Evolution of Rabies Virus Isolates: Virulence Signatures and Effects of Modulation by Neutralizing Antibodies
Abstract
1. Introduction
2. Materials and Methods
2.1. Viruses and Cells
2.2. Serial Passages in Neuro-2a Cell Line
2.3. Serial Virus Neutralization (SVN) Assay in Neuro-2a Cell Line
2.4. RNA Extraction and Reverse Transcription Reaction (RT)
2.5. Primers for N and G genes Amplification
2.6. Polymerase Chain Reaction (PCR) for N and G genes
2.7. Purification of PCR Products and Sanger Sequencing
2.8. Sequence Editing and Analysis
2.9. Viral Titration
2.10. Replication Kinetics
2.11. In Vivo Assay—Neurotropism Assessment and Ethics Statement
2.12. Competition Assays
2.13. Quantification of Viral Load by qPCR
2.14. Three-Dimensional (3D) Modeling of G Protein, Optimization, Validation and Analysis
2.15. Molecular Dynamics Simulations
2.16. Molecular Docking
2.17. Statistical Analysis
3. Results
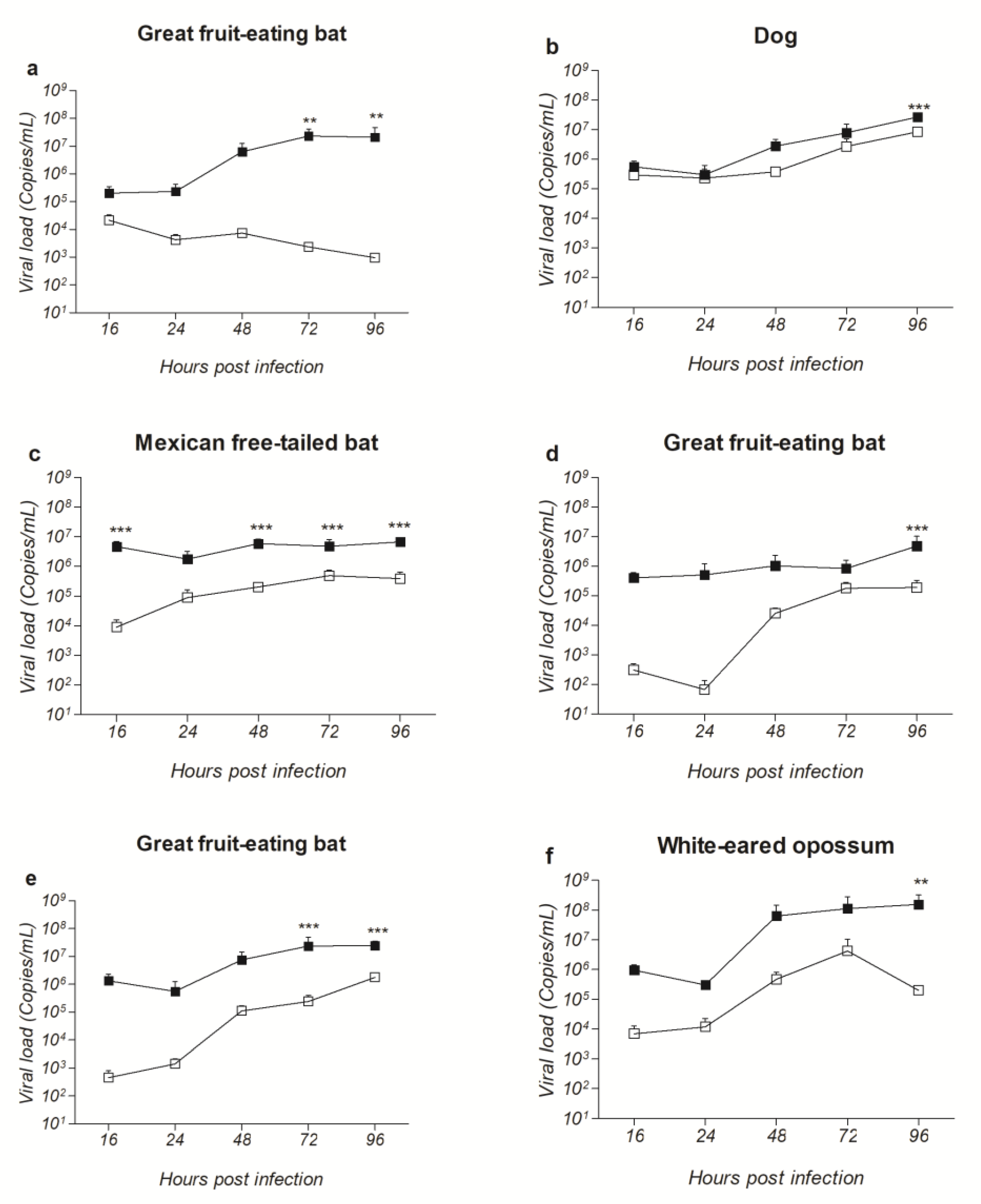
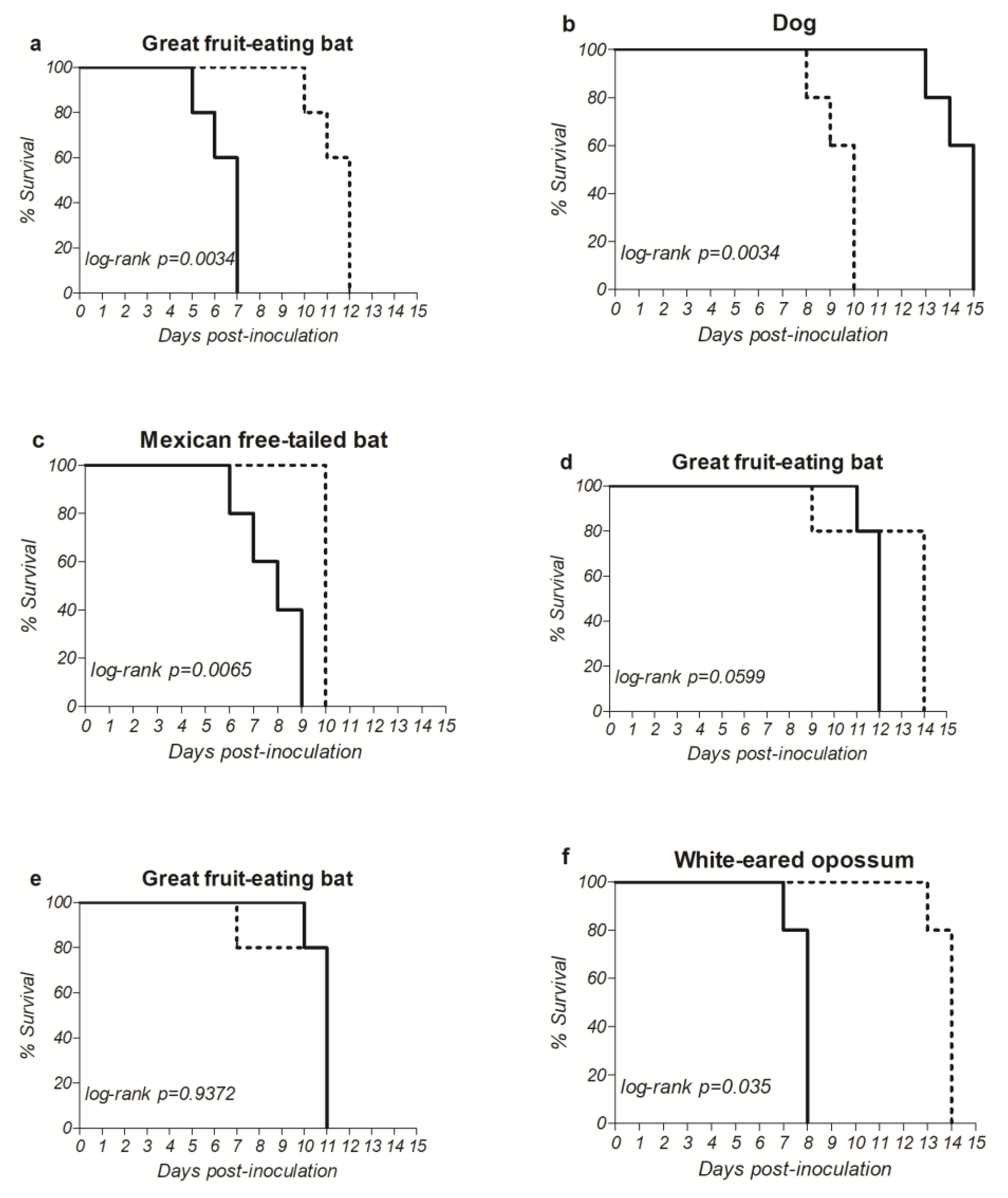
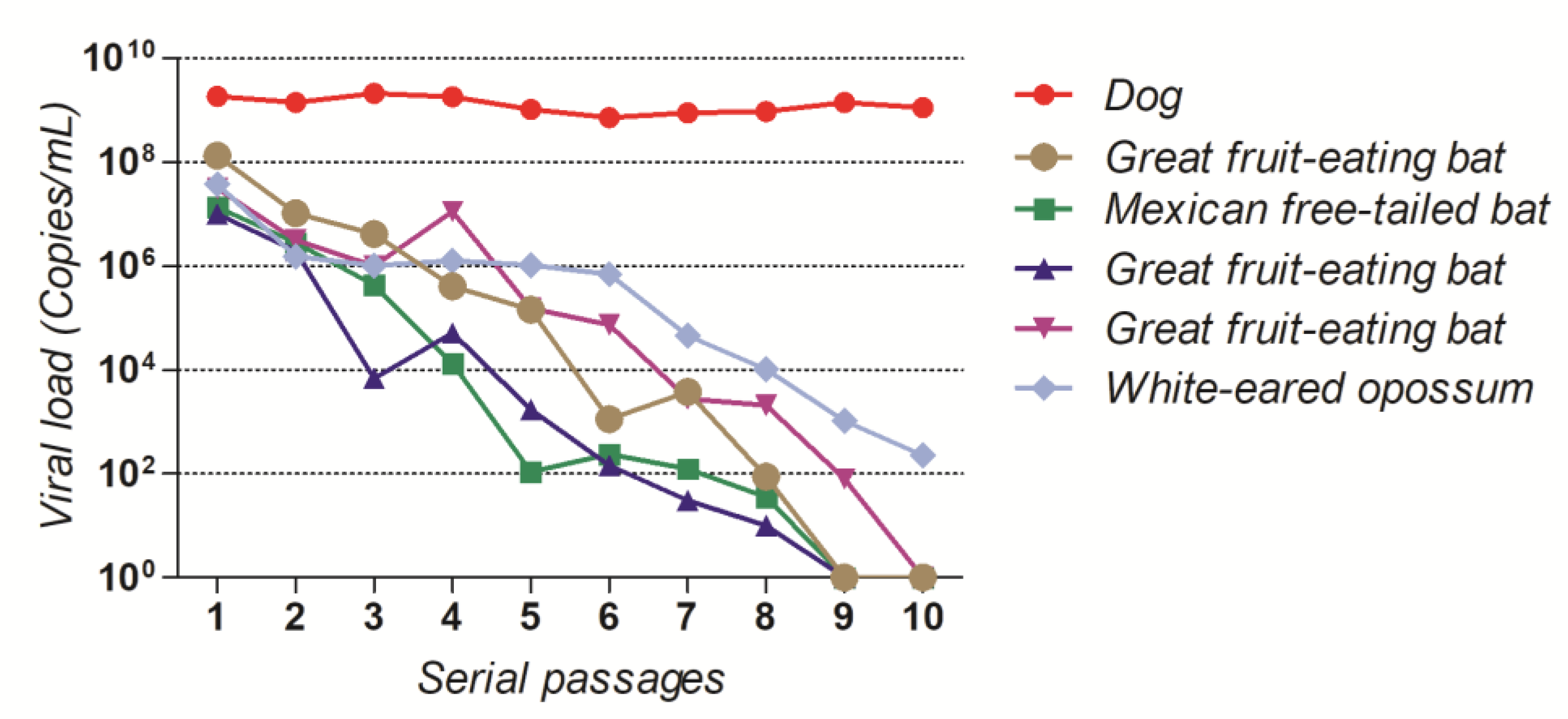
3.1. Amino Acid Substitutions during In Vitro Evolution of RABV Glycoprotein Gene Contribute to Increased Viral Loads in Neuronal Cell Line and Neurotropism In Vivo
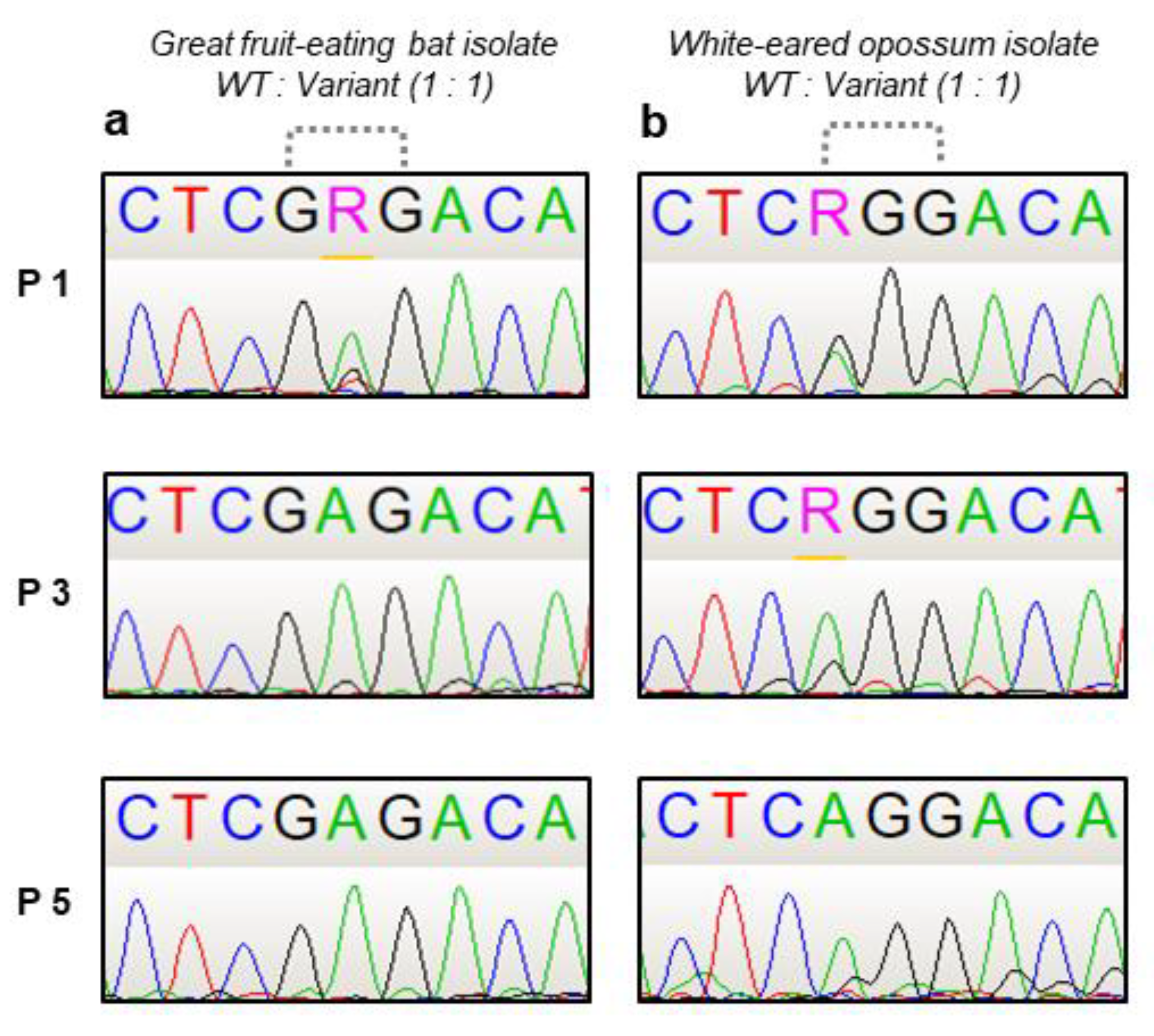
3.2. G186E and G186R+S188P Glycoprotein Gene Variants Show Enhancement of Replicative Fitness In Vitro and Are Present in Natura
3.3. Amino Acid Substitutions G186E and G186R+S188P in the G gene Affects Glycoprotein Structure and Dynamics
3.4. Mutant G186R Shows Interaction with Heparin In Silico
3.5. Mutation in G Gene Can Promote Escape from Neutralizing Antibodies in a Field RABV Isolate
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rupprecht, C.; Kuzmin, I.; Meslin, F. Lyssaviruses and rabies: Current conundrums, concerns, contradictions and controversies. F1000Research 2017, 6, 184. [Google Scholar] [CrossRef]
- Wunner, W.H.; Conzelmann, K.-K. Chapter 2-Rabies virus. In Rabies, 4th ed.; Fooks, A.R., Jackson, A.C., Eds.; Academic Press: London, UK, 2020; pp. 43–81. [Google Scholar] [CrossRef]
- World Health Organization. WHO Expert Consultation on Rabies: Third Report; World Health Organization: Geneva, Switzerland, 2018.
- Marston, D.A.; McElhinney, L.M.; Johnson, N.; Müller, T.; Conzelmann, K.K.; Tordo, N.; Fooks, A.R. Comparative analysis of the full genome sequence of European bat lyssavirus type 1 and type 2 with other lyssaviruses and evidence for a conserved transcription termination and polyadenylation motif in the G-L 3′ non-translated region. J. Gen. Virol. 2007, 88 Pt 4, 1302–1314. [Google Scholar] [CrossRef] [PubMed]
- Warrilow, D.; Smith, I.L.; Harrower, B.; Smith, G.A. Sequence analysis of an isolate from a fatal human infection of Australian bat lyssavirus. Virology 2002, 297, 109–119. [Google Scholar] [CrossRef] [PubMed]
- Ito, N.; Takayama, M.; Yamada, K.; Sugiyama, M.; Minamoto, N. Rescue of rabies virus from cloned cDNA and identification of the pathogenicity-related gene: Glycoprotein gene is associated with virulence for adult mice. J. Virol. 2001, 75, 9121–9128. [Google Scholar] [CrossRef]
- Yan, X.; Mohankumar, P.S.; Dietzschold, B.; Schnell, M.J.; Fu, Z.F. The rabies virus glycoprotein determines the distribution of different rabies virus strains in the brain. J. Neurovirol. 2002, 8, 345–352. [Google Scholar] [CrossRef] [PubMed]
- Domingo, E.; Sheldon, J.; Perales, C. Viral quasispecies evolution. Microbiol. Mol. Biol. Rev. MMBR 2012, 76, 159–216. [Google Scholar] [CrossRef] [PubMed]
- Domingo, E.; Perales, C. Viral quasispecies. PLoS Genet. 2019, 15, e1008271. [Google Scholar] [CrossRef] [PubMed]
- Morimoto, K.; Hooper, D.C.; Carbaugh, H.; Fu, Z.F.; Koprowski, H.; Dietzschold, B. Rabies virus quasispecies: Implications for pathogenesis. Proc. Natl. Acad. Sci. USA 1998, 95, 3152–3156. [Google Scholar] [CrossRef]
- Domingo, E. QUASISPECIES. In Encyclopedia of Virology, 2nd ed.; Granoff, A., Webster, R.G., Eds.; Academic Press: London, UK, 1999; pp. 1431–1436. [Google Scholar] [CrossRef]
- Liu, F.; Wu, X.; Li, L.; Zou, Y.; Liu, S.; Wang, Z. Evolutionary characteristics of morbilliviruses during serial passages in vitro: Gradual attenuation of virus virulence. Comp. Immunol. Microbiol. Infect. Dis. 2016, 47, 7–18. [Google Scholar] [CrossRef]
- Domingo, E.; de Ávila, A.I.; Gallego, I.; Sheldon, J.; Perales, C. Viral fitness: History and relevance for viral pathogenesis and antiviral interventions. Pathog. Dis. 2019, 77, ftz021. [Google Scholar] [CrossRef]
- Bonnaud, E.M.; Troupin, C.; Dacheux, L.; Holmes, E.C.; Monchatre-Leroy, E.; Tanguy, M.; Bouchier, C.; Cliquet, F.; Barrat, J.; Bourhy, H. Comparison of intra- and inter-host genetic diversity in rabies virus during experimental cross-species transmission. PLoS Pathog. 2019, 15, e1007799. [Google Scholar] [CrossRef] [PubMed]
- Ng, P.C.; Henikoff, S. Predicting the effects of amino acid substitutions on protein function. Annu. Rev. Genom. Hum. Genet. 2006, 7, 61–80. [Google Scholar] [CrossRef]
- Sasaki, M.; Anindita, P.D.; Ito, N.; Sugiyama, M.; Carr, M.; Fukuhara, H.; Ose, T.; Maenaka, K.; Takada, A.; Hall, W.W.; et al. The Role of Heparan Sulfate Proteoglycans as an Attachment Factor for Rabies Virus Entry and Infection. J. Infect. Dis. 2018, 217, 1740–1749. [Google Scholar] [CrossRef] [PubMed]
- Domingo, E. Virus population dynamics examined with experimental model systems. In Virus as Populations; Academic Press: London, UK; Amsterdam, The Netherlands, 2020; pp. 195–223. [Google Scholar] [CrossRef]
- Domingo, E.; Mas, A.; Yuste, E.; Pariente, N.; Sierra, S.; Gutiérrez-Riva, M.; Menéndez-Arias, L. Virus population dynamics, fitness variations and the control of viral disease: An update. Prog. Drug Res. Fortschr. Arzneim. Progres Rech. Pharm. 2001, 57, 77–115. [Google Scholar] [CrossRef]
- Martínez, M.A.; Martrus, G.; Capel, E.; Parera, M.; Franco, S.; Nevot, M. Quasispecies Dynamics of RNA Viruses. In Viruses: Essential Agents of Life; Witzany, G., Ed.; Springer: Dordrecht, The Netherlands, 2012; pp. 21–42. [Google Scholar] [CrossRef]
- Coffey, L.L.; Vignuzzi, M. Host alternation of chikungunya virus increases fitness while restricting population diversity and adaptability to novel selective pressures. J. Virol. 2011, 85, 1025–1035. [Google Scholar] [CrossRef]
- Woelk, C.H.; Jin, L.; Holmes, E.C.; Brown, D.W.G. Immune and artificial selection in the haemagglutinin (H) glycoprotein of measles virus. J. Gen. Virol. 2001, 82 Pt 10, 2463–2474. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Cui, Z. Evolution of gp85 gene of subgroup J avian leukosis virus under the selective pressure of antibodies. Sci. China Ser. C Life Sci. 2006, 49, 227–234. [Google Scholar] [CrossRef]
- Costers, S.; Vanhee, M.; Van Breedam, W.; Van Doorsselaere, J.; Geldhof, M.; Nauwynck, H.J. GP4-specific neutralizing antibodies might be a driving force in PRRSV evolution. Virus Res. 2010, 154, 104–113. [Google Scholar] [CrossRef]
- Zhao, P.; Ma, C.; Dong, X.; Cui, Z. Evolution of quasispecies diversity for porcine reproductive and respiratory syndrome virus under antibody selective pressure. Sci. China Life Sci. 2012, 55, 788–792. [Google Scholar] [CrossRef]
- Su, H.; Zhao, Y.; Zheng, L.; Wang, S.; Shi, H.; Liu, X. Effect of the selection pressure of vaccine antibodies on evolution of H9N2 avian influenza virus in chickens. AMB Express 2020, 10, 98. [Google Scholar] [CrossRef]
- Vellas, C.; Del Bello, A.; Debard, A.; Steinmeyer, Z.; Tribaudeau, L.; Ranger, N.; Jeanne, N.; Martin-Blondel, G.; Delobel, P.; Kamar, N.; et al. Influence of treatment with neutralizing monoclonal antibodies on the SARS-CoV-2 nasopharyngeal load and quasispecies. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2022, 28, 139.e5–139.e8. [Google Scholar] [CrossRef] [PubMed]
- Sato, G.; Itou, T.; Shoji, Y.; Miura, Y.; Mikami, T.; Ito, M.; Kurane, I.; Samara, S.I.; Carvalho, A.A.B.; Nociti, D.P.; et al. Genetic and phylogenetic analysis of glycoprotein of rabies virus isolated from several species in Brazil. J. Vet. Med. Sci. 2004, 66, 747–753. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hepperle, D. DNA Dragon: DNA Contig Sequence Assembler Software. Available online: https://www.dna-dragon.com/ (accessed on 2 November 2022).
- Dagona, A.G. BioEdit: A user-friendly biological sequence alignment editor and analysis program for Windows 95/98/NT. Nucleic Acids Symp. Ser. 1999, 41, 95–98. [Google Scholar]
- Cliquet, F.; Aubert, M.; Sagné, L. Development of a fluorescent antibody virus neutralisation test (FAVN test) for the quantitation of rabies-neutralising antibody. J. Immunol. Methods 1998, 212, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Dean, D.; Abelseth, M.K.; Atanasiu, P. The fluorescent antibody test. In Laboratory Techniques in Rabies; Mesli, F.X., Kaplan, M.M., Koprowski, H., Eds.; World Health Organization: Geneva, Switzerland, 1996; pp. 88–93. [Google Scholar]
- Wakeley, P.R.; Johnson, N.; McElhinney, L.M.; Marston, D.; Sawyer, J.; Fooks, A.R. Development of a real-time, TaqMan reverse transcription-PCR assay for detection and differentiation of lyssavirus genotypes 1, 5, and 6. J. Clin. Microbiol. 2005, 43, 2786–2792. [Google Scholar] [CrossRef]
- Waterhouse, A.; Bertoni, M.; Bienert, S.; Studer, G.; Tauriello, G.; Gumienny, R.; Heer, F.T.; de Beer, T.A.P.; Rempfer, C.; Bordoli, L.; et al. SWISS-MODEL: Homology modelling of protein structures and complexes. Nucleic Acids Res. 2018, 46, W296–W303. [Google Scholar] [CrossRef]
- Xu, D.; Zhang, Y. Improving the physical realism and structural accuracy of protein models by a two-step atomic-level energy minimization. Biophys. J. 2011, 101, 2525–2534. [Google Scholar] [CrossRef]
- Pettersen, E.F.; Goddard, T.D.; Huang, C.C.; Couch, G.S.; Greenblatt, D.M.; Meng, E.C.; Ferrin, T.E. UCSF Chimera--a visualization system for exploratory research and analysis. J. Comput. Chem. 2004, 25, 1605–1612. [Google Scholar] [CrossRef]
- Van Der Spoel, D.; Lindahl, E.; Hess, B.; Groenhof, G.; Mark, A.E.; Berendsen, H.J.C. GROMACS: Fast, flexible, and free. J. Comput. Chem. 2005, 26, 1701–1718. [Google Scholar] [CrossRef]
- Turner, P.J. XMGRACE. 2005. Available online: https://plasma-gate.weizmann.ac.il/Grace/ (accessed on 2 November 2022).
- Kozakov, D.; Hall, D.R.; Xia, B.; Porter, K.A.; Padhorny, D.; Yueh, C.; Beglov, D.; Vajda, S. The ClusPro web server for protein-protein docking. Nat. Protoc. 2017, 12, 255–278. [Google Scholar] [CrossRef]
- Ebert, D. Experimental evolution of parasites. Science 1998, 282, 1432–1435. [Google Scholar] [CrossRef] [PubMed]
- Nitschel, S.; Zaeck, L.M.; Potratz, M.; Nolden, T.; Te Kamp, V.; Franzke, K.; Höper, D.; Pfaff, F.; Finke, S. Point Mutations in the Glycoprotein Ectodomain of Field Rabies Viruses Mediate Cell Culture Adaptation through Improved Virus Release in a Host Cell Dependent and Independent Manner. Viruses 2021, 13, 1989. [Google Scholar] [CrossRef] [PubMed]
- Kissi, B.; Badrane, H.; Audry, L.; Lavenu, A.; Tordo, N.; Brahimi, M.; Bourhy, H. Dynamics of rabies virus quasispecies during serial passages in heterologous hosts. J. Gen. Virol. 1999, 80 Pt 8, 2041–2050. [Google Scholar] [CrossRef] [PubMed]
- Holmes, E.C.; Woelk, C.H.; Kassis, R.; Bourhy, H. Genetic constraints and the adaptive evolution of rabies virus in nature. Virology 2002, 292, 247–257. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, R.N.; de Souza, S.P.; Lobo, R.S.V.; Castilho, J.G.; Macedo, C.I.; Carnieli, P.; Fahl, W.O.; Achkar, S.M.; Scheffer, K.C.; Kotait, I.; et al. Rabies virus in insectivorous bats: Implications of the diversity of the nucleoprotein and glycoprotein genes for molecular epidemiology. Virology 2010, 405, 352–360. [Google Scholar] [CrossRef]
- De Almeida, M.F.; Favoretto, S.R.; Martorelli, L.F.A.; Trezza-Netto, J.; de Campos, A.C.A.; Ozahata, C.H.; Sodré, M.M.; Kataoka, A.P.A.G.; Sacramento, D.R.V.; Durigon, E.L. Characterization of rabies virus isolated from a colony of Eptesicus furinalis bats in Brazil. Rev. Inst. Med. Trop. Sao Paulo 2011, 53, 31–37. [Google Scholar] [CrossRef][Green Version]
- Fahl, W.O.; Carnieli, P.; Castilho, J.G.; Carrieri, M.L.; Kotait, I.; Iamamoto, K.; Oliveira, R.N.; Brandão, P.E. Desmodus rotundus and Artibeus spp. bats might present distinct rabies virus lineages. Braz. J. Infect. Dis. Off. Publ. Braz. Soc. Infect. Dis. 2012, 16, 545–551. [Google Scholar] [CrossRef]
- Carnieli, P.; de Fahl, W.O.; Castilho, J.G.; de Oliveira, R.N.; Macedo, C.I.; Durymanova, E.; Jorge, R.S.P.; Morato, R.G.; Spíndola, R.O.; Machado, L.M.; et al. Characterization of Rabies virus isolated from canids and identification of the main wild canid host in Northeastern Brazil. Virus Res. 2008, 131, 33–46. [Google Scholar] [CrossRef]
- Favoretto, S.R.; de Mattos, C.C.; Morais, N.B.; Alves Araújo, F.A.; de Mattos, C.A. Rabies in marmosets (Callithrix jacchus), Ceará, Brazil. Emerg. Infect. Dis. 2001, 7, 1062–1065. [Google Scholar] [CrossRef]
- Ito, N.; Kakemizu, M.; Ito, K.A.; Yamamoto, A.; Yoshida, Y.; Sugiyama, M.; Minamoto, N. A comparison of complete genome sequences of the attenuated RC-HL strain of rabies virus used for production of animal vaccine in Japan, and the parental Nishigahara strain. Microbiol. Immunol. 2001, 45, 51–58. [Google Scholar] [CrossRef]
- Takayama-Ito, M.; Ito, N.; Yamada, K.; Minamoto, N.; Sugiyama, M. Region at amino acids 164 to 303 of the rabies virus glycoprotein plays an important role in pathogenicity for adult mice. J. Neurovirol. 2004, 10, 131–135. [Google Scholar] [CrossRef] [PubMed]
- Cai, M.; Liu, H.; Jiang, F.; Sun, Y.; Wang, W.; An, Y.; Zhang, M.; Li, X.; Liu, D.; Li, Y.; et al. Analysis of the evolution, infectivity and antigenicity of circulating rabies virus strains. Emerg. Microbes Infect. 2022, 11, 1474–1487. [Google Scholar] [CrossRef] [PubMed]
- George, R.A.; Heringa, J. An analysis of protein domain linkers: Their classification and role in protein folding. Protein Eng. 2002, 15, 871–879. [Google Scholar] [CrossRef] [PubMed]
- Callaway, H.M.; Zyla, D.; Larrous, F.; de Melo, G.D.; Hastie, K.M.; Avalos, R.D.; Agarwal, A.; Corti, D.; Bourhy, H.; Saphire, E.O. Structure of the rabies virus glycoprotein trimer bound to a prefusion-specific neutralizing antibody. Sci. Adv. 2022, 8, eabp9151. [Google Scholar] [CrossRef]
- Tokuriki, N.; Tawfik, D.S. Protein dynamism and evolvability. Science 2009, 324, 203–207. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Lin, S.; Ye, F.; Yang, J.; Qi, J.; Chen, Z.; Lin, X.; Wang, J.; Yue, D.; Cheng, Y.; et al. Structural Analysis of Rabies Virus Glycoprotein Reveals pH-Dependent Conformational Changes and Interactions with a Neutralizing Antibody. Cell Host Microbe 2020, 27, 441–453.e7. [Google Scholar] [CrossRef] [PubMed]
- Carneiro, F.A.; Vandenbussche, G.; Juliano, M.A.; Juliano, L.; Ruysschaert, J.-M.; Da Poian, A.T. Charged residues are involved in membrane fusion mediated by a hydrophilic peptide located in vesicular stomatitis virus G protein. Mol. Membr. Biol. 2006, 23, 396–406. [Google Scholar] [CrossRef]
- Gaudin, Y.; Ruigrok, R.W.; Knossow, M.; Flamand, A. Low-pH conformational changes of rabies virus glycoprotein and their role in membrane fusion. J. Virol. 1993, 67, 1365–1372. [Google Scholar] [CrossRef]
- Da Poian, A.T.; Carneiro, F.A.; Stauffer, F. Viral membrane fusion: Is glycoprotein G of rhabdoviruses a representative of a new class of viral fusion proteins? Braz. J. Med. Biol. Res. Rev. Bras. Pesqui. Medicas E Biol. 2005, 38, 813–823. [Google Scholar] [CrossRef]
- Seganti, L.; Superti, F.; Bianchi, S.; Orsi, N.; Divizia, M.; Panà, A. Susceptibility of mammalian, avian, fish, and mosquito cell lines to rabies virus infection. Acta Virol. 1990, 34, 155–163. [Google Scholar]
- Compton, T.; Nowlin, D.M.; Cooper, N.R. Initiation of human cytomegalovirus infection requires initial interaction with cell surface heparan sulfate. Virology 1993, 193, 834–841. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Maguire, T.; Hileman, R.E.; Fromm, J.R.; Esko, J.D.; Linhardt, R.J.; Marks, R.M. Dengue virus infectivity depends on envelope protein binding to target cell heparan sulfate. Nat. Med. 1997, 3, 866–871. [Google Scholar] [CrossRef] [PubMed]
- Byrnes, A.P.; Griffin, D.E. Binding of Sindbis virus to cell surface heparan sulfate. J. Virol. 1998, 72, 7349–7356. [Google Scholar] [CrossRef] [PubMed]
- Chung, C.S.; Hsiao, J.C.; Chang, Y.S.; Chang, W. A27L protein mediates vaccinia virus interaction with cell surface heparan sulfate. J. Virol. 1998, 72, 1577–1585. [Google Scholar] [CrossRef]
- Feldman, S.A.; Hendry, R.M.; Beeler, J.A. Identification of a linear heparin binding domain for human respiratory syncytial virus attachment glycoprotein G. J. Virol. 1999, 73, 6610–6617. [Google Scholar] [CrossRef]
- Bruett, L.; Barber, S.A.; Clements, J.E. Characterization of a membrane-associated protein implicated in visna virus binding and infection. Virology 2000, 271, 132–141. [Google Scholar] [CrossRef]
- Dechecchi, M.C.; Tamanini, A.; Bonizzato, A.; Cabrini, G. Heparan sulfate glycosaminoglycans are involved in adenovirus type 5 and 2-host cell interactions. Virology 2000, 268, 382–390. [Google Scholar] [CrossRef]
- Belot, L.; Albertini, A.; Gaudin, Y. Structural and cellular biology of rhabdovirus entry. Adv. Virus Res. 2019, 104, 147–183. [Google Scholar] [CrossRef]
- Mandl, C.W.; Kroschewski, H.; Allison, S.L.; Kofler, R.; Holzmann, H.; Meixner, T.; Heinz, F.X. Adaptation of tick-borne encephalitis virus to BHK-21 cells results in the formation of multiple heparan sulfate binding sites in the envelope protein and attenuation in vivo. J. Virol. 2001, 75, 5627–5637. [Google Scholar] [CrossRef]
- Karger, A.; Saalmüller, A.; Tufaro, F.; Banfield, B.W.; Mettenleiter, T.C. Cell surface proteoglycans are not essential for infection by pseudorabies virus. J. Virol. 1995, 69, 3482–3489. [Google Scholar] [CrossRef]
- Dietzschold, B.; Wunner, W.H.; Wiktor, T.J.; Lopes, A.D.; Lafon, M.; Smith, C.L.; Koprowski, H. Characterization of an antigenic determinant of the glycoprotein that correlates with pathogenicity of rabies virus. Proc. Natl. Acad. Sci. USA 1983, 80, 70–74. [Google Scholar] [CrossRef] [PubMed]
- Seif, I.; Coulon, P.; Rollin, P.E.; Flamand, A. Rabies virulence: Effect on pathogenicity and sequence characterization of rabies virus mutations affecting antigenic site III of the glycoprotein. J. Virol. 1985, 53, 926–934. [Google Scholar] [CrossRef] [PubMed]
- Tuffereau, C.; Leblois, H.; Bénéjean, J.; Coulon, P.; Lafay, F.; Flamand, A. Arginine or lysine in position 333 of ERA and CVS glycoprotein is necessary for rabies virulence in adult mice. Virology 1989, 172, 206–212. [Google Scholar] [CrossRef] [PubMed]
- Coulon, P.; Ternaux, J.P.; Flamand, A.; Tuffereau, C. An avirulent mutant of rabies virus is unable to infect motoneurons in vivo and in vitro. J. Virol. 1998, 72, 273–278. [Google Scholar] [CrossRef]
- Coulon, P.; Lafay, F.; Tuffereau, C.; Flamand, A. The molecular basis for altered pathogenicity of lyssavirus variants. Curr. Top. Microbiol. Immunol. 1994, 187, 69–84. [Google Scholar] [CrossRef]
- Lafay, F.; Bénéjean, J.; Tuffereau, C.; Flamand, A.; Coulon, P. Vaccination against rabies: Construction and characterization of SAG2, a double avirulent derivative of SADBern. Vaccine 1994, 12, 317–320. [Google Scholar] [CrossRef]
- Tuffereau, C.; Bénéjean, J.; Blondel, D.; Kieffer, B.; Flamand, A. Low-affinity nerve-growth factor receptor (P75NTR) can serve as a receptor for rabies virus. EMBO J. 1998, 17, 7250–7259. [Google Scholar] [CrossRef]



| Identification | Host Species | Common Name | Variant |
|---|---|---|---|
| 1069/18 | Artibeus lituratus | Great fruit-eating bat | Bat |
| IP3629/11 | Canis lupus familiaris | Dog | Cosmopolitan dog |
| 203/21 | Tadarida brasiliensis | Mexican free-tailed bat | Bat |
| 1833/21 | Artibeus lituratus | Great fruit-eating bat | Bat |
| 2193/21 | Artibeus lituratus | Great fruit-eating bat | Bat |
| 2253/21 | Didelphis albiventris | White-eared opossum | Bat |
| Primer | Sense | Sequence | Size | Position * |
|---|---|---|---|---|
| N55 | F | 5′ ATGTAACACCTCTACAATGG 3′ | 842 bp | 55–74 |
| N879 ** | R | 5′ CAGGCTCGAACATTCTTC 3′ | 842 bp | 879–896 |
| N878 *** | R | 5′ CCCGGGCTCGAACATTCTTCT 3′ | 844 bp | 878–898 |
| N750 | F | 5′ GCACAGTTGTCACTGCTT 3′ | 793 bp | 750–767 |
| N1525B ** | R | 5′ GCACTTGGGCTGACAAAA 3′ | 793 bp | 1525–1542 |
| N1525D *** | R | 5′ TGCACTAGGATTGACAAAG 3′ | 793 bp | 1525–1542 |
| Isolate | Substitution | |||||
|---|---|---|---|---|---|---|
| Host | nt | Position * | aa | Position * | Passage no. | |
| 1069/18 | Great fruit-eating bat | GGG–GAG | 613 | G–E | 186 | 3 |
| IP3629/11 | Dog | CGG–CAG | 1055 | R–Q | 333 | 6 |
| 203/21 | Mexican free-tailed bat | TCC–CCC | 550 | S–P | 165 | 6 |
| 1833/21 | Great fruit-eating bat | GGG–AGG | 613 | G–R | 186 | 5 |
| TCT–TTT | 620 | S–F | 188 | 8 | ||
| 2193/21 | Great fruit-eating bat | GGG–AGG | 613 | G–R | 186 | 5 |
| TCT–CCT | 619 | S–P | 188 | 6 | ||
| 2253/21 | White-eared opossum | GGG–AGG | 613 | G–R | 186 | 5 |
| TCT–CCT | 619 | S–P | 188 | 6 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Conselheiro, J.A.; Barone, G.T.; Miyagi, S.A.T.; de Souza Silva, S.O.; Agostinho, W.C.; Aguiar, J.; Brandão, P.E. Evolution of Rabies Virus Isolates: Virulence Signatures and Effects of Modulation by Neutralizing Antibodies. Pathogens 2022, 11, 1556. https://doi.org/10.3390/pathogens11121556
Conselheiro JA, Barone GT, Miyagi SAT, de Souza Silva SO, Agostinho WC, Aguiar J, Brandão PE. Evolution of Rabies Virus Isolates: Virulence Signatures and Effects of Modulation by Neutralizing Antibodies. Pathogens. 2022; 11(12):1556. https://doi.org/10.3390/pathogens11121556
Chicago/Turabian StyleConselheiro, Juliana Amorim, Gisely Toledo Barone, Sueli Akemi Taniwaki Miyagi, Sheila Oliveira de Souza Silva, Washington Carlos Agostinho, Joana Aguiar, and Paulo Eduardo Brandão. 2022. "Evolution of Rabies Virus Isolates: Virulence Signatures and Effects of Modulation by Neutralizing Antibodies" Pathogens 11, no. 12: 1556. https://doi.org/10.3390/pathogens11121556
APA StyleConselheiro, J. A., Barone, G. T., Miyagi, S. A. T., de Souza Silva, S. O., Agostinho, W. C., Aguiar, J., & Brandão, P. E. (2022). Evolution of Rabies Virus Isolates: Virulence Signatures and Effects of Modulation by Neutralizing Antibodies. Pathogens, 11(12), 1556. https://doi.org/10.3390/pathogens11121556






