Doctors’ Perceptions of Multiracial Adolescents
Abstract
:1. Racial Disparities in Health Care
2. Perceptions of Race
3. Multiracial Targets
4. Method
Participants and Measures
5. Procedure
6. Results
6.1. Targets
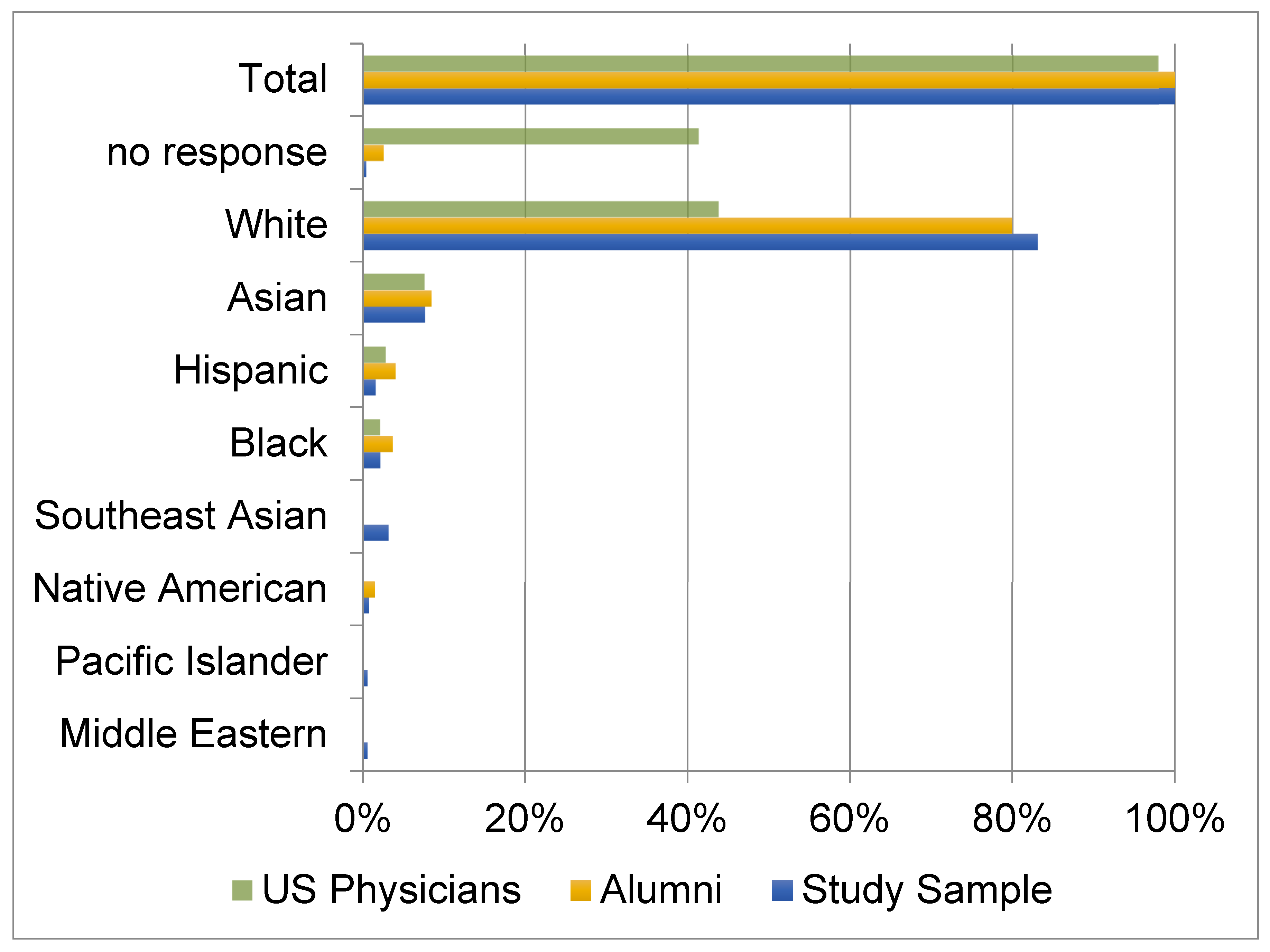
6.2. Doctors
6.3. Targets and Doctors
7. Discussion/Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
| 1 | Note: Although race and ethnicity are not synonymous, I use the terms interchangeably in this paper for several reasons. First, the question used in the original survey asked respondents to “select the one major ethnic group that best describes you” and the list of response categories included both racial and ethnic groups. Second, two-thirds of Hispanic-identifying American adults say that being Hispanic is part of their racial background—not something separate (Pew Research Center 2015). Thus, Hispanics view race in a way that does not match the way scholars gather racial/ethnic demographic data. Third, Americans more generally see Hispanic as “one of the racial/ethnic categories” despite the scholarly definition of it only as an ethnic group (Compton et al. 2010; Porter and Snipp 2018; Sandefur et al. 2004). |
| 2 | While the original survey called all of the response options ethnic groups, some scholars would argue that Middle Eastern and Hispanic are the two ethnic groups among a list of race groups. I call them all race groups for simplicity and because there is some debate about whether Hispanic and Middle Eastern should be treated as races or ethnic groups (Compton et al. 2010; Porter and Snipp 2018; Sandefur et al. 2004). |
| 3 | I could have calculated Type 3 congruence using percentage correct, percentage incorrect, or percentage missing but the results were so similar that I chose the percentage correct method. |
References
- AMA. 2019. Physicians Professional Data, Special Data Request. Chicago: American Medical Association. [Google Scholar]
- Berthold, Jessica. 2008. Consider Race-Based Risks but Treat Patients Individually. LCP Internist. Available online: https://acpinternist.org/archives/2008/07/race.htm (accessed on 19 October 2021).
- Bertrand, Marianne, and Sendhil Mullainathan. 2003. Are Emily and Greg More Employable than Lakisha and Jamal? A Field Experiment on Labor Market Discrimination. Cambridge: National Bureau of Economic Research. [Google Scholar]
- Blascovich, Jim, Natalie A. Wyer, Laura A. Swart, and Jeffrey L. Kibler. 1997. Racism and Racial Categorization. Journal of Personality & Social Psychology 72: 1364–72. [Google Scholar]
- Braunstein, Joel B., Noëlle S. Sherber, Steven P. Schulman, Eric L. Ding, and Neil R. Powe. 2008. Race, Medical Researcher Distrust, Perceived Harm, and Willingness to Participate in Cardiovascular Prevention Trials. Medicine 87: 1–9. [Google Scholar] [CrossRef] [PubMed]
- Brown, Terry D., Jr., Francis C. Dane, and Marcus D. Durham. 1998. Perception of Race and Ethnicity. Journal of Social Behavior & Personality 13: 295–307. [Google Scholar]
- Brunsma, David L. 2005. Interracial Families and the Racial Identification of Mixed-Race Children:Evidence From the Early Childhood Longitudinal Study. Social Forces 84: 1129–55. [Google Scholar] [CrossRef]
- Campbell, Mary E. 2007. Thinking outside the (black) box: Measuring black and multiracial identification on surveys. Social Science Research 36: 921–45. [Google Scholar] [CrossRef]
- Campbell, Mary E., and Christabel L. Rogalin. 2006. Categorical Imperatives: The interaction of Latino and racial identification. Social Science Quarterly 87: 1030–52. [Google Scholar] [CrossRef]
- Campbell, Mary E., and Lisa Troyer. 2011. Further Data on Misclassification: A Reply to Cheng and Powell. American Sociological Review 76: 356–64. [Google Scholar] [CrossRef]
- Chapman, Elizabeth N., Anna Kaatz, and Molly Carnes. 2013. Physicians and implicit bias: How doctors may unwittingly perpetuate health care disparities. Journal of General Internal Medicine 28: 1504–10. [Google Scholar] [CrossRef] [Green Version]
- Choi, Kristen, June Rondinelli, Emma Cuenca, Bruno Lewin, John Chang, Yi X. Luo, David Bronstein, and Katia Bruxvoort. 2022. Race/Ethnicity Differences in COVID-19 Vaccine Uptake Among Nurses. Journal of Transcultural Nursing: Official Journal of the Transcultural Nursing Society 33: 10436596211065395. [Google Scholar] [CrossRef]
- Cobb, Ryon J., Courtney S. Thomas, Whitney N. Laster Pirtle, and William A. Darity. 2016. Self-Identified Race, Socially Assigned Skin Tone, and Adult Physiological Dysregulation: Assessing Multiple Dimensions of ‘Race’ in Health Disparities Research. SSM-Population Health 2: 595–602. [Google Scholar] [CrossRef] [Green Version]
- Compton, Elizabeth, Michael Bently, Sharon Ennis, and Sonya Rastogi. 2010. 2010 Census Race and Hispanic Origin Alternative Questionnaire Experiment. U.S. Census. Available online: https://www.census.gov/content/dam/Census/library/publications/2013/dec/2010_cpex_211.pdf (accessed on 15 March 2021).
- Cooper, Richard E., Jay S. Kaufman, and Ryk Ward. 2003. Race and genomics. New England Journal of Medicine 348: 1166–70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Daniel, G. Reginald. 2002. More than Black?: Multiracial Identity and the New Racial Order. Philadelphia: Temple University Press. [Google Scholar]
- Feliciano, Cynthia. 2016. Shades of Race: How Phenotype and Observer Characteristics Shape Racial Classification. American Behavioral Scientist 60: 390–419. [Google Scholar] [CrossRef] [Green Version]
- Ferdinand, Keith C. 2006. Coronary Artery Disease in Minority Racial and Ethnic Groups in the United States. American Journal of Cardiology 97: 12. [Google Scholar] [CrossRef] [PubMed]
- FitzGerald, Chloë, and Samia Hurst. 2017. Implicit bias in healthcare professionals: A systematic review. BMC Medical Ethics 18: 19. [Google Scholar] [CrossRef] [Green Version]
- Flores, Glen, and Sandra C. Tomany-Korman. 2008. Racial and Ethnic Disparities in Medical and Dental Health, Access to Care, and Use of Services in US Children. Pediatrics 121: e286–e298. [Google Scholar] [CrossRef]
- Franco, Marisa G., and Karen M. OBrien’. 2018. Racial Identity Invalidation with Multiracial Individuals: An Instrument Development Study. Cultural Diversity and Ethnic Minority Psychology 24: 112. [Google Scholar] [CrossRef]
- Fu, Xuanning. 2000. An interracial study of marital disruption in Hawaii: 1983–1996. Journal of Divorce and Remarriage 32: 73–92. [Google Scholar] [CrossRef]
- Gaskins, Pearl F., ed. 1999. What Are You? New York: Holt. [Google Scholar]
- Green, Alexander R., Dana R. Carney, Daniel J. Pallin, Long H. Ngo, Kristal L. Raymond, Lisa I. Iezzoni, and Mahzarin R. Banaji. 2007. Implicit Bias among Physicians and its Prediction of Thrombolysis Decisions for black and white patients. Journal of General Internal Medicine 22: 1231–38. [Google Scholar] [CrossRef] [Green Version]
- Grilo, Stephanie A., J. S. Santelli, C. A. Nathanson, M. Catallozzi, A. Abraido-Lanza, Sarah Adelman, and D. Hernandez. 2022. Social and Structural Influences on Multiracial Identification and Health: A Public Health Mandate to Precisely Measure, Theorize, and Better Understand Multiracial Populations. Journal of Racial and Ethnic Health Disparities 9: 1–19. [Google Scholar] [CrossRef]
- Hannon, Lance, and Robert DeFina. 2014. Just Skin Deep? The Impact of Interviewer Race on the Assessment of African American Respondent Skin Tone. Race and Social Problems 6: 356–64. [Google Scholar] [CrossRef]
- Hannon, Lance, Verna M. Keith, Robert DeFina, and Mary E. Campbell. 2020. Do White People See Variation in Black Skin Tones? Reexamining a Purported Outgroup Homogeneity Effect. Social Psychology Quarterly 84: 95–106. [Google Scholar] [CrossRef]
- Harris, David R. 2002. In the Eye of the Beholder: Observed Race and Observer Characteristics. Ann Arbor: Institute for Social Research, University of Michigan. [Google Scholar]
- Hedges Greising, Cynthia. 2005. Collecting Race, Ethnicity, and Primary Language Data: Tools to Improve Quality of Care and Reduce Health Care Disparities. Edited by Health Research and Educational Trust. Chicago: HRET. [Google Scholar]
- Herman, Melissa R. 2004. Forced to choose: Some determinants of racial identification among multi-racial adolescents. Child Development 75: 730–48. [Google Scholar] [CrossRef] [PubMed]
- Herman, Melissa R. 2007. Racial Identification among Multiracial Youth: Implications for Adjustment. In Race and the Developing Child. Edited by Stephen Quintana and Clark McKowan. New York: Wiley Publishing Group, Sec. 2, chp. 6. [Google Scholar]
- Herman, Melissa R. 2010. Do You See What I Am? How observers’ backgrounds affect their perceptions of multiracial faces. Social Psychology Quarterly 73: 58–78. [Google Scholar] [CrossRef]
- Herman, Melissa R., and Mary E. Campbell. 2012. I wouldn’t, but you can: Attitudes toward interracial relationships. Social Science Research 41: 343–58. [Google Scholar] [CrossRef] [PubMed]
- Hill, Mark E. 2002. Race of the Interviewer and Perception of Skin Color: Evidence from the Multi-City Study of Urban Equality. American Sociological Review 67: 99–108. [Google Scholar] [CrossRef]
- Jackson, Fatimah L. C. 2008. Ancestral links of Chesapeake Bay region African Americans to specific Bight of Bonny (West Africa) microethnic groups and increased frequency of aggressive breast cancer in both regions. American Journal of Human Biology 20: 165–73. [Google Scholar] [CrossRef]
- Jones, Nicholas, Rachel Marks, Roberto Ramirez, and Merarys Rios-Vargas. 2021. Census Illuminates Racial and Ethnic Composition of the Country. Available online: https://www.census.gov/library/stories/2021/08/improved-race-ethnicity-measures-reveal-united-states-population-much-more-multiracial.html (accessed on 15 March 2022).
- Kao, Grace. 1999. Racial identity and academic performance: An examination of biracial Asian and African American youth. Journal of Asian American Studies 2: 223–49. [Google Scholar] [CrossRef]
- Kateri Hernandez, Tanya. 2018. Multiracials and Civil Rights: Mixed-Race Stories of Discrimination. New York: NYU Press. [Google Scholar]
- Kressin, Nancy R., Bei-Hung Chang, Ann Hendricks, and Lewis Kazis. 2003. Agreement Between Administrative Data and Patients’ Self-Reports of Race/Ethnicity. American Journal of Public Health 93: 1734–39. [Google Scholar] [CrossRef]
- Latkin, Carl A., Lauren Dayton, Grace Yi, Arianna Konstantopoulos, and Basmattee Boodram. 2021. Trust in a COVID-19 vaccine in the U.S.: A social-ecological perspective. Social Science Medicine 270: 113684. [Google Scholar] [CrossRef]
- Lau, May, Hua Lin, and Glenn Flores. 2012. Racial/Ethnic Disparities in Health and Health Care among U.S. Adolescents. Health Services Research 47: 2031–59. [Google Scholar] [CrossRef] [Green Version]
- LaVeist, Thomas A., and Amani Nuru-Jeter. 2002. Is doctor-patient race concordance associated with greater satisfaction with care? Journal of Health and Social Behavior 43: 269–306. [Google Scholar] [CrossRef]
- Levin, Shana, Pamela L. Taylor, and Elena Caudle. 2007. Interethnic and Interracial Dating in College: A Longitudinal Study. Journal of Social and Personal Relationships 24: 323–41. [Google Scholar] [CrossRef]
- Littrell, Jill. 2008. New developments in understanding cardiovascular disease and the implications for social work. Social Work Helath Care 46: 35–49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Sze Yan, Roman Pabayo, and Peter Muennig. 2021. Perceived Discrimination and Increased Odds of Unmet Medical Needs Among US Children. International Journal of Health Services 51: 364–70. [Google Scholar] [CrossRef]
- Livingston, Robert W., and Marilynn B. Brewer. 2002. What are we really priming? Cue-based versus category-based processing of facial stimuli. Journal of Personality & Social Psychology 82: 5. [Google Scholar]
- López, Nancy, Edward Vargas, Melina Juarez, Lisa Cacari-Stone, and Sonia Bettez. 2018. What’s Your ‘Street Race’? Leveraging Multidimensional Measures of Race and Intersectionality for Examining Physical and Mental Health Status among Latinxs. Sociology of Race and Ethnicity 4: 49–66. [Google Scholar] [CrossRef] [Green Version]
- Maddox, Keith B. 2004. Perspectives on Racial Phenotypicality Bias. Personality and Social Psychology Review 8: 383–401. [Google Scholar] [CrossRef]
- Maddox, Keith B., and Stephanie A. Gray. 2002. Cognitive Representations of Black Americans: Reexploring the Role of Skin Tone. Personality and Social Psychology Bulletin 28: 250–59. [Google Scholar] [CrossRef]
- Meghani, Selimah H., Jacqueline M. Brooks, Trina Gipson-Jones, Roberta Waite, Lisa Whitfield-Harris, and Janet A. Deatrick. 2009. Patient-Provider Race-Concordance: Does It Matter in Improving Minority Patients’ Health Outcomes? Ethnicity & Health 14: 107–30. [Google Scholar]
- Monk, Ellis P. 2015. The Cost of Color: Skin Color, Discrimination, and Health among African-Americans. American Journal of Sociology 121: 396–444. [Google Scholar] [CrossRef] [Green Version]
- Ndugga, Nambi, Latoya Hill, Samantha Artiga, and Sweta Haldar. 2021. Latest Data on COVID-19 Vaccinations by Race/Ethnicity, Kaiser Family Foundation Report. Available online: https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-by-race-ethnicity/ (accessed on 15 March 2022).
- Nelson, Alan R. 2002. What Healthcare Consumers Need to Know about Racial and Ethnic Disparities in Healthcare. Washington, DC: National Academy of Sciences, Institute of Medicine. [Google Scholar]
- Oliver, Mary Beth, and Dana Fonash. 2002. Race and Crime in the News: Whites’ Identification and Misidentification of Violent and Nonviolent Criminal Suspects. Media Psychology 4: 137–56. [Google Scholar] [CrossRef]
- Pager, Devah. 2003. The Mark of a Criminal Record. American Journal of Sociology 108: 937–75. [Google Scholar] [CrossRef] [Green Version]
- Pager, Devah. 2007. Marked: Race, Crime, and Finding Work in an Era of Mass Incarceration. Chicago: University of Chicago Press. [Google Scholar]
- Panter, Abigail T., Charles C. Daye, Walter R. Allen, Linda F. Wightman, and Meera E. Deo. 2008. It matters how and when you ask: Self-reported race/ethnicity of incoming law students. Cultural Diversity and Ethnic Minority Psychology 15: 51–66. [Google Scholar] [CrossRef]
- Pauker, Kristin, Nalini Ambady, and Evan P. Apfelbaum. 2010. Race Salience and Essentialist Thinking in Racial Stereotype Development. Child Development 81: 1799–813. [Google Scholar] [CrossRef]
- Peery, Destiny, and Galen V. Bodenhausen. 2008. Black + White = Black: Hypodescent in Reflexive Categorization of Racially Ambiguous Faces. Psychological Science. in press. [Google Scholar] [CrossRef] [PubMed]
- Pew Research Center. 2015. Multiracial in America. Chapter 7: The Many Dimensions of Hispanic Racial Identity. Available online: http://www.pewsocialtrends.org/2015/06/11/chapter-7-the-many-dimensions-of-hispanic-racial-identity/ (accessed on 15 March 2022).
- Pickett, Robert E. M., Aliya Saperstein, and Andrew M. Penner. 2019. Placing Racial Classification in Context. Socius 5: 1–15. [Google Scholar] [CrossRef] [PubMed]
- Porter, Sonya R., and C. Matthew Snipp. 2018. Measuring Hispanic Origin: Reflections on Hispanic Race Reporting. The ANNALS of the American Academy of Political and Social Science 677: 140–52. [Google Scholar] [CrossRef]
- Quillian, Lincoln, and Rozlyn Redd. 2008. The Social Networks of Multiracial Adolescents. Evanston: Northwestern University. [Google Scholar]
- Rao, Deepa, Joseph M. Feinglass, and Patrick Corrigan. 2007. Racial and ethnic disparities in mental illness stigma. The Journal of Nervous and Mental Disease 195: 1020–23. [Google Scholar] [CrossRef]
- Rhoades, Dorothy A. 2005. Racial Misclassification and Disparities in Cardiovascular Disease Among American Indians and Alaska Natives. Circulation 111: 1250–56. [Google Scholar] [CrossRef] [Green Version]
- Richeson, Jennifer A., and Sophie Trawalter. 2005. On the Categorization of Admired and Disliked Exemplars of Admired and Disliked Racial Groups. Journal of Personality & Social Psychology 89: 517–30. [Google Scholar]
- Rockquemore, Kerry Ann, and David L. Brunsma. 2002. Beyond Black: Biracial Identity in America. New York: Sage Publications, Inc. [Google Scholar]
- Romano, Max J. 2018. White Privilege in a White Coat: How Racism Shaped my Medical Education. Annals of Family Medicine 16: 261–63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Root, Maria P. P. 1997. Biracial identity. In Children’s Needs II: Development, Problems, and Alternatives. Edited by George G. Bear, Kathleen M. Minke and Alex Thomas. Bethesda: National Association of School Psychologists. [Google Scholar]
- Root, Maria P. P. 2001. Factors Influencing the Variations in Racial and Ethnic Identity of Mixed-Heritage Persons of Asian Ancestry. In The Sum of Our Parts: Mixed Heritage Asian Americans. Edited by T. Williams-Leon and Cynthia L. Nakashima. Philadelphia: Temple University Press, pp. 61–70. [Google Scholar]
- Sandefur, Gary, Mary E. Campbell, and Jennifer Eggerling-Boeck. 2004. Racial and Ethnic Identification, Official Classifications, and Health Disparities. In Critical Perspectives on Racial and Ethnic Differences in Health in Late Life, National Research Council Panel on Race, Ethnicity, and Health in Later Life. Edited by Norman B. Anderson, Randy A. Bulatao and Barney Cohen. Washington, DC: National Academies Press, chp. 2. [Google Scholar]
- Saperstein, Aliya. 2006. Double-Checking the Race Box: Examining Inconsistency between Survey Measures of Observed and Self-Reported Race. Social Forces 85: 57–74. [Google Scholar] [CrossRef]
- Senna, Danzy. 2009. Where Did You Sleep Last Night? New York: Picador. [Google Scholar]
- Shih, Margaret, and Diana T. Sanchez. 2005. Perspectives and research on the positive and negative implications of having multiple racial identities. Psychological Bulletin 131: 569–91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, Alex. 2021. Flawed Data In Missouri Skews Tracking For Vaccine Equity, NPR Weekend Edition. Available online: https://www.npr.org/2021/05/29/1001522018/flawed-data-in-missouri-skews-tracking-for-vaccine-equity (accessed on 15 March 2022).
- Snyder, Cyndy R., Prince Z. Wang, and Anjali R. Truitt. 2018. Multiracial Patient Experiences with Racial Microaggressions in Health Care Settings. Journal of Patient-Centered Research and Reviews 5: 229–38. [Google Scholar] [CrossRef]
- Sporer, Sigfried Ludwig. 2001. Recognizing faces of other ethnic groups: An integration of theories. Psychology, Public Policy, & Law 7: 36–97. [Google Scholar]
- Tashiro, Cathy J. 2005. Health Disparities in the Context of Mixed Race: Challenging the ideology of race. Advances in Nursing Science 28: 203–11. [Google Scholar] [CrossRef]
- Tashiro, C. J. 2008. (University of Washington, Tacoma, WA, USA). Personal communication.
- Udry, J. Richard, Rose Maria Li, and Janet Hendrickson-Smith. 2003. Health and behavior risks of adolescents with mixed-race identity. American Journal of Public Health 93: 1865–70. [Google Scholar] [CrossRef]
- Van Bavel, Jay J., and William A. Cunningham. 2012. A social identity approach to person memory: Group membership, collective identification, and social role shape attention and memory. Personality and Social Psychology Bulletin 38: 1566. [Google Scholar] [CrossRef] [Green Version]
- van Ryn, Michelle, and Jane Burke. 2000. The effect of patient race and socio-economic status on physicians’ perceptions of patients. Social Science and Medicine 50: 813. [Google Scholar] [CrossRef]
- Vargas, Nicholas, and Kevin Stainback. 2016. Documenting Contested Racial Identities Among Self-Identified Latina/Os, Asians, Blacks, and Whites. American Behavioral Scientist 60: 442–64. [Google Scholar] [CrossRef]
- Westergaard, Ryan P., Mary C. Beach, Somnath Saha, and Elizabeth A. Jacobs. 2014. Racial/ethnic differences in trust in health care: HIV conspiracy beliefs and vaccine research participation. Journal of General Internal Medicine 29: 140–46. [Google Scholar] [CrossRef] [Green Version]
- White-Means, Shelley, Zhiyong Dong, Meghan Hufstader, and Lawrence T. Brown. 2009. Cultural competency, race, and skin tone bias among pharmacy, nursing, and medical students. Medical Care Research and Review 66: 436–55. [Google Scholar] [CrossRef] [PubMed]
- Willadsen-Jensen, Eve C., and Tiffany A. Ito. 2006. Ambiguity and the Timecourse of Racial Perception. Social Cognition 24: 580–606. [Google Scholar] [CrossRef]
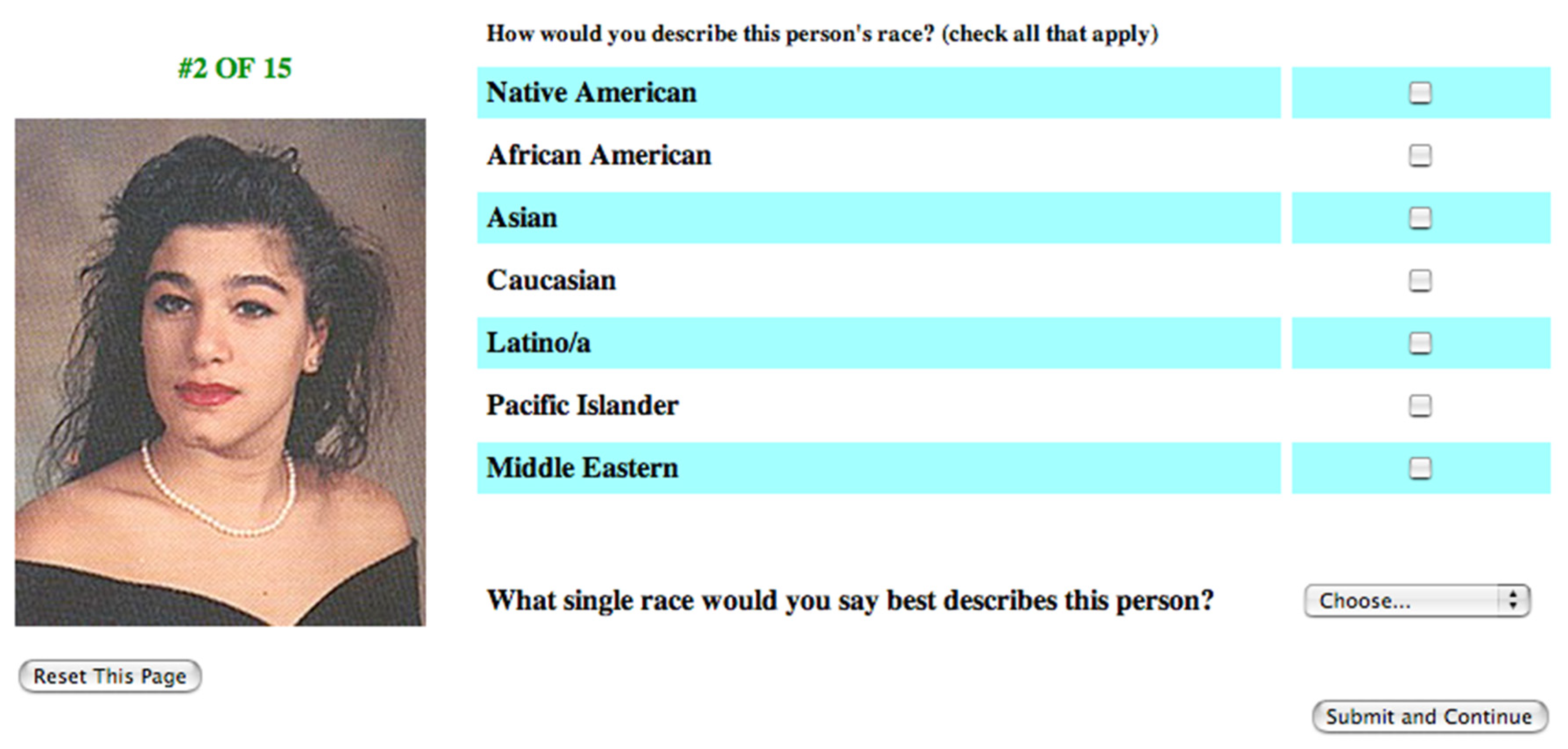
| Photo # | Ancestries | Identification | Gender |
|---|---|---|---|
| 1 | Black–American Indian | Black | female |
| 2 | Black–American Indian | Black | male |
| 3 | Black–American Indian | American Indian | female |
| 4 | Black–American Indian | American Indian | male |
| 5 | Black–White | Black | female |
| 6 | Black–White | Black | male |
| 7 | Black–White | White | female |
| 8 | Black–White | White | male |
| 9 | Black–Asian | Black | female |
| 10 | Black–Asian | Black | male |
| 11 | Black–Hispanic | Black | female |
| 12 | Black–Hispanic | Hispanic | female |
| 13 | Black–Hispanic | Hispanic | male |
| 14 | Black–Pacific Islander | Pacific Islander | female |
| 15 | American Indian–White | American Indian | female |
| 16 | American Indian–White | American Indian | male |
| 17 | American Indian–White | American Indian | female |
| 18 | American Indian–White | White | female |
| 19 | American Indian–White | White | male |
| 20 | American Indian–Hispanic | American Indian | female |
| 21 | American Indian–Hispanic | American Indian | male |
| 22 | White–Asian | White | female |
| 23 | White–Asian | White | male |
| 24 | White–Asian | Hispanic (Filipino) | female |
| 25 | White–Asian | Asian | male |
| 26 | White–Hispanic | White | female |
| 27 | White–Hispanic | White | male |
| 28 | White–Hispanic | Hispanic | female |
| 29 | White–Hispanic | Hispanic | male |
| 30 | White–Middle Eastern | White | male |
| 31 | White–Middle Eastern | Middle Eastern | female |
| 32 | White–Middle Eastern | Middle Eastern | male |
| 33 | White–Pacific Islander | Pacific Islander | female |
| 34 | White–Pacific Islander | White | male |
| 35 | Hispanic–Middle Eastern | Hispanic | male |
| % | Min | Max | Mean | Std. Dev. | |
|---|---|---|---|---|---|
| Middle Eastern | 0.6% | ||||
| Pacific Islander | 0.6% | 3 | |||
| American Indian | 0.8% | 3 | |||
| Southeast Asian | 3.1% | 4 | |||
| Black | 2.2% | 16 | |||
| Hispanic | 1.6% | 11 | |||
| Asian | 7.7% | 8 | |||
| White | 83.1% | 39 | |||
| No response | 0.4% | 423 | |||
| Female | 37.0% | ||||
| Foreign born | 4.1% | ||||
| Age | 25 | 84 | 45.02 | 15.52 | |
| Roommate of a different race | 69.0% | ||||
| Dated or married someone of a different race | 47.4% | ||||
| Parent, sibling, spouse, or child of another race | 13.6% | ||||
| Non-White patients in caseload | 30.0% | ||||
| Non-White co-workers | 14.8% | ||||
| How often do you consider the race of the patient? | |||||
| 0 = never | 28.50% | 1.18 | 0.97 | ||
| 1 = rarely | 34.80% | ||||
| 2 = sometimes | 29.10% | ||||
| 3 = frequently | 5.90% | ||||
| 4 = always | 1.80% | ||||
| If you do consider the race of the patient in making treatment decisions, how do you ascertain it? (check all that apply) | |||||
| Ask directly | 53.4% | ||||
| Look in chart | 32.4% | ||||
| Observe cultural clues | 32.0% | ||||
| Observe skin tone | 36.2% | ||||
| Other | 5.5% | ||||
| N = 509 doctors | |||||
| Target Self-Identification | Type 1: Forced-Choice Congruence | Type 2: Binary Congruence | Type 3: Percentage Congruence |
|---|---|---|---|
| Black | 77% | 39% | 69% |
| American Indian | 6% | 44% | 64% |
| White | 60% | 35% | 76% |
| Asian | 46% | 40% | 72% |
| Hispanic | 41% | 51% | 63% |
| Middle Eastern | 37% | 63% | 73% |
| Pacific Islander | 12% | 59% | 45% |
| Total | 49% | 43% | 68% |
| N = 7643 photo views for all types of congruence | |||
| B | S.E. | p-Value | ||
|---|---|---|---|---|
| Female | 0.095 | 0.227 | 0.676 | |
| Black | −0.276 | 0.624 | 0.659 | |
| Hispanic | 0.150 | 0.814 | 0.854 | |
| Asian | −0.855 | 0.405 | 0.035 | * |
| Age | 0.014 | 0.007 | 0.046 | * |
| Foreign born | 0.548 | 0.600 | 0.361 | |
| Family members of another race | 0.283 | 0.337 | 0.401 | |
| Roommate of another race | 0.234 | 0.237 | 0.324 | |
| Dated or married another race | 0.054 | 0.225 | 0.810 | |
| Non-White patients | 0.008 | 0.004 | 0.046 | * |
| Non-White colleagues | −0.002 | 0.005 | 0.689 | |
| Constant | −26.513 | 14.353 | 0.065 | |
| N = 509 doctors | ||||
| Log Likelihood = 591.241 | ||||
| Cox & Snell R2 = 0.033 | ||||
| R2 = 17.020 df = 11, p < 0.108 |
| B | S.E. | Sig. | ||
|---|---|---|---|---|
| Doctor | ||||
| Female | −0.081 | 0.063 | 0.198 | |
| Black | 0.114 | 0.171 | 0.505 | |
| Hispanic | 0.043 | 0.194 | 0.824 | |
| Asian | 0.019 | 0.119 | 0.873 | |
| American Indian | 0.191 | 0.189 | 0.312 | |
| Pacific Islander | 0.390 | 0.635 | 0.539 | |
| Middle Eastern | 0.244 | 0.248 | 0.325 | |
| Southeast Asian | 0.492 | 0.297 | 0.098 | |
| Other | −0.090 | 0.162 | 0.578 | |
| Age | 0.006 | 0.002 | 0.003 | ** |
| Family members of another race | 0.105 | 0.091 | 0.249 | |
| Dated or married another race | −0.116 | 0.064 | 0.070 | |
| Roommate of another race | −0.013 | 0.068 | 0.849 | |
| % non-White patients | −0.001 | 0.001 | 0.317 | |
| % non-White colleagues | −0.001 | 0.001 | 0.317 | |
| Foreign born | −0.278 | 0.157 | 0.077 | |
| Frequency of using race in diagnosis | −0.064 | 0.038 | 0.092 | |
| Determine race using skin tone | −0.134 | 0.079 | 0.090 | |
| Determine race by asking | 0.074 | 0.047 | 0.116 | |
| Determine race by cultural overtones | 0.147 | 0.081 | 0.070 | |
| Target | ||||
| Female | −0.586 | 0.063 | 0.000 | *** |
| Black | 0.926 | 0.075 | 0.000 | *** |
| American Indian | −3.027 | 0.137 | 0.000 | *** |
| Asian | −0.886 | 0.102 | 0.000 | *** |
| Hispanic | −0.782 | 0.086 | 0.000 | *** |
| Middle Eastern | −0.661 | 0.126 | 0.000 | *** |
| Pacific Islander | −2.160 | 0.174 | 0.000 | *** |
| Number of ancestries | −0.290 | 0.030 | 0.000 | *** |
| Constant | −10.999 | 4.227 | 0.009 | ** |
| N = 7089 photo views | ||||
| Cox & Snell R2 = 0.272 | ||||
| Log likelihood = 7511.665 | ||||
| R2 = 2236.976 df = 28, p < 0.000 |
| B | S.E. | Beta | Sig. | |
|---|---|---|---|---|
| Doctor | ||||
| Female | 0.000 | 0.004 | −0.003 | |
| Black | 0.000 | 0.011 | 0.000 | |
| Hispanic | −0.019 | 0.012 | −0.017 | |
| Asian | −0.006 | 0.008 | −0.009 | |
| American Indian | 0.006 | 0.012 | 0.005 | |
| Pacific Islander | 0.026 | 0.040 | 0.007 | |
| Middle Eastern | 0.012 | 0.015 | 0.008 | |
| Southeast Asian | 0.041 | 0.019 | 0.023 | * |
| Other | 0.013 | 0.010 | 0.014 | |
| Age | 0.001 | 0.000 | 0.048 | *** |
| Family members of another race | 0.003 | 0.006 | 0.007 | |
| Dated or married another race | −0.007 | 0.004 | −0.021 | |
| Roommate of another race | 0.001 | 0.004 | 0.003 | |
| % non-White patients | 0.000 | 0.000 | 0.007 | |
| % non-White colleagues | 0.000 | 0.000 | −0.008 | |
| Foreign born | −0.016 | 0.010 | −0.018 | |
| Frequency of using race in diagnosis | −0.004 | 0.002 | −0.021 | |
| Determine race using skin tone | −0.006 | 0.005 | −0.016 | |
| Determine race by asking | 0.001 | 0.003 | 0.006 | |
| Determine race by cultural overtones | 0.006 | 0.005 | 0.017 | |
| Target | ||||
| Female | 0.005 | 0.004 | 0.015 | |
| Black | −0.071 | 0.005 | −0.182 | *** |
| American Indian | −0.116 | 0.006 | −0.245 | *** |
| Asian | −0.040 | 0.007 | −0.064 | *** |
| Hispanic | −0.116 | 0.006 | −0.225 | *** |
| Middle Eastern | −0.005 | 0.009 | −0.007 | |
| Pacific Islander | −0.292 | 0.009 | −0.374 | *** |
| Number of ancestries | −0.048 | 0.002 | −0.277 | *** |
| Constant | −0.204 | 0.265 | ||
| N = 7089 photo views | ||||
| R2 = 00.262 |
| Doctor Perception of Target | ||||||||
|---|---|---|---|---|---|---|---|---|
| Target Self-Identification | Black | White | Asian | American Indian | Middle | Hispanic | Pacific | |
| Black | 77% | 5% | 2% | 1% | 3% | 7% | 5% | 100% |
| White | 13% | 60% | 3% | 2% | 3% | 14% | 5% | 100% |
| Asian | 0% | 45% | 46% | 2% | 0% | 2% | 5% | 100% |
| American Indian | 39% | 28% | 1% | 6% | 1% | 21% | 4% | 100% |
| Middle | 2% | 25% | 0% | 4% | 37% | 29% | 3% | 100% |
| Hispanic | 16% | 6% | 25% | 1% | 4% | 41% | 7% | 100% |
| Pacific | 7% | 6% | 10% | 7% | 28% | 31% | 12% | 100% |
| Total | 33% | 28% | 9% | 3% | 5% | 17% | 5% | 100% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herman, M. Doctors’ Perceptions of Multiracial Adolescents. Soc. Sci. 2022, 11, 146. https://doi.org/10.3390/socsci11040146
Herman M. Doctors’ Perceptions of Multiracial Adolescents. Social Sciences. 2022; 11(4):146. https://doi.org/10.3390/socsci11040146
Chicago/Turabian StyleHerman, Melissa. 2022. "Doctors’ Perceptions of Multiracial Adolescents" Social Sciences 11, no. 4: 146. https://doi.org/10.3390/socsci11040146
APA StyleHerman, M. (2022). Doctors’ Perceptions of Multiracial Adolescents. Social Sciences, 11(4), 146. https://doi.org/10.3390/socsci11040146





