An Improvement in Diagnostic Blood Culture Conditions Allows for the Rapid Detection and Isolation of the Slow Growing Pathogen Yersinia pestis
Abstract
1. Introduction
2. Results and Discussion
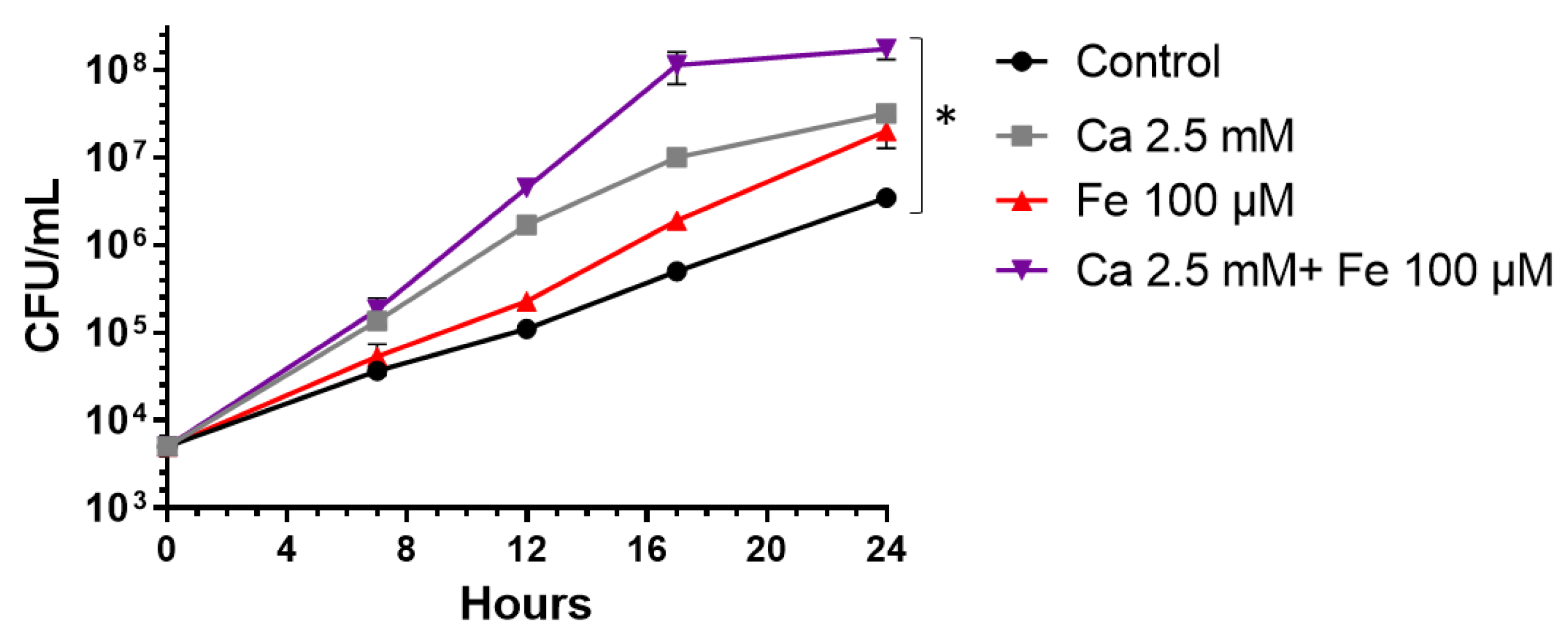
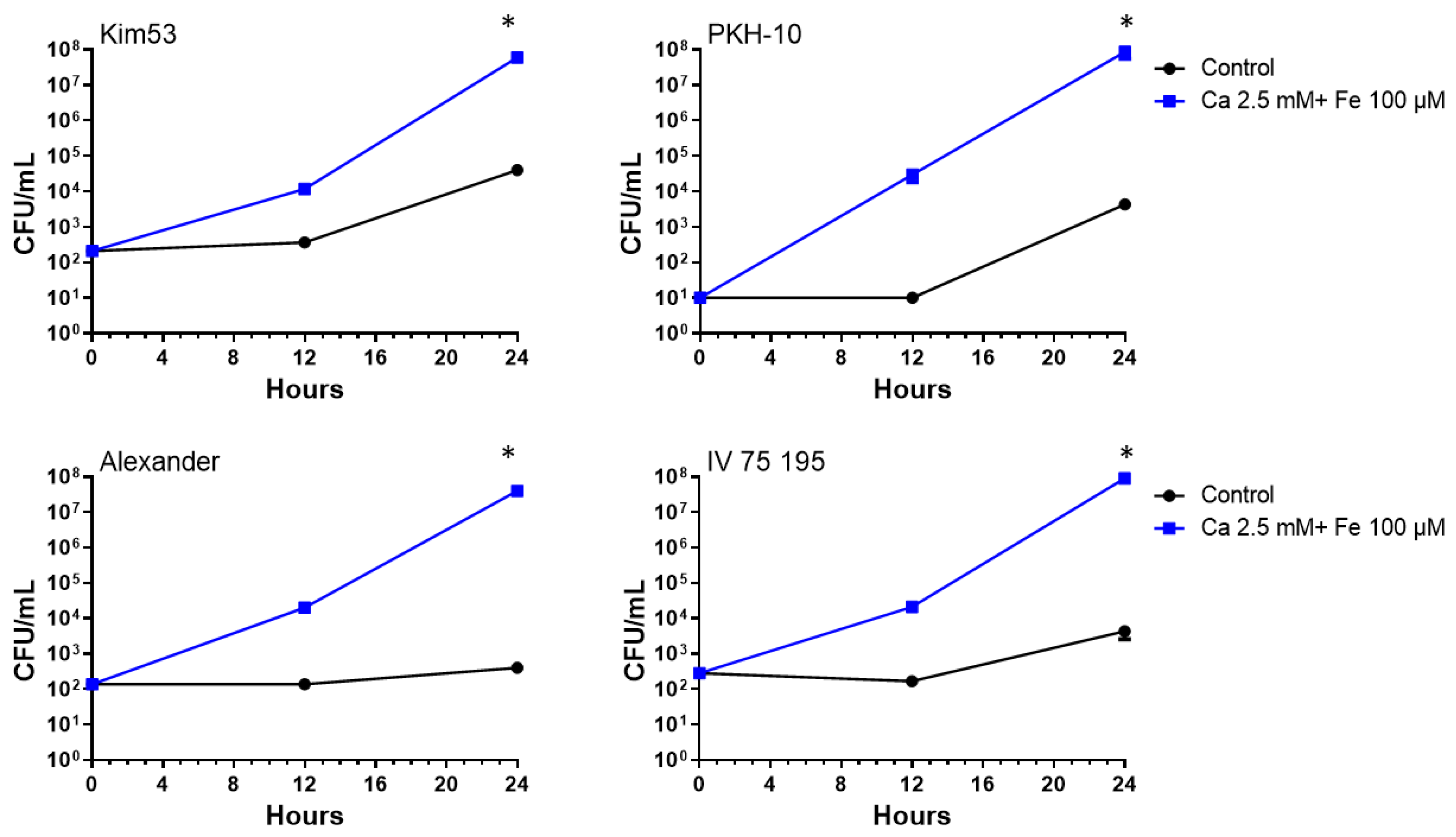
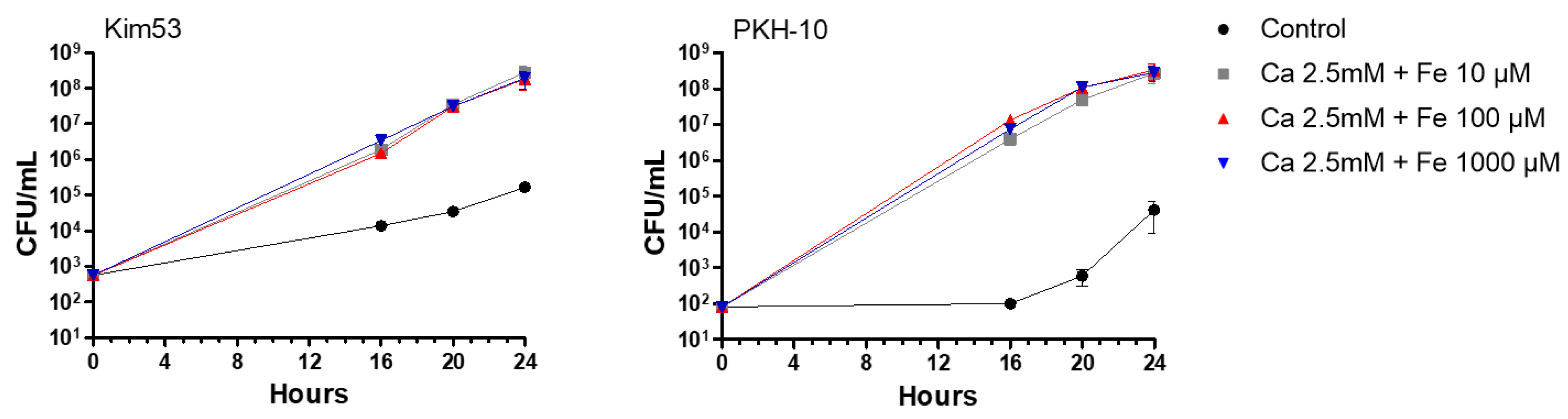
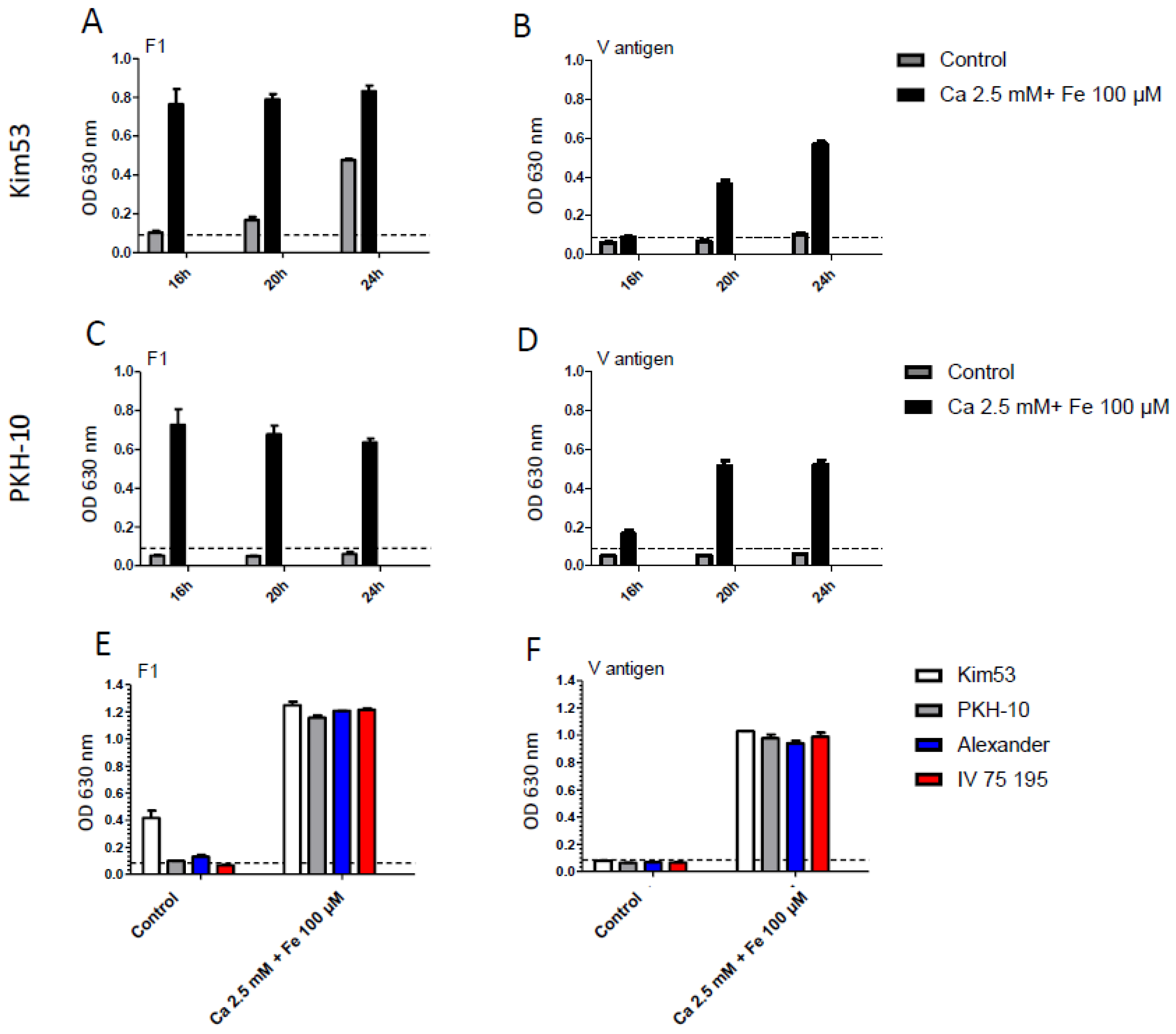
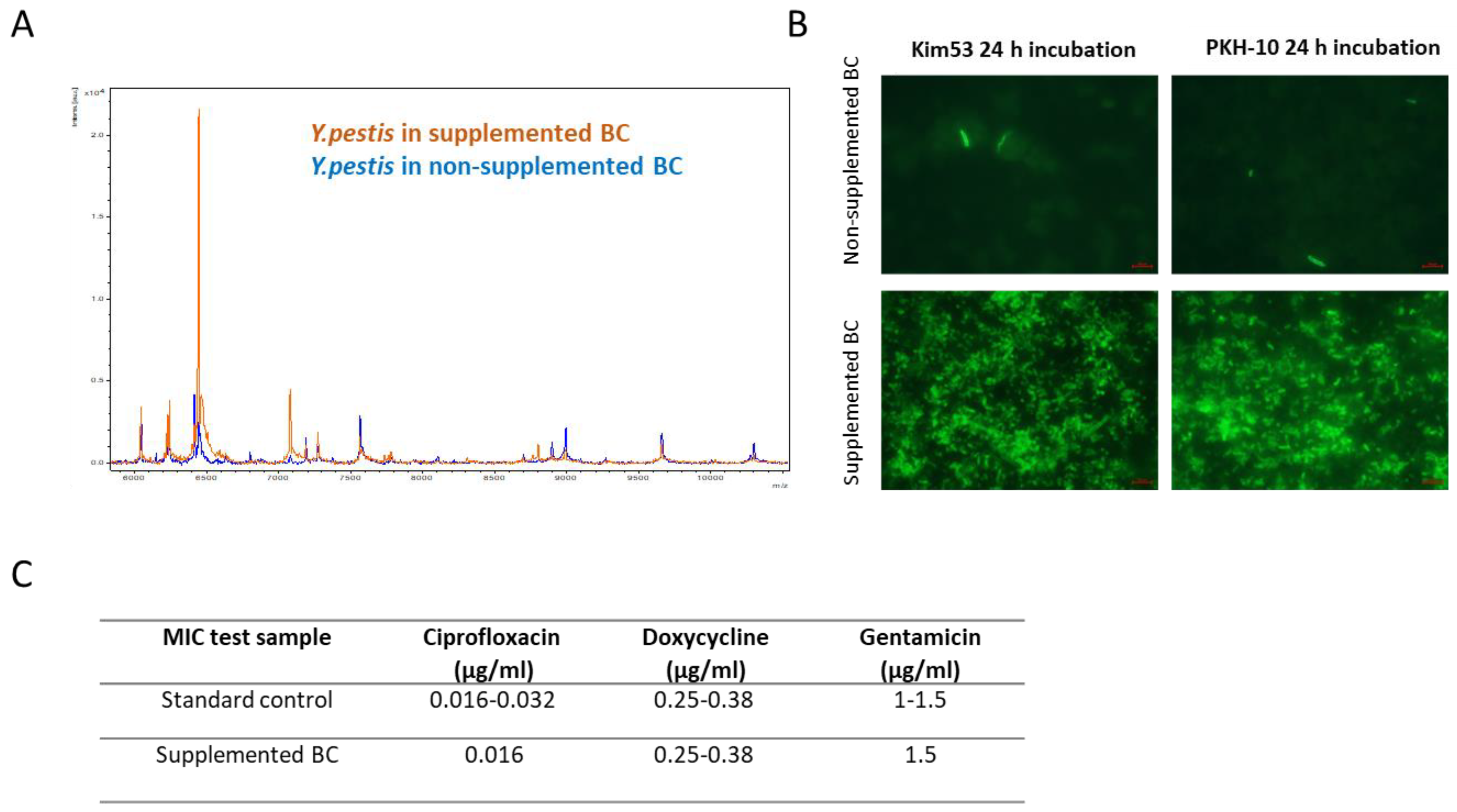
2.1. Accelerated Growth Rates of Y. pestis in Iron- and Calcium-Supplemented Blood Cultures
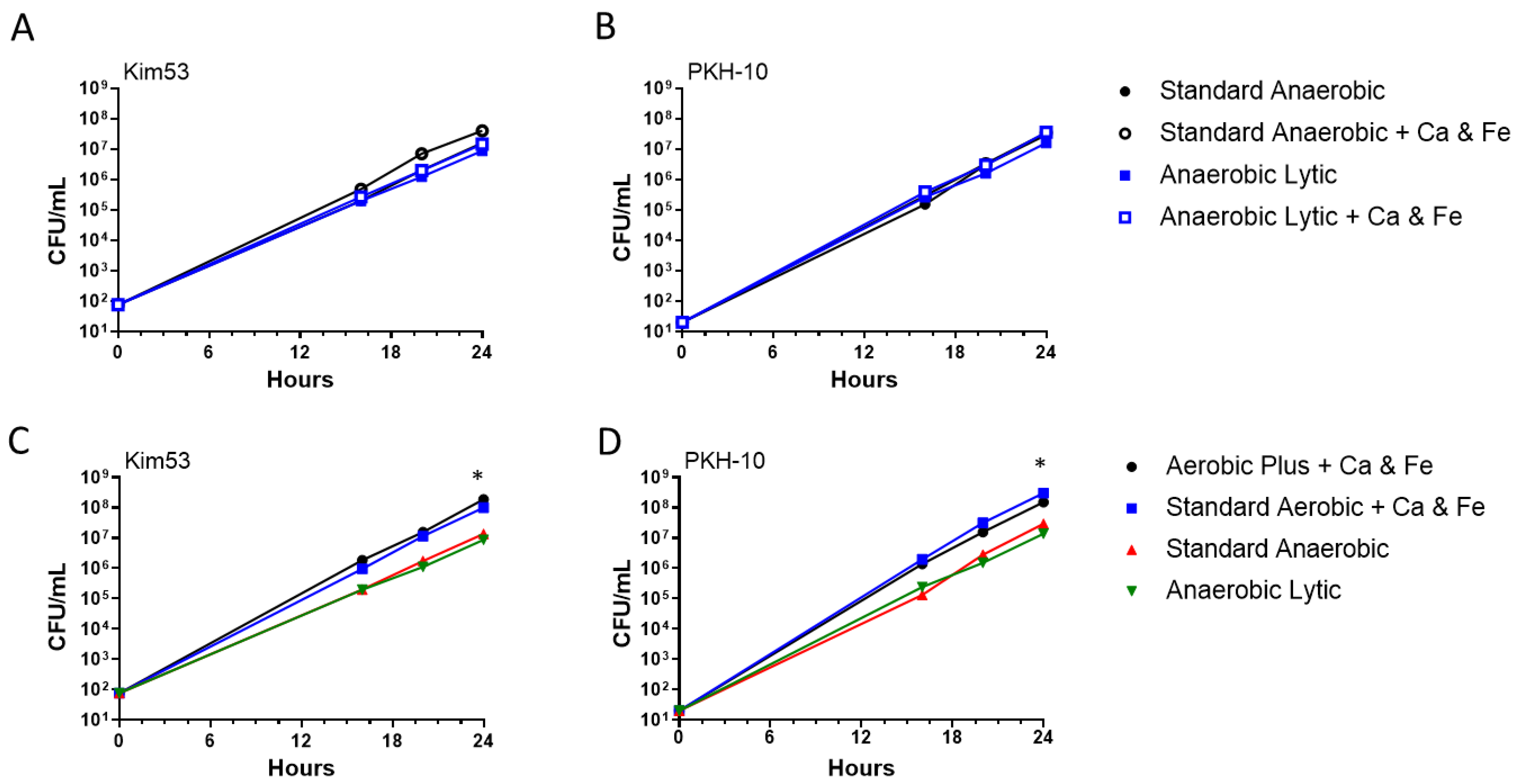
2.2. Y. pestis Growth in Aerobic and Anaerobic Blood Culture Vials
2.3. Accurate Identification and Antibiotic Susceptibility Testing of Y. pestis in Supplemented Blood Cultures
3. Conclusions
4. Materials and Methods
4.1. Y. pestis Strains
4.2. Culture Media
4.3. MIC Determination
4.4. Immunofluorescence Assay (IFA) for Y. pestis Detection
4.5. Detection of F1 and V Antigens from Inoculated Blood Cultures by ELISA
4.6. Bacterial Identification by MALDI-TOF MS
4.7. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Respicio-Kingry, L.B.; Yockey, B.M.; Acayo, S.; Kaggwa, J.; Apangu, T.; Kugeler, K.J.; Eisen, R.J.; Griffith, K.S.; Mead, P.S.; Schriefer, M.E.; et al. Two Distinct Yersinia pestis Populations Causing Plague among Humans in the West Nile Region of Uganda. PLoS Negl. Trop. Dis. 2016, 10, e0004360. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.Y.; Ding, Y.B.; Tan, H.L.; Guo, Y.; Zhang, H.P.; Duan, C.J.; Li, W.; Wang, P. Source tracing of the Yersinia pestis strains isolated from Heqing county, Yunnan province in 2017. Zhonghua Liu Xing Bing Xue Za Zhi 2018, 39, 983–987. [Google Scholar] [PubMed]
- Abedi, A.A.; Shako, J.-C.; Gaudart, J.; Sudre, B.; Ilunga, B.K.; Shamamba, S.K.B.; Diatta, G.; Davoust, B.; Tamfum, J.-J.M.; Piarroux, R.; et al. Ecologic Features of Plague Outbreak Areas, Democratic Republic of the Congo, 2004–2014. Emerg. Infect. Dis. 2018, 24, 210–220. [Google Scholar] [CrossRef] [PubMed]
- Randremanana, R.; Andrianaivoarimanana, V.; Nikolay, B.; Ramasindrazana, B.; Paireau, J.; Bosch, Q.A.T.; Rakotondramanga, J.M.; Rahajandraibe, S.; Rahelinirina, S.; Rakotomanana, F.; et al. Epidemiological characteristics of an urban plague epidemic in Madagascar, August–November, 2017: An outbreak report. Lancet Infect. Dis. 2019, 19, 537–545. [Google Scholar] [CrossRef]
- Inglesby, T.V.; Dennis, D.T.; Henderson, D.A.; Bartlett, J.G.; Ascher, M.S.; Eitzen, E.; Fine, A.D.; Friedlander, A.M.; Hauer, J.; Koerner, J.F.; et al. Plague as a biological weapon: Medical and public health management. JAMA 2000, 283, 2281–2290. [Google Scholar] [CrossRef]
- Towns, M.L.; Jarvis, W.R.; Hsueh, P.R. Guidelines on Blood Cultures. J. Microbiol. Immunol. Infect. 2010, 43, 347–349. [Google Scholar] [CrossRef]
- Aftalion, M.; Aloni-Grinstein, R.; Andrianaivoarimanana, V.; Iharisoa, A.L.; Shmaya, S.; Gur, D.; Laskar, O.; Rajerison, M.; Mamroud, E. Improved Selective BIN Agar for a Better Rate of Yersinia pestis Isolation from Primary Clinical Specimens in Suspected Madagascar Plague Cases. J. Clin. Microbiol. 2021, 59, e0056421. [Google Scholar] [CrossRef]
- Ber, R.; Mamroud, E.; Aftalion, M.; Gur, D.; Tidhar, A.; Flashner, Y.; Cohen, S. A new selective medium provides improved growth and recoverability of Yersinia pestis. Adv. Exp. Med. Biol. 2003, 529, 467–468. [Google Scholar]
- Ber, R.; Mamroud, E.; Aftalion, M.; Tidhar, A.; Gur, D.; Flashner, Y.; Cohen, S. Development of an improved selective agar medium for isolation of Yersinia pestis. Appl. Environ. Microbiol. 2003, 69, 5787–5792. [Google Scholar] [CrossRef]
- Mechaly, A.; Vitner, E.; Levy, H.; Weiss, S.; Bar-David, E.; Gur, D.; Koren, M.; Cohen, H.; Cohen, O.; Mamroud, E.; et al. Simultaneous Immunodetection of Anthrax, Plague, and Tularemia from Blood Cultures by Use of Multiplexed Suspension Arrays. J. Clin. Microbiol. 2018, 4, 56. [Google Scholar] [CrossRef]
- Mechaly, A.; Vitner, E.; Levy, Y.; Gur, D.; Barlev-Gross, M.; Sittner, A.; Koren, M.; Levy, H.; Mamroud, E.; Fisher, M. Epitope Binning of Novel Monoclonal Anti F1 and Anti LcrV Antibodies and Their Application in a Simple, Short, HTRF Test for Clinical Plague Detection. Pathogens 2021, 10, 285. [Google Scholar] [CrossRef]
- Moses, S.; Aftalion, M.; Mamroud, E.; Rotem, S.; Steinberger-Levy, I. Reporter-Phage-Based Detection and Antibiotic Susceptibility Testing of Yersinia pestis for a Rapid Plague Outbreak Response. Microorganisms 2021, 9, 1278. [Google Scholar] [CrossRef]
- Moses, S.; Aftalion, M.; Mamroud, E.; Rotem, S.; Steinberger-Levy, I. Characterization of Yersinia pestis Phage Lytic Activity in Human Whole Blood for the Selection of Efficient Therapeutic Phages. Viruses 2021, 13, 89. [Google Scholar] [CrossRef]
- Vandamm, J.P.; Rajanna, C.; Sharp, N.J.; Molineux, I.J.; Schofield, D.A. Rapid detection and simultaneous antibiotic susceptibility analysis of Yersinia pestis directly from clinical specimens by use of reporter phage. J. Clin. Microbiol. 2014, 52, 2998–3003. [Google Scholar] [CrossRef][Green Version]
- Israeli, O.; Makdasi, E.; Cohen-Gihon, I.; Zvi, A.; Lazar, S.; Shifman, O.; Levy, H.; Gur, D.; Laskar, O.; Beth-Din, A. A rapid high-throughput sequencing-based approach for the identification of unknown bacterial pathogens in whole blood. Futur. Sci. OA 2020, 6, FSO476. [Google Scholar] [CrossRef]
- McHugh, J.P.; Rodríguez-Quiñones, F.; Abdul-Tehrani, H.; Svistunenko, D.A.; Poole, R.K.; Cooper, C.E.; Andrews, S.C. Global iron-dependent gene regulation in Escherichia coli. A new mechanism for iron homeostasis. J. Biol. Chem. 2003, 278, 29478–29486. [Google Scholar] [CrossRef]
- Litwin, C.M.; Calderwood, S.B. Role of iron in regulation of virulence genes. Clin. Microbiol. Rev. 1993, 6, 137–149. [Google Scholar] [CrossRef]
- Schaible, U.E.; Kaufmann, S.H. Iron and microbial infection. Nat. Rev. Microbiol. 2004, 2, 946–953. [Google Scholar] [CrossRef]
- Zauberman, A.; Vagima, Y.; Tidhar, A.; Aftalion, M.; Gur, D.; Rotem, S.; Chitlaru, T.; Levy, Y.; Mamroud, E. Host Iron Nutritional Immunity Induced by a Live Yersinia pestis Vaccine Strain Is Associated with Immediate Protection against Plague. Front. Cell. Infect. Microbiol. 2017, 7, 277. [Google Scholar] [CrossRef]
- Avanian, L.A.; Gubina, N.E. Effect of iron on the growth of virulent plague microbes. J. Mikrobiol. Epidemiol. Immunobiol. 1961, 32, 92–97. [Google Scholar]
- Kravtsov, A.N.; Tynianova, V.I.; Ziuzina, V.P. An increase in the virulence of Yersinia pestis bacteria when the cells are incubated in hemolyzed human erythrocytes. J. Mikrobiol. Epidemiol. Immunobiol. 1993, 1993, 3–6. [Google Scholar]
- Tsukano, H.; Yamamoto, M.; Wake, A. The effect of an iron drug on the growth of plague microorganisms in vitro and in guinea pig skin. Jpn. J. Med. Sci. Biol. 1972, 25, 85–93. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sample, A.K.; Fowler, J.M.; Brubaker, R.R. Modulation of the low-calcium response in Yersinia pestis via plasmid-plasmid interaction. Microb. Pathog. 1987, 2, 443–453. [Google Scholar] [CrossRef]
- Straley, S.C.; Plano, G.V.; Skrzypek, E.; Haddix, P.L.; Fields, K.A. Regulation by Ca2+ in the Yersinia low-Ca2+ response. Mol. Microbiol. 1993, 8, 1005–1010. [Google Scholar] [CrossRef]
- Fowler, J.M.; Brubaker, R.R. Physiological basis of the low calcium response in Yersinia pestis. Infect. Immun. 1994, 62, 5234–5241. [Google Scholar] [CrossRef]
- Mehigh, R.J.; Sample, A.K.; Brubaker, R.R. Expression of the low calcium response in Yersinia pestis. Microb. Pathog. 1989, 6, 203–217. [Google Scholar] [CrossRef]
- Price, S.B.; Cowan, C.; Perry, R.D.; Straley, S.C. The Yersinia pestis V antigen is a regulatory protein necessary for Ca2(+)-dependent growth and maximal expression of low-Ca2+ response virulence genes. J. Bacteriol. 1991, 173, 2649–2657. [Google Scholar] [CrossRef]
- Cockerill, F.R., 3rd; Wilson, J.W.; Vetter, E.A.; Goodman, K.M.; Torgerson, C.A.; Harmsen, W.S.; Schleck, C.D.; Ilstrup, D.M.; Washington, J.A., II; Wilson, W.R. Optimal testing parameters for blood cultures. Clin. Infect. Dis. 2004, 38, 1724–1730. [Google Scholar] [CrossRef]
- Weinstein, M.P. Current blood culture methods and systems: Clinical concepts, technology, and interpretation of results. Clin. Infect. Dis. 1996, 23, 40–46. [Google Scholar] [CrossRef]
- Grohs, P.; Mainardi, J.-L.; Podglajen, I.; Hanras, X.; Eckert, C.; Buu-Hoï, A.; Varon, E.; Gutmann, L. Relevance of routine use of the anaerobic blood culture bottle. J. Clin. Microbiol. 2007, 45, 2711–2715. [Google Scholar] [CrossRef]
- Reimer, L.G.; Wilson, M.L.; Weinstein, M.P. Update on detection of bacteremia and fungemia. Clin. Microbiol. Rev. 1997, 10, 444–465. [Google Scholar] [CrossRef]
- Shifman, O.; Aminov, T.; Aftalion, M.; Gur, D.; Cohen, H.; Bar-David, E.; Cohen, O.; Mamroud, E.; Levy, H.; Aloni-Grinstein, R.; et al. Evaluation of the European Committee on Antimicrobial Susceptibility Testing Guidelines for Rapid Antimicrobial Susceptibility Testing of Bacillus anthracis-, Yersinia pestis and Francisella tularensis-Positive Blood Cultures. Microorganisms 2021, 9, 1055. [Google Scholar] [CrossRef] [PubMed]
- Guajardo-Lara, C.E.; Saldaña-Ramírez, M.I.; Ayala-Gaytán, J.J.; Valdovinos-Chávez, S.B. Role of anaerobic blood culture in the simultaneous blood culture taking for the diagnosis of bacteremia. Rev. Med. Inst. Mex. Seguro. Soc. 2016, 54, 292–296. [Google Scholar]
- Lafaurie, M.; D’Anglejan, E.; Donay, J.L.; Glotz, D.; Sarfati, E.; Mimoun, M.; Legrand, M.; Oksenhendler, E.; Bagot, M.; Valade, S.; et al. Utility of anaerobic bottles for the diagnosis of bloodstream infections. BMC Infect. Dis. 2020, 20, 142. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Sun, J.; Pan, S.; Li, W.; Zhang, S.; Wang, Y.; Sun, X.; Xu, H.; Ming, L. Comparison of the Performance of Three Blood Culture Systems in a Chinese Tertiary-Care Hospital. Front. Cell. Infect. Microbiol. 2019, 9, 285. [Google Scholar] [CrossRef] [PubMed]
- Rohner, P.; Pepey, B.; Auckenthaler, R. Advantage of combining resin with lytic BACTEC blood culture media. J. Clin. Microbiol. 1997, 35, 2634–2638. [Google Scholar] [CrossRef]
- Leal, N.C.; Almeida, A.M. Diagnosis of plague and identification of virulence markers in Yersinia pestis by multiplex-PCR. Rev. Inst. Med. Trop. 1999, 41, 339–342. [Google Scholar] [CrossRef]
- Nikiforov, V.V.; Gao, H.; Zhou, L.; Anisimov, A. Plague: Clinics, Diagnosis and Treatment. Adv. Exp. Med. Biol. 2016, 918, 293–312. [Google Scholar]
- Flashner, Y.; Fisher, M.; Tidhar, A.; Mechaly, A.; Gur, D.; Halperin, G.; Zahavy, E.; Mamroud, E.; Cohen, S. The search for early markers of plague: Evidence for accumulation of soluble Yersinia pestis LcrV in bubonic and pneumonic mouse models of disease. FEMS Immunol. Med. Microbiol. 2010, 59, 197–206. [Google Scholar] [CrossRef]
- Gode-Potratz, C.J.; Chodur, D.M.; McCarter, L.L. Calcium and iron regulate swarming and type III secretion in Vibrio parahaemolyticus. J. Bacteriol. 2010, 192, 6025–6038. [Google Scholar] [CrossRef]
- Bhavsar, S.M.; Dingle, T.C.; Hamula, C.L. The impact of blood culture identification by MALDI-TOF MS on the antimicrobial management of pediatric patients. Diagn. Microbiol. Infect. Dis. 2018, 92, 220–225. [Google Scholar] [CrossRef] [PubMed]
- Osthoff, M.; Gürtler, N.; Bassetti, S.; Balestra, G.; Marsch, S.; Pargger, H.; Weisser, M.; Egli, A. Impact of MALDI-TOF-MS-based identification directly from positive blood cultures on patient management: A controlled clinical trial. Clin. Microbiol. Infect. 2017, 23, 78–85. [Google Scholar] [CrossRef] [PubMed]
- CDC Web Site. Available online: https://www.cdc.gov/plague/healthcare/clinicians.html (accessed on 10 February 2022).
- Joshi, K.; Thakur, J.; Kumar, R.; Singh, A.; Ray, P.; Jain, S.; Varma, S. Epidemiological features of pneumonic plague outbreak in Himachal Pradesh, India. Trans. R. Soc. Trop. Med. Hyg. 2009, 103, 455–460. [Google Scholar] [CrossRef]
- Zahavy, E.; Heleg-Shabtai, V.; Zafrani, Y.; Marciano, D.; Yitzhaki, S. Application of fluorescent nanocrystals (q-dots) for the detection of pathogenic bacteria by flow-cytometry. J. Fluoresc. 2010, 20, 389–399. [Google Scholar] [CrossRef]
- Levy, Y.; Flashner, Y.; Zauberman, A.; Tidhar, A.; Aftalion, M.; Lazar, S.; Gur, D.; Cohen, S.; Shafferman, A.; Mamroud, E. Protection against Plague Afforded by Treatment with Polyclonal αLcrV and αF1 Antibodies; Springer: Dordrecht, The Netherlands, 2010; pp. 269–274. [Google Scholar]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Makdasi, E.; Atiya-Nasagi, Y.; Gur, D.; Zauberman, A.; Schuster, O.; Glinert, I.; Shmaya, S.; Milrot, E.; Levy, H.; Weiss, S.; et al. An Improvement in Diagnostic Blood Culture Conditions Allows for the Rapid Detection and Isolation of the Slow Growing Pathogen Yersinia pestis. Pathogens 2022, 11, 255. https://doi.org/10.3390/pathogens11020255
Makdasi E, Atiya-Nasagi Y, Gur D, Zauberman A, Schuster O, Glinert I, Shmaya S, Milrot E, Levy H, Weiss S, et al. An Improvement in Diagnostic Blood Culture Conditions Allows for the Rapid Detection and Isolation of the Slow Growing Pathogen Yersinia pestis. Pathogens. 2022; 11(2):255. https://doi.org/10.3390/pathogens11020255
Chicago/Turabian StyleMakdasi, Efi, Yafit Atiya-Nasagi, David Gur, Ayelet Zauberman, Ofir Schuster, Itai Glinert, Shlomo Shmaya, Elad Milrot, Haim Levy, Shay Weiss, and et al. 2022. "An Improvement in Diagnostic Blood Culture Conditions Allows for the Rapid Detection and Isolation of the Slow Growing Pathogen Yersinia pestis" Pathogens 11, no. 2: 255. https://doi.org/10.3390/pathogens11020255
APA StyleMakdasi, E., Atiya-Nasagi, Y., Gur, D., Zauberman, A., Schuster, O., Glinert, I., Shmaya, S., Milrot, E., Levy, H., Weiss, S., Chitlaru, T., Mamroud, E., & Laskar, O. (2022). An Improvement in Diagnostic Blood Culture Conditions Allows for the Rapid Detection and Isolation of the Slow Growing Pathogen Yersinia pestis. Pathogens, 11(2), 255. https://doi.org/10.3390/pathogens11020255






