhu, C. Positive rate of RT-PCR detection of SARS-CoV-2 infection in 4880 cases from one hospital in Wuhan, China, from Jan to Feb 2020. Clin. Chim. Acta 2020, 505, 172–175. [Google Scholar] [CrossRef] [PubMed]
- Diao, B.; Wen, K.; Zhang, J.; Chen, J.; Han, C.; Chen, Y.; Wang, S.; Deng, G.; Zhou, H.; Wu, Y. Accuracy of a nucleocapsid protein antigen rapid test in the diagnosis of SARS-CoV-2 infection. Clin. Microbiol. Infect. 2020, 27, 289.e1–289.e4. [Google Scholar] [CrossRef] [PubMed]
- Baker, A.N.; Richards, S.-J.; Pandey, S.; Guy, C.S.; Ahmad, A.; Hasan, M.; Biggs, C.I.; Georgiou, P.G.; Zwetsloot, A.J.; Straube, A.; et al. Glycan-Based Flow-Through Device for the Detection of SARS-CoV-2. ACS Sens. 2021, 6, 3696–3705. [Google Scholar] [CrossRef]
- Hu, X.; Deng, Q.; Li, J.; Chen, J.; Wang, Z.; Zhang, X.; Fang, Z.; Li, H.; Zhao, Y.; Yu, P.; et al. Development and Clinical Application of a Rapid and Sensitive Loop-Mediated Isothermal Amplification Test for SARS-CoV-2 Infection. mSphere 2020, 5, e00808-20. [Google Scholar] [CrossRef]
- Jia, Z.; Yan, X.; Gao, L.; Ding, S.; Bai, Y.; Zheng, Y.; Cui, Y.; Wang, X.; Li, J.; Lu, G.; et al. Comparison of Clinical Characteristics Among COVID-19 and Non-COVID-19 Pediatric Pneumonias: A Multicenter Cross-Sectional Study. Front. Cell. Infect. Microbiol. 2021, 11, 663884. [Google Scholar] [CrossRef]
- Kıymet, E.; Böncüoğlu, E.; Şahinkaya, Ş.; Cem, E.; Çelebi, M.Y.; Düzgöl, M.; Kara, A.A.; Arıkan, K.; Aydın, T.; Işgüder, R.; et al. Distribution of spreading viruses during COVID-19 pandemic: Effect of mitigation strategies. Am. J. Infect. Control 2021, 49, 1142–1145. [Google Scholar] [CrossRef]
- Brendish, N.J.; Poole, S.; Naidu, V.V.; Mansbridge, C.T.; Norton, N.J.; Wheeler, H.; Presland, L.; Kidd, S.; Cortes, N.J.; Borca, F.; et al. Clinical impact of molecular point-of-care testing for suspected COVID-19 in hospital (COV-19POC): A prospective, interventional, non-randomised, controlled study. Lancet Respir. Med. 2020, 8, 1192–1200. [Google Scholar] [CrossRef]
- Zhao, M.-C.; Li, G.-X.; Zhang, D.; Zhou, H.-Y.; Wang, H.; Yang, S.; Wang, L.; Feng, Z.-S.; Ma, X.-J. Clinical evaluation of a new single-tube multiplex reverse transcription PCR assay for simultaneous detection of 11 respiratory viruses, Mycoplasma pneumoniae and Chlamydia in hospitalized children with acute respiratory infections. Diagn. Microbiol. Infect. Dis. 2017, 88, 115–119. [Google Scholar] [CrossRef]
- Fu, G.; Miles, A.; Alphey, L. Multiplex Detection and SNP Genotyping in a Single Fluorescence Channel. PLoS ONE 2012, 7, e30340. [Google Scholar] [CrossRef]
- Wang, J.; Xiao, T.; Xiao, F.; Hong, S.; Wang, S.; Lin, J.; Li, Y.; Wang, X.; Yan, K.; Zhuang, D. Time Distributions of Common Respiratory Pathogens Under the Spread of SARS-CoV-2 Among Children in Xiamen, China. Front. Pediatr. 2021, 9, 584874. [Google Scholar] [CrossRef] [PubMed]
- Zhu, G.; Xu, D.; Zhang, Y.; Wang, T.; Zhang, L.; Gu, W.; Shen, M. Epidemiological characteristics of four common respiratory viral infections in children. Virol. J. 2021, 18, 10. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Wang, H.; Liu, A.; Wang, R.; Zhi, T.; Zheng, Y.; Bao, Y.; Chen, Y.; Wang, W. Comparison of 11 respiratory pathogens among hospitalized children before and during the COVID-19 epidemic in Shenzhen, China. Virol. J. 2021, 18, 202. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Chen, L.; Ding, Y.; Zhang, J.; Hua, J.; Geng, Q.; Ya, X.; Zeng, S.; Wu, J.; Jiang, Y.; et al. Viral etiology of medically attended influenza-like illnesses in children less than five years old in Suzhou, China, 2011–2014. J. Med. Virol. 2016, 88, 1334–1340. [Google Scholar] [CrossRef]
- Lai, C.-C.; Wang, C.-Y.; Hsueh, P.-R. Co-infections among patients with COVID-19: The need for combination therapy with non-anti-SARS-CoV-2 agents? J. Microbiol. Immunol. Infect. 2020, 53, 505–512. [Google Scholar] [CrossRef] [PubMed]
- Leuzinger, K.; Roloff, T.; Gosert, R.; Sogaard, K.; Naegele, K.; Rentsch, K.; Bingisser, R.; Nickel, C.H.; Pargger, H.; Bassetti, S.; et al. Epidemiology of Severe Acute Respiratory Syndrome Coronavirus 2 Emergence Amidst Community-Acquired Respiratory Viruses. J. Infect. Dis. 2020, 222, 1270–1279. [Google Scholar] [CrossRef]
- De Mello Malta, F.; Amgarten, D.; Val, F.C.; Cervato, M.C.; de Azevedo, B.M.C.; de Souza Basqueira, M.; dos Santos Alves, C.O.; Nobrega, M.S.; de Souza Reis, R.; Sebe, P.; et al. Mass molecular testing for COVID19 using NGS-based technology and a highly scalable workflow. Sci. Rep. 2021, 11, 7122. [Google Scholar] [CrossRef]
- Wu, Z.-Q.; Zhang, Y.; Zhao, N.; Yu, Z.; Pan, H.; Chan, T.-C.; Zhang, Z.-R.; Liu, S.-L. Comparative Epidemiology of Human Fatal Infections with Novel, High (H5N6 and H5N1) and Low (H7N9 and H9N2) Pathogenicity Avian Influenza A Viruses. Int. J. Environ. Res. Public Health 2017, 14, 263. [Google Scholar] [CrossRef]
- Pan, M.; Gao, R.; Lv, Q.; Huang, S.; Zhou, Z.; Yang, L.; Li, X.; Zhao, X.; Zou, X.; Tong, W.; et al. Human infection with a novel, highly pathogenic avian influenza A (H5N6) virus: Virological and clinical findings. J. Infect. 2015, 72, 52–59. [Google Scholar] [CrossRef]
- Qin, Y.; Horby, P.W.; Tsang, T.K.; Chen, E.; Gao, L.; Ou, J.; Nguyen, T.H.; Duong, T.N.; Gasimov, V.; Feng, L.; et al. Differences in the Epidemiology of Human Cases of Avian Influenza A(H7N9) and A(H5N1) Viruses Infection. Clin. Infect. Dis. 2015, 61, 563–571. [Google Scholar] [CrossRef]
- Sakellariou, G.K.; Bilski, M.; Moreau, M.; Stofanko, M.; Liu, Y.; Boland, E.; Kapadia, D.; Harrison, M.; Fu, G. Principles and analytical performance of Papilloplex® HR-HPV, a new commercial CE-IVD molecular diagnostic test for the detection of high-risk HPV genotypes. Diagn. Microbiol. Infect. Dis. 2019, 95, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Luo, T.; Jiang, L.; Sun, W.; Fu, G.; Mei, J.; Gao, Q. Multiplex Real-Time PCR Melting Curve Assay To Detect Drug-Resistant Mutations of Mycobacterium tuberculosis. J. Clin. Microbiol. 2011, 49, 3132–3138. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bhatia, R.; Serrano, I.; Wennington, H.; Graham, C.; Cubie, H.; Boland, E.; Fu, G.; Cuschieri, K. Evaluation of a Novel Single-Tube Method for Extended Genotyping of Human Papillomavirus. J. Clin. Microbiol. 2018, 56, e01687-17. [Google Scholar] [CrossRef]
- Visseaux, B.; Le Hingrat, Q.; Collin, G.; Bouzid, D.; Lebourgeois, S.; Le Pluart, D.; Deconinck, L.; Lescure, F.-X.; Lucet, J.-C.; Bouadma, L.; et al. Evaluation of the QIAstat-Dx Respiratory SARS-CoV-2 Panel, the First Rapid Multiplex PCR Commercial Assay for SARS-CoV-2 Detection. J. Clin. Microbiol. 2020, 58, e00630-20. [Google Scholar] [CrossRef]
- Cassidy, H.; van Genne, M.; Lizarazo-Forero, E.; Niesters, H.G.M.; Gard, L. Evaluation of the QIAstat-Dx RP2.0 and the BioFire FilmArray RP2.1 for the Rapid Detection of Respiratory Pathogens Including SARS-CoV-2. Front. Microbiol. 2022, 13, 854209. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.-C.; Hsiao, C.-T.; Chen, W.-L.; Su, Y.-D.; Hsueh, P.-R. BioFire FilmArray respiratory panel RP2.1 for SARS-CoV-2 detection: The pitfalls. J. Infect. 2022, 85, e149–e151. [Google Scholar] [CrossRef] [PubMed]
- Creager, H.M.; Cabrera, B.; Schnaubelt, A.; Cox, J.L.; Cushman-Vokoun, A.M.; Shakir, S.M.; Tardif, K.D.; Huang, M.-L.; Jerome, K.R.; Greninger, A.L.; et al. Clinical evaluation of the BioFire® Respiratory Panel 2.1 and detection of SARS-CoV-2. J. Clin. Virol. 2020, 129, 104538. [Google Scholar] [CrossRef]
| Pathogen | Primers | Sequence (5′–3′) | Ampliconsize (bp) |
|---|---|---|---|
| SARS-CoV-2-N | Seq-F | CACCGCTCTCACTCAACATG | 120 |
| Seq-R | CGTCTGGTAGCTCTTCGGTA | ||
| SARS-CoV-2-ORF1ab | Seq-F | GGTGCTTGCATACGTAGACC | 120 |
| Seq-R | ATCACAACCTGGAGCATTGC | ||
| IFA | Seq-F | TCTCATGGAGTGGCTAAAGACA | 471 |
| Seq-R | TGTTCACTCGATCCAGCCAT | ||
| IFB | Seq-F | TGGAGAAGGCAAAGCAGAAC | 490 |
| Seq-R | GACCATCTGCATTTCCCGTC | ||
| RSV | Seq-F | AGGTGGGGCAAATATGGAAAC | 440 |
| Seq-R | TGTCATGTGTTGGGTTGAGTG | ||
| HADV | Seq-F | CATCTCGATCCAGCAGACCT | 456 |
| Seq-R | GATGAGCCGGATCTGACCTG | ||
| HMPV | Seq-F | TGTGCGGCAATTTTCAGACA | 549 |
| Seq-R | TTGTARCAAGCAACCARAGC | ||
| HBOV | Seq-F | AACGTCGTCTAACTGCTCCA | 451 |
| Seq-R | TGCGAGTAGAGTGCCAGTAG | ||
| MP | Seq-F | AAACTGAACCTCCCCGCTTA | 499 |
| Seq-R | TGGCACTACTTGTAGCTGCT | ||
| CP | Seq-F | GATCCTTGCGCTACTTGGTG | 600 |
| Seq-R | GTCTGTTGGCAAGGGGAAAG | ||
| HRV | Seq-F | TGAGGCTAGARATTCCCCAC | 242 |
| Seq-R | AGAGAAACACGGACACCCAA | ||
| COV-229E | Seq-F | GCGTGTTGAAGGTGTTGTCT | 520 |
| Seq-R | TCTGGGGCCAAAACATTGTG | ||
| COV-NL63 | Seq-F | GCAGTCGTTCTTCAACTCGT | 524 |
| Seq-R | CTGCTCAATGAACTTAGGAAGGT | ||
| COV-OC43 | Seq-F | GCAACAGAACCCCTACCTCT | 526 |
| Seq-R | CGCTGTGGTTTTGGACTCAT | ||
| COV-HKU1 | Seq-F | ACTCCCGGTCATTATGCTGG | 538 |
| Seq-R | GAGGCAAAATCGTACCAGGC | ||
| PIV-1 | Seq-F | GGCCAAAGATTGTTGTCGAGA | 215 |
| Seq-R | GTTGCAGTCTGGGTTTCCTG | ||
| PIV-2 | Seq-F | AGCACGGGGTTCCTATGTYA | 544 |
| Seq-R | TGCTGCTTTGTGATTGGTGT | ||
| PIV-3 | Seq-F | CAGAACCCCGTCCTTAGTGA | 492 |
| Seq-R | CACCCAGTTGTGTTGCAGAT | ||
| PIV-4 | Seq-F | CAGGCCACATCAATGCAGAA | 572 |
| Seq-R | AAGAACGCACTCATTCCGAC | ||
| RNP | Seq-F | TGCATAACTGTAACAGAGAAACTACCA | 148 |
| Seq-R | TGAGGGCACTGGAAATTGTATAC |
| Patients | Number (%) (n = 1070) |
|---|---|
| Age Median [IQR] | 31.75 (2–58) |
| Male | 617 (57.66) |
| Signs and symptoms at admission | |
| Fever | 637 (59.53) |
| Cough | 650 (60.74) |
| Expectoration | 441 (41,21) |
| Fatigue | 94 (8.79) |
| Muscle or body aches | 72 (6.73) |
| Headache | 63 (5.89) |
| Sore throat | 74 (6.92) |
| Chest pain | 39 (3.64) |
| Shortness of breath | 245 (22.90) |
| Runny or stuffy nose | 109 (10.19) |
| Diarrhea | 30 (2.80) |
| Nausea or vomiting | 59 (5.51) |
| Trouble breathing | 65 (6.07) |
| Pathogens | No. of Specimens with Indicated MPA Assay/NGS Result | Performance of the MPA Assay Compared with NGS | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| +/+ | +/− | −/+ | −/− | Se (%) [95% CI] | Sp (%) [95% CI] | PPV (%) [95% CI] | NPV (%) [95% CI] | Kappa | McNemar Test (p) | |
| COVID-19 | 28 | 1 | 1 | 86 | 96.55 | 98.85 | 96.55 | 98.85 | 1 | 0.954 |
| IF A | 11 | 0 | 3 | 102 | 78.57 | 100.00 | 100.00 | 97.14 | 0.866 | 0.250 |
| IF B | 4 | 0 | 0 | 112 | 100.00 | 100.00 | 100.00 | 100.00 | 1 | 1 |
| PIV 1 | 0 | 0 | 0 | 116 | 100.00 | 100.00 | ||||
| PIV 2 | 3 | 1 | 0 | 112 | 100.00 | 99.12 | 75.00 | 100.00 | 0.853 | 1 |
| PIV 3 | 2 | 0 | 0 | 114 | 100.00 | 100.00 | 100.00 | 100.00 | 1.000 | 1 |
| PIV 4 | 0 | 0 | 0 | 116 | 100.00 | 100.00 | ||||
| HADV | 9 | 0 | 1 | 106 | 90.00 | 100.00 | 100.00 | 99.07 | 0.943 | 1 |
| MP | 25 | 0 | 1 | 90 | 96.15 | 100.00 | 100.00 | 98.90 | 0.975 | 1 |
| CP | 1 | 0 | 1 | 114 | 50.00 | 100.00 | 100.00 | 99.13 | 0.664 | 1 |
| HRV | 10 | 0 | 0 | 108 | 100.00 | 100.00 | 100.00 | 100.00 | 1 | 1 |
| RSV | 21 | 0 | 0 | 95 | 100.00 | 100.00 | 100.00 | 100.00 | 1 | 1 |
| HBOV | 0 | 0 | 0 | 116 | 100.00 | 100.00 | ||||
| HMPV | 1 | 0 | 0 | 115 | 100.00 | 100.00 | 100.00 | 100.00 | 1 | 1 |
| COV 229E | 5 | 0 | 0 | 111 | 100.00 | 100.00 | 100.00 | 100.00 | 1 | 1 |
| COV HKU1 | 0 | 0 | 0 | 116 | 100.00 | 100.00 | ||||
| COV NL63 | 0 | 0 | 0 | 116 | 100.00 | 100.00 | ||||
| COV OC43 | 1 | 0 | 0 | 115 | 100.00 | 100.00 | 100.00 | 100.00 | 1 | 1 |
| Total | 95 | 1 | 5 | 15 | 95.00 [88.17–98.14] | 93.75 [67.71–99.67] | 98.96 [93.51–99.9] | 75.00 [50.59–90.41] | 0.803 | 0.219 |
| Specimen Number | MPA | NGS |
|---|---|---|
| 7806 | SARS-CoV-2N/ORF1AB (35.3) | − |
| 2877 | − | SARS-CoV-2-ORF1AB |
| 2804 | − | CP |
| 2840 | − | IFA |
| 512 | − | IFA |
| 522 | − | IFA |
| 2809 | PIV2/MP/RSV | MP/RSV |
| 2831 | MP | MP/HADV |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, W.; Wang, X.; Cui, W.; Yuan, L.; Hu, X. Clinical Evaluation of a Multiplex PCR Assay for Simultaneous Detection of 18 Respiratory Pathogens in Patients with Acute Respiratory Infections. Pathogens 2023, 12, 21. https://doi.org/10.3390/pathogens12010021
Li W, Wang X, Cui W, Yuan L, Hu X. Clinical Evaluation of a Multiplex PCR Assay for Simultaneous Detection of 18 Respiratory Pathogens in Patients with Acute Respiratory Infections. Pathogens. 2023; 12(1):21. https://doi.org/10.3390/pathogens12010021
Chicago/Turabian StyleLi, Wenmin, Xiaoxiao Wang, Wenhao Cui, Leyong Yuan, and Xuejiao Hu. 2023. "Clinical Evaluation of a Multiplex PCR Assay for Simultaneous Detection of 18 Respiratory Pathogens in Patients with Acute Respiratory Infections" Pathogens 12, no. 1: 21. https://doi.org/10.3390/pathogens12010021
APA StyleLi, W., Wang, X., Cui, W., Yuan, L., & Hu, X. (2023). Clinical Evaluation of a Multiplex PCR Assay for Simultaneous Detection of 18 Respiratory Pathogens in Patients with Acute Respiratory Infections. Pathogens, 12(1), 21. https://doi.org/10.3390/pathogens12010021






