Impact of ASFV Detergent Inactivation on Biomarkers in Serum and Saliva Samples
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
Animal Trial Samples
2.2. Detergent and Heat Treatments
2.3. Virus Isolation and Titration
2.4. Assessment of Cell Toxicity
2.5. Effects of ASFV Inactivation in Different Biomarkers
3. Results
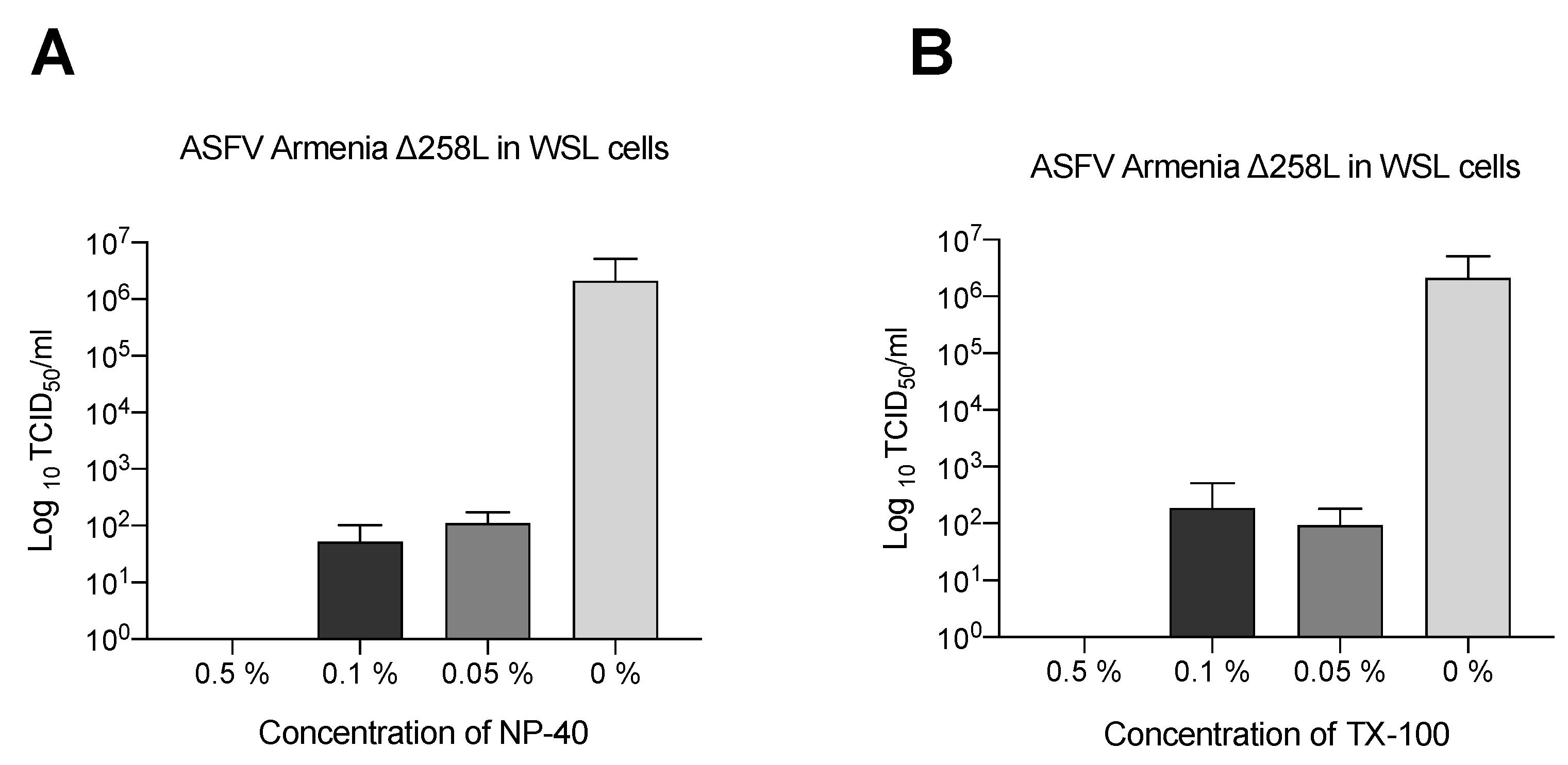
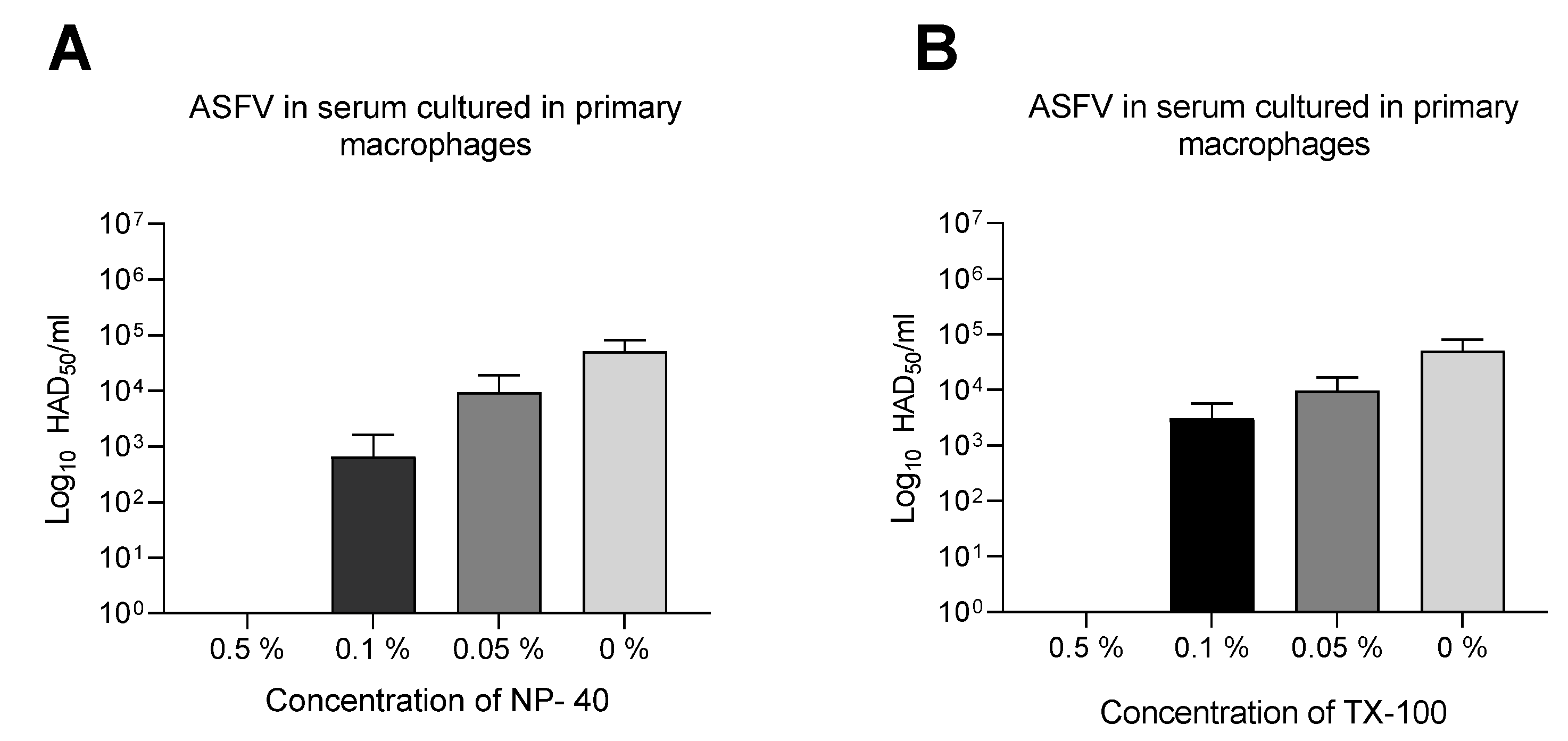
3.1. Triton X-100 and NP-40 Produce Dilution-Dependent Inactivation
3.2. Virus Infectivity
3.3. Effects of ASFV Inactivation on Different Biomarkers
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gallardo, C.; Fernández-Pinero, J.; Pelayo, V.; Gazaev, I.; Markowska-Daniel, I.; Pridotkas, G.; Nieto, R.; Fernández-Pacheco, P.; Bokhan, S.; Nevolko, O.; et al. Genetic Variation among African Swine Fever Genotype II Viruses, Eastern and Central Europe. Emerg. Infect. Dis. 2014, 20, 1544–1547. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gallardo, C.; Soler, A.; Nieto, R.; Cano, C.; Pelayo, V.; Sánchez, M.A.; Pridotkas, G.; Fernandez-Pinero, J.; Briones, V.; Arias, M. Experimental Infection of Domestic Pigs with African Swine Fever Virus Lithuania 2014 Genotype II Field Isolate. Transbound. Emerg. Dis. 2015, 64, 300–304. [Google Scholar] [CrossRef] [PubMed]
- Sauter-Louis, C.; Conraths, F.J.; Probst, C.; Blohm, U.; Schulz, K.; Sehl, J.; Fischer, M.; Forth, J.H.; Zani, L.; Depner, K.; et al. African Swine Fever in Wild Boar in Europe—A Review. Viruses 2021, 13, 1717. [Google Scholar] [CrossRef] [PubMed]
- Ward, M.P.; Tian, K.; Nowotny, N. African Swine Fever, the forgotten pandemic. Transbound. Emerg. Dis. 2021, 68, 2637–2639. [Google Scholar] [CrossRef]
- Penrith, M.-L.; Thomson, G.; Bastos, A.; Phiri, O.; Lubisi, B.; Du Plessis, E.; Macome, F.; Pinto, F.; Botha, B.; Esterhuysen, J. An investigation into natural resistance to African swine fever in domestic pigs from an endemic area in southern Africa. Rev. Sci. Tech. OIE 2004, 23, 965–977. [Google Scholar] [CrossRef]
- Blome, S.; Franzke, K.; Beer, M. African swine fever—A review of current knowledge. Virus Res. 2020, 287, 198099. [Google Scholar] [CrossRef]
- Lopez-Arjona, M.; Tecles, F.; Mateo, S.V.; Contreras-Aguilar, M.D.; Martínez-Miró, S.; Cerón, J.J.; Martínez-Subiela, S. Measurement of cortisol, cortisone and 11beta-hydroxysteroid dehydrogenase type 2 activity in hair of sows during different phases of the reproductive cycle. Vet. J. 2020, 259–260, 105458. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Cordón, P.J.; Cerón, J.J.; Núñez, A.; Martínez-Subiela, S.; Pedrera, M.; Romero-Trevejo, J.L.; Garrido, M.R.; Gómez-Villamandos, J.C. Serum concentrations of C-reactive protein, serum amyloid A, and haptoglobin in pigs inoculated with African swine fever or classical swine fever viruses. Am. J. Vet.-Res. 2007, 68, 772–777. [Google Scholar] [CrossRef] [PubMed]
- Carpintero, R.; Alonso, C.; Piñeiro, M.; Iturralde, M.; Andrés, M.; Le Potier, M.F.; Madec, F.; Álava, M.Á.; Piñeiro, A.; Lampreave, F. Pig major acute-phase protein and apolipoprotein A-I responses correlate with the clinical course of experimentally induced African Swine Fever and Aujeszky’s disease. Vet. Res. 2007, 38, 741–753. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mur, L.; Gallardo, C.; Soler, A.; Zimmermman, J.; Pelayo, V.; Nieto, R.; Sánchez-Vizcaíno, J.M.; Arias, M. Potential use of oral fluid samples for serological diagnosis of African swine fever. Vet.-Microbiol. 2013, 165, 135–139. [Google Scholar] [CrossRef] [PubMed]
- Cerón, J.J.; Contreras-Aguilar, M.D.; Escribano, D.; Martínez-Miró, S.; López-Martínez, M.J.; Ortín-Bustillo, A.; Franco-Martínez, L.; Rubio, C.P.; Muñoz-Prieto, A.; Tvarijonaviciute, A.; et al. Basics for the potential use of saliva to evaluate stress, inflammation, immune system, and redox homeostasis in pigs. BMC Vet.-Res. 2022, 18, 81. [Google Scholar] [CrossRef]
- Ukkonen, P.; Korpela, J.; Suni, J.; Hedman, K. Inactivation of human immunodeficiency virus in serum specimens as a safety measure for diagnostic immunoassays. Eur. J. Clin. Microbiol. Infect. Dis. 1988, 7, 518–523. [Google Scholar] [CrossRef] [PubMed]
- Song, H.; Li, J.; Shi, S.; Yan, L.; Zhuang, H.; Li, K. Thermal stability and inactivation of hepatitis C virus grown in cell culture. Virol. J. 2010, 7, 40. [Google Scholar] [CrossRef] [Green Version]
- Hübner, A.; Petersen, B.; Keil, G.M.; Niemann, H.; Mettenleiter, T.C.; Fuchs, W. Efficient inhibition of African swine fever virus replication by CRISPR/Cas9 targeting of the viral p30 gene (CP204L). Sci. Rep. 2018, 8, 1449. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hübner, A.; Keßler, C.; Pannhorst, K.; Forth, J.H.; Kabuuka, T.; Karger, A.; Mettenleiter, T.C.; Fuchs, W. Identification and characterization of the 285L and K145R proteins of African swine fever virus. J. Gen. Virol. 2019, 100, 1303–1314. [Google Scholar] [CrossRef] [PubMed]
- Roszyk, H.; Franzke, K.; Breithaupt, A.; Deutschmann, P.; Pikalo, J.; Carrau, T.; Blome, S.; Sehl-Ewert, J. The Role of Male Reproductive Organs in the Transmission of African Swine Fever—Implications for Transmission. Viruses 2021, 14, 31. [Google Scholar] [CrossRef] [PubMed]
- Tanneberger, F.; El Wahed, A.A.; Fischer, M.; Deutschmann, P.; Roszyk, H.; Carrau, T.; Blome, S.; Truyen, U. Efficacy of Liming Forest Soil in the Context of African Swine Fever Virus. Viruses 2022, 14, 734. [Google Scholar] [CrossRef] [PubMed]
- Rubio, C.P.; Mainau, E.; Cerón, J.J.; Contreras-Aguilar, M.D.; Martínez-Subiela, S.; Navarro, E.; Tecles, F.; Manteca, X.; Escribano, D. Biomarkers of oxidative stress in saliva in pigs: Analytical validation and changes in lactation. BMC Vet.-Res. 2019, 15, 144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tecles, F.; Fuentes, P.; Subiela, S.M.; Parra, M.; Muñoz, A.; Cerón, J. Analytical validation of commercially available methods for acute phase proteins quantification in pigs. Res. Vet.-Sci. 2007, 83, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Pastorino, B.; Touret, F.; Gilles, M.; Luciani, L.; De Lamballerie, X.; Charrel, R.N. Evaluation of Chemical Protocols for Inactivating SARS-CoV-2 Infectious Samples. Viruses 2020, 12, 624. [Google Scholar] [CrossRef] [PubMed]
- Franco-Martínez, L.; Cerón, J.J.; Vicente-Romero, M.R.; Bernal, E.; Cantero, A.T.; Tecles, F.; Resalt, C.S.; Martínez, M.; Tvarijonaviciute, A.; Martínez-Subiela, S. Salivary Ferritin Changes in Patients with COVID-19. Int. J. Environ. Res. Public Health 2021, 19, 41. [Google Scholar] [CrossRef] [PubMed]
- Patterson, E.I.; Prince, T.; Anderson, E.R.; Casas-Sanchez, A.; Smith, S.L.; Cansado-Utrilla, C.; Solomon, T.; Griffiths, M.J.; Acosta-Serrano, Á.; Turtle, L.; et al. Methods of Inactivation of SARS-CoV-2 for Downstream Biological Assays. J. Infect. Dis. 2020, 222, 1462–1467. [Google Scholar] [CrossRef]
- Prince, A.; Horowitz, B.; Horowitz, M.; Zang, E. The development of virus-free labile blood derivatives? A review. Eur. J. Epidemiol. 1987, 3, 103–118. [Google Scholar] [CrossRef] [PubMed]
- Rubio, C.P.; Franco-Martínez, L.; Resalt, C.S.; Torres-Cantero, A.; Morata-Martínez, I.; Bernal, E.; Alcaraz, M.J.; Vicente-Romero, M.R.; Martínez-Subiela, S.; Tvarijonaviciute, A.; et al. Evaluation of different sample treatments options in a simple and safe procedure for the detection of SARS-CoV-2 in saliva. Int. J. Infect. Dis. 2021, 108, 413–418. [Google Scholar] [CrossRef] [PubMed]
- Yangüela, B.D.E.; Gracia, J.R.; González, G.M.; Tello, B.C.G.; Roldán, M.R.; Del Castaño, V.A. Microvascular pulmonary tumor embolism in a patient with urothelial tumor. An. Sist. Sanit. Navar. 2015, 38, 339–343. [Google Scholar] [CrossRef]
- Hersberger, M.; Nusbaumer, C.; Scholer, A.; Knöpfli, V.; Von Eckardstein, A. Influence of Practicable Virus Inactivation Procedures on Tests for Frequently Measured Analytes in Plasma. Clin. Chem. 2004, 50, 944–946. [Google Scholar] [CrossRef]
| Treatment | Infectious Titers before Treatment | Titers after Treatment | Titers after Virus Isolation at the 3rd Cell Passage |
|---|---|---|---|
| 0.5% (v/v) Triton X-100 | |||
| ASFV in porcine serum (HAD50) | 5.07 × 104 | negative | negative |
| ASFV in porcine saliva (HAD50) | negative | negative | negative |
| ASFV in culture medium (TCID50) | 2.12 × 106 | negative | negative |
| 0.5% (v/v) NP-40 | |||
| ASFV in porcine serum (HAD50) | 5.07 × 104 | negative | negative |
| ASFV in porcine saliva (HAD50) | negative | negative | negative |
| ASFV in culture medium (TCID50) | 2.12 × 106 | negative | negative |
| Serum | Saliva | ||||||
|---|---|---|---|---|---|---|---|
| NT | TX-100 | NP-40 | NT | TX-100 | NP-40 | 95 °C | |
| Cortisol | 100 | 112 (105–127) * | 102 (98.7–112) | 100 | 117 (88.7–155) | 136 (104–235) | 0 (0–0) * |
| Amylase/Alpha-amylase | 100 | 91.6 (89.7–92.6) *** | 99.2 (97.1–100) | 100 | 90.8 (88.4–102) | 95.3 (91.6–113) | 0 (0–0) *** |
| Haptoglobin | 100 | 83.5 (71.8–100) * | 96.5 (88.7–113) | 100 | 91.5 (81.7–119) | 128 (114–182) | 0 (0–0) ** |
| tADA | 100 | 91 (88.5–95.2) *** | 93.7 (86.9–97.1) * | 100 | 95.8 (91.5–98.5) | 100 (93.9–104) | 0 (0–0.1) *** |
| ADA2 | 100 | 108 (105–110) | 112 (111–114) *** | 100 | 97.4 (88.8–114) | 103 (91.4–120) | 0 (0–19.3) ** |
| CUPRAC | 100 | 118 (112–124) * | 112 (110–118) | 100 | 101 (95.5–113) | 110 (103–112) | 98.4 (94.7–101) |
| FRAP/FRAS | 100 | 98.2 (96.9–99.8) | 98 (93.8–98.8) ** | 100 | 90.1 (87.3–93.3) * | 91.4 (88.5–94.2) * | 98. (88.3–105) |
| TEACH | 100 | 93.4 (90.3–95.8) *** | 97.7 (94–100) | 100 | 99.4 (94.9–101) | 104 (94.9–108) | 81.7 (78.3–90) ** |
| GGT | 100 | 97.8 (96–99.2) * | 99.8 (97.9–101) | 100 | 193 (131–288) * | 123 (111–167) | 0 (0–25) * |
| LDH | 100 | 100 (97.8–103) | 102 (102–104) * | 100 | 56.2 (46.2–71.4) * | 98 (88.3–101) | 0.1 (0–2.4) *** |
| TP | 100 | 93.5 (91.7–95.5) * | 102 (100–103) | 100 | 91.5 (86.7–94.5) | 124 (118–134) * | 120 (115–123) |
| Serum | Saliva | ||||
|---|---|---|---|---|---|
| TX-100 | NP-40 | TX-100 | NP-40 | 95 °C | |
| Cortisol | r = 0.879; p = 0.001 | r = 0.867; p = 0.002 | r = 0.4895; p = 0.11 | r = 0.6294; p = 0.032 | r = 0.0843; p = 0.895 |
| Amylase/Alpha-amylase | r = 0.9879; p = 0.001 | r = 0.9879; p = 0.001 | r = 1; p = 0.001 | r = 1; p = 0.001 | r = 0.1741; p = 0.8 |
| Haptoglobin | r = 0.9758; p = 0.001 | r = 0.9879; p = 0.001 | r = 0.9429; p = 0.017 | r = 1; p = 0.003 | r = 0.1243; p = 0.79 |
| tADA | r = 0.9726; p = 0.001 | r = 0.9605; p = 0.001 | r = 0.9879; p = 0.001 | r = 0.9515; p = 0.001 | r = −0.2593; p = 0.4656 |
| ADA2 | r = 0.8831; p = 0.001 | r = 0.9319; p = 0.001 | r = 0.9205; p = 0.001 | r = 0.9146; p = 0.001 | r = −0.02055; p = 0.9558 |
| CUPRAC | r = 0.7333; p = 0.02 | r = 0.9879; p = 0.001 | r = 0.9273; p = 0.001 | r = 0.9515; p = 0.001 | r = 0.9636; p = 0.001 |
| FRAP | r = 0.8061; p = 0.007 | r = 0.9515; p = 0.001 | r = 1; p = 0.001 | r = 0.9758; p = 0.001 | r = 0.9785; p = 0.001 |
| TEACH | r = 0.7939; p = 0.009 | r = 0.903; p = 0.009 | r = 0.9758; p = 0.001 | r = 0.9636; p = 0.001 | r = 0.9758; p = 0.001 |
| GGT | r = 0.9273; p = 0.001 | r = 0.9879; p = 0.001 | r = 0.924; p = 0.001 | r = 0.9024; p = 0.001 | r = −0.1524; p = 0.716 |
| LDH | r = 0.8061; p = 0.007 | r = 0.9273; p = 0.001 | r = 0.8788; p = 0.001 | r = 0.9273; p = 0.001 | r = 0.4282; p = 0.219 |
| TP | r = 0.7815; p = 0.016 | r = 0.8452; p = 0.006 | r = 0.9636; p = 0.001 | r = 0.9879; p = 0.001 | r = 0.9879; p = 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Franco-Martínez, L.; Beer, M.; Martínez-Subiela, S.; García-Manzanilla, E.; Blome, S.; Carrau, T. Impact of ASFV Detergent Inactivation on Biomarkers in Serum and Saliva Samples. Pathogens 2022, 11, 750. https://doi.org/10.3390/pathogens11070750
Franco-Martínez L, Beer M, Martínez-Subiela S, García-Manzanilla E, Blome S, Carrau T. Impact of ASFV Detergent Inactivation on Biomarkers in Serum and Saliva Samples. Pathogens. 2022; 11(7):750. https://doi.org/10.3390/pathogens11070750
Chicago/Turabian StyleFranco-Martínez, Lorena, Martin Beer, Silvia Martínez-Subiela, Edgar García-Manzanilla, Sandra Blome, and Tessa Carrau. 2022. "Impact of ASFV Detergent Inactivation on Biomarkers in Serum and Saliva Samples" Pathogens 11, no. 7: 750. https://doi.org/10.3390/pathogens11070750
APA StyleFranco-Martínez, L., Beer, M., Martínez-Subiela, S., García-Manzanilla, E., Blome, S., & Carrau, T. (2022). Impact of ASFV Detergent Inactivation on Biomarkers in Serum and Saliva Samples. Pathogens, 11(7), 750. https://doi.org/10.3390/pathogens11070750








