Abstract
The microbiota of the gastrointestinal tract of humans and animals is inhabited by a diverse community of bacteria, fungi, protozoa, and viruses. In cases where there is an imbalance in the normal microflora or an immunosuppression on the part of the host, these opportunistic microorganisms can cause severe infections. The study presented here evaluates the biochemical and antifungal susceptibility features of Trichosporon spp., uncommon non-Candida strains isolated from the gastrointestinal tract of healthy turkeys. The Trichosporon coremiiforme and Trichosporon (Apiotrichum) montevideense accounted for 7.7% of all fungi isolates. The biochemical tests showed that Trichosporon coremiiforme had active esterase (C4), esterase-lipase (C8) valine arylamidase, naphthol-AS-BI phosphohydrolase, α-galactosidase, and β-glucosidase. Likewise, Trichosporon montevideense demonstrated esterase-lipase (C8), lipase (C14), valine arylamidase, naphthol-AS-BI phosphohydrolase, α-galactosidase, and β-glucosidase activity. T.coremiiforme and T. monteviidense isolated from turkeys were itraconazole resistant and amphotericin B, fluconazole, and voriconazole susceptible. Compared with human isolates, the MIC range and MIC values of turkey isolates to itraconazole were in a higher range limit in both species, while MIC values to amphotericin B, fluconazole, and voriconazole were in a lower range limit. Furthermore, the obtained ITS1—5.8rRNA—ITS2 fragment sequences were identical with T. coremiiforme and T. montevideense sequences isolated from humans indicating that these isolates are shared pathogens.
1. Introduction
The microbiota of the gastrointestinal tract of poultry consists of a diverse collection of bacteria, fungi, protozoa, and viruses which are natural occupants in healthy birds [1]. In cases where there were changes to the host’s immune system, such as an imbalance in the normal microflora, the integrity of the mucocutaneous barrier, a failure to mount a proper immune response or an immunocompromised condition brought on by stress, the opportunistic organisms can cause severe infections [2,3,4].
This is often observed when the microbiota balance is disturbed after an antimicrobial treatment and fungal development is thereby facilitated. Fungal infections in birds should be monitored not only to safeguard poultry health and production, but also in order to protect human health since birds are a reservoir of harmful fungi such as dermatophytes and yeast, which has been confirmed by many research studies [5,6,7].
The best described potential avian sources of pathogenic yeasts are pigeon droppings in which genera Candida, Cryptococcus, Rhodotorula, Saccharomyces, Trichosporon were commonly identified [8,9,10]. Among birds kept as pets, parrots might be a source of fungi, mainly Candida species which could be hazardous to human health, especially to immuno-compromised individuals, children, and the elderly. The most prevalent species were Candida albicans, C. tropicalis, C. krusei and among non-Candida species Trichosporon asteroides was noted [5,11].
Due to the increased reports of uncommon yeast infections in humans and the antifungal resistance of isolates [12,13,14,15,16], the present study was undertaken to characterize the non-Candida fungi isolates from healthy turkeys according to the biochemical and antifungal features of the strains.
2. Materials and Methods
2.1. Animals and Mycological Investigation
Fungi isolates were taken from 6-week-old British United Turkey (BUT) Big 6 turkeys from 7 flocks—10 birds from each flock reared in Poland [17]. During the rearing period, the birds were monitored for gastrointestinal disorders, and no cases of clinical mycosis were found in the gastrointestinal tract. Additionally, the birds had not been treated with antimicrobials. Swabs (BioMaxima, Lubelskie, Poland) were taken from the beak cavity, crop, and cloaca and cultured on Sabouraud glucose agar with chloramphenicol (Emapol, Warsaw, Poland). Then, they were incubated at 37 °C for 48 h. The negative control was unopened plates taken from batches used for the swab culture. Using classical mycological diagnostic methods, microbiological cultures and microscopic examination, the strains were isolated and identified. Identification of the genera of the fungi was based on the morphological characteristics of the isolates and their growth on CHROMagar media (Emapol, Warsaw, Poland) [17].
2.2. Biochemical Analysis of Isolates
The hydrolytic activity of fungi was determined by the API ZYM test (BioMerieux, Marcy-l’Étoile, France) composed of 20 microcupules containing substrates for the evaluation of 19 hydrolytic enzymes: Alkaline phosphatase, esterase, esterase lipase, lipase, leucine arylamidase, valine arylamidase, cystine arylamidase, trypsin, chymotrypsin, acid phosphatase, naphthol-AS-BI phosphohydrolase, α-galactosidase, β-galactosidase, β-glucuronidase, α-glucosidase, β-glucosidase, N-acetyl-β-glucosaminidase, α-mannosidase, and α-fucosidase as well as a control. A suspension of fungus cells was prepared from the 24-h culture with the Sabouraud medium, (density—6° according to the McFarland scale) and placed in the microcupules on the API ZYM strip. The results were read according to the instructions provided by the producer.
2.3. Antifungal Susceptibility Profile
Yeast inoculum suspensions were prepared as described in the Clinical and Laboratory Standards Institute (CLSI) M27-A3 [18,19]. The inoculum suspensions of fungi isolates were prepared in 0.9% saline solution and adjusted to the turbidity of 0.5 McFarland standard with approximately 1–5 × 106 CFU/mL. This suspension was used directly to inoculate agar plates for the E-test (BioMérieux Polska sp. z o.o., Poland). Quality control was ensured by testing the CLSI recommended strain C. parapsilosis ATCC 22019. A purchase was made from BioMérieux Polska sp. z o.o. for E-test strips for amphotericin B (AMB) 0.002–32 μg/mL, itraconazole (ITC) 0.002–32 μg/mL, voriconazole (VOR) 0.002–32 μg/mL, and fluconazole (FLU) 0.016–256 μg/mL). The E-test was carried out according to the manufacturer’s instructions. A RPMI 1640 medium containing 2% glucose (Emapol, Warsaw, Poland) was used for the antifungal susceptibility testing. Each solidified medium was inoculated with a sterile swab dipped into the respective inoculum suspension and then evenly smeared over the surface of the plate. The surface of the agar plate was allowed to dry for 15 min before the E-test strip was placed on it. After drying, the plates were incubated at 35 °C for 48 h. After the plates had been incubated for 24 and 48 h, MICs were read as the lowest drug concentrations at which the border of the ellipse touched the scale on the strip. The final MIC values were based on the consensus between two readers. The minimum inhibitory concentration (MIC) breakpoints are not yet described for Trichosporon spp., so the breakpoints recommended for Candida albicans as per the CLSI M27-A3 for Candida spp. were followed [18,19,20]. The isolate was considered to be susceptible if the MIC value was ≤2 µg/mL for fluconazole, ≤0.125 µg/mL for itraconazole, and ≤0.12 µg/mL for voriconazole. The interpretative criteria for amphotericin B (AMB) were adopted from the literature and the isolates were susceptible if the MIC value was ≤1 µg/mL [20,21,22].
2.4. PCR Amplification, Gene Sequencing, and Phylogenetic Analysis
The DNA was isolated using the Genomic Mini AX Yeast (A&A Biotechnology, Gdynia, Poland) according to the manufacturer’s instructions. The general primers ITS1 (5′-TCCGTAGGTGAACCTGCGG-3′) and ITS4 (5′-TCCTCCGCTTATTGATATGC-3′) were used for the ITS1—5.8rRNA—ITS2 fragment amplification [23]. PCR was carried out in a 25 µL reaction mixture containing 50 ng of DNA in 2 µL, 0.25 µL of forward and reverse primer at a concentration of 25 mM, 12.5 µL of PCR Mix Plus (A&A Biotechnology, Gdynia, Poland), and 10 µL DNAse and RNAse water. Amplification was performed in a Bio-Rad T100 PCR Thermal Cycler.
Following an initial denaturation step at 95 °C for 5 min, the reaction mixtures were subjected to 35 cycles of heat denaturation at 95 °C for 30 s, primer annealing at 55 °C for 1 min, and DNA extension at 72 °C for 2 min. Samples were maintained at 72 °C for 10 min for the final extension step. The PCR products were subjected to electrophoresis in a 1.5% agarose gel stained with CybrGreen (Sigma-Aldrich, Poznan, Poland) and visualized under ultraviolet light. The size of the respective PCR products was determined using a molecular mass marker, DNA Marker 1 (A&A Biotechnology, Gdynia, Poland).
The PCR products were isolated from agarose gel using a Gel Out Concentrator Kit (A&A Biotechnology, Gdynia, Poland) and were subsequently sent to Macrogen (Amsterdam, The Netherlands) for Sanger sequencing with the above-mentioned PCR primers (Genomed, Warsaw, Poland). The sequences were analyzed using the Mega 6 software, then compared to sequences from the National Center for Biotechnology Information (NCBI) GenBank database. The sequences were analyzed in comparison with genes sequences of human Trichosporon isolates. Moreover, the phylogenetic tree was generated using a MEGA6 software by the neighbor-joining method.
3. Results and Discussion
Among the 210 samples taken from healthy turkeys, a total of 26 isolates were identified with the majority (92%) being Candida spp., in which two were identified as Trichosporon spp. (8%) [17]. Moreover, Trichosporon was isolated by other researchers from the intestinal tract of Gallus gallus—chickens and hens [6,24,25]. The analysis of metagenomic sequences available in the public bases showed that in poultry the intestinal tract predominates bacteria and fungal species comprising less than 0.1% of the microbiota. In most of the samples in which fungi were detected, the taxonomy analysis showed the presence of Ascomycota, to which Saccharomyces and Candida species belong. The predominance of Ascomycota in the chicken gastrointestinal tract was described by Robinsin et al., but in contrast to our own research, the Basidiomycota with Trichosporon represented 11.7 to 26.8% of the total fungal population [25], while in turkeys it was 8%. In this study, the obtained data from turkey flocks showed a low frequency of Trichosporon occurrence, which is lower than in chickens, probably due to the birds species and age. In young chickens, Trichosporon was a predominant genus [25], when in older hens the percent of isolates ranged between 0.5 and 10% [6,24], which was similar in turkeys. The PCR amplification of a ITS1-5.8rRNA-ITS2 fragment and sequencing of turkey isolates confirmed growth of the pre-identified Trichosporon coremiiforme (MF992258) and Trichosporon (Apiotrichum) montevideense (MF992256). Compared to chickens from which T. moniliiforme and T. asahii were isolated, the Trichosporon species found in turkeys are more comparable with hens and pigeons where Trichosporon coremiiforme was also isolated [6,10,25]. Trichosporon (Apiotrichum) montevideense was not detected in any other poultry species.
In an attempt to create a phylogenetic relationship of turkey isolates by neighbor-joining, the BLAST programme on the National Center for Biotechnology Information GenBank database was used with Trichosporon species isolated from humans. The analysis showed that the obtained turkey sequences were identical with other Trichosporon coremiiforme and Trichosporon (Apiotrichum) montevideense sequences (Figure 1), of human origin. The ITS regions are recommended as the universal fungal barcode within the species, which may identify the geographic and hosts. The presence of mutations in those regions was able to evaluate the genetic distance between the isolates [26].
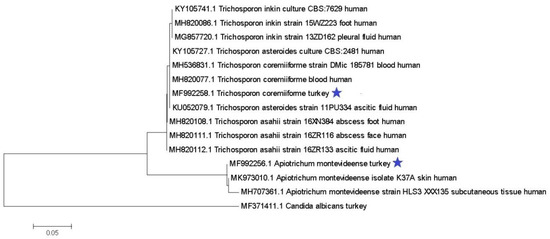
Figure 1.
Neighbor-joining tree based on the ITS1-5.8S-ITS2 region. The turkey isolates are marked with an asterisk.
Biochemical tests showed that Trichosporon coremiiforme demonstrated the activity of esterase (C4), esterase-lipase (C8) valine arylamidase, naphthol-AS-BI phosphohydrolase, α-galactosidase, and β-glucosidase. Trichosporon montevideense showed the activity of esterase-lipase (C8), lipase (C14), valine arylamidase, naphthol-AS-BI phosphohydrolase, α-galactosidase, and β-glucosidase activity. It is the first biochemical characterization of non-Candida strains isolated from turkeys.
The enzymatic activity of T. coremiiforme and T. montevideense makes it possible to hydrolase many structures of the cell wall such as esters, lipids, glycolipids, glycoproteins, and oligosaccharides, as well as penetrating the host cell membranes. Features which are under normal conditions beneficial to the host, for example, when fungi in the gastrointestinal tract help digest cellulose, may become dangerous when present in organs and the bloodstream since hemolysins, proteases, and lipases allow for the destabilization of host membranes and the degradation of host connective tissues [27].
For an immunocompromised host aside from enzymatic activity, the resistance of antifungal agents is crucial. If the isolates are resistant to antifungal agents, the infection may be life-threatening for the host. T.coremiiforme and T. monteviidense isolated from turkeys were susceptible to amphotericin, fluconazole, and voriconazole. Among the triazole derivatives, itraconazole was the least active antifungal agent (Table 1), with both isolates being resistant.

Table 1.
Antifungal susceptibilities of Trichosporon isolates after 48 h of incubation compared to human isolates.
Compared to human isolates, the MIC range (0.125–2 and 0.12–1 μg/mL) and MIC values of turkey isolates to itraconazole were in a higher range limit in both species (1.5 and 1 μg/mL). In contrast to itraconazole, the MIC values of Trichosporon isolated from turkeys to amphotericin B, fluconazole, and voriconazole were in a lower range limit. Previously, these non-Candida strains of antimicrobial resistance had only been observed in wild birds. Isolates from bird feces were tested for antifungal resistance using a commercial kit that covered 11 frequently employed agents, 144 Candida, Cryptococcus, Rhodotorula, and Trichosporon. It was reported that 45.8% of the strains were resistant to at least four of the 11 drugs, and 18.1% were resistant to all the antifungals tested [32].
In recent years, interest in the human microbiome has increased, and Trichosporon has been recognized as a part of it, but also as an emergent pathogen causing invasive and life-threatening fungal infections [33,34]. Most Trichosporon species reside harmlessly as commensals on the skin and in the gastrointestinal tract of healthy individuals and are classic opportunistic pathogens, where they are kept under the watchful eye of the immune system and through interactions with the resident microbiome [27].
Among the most frequently isolated Trichosporon species in humans, T. asahii, T.asteroides, and T. inkin were noted [16,30], while T. coremiiforme and T. montevideense were rarely isolated. Those two species, isolated from turkeys, were not predominant in human infections. However, more biochemical properties and antimicrobial susceptibility data are needed. To the best of our knowledge, this is the first study characterizing the Trichosporon spp. isolated from the turkey intestinal tract.
4. Conclusions
The Trichosporon species are rarely isolated from the intestinal tract of healthy turkeys. There is no genetic diversity in ITS1-5.8rRNA-ITS2 fragments of T.coremiiforme and T. monteviidense between the turkey and human strains, but turkey isolates in contrast to human strains are more resistant to itraconazole.
Author Contributions
Conceptualization, K.B., I.S., A.G., methodology and sampling, K.B. and I.S.; writing—original draft preparation, K.B.; writing—review and editing, K.B.; supervision, A.G. and I.S. All authors have read and agreed to the published version of the manuscript.
Funding
The publication is financed under the Leading Research Groups support project from the subsidy increased for the period 2020–2025 in the amount of 2% of the subsidy referred to Art. 387(3) of the Law of 20 July 2018 on Higher Education and Science, obtained in 2019.
Institutional Review Board Statement
The ethical review and approval were waived for this study, since taking cloacal swabs and fecal samples are standard veterinary procedures, which are not subject to the local ethical committee for animal experiment assessment.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Yegani, M.; Korver, D. Factors affecting intestinal health in poultry. Poult. Sci. 2008, 87, 2052–2063. [Google Scholar] [CrossRef] [PubMed]
- Colombo, A.L.; Padovan, A.C.; Chaves, G.M. Current knowledge of Trichosporon spp. and Trichosporonosis. Clin. Microbiol. Rev. 2011, 24, 682–700. [Google Scholar] [CrossRef]
- Arabatzis, M.; Abel, P.; Kanellopoulou, M.; Adamou, D.; Alexandrou-Athanasoulis, H.; Stathi, A.; Platsouka, A.; Milioni, A.; Pangalis, A.; Velegraki, A. Sequence-based identification, genotyping and EUCAST antifungal susceptibilities of Trichosporon clinical isolates from Greece. Clin. Microbiol. Infect. 2014, 20, 777–783. [Google Scholar] [CrossRef] [PubMed]
- Taei, M.; Chadeganipour1, M.; Mohammadi1, R. An alarming rise of non-albicans Candida species and uncommon yeasts in the clinical samples; a combination of various molecular techniques for identification of etiologic agents. BMC Res. Notes 2019, 12, 779. [Google Scholar] [CrossRef] [PubMed]
- Brilhante, R.S.N.; Castelo-Branco, D.S.C.M.; Soares, G.D.P.; Astete-Medrano, D.J.; Monteiro, A.J.; Cordeiro, R.A.; Sidrim, J.J.C.; Rocha, M.F.G. Characterization of the gastrointestinal yeast microbiota of cockatiels (Nymphicus hollandicus): A potential hazard to human health. J. Med. Microbiol. 2010, 59 Pt 6, 718–723. [Google Scholar] [CrossRef]
- Subramanya, S.H.; Sharan, N.K.; Baral, B.P.; Hamal, D.; Nayak, N.; Prakash, P.Y.; Sathian, B.; Bairy, I.; Gokhale, S. Diversity, in-vitro virulence traits and antifungal susceptibility pattern of gastrointestinal yeast flora of healthy poultry, Gallus gallus domesticus. BMC Microbiol. 2017, 17, 113. [Google Scholar] [CrossRef] [PubMed]
- Quandt, S.; Schultz, M.; Feldman, S.; Vallejos, Q.; Marin, A.; Carrillo, L.; Arcury, T. Dermatological illness of immigrant poultry processing workers in North Carolina. Arch. Environ. Occup. Health 2005, 60, 165–169. [Google Scholar] [CrossRef][Green Version]
- Costa, A.K.F.; Sidrim, J.J.C.; Cordeiro, R.A.; Brilhante, R.S.N.; Monteiro, A.J.; Rocha, M.F. Urban pigeons (Columba livia) as a potential source of pathogenic yeasts: A focus on antifungal susceptibility of Cryptococcusstrains in Northeast Brazil. Mycopathologia 2010, 169, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Rosario Medina, I.; Román Fuentes, L.; Batista Arteaga, M.; Real Valcárcel, F.; Acosta Arbelo, F.; Padilla Del Castillo, D.; Déniz Suárez, S.; Ferrer Quintana, O.; Vega Gutiérrez, B.; Silva Sergent, F.; et al. Pigeons and their droppings as reservoirs of Candida and other zoonotic yeasts. Rev. Iberoam. Micol. 2017, 34, 211–214. [Google Scholar] [CrossRef]
- Pakshir, K.; Zareshahrabadi, Z.; Zomorodian, K.; Ansari, S.; Nouraei, H.; Gharavi, A. Molecular identification of non-Cryptococcus yeasts associated with pigeon droppings in Shiraz, Southern Iran. Iran J. Vet. Res. 2019, 20, 204–208. [Google Scholar]
- Simi, W.B.; Leite, D.P., Jr.; Paula, C.R.; Hoffmann-Santos, H.D.; Takahara, D.T.; Hahn, R.C. Yeasts and filamentous fungi in psittacidae and birds of prey droppings in midwest region of Brazil: A potential hazard to human health. Braz. J. Biol. 2019, 79, 414–422. [Google Scholar] [CrossRef] [PubMed]
- Chagas-Neto, T.; Guilherme, M.; Chaves, S.; Melo, A.; Colombo, A. Bloodstream Infections Due to Trichosporon spp.: Species Distribution, Trichosporon asahii Genotypes Determined on the Basis of Ribosomal DNA Intergenic Spacer 1 Sequencing, and Antifungal Susceptibility Testing. J. Clin. Microbiol. 2009, 1, 1074–1081. [Google Scholar] [CrossRef] [PubMed]
- Do Espirito Santo, E.T.; Monteiro, R.C.; da Costa, A.; Marques da Silva, S.H. Molecular identification, genotyping, phenotyping and antifungal susceptibilities of medically important Trichosporon, Apiotrichum and Cutaneotrichosporon species. Mycopathologia 2020, 185, 307–317. [Google Scholar] [CrossRef] [PubMed]
- Montagna, M.T.; Lovero, G.; Coretti, C.; De Giglio, O.; Martinelli, D.; Bedini, A. In vitro activities of amphotericin B deoxycholate and liposomal amphotericin B against 604 clinical yeast isolates. J. Med. Microbiol. 2014, 63, 1638–1643. [Google Scholar] [CrossRef]
- Guo, L.N.; Yu, S.Y.; Hsueh, P.R.; Al-Hatmi, A.M.; Meis, J.F.; Hagen, F.; Xiao, M.; Wang, H.; Barresi, C.; Zhou, M.L.; et al. Invasive infections due to Trichosporon: Species distribution, genotyping, and antifungal susceptibilities from a multicenter study in China. J. Clin. Microbiol. 2019, 57, e01505-18. [Google Scholar] [CrossRef]
- Francisco, E.C.; de Almeida Junior, J.N.; de Queiroz Telles, F.; Aquino, V.R.; Mendes, A.V.A.; de Andrade Barberino, M.G.; de Tarso, O.; Castro, P.; Guimarães, T.; Hahn, R.C. Species distribution and antifungal susceptibility of 358 Trichosporon clinical isolates collected in 24 medical centres. Clin. Microbiol. Infect. 2019, 25, e1–e909. [Google Scholar] [CrossRef] [PubMed]
- Sokół, I.; Gaweł, A.; Bobrek, K. The Prevalence of Yeast and Characteristics of the Isolates from the Digestive Tract of Clinically Healthy Turkeys. Avian Dis. 2018, 62, 286–290. [Google Scholar] [CrossRef]
- Rex, J.; Alexander, B.; Andres, D.; Arthinton-Skaggs, B.; Brown, S.; Chaurvedi, V.; Ghannoum, M.; Espinel-Ingroff, A.; Knapp, C.; Ostrosky-Zeichner, L.; et al. Clinical and Laboratory Standards Institute: M27-A3 Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts; Approved Standard—Third Edition; CLSI: Wayne, NJ, USA, 2008. [Google Scholar]
- Procop, G.; Dufresne, P.; Berkow, E.; Fuller, J.; Hanson, K.; Holliday, N.; Pincus, D.; Schuetz, A.; Verweij, P.; Wiederhold, N.; et al. Clinical and Laboratory Standards Institute:M60-ED 1: Performance Standards for Antifungal Susceptibility Testing of Yeasts; CLSI: Wayne, NJ, USA, 2017. [Google Scholar]
- Dabas, Y.; Xess, I.; Kale, P. Molecular and antifungal susceptibility study on trichosporonemia and emergence of Trichosporon mycotoxinivorans as a bloodstream pathogen. Med. Mycol. 2017, 55, 518–527. [Google Scholar]
- Negri, M.; Henriques, M.; Svidzinski, T.I.; Paula, C.R.; Oliveira, R. Correlation between Etest, disk diffusion, and microdilution methods for antifungal susceptibility testing of Candida species from infection and colonization. J. Clin. Lab. Anal. 2009, 23, 324–330. [Google Scholar] [CrossRef]
- Song, Y.B.; Suh, M.K.; Ha, G.Y.; Kim, H. Antifungal Susceptibility Testing with Etest for Candida Species Isolated from Patients with Oral Candidiasis. Ann. Dermatol. 2015, 27, 715–720. [Google Scholar] [CrossRef]
- White, T.J.; Bruns, T.; Lee, S.; Taylor, L. Amplification and direct sequencing of fungal ribosomal RNA genes for phylogenetics. In PCR Protocols: A Guide to Methods and Applications; Innis, M.A., Gelfand, D.H., Sninsky, J.J., White, T.J., Eds.; Academic Press, Inc.: New York, NY, USA, 1990; pp. 315–322. [Google Scholar]
- Cafarchia, C.; Iatta, R.; Danesi, P.; Camarda, A.; Capelli, G.; Otranto, D. Yeasts isolated from cloacal swabs, feces, and eggs of laying hens. Med. Mycol. 2019, 57, 340–345. [Google Scholar] [CrossRef]
- Robinson, K.; Xiao, Y.; Johnson, T.; Chen, B.; Yang, Q.; Lyu, W.; Wang, J.; Fansler, N.; Becker, S.; Liu, J.; et al. Chicken Intestinal Mycobiome: Initial Characterization and Its Response to Bacitracin Methylene Disalicylate. Appl. Environ. Microbiol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Schoch, C.L.; Seifert, K.A.; Huhndorf, S.; Robert, V.; Spouge, J.L.; Levesque, C.A.; Chen, W.; Bolchacova, E.; Voigt, K.; Crous, P.W. Nuclear Ribosomal Internal Transcribed Spacer (ITS) Region as a Universal DNA Barcode Marker for Fungi. Proc. Natl. Acad. Sci. USA 2012, 109, 6241–6246. [Google Scholar] [CrossRef] [PubMed]
- Duarte-Oliveira, C.; Rodrigues, F.; Gonçalves, S.M.; Goldman, G.H.; Carvalho, A.; Cunha, C. The Cell Biology of the Trichosporon-Host Interaction. Front. Cell Infect. Microbiol. 2017, 7, 118. [Google Scholar] [CrossRef] [PubMed]
- Lemes, R.M.; Lyon, J.P.; Moreira, L.M.; de Resende, M.A. Antifungal susceptibility profile of Trichosporon isolates: Correlation between CLSI and etest methodologies. Braz. J. Microbiol. 2010, 41, 310–315. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rodriguez-Tudela, J.L.; Diaz-Guerra, T.M.; Mellado, E.; Cano, V.; Tapia, C.; Perkins, A.; Gomez-Lopez, A.; Rodero, L.; Cuenca-Estrella, M. Susceptibility patterns and molecular identification of Trichosporon species. Antimicrob. Agents Chemother. 2005, 49, 4026–4034. [Google Scholar] [CrossRef] [PubMed]
- Iturrieta-Gonzalez, I.A.; Padovan, A.C.; Bizerra, F.C.; Hahn, R.C.; Colombo, A.L. Multiple Species of Trichosporon Produce Biofilms Highly Resistant to Triazoles and Amphotericin, B. PLoS ONE 2014, 9, e109553. [Google Scholar] [CrossRef] [PubMed]
- Taverna, C.G.; Córdoba, S.; Murisengo, O.A.; Vivot, W.; Davel, G.; Bosco-Borgeat, M.E. Molecular identification, genotyping, and antifungal susceptibility testing of clinically relevant Trichosporon species from Argentina. Med. Mycol. 2014, 52, 356–366. [Google Scholar] [CrossRef]
- Lord, A.T.; Mohandas, K.; Somanath, S. Multidrug resistant yeasts in synanthropic wild birds. Ann. Clin. Microbiol. Antimicrob. 2010, 9, 11. [Google Scholar] [CrossRef]
- Hoggard, M.; Vesty, A.; Wong, G.; Montgomery, J.M.; Fourie, C.; Douglas, R.G. Characterizing the Human Mycobiota: A Comparison of Small Subunit rRNA, ITS1, ITS2, and Large Subunit rRNA Genomic Targets. Front. Microbiol. 2018, 9, 2208. [Google Scholar] [CrossRef]
- Ruszkowski, J.; Kaźmierczak-Siedlecka, K.; Witkowski, J.; Dębska-Ślizień, A. Mycobiota of the human gastrointestinal tract. Postepy Hig. Med. Dosw. 2020, 74, 301–313. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).