Racial/Ethnic Residential Segregation, the Distribution of Physician’s Offices and Access to Health Care: The Case of Houston, Texas
Abstract
1. Introduction
2. Literature Review and Theoretical Framework
2.1. Segregation and the Link to Health Care
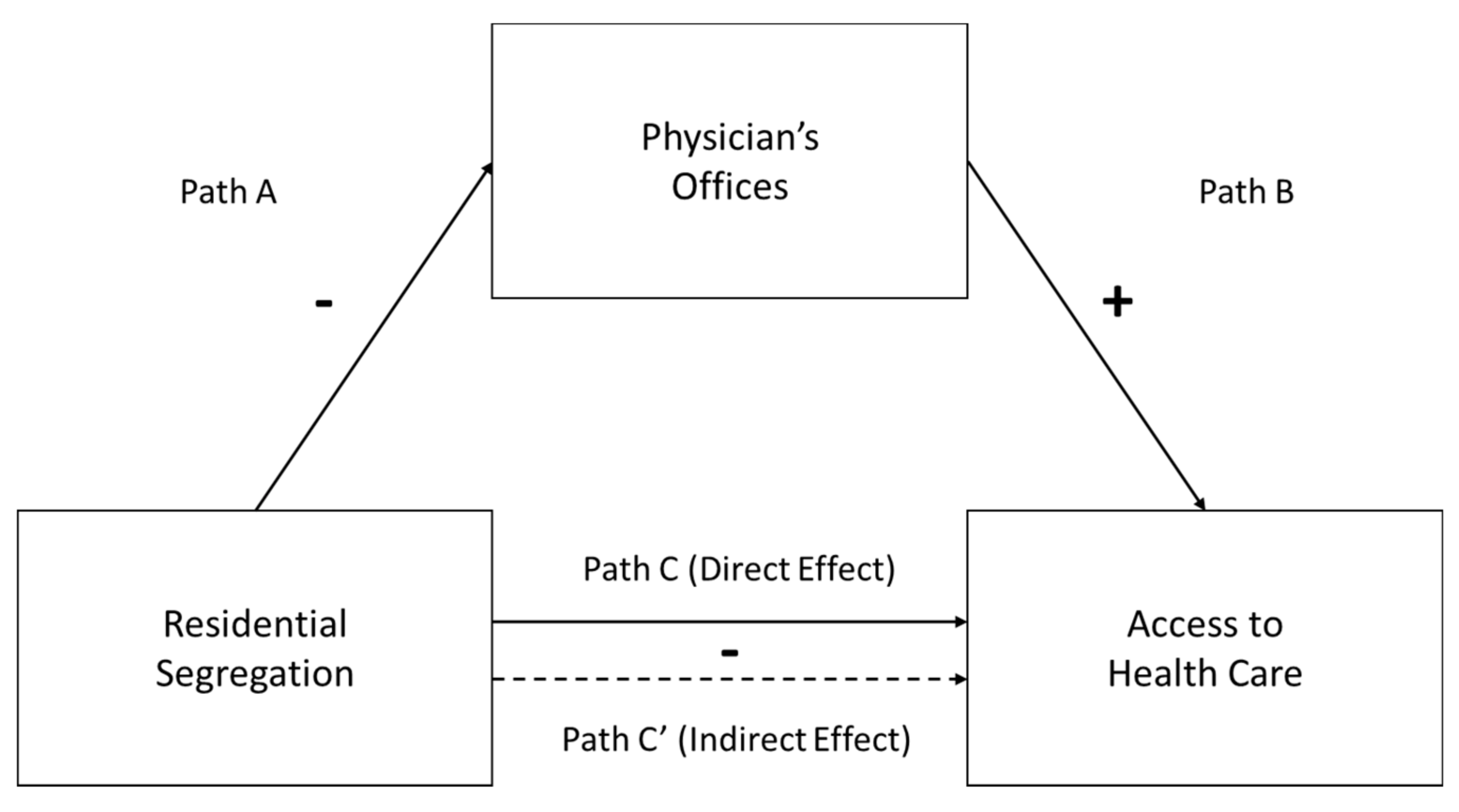
2.2. Conceptual Framework and Hypotheses
3. Data and Methods
3.1. Data
3.2. Dependent Variables
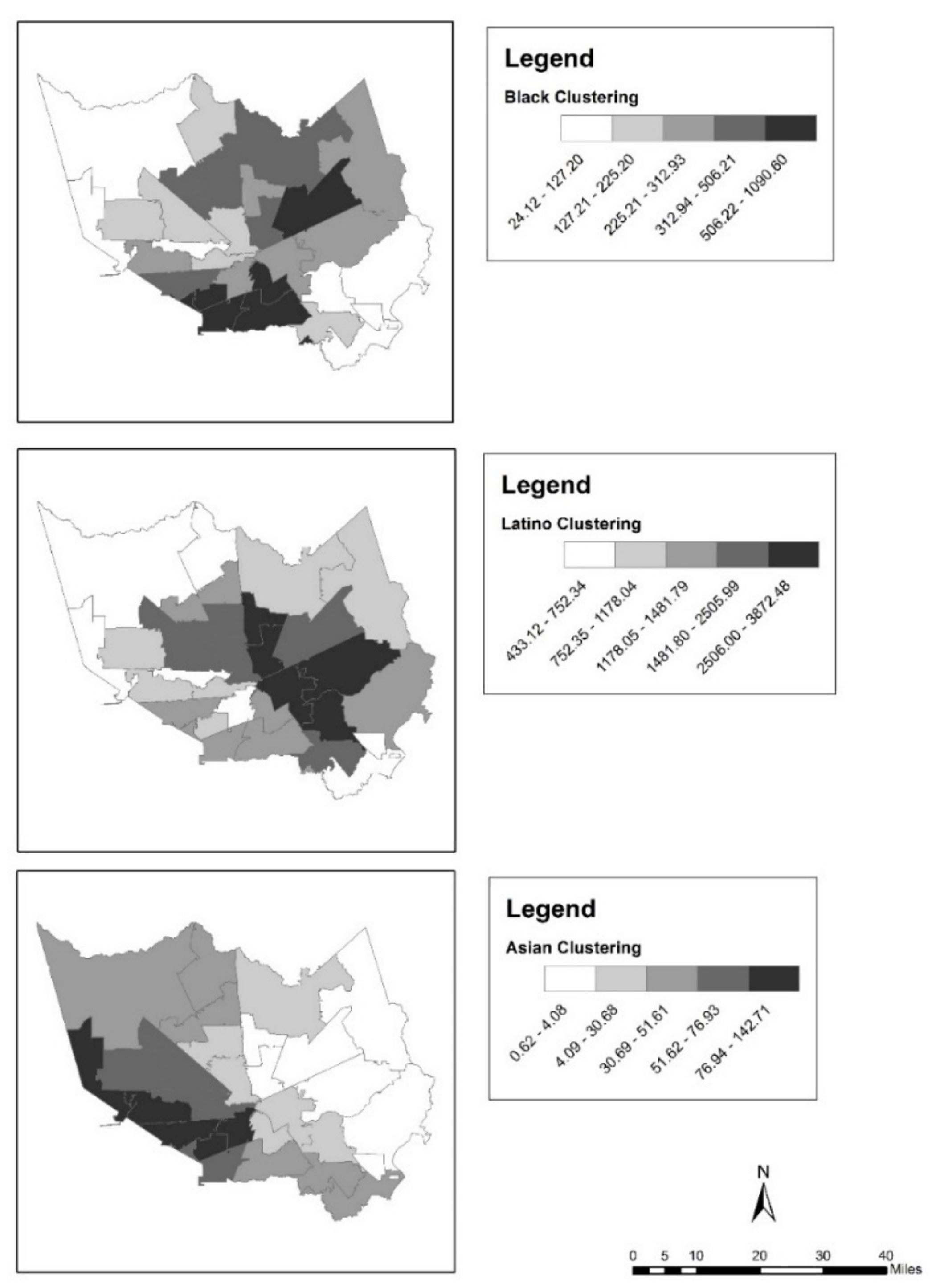
3.3. Independent Variables
3.4. Methods
4. Results
5. Discussion and Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Algert, Susan J., Aditya Agrawal, and Douglas S. Lewis. 2006. Disparities in Access to Fresh Produce in Low-Income Neighborhoods in Los Angeles. American Journal of Preventive Medicine 30: 365–70. [Google Scholar] [CrossRef] [PubMed]
- Allard, Scott W. 2009. Out of Reach: Place, Poverty, and the New American Welfare State. New Haven: Yale University Press. [Google Scholar]
- Allard, Scott W., Daniel Rosen, and Richard M. Tolman. 2003a. Access to Mental Health and Substance Abuse Services among Women Receiving Welfare in Detroit. Urban Affairs Review 38: 787–807. [Google Scholar] [CrossRef]
- Allard, Scott W., Richard M. Tolman, and Daniel Rosen. 2003b. Proximity to service providers and service utilization among welfare recipients: The interaction of place and race. Journal of Policy Analysis and Management 22: 599–613. [Google Scholar] [CrossRef] [PubMed]
- Anderson, Kathryn Freeman. 2016. Residential Segregation and Health Outcomes in the United States: Moving Beyond Black and White. Population Review 55: 45–74. [Google Scholar] [CrossRef]
- Anderson, Kathryn Freeman. 2017a. Racial Residential Segregation and the Distribution of Auxiliary Health Care Practitioners across Urban Space. Research in the Sociology of Health Care 35: 145–67. [Google Scholar]
- Anderson, Kathryn Freeman. 2017b. Racial Residential Segregation and the Distribution of Health-Related Organizations in Urban Neighborhoods. Social Problems 64: 256–76. [Google Scholar] [CrossRef]
- Anderson, Kathryn Freeman, and Andrew S. Fullerton. 2012. Racial Residential Segregation and Access to Health-Care Coverage: A Multilevel Analysis. Research in the Sociology of Health Care 30: 133–58. [Google Scholar]
- Anderson, Kathryn Freeman, and Andrew S. Fullerton. 2014. Residential Segregation, Health, and Health Care: Answering the Latino Question. Race and Social Problems 6: 262–79. [Google Scholar] [CrossRef]
- Beaulac, Julie, Elizabeth Kristjansson, and Steven Cummins. 2009. A Systematic Review of Food Deserts 1966–2007. Preventing Chronic Disease 6: 10. [Google Scholar]
- Black, Jennifer L., James Macinko, L. Beth Dixon, and George E. Fryer. 2010. Neighborhoods and obesity in New York City. Health & Place 16: 489–99. [Google Scholar]
- Blitstein, Jonathan L., Jeremy Snider, and W. Douglas Evans. 2012. Perceptions of the food shopping environment are associated with greater consumption of fruits and vegetables. Public Health Nutrition 15: 1124–29. [Google Scholar] [CrossRef] [PubMed]
- Bower, Kelly M., Roland J. Thorpe, Jr., Charles Rohde, and Darrell J. Gaskin. 2014. The intersection of neighborhood racial segregation, poverty, and urbanicity and its impact on food store availability in the United States. Preventive Medicine 58: 33–39. [Google Scholar] [CrossRef] [PubMed]
- Chan, K. S., D. J. Gaskin, G. Y. Dinwiddie, and R. McCleary. 2012. Do Diabetic Patients Living in Racially Segregated Neighborhoods Experience Different Access and Quality of Care? Medical Care 50: 692–99. [Google Scholar] [CrossRef] [PubMed]
- Charles, Camille Z. 2003. The dynamics of racial residential segregation. Annual Review of Sociology 29: 167–207. [Google Scholar] [CrossRef]
- Collins, Chiquita A. 1999. Racism and health: Segregation and causes of death amenable to medical intervention in major US cities. In Socioeconomic Status and Health in Industrial Nations: Psychological, and Biological Pathways. Edited by Nancy E. Adler, Michael Marmot, Bruce S. McEwen and Judith Stewart. New York: The NY Academy of Sciences, pp. 396–98. [Google Scholar]
- Collins, Chiquita A., and David R. Williams. 1999. Segregation and mortality: The deadly effects of racism? Sociological Forum 14: 495–523. [Google Scholar] [CrossRef]
- Dai, Dajun. 2010. Black residential segregation, disparities in spatial access to health care facilities, and late-stage breast cancer diagnosis in metropolitan Detroit. Health & Place 16: 1038–52. [Google Scholar]
- Dinwiddie, Gniesha Y., Darrell J. Gaskin, Kitty S. Chan, Janette Norrington, and Rachel McCleary. 2013. Residential segregation, geographic proximity and type of services used: Evidence for racial/ethnic disparities in mental health. Social Science & Medicine 80: 67–75. [Google Scholar]
- Ellen, Ingrid Gould, David M. Cutler, and William Dickens. 2000. Is Segregation Bad for Your Health?: The Case of Low Birth Weight. Brookings-Wharton Papers on Urban Affairs, 203–38. [Google Scholar] [CrossRef]
- Estabrooks, Paul A., Rebecca E. Lee, and Nancy C. Gyurcsik. 2003. Resources for physical activity participation: Does availability and accessibility differ by neighborhood socioeconomic status? Annals of Behavioral Medicine 25: 100–4. [Google Scholar] [CrossRef] [PubMed]
- Galaskiewicz, Joseph, Olga V. Mayorova, and Beth M. Duckles. 2013. Studying the Roles of Nonprofits, Government, and Business in Providing Activities and Services to Youth in the Phoenix Metropolitan Area. Annals of the American Academy of Political and Social Science 647: 50–82. [Google Scholar] [CrossRef]
- Gaskin, Darrell J., Gniesha Y. Dinwiddie, Kitty S. Chan, and Rachael R. McCleary. 2012. Residential Segregation and the Availability of Primary Care Physicians. Health Services Research 47: 2353–76. [Google Scholar] [CrossRef] [PubMed]
- Gaskin, Darrell J., Adrian Price, Dwayne T. Brandon, and Thomas A. LaVeist. 2009. Segregation and Disparities in Health Services Use. Medical Care Research and Review 66: 578–89. [Google Scholar] [CrossRef] [PubMed]
- Gordon-Larsen, Penny, Melissa C. Nelson, Phil Page, and Barry M. Popkin. 2006. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics 117: 417–24. [Google Scholar] [CrossRef] [PubMed]
- Grady, Sue C. 2006. Racial disparities in low birthweight and the contribution of residential segregation: A multilevel analysis. Social Science & Medicine 63: 3013–29. [Google Scholar]
- Hart, Kevin D., Stephen J. Kunitz, Ralph R. Sell, and Dana B. Mukamel. 1998. Metropolitan governance, residential segregation, and mortality among African Americans. American Journal of Public Health 88: 434–38. [Google Scholar] [CrossRef] [PubMed]
- Hayanga, Awori J., Heather E. Kaiser, Rakhi Sinha, Sean M. Berenholtz, Marty Makary, and David Chang. 2009. Residential Segregation and Access to Surgical Care by Minority Populations in US Counties. Journal of the American College of Surgeons 208: 1017–22. [Google Scholar] [CrossRef] [PubMed]
- Horowitz, Carol R., Kathryn A. Colson, Paul L. Hebert, and Kristie Lancaster. 2004. Barriers to Buying Healthy Foods for People with Diabetes: Evidence of Environmental Disparities. American Journal of Public Health 94: 1549–54. [Google Scholar]
- Iceland, John. 2004. Beyond Black and, White-Metropolitan residential segregation in multi-ethnic America. Social Science Research 33: 248–71. [Google Scholar] [CrossRef]
- Inagami, Sanae, Deborah A. Cohen, Brian Karl Finch, and Steven M. Asch. 2006. You Are Where You Shop: Grocery Store Locations, Weight, and Neighborhoods. American Journal of Preventive Medicine 31: 10–17. [Google Scholar] [CrossRef] [PubMed]
- Jetter, Karen M., and Diana L. Cassady. 2006. The Availability and Cost of Healthier Food Alternatives. American Journal of Preventive Medicine 30: 38–44. [Google Scholar] [CrossRef] [PubMed]
- Ko, Michelle, Jack Needleman, Kathryn Pitkin Derose, Miriam J. Laugesen, and Ninez A. Ponce. 2014. Residential Segregation and the Survival of U.S. Urban Public Hospitals. Medical Care Research and Review 71: 243–60. [Google Scholar] [CrossRef] [PubMed]
- LeClere, Felicia B., Richard G. Rogers, and Kimberley D. Peters. 1997. Ethnicity and mortality in the United States: Individual and community correlates. Social Forces 76: 169–98. [Google Scholar] [CrossRef]
- Lee, Min-Ah. 2009. Neighborhood residential segregation and mental health: A multilevel analysis on Hispanic Americans in Chicago. Social Science & Medicine 68: 1975–84. [Google Scholar]
- Lee, Min-Ah, and Kenneth F. Ferraro. 2007. Neighborhood Residential Segregation and Physical Health among Hispanic Americans: Good, Bad, or Benign? Journal of Health and Social Behavior 48: 131–48. [Google Scholar] [CrossRef] [PubMed]
- Link, Bruce G., and Jo Phelan. 1995. Social Conditions as Fundamental Causes of Disease. Journal of Health and Social Behavior 35: 80–94. [Google Scholar] [CrossRef]
- Marwell, Nicole P., and Aaron Gullickson. 2013. Inequality in the Spatial Allocation of Social Services: Government Contracts to Nonprofit Organizations in New York City. Social Service Review 87: 319–53. [Google Scholar] [CrossRef]
- Massey, Douglas S., and Nancy A. Denton. 1988. The Dimensions of Residential Segregation. Social Forces 67: 281–315. [Google Scholar] [CrossRef]
- Massey, Douglas S., and Nancy A. Denton. 1993. American Apartheid: Segregation and the Making of the Underclass. Cambridge: Harvard University Press. [Google Scholar]
- Massey, Douglas S., Andrew B. Gross, and Kumiko Shibuya. 1994. Migration, Segregation, and the Geographic Concentration of Poverty. American Sociological Review 59: 425–45. [Google Scholar] [CrossRef]
- Mayberry Robert M., Fatima Mili, and Elizabeth Ofili. 2000. Racial and ethnic differences in access to medical care. Medical Care Research Review 57: 108–45. [Google Scholar] [CrossRef] [PubMed]
- McFarland, Michael, and Cheryl A. Smith. 2011. Segregation, Race, and Infant Well Being. Population Research and Policy Review 30: 467–93. [Google Scholar] [CrossRef]
- Moore, Latetia V., Ana V. Diez Roux, Kelly R. Evenson, Aileen P. McGinn, and Shannon J. Brines. 2008. Availability of recreational resources in minority and low socioeconomic status areas. American Journal of Preventive Medicine 34: 16–22. [Google Scholar] [CrossRef] [PubMed]
- Moore, Latetia V., and Ana V. Diez Roux. 2006. Associations of Neighborhood Characteristics with the Location and, Type of Food Stores. American Journal of Public Health 96: 325–31. [Google Scholar] [CrossRef] [PubMed]
- Morland, Kimberly, Ana V. Diez Roux, and Steve Wing. 2006. Supermarkets, Other Food Stores, and Obesity: The Atherosclerosis Risk in Communities Study. American Journal of Preventive Medicine 30: 333–39. [Google Scholar] [CrossRef] [PubMed]
- Morland, Kimberly, Steve Wing, and Ana Diez Roux. 2002a. The Contextual Effect of the Local Food Environment on Residents’ Diets: The Atherosclerosis Risk in Communities Study. American Journal of Public Health 92: 1761–67. [Google Scholar] [CrossRef]
- Morland, Kimberly, Steve Wing, Ana Diez Roux, and Charles Poole. 2002b. Neighborhood characteristics associated with the location of food stores and food service places. American Journal of Preventive Medicine 22: 23–29. [Google Scholar] [CrossRef]
- Polednak, Anthony P. 1997. Segregation, poverty, and mortality in urban African Americans. New York: Oxford University Press. [Google Scholar]
- Powell, Lisa M., Sandy Slater, Donka Mirtcheva, Yanjun Bao, and Frank J. Chaloupka. 2007. Food store availability and neighborhood characteristics in the United States. Preventive Medicine 44: 189–95. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, Rudolph A., Saunak Sen, Kala Mehta, Sandra Moody-Ayers, Peter Bacchetti, and Ann M. O’Hare. 2007. Geography matters: Relationships among urban residential segregation, dialysis facilities, and patient outcomes. Annals of Internal Medicine 146: 493–501. [Google Scholar] [CrossRef] [PubMed]
- Small, Mario L., and Monica McDermott. 2006. The presence of organizational resources in poor urban neighborhoods: An analysis of average and contextual effects. Social Forces 84: 1697–724. [Google Scholar] [CrossRef]
- Small, Mario Luis, and Laura Stark. 2005. Are poor neighborhoods resource deprived? A case study of childcare centers in New York. Social Science Quarterly 86: 1013–36. [Google Scholar] [CrossRef]
- Smiley, Melissa J., Ana V. Diez Roux, Shannon J. Brines, Daniel G. Brown, Kelly R. Evenson, and Daniel A. Rodriguez. 2010. A spatial analysis of health-related resources in three diverse metropolitan areas. Health & Place 16: 885–92. [Google Scholar]
- Smith, David Barton, Zhanlian Feng, Mary L. Fennell, Jacqueline S. Zinn, and Vincent Mor. 2007. Separate and unequal: Racial segregation and disparities in quality across U.S. nursing homes. Health Affairs 26: 1794–94. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, Subu V., Dolores Acevedo-Garcia, and Theresa L. Osypuk. 2005. Racial residential segregation and geographic heterogeneity in black/white disparity in poor self-rated health in the US: a multilevel statistical analysis. Social Science & Medicine 60: 1667–79. [Google Scholar]
- Walker, Renee E., Christopher R. Keane, and Jessica G. Burke. 2010. Disparities and access to healthy food in the United States: A review of food deserts literature. Health & Place 16: 876–84. [Google Scholar]
- White, Kellee, Jennifer S. Haas, and David R. Williams. 2012. Elucidating the Role of Place in Health Care Disparities: The Example of Racial/Ethnic Residential Segregation. Health Services Research 47: 1278–99. [Google Scholar] [CrossRef] [PubMed]
- Williams, David R., and Chiquita Collins. 2001. Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Reports 116: 404–16. [Google Scholar] [CrossRef]
- Wilson, Dawn K., Karen A. Kirtland, Barbara E. Ainsworth, and Cheryl L. Addy. 2004. Socioeconomic status and perceptions of access and safety for physical activity. Annals of Behavioral Medicine 28: 20–28. [Google Scholar] [CrossRef] [PubMed]
- Wilson, William J. 1987. The Truly Disadvantaged: The Inner City, the Underclass, and Public Policy. Chicago: University of Chicago Press. [Google Scholar]
- Wilson, William J. 1996. When Work Disappears: The World of the New Urban Poor. New York: Knopf, Distributed by Random House, Inc. [Google Scholar]
- Zick, Cathleen D., Ken R. Smith, Jessie X. Fan, Barbara B. Brown, Ikuho Yamada, and Lori Kowaleski-Jones. 2009. Running to the Store? The relationship between neighborhood environments and the risk of obesity. Social Science & Medicine 69: 1493–500. [Google Scholar]
| Variable Name | Mean | SD | Range | Description |
|---|---|---|---|---|
| Area Level Variables | ||||
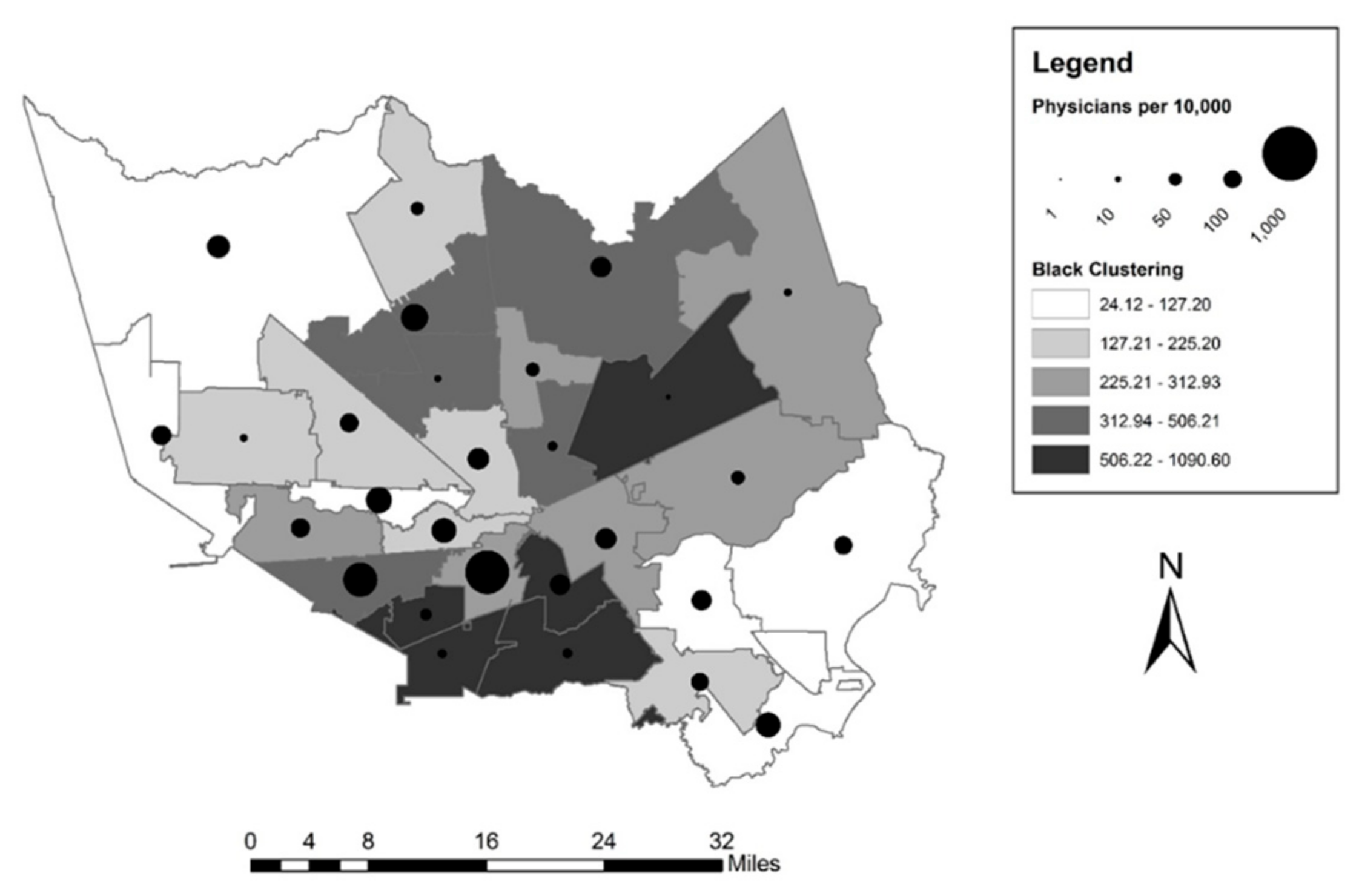
| Physician’s Offices | 8.93 | 10.04 | 0.53 to 46.52 | Physician’s offices per 10,000 people |
| % Black Clustering | 358.53 | 293.23 | 24.12 to 1090.60 | Clustering measure of percent Black |
| % Latino Clustering | 1588.71 | 981.90 | 433.12 to 3872.48 | Clustering measure of percent Latino |
| % Asian Clustering | 43.81 | 39.37 | 0.62 to 142.71 | Clustering measure of percent Asian |
| % in Poverty | 17.38 | 8.23 | 4.4 to 34.5 | Percent under the federal poverty line |
| % Foreign Born | 23.73 | 8.27 | 7.52 to 45.29 | Percent born outside of the U.S. |
| % Age 65 and Up | 8.59 | 2.35 | 4.65 to 16.20 | Percent aged 65 and above |
| Individual-Level Dependent Variables | ||||
| Personal Physician | 0.77 | 0.42 | 0 to 1 | 1 = At least one physician, 0 = else |
| Travel Time to Physician | 21.84 | 16.07 | 7.5 to 12 | Travel time to physician’s office in minutes |
| Individual-Level Independent Variables | ||||
| Age | 10.17 | 2.00 | 5 to 15 | Age in categories |
| Female | 0.63 | 0.48 | 0 to 1 | 1 = female, 0 = else |
| Race | ||||
| White (ref.) | 0.40 | 0.49 | 0 to 1 | 1 = White, 0 = else |
| Black | 0.19 | 0.39 | 0 to 1 | 1 = Black, 0 = else |
| Latino | 0.24 | 0.43 | 0 to 1 | 1 = Latino, 0 = else |
| Asian | 0.14 | 0.34 | 0 to 1 | 1 = Asian, 0 = else |
| Other | 0.03 | 0.16 | 0 to 1 | 1 = other racial category, 0 = else |
| Education | 14.55 | 3.36 | 0 to 20 | Education in years of schooling |
| Married | 0.52 | 0.50 | 0 to 1 | 1 = married, 0 = else |
| Spanish speaking | 0.09 | 0.29 | 0 to 1 | 1 = Spanish-speaking household, 0 = else |
| Unemployed | 0.11 | 0.31 | 0 to 1 | 1 = Spanish-speaking household, 0 = else |
| % FPL | 260.30 | 147.23 | 0.01 to 500 | Household income as a percent of the federal poverty line |
| Car Use | 0.93 | 0.26 | 0 to 1 | 1 = Regular access to car, 0 = else |
| Health Insurance | ||||
| No Insurance (ref.) | 0.23 | 0.42 | 0 to 1 | 1 = No health insurance, 0 = else |
| Private | 0.54 | 0.50 | 0 to 1 | 1 = Private health insurance, 0 = else |
| Public | 0.23 | 0.42 | 0 to 1 | 1 = Public health insurance, 0 = else |
| Variable Name | β | SE | β | SE |
|---|---|---|---|---|
| Black Clustering | −0.011 * | (0.004) | –0.011 *** | (0.003) |
| Latino Clustering | −0.002 | (0.002) | –0.001 | (0.003) |
| Asian Clustering | 0.063 | (0.050) | 0.099 | (0.124) |
| % in Poverty | 0.333 | (0.236) | ||
| % Foreign Born | –0.098 | (0.505) | ||
| % Age 65 and Up | 2.023 *** | (0.323) | ||
| Lambda | 0.193 | (0.213) | –0.346 | (0.223) |
| Constant | 13.600 ** | (4.802) | –9.664 * | (4.491) |
| Pseudo R2 | 0.238 | 0.414 |
| Path C | Path B | Path C’ | ||||
|---|---|---|---|---|---|---|
| Variable Name | OR | SE | OR | SE | OR | SE |
| Fixed Effects | ||||||
| Individual-Level Variables | ||||||
| Age | 1.319 *** | (0.031) | 1.320 *** | (0.031) | 1.319 *** | (0.031) |
| Female | 1.833 *** | (0.144) | 1.828 *** | (0.143) | 1.832 *** | (0.144) |
| Race (reference = White) | ||||||
| Black | 0.945 | (0.114) | 0.947 | (0.115) | 0.944 | (0.114) |
| Latino | 0.892 | (0.109) | 0.888 | (0.108) | 0.892 | (0.109) |
| Asian | 0.858 | (0.104) | 0.858 | (0.104) | 0.858 | (0.104) |
| Other | 0.947 | (0.227) | 0.948 | (0.227) | 0.948 | (0.227) |
| Education | 1.019 | (0.014) | 1.019 | (0.014) | 1.019 | (0.014) |
| Married | 1.269 ** | (0.102) | 1.268 ** | (0.101) | 1.286 ** | (0.101) |
| Spanish Speaking | 0.827 | (0.115) | 0.825 | (0.115) | 0.828 | (0.115) |
| Unemployed | 0.858 | (0.094) | 0.853 | (0.094) | 0.857 | (0.094) |
| % FLP | 1.000 | (0.000) | 1.000 | (0.000) | 1.000 | (0.000) |
| Car Use | 1.263 | (0.183) | 1.267 | (0.185) | 1.263 | (0.183) |
| Health Insurance (reference = none) | ||||||
| Private Insurance | 5.044 *** | (0.515) | 5.110 *** | (0.523) | 5.048 *** | (0.517) |
| Public Insurance | 4.263 *** | (0.534) | 4.317 *** | (0.543) | 4.271 *** | (0.535) |
| Area-Level Variables | ||||||
| Black Clustering | 0.971 | (0.000) | 0.949 | (0.000) | ||
| Latino Clustering | 0.824 ** | (0.000) | 0.807 *** | (0.000) | ||
| Asian Clustering | 0.936 | (0.002) | 0.955 | (0.002) | ||
| Physicians per 10,000 | 0.998 | (0.006) | 0.991 | (0.006) | ||
| Random Effect | ||||||
| Intercept Variance | 0.035 | 0.061 | 0.030 | |||
| Level 2 Pseudo R2 | 0.419 | 0.016 | 0.516 | |||
| Path C | Path B | Path C’ | ||||
|---|---|---|---|---|---|---|
| Variable Name | β | SE | β | SE | β | SE |
| Fixed Effects | ||||||
| Individual-Level Variables | ||||||
| Age | 0.014 | (0.140) | 0.015 | (0.140) | 0.015 | (0.140) |
| Female | −0.208 | (0.474) | −0.203 | (0.474) | −0.205 | (0.474) |
| Race (reference = White) | ||||||
| Black | 2.994 *** | (0.704) | 2.999 *** | (0.704) | 2.999 *** | (0.704) |
| Latino | 1.190 | (0.746) | 1.186 | (0.746) | 1.192 | (0.746) |
| Asian | 4.009 *** | (0.730) | 4.000 *** | (0.730) | 3.998 *** | (0.730) |
| Other | 3.464 * | (1.432) | 3.442 * | (1.432) | 3.442 * | (1.433) |
| Education | 0.122 | (0.083) | 0.122 | (0.083) | 0.122 | (0.083) |
| Married | −0.585 | (0.482) | −0.580 | (0.482) | −0.579 | (0.482) |
| Spanish Speaking | −0.806 | (0.965) | −0.806 | (0.965) | −0.814 | (0.966) |
| Unemployed | 2.129 ** | (0.760) | 2.139 ** | (0.760) | 2.134 ** | (0.760) |
| % FLP | −0.005 ** | (0.002) | −0.005 ** | (0.002) | −0.005 ** | (0.002) |
| Car Use | −8.790 *** | (0.927) | −8.791 *** | (0.927) | −8.787 *** | (0.927) |
| Health Insurance (reference = none) | ||||||
| Private Insurance | −0.602 | (0.680) | −0.603 | (0.680) | −0.602 | (0.680) |
| Public Insurance | 1.406 | (0.808) | 1.408 | (0.808) | 1.405 | (0.808) |
| Area-Level Variables | ||||||
| Black Clustering | 0.004 ** | (0.001) | 0.003 ** | (0.001) | ||
| Latino Clustering | 0.000 | (0.000) | 0.000 | (0.000) | ||
| Asian Clustering | −0.012 | (0.010) | −0.003 | (0.007) | ||
| Physicians per 10,000 | −0.156 *** | (0.031) | −0.123 *** | (0.029) | ||
| Random Effects | ||||||
| Level 1 Error Variance | 243.215 | 243.238 | 243.335 | |||
| Level 2 Error Variance | 1.794 | 1.099 | 0.371 | |||
| Level 2 Pseudo R2 | 0.525 | 0.709 | 0.902 | |||
| Effect | Coefficient | SE |
|---|---|---|
| Indirect Effect | 0.001 | 0.001 |
| Direct Effect | 0.003 | 0.001 |
| Total Effect | 0.004 * | 0.002 |
| Proportion of total effect mediated | 0.321 | |
| Ratio of indirect to direct effect | 0.472 | |
| Ratio of total to direct effect | 1.472 |
© 2018 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anderson, K.F. Racial/Ethnic Residential Segregation, the Distribution of Physician’s Offices and Access to Health Care: The Case of Houston, Texas. Soc. Sci. 2018, 7, 119. https://doi.org/10.3390/socsci7080119
Anderson KF. Racial/Ethnic Residential Segregation, the Distribution of Physician’s Offices and Access to Health Care: The Case of Houston, Texas. Social Sciences. 2018; 7(8):119. https://doi.org/10.3390/socsci7080119
Chicago/Turabian StyleAnderson, Kathryn Freeman. 2018. "Racial/Ethnic Residential Segregation, the Distribution of Physician’s Offices and Access to Health Care: The Case of Houston, Texas" Social Sciences 7, no. 8: 119. https://doi.org/10.3390/socsci7080119
APA StyleAnderson, K. F. (2018). Racial/Ethnic Residential Segregation, the Distribution of Physician’s Offices and Access to Health Care: The Case of Houston, Texas. Social Sciences, 7(8), 119. https://doi.org/10.3390/socsci7080119




