Pet Reptiles in Poland as a Potential Source of Transmission of Salmonella
Abstract
1. Introduction
2. Materials and Methods
2.1. Collection of Faecal Samples
2.2. Salmonella sp. Isolation
2.3. Identification of Salmonella by MALDI-TOF Mass Spectrometry
2.4. Biochemical Profiles of Salmonella Strains
2.5. Serotyping
2.6. Whole Genome Sequencing (WGS) and Bioinformatics Tools
2.7. Evaluation of Pathogenic and Zoonotic Potential of Identified Salmonella Serovars Based on Review of Cases
2.8. Evaluation of Antimicrobial Susceptibility of Salmonella Isolates
2.9. Detection of Aminoglycoside Resistance Genes
2.10. Statistical Analysis
3. Results
3.1. Identification and Prevalence of Salmonella Isolates
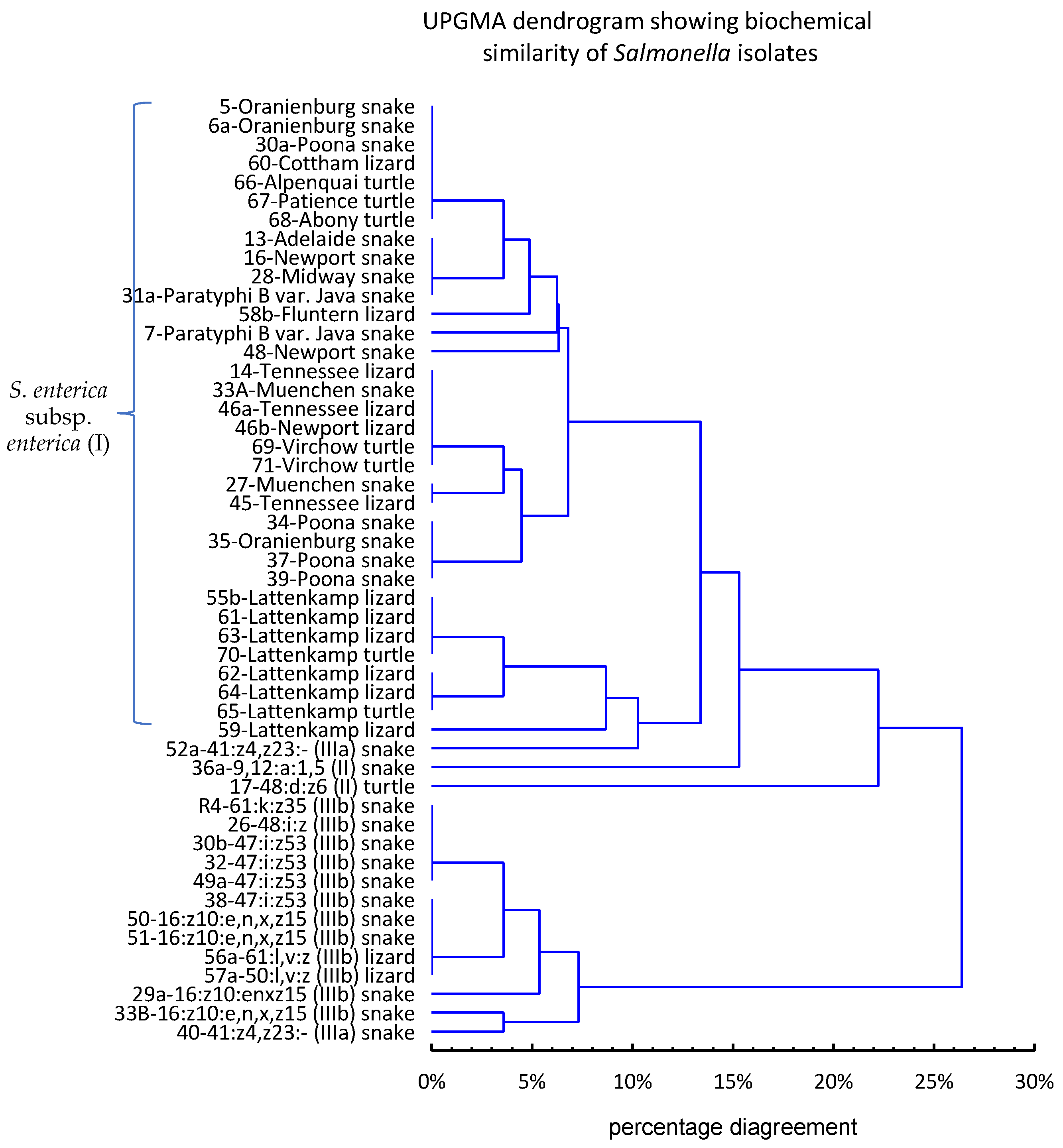
3.2. Biochemical Profiles of Salmonella Strains
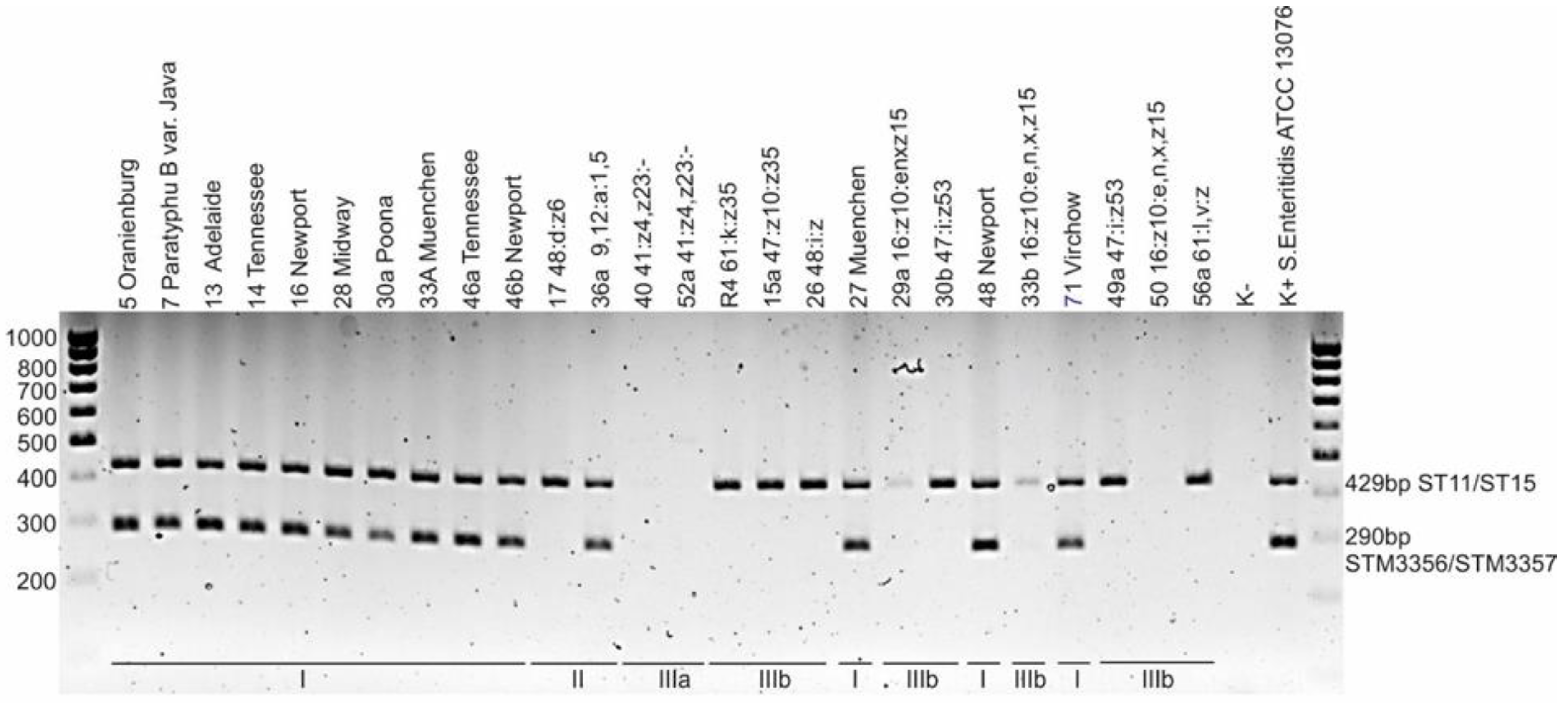
3.3. Serotyping
3.4. Antimicrobial Testing
3.5. WGS
3.6. Pathogenic and Zoonotic Potential of Salmonella Serovars Identified in Reptiles
4. Discussion
4.1. Prevalence of Salmonella spp. in Captive Reptiles in Poland
4.2. Subspecies and Serovars of Reptile Salmonella Strains
4.3. Zoonotic Potential of Identified Salmonella Serovars
4.4. Antimicrobial Susceptibility
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- The European Union One Health 2020 Zoonoses Report. EFSA J. 2021, 19, 6971. Available online: https://efsa.onlinelibrary.wiley.com/doi/epdf/10.2903/j.efsa.2021.6971 (accessed on 12 September 2022).
- Report of Centers for Disease Control and Prevention, USA. Available online: https://www.cdc.gov/salmonella/ (accessed on 20 August 2022).
- Milczarek, M.; Sadkowska-Todys, M.; Czarkowski, M.P.; Kitowska, W. Salmonellosis in Poland in 2017. Prz. Epidemiol. 2019, 73, 463–477. [Google Scholar]
- Ruszel, K.; Dubel, R.; Chodun, W.; Nieradko-Iwanicka, B. Salmonella—Still a threat? Epidemiological analysis of infecion. J. Educ. Health Sport 2021, 11, 38–43. [Google Scholar] [CrossRef]
- Issenhuth-Jeanjean, S.; Roggentin, P.; Mikoleit, M.; Guibourdenche, M.; de Pinna, E.; Nair, S.; Fields, P.I.; Weill, F.X. Supplement 2008–2010 (no. 48) to the White-Kauffmann-Le Minor scheme. Res. Microbiol. 2014, 165, 526–530. [Google Scholar] [CrossRef] [PubMed]
- Dróżdż, M.; Małaszczuk, M.; Paluch, E.; Pawlak, A. Zoonotic potential and prevalence of Salmonella serovars isolated from pets. Infect. Ecol. Epidemiol. 2021, 11, 1975530. [Google Scholar] [CrossRef]
- Mermin, J.; Hutwagner, L.; Vugia, D.; Shallow, S.; Daily, P.; Bender, J.; Koehler, J.; Marcus, R.; Angulo, F.J. Emerging Infections Program FoodNet Working Group. Reptiles, amphibians, and human Salmonella infection: A population-based, case-control study. Clin. Infect. Dis. 2004, 38 (Suppl. S3), S253–S261. [Google Scholar] [CrossRef]
- FEDIAF (The European Pet Food Industry). FEDIAF Annual Report 2021. p. 44, 50. Available online: https://europeanpetfood.org/about/statistics/ (accessed on 20 January 2022).
- Zając, M.; Skarżyńska, M.; Lalak, A.; Kwit, R.; Śmiałowska-Węglińska, A.; Pasim, P.; Szulowski, K.; Wasyl, D. Salmonella in Captive Reptiles and Their Environment-Can We Tame the Dragon? Microorganisms 2021, 9, 1012. [Google Scholar] [CrossRef]
- Bosch, S.; Tauxe, R.V.; Behravesh, C.B. Turtle-Associated Salmonellosis, United States, 2006–2014. Emerg. Infect. Dis. 2016, 22, 1149–1155. [Google Scholar] [CrossRef]
- Gambino-Shirley, K.; Stevenson, L.; Concepción-Acevedo, J.; Trees, E.; Wagner, D.; Whitlock, L.; Roberts, J.; Garrett, N.; Van Duyne, S.; McAllister, G.; et al. Flea market finds and global exports: Four multistate outbreaks of human Salmonella infections linked to small turtles, United States-2015. Zoonoses Public Health 2018, 65, 560–568. [Google Scholar] [CrossRef]
- Dec, M.; Stępień-Pyśniak, D.; Puchalski, A.; Hauschild, T.; Pietras-Ożga, D.; Ignaciuk, S.; Urban-Chmiel, R. Biodiversity of Ligilactobacillus salivarius Strains from Poultry and Domestic Pigeons. Animals 2021, 11, 972. [Google Scholar] [CrossRef]
- Grimont, P.A.D.; Weill, F.X. Antigenic Formulae of Salmonella Serovars, 9th ed.; WHO Collaborating Centre for Research on Salmonella, Institute Pasteur: Paris, France, 2017; Available online: https://www.pasteur.fr/sites/default/files/veng_0.pdf (accessed on 12 September 2022).
- Ewing, W.H. Edwards and Ewing’s Identification of Enterobacteriaceae, 4th ed.; Elsevier: New York, NY, USA, 1986. [Google Scholar]
- Malorny, B.; Bunge, C.; Helmuth, R. Discrimination of d-tartrate-fermenting and -nonfermenting Salmonella enterica subsp. enterica isolates by genotypic and phenotypic methods. J. Clin. Microbiol. 2003, 41, 4292–4297. [Google Scholar] [CrossRef]
- Hoszowski, A.; Wasyl, D. Pożywka Agarowa AKG do Ekspresji faz Antygenów Rzęskowych Salmonella, Sposób jej Wytwarzania Oraz Zastosowanie Pożywki do Identyfikacji Antygenów Rzęskowych Salmonella; Państwowy Instytut Weterynaryjny—Państwowy Instytut Badawczy: Puławy, Poland, 2012; p. 401498. [Google Scholar]
- Bolger, A.M.; Lohse, M.; Usadel, B. Trimmomatic: A flexible trimmer for Illumina sequence data. Bioinformatics 2014, 30, 2114–2120. [Google Scholar] [CrossRef] [PubMed]
- Bankevich, A.; Nurk, S.; Antipov, D.; Gurevich, A.A.; Dvorkin, M.; Kulikov, A.S.; Lesin, V.M.; Nikolenko, S.I.; Pham, S.; Prjibelski, A.D.; et al. SPAdes: A new genome assembly algorithm and its applications to single-cell sequencing. J. Comput. Biol. 2012, 19, 455–477. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Yin, Y.; Jones, M.B.; Zhang, Z.; Deatherage Kaiser, B.L.; Dinsmore, B.A.; Fitzgerald, C.; Fields, P.I.; Deng, X. Salmonella serotype determination utilizing high-throughput genome sequencing data. J. Clin. Microbiol. 2015, 53, 1685–1692. [Google Scholar] [CrossRef]
- Bortolaia, V.; Kaas, R.F.; Ruppe, E.; Roberts, M.C.; Schwarz, S.; Cattoir, V.; Philippon, A.; Allesoe, R.L.; Rebelo, A.R.; Florensa, A.R.; et al. ResFinder 4.0 for predictions of phenotypes from genotypes. J. Antimicrob. Chemother. 2020, 75, 3491–3500. [Google Scholar] [CrossRef] [PubMed]
- EUCAST, Antimicrobial wild type distributions of microorganisms. Available online: https://mic.eucast.org/search/ (accessed on 20 August 2022).
- CLSI Supplement M100; Performance Standards for Antimicrobial Susceptibility Testing, 28th ed. Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2018.
- EUCAST. The European Committee on Antimicrobial Susceptibility Testing. Breakpoint Tables for Interpretation of MICs and Zone Diameters. Version 11.0. 2021. Available online: http://www.eucast.org (accessed on 20 August 2022).
- Dec, M.; Stępień-Pyśniak, D.; Szczepaniak, K.; Turchi, B.; Urban-Chmiel, R. Virulence Profiles and Antibiotic Susceptibility of Escherichia coli Strains from Pet Reptiles. Pathogens 2022, 11, 127. [Google Scholar] [CrossRef] [PubMed]
- CDC. National enteric disease surveillance: Salmonella annual report 2016. Available online: https://www.cdc.gov/nationalsurveillance/pdfs/2016-Salmonella-report-508.pdf (accessed on 20 August 2022).
- Parisi, A.; Crump, J.A.; Stafford, R.; Glass, K.; Howden, B.P.; Kirk, M.D. Increasing incidence of invasive nontyphoidal Salmonella infections in Queensland, Australia, 2007–2016. PLOS Negl. Trop. Dis. 2019, 13, e0007187. [Google Scholar] [CrossRef]
- Kuroki, T.; Ito, K.; Ishihara, T.; Furukawa, I.; Kaneko, A.; Suzuki, Y.; Seto, J.; Kamiyama, T. Turtle-Associated Salmonella Infections in Kanagawa, Japan. Jpn. J. Infect. Dis. 2015, 68, 333–337. [Google Scholar] [CrossRef]
- Van Meervenne, E.; Botteldoorn, N.; Lokietek, S.; Vatlet, M.; Cupa, A.; Naranjo, M.; Dierick, K.; Bertrand, S. Turtle-associated Salmonella septicaemia and meningitis in a 2-month-old baby. J. Med. Microbiol. 2009, 58, 1379–1381. [Google Scholar] [CrossRef]
- Kiebler, C.A.; Bottichio, L.; Simmons, L.; Basler, C.; Klos, R.; Gurfield, N.; Roberts, E.; Kimura, A.; Lewis, L.S.; Bird, K.; et al. Outbreak of human infections with uncommon Salmonella serotypes linked to pet bearded dragons. Zoonoses Public Health 2020, 67, 425–434. [Google Scholar] [CrossRef]
- Murphy, D.; Oshin, F. Reptile-associated salmonellosis in children aged under 5 years in South West England. Arch. Dis. Child. 2015, 100, 364–365. [Google Scholar] [CrossRef] [PubMed]
- Braun, S.; Spalloni, W.; Ferreccio, F.; Postigo, J.; Fernández, A.; Porte, L.; Saldivia, A.; Wigant, W.; Triantafilo, V. Salmonella spp. gastroenteritis associated to pet turtles in three infants. Rev. Chilena. Infectol. 2015, 32, 334–338. [Google Scholar] [CrossRef] [PubMed][Green Version]
- CDC’s 2019 Salmonella Outbreak Report. Available online: https://www.cdc.gov/salmonella/oranienburg-10-19/index.html (accessed on 20 August 2022).
- Tomaštíková, Z.; Mrázková, M.; Kaňáková, M.; Karpíšková, R. Salmonellosis in an infant as a result of indirect contact with reptiles. Klin. Mikrobiol. Infekc. Lek. 2017, 23, 61–63. [Google Scholar]
- Hernandez, E.; Rodriguez, J.L.; Herrera-Leon, S.; Garcia, I.; de Castro, V.; Muniozguren, N. Salmonella Paratyphi B var Java infections associated with exposure to turtles in Bizkaia, Spain, September 2010 to October 2011. Euro Surveill. 2012, 17, 20201. [Google Scholar] [CrossRef] [PubMed]
- Lafuente, S.; Bellido, J.B.; Moraga, F.A.; Herrera, S.; Yagüe, A.; Montalvo, T.; de Simó, M.; Simón, P.; Caylà, J.A. Salmonella paratyphi B and Salmonella litchfield outbreaks associated with pet turtle exposure in Spain. Enferm. Infecc. Microbiol. Clin. 2013, 31, 32–35. [Google Scholar] [CrossRef] [PubMed]
- Editorial team; Bertrand, S.; Rimhanen-Finne, R.; Weill, F.X.; Rabsch, W.; Thornton, L.; Perevoscikovs, J.; van Pelt, W.; Heck, M. Salmonella infections associated with reptiles: The current situation in Europe. Euro. Surveill. 2008, 13, 18902. [Google Scholar]
- CDC. Reptile-associated salmonellosis—Selected states, 1998–2002. MMWR 2003, 52, 1206–1209. [Google Scholar]
- Sumiyama, D.; Shimizu, A.; Kanazawa, T.; Anzai, H.; Murata, K. Prevalence of Salmonella in green anoles (Anolis Carolinensis), an invasive alien species in Naha and Tomigusuku Cities, Okinawa Main Island, Japan. J. Vet. Med. Sci. 2020, 82, 678–680. [Google Scholar] [CrossRef]
- Zając, M.; Wasyl, D.; Różycki, M.; Ewa Bilska-Zając, E.; Fafiński, Z.; Iwaniak, W.; Krajewska, M.; Hoszowski, A.; Konieczna, O.; Fafińska, P.; et al. Free-living snakes as a source and possible vector of Salmonella spp. and parasites. Eur. J. Wildl. Res. 2016, 62, 161–166. [Google Scholar] [CrossRef]
- Geue, L.; Löschner, U. Salmonella enterica in reptiles of German and Austrian origin. Vet. Microbiol. 2002, 84, 79–91. [Google Scholar] [CrossRef]
- Nakadai, A.; Kuroki, T.; Kato, Y.; Suzuki, R.; Yamai, S.; Yaginuma, C.; Shiotani, R.; Yamanouchi, A.; Hayashidani, H. Prevalence of Salmonella spp. in pet reptiles in Japan. J. Vet. Med. Sci. 2005, 67, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.Y.; Chen, W.C.; Chin, S.C.; Lai, Y.H.; Tung, K.C.; Chiou, C.S.; Hsu, Y.M.; Chang, C.C. Prevalence and antimicrobial susceptibility of salmonellae isolates from reptiles in Taiwan. J. Vet. Diagn. Investig. 2010, 22, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Marin, C.; Lorenzo-Rebenaque, L.; Laso, O.; Villora-Gonzalez, J.; Vega, S. Pet Reptiles: A Potential Source of Transmission of Multidrug-Resistant Salmonella. Front. Vet. Sci. 2021, 7, 613718. [Google Scholar] [CrossRef] [PubMed]
- Bertelloni, F.; Chemaly, M.; Cerri, D.; Gall, F.L.; Ebani, V.V. Salmonella infection in healthy pet reptiles: Bacteriological isolation and study of some pathogenic characters. Acta Microbiol. Immunol. Hung. 2016, 63, 203–216. [Google Scholar] [CrossRef]
- Arnafia, W.; Ningrum, S.G.; Adji, R.S.; Lukman, D.W.; Pasaribu, F.H.; Wibawan, I.T. Isolation of Salmonella from reptiles in pet shop and its susceptibility to antibiotics in Indonesia. Inter. J. Bioflux. Soc. 2016, 8, 177–181. [Google Scholar]
- Lukac, M.; Pedersen, K.; Prukner-Radovcic, E. Prevalence of salmonella in captive reptiles from Croatia. J. Zoo Wildl. Med. 2015, 46, 234–240. [Google Scholar] [CrossRef]
- Leonard, S.R.; Lacher, D.W.; Lampel, K.A. Acquisition of the lac operon by Salmonella enterica. BMC Microbiol. 2015, 15, 173. [Google Scholar] [CrossRef][Green Version]
- Smirnova, I.N.; Kaback, H.R. A mutation in the lactose permease of Escherichia coli that decreases conformational flexibility and increases protein stability. Biochemistry 2003, 42, 3025–3031. [Google Scholar] [CrossRef]
- Callaway, Z.; Thomas, A.; Melrose, W.; Buttner, P.; Speare, R. Salmonella Virchow and Salmonella Weltevreden in a random survey of the Asian house gecko, Hemidactylus frenatus, in houses in northern Australia. Vector Borne Zoonotic Dis. 2011, 11, 621–625. [Google Scholar] [CrossRef]
- Smith, K.F.; Yabsley, M.J.; Sanchez, S.; Casey, C.L.; Behrens, M.D.; Hernandez, S.M. Salmonella isolates from wild-caught Tokay geckos (Gekko gecko) imported to the U.S. from Indonesia. Vector Borne Zoonotic Dis. 2012, 12, 575–582. [Google Scholar] [CrossRef]
- Ebani, V.V.; Cerri, D.; Fratini, F.; Meille, N.; Valentini, P.; Andreani, E. Salmonella enterica isolates from faeces of domestic reptiles and a study of their antimicrobial in vitro sensitivity. Res. Vet. Sci. 2005, 78, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Gorski, L.; Jay-Russell, M.T.; Liang, A.S.; Walker, S.; Bengson, Y.; Govoni, J.; Mandrell, R.E. Diversity of pulsed-field gel electrophoresis pulsotypes, serovars, and antibiotic resistance among Salmonella isolates from wild amphibians and reptiles in the California Central Coast. Foodborne Pathog. Dis. 2013, 10, 540–548. [Google Scholar] [CrossRef]
- Report of the Sweedesh National Veterinary Institute to the Commission 2001. Available online: https://www.sva.se/media/da2px1k2/zoonos-2000-eng.pdf (accessed on 12 September 2022).
- Horvath, L.; Kraft, M.; Fostiropoulos, K.; Falkowski, A.; Tarr, P.E. Salmonella enterica Subspecies diarizonae Maxillary Sinusitis in a Snake Handler: First Report. Open Forum Infect. Dis. 2016, 3, ofw066. [Google Scholar] [CrossRef] [PubMed]
- Gavrilovici, C.; Pânzaru, C.V.; Cozma, S.; Mârţu, C.; Lupu, V.V.; Ignat, A.; Miron, I.; Stârcea, M. Message from a turtle: Otitis with salmonella arizonae in children: Case report. Medicine 2017, 96, e8455. [Google Scholar] [CrossRef] [PubMed]
- Baranzelli, A.; Loïez, C.; Bervar, J.F.; Scherpereel, A.; Wallet, F. The snake raiser lung: An unusual cause of Salmonella enterica subspecies arizonae pneumonia. Med. Mal. Infect. 2017, 47, 424–425. [Google Scholar] [CrossRef]
- Hervás, J.A.; Rosell, A.; Hervás, D.; Rubio, R.; Dueñas, J.; Mena, A. Reptile pets-associated Salmonella enterica subspecies diarizonae gastroenteritis in a neonate. Pediatr. Infect. Dis. J. 2012, 31, 1102–1103. [Google Scholar] [CrossRef]
- Meletiadis, A.; Biolatti, C.; Mugetti, D.; Zaccaria, T.; Cipriani, R.; Pitti, M.; Decastelli, L.; Cimino, F.; Dondo, A.; Maurella, C.; et al. Surveys on Exposure to Reptile-Associated Salmonellosis (RAS) in the Piedmont Region-Italy. Animals 2022, 12, 906. [Google Scholar] [CrossRef]
- CDC. Reptile-associated salmonellosis—Selected states, 1994–1995. MMWR 1995, 44, 347–350. [Google Scholar]
- CDC. Reptile-associated salmonellosis—Selected states, 1996–1998. MMWR 1999, 48, 1009–1013. [Google Scholar]
- Bjelland, A.M.; Sandvik, L.M.; Skarstein, M.M.; Svendal, L.; Debenham, J.J. Prevalence of Salmonella serovars isolated from reptiles in Norwegian zoos. Acta Vet. Scand. 2020, 62, 3. [Google Scholar] [CrossRef]
- McWhorter, A.; Owens, J.; Valcanis, M.; Olds, L.; Myers, C.; Smith, I.; Trott, D.; McLelland, D. In vitro invasiveness and antimicrobial resistance of Salmonella enterica subspecies isolated from wild and captive reptiles. Zoonoses Public Health 2021, 68, 402–412. [Google Scholar] [CrossRef] [PubMed]
- Pasmans, F.; Martel, A.; Boyen, F.; Vandekerchove, D.; Wybo, I.; Immerseel, F.V.; Heyndrickx, M.; Collard, J.M.; Ducatelle, R.; Haesebrouck, F. Characterization of Salmonella isolates from captive lizards. Vet. Microbiol. 2005, 110, 285–291. [Google Scholar] [CrossRef]
- Guyomard-Rabenirina, S.; Weill, F.X.; Le Hello, S.; Bastian, S.; Berger, F.; Ferdinand, S.; Legreneur, P.; Loraux, C.; Malpote, E.; Muanza, B.; et al. Reptiles in Guadeloupe (French West Indies) are a reservoir of major human Salmonella enterica serovars. PLoS ONE 2019, 14, e0220145. [Google Scholar] [CrossRef]
- Tomastikova, Z.; Barazorda Romero, S.; Knotek, Z.; Karpiskova, R. Prevalence and characteristics of Salmonella species isolated from captive reptiles in the Czech Republic. Vet. Med. 2017, 62, 456–469. [Google Scholar] [CrossRef]
- Pławińska-Czarnak, J.; Wódz, K.; Kizerwetter-Swida, M.; Bogdan, J.; Kwieciński, P.; Nowak, T.; Strzałkowska, Z.; Anusz, K. Multi-Drug Resistance to Salmonella spp. When Isolated from Raw Meat Products. Antibiotics 2022, 11, 876. [Google Scholar] [CrossRef] [PubMed]
- Qin, X.; Yang, M.; Cai, H.; Liu, Y.; Gorris, L.; Aslam, M.Z.; Jia, K.; Sun, T.; Wang, X.; Dong, Q. Antibiotic Resistance of Salmonella Typhimurium Monophasic Variant 1,4,[5],12:i:-in China: A Systematic Review and Meta-Analysis. Antibiotics 2022, 11, 532. [Google Scholar] [CrossRef]
- Magnet, S.; Courvalin, P.; Lambert, T. Activation of the Cryptic aac(6′)-Iy Aminoglycoside Resistance Gene of Salmonella by a Chromosomal Deletion Generating a Transcriptional Fusion. J. Bacteriol. 1999, 181, 6650–6655. [Google Scholar] [CrossRef]
- Zhou, M.; Shi, Q.; Zhang, X.; Mei, L.; Ye, Y.; Fang, C.; Shang, S. Salmonella enterica subsp. diarizonae Harboring ST233, ST1263, and ST1845 in Children. Front. Cell Infect. Microbiol. 2021, 11, 727811. [Google Scholar] [CrossRef]
- García-Soto, S.; Abdel-Glil, M.Y.; Tomaso, H.; Linde, J.; Methner, U. Emergence of Multidrug-Resistant Salmonella enterica Subspecies enterica Serovar Infantis of Multilocus Sequence Type 2283 in German Broiler Farms. Front. Microbiol. 2020, 11, 1741. [Google Scholar] [CrossRef]
| Animals | Number of Samples | Species (Number of Samples) | Diet Group | Number of Salmonella Positive Samples | Number of Salmonella Isolates |
|---|---|---|---|---|---|
| Snakes | 31 | Pantheropsis guttatus (14) Python regius (3) Boa constrictor (4) Lampropeltis triangulum (4) Morelia pilota (1) Orthrophis teaniurus (5) | carnivore carnivore carnivore carnivore carnivore carnivore | 12 (86%) 3 (100%) 4 (100%) 3 (75%) 1 (100%) 4 (80%) | 13 3 4 4 1 4 |
| Total: 27/31 (87.1%) | Total: 29/51 (56.9%) | ||||
| Lizards | 18 | Pogona vitticeps (6) Iguana iguana (4) Eublepharis macularius (3) Furcifer pardali (5) | omnivore herbivore carnivore omnivore | 6 (100%) 3 (75%) 3 (100%) 2 (40%) | 7 3 3 2 |
| Total: 14/18 (77.8%) | Total: 15/51 (29.4%) | ||||
| Turtles | 18 | Testudo horsfieldii (8) Testudo hermanni (9) Chelonoidis carbonaria (1) | herbivore herbivore herbivore | 4 (50%) 3 (33%) 0 | 4 3 0 |
| Total: 7/18 (38.9%) | Total: 7/51 (13.7%) | ||||
| Total: | 67 | 48/67 (71.6%) | 51 (100%) |
| Species | Salmonella enterica | |||
|---|---|---|---|---|
| Subspecies Number of Strains | enterica n = 34 | salamae n = 2 | arizonae n = 2 | diarizonae n = 13 |
| ONPG (24 h) | 10 [29%] | 1 [50%] | 2 [100%] | 13 [100%] |
| Lactose | 8 [23.5%] * | 0 | 1 [50%] | 10 [77%] |
| Salicin | 0 | 0 | 0 | 0 |
| Dulcitol | 34 [100%] | 2 [100%] | 0 | 0 |
| Sorbitol | 34 [100%] | 1 [50%] | 2 [100%] | 11 [85%] |
| L(+)-tartrate ** | 34 [100%] | 1 [50%] | 0 | 0 |
| Mucate | 34 [100%] | 2 [100%] | 1 [50%] | 0 |
| Malonate | 2 [6%] | 2 [100%] | 2 [100%] | 13 [100%] |
| Galacturonate | 0 | 2 [100%] | 1 [50%] | 13 [100%] |
| β-glucuronidase | 11 [32%] | 1 [50%] | 0 | 13 [100%] |
| Gelatinase | 0 | 0 | 0 | 0 |
| No. | Serovar | Subsp. | Number of Strains (%) | Snakes n = 31 | Lizards n = 18 | Turtles n = 18 | Host | Strain ID |
|---|---|---|---|---|---|---|---|---|
| 1 | 9,12:a:1,5 | II | 1 (2.0) | 1 | boa constrictor | 36a | ||
| 2 | 48:d:z6 | II | 1 (2.0) | 1 | steppe tortoise | 17 | ||
| 3 | 41:z4,z23:- | IIIa | 2 (3.9) | 2 | milk snake beauty rat snake | 40 52a | ||
| 4 | 16:z10:e,n,x,z15 | IIIb | 4 (7.8) | 4 | corn snake milk snake beauty rat snake beauty rat snake | 29a 33B 50 51 | ||
| 5 | 47:i:z53 | IIIb | 4 (7.8) | 4 | corn snake milk snake corn snake beauty rat snake | 30b 32 38 49a | ||
| 6 | 47:z10:z35 | IIIb | 1 (2.0) | 1 | ball python | 15a | ||
| 7 | 48:i:z | IIIb | 1 (2.0) | 1 | boa constrictor | 26 | ||
| 8 | 50:l,v:z | IIIb | 1 (2.0) | 1 | panther chameleon | 57a | ||
| 9 | 61:k:z35 | IIIb | 1 (2.0) | 1 | corn snake | R4 | ||
| 10 | 61:l,v:z | IIIb | 1 (2.0) | 1 | panther chameleon | 56a | ||
| 11 | Abony | I | 1 (2.0) | 1 | Greek tortoise | 68 | ||
| 12 | Adelaide | I | 1 (2.0) | 1 | ball python | 13 | ||
| 13 | Alpenquai | I | 1 (2.0) | 1 | Greek tortoise | 66 | ||
| 14 | Cotham | I | 1 (2.0) | 1 | leopard gecko | 60 | ||
| 15 | Fluntern | I | 1 (2.0) | 1 | leopard gecko | 58b | ||
| 16 | Lattenkamp | I | 8 (15.7) | 7 | 1 | bearded dragon leopard gecko bearded dragon bearded dragon bearded dragon green iguana green iguana steppe tortoise | 55b 59 61 62 63 64 65 70 | |
| 17 | Midway | I | 1 (2.0) | 1 | corn snake | 28 | ||
| 18 | Muenchen | I | 2 (3.9) | 2 | boa constrictor milk snake | 27 33A | ||
| 19 | Newport | I | 3 (5.9) | 2 | 1 | corn snake bearded dragon carpet python | 16 46b 48 | |
| 20 | Oranienburg | I | 3 (5.9) | 3 | corn snake corn snake boa constrictor | 5 6a 35 | ||
| 21 | Paratyphi B var. Java | I | 2 (3.9) | 2 | corn snake corn snake | 7 31a | ||
| 22 | Patience | I | 1 (2.0) | 1 | Greek tortoise | 67 | ||
| 23 | Poona | I | 4 (7.8) | 4 | corn snake ball python corn snake corn snake | 30a 34 37 39 | ||
| 24 | Tennessee | I | 3 (5.9) | 3 | bearded dragon green iguana bearded dragon | 14 45 46a | ||
| 25 | Virchow | I | 2 (3.9) | 2 | steppe tortoise Greek tortoise | 69 71 | ||
| Total number (%) | 51 (100) | 29 (57) | 15 (29) | 7 (14) |
| Isolate ID | 50 (S21_0833) | 51 (S21_0834) | 33B (S21_1654) | 33A (S21_0821) |
|---|---|---|---|---|
| Subspecies | IIIb | IIIb | IIIb | I |
| Serotype | 16:z10:e,n,x,z15 | 16:z10:e,n,x,z15 | 16:z10:e,n,x,z15 | Muenchen (6,8:d:1,2) |
| Source | beauty rat snake (Orthriophis taeniurus) | beauty rat snake (Orthriophis taeniurus) | milk snake (Lampropeltis triangulum) | milk snake (Lampropeltis triangulum) |
| Acc. No. | SAMN25211032 | SAMN25211031 | SAMN25211030 | SAMN25046248 |
| Genome size | 5921031 bp | 5922870 bp | 5984163 bp | 5376408 bp |
| Contigs | 339 | 293 | 245 | 115 |
| Resistance genes | aac(6′)-Iaa *, kdeA, mdtM, acrF, emrD | aac(6′)-Iaa, kdeA, mdtM, acrF, emrD | aac(6′)-Iaa, kdeA, mdtM, acrF, emrD | aac(6′)-Iaa, kdeA, mdtM, acrF, emrD mdsA, mdsB |
| Lactose operon genes | lacZ **, locus_tag L4A35_20235 (oligosaccharide MFS transporter), lacA ***, lacI **** (Acc. No. JAKJQB010000022.1) | lacZ, locus_tag L4B25_00380 (oligosaccharide MFS transporter), lacA, lacI (Acc. No. JAKJQC010000001.1) | lacZ, locus_tag L4A43_06620 (oligosaccharide MFS transporter), lacA, lacI (Acc. No. JAKJQD010000004.1) | Not found |
| Pathogenic Potential | Zoonotic Potential | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Serovar | Subsp. | Number of Infections in US in 2006–2016 [25] | Number of Infections in EU in 2018–2020 [1] | Number of Infections in Queensland in 2007–2016 [26] | Host | Age of Patients with RAS/Median [years] | Number of Infections | Country | Year | Reference |
| Abony | I | 62 | – a | – | turtle turtle | 4 <1 | 1 1 | Japan Belgium | 2007–8 2008 | [27] [28] |
| Adelaide | I | 1001 | – | – | ||||||
| Alpenquai | I | – | – | – | ||||||
| Cotham | I | 429 | – | – | lizards | <1–79/3 | 160 | USA | 2012–14 | [29] |
| Fluntern | I | 77 | – | – | ||||||
| Lattenkamp | I | 17 | – | – | ||||||
| Midway | I | – | – | – | ||||||
| Muenchen | I | 1216 | 703 | – | reptiles b turtle | <5 <1–60/10 | 48 132 | UK USA | 2015 2009 | [30] [10] |
| Newport | I | 47,481 | 2233 | 160 | reptiles b turtle turtles | <5 1.25 <1–85/6 | 48 1 124 | UK Chile USA | 2015 ? 2012 | [30] [31] [10] |
| Oranienburg | I | 8012 | – | 88 | reptiles b turtle bearded dragon | <5 <5 ? | 48 26 1 | UK USA Czech Republic | 2015 2019 2016 | [30] [32] [33] |
| Paratyphi B var. Java | I | 4486 | – | 355 | turtle turtle turtle turtle snake b | <1–10 <1–4 1–87/7 1–75/6 50 | 8 4 107 132 1 | Spain Spain USA USA Finland | 2010–11 2009 2007 2011 2005–8 | [34] [35] [10] [10] [36] |
| Patience | I | – | – | – | ||||||
| Poona | I | 3844 | – | – | turtle turtle turtle turtle turtle snake iguana | <1 to 82/6 5 <1–84/3.5 <1–83/3 <1–75/5 <1 2 | 61 1 58 78 40 1 1 | USA Japan USA USA USA Germany USA | 2015 2007–8 2012 2012 2014 2008 2002 | [11] [27] [10] [10] [10] [36] [37] |
| Tennessee | I | 1326 | – | – | bearded dragon | <1 | 1 | USA | 2000 | [37] |
| Virchow | I | 980 | – | 2804 | ||||||
| 9,12:a:1,5 | II | 2 | – | – | ||||||
| 48:d:z6 | II | 10 | – | – | ||||||
| 41:z4,z23:- | IIIa | 146 | – | – | snake or lizard snake | <1 <1–57 | 2 3 | Germany Belgium | 2007–8 2008 | [36] [36] |
| 16:z10:e,n,x,z15 | IIIb | 21 | – | – | ||||||
| 47:i:z53 | IIIb | – | – | – | snake | 25 | 1 | Germany | 2006 | [36] |
| 47:z10:z35 | IIIb | 3 | – | – | ||||||
| 48:i:z | IIIb | 69 | – | – | ||||||
| 50:l,v:z | IIIb | 3 | – | – | ||||||
| 61:k:z35 | IIIb | – | – | – | ||||||
| 61:l,v:z | IIIb | – | – | – | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dec, M.; Zając, M.; Puchalski, A.; Szczepaniak, K.; Urban-Chmiel, R. Pet Reptiles in Poland as a Potential Source of Transmission of Salmonella. Pathogens 2022, 11, 1125. https://doi.org/10.3390/pathogens11101125
Dec M, Zając M, Puchalski A, Szczepaniak K, Urban-Chmiel R. Pet Reptiles in Poland as a Potential Source of Transmission of Salmonella. Pathogens. 2022; 11(10):1125. https://doi.org/10.3390/pathogens11101125
Chicago/Turabian StyleDec, Marta, Magdalena Zając, Andrzej Puchalski, Klaudiusz Szczepaniak, and Renata Urban-Chmiel. 2022. "Pet Reptiles in Poland as a Potential Source of Transmission of Salmonella" Pathogens 11, no. 10: 1125. https://doi.org/10.3390/pathogens11101125
APA StyleDec, M., Zając, M., Puchalski, A., Szczepaniak, K., & Urban-Chmiel, R. (2022). Pet Reptiles in Poland as a Potential Source of Transmission of Salmonella. Pathogens, 11(10), 1125. https://doi.org/10.3390/pathogens11101125







