A Case of Plasmodium malariae in Bangladesh: A Representation of the Suboptimal Performance of Rapid Diagnostic Approaches in Malaria Elimination Settings
Abstract
1. Introduction
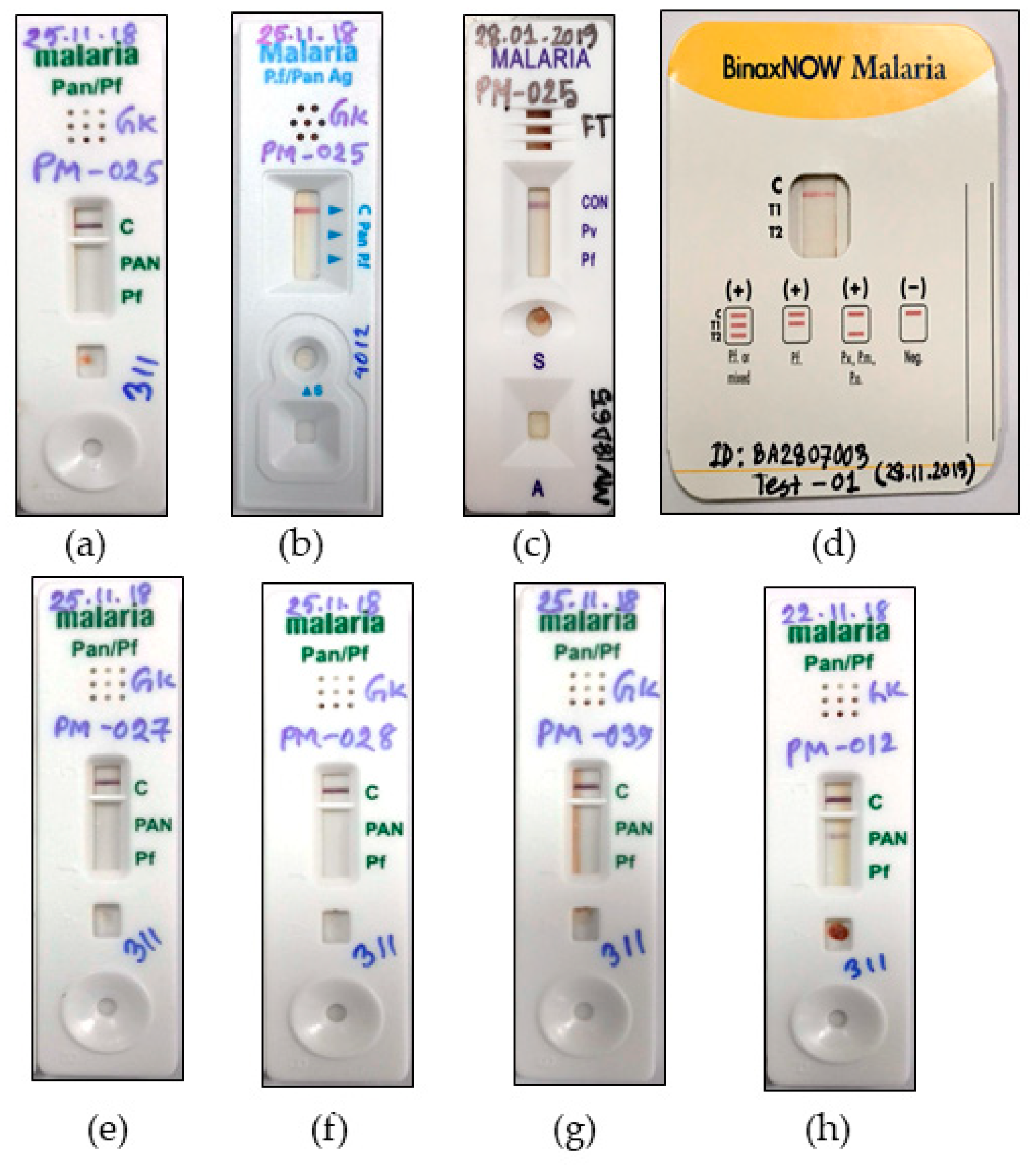
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fuehrer, H.P.; Campino, S.; Sutherland, C.J. The primate malaria parasites Plasmodium malariae, Plasmodium brasilianum and Plasmodium ovale spp.: Genomic insights into distribution, dispersal and host transitions. Malar. J. 2022, 21, 138. [Google Scholar] [CrossRef] [PubMed]
- Rahman, W.; Chotivanich, K.; Silamut, K.; Tanomsing, N.; Hossain, A.; Faiz, M.A.; Dondorp, A.M.; Maude, R.J. Plasmodium malariae in Bangladesh. Trans. R. Soc. Trop. Med. Hyg. 2010, 104, 78–80. [Google Scholar] [CrossRef][Green Version]
- Fuehrer, H.P.; Swoboda, P.; Harl, J.; Starzengruber, P.; Habler, V.E.; Bloeschl, I.; Haque, R.; Matt, J.; Khan, W.A.; Noedl, H. High prevalence and genetic diversity of Plasmodium malariae and no evidence of Plasmodium knowlesi in Bangladesh. Parasitol. Res. 2014, 113, 1537–1543. [Google Scholar] [CrossRef] [PubMed]
- Swoboda, P.; Fuehrer, H.P.; Ley, B.; Starzengruber, P.; Ley-Thriemer, K.; Jung, M.; Matt, J.; Fally, M.A.; Mueller, M.K.; Reismann, J.A.; et al. Evidence of a major reservoir of non-malarial febrile diseases in malaria-endemic regions of Bangladesh. Am. J. Trop. Med. Hyg. 2014, 90, 377–382. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Starzengruber, P.; Fuehrer, H.P.; Ley, B.; Thriemer, K.; Swoboda, P.; Habler, V.E.; Jung, M.; Graninger, W.; Khan, W.A.; Haque, R.; et al. High prevalence of asymptomatic malaria in south-eastern Bangladesh. Malar. J. 2014, 13, 16. [Google Scholar] [CrossRef] [PubMed]
- Vinetz, J.M.; Li, J.; McCutchan, T.F.; Kaslow, D.C. Plasmodium malariae infection in an asymptomatic 74-year-old Greek woman with splenomegaly. N. Engl. J. Med. 1998, 338, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Gilles, H.M.; Hendrickse, R.G. Nephrosis in Nigerian children. Role of Plasmodium malariae, and effect of antimalarial treatment. Br. Med. J. 1963, 2, 27–31. [Google Scholar] [CrossRef]
- Mueller, I.; Zimmerman, P.A.; Reeder, J.C. Plasmodium malariae and Plasmodium ovale—The “bashful” malaria parasites. Trends Parasitol. 2007, 23, 278–283. [Google Scholar] [CrossRef]
- Betson, M.; Sousa-Figueiredo, J.C.; Atuhaire, A.; Arinaitwe, M.; Adriko, M.; Mwesigwa, G.; Nabonge, J.; Kabatereine, N.B.; Sutherland, C.J.; Stothard, J.R. Detection of persistent Plasmodium spp. infections in Ugandan children after artemether-lumefantrine treatment. Parasitology 2014, 141, 1880–1890. [Google Scholar] [CrossRef]
- Dinko, B.; Oguike, M.C.; Larbi, J.A.; Bousema, T.; Sutherland, C.J. Persistent detection of Plasmodium falciparum, P. malariae, P. ovale curtisi and P. ovale wallikeri after ACT treatment of asymptomatic Ghanaian school-children. Int. J. Parasitol. Drugs Drug Resist. 2013, 3, 45–50. [Google Scholar] [CrossRef]
- Wongsrichanalai, C.; Barcus, M.J.; Muth, S.; Sutamihardja, A.; Wernsdorfer, W.H. A review of malaria diagnostic tools: Microscopy and rapid diagnostic test (RDT). Am. J. Trop. Med. Hyg. 2007, 77, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Mukkala, A.N.; Kwan, J.; Lau, R.; Harris, D.; Kain, D.; Boggild, A.K. An Update on Malaria Rapid Diagnostic Tests. Curr. Infect. Dis. Rep. 2018, 20, 49. [Google Scholar] [CrossRef] [PubMed]
- Ong, C.W.; Lee, S.Y.; Koh, W.H.; Ooi, E.E.; Tambyah, P.A. Monkey malaria in humans: A diagnostic dilemma with conflicting laboratory data. Am. J. Trop. Med. Hyg. 2009, 80, 927–928. [Google Scholar] [CrossRef] [PubMed]
- Directorate General of Health Services. Revised Malaria Treatment Regimen-2017; Directorate General of Health Services: Dhaka, Bangladesh, 2017.
- Snounou, G.; Viriyakosol, S.; Zhu, X.P.; Jarra, W.; Pinheiro, L.; do Rosario, V.E.; Thaithong, S.; Brown, K.N. High sensitivity of detection of human malaria parasites by the use of nested polymerase chain reaction. Mol. Biochem. Parasitol. 1993, 61, 315–320. [Google Scholar] [CrossRef]
- Talman, A.M.; Duval, L.; Legrand, E.; Hubert, V.; Yen, S.; Bell, D.; Le Bras, J.; Ariey, F.; Houze, S. Evaluation of the intra- and inter-specific genetic variability of Plasmodium lactate dehydrogenase. Malar. J. 2007, 6, 140. [Google Scholar] [CrossRef] [PubMed]
- Moody, A. Rapid diagnostic tests for malaria parasites. Clin. Microbiol. Rev. 2002, 15, 66–78. [Google Scholar] [CrossRef] [PubMed]
- Xia, J.; Fan, L.; Si, L.; Lu, Q.; Zhao, Y.; Zhang, M.; Xu, Y.; Wang, B. A Case Report of Serological Rapid Diagnostic Test-Negative Plasmodium malariae Malaria Imported from West Africa. Clin. Lab. 2021, 67, 10. [Google Scholar] [CrossRef]
- Yerlikaya, S.; Campillo, A.; Gonzalez, I.J. A Systematic Review: Performance of Rapid Diagnostic Tests for the Detection of Plasmodium knowlesi, Plasmodium malariae, and Plasmodium ovale Monoinfections in Human Blood. J. Infect. Dis. 2018, 218, 265–276. [Google Scholar] [CrossRef]
- Richter, J.; Göbels, K.; Müller-Stöver, I.; Hoppenheit, B.; Häussinger, D. Co-reactivity of plasmodial histidine-rich protein 2 and aldolase on a combined immuno-chromographic-malaria dipstick (ICT) as a potential semi-quantitative marker of high Plasmodium falciparum parasitaemia. Parasitol. Res. 2004, 94, 384–385. [Google Scholar] [CrossRef]
- Moody, A.H.; Chiodini, P.L. Non-microscopic method for malaria diagnosis using OptiMAL IT, a second-generation dipstick for malaria pLDH antigen detection. Br. J. Biomed. Sci. 2002, 59, 228–231. [Google Scholar] [CrossRef]
- Zhang, S.X.; Kronmann, K.C.; Kavanaugh, M.J. Plasmodium malariae-Repeat Light Microscopy when Molecular Testing is Not Available. Am. J. Trop. Med. Hyg. 2019, 100, 233–234. [Google Scholar] [CrossRef] [PubMed]
- Niño, C.H.; Cubides, J.R.; Camargo-Ayala, P.A.; Rodríguez-Celis, C.A.; Quiñones, T.; Cortés-Castillo, M.T.; Sánchez-Suárez, L.; Sánchez, R.; Patarroyo, M.E.; Patarroyo, M.A. Plasmodium malariae in the Colombian Amazon region: You don’t diagnose what you don’t suspect. Malar. J. 2016, 15, 576. [Google Scholar] [CrossRef] [PubMed]
- Dyer, M.E.; Tjitra, E.; Currie, B.J.; Anstey, N.M. Failure of the ‘pan-malarial’ antibody of the ICT Malaria P.f/P.v immunochromatographic test to detect symptomatic Plasmodium malariae infection. Trans. R. Soc. Trop. Med. Hyg. 2000, 94, 518. [Google Scholar] [CrossRef]
- Deng, Y.; Zhou, R.M.; Zhang, H.W.; Qian, D.; Liu, Y.; Chen, W.Q.; Zhao, X.D. Diagnosis and treatment for three imported Plasmodium malariae malaria cases in Henan Province. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 2014, 32, 61–63. [Google Scholar]
- Kosack, C.S.; Naing, W.T.; Piriou, E.; Shanks, L. Routine parallel diagnosis of malaria using microscopy and the malaria rapid diagnostic test SD 05FK60: The experience of Médecins Sans Frontières in Myanmar. Malar. J. 2013, 12, 167. [Google Scholar] [CrossRef]
- Moody, A.; Hunt-Cooke, A.; Gabbett, E.; Chiodini, P. Performance of the OptiMAL malaria antigen capture dipstick for malaria diagnosis and treatment monitoring at the Hospital for Tropical Diseases, London. Br. J. Haematol. 2000, 109, 891–894. [Google Scholar] [CrossRef]
- Piper, R.C.; Buchanan, I.; Choi, Y.H.; Makler, M.T. Opportunities for improving pLDH-based malaria diagnostic tests. Malar J. 2011, 10, 213. [Google Scholar] [CrossRef]
- Elizardez, Y.B.; Fotoran, W.L.; Junior, A.J.G.; Curado, I.; Junior, N.K.; Monteiro, E.F.; Romero Neto, I.; Wunderlich, G.; Kirchgatter, K. Recombinant proteins of Plasmodium malariae merozoite surface protein 1 (PmMSP1): Testing immunogenicity in the BALB/c model and potential use as diagnostic tool. PLoS ONE 2019, 14, e0219629. [Google Scholar] [CrossRef] [PubMed]
- Woodford, J.; Collins, K.A.; Odedra, A.; Wang, C.; Jang, I.K.; Domingo, G.J.; Watts, R.; Marquart, L.; Berriman, M.; Otto, T.D.; et al. An Experimental Human Blood-Stage Model for Studying Plasmodium malariae Infection. J. Infect. Dis. 2020, 221, 948–955. [Google Scholar] [CrossRef]
- Paul, R.; Sinha, P.K.; Bhattacharya, R.; Banerjee, A.K.; Raychaudhuri, P.; Mondal, J. Study of C reactive protein as a prognostic marker in malaria from Eastern India. Adv. Biomed. Res. 2012, 1, 41. [Google Scholar] [CrossRef]
- Ho, M.-F.; Baker, J.; Lee, N.; Luchavez, J.; Ariey, F.; Nhem, S.; Oyibo, W.; Bell, D.; González, I.; Chiodini, P.; et al. Circulating antibodies against Plasmodium falciparum histidine-rich proteins 2 interfere with antigen detection by rapid diagnostic tests. Malar. J. 2014, 13, 480. [Google Scholar] [CrossRef] [PubMed]
- Collins, W.E.; Jeffery, G.M. Plasmodium malariae: Parasite and disease. Clin. Microbiol. Rev. 2007, 20, 579–592. [Google Scholar] [CrossRef] [PubMed]
- Lover, A.A.; Baird, J.K.; Gosling, R.; Price, R.N. Malaria Elimination: Time to Target All Species. Am. J. Trop. Med. Hyg. 2018, 99, 17–23. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Johora, F.T.; Kibria, M.G.; Fuehrer, H.-P.; Alam, M.S. A Case of Plasmodium malariae in Bangladesh: A Representation of the Suboptimal Performance of Rapid Diagnostic Approaches in Malaria Elimination Settings. Pathogens 2022, 11, 1072. https://doi.org/10.3390/pathogens11101072
Johora FT, Kibria MG, Fuehrer H-P, Alam MS. A Case of Plasmodium malariae in Bangladesh: A Representation of the Suboptimal Performance of Rapid Diagnostic Approaches in Malaria Elimination Settings. Pathogens. 2022; 11(10):1072. https://doi.org/10.3390/pathogens11101072
Chicago/Turabian StyleJohora, Fatema Tuj, Mohammad Golam Kibria, Hans-Peter Fuehrer, and Mohammad Shafiul Alam. 2022. "A Case of Plasmodium malariae in Bangladesh: A Representation of the Suboptimal Performance of Rapid Diagnostic Approaches in Malaria Elimination Settings" Pathogens 11, no. 10: 1072. https://doi.org/10.3390/pathogens11101072
APA StyleJohora, F. T., Kibria, M. G., Fuehrer, H.-P., & Alam, M. S. (2022). A Case of Plasmodium malariae in Bangladesh: A Representation of the Suboptimal Performance of Rapid Diagnostic Approaches in Malaria Elimination Settings. Pathogens, 11(10), 1072. https://doi.org/10.3390/pathogens11101072







