Prevalence and Genotyping of HPV in Oral Squamous Cell Carcinoma in Northern Brazil
Abstract
1. Introduction
2. Materials and Methods
2.1. Clinical Parameters
2.2. Sample Collection and Processing
2.3. DNA Extraction from Paraffin Samples
2.4. HPV Detection and Typification
2.5. Statistical Analysis
3. Results
3.1. Sample Characteristics and Anatomical Subsites
3.2. Histological Analysis
3.3. HPV Prevalence and Typification
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Monteiro, J.C.; Fonseca, R.R.D.S.; Ferreira, T.C.D.S.; Rodrigues, L.L.S.; Da Silva, A.R.B.; Gomes, S.T.; Silvestre, R.V.D.; Silva, A.N.M.R.; Pamplona, I.; Vallinoto, A.C.R.; et al. Prevalence of High Risk HPV in HIV-Infected women from Belem, Para, Amazon Region of Brazil: A Cross-Sectional Study. Front. Public Health 2021, 9, 649152. [Google Scholar] [CrossRef] [PubMed]
- International Committee on Taxonomy of Viruses (ICTV). Virus Taxonomy: Release. 2020. Available online: http://www.ictvonline.org/virusTaxonomy.asp (accessed on 2 June 2021).
- Bzhalava, D.; Eklund, C.; Dillner, J. International standardization and classification of human papillomavirus types. Virology 2015, 476, 341–344. [Google Scholar] [CrossRef] [PubMed]
- Melo, B.A.C.; Vilar, L.G.; Oliveira, N.R.; Lima, P.O.; Pinheiro, M.B.; Domingueti, C.P.; Pereira, M.C. Human papillomavirus infection and oral squamous cell carcinoma—A systematic review. Braz. J. Otorhinolaryngol. 2021, 87, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Machado, A.P.; Gatto de Almeida, F.; Bonin, C.M.; Martins Prata, T.T.; Sobrinho Ávilla, L.; Junqueira Padovani, C.T.; Teixeira Ferreira, A.M.; Fernandes, C.E.D.S.; Tozetti, I.A. Presence of highly oncogenic human papillomavirus in the oral mucosa of asymptomatic men. Braz. J. Infect. Dis. 2014, 18, 266–270. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, A.C.D.S.; Nocetti, M.C.; Lugo, L.Z.A.; Jacob, C.M.B.; Machado, A.P.; Padovani, C.T.J.; Ferreira, A.M.T.; Fernandes, C.E.D.S.; Tozetti, I.A. Oncogenic high-risk human papillomavirus in patients with full denture. Braz. Oral Res. 2019, 25, e091. [Google Scholar] [CrossRef] [PubMed]
- de Sanjosé, S.; Brotons, M.; Pavón, M.A. The natural history of human papillomavirus infection. Best Pract. Res. Clin. Obstet. Gynaecol. 2018, 47, 2–13. [Google Scholar] [CrossRef] [PubMed]
- Burd, E.M.; Dean, C.L. Human Papillomavirus. Microbiol. Spectr. 2016, 4, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Rampias, T.; Sasaki, C.; Weinberger, P.; Psyrri, A. E6 and e7 gene silencing and transformed phenotype of human papillomavirus 16-positive oropharyngeal cancer cells. J. Natl. Cancer Inst. 2009, 101, 412–423. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Xu, C.; Long, J.; Shen, D.; Zhou, W.; Zhou, Q.; Yang, J.; Jiang, M. E6 and E7 gene silencing results in decreased methylation of tumor suppressor genes and induces phenotype transformation of human cervical carcinoma cell lines. Oncotarget 2015, 6, 23930–23943. [Google Scholar] [CrossRef][Green Version]
- Dvoryaninova, O.Y.; Chainzonov, E.L.; Litvyakov, N.V. The clinical aspects of HPV-positive cancer of the oral cavity and oropharynx. Vestnik Otorinolaringol. 2016, 81, 72–77. [Google Scholar] [CrossRef]
- Bruni, L.; Diaz, M.; Castellsagué, X.; Ferrer, E.; Bosch, F.X.; de Sanjosé, S. Cervical human papillomavirus prevalence in 5 continents: Meta-analysis of 1 million women with normal cytological findings. J. Infect. Dis. 2010, 202, 1789–1799. [Google Scholar] [CrossRef] [PubMed]
- Simms, K.T.; Steinberg, J.; Caruana, M.; Smith, M.A.; Lew, J.-B.; Soerjomataram, I.; Castle, P.E.; Bray, F.; Canfell, K. Impact of scaled up human papillomavirus vaccination and cervical screening and the potential for global elimination of cervical cancer in 181 countries, 2020–2099: A modelling study. Lancet Oncol. 2019, 20, 394–407. [Google Scholar] [CrossRef]
- Colpani, V.; Bidinotto, A.B.; Falavigna, M.; Giozza, S.P.; Benzaken, A.S.; Pimenta, C.; Maranhão, A.G.; Domingues, C.M.A.S.; Hammes, L.S.; Wendland, E.M. Prevalence of papillomavirus in Brazil: A systematic review protocol. BMJ Open 2016, 6, e011884. [Google Scholar] [CrossRef] [PubMed]
- Colpani, V.; Soares Falcetta, F.; Bacelo Bidinotto, A.; Kops, N.L.; Falavigna, M.; Serpa Hammes, L.; Schwartz Benzaken, A.; Kalume Maranhão, A.G.; Domingues, C.M.A.S.; Wendland, E.M. Prevalence of human papillomavirus (HPV) in Brazil: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0229154. [Google Scholar] [CrossRef]
- Syrjänen, K.; Syrjänen, S.; Lamberg, M.; Pyrhönen, S.; Nuutinen, J. Morphological and immunohistochemical evidence suggesting human papillomavirus (HPV) involvement in oral squamous cell carcinogenesis. Int. J. Oral Surg. 1983, 12, 418–424. [Google Scholar] [CrossRef]
- Hübbers, C.U.; Akgül, B. HPV and cancer of the oral cavity. Virulence 2015, 6, 244–248. [Google Scholar] [CrossRef]
- van der Waal, I. Potentially malignant disorders of the oral and oropharyngeal mucosa; terminology, classification and present concepts of management. Oral Oncol. 2009, 45, 317–323. [Google Scholar] [CrossRef]
- Jiang, S.; Dong, Y. Human papillomavirus and oral squamous cell carcinoma: A review of HPV-positive oral squamous cell carcinoma and possible strategies for future. Curr. Probl. Cancer 2017, 41, 323–327. [Google Scholar] [CrossRef]
- Syrjänen, S. Oral manifestations of human papillomavirus infections. Eur. J. Oral Sci. 2018, 126, 49–66. [Google Scholar] [CrossRef]
- Tumban, E. A Current Update on Human Papillomavirus-Associated Head and Neck Cancers. Viruses 2019, 11, 922. [Google Scholar] [CrossRef]
- Panarese, I.; Aquino, G.; Ronchi, A.; Longo, F.; Montella, M.; Cozzolino, I.; Roccuzzo, G.; Colella, G.; Caraglia, M.; Franco, R. Oral and Oropharyngeal squamous cell carcinoma: Prognostic and predictive parameters in the etiopathogenetic route. Expert Rev. Anticancer Ther. 2019, 19, 105–119. [Google Scholar] [CrossRef] [PubMed]
- Maymone, M.B.C.; Greer, R.O.; Burdine, L.K.; Dao-Cheng, A.; Venkatesh, S.; Sahitya, P.C.; Maymone, A.C.; Kesecker, J.; Vashi, N.A. Benign oral mucosal lesions: Clinical and pathological findings. J. Am. Acad Dermatol 2019, 81, 43–56. [Google Scholar] [CrossRef]
- Georgaki, M.; Avgoustidis, D.; Theofilou, V.; Piperi, E.; Pettas, E.; Kalyvas, D.; Vlachodimitropoulos, D.; Perisanidis, C.; Lazaris, A.; Nikitakis, N. Recurrence in Oral Premalignancy: Clinicopathologic and Immunohistochemical Analysis. Diagnostics 2021, 11, 872. [Google Scholar] [CrossRef]
- Sadeghipour, A.; Babaheidarian, P. Making Formalin-Fixed, Paraffin Embedded Blocks. Methods Mol. Biol. 2019, 1897, 253–268. [Google Scholar] [PubMed]
- Araújo, M.V.; Pinheiro, H.H.; Pinheiro, J.d.J.; Quaresma, J.A.; Fuzii, H.T.; Medeiros, R.C. Prevalence of human papillomavirus (HPV) in Belem, Para State, Brazil, in the oral cavity of individuals without clinically diagnosable injuries. Cad. Saude Publica 2014, 30, 1115–1119. [Google Scholar] [CrossRef] [PubMed]
- Matos, L.L.; Miranda, G.A.; Cernea, C.R. Prevalence of oral and oropharyngeal human papillomavirus infection in Brazilian population studies: A systematic review. Braz. J. Otorhinolaryngol. 2015, 81, 554–567. [Google Scholar] [CrossRef] [PubMed]
- Moro, J.D.S.; Maroneze, M.C.; Ardenghi, T.M.; Barin, L.M.; Danesi, C.C. Oral and oropharyngeal cancer: Epidemiology and survival analysis. Einstein 2018, 16, eAO4248. [Google Scholar] [CrossRef]
- dos Santos, J.I.D.O.; Ferreira, J.S.; Munhoz, I.G.A.; de Lemos, D.L.P.; Tenório, D.D.P.Q.; Rodas, L.O.; de Almeida, F.; Fernandes, M.C.B.; Vieira, L.L.M.; de Freitas Melo, M.E.; et al. Perspectives of oral cancer’s epidemiological panorama in Brazil. Rev. Med. 2020, 99, 556–562. [Google Scholar]
- Rodrigues, M.S.A.; Nascimento, R.S.; Fonseca, R.R.S.; Silva-Oliveira, G.C.; Machado, L.F.A.; Kupek, E.; Fischer, B.; Oliveira-Filho, A.B. Oral HPV among people who use crack-cocaine: Prevalence, genotypes, risk factors, and key interventions in a remote Northern Brazilian region. Clin. Oral Investig. 2021, 25, 759–767. [Google Scholar] [CrossRef]
- Drop, B.; Strycharz-Dudziak, M.; Kliszczewska, E.; Polz-Dacewicz, M. Coinfection with Epstein-Barr Virus (EBV), Human Papilloma Virus (HPV) and Polyoma BK Virus (BKPyV) in Laryngeal, Oropharyngeal and Oral Cavity Cancer. Int. J. Mol. Sci. 2017, 18, 2752. [Google Scholar] [CrossRef]
- Madathil, S.; Rousseau, M.C.; Joseph, L.; Coutlée, F.; Schlecht, N.F.; Franco, E.; Nicolau, B. Latency of tobacco smoking for head and neck cancer among HPV-positive and HPV-negative individuals. Int. J. Cancer 2020, 147, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Auguste, A.; Deloumeaux, J.; Joachim, C.; Gaete, S.; Michineau, L.; Herrmann-Storck, C.; Duflo, S.; Luce, D. Joint effect of tobacco, alcohol, and oral HPV infection on head and neck cancer risk in the French West Indies. Cancer Med. 2020, 9, 6854–6863. [Google Scholar] [CrossRef]
- Smith, E.M.; Rubenstein, L.M.; Haugen, T.H.; Hamsikova, E.; Turek, L.P. Tobacco and alcohol use increases the risk of both HPV-associated and HPV-independent head and neck cancers. Cancer Causes Control. 2010, 21, 1369–1378. [Google Scholar] [CrossRef] [PubMed]
- Bezerra, N.V.; Leite, K.L.; de Medeiros, M.M.; Martins, M.L.; Cardoso, A.M.; Alves, P.M.; Padilha, W.; Cavalcanti, Y. Impact of the anatomical location, alcoholism and smoking on the prevalence of advanced oral cancer in Brazil. Med. Oral Patol. Oral Cir. Bucal. 2018, 23, e295–e301. [Google Scholar] [CrossRef] [PubMed]
- Bean, M.B.; Switchenko, J.M.; Steuer, C.E.; Patel, M.; Higgins, K.; McDonald, M.; Chen, G.Z.; Beitler, J.J.; Shin, D.M.; Gillespie, T.; et al. Demographic and Socioeconomic Factors Associated with Metastases at Presentation in HPV-Related Squamous Cell Carcinoma of the Head and Neck: An NCDB Analysis. JCO Oncol. Pract. 2020, 16, e476–e487. [Google Scholar] [CrossRef] [PubMed]
- Freire, A.R.; Freire, D.E.W.G.; Araújo, E.C.F.; de Lucena, E.H.G.; Cavalcanti, Y.W. Influence of Public Oral Health Services and Socioeconomic Indicators on the Frequency of Hospitalization and Deaths due to Oral Cancer in Brazil, between 2002–2017. Int. J. Environ. Res. Public Health 2020, 18, 238. [Google Scholar] [CrossRef]
- Celeste, R.K.; Moura, F.R.; Santos, C.P.; Tovo, M.F. Analysis of outpatient care in Brazilian municipalities with and without specialized dental clinics, 2010. Cad. Saude Publica 2014, 30, 511–521. [Google Scholar] [CrossRef]
| Parameters | Total (n = 101) | Malignant (n = 59) | Benign (n = 42) | p Value |
|---|---|---|---|---|
| Gender | ||||
| Female | 55 | 29 (49.2%) | 26 (62%) | 0.2866 a |
| Male | 46 | 30 (50.8%) | 16 (38%) | |
| Ethnicity † | ||||
| White | 37 | 22 (37.2%) | 15 (35.8%) | 0.9818 b |
| Black | 15 | 9 (15.5%) | 6 (14.2%) | |
| Mixed | 46 | 26 (44%) | 20 (47.6%) | |
| Indigenous | 3 | 2 (3.3%) | 1 (2.4%) | |
| Age (years) | ||||
| 18–29 | 20 | 5 (8.4%) | 15 (35.8%) | 0.0004 b |
| 30–39 | 9 | 2 (3.3%) | 7 (16.6%) | |
| 40–49 | 13 | 8 (13.5%) | 5 (12%) | |
| 50–59 | 16 | 9 (15.5%) | 7 (16.6%) | |
| 60–69 | 25 | 19 (32.2%) | 6 (14.2%) | |
| 70–79 | 7 | 6 (10.1%) | 1 (2.4%) | |
| ≥80 | 11 | 10 (17%) | 1 (2.4%) | |
| Smoking | ||||
| Yes | 71 | 37 (62.7%) | 34 (81%) | 0.2687 a |
| No | 30 | 22 (37.3%) | 8 (19%) | |
| Alcohol overconsumption | ||||
| Yes | 71 | 44 (74.5%) | 27 (64.3%) | 0.3710 a |
| No | 30 | 15 (25.5%) | 15 (35.7%) | |
| Tobacco chewing | ||||
| Yes | 18 | 10 (17%) | 8 (19%) | 0.9937 a |
| No | 83 | 49 (83%) | 34 (81%) | |
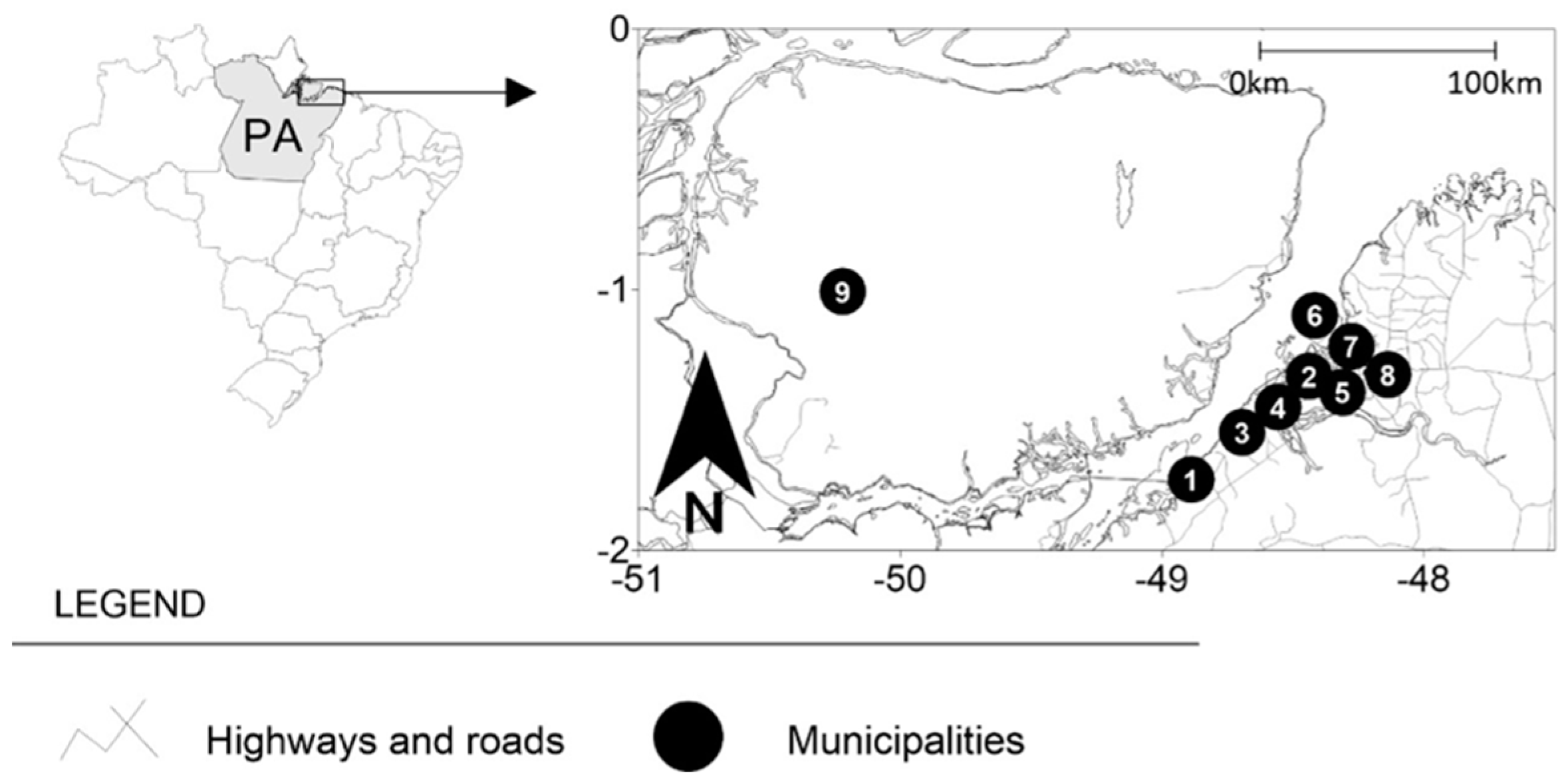
| Source | ||||
| Urban cities * | 75 | 44 (58.7%) | 31 (41.3%) | 0.8855 a |
| Rural cities ‡ | 26 | 15 (57.7%) | 11 (42.3) | |
| Belém * | 36 | 20 (33.8%) | 16 (38%) | 0.9419 b |
| Ananindeua * | 20 | 13 (22%) | 7 (16.6%) | |
| Marituba * | 9 | 5 (8.4%) | 4 (9.5%) | |
| Santa Bárbara * | 10 | 6 (10.1%) | 4 (9.5%) | |
| Mosqueiro ‡ | 4 | 1 (1.7%) | 3 (7.1%) | |
| Abaetetuba ‡ | 6 | 4 (6.7%) | 2 (4.7%) | |
| Santa Izabel ‡ | 9 | 5 (8.4%) | 4 (9.5%) | |
| Marajó ‡ | 3 | 2 (3.3%) | 1 (2.4%) | |
| Barcarena ‡ | 4 | 3 (5.6%) | 1 (2.4%) | |
| Sexually active | ||||
| Yes | 90 | 50 (84.7%) | 40 (95.2%) | 0.1647 b |
| No | 11 | 9 (15.3%) | 2 (4.8%) | |
| Condom use | ||||
| Always | 76 | 47 (79.6%) | 29 (69%) | 0.4118 b |
| Sometimes | 22 | 10 (17%) | 12 (28.5%) | |
| Never | 3 | 2 (3.4%) | 1 (2.5%) | |
| Partners n°/past year | ||||
| 1 | 61 | 41 (69.5%) | 20 (%) | 0.0446 a |
| >2 | 40 | 18 (30.5%) | 22 (%) | |
| Previous STI’s diagnosis | ||||
| Yes | 49 | 28 (47.5%) | 21 (50%) | 0.9601 a |
| No | 52 | 31 (52.5%) | 21 (50%) |
| Parameters | Total | Malignant (n = 59) | Benign (n = 42) | p Value |
|---|---|---|---|---|
| Anatomic region | ||||
| Upper gingiva | 46 | 24 (40.6%) | 22 (52.3%) | 0.4713 b |
| Lower gingiva | 17 | 11 (18.7%) | 6 (14.2%) | |
| Tongue | 19 | 12 (20.3%) | 7 (16.9%) | |
| Lips and buccal mucosa | 16 | 10 (17%) | 6 (14.2%) | |
| Oropharynx | 3 | 2 (3.4%) | 1 (2.4%) |
| Parameters | Total | Malignant (n = 59) | Benign (n = 42) | p Value |
|---|---|---|---|---|
| Histopathological diagnosis | ||||
| Oral Squamous Cell Carcinoma | 40 | 40 (67.7%) | - | <0.0001 b |
| Leukoplakia | 9 | 9 (15.2%) | - | |
| Erythroplakia | 7 | 7 (11.8%) | - | |
| Oral Lichen planus | 2 | 2 (3.3%) | - | |
| Carcinoma in situ | 1 | 1 (2%) | - | |
| Traumatic fibroma | 20 | - | 20 (47.6%) | |
| Verruca vulgaris | 3 | - | 3 (7.1%) | |
| Focal epithelial hyperplasia | 5 | - | 5 (12%) | |
| Papilloma | 4 | - | 4 (9.5%) | |
| Condyloma acuminatum | 8 | - | 8 (19%) | |
| Pyogenic granuloma | 1 | - | 1 (2.4%) | |
| Periodontal abscess | 1 | - | 1 (2.4%) |
| Parameters | Malignant (n = 59) | Benign (n = 42) | p Value |
|---|---|---|---|
| HPV negative | 42 (71.2%) | 32 (76.2%) | 0.6520 c |
| HPV positive | 17 (28.8%) | 10 (23.8%) | |
| Oral Squamous Cell Carcinoma | 12 (70.5%) | - | |
| Leukoplakia | 4 (23.5%) | - | |
| Erythroplakia | 1 (6%) | - | |
| Papilloma | - | 3 (30%) | |
| Verruca vulgaris | - | 3 (30%) | |
| Condyloma Acuminatum | - | 4 (40%) | |
| Genotypes | |||
| High oncogenic risk (n = 17) | |||
| HPV-16 | 10 (58.8%) | ||
| HPV-18 | 5 (29.4%) | - | |
| HPV-52 | 1 (5.9%) | - | |
| HPV-58 | 1 (5.9%) | - | |
| Low oncogenic risk (n = 10) | |||
| HPV-6 | - | 6 (60.0%) | |
| HPV-11 | - | 3 (30.0%) | |
| HPV-42 | - | 1 (10.0%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Menezes, S.A.F.; Miranda, Y.M.S.; da Silva, Y.M.; Carvalho, T.R.B.; Alves, F.R.S.; Silvestre, R.V.D.; Oliveira-Filho, A.B.; de Alencar Menezes, T.O.; de Souza Fonseca, R.R.; Laurentino, R.V.; et al. Prevalence and Genotyping of HPV in Oral Squamous Cell Carcinoma in Northern Brazil. Pathogens 2022, 11, 1106. https://doi.org/10.3390/pathogens11101106
de Menezes SAF, Miranda YMS, da Silva YM, Carvalho TRB, Alves FRS, Silvestre RVD, Oliveira-Filho AB, de Alencar Menezes TO, de Souza Fonseca RR, Laurentino RV, et al. Prevalence and Genotyping of HPV in Oral Squamous Cell Carcinoma in Northern Brazil. Pathogens. 2022; 11(10):1106. https://doi.org/10.3390/pathogens11101106
Chicago/Turabian Stylede Menezes, Silvio Augusto Fernandes, Yasmim Marçal Soares Miranda, Yngrid Monteiro da Silva, Tábata Resque Beckmann Carvalho, Flávia Rayane Souza Alves, Rodrigo Vellasco Duarte Silvestre, Aldemir Branco Oliveira-Filho, Tatiany Oliveira de Alencar Menezes, Ricardo Roberto de Souza Fonseca, Rogério Valois Laurentino, and et al. 2022. "Prevalence and Genotyping of HPV in Oral Squamous Cell Carcinoma in Northern Brazil" Pathogens 11, no. 10: 1106. https://doi.org/10.3390/pathogens11101106
APA Stylede Menezes, S. A. F., Miranda, Y. M. S., da Silva, Y. M., Carvalho, T. R. B., Alves, F. R. S., Silvestre, R. V. D., Oliveira-Filho, A. B., de Alencar Menezes, T. O., de Souza Fonseca, R. R., Laurentino, R. V., & Machado, L. F. A. (2022). Prevalence and Genotyping of HPV in Oral Squamous Cell Carcinoma in Northern Brazil. Pathogens, 11(10), 1106. https://doi.org/10.3390/pathogens11101106






