Bibliometric Analysis of Hospital Design: Knowledge Mapping Evolution and Research Trends
Abstract
1. Introduction
2. Literature Review
3. Materials and Methods
3.1. Data Collection
3.2. Bibliometric Tools and Settings
- Setting time period as 1932–2025 (the full time period), with 1 year per slice, where each slice selected 50 high-frequency nodes (Top N = 50);
- Adjusting the k-value flexibly to the requirements of different analysis types to optimize the clarity and structural presentation of the graph based on the g-index algorithm;
- Using the ‘Pathfinder’ and ‘Pruning the merged network’ settings for network structure pruning;
- Using the Log-Likelihood Ratio (LLR) clustering algorithm for cluster analysis to extract noun terms from the titles of these documents to name the research contents corresponding to the clusters [105].
3.3. Visualization and Network Construction
- Collaboration networks at country/region, institution, and author levels to reveal cooperation structures;
- Co-citation networks of authors and journals to identify influential intellectual bases;
- Reference co-citation and disciplinary co-occurrence maps to outline knowledge structure and disciplinary distribution;
- Keyword co-occurrence maps to capture research themes and hotspots.
3.4. Interpretation Strategy
4. Results
4.1. Research Trends and Overview of Research Groups
4.1.1. Analysis of the Number of Publications
4.1.2. Analysis of the Cooperation Network of Countries
4.1.3. Analysis of the Cooperation Network of Institutions
4.1.4. Analysis of the Cooperation Network of Authors
4.2. Identification of Core Contributions and Influence
4.2.1. Analysis of Reference Citations
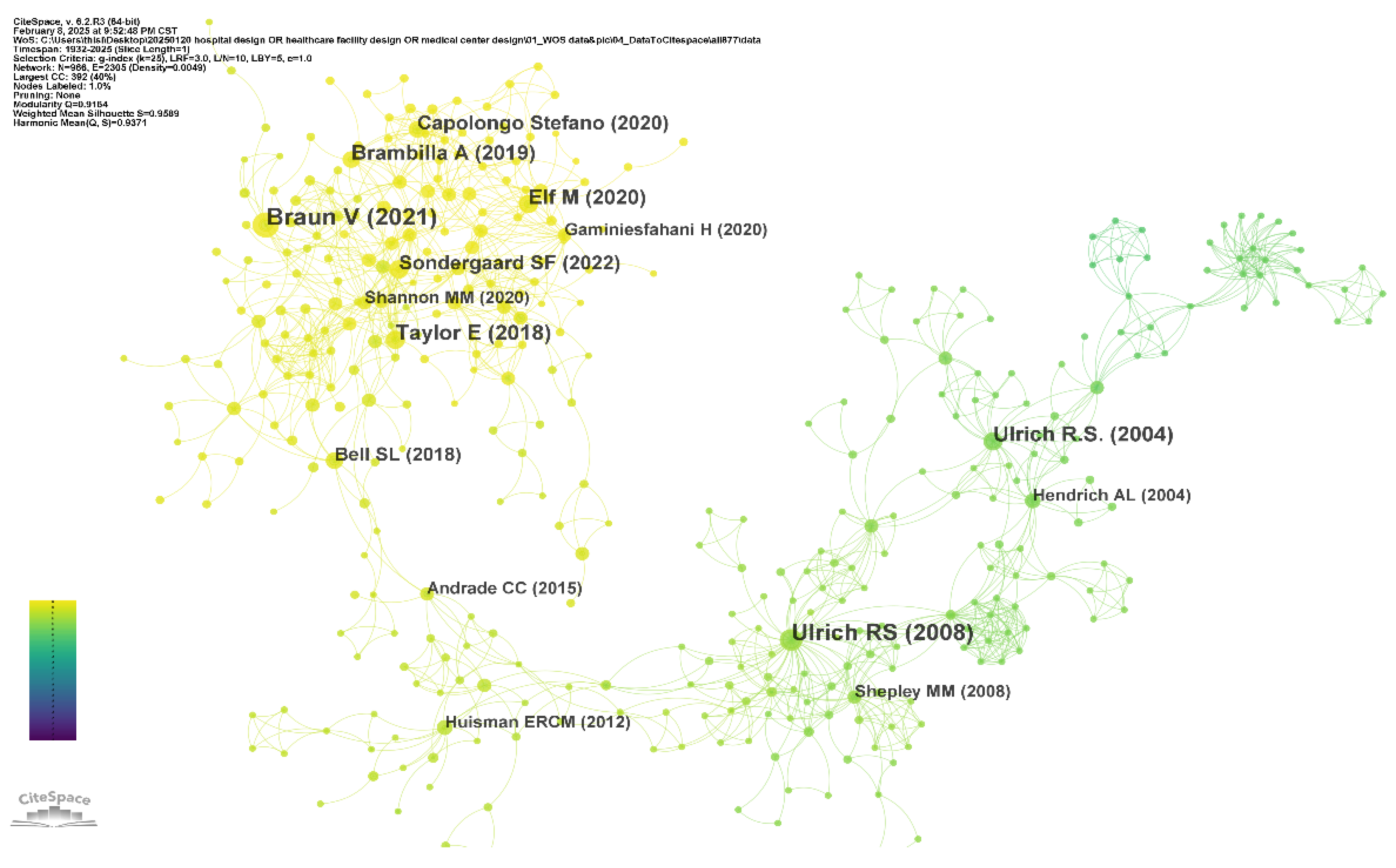
4.2.2. Analysis of the Co-Citation Network of Authors
4.2.3. Analysis of the Co-Citation Network of Journals
- The Health Environments Research & Design Journal (HERD) is the journal with the highest co-citation frequency in this field, reflecting its importance as a specialized journal in the hospital design field.
- The Lancet and New England Journal of Medicine (NEJM) are authoritative journals in the medical field, which also play an important role in supporting the literature on the research of medical buildings.
- The Journal of the American Medical Association (JAMA) shows a high centrality, indicating that it has a sound knowledge intermediary role between different research groups.
- The Journal of Advanced Nursing and Journal of Clinical Nursing show the contribution of the nursing field to healthcare space.
- Environment and Behavior is the journal with the highest co-citation centrality, indicating that it has a significant bridging role in connecting environmental psychology and medical building research.
- PLOS ONE, the British Medical Journal (BMJ), the Journal of Environmental Psychology, and other journals also have a high co-citation frequency, reflecting the obvious interdisciplinary characteristics of this field, involving multiple directions, such as medicine, psychology, environmental behavioral science, and architecture.
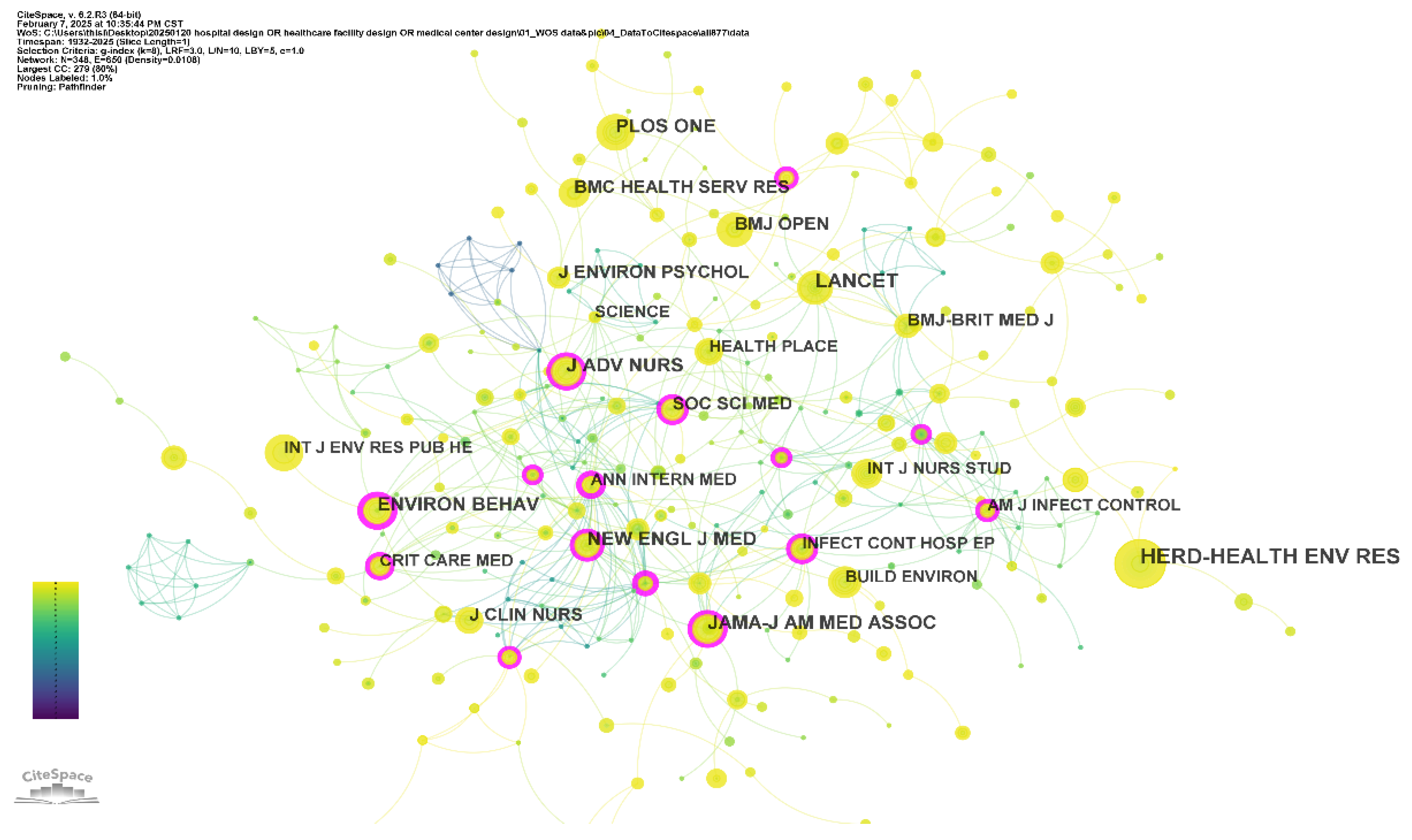
| No. | Cited Journals | Count | Centrality | Year |
|---|---|---|---|---|
| 1 | HERD-HEALTH ENV RES | 226 | 0.02 | 2010 |
| 2 | LANCET | 140 | 0.08 | 1987 |
| 3 | JAMA-J AM MED ASSOC | 121 | 0.11 | 1995 |
| 4 | J ADV NURS | 112 | 0.1 | 2004 |
| 5 | NEW ENGL J MED | 102 | 0.15 | 1999 |
| 6 | ENVIRON BEHAV | 94 | 0.21 | 2006 |
| 7 | PLOS ONE | 91 | 0.02 | 2013 |
| 8 | BMJ-BRIT MED J | 85 | 0.1 | 1989 |
| 9 | J ENVIRON PSYCHOL | 76 | 0.06 | 2011 |
| 10 | J CLIN NURS | 75 | 0.07 | 2013 |
4.3. Knowledge Base and Disciplinary Structure Evolution
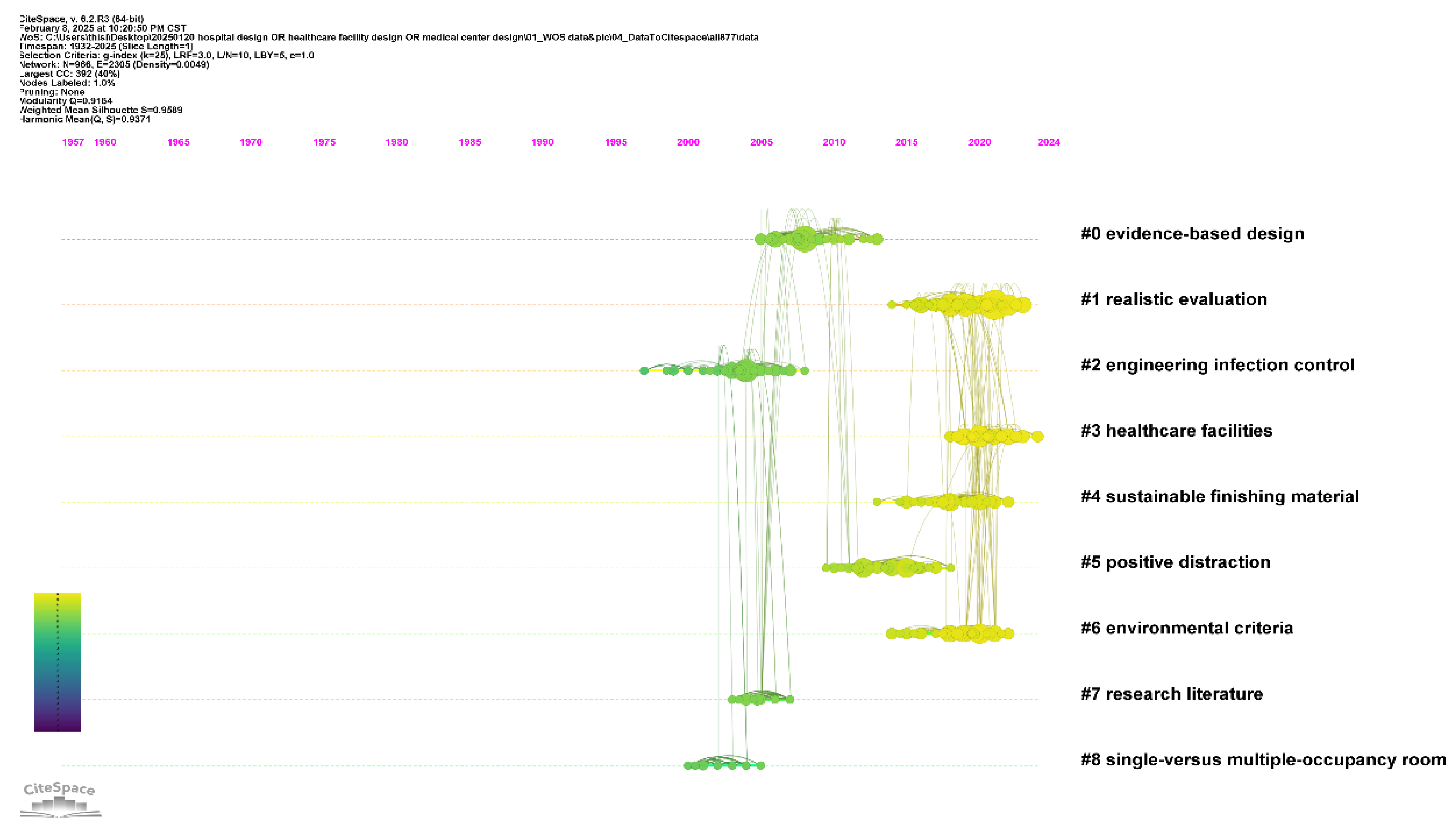
4.3.1. Analysis of the Cited References
- Cluster #0 (evidence-based design): This cluster focuses on optimizing hospital design based on empirical research, emphasizing the impact of the physical environment on patient recovery and employee performance. As the core and most node-dense area of the entire network, it shows that EBD is the most representative and structurally stable theoretical foundation in this field.
- Cluster #1 (realistic evaluation) and Cluster #3 (healthcare facilities): They focus on “design effect evaluation” and “medical institution design practice”, respectively, explore the methodology and practical application challenges of the effect evaluation of healthcare facilities environmental intervention measures, as well as the functional layout optimization and design evolution, forming relatively independent but interconnected secondary research topics in the network structure.
- Cluster #2 (engineering infection control) and Cluster #8 (single- versus multiple-occupancy room): Located at the edge of the network but with clear cluster boundaries, they focus on how architectural engineering design intervenes in hospital infection prevention and control, especially in ventilation systems and spatial layout strategies. They also compare single-patient rooms to multi-occupancy rooms in terms of infection control, patient privacy, and treatment effects. This reflects the importance of research on infection control and ward type selection at a specific stage.
- Clusters #4 (sustainable finishing material) and #6 (environmental criteria): Research on the application of sustainable materials in medical buildings, emphasizing environmental performance and indoor health standards and focusing on environmental performance standards for healthcare environment design, including air quality, energy consumption, lighting conditions, etc. They show the expansion trend of green medical building research in recent years.
- Cluster #5 (positive distraction): As an interdisciplinary integration attempt, it reflects the research related to “psychological healing design” in the medical space and analyzes the strategy of providing positive sensory stimulation (such as natural landscape and color application) through architectural design to promote patient recovery.
- Cluster #7 (research literature): It covers review citations of the existing research and summarizes and generalizes important research methods in the field of hospital design, indicating that this topic is mostly directed towards methodology and literature system construction.
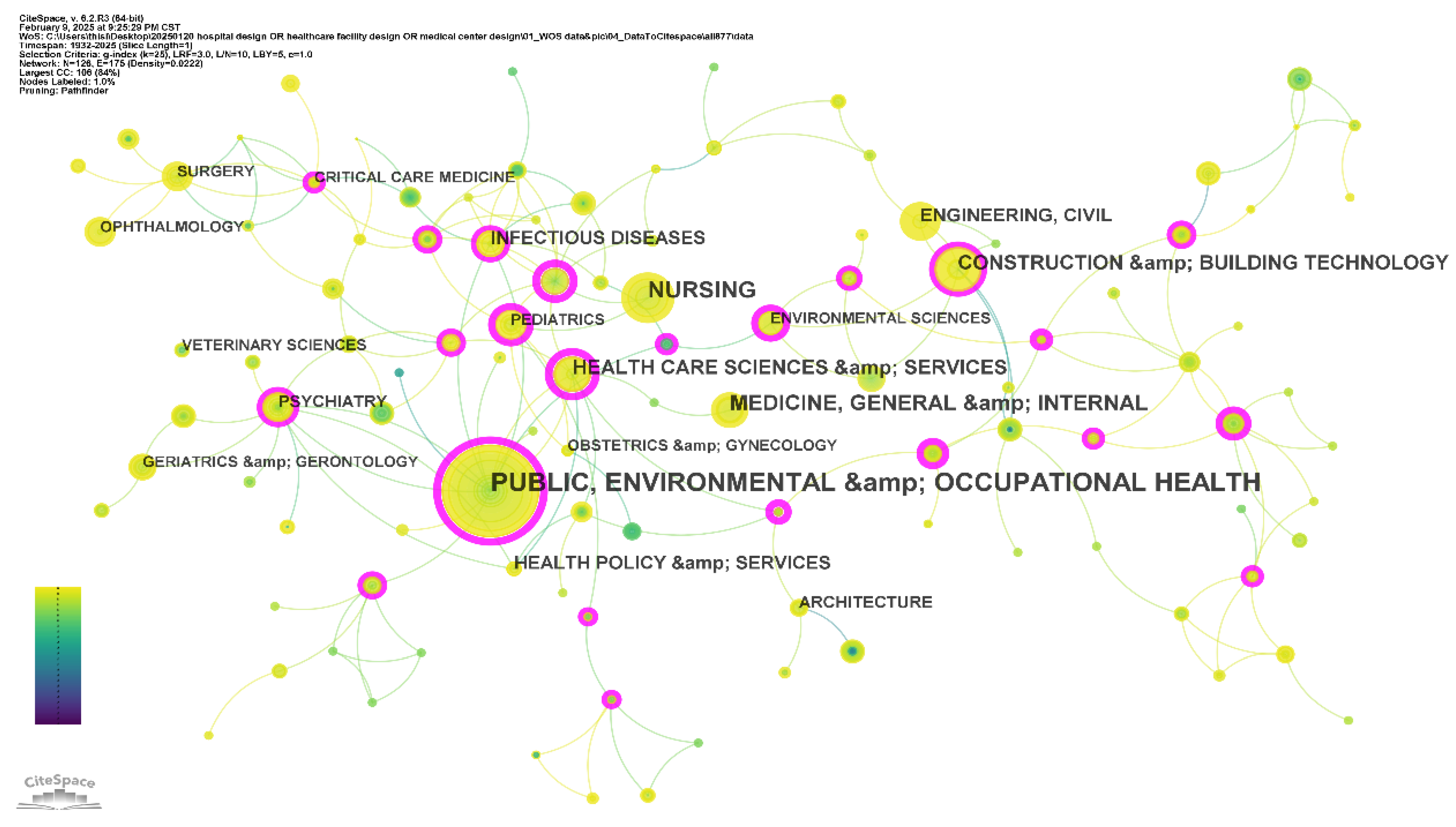
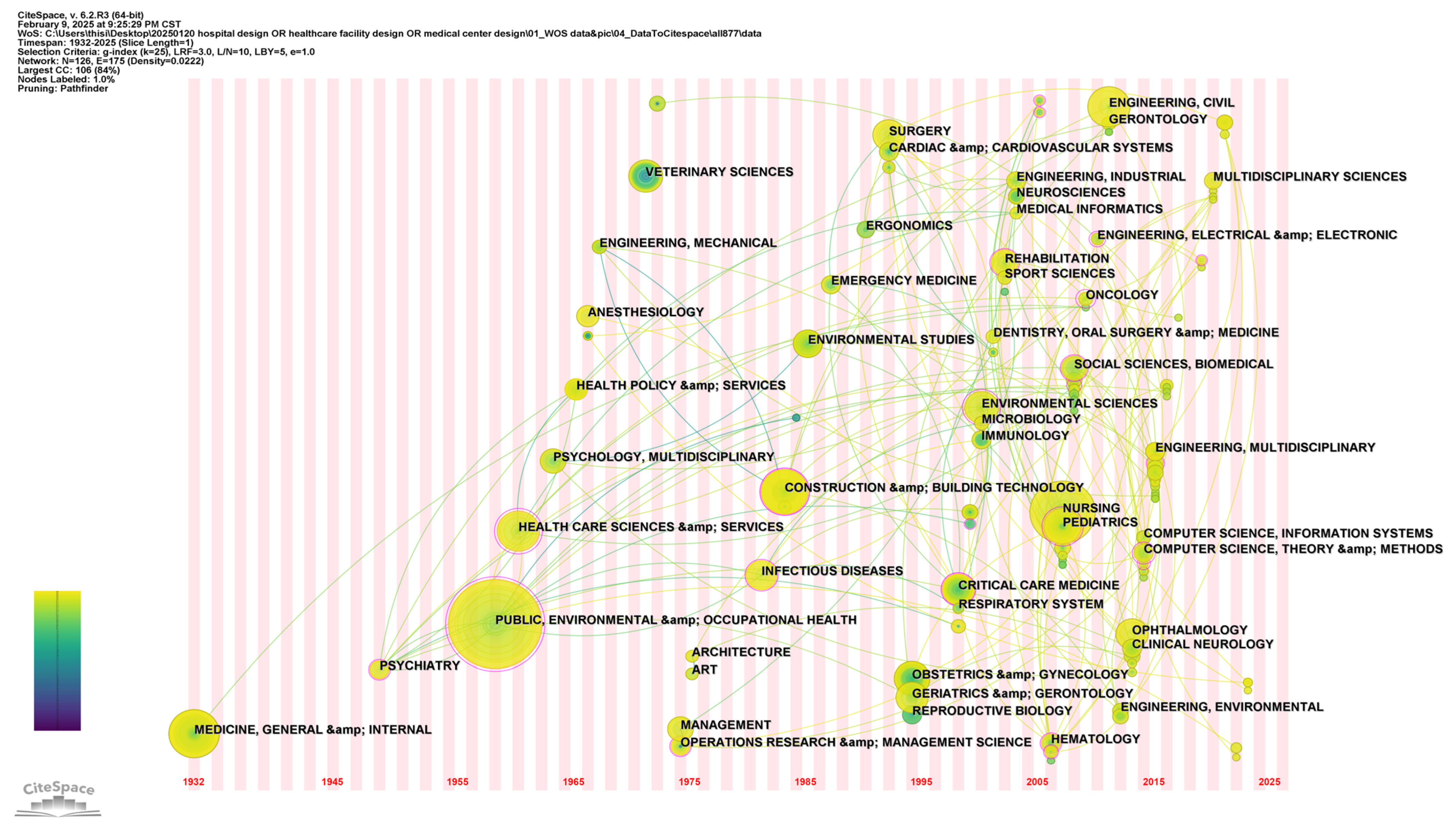
4.3.2. Analysis of the Subject Categories
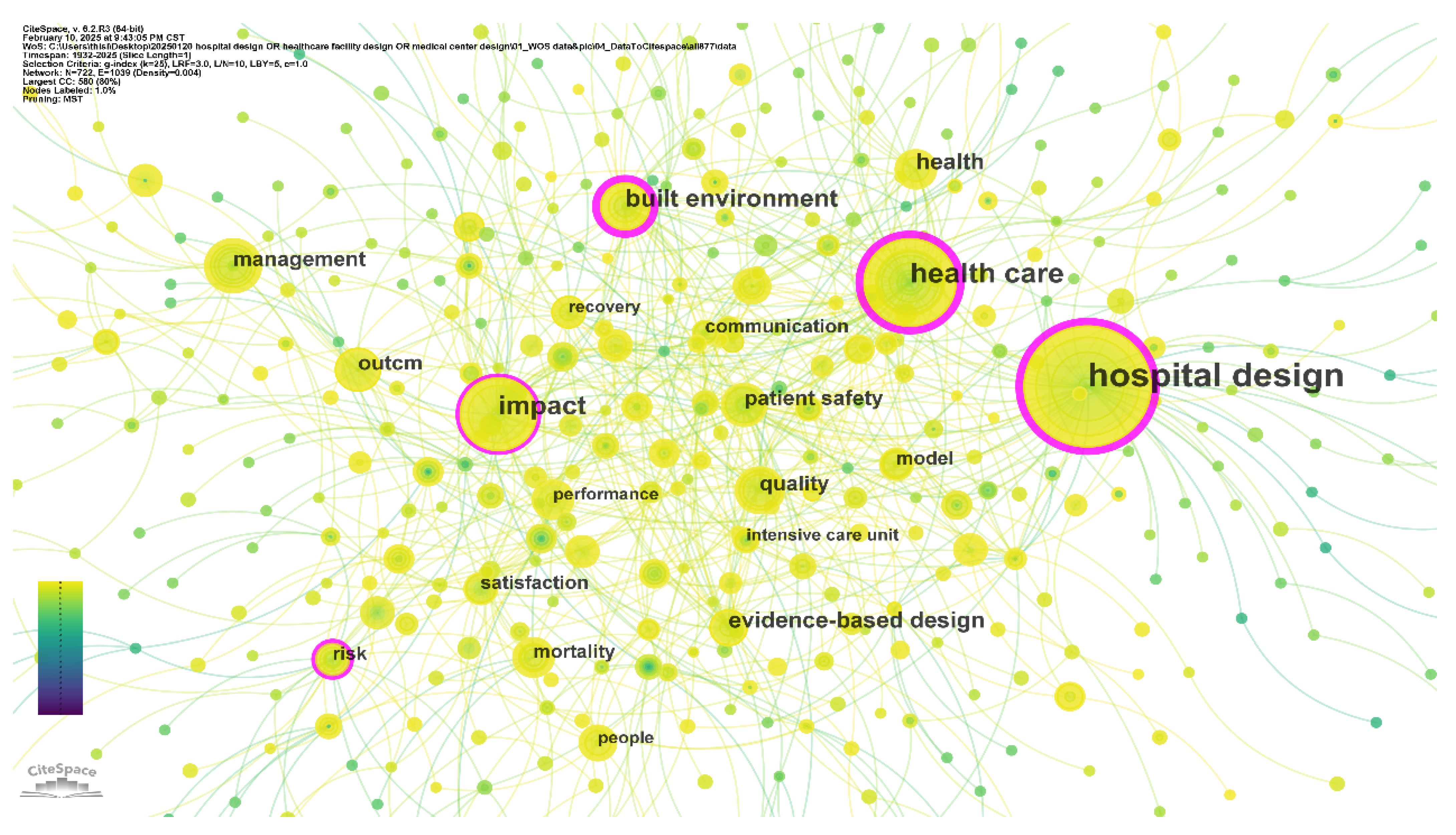
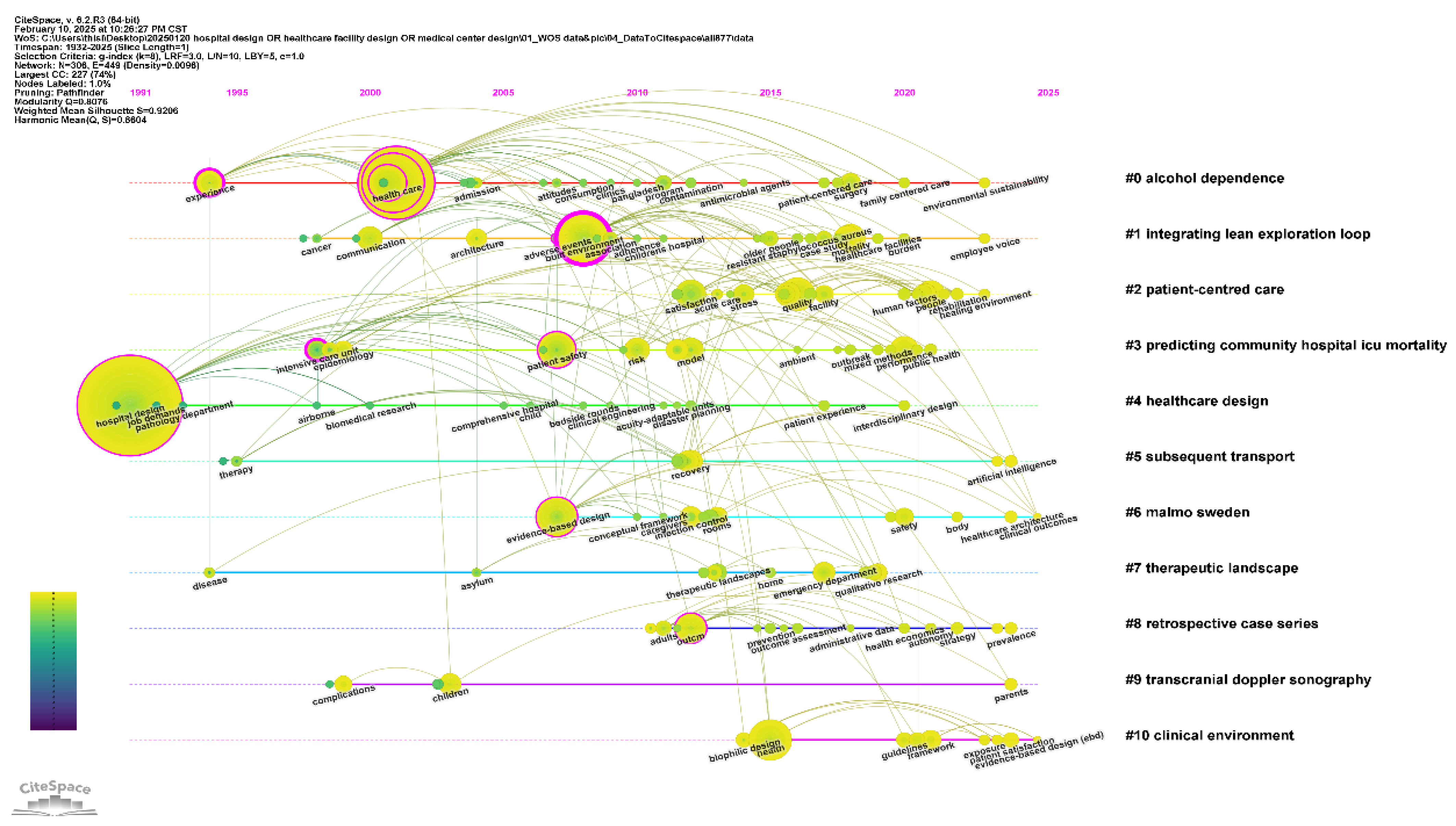
4.4. Research Topics, Hotspots, and Future Trends—Analysis of the Keywords
- Cluster #0 and Cluster #1 are the largest, reflecting their significant aggregation and high research density.
- Cluster #2 highlights terms such as “hospital design”, “physical environment”, and “treatment context”, emphasizing the growing importance of patient-centered design and experiential outcomes.
- Cluster #4 includes terms like “energy efficiency” and “pollution prevention”, signaling the rise of green hospitals and sustainable building practices.
- Cluster #10 emphasizes “biophilic design parameters” and “natural material”, illustrating the trend of integrating natural elements into healthcare spaces.
- Smaller clusters capture more specialized themes, such as population-specific psychological healing and the design of psychiatric hospital environments, pointing to the diversification of research interests.
4.5. Summary of Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ulrich, R.S.; Bogren, L.; Gardiner, S.K.; Lundin, S. Psychiatric Ward Design Can Reduce Aggressive Behavior. J. Environ. Psychol. 2018, 57, 53–66. [Google Scholar] [CrossRef]
- Stiller, A.; Salm, F.; Bischoff, P.; Gastmeier, P. Relationship between Hospital Ward Design and Healthcare-Associated Infection Rates: A Systematic Review and Meta-Analysis. Antimicrob. Resist. Infect. Control 2016, 5, 51. [Google Scholar] [CrossRef]
- Rechel, B.; Wright, S.; Edwards, N.; Dowdeswell, B.; McKee, M. Investing in Hospitals of the Future; World Health Organization, Regional Office for Europe: Copenhagen, Denmark, 2009; ISBN 978-92-890-4304-5. [Google Scholar]
- van de Glind, I.; de Roode, S.; Goossensen, A. Do Patients in Hospitals Benefit from Single Rooms? A Literature Review. Health Policy 2007, 84, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Dettenkofer, M.; Seegers, S.; Antes, G.; Motschall, E.; Schumacher, M.; Daschner, F.D. Does the Architecture of Hospital Facilities Influence Nosocomial Infection Rates? A Systematic Review. Infect. Control Hosp. Epidemiol. 2004, 25, 21–25. [Google Scholar] [CrossRef]
- Becker, F. Nursing Unit Design and Communication Patterns: What Is “Real” Work? HERD Health Environ. Res. Des. J. 2007, 1, 58–62. [Google Scholar] [CrossRef]
- Hospitals. Available online: https://www.who.int/health-topics/hospitals (accessed on 22 July 2025).
- World Health Organization Ebola and Marburg Treatment Centres. Facility Design and Construction Standards for Preparing for and Responding to Outbreaks; World Health Organization: Geneva, Switzerland, 2024; ISBN 978-92-4-009008-8. [Google Scholar]
- Rapid Hospital Readiness Checklist: Interim Guidance. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-hospital-readiness-checklist-2020.1 (accessed on 26 July 2025).
- Barasa, E.; Mbau, R.; Gilson, L. What Is Resilience and How Can It Be Nurtured? A Systematic Review of Empirical Literature on Organizational Resilience. Int. J. Health Policy Manag. 2018, 7, 491–503. [Google Scholar] [CrossRef]
- Pereira, L.M.; Ornstein, S.W. A Systematic Literature Review on Healthcare Facility Evaluation Methods. HERD Health Environ. Res. Des. J. 2023, 16, 338–361. [Google Scholar] [CrossRef]
- Brambilla, A.; Brambilla, A.; Capolongo, S. Evidence Based Hospital Design. A Literature Review of the Recent Publications about the EBD Impact of Built Environment on Hospital Occupants’ and Organizational Outcomes. Ann. Ig. Med. Prev. Comunità 2019, 31, 165–180. [Google Scholar] [CrossRef]
- Laursen, J.; Danielsen, A.; Rosenberg, J. Effects of Environmental Design on Patient Outcome: A Systematic Review. HERD Health Environ. Res. Des. J. 2014, 7, 108–119. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, R. Effects of Healthcare Environmental Design on Medical Outcomes. In Proceedings of the Design and Health: Proceedings of the Second International Conference on Health and Design, Stockholm, Sweden, 21–24 June 2001. [Google Scholar]
- Inalhan, G.; Golembiewski, J.A. Start Making Sense Applying a Salutogenic Model to Architectural Design for Psychiatric Care. Facilities 2010, 28, 100–117. [Google Scholar] [CrossRef]
- Han, K.-T.; Ruan, L.-W.; Liao, L.-S. Effects of Indoor Plants on Human Functions: A Systematic Review with Meta-Analyses. Int. J. Environ. Res. Public Health 2022, 19, 7454. [Google Scholar] [CrossRef]
- Miola, L.; Boldrini, A.; Pazzaglia, F. The Healing Power of Nature. Biophilic Design Applied to Healthcare Facilities. Curr. Opin. Psychol. 2025, 64, 102049. [Google Scholar] [CrossRef]
- Elf, M.; Lipson-Smith, R.; Kylén, M.; Saa, J.P.; Sturge, J.; Miedema, E.; Nordin, S.; Bernhardt, J.; Anåker, A. A Systematic Review of Research Gaps in the Built Environment of Inpatient Healthcare Settings. HERD Health Environ. Res. Des. J. 2024, 17, 372–394. [Google Scholar] [CrossRef] [PubMed]
- Deng, L.; Romainoor, N.H. A Bibliometric Analysis of Published Literature on Healthcare Facilities’ Wayfinding Research from 1974 to 2020. Heliyon 2022, 8, e10723. [Google Scholar] [CrossRef]
- Chen, C. Science Mapping: A Systematic Review of the Literature. J. Data Inf. Sci. 2017, 2, 1–40. [Google Scholar] [CrossRef]
- Chen, C. CiteSpace II: Detecting and Visualizing Emerging Trends and Transient Patterns in Scientific Literature. J. Am. Soc. Inf. Sci. Technol. 2006, 57, 359–377. [Google Scholar] [CrossRef]
- Aria, M.; Cuccurullo, C. Bibliometrix: An R-Tool for Comprehensive Science Mapping Analysis. J. Informetr. 2017, 11, 959–975. [Google Scholar] [CrossRef]
- Zhao, X.; Zuo, J.; Wu, G.; Huang, C. A Bibliometric Review of Green Building Research 2000–2016. Archit. Sci. Rev. 2019, 62, 74–88. [Google Scholar] [CrossRef]
- Jia, B.; Chen, Y.; Wu, J. Bibliometric Analysis and Research Trend Forecast of Healthy Urban Planning for 40 Years (1981–2020). Int. J. Environ. Res. Public Health 2021, 18, 9444. [Google Scholar] [CrossRef]
- Li, Y.; Rong, Y.; Ahmad, U.M.; Wang, X.; Zuo, J.; Mao, G. A Comprehensive Review on Green Buildings Research: Bibliometric Analysis during 1998–2018. Environ. Sci. Pollut. Res. 2021, 28, 46196–46214. [Google Scholar] [CrossRef]
- WHO Regional Office for the Western Pacific. District Hospitals: Guidelines for Development, 2nd ed.; WHO Regional Office for the Western Pacific: Manila, Philippines, 1996; ISBN 978-92-9061-117-2. [Google Scholar]
- WHO Regional Office for the Western Pacific. Regional Action Framework on Improving Hospital Planning and Management in the Western Pacific; WHO Regional Office for the Western Pacific: Manila, Philippines, 2020; ISBN 978-92-9061-893-5. [Google Scholar]
- Hospitals of the Future: A Technical Brief on Re-Thinking the Architecture of Hospitals. Available online: https://www.who.int/europe/publications/i/item/WHO-EURO-2023-7525-47292-69380 (accessed on 26 July 2025).
- Hospital Facilities Design Code, 2022 (FGI Hospital, 2022). Available online: https://up.codes/code/fgi-guidelines-for-design-and-construction-of-hospitals-2022 (accessed on 23 July 2025).
- Program Support Center (PSC). Chapter 8. HHS Facility Design and Construction. Available online: https://www.hhs.gov/about/hhs-manuals/hhs-facilities-manual/hhs-facility-design-construction/index.html (accessed on 23 July 2025).
- NHS England. Health Building Note 00-01: General Design Guidance for Healthcare Buildings. Available online: https://www.england.nhs.uk/publication/designing-health-and-community-care-buildings-hbn-00-01/ (accessed on 23 July 2025).
- NSQHS Standards Guide for Hospitals|Australian Commission on Safety and Quality in Health Care. Available online: https://www.safetyandquality.gov.au/publications-and-resources/resource-library/nsqhs-standards-guide-hospitals (accessed on 23 July 2025).
- Chunyang, Z.; Peng, D.; Wenyu, Z. Consideration of Green Hospital Building Planning and Design in China. In Proceedings of the Conference: The Symposium on Healthcare Architecture in Asia 2013, Shanghai, China, 26–27 February 2013. [Google Scholar]
- Douglas, C.H.; Douglas, M.R. Patient-Centred Improvements in Health-Care Built Environments: Perspectives and Design Indicators. Health Expect. 2005, 8, 264–276. [Google Scholar] [CrossRef]
- Zborowsky, T.; Kreitzer, M.J. Creating Optimal Healing Environments in a Health Care Setting. Minn. Med. 2008, 91, 35–38. [Google Scholar]
- Nejati, A.; Shepley, M.; Rodiek, S.; Lee, C.; Varni, J. Restorative Design Features for Hospital Staff Break Areas: A Multi-Method Study. HERD Health Environ. Res. Des. J. 2016, 9, 16–35. [Google Scholar] [CrossRef] [PubMed]
- Zhu, X.; Shepley, M. Assessing Preferences and Perceived Restorative Qualities of Break Spaces for Nurses in China. HERD Health Environ. Res. Des. J. 2022, 15, 126–142. [Google Scholar] [CrossRef] [PubMed]
- Architectural Spatial Layout Design for Hospitals: A Review. J. Build. Eng. 2024, 97, 110835. [CrossRef]
- Ulrich, R.S.; Zimring, C.; Zhu, X.; DuBose, J.; Seo, H.-B.; Choi, Y.-S.; Quan, X.; Joseph, A. A Review of the Research Literature on Evidence-Based Healthcare Design. HERD Health Environ. Res. Des. J. 2008, 1, 61–125. [Google Scholar] [CrossRef]
- Ulrich, R.S. View through a Window May Influence Recovery from Surgery. Science 1984, 224, 420–421. [Google Scholar] [CrossRef]
- Zimring, C.; Joseph, A.; Choudhary, R. The Role of the Physical Environment in the Hospital of the 21st Century: A Once-in-a-Lifetime Opportunity; The Center for Health Design: Concord, CA, USA, 2004; Volume 311. [Google Scholar]
- Boubekri, M. Daylighting, Architecture and Health; Routledge: London, UK, 2008; ISBN 978-0-08-094071-7. [Google Scholar]
- Perkins, L.B. Book Review: A Visual Reference for Evidence-Based Design. HERD Health Environ. Res. Des. J. 2008, 1, 141–143. [Google Scholar] [CrossRef]
- Boby, P. A Review of Post Pandemic Healthcare Design. Evol. Sch. 2021. [Google Scholar] [CrossRef]
- Hamilton, D.K.; Watkins, D.H. Evidence-Based Design for Multiple Building Types; Wiley: Hoboken, NJ, USA, 2009; ISBN 978-0-470-12934-0. [Google Scholar]
- Li, Y.; Huang, X.; Yu, I.T.S.; Wong, T.W.; Qian, H. Role of Air Distribution in SARS Transmission during the Largest Nosocomial Outbreak in Hong Kong. Indoor Air 2005, 15, 83–95. [Google Scholar] [CrossRef]
- Joseph, A.; Rashid, M. The Architecture of Safety: Hospital Design. Curr. Opin. Crit. Care 2007, 13, 714. [Google Scholar] [CrossRef]
- Bagaria, J.; Heggie, C.; Abrahams, J.; Murray, V. Evacuation and Sheltering of Hospitals in Emergencies: A Review of International Experience. Prehosp. Disaster Med. 2009, 24, 461–467. [Google Scholar] [CrossRef]
- Morag, I.; Heylighen, A.; Pintelon, L. Evaluating the Inclusivity of Hospital Wayfinding Systems for People with Diverse Needs and Abilities. J. Health Serv. Res. Policy 2016, 21, 243–248. [Google Scholar] [CrossRef]
- Dilani, A. Psychosocially Supportive Design--Scandinavian Health Care Design. World Hosp. Health Serv. 2001, 37, 20–24. [Google Scholar]
- A, D. A New Paradigm of Design and Health in Hospital Planning. World Hosp. Health Serv. Off. J. Int. Hosp. Fed. 2005, 41, 7–21. [Google Scholar]
- Dijkstra, K.; Pieterse, M.; Pruyn, A. Physical Environmental Stimuli That Turn Healthcare Facilities into Healing Environments through Psychologically Mediated Effects: Systematic Review. J. Adv. Nurs. 2006, 56, 166–181. [Google Scholar] [CrossRef] [PubMed]
- Thompson, D.R.; Hamilton, D.K.; Cadenhead, C.D.; Swoboda, S.M.; Schwindel, S.M.; Anderson, D.C.; Schmitz, E.V.; St. Andre, A.C.; Axon, D.C.; Harrell, J.W.; et al. Guidelines for Intensive Care Unit Design*. Crit. Care Med. 2012, 40, 1586. [Google Scholar] [CrossRef] [PubMed]
- Innovative Designs for the Smart ICU. Chest 2014, 145, 646–658. [CrossRef]
- Verderber, S.; Gray, S.; Suresh-Kumar, S.; Kercz, D.; Parshuram, C. Intensive Care Unit Built Environments: A Comprehensive Literature Review (2005–2020). HERD Health Environ. Res. Des. J. 2021, 14, 368–415. [Google Scholar] [CrossRef] [PubMed]
- Gokeler, A.; McKeon, P.O.; Hoch, M.C. Shaping the Functional Task Environment in Sports Injury Rehabilitation: A Framework to Integrate Perceptual-Cognitive Training in Rehabilitation. Athl. Train. Sports Health Care 2020, 12, 283–292. [Google Scholar] [CrossRef]
- Fadda, J. Quality of Healthcare: A Review of the Impact of the Hospital Physical Environment on Improving Quality of Care. In Sustainable Building for a Cleaner Environment: Selected Papers from the World Renewable Energy Network’s Med Green Forum 2017; Sayigh, A., Ed.; Springer International Publishing: Cham, Switzerland, 2019; pp. 217–253. ISBN 978-3-319-94595-8. [Google Scholar]
- Wood, L.C.; Wang, C.; Abdul-Rahman, H.; Jamal Abdul-Nasir, N.S. Green Hospital Design: Integrating Quality Function Deployment and End-User Demands. J. Clean. Prod. 2016, 112, 903–913. [Google Scholar] [CrossRef]
- Li, Y.; Pan, X.; Han, Y.; Taylor, J.E. Sustainable Healthcare Facilities: A Scoping Review. J. Constr. Eng. Manag. 2021, 147, 03121007. [Google Scholar] [CrossRef]
- Soares, A.L.; Buttigieg, S.C.; Bak, B.; McFadden, S.; Hughes, C.; McClure, P.; Couto, J.G.; Bravo, I. A Review of the Applicability of Current Green Practices in Healthcare Facilities. Int. J. Health Policy Manag. 2023, 12, 6947. [Google Scholar] [CrossRef] [PubMed]
- Lawson, B. Healing Architecture. Arts Health 2010, 2, 95–108. [Google Scholar] [CrossRef]
- Sosa, A.V. Healing Architecture and Evidence-Based Design. Available online: https://www.buildinghealth.eu/wp-content/uploads/2020/12/DOM-Publishers_-Healing-Architecture-and-EbD_-Alvaro-Valera-sosa.pdf (accessed on 27 July 2025).
- Huisman, E.; Morales, E.; van Hoof, J.; Kort, H.S.M. Healing Environment: A Review of the Impact of the Physical Environmental Factors on Users. Build. Environ. 2012, 58, 70–80. [Google Scholar] [CrossRef]
- Golembiewski, J.A. Salutogenic Architecture in Healthcare Settings. In The Handbook of Salutogenesis; Mittelmark, M.B., Sagy, S., Eriksson, M., Bauer, G.F., Pelikan, J.M., Lindström, B., Espnes, G.A., Eds.; Springer: Cham, Switzerland, 2017; ISBN 978-3-319-04599-3. [Google Scholar]
- Golembiewski, J.A. Salutogenic Architecture. In The Handbook of Salutogenesis; Mittelmark, M.B., Bauer, G.F., Vaandrager, L., Pelikan, J.M., Sagy, S., Eriksson, M., Lindström, B., Meier Magistretti, C., Eds.; Springer: Cham, Switzerland, 2022; ISBN 978-3-030-79514-6. [Google Scholar]
- Dilani, A. Psychosocially Supportive Design: A Salutogenic Approach to the Design of the Physical Environment. Des. Health Sci. Rev. 2008, 1, 47–55. [Google Scholar]
- Hwang, K.-E.; Kim, I. Post-COVID-19 Modular Building Review on Problem-Seeking Framework: Function, Form, Economy, and Time. J. Comput. Des. Eng. 2022, 9, 1369–1387. [Google Scholar] [CrossRef]
- Gao, M.-Z.; Chou, Y.-H.; Chang, Y.-Z.; Pai, J.-Y.; Bair, H.; Pai, S.; Yu, N.-C. Designing Mobile Epidemic Prevention Medical Stations for the COVID-19 Pandemic and International Medical Aid. Int. J. Environ. Res. Public Health 2022, 19, 9959. [Google Scholar] [CrossRef] [PubMed]
- Optimized Mechanism for Fast Removal of Infectious Pathogen-Laden Aerosols in the Negative-Pressure Unit. J. Hazard. Mater. 2022, 435, 128978. [CrossRef]
- Kucan, G.; Tan, T.; Grossmann, D.; Graser, K.; Hall, D.M. Sustainable Future-Proof Healthcare Facilities: Modular and Adaptable Design Approach. J. Manag. Eng. 2024, 40, 04024053. [Google Scholar] [CrossRef]
- Gatheeshgar, P.; Poologanathan, K.; Gunalan, S.; Shyha, I.; Sherlock, P.; Rajanayagam, H.; Nagaratnam, B. Development of Affordable Steel-Framed Modular Buildings for Emergency Situations (Covid-19). Structures 2021, 31, 862–875. [Google Scholar] [CrossRef]
- Pan, W.; Zhang, Z. Evaluating Modular Healthcare Facilities for COVID-19 Emergency Response—A Case of Hong Kong. Buildings 2022, 12, 1430. [Google Scholar] [CrossRef]
- Cho, J.; Jang, S.; Song, J. Onsite Measurement and Dilution-Based Infection Risk Assessment for a New Mobile Negative Pressure Isolation Room (MNPIR) as a Solution to Minimize Cross-Infection. Sustain. Cities Soc. 2023, 95, 104583. [Google Scholar] [CrossRef]
- Whitelaw, S.; Mamas, M.A.; Topol, E.; Spall, H.G.C.V. Applications of Digital Technology in COVID-19 Pandemic Planning and Response. Lancet Digit. Health 2020, 2, e435–e440. [Google Scholar] [CrossRef] [PubMed]
- Maramba, I.D.; Jones, R.; Austin, D.; Edwards, K.; Meinert, E.; Chatterjee, A. The Role of Health Kiosks: Scoping Review. JMIR Med. Inform. 2022, 10, e26511. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Lu, L.; Shi, J.; Zhang, X.; Fan, H.; Fan, B.; Qu, B.; Lv, Q.; Hou, S. Application and Prospect of a Mobile Hospital in Disaster Response. Disaster Med. Public Health Prep. 2020, 14, 377–383. [Google Scholar] [CrossRef]
- COVID-19: Reduction of Airborne Transmission Needs Paradigm Shift in Ventilation. Build. Environ. 2020, 186, 107336. [CrossRef]
- Knutsen Glette, M.; Ludlow, K.; Wiig, S.; Bates, D.W.; Austin, E.E. Resilience Perspective on Healthcare Professionals’ Adaptations to Changes and Challenges Resulting from the COVID-19 Pandemic: A Meta-Synthesis. BMJ Open 2023, 13, e071828. [Google Scholar] [CrossRef] [PubMed]
- Smyth, E. Adapting the ICU Model to Deliver Flexible, Innovative and Personalised Care in a Post-Pandemic Society. 15 March 2024. Available online: https://dapp.orvium.io/deposits/626bf636cf1249c7f9f02b62/view (accessed on 27 July 2025).
- Zhao, Y.; Zhan, Q.; Xu, T. Biophilic Design as an Important Bridge for Sustainable Interaction between Humans and the Environment: Based on Practice in Chinese Healthcare Space. Comput. Math. Methods Med. 2022, 2022, 8184534. [Google Scholar] [CrossRef]
- Zhong, L.; Lopez, D.; Pei, S.; Gao, J. Healthcare System Resilience and Adaptability to Pandemic Disruptions in the United States. Nat. Med. 2024, 30, 2311–2319. [Google Scholar] [CrossRef]
- Capolongo, S.; Gola, M.; Brambilla, A.; Morganti, A.; Mosca, E.I.; Barach, P. COVID-19 and Healthcare Facilities: A Decalogue of Design Strategies for Resilient Hospitals. Acta Biomed. 2020, 91, 50–60. [Google Scholar] [CrossRef]
- Haq, S.; Luo, Y. Space Syntax in Healthcare Facilities Research: A Review. HERD Health Environ. Res. Des. J. 2012, 5, 98–117. [Google Scholar] [CrossRef]
- Experimental Study and CFD Modelling of Four-Bed Hospital Ward with All-Air Wall Induction Unit for Air-Conditioning. Build. Environ. 2022, 222, 109388. [CrossRef]
- Shultz, J.; Jha, R. Using Virtual Reality (VR) Mock-Ups for Evidence-Based Healthcare Facility Design Decisions. Int. J. Environ. Res. Public Health 2021, 18, 11250. [Google Scholar] [CrossRef] [PubMed]
- Cambra-Rufino, L. EURAU 18 Proceedings: Designing a Post-Occupancy Evaluation (POE) Tool for Hospitals. 2018. Available online: https://www.researchgate.net/publication/328686504_EURAU_18_Proceedings_Designing_a_Post-Occupancy_Evaluation_POE_Tool_for_Hospitals (accessed on 27 July 2025).
- Wen, Y.; Tang, L.; Ho, D. A BIM-Based Space-Oriented Solution for Hospital Facilities Management. Facilities 2021. ahead-of-print. [Google Scholar] [CrossRef]
- Han, Y.; Li, Y.; Li, Y.; Yang, B.; Cao, L. Digital Twinning for Smart Hospital Operations: Framework and Proof of Concept. Technol. Soc. 2023, 74, 102317. [Google Scholar] [CrossRef]
- Jung, D.; Kim, D.I.; Kim, N. Bringing Nature into Hospital Architecture: Machine Learning-Based EEG Analysis of the Biophilia Effect in Virtual Reality. J. Environ. Psychol. 2023, 89, 102033. [Google Scholar] [CrossRef]
- Tan, T.; Mills, G.; Papadonikolaki, E.; Xu, Y.; Chen, K. Building Information Modelling in Healthcare Design and Construction: A Bibliometric Review and Systematic Review. In Advances in Information Technology in Civil and Building Engineering; Skatulla, S., Beushausen, H., Eds.; Springer International Publishing: Cham, Switzerland, 2024; pp. 401–415. [Google Scholar]
- van Eck, N.J.; Waltman, L. Software Survey: VOSviewer, a Computer Program for Bibliometric Mapping. Scientometrics 2010, 84, 523–538. [Google Scholar] [CrossRef]
- Yang, W.; Liu, Y.; Zeng, T.; Wang, Y.; Hao, X.; Yang, W.; Wang, H. Research Focus and Thematic Trends in Magnet Hospital Research: A Bibliometric Analysis of the Global Publications. J. Adv. Nurs. 2021, 77, 2012–2025. [Google Scholar] [CrossRef] [PubMed]
- Philip, A.M.; Prasannavenkatesan, S.; Mustafee, N. Simulation Modelling of Hospital Outpatient Department: A Review of the Literature and Bibliometric Analysis. SIMULATION 2023, 99, 573–597. [Google Scholar] [CrossRef]
- Nepomuceno, T.C.C.; Piubello Orsini, L.; de Carvalho, V.D.H.; Poleto, T.; Leardini, C. The Core of Healthcare Efficiency: A Comprehensive Bibliometric Review on Frontier Analysis of Hospitals. Healthcare 2022, 10, 1316. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Ravi, P. Lean Six-Sigma (LSS) Applications in Hospitals: A Decade (2011–2020) Bibliometric Analysis. Int. J. Product. Perform. Manag. 2023, 72, 2270–2291. [Google Scholar] [CrossRef]
- Wahyuni, S.; Pranata, S.; Setiaprabhawa, F.B.; Maftuchah, L. Exploring the Trend of Technology Use and Innovation in Health Care Service in Hospitals through a Bibliometric Analysis. Babcock Univ. Med. J. 2024, 7, 51–63. [Google Scholar] [CrossRef]
- Verderber, S. Innovations in Hospital Architecture; Routledge: London, UK, 2010; ISBN 978-1-136-99978-9. [Google Scholar]
- Becker, F.; Parsons, K.S. Hospital Facilities and the Role of Evidence-based Design. J. Facil. Manag. 2007, 5, 263–274. [Google Scholar] [CrossRef]
- Kobus, R.L.; Skaggs, R.L.; Bobrow, M.; Thomas, J.; Payette, T.M.; Kliment, S.A. Building Type Basics for Healthcare Facilities; John Wiley & Sons: Hoboken, NJ, USA, 2008; ISBN 978-0-470-13541-9. [Google Scholar]
- Schweitzer, M.; Gilpin, L.; Frampton, S. Healing Spaces: Elements of Environmental Design That Make an Impact on Health. J. Altern. Complement. Med. 2004, 10 (Suppl. 1), S71–S83. [Google Scholar] [CrossRef]
- Chen, C.; Song, M. Visualizing a Field of Research: A Methodology of Systematic Scientometric Reviews. PLoS ONE 2019, 14, e0223994. [Google Scholar] [CrossRef]
- Niazi, M.A. Review of “CiteSpace: A Practical Guide For Mapping Scientific Literature” by Chaomei Chen. Complex Adapt. Syst. Model. 2016, 4, 23. [Google Scholar] [CrossRef]
- Liu, W. The Data Source of This Study Is Web of Science Core Collection? Not Enough. Scientometrics 2019, 121, 1815–1824. [Google Scholar] [CrossRef]
- Chen, C. How to Use CiteSpace (c) 2015–2020. 2020. Available online: https://www.researchgate.net/publication/320699133_How_to_Use_CiteSpace_c_2015-2020 (accessed on 27 July 2025).
- Chen, C.; Ibekwe-SanJuan, F.; Hou, J. The Structure and Dynamics of Cocitation Clusters: A Multiple-Perspective Cocitation Analysis. J. Am. Soc. Inf. Sci. Technol. 2010, 61, 1386–1409. [Google Scholar] [CrossRef]
- Mongeon, P.; Paul-Hus, A. The Journal Coverage of Web of Science and Scopus: A Comparative Analysis. Scientometrics 2016, 106, 213–228. [Google Scholar] [CrossRef]
- Asubiaro, T.; Onaolapo, S.; Mills, D. Regional Disparities in Web of Science and Scopus Journal Coverage. Scientometrics 2024, 129, 1469–1491. [Google Scholar] [CrossRef]
- Liu, W.; Ni, R.; Hu, G. Web of Science Core Collection’s Coverage Expansion: The Forgotten Arts & Humanities Citation Index? Scientometrics 2024, 129, 933–955. [Google Scholar] [CrossRef]
- Liu, F. Retrieval Strategy and Possible Explanations for the Abnormal Growth of Research Publications: Re-Evaluating a Bibliometric Analysis of Climate Change. Scientometrics 2023, 128, 853–859. [Google Scholar] [CrossRef]
- Draper, N.R.; Smith, H. Applied Regression Analysis; John Wiley & Sons: Hoboken, NJ, USA, 1998; ISBN 978-0-471-17082-2. [Google Scholar]
- Liu, W.; Hu, G.; Li, T. Missing Author Address Information in Web of Science—An Explorative Study. J. Informetr. 2018, 12, 985–997. [Google Scholar] [CrossRef]
- Barthélemy, M. Betweenness Centrality in Large Complex Networks. Eur. Phys. J. B 2004, 38, 163–168. [Google Scholar] [CrossRef]
- Hassan, W.; Duarte, A.E. Bibliometric Analysis: A Few Suggestions. Curr. Probl. Cardiol. 2024, 49, 102640. [Google Scholar] [CrossRef]
- Chen, C. CiteSpace: A Practical Guide for Mapping Scientific Literature; Nova Science Publishers: Hauppauge, NY, USA, 2016; ISBN 978-1-5361-0280-2. [Google Scholar]
- Aksnes, D.W.; Langfeldt, L.; Wouters, P. Citations, Citation Indicators, and Research Quality: An Overview of Basic Concepts and Theories. SAGE Open 2019. [Google Scholar] [CrossRef]
- Priestley, G.; Watson, W.; Rashidian, A.; Mozley, C.; Russell, D.; Wilson, J.; Cope, J.; Hart, D.; Kay, D.; Cowley, K.; et al. Introducing Critical Care Outreach: A Ward-Randomised Trial of Phased Introduction in a General Hospital. Intensive Care Med. 2004, 30, 1398–1404. [Google Scholar] [CrossRef] [PubMed]
- Shaughnessy, M.K.; Micielli, R.L.; DePestel, D.D.; Arndt, J.; Strachan, C.L.; Welch, K.B.; Chenoweth, C.E. Evaluation of Hospital Room Assignment and Acquisition of Clostridium Difficile Infection. Infect. Control Hosp. Epidemiol. 2011, 32, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Lankford, M.G.; Zembower, T.R.; Trick, W.E.; Hacek, D.M.; Noskin, G.A.; Peterson, L.R. Influence of Role Models and Hospital Design on Hand Hygiene of Healthcare Workers. Emerg. Infect. Dis. 2003, 9, 217–223. [Google Scholar] [CrossRef]
- Gesler, W.; Bell, M.; Curtis, S.; Hubbard, P.; Francis, S. Therapy by Design: Evaluating the UK Hospital Building Program. Health Place 2004, 10, 117–128. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, R.S.; Berry, L.L.; Quan, X.; Parish, J.T. A Conceptual Framework for the Domain of Evidence-Based Design. HERD Health Environ. Res. Des. J. 2010, 4, 95–114. [Google Scholar] [CrossRef]
- Warshaw, G.A.; Moore, J.T.; Friedman, S.W.; Currie, C.T.; Kennie, D.C.; Kane, W.J.; Mears, P.A. Functional Disability in the Hospitalized Elderly. JAMA 1982, 248, 847–850. [Google Scholar] [CrossRef] [PubMed]
- McGain, F.; Naylor, C. Environmental Sustainability in Hospitals—A Systematic Review and Research Agenda. J. Health Serv. Res. Policy 2014, 19, 245–252. [Google Scholar] [CrossRef]
- Curtis, S.; Gesler, W.; Fabian, K.; Francis, S.; Priebe, S. Therapeutic Landscapes in Hospital Design: A Qualitative Assessment by Staff and Service Users of the Design of a New Mental Health Inpatient Unit. Environ. Plan. C Gov. Policy 2007, 25, 591–610. [Google Scholar] [CrossRef]
- Lip, G.Y.; Tean, K.N.; Dunn, F.G. Treatment of Atrial Fibrillation in a District General Hospital. Br. Heart J. 1994, 71, 92–95. [Google Scholar] [CrossRef]
- Chaudhury, H.; Mahmood, A.; Valente, M. Advantages and Disadvantages of Single-Versus Multiple-Occupancy Rooms in Acute Care Environments. Environ. Behav. 2005, 37, 760–786. [Google Scholar] [CrossRef]
- Dalke, H.; Little, J.; Niemann, E.; Camgoz, N.; Steadman, G.; Hill, S.; Stott, L. Colour and Lighting in Hospital Design. Opt. Laser Technol. 2006, 38, 343–365. [Google Scholar] [CrossRef]
- Boyack, K.W.; Klavans, R. Co-Citation Analysis, Bibliographic Coupling, and Direct Citation: Which Citation Approach Represents the Research Front Most Accurately? J. Am. Soc. Inf. Sci. Technol. 2010, 61, 2389–2404. [Google Scholar] [CrossRef]
- Small, H. Co-Citation in the Scientific Literature: A New Measure of the Relationship between Two Documents. J. Am. Soc. Inf. Sci. 1973, 24, 265–269. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qual. Res. Psychol. 2021, 18, 328–352. [Google Scholar] [CrossRef]
- Taylor, E.; Card, A.J.; Piatkowski, M. Single-Occupancy Patient Rooms: A Systematic Review of the Literature Since 2006. HERD Health Environ. Res. Des. J. 2018, 11, 85–100. [Google Scholar] [CrossRef]
- Neumann, R.; Parry, S.; Becher, T. Teaching and Learning in Their Disciplinary Contexts: A Conceptual Analysis. Stud. High. Educ. 2002, 27, 405–417. [Google Scholar] [CrossRef]
- Zuo, Z.; Cheng, J.; Guo, H.; Li, Y. Knowledge Mapping of Research on Strategic Mineral Resource Security: A Visual Analysis Using CiteSpace. Resour. Policy 2021, 74, 102372. [Google Scholar] [CrossRef]
- Cheng, Q.; Wang, J.; Lu, W.; Huang, Y.; Bu, Y. Keyword-Citation-Keyword Network: A New Perspective of Discipline Knowledge Structure Analysis. Scientometrics 2020, 124, 1923–1943. [Google Scholar] [CrossRef]
- Liu, W. Caveats for the Use of Web of Science Core Collection in Old Literature Retrieval and Historical Bibliometric Analysis. Technol. Forecast. Soc. Change 2021, 172, 121023. [Google Scholar] [CrossRef]
- Li, Y.; Xu, Z.; Wang, X.; Wang, X. A Bibliometric Analysis on Deep Learning during 2007–2019. Int. J. Mach. Learn. Cyber. 2020, 11, 2807–2826. [Google Scholar] [CrossRef]
- Rawat, K.S.; Sood, S.K. Knowledge Mapping of Computer Applications in Education Using CiteSpace. Comput. Appl. Eng. Educ. 2021, 29, 1324–1339. [Google Scholar] [CrossRef]
- Predicting Scientific Research Trends Based on Link Prediction in Keyword Networks. J. Informetr. 2020, 14, 101079. [CrossRef]
- Falagas, M.E.; Pitsouni, E.I.; Malietzis, G.A.; Pappas, G. Comparison of PubMed, Scopus, Web of Science, and Google Scholar: Strengths and Weaknesses. FASEB J. 2008, 22, 338–342. [Google Scholar] [CrossRef]
- Baas, J.; Schotten, M.; Plume, A.; Côté, G.; Karimi, R. Scopus as a Curated, High-Quality Bibliometric Data Source for Academic Research in Quantitative Science Studies. Quant. Sci. Stud. 2020, 1, 377–386. [Google Scholar] [CrossRef]
- Harzing, A.-W.; Alakangas, S. Google Scholar, Scopus and the Web of Science: A Longitudinal and Cross-Disciplinary Comparison. Scientometrics 2016, 106, 787–804. [Google Scholar] [CrossRef]






| No. | Country | Count | Centrality |
|---|---|---|---|
| 1 | USA | 260 | 0.17 |
| 2 | AUSTRALIA | 86 | 0.17 |
| 3 | United Kingdom (UK) | 82 | 0.2 |
| 4 | PEOPLE’S R CHINA | 43 | 0.13 |
| 5 | CANADA | 40 | 0.08 |
| No. | Author | Title | Citation Count |
|---|---|---|---|
| 1 | Ulrich et al. (2008) [39] | A systematic overview of the positive impact of the built environment on patient recovery, healthcare outcomes, and employee performance; a seminal text in EBD. | 828 |
| 2 | Huisman et al. (2012) [63] | Assessed the impact of physical environmental factors such as light, noise, and air quality on the physical and mental health and quality of care of hospitalized patients, emphasizing the critical role of environmental variables in healthcare design. | 293 |
| 3 | Priestley et al. (2004) [116] | Empirical support for clinical interventions and spatial coordination through a field trial examining the effectiveness of ICU outreach services in improving the efficiency of critical care management. | 250 |
| 4 | Shaughnessy et al. (2011) [117] | An empirical analysis of the impact of ward allocation patterns on the transmission of Clostridium difficile infection, emphasizing the effectiveness of single-occupancy wards in infection control. | 238 |
| 5 | Lankford et al. (2003) [118] | Investigated the effects of role modeling and hospital spatial layout on healthcare workers’ hand hygiene behavior to reveal the interactive mechanisms between behavioral interventions and environmental factors. | 200 |
| 6 | Gesler et al. (2004) [119] | Evaluated the impact of UK hospital architectural reforms on patient experience and outcomes and proposed a patient-centered design orientation. | 172 |
| 7 | Ulrich et al. (2010) [120] | A systematic conceptual framework for EBD was proposed to establish a theoretical foundation and practical assessment logic for healthcare building research. | 171 |
| 8 | Warshaw et al. (1982) [121] | Early exploration of spatial adaptations for dysfunction in hospitalized older adults provides important clues to the design of healthcare spaces for special populations. | 152 |
| 9 | McGain et al. (2014) [122] | Summarized environmental sustainability topics in hospital buildings and proposed a strategic framework and research agenda for green healthcare design. | 134 |
| 10 | Curtis et al. (2007) [123] | Assessed the healing landscape and spatial perceptual effects of a new psychiatric ward based on a psycho-geographic perspective, emphasizing the importance of the subjective experience of the user. | 129 |
| 11 | Lip et al. (1994) [124] | Explored the efficiency of room configurations in intervening in the treatment of atrial fibrillation in a general hospital, reflecting the role of ward layout in supporting specific clinical processes. | 124 |
| 12 | Chaudhury et al. (2005) [125] | Summarized the advantages and limitations of single- versus multi-occupancy wards in terms of privacy, infection control, and patient satisfaction. | 119 |
| 13 | Dalke et al. (2006) [126] | Investigated the psychological and physiological roles of color and lighting in the hospital space and proposed a design approach to optimize the hospital experience with sensory modulation. | 116 |
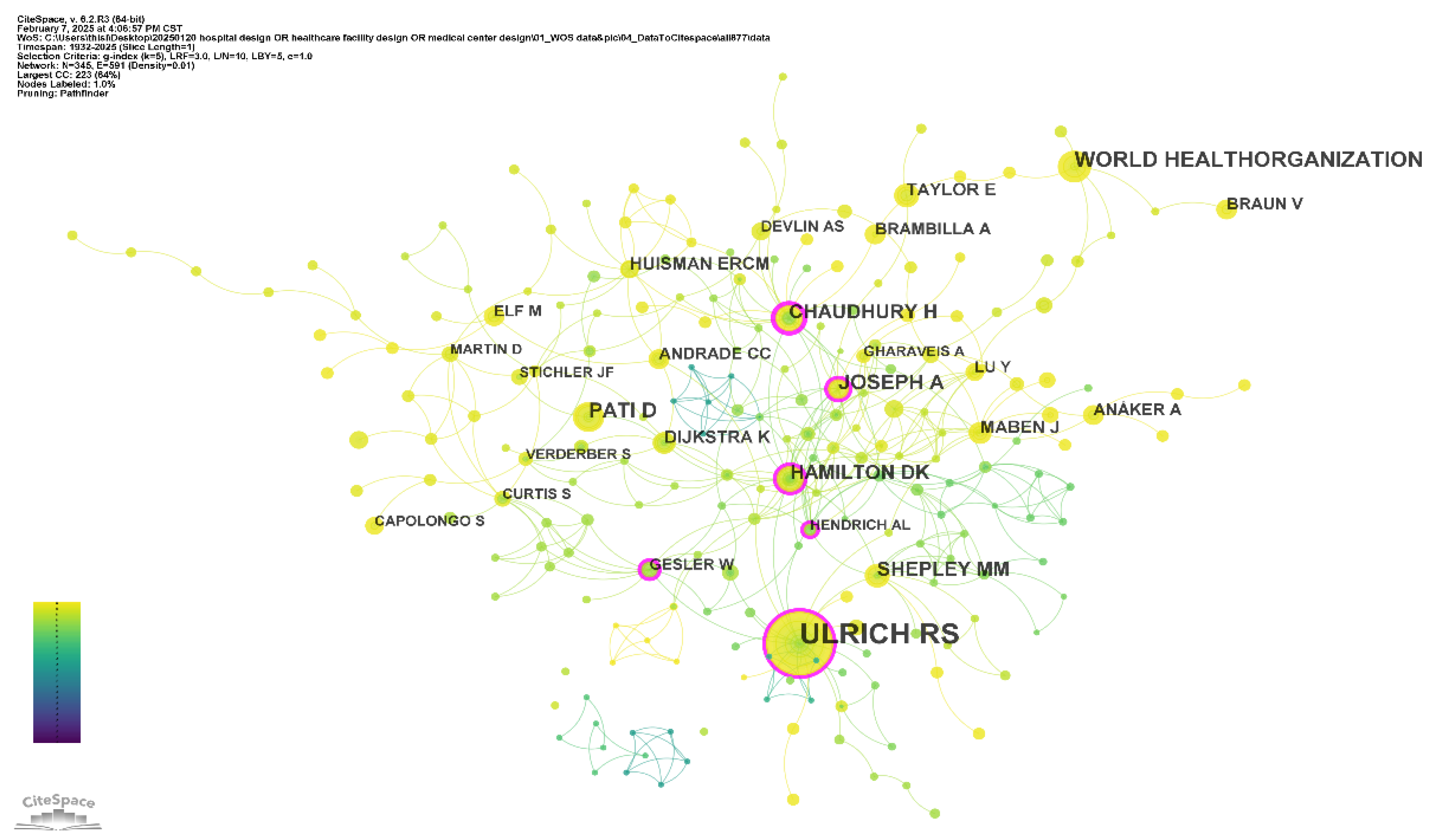
| No. | Author | Count | Centrality | Year |
|---|---|---|---|---|
| 1 | ULRICH RS | 193 | 0.2 | 1991 |
| 2 | WORLD HEALTH ORGANIZATION | 42 | 0.03 | 2019 |
| 3 | PATI D | 40 | 0.01 | 2011 |
| 4 | JOSEPH A | 38 | 0.15 | 2008 |
| 5 | CHAUDHURY H | 32 | 0.23 | 2007 |
| 6 | SHEPLEY MM | 31 | 0.09 | 2010 |
| 7 | HAMILTON DK | 29 | 0.19 | 2008 |
| 8 | HUISMAN ERCM | 21 | 0.08 | 2017 |
| 9 | MABEN J | 21 | 0.06 | 2018 |
| 10 | TAYLOR E | 20 | 0.01 | 2020 |
| No. | WoS Categories | Count | Centrality | Year |
|---|---|---|---|---|
| 1 | PUBLIC, ENVIRONMENTAL & OCCUPATIONAL HEALTH | 203 | 0.44 | 1958 |
| 2 | NURSING | 91 | 0 | 2007 |
| 3 | MEDICINE, GENERAL & INTERNAL | 84 | 0 | 1932 |
| 4 | HEALTH CARE SCIENCES & SERVICES | 59 | 0.58 | 1960 |
| 5 | CONSTRUCTION & BUILDING TECHNOLOGY | 53 | 0.17 | 1983 |
| 6 | INFECTIOUS DISEASES | 46 | 0.12 | 1981 |
| 7 | HEALTH POLICY & SERVICES | 39 | 0.05 | 1965 |
| 8 | ENGINEERING, CIVIL | 38 | 0.05 | 2011 |
| 9 | PSYCHIATRY | 29 | 0.18 | 1948 |
| 10 | ARCHITECTURE | 27 | 0.05 | 1975 |
| Keyword | Year | Strength | Beginning | End | 1932–2025 |
|---|---|---|---|---|---|
| intensive care unit | 1998 | 3.14 | 1998 | 2010 |  |
| evidence-based design | 2007 | 3.82 | 2007 | 2013 |  |
| satisfaction | 2012 | 5.44 | 2012 | 2017 |  |
| people | 2021 | 3.69 | 2021 | 2025 |  |
| patient safety | 2007 | 3.43 | 2015 | 2019 |  |
| management | 2001 | 2.84 | 2017 | 2021 |  |
| work | 2021 | 2.36 | 2021 | 2025 |  |
| patient | 2018 | 3.79 | 2022 | 2025 |  |
| quality | 2016 | 3.1 | 2018 | 2021 |  |
| healthcare | 2001 | 2.28 | 2007 | 2010 |  |
| mental health | 2021 | 4.06 | 2021 | 2023 |  |
| therapeutic landscapes | 2013 | 3.7 | 2013 | 2015 |  |
| performance | 2020 | 3.48 | 2020 | 2022 |  |
| space | 2019 | 3.26 | 2019 | 2021 |  |
| model | 2012 | 2.91 | 2020 | 2022 |  |
| safety | 2020 | 2.73 | 2020 | 2022 |  |
| mortality | 2018 | 2.55 | 2020 | 2022 |  |
| impact | 2001 | 5.78 | 2022 | 2023 |  |
| hospital design | 1991 | 3.92 | 2008 | 2009 |  |
| environmental design | 2021 | 3.27 | 2021 | 2022 |  |
| design process | 2013 | 3.22 | 2013 | 2014 |  |
| surgery | 2018 | 2.79 | 2018 | 2019 |  |
| environments | 2013 | 2.7 | 2022 | 2023 |  |
| experience | 1994 | 2.51 | 2020 | 2021 |  |
| outcome | 2012 | 2.4 | 2021 | 2022 |  |
| risk | 2010 | 2.37 | 2018 | 2019 |  |
| stress | 2014 | 2.34 | 2021 | 2022 |  |
| framework | 2021 | 2.3 | 2024 | 2025 |  |
| Analysis Dimension | Key Findings | Interpretation |
|---|---|---|
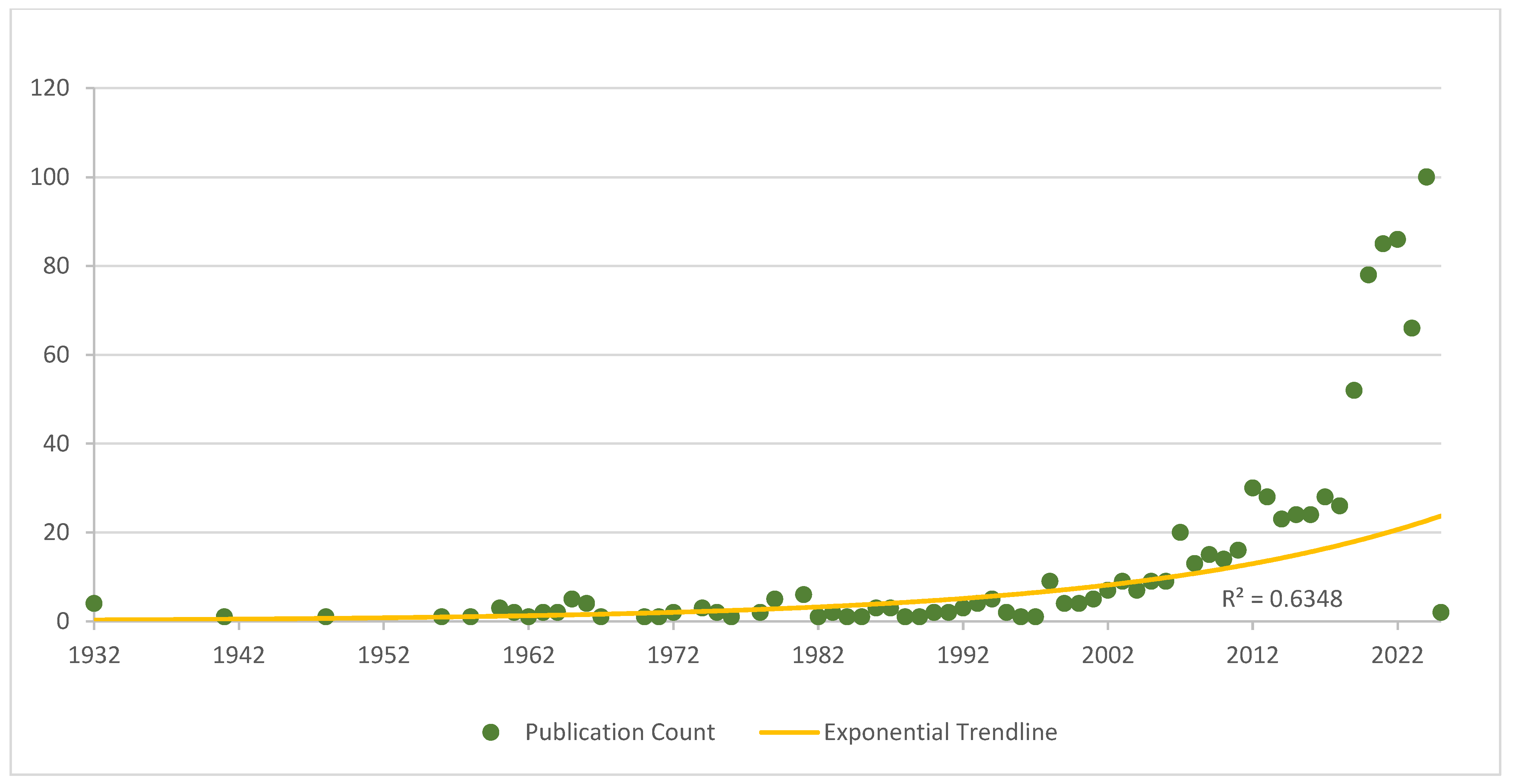
| Publication Trends | Total of 877 papers (1932–2025); rapid growth since 2020 (417 papers; 47.56% of total). | Reflects both WoSCC coverage expansion and a genuine surge of interest post-COVID-19; indicates hospital design has become a rapidly developing interdisciplinary field. |
| Country Collaboration | The USA leads (260 papers, high centrality), followed by the UK and Australia; China and Canada are emerging; Japan, Turkey, and Italy act as regional bridges. | Global research is concentrated in developed countries; some nations act as strategic connectors. Regional disparities persist (e.g., Africa and South America are underrepresented). |
| Institution Collaboration | Leading institutions: Univ. of London, Aarhus Univ., and Univ. of Toronto; regional clusters in Europe, North America, and Asia-Pacific. | Institutional collaboration remains fragmented, with geographic clustering; scope for broader international partnerships. |
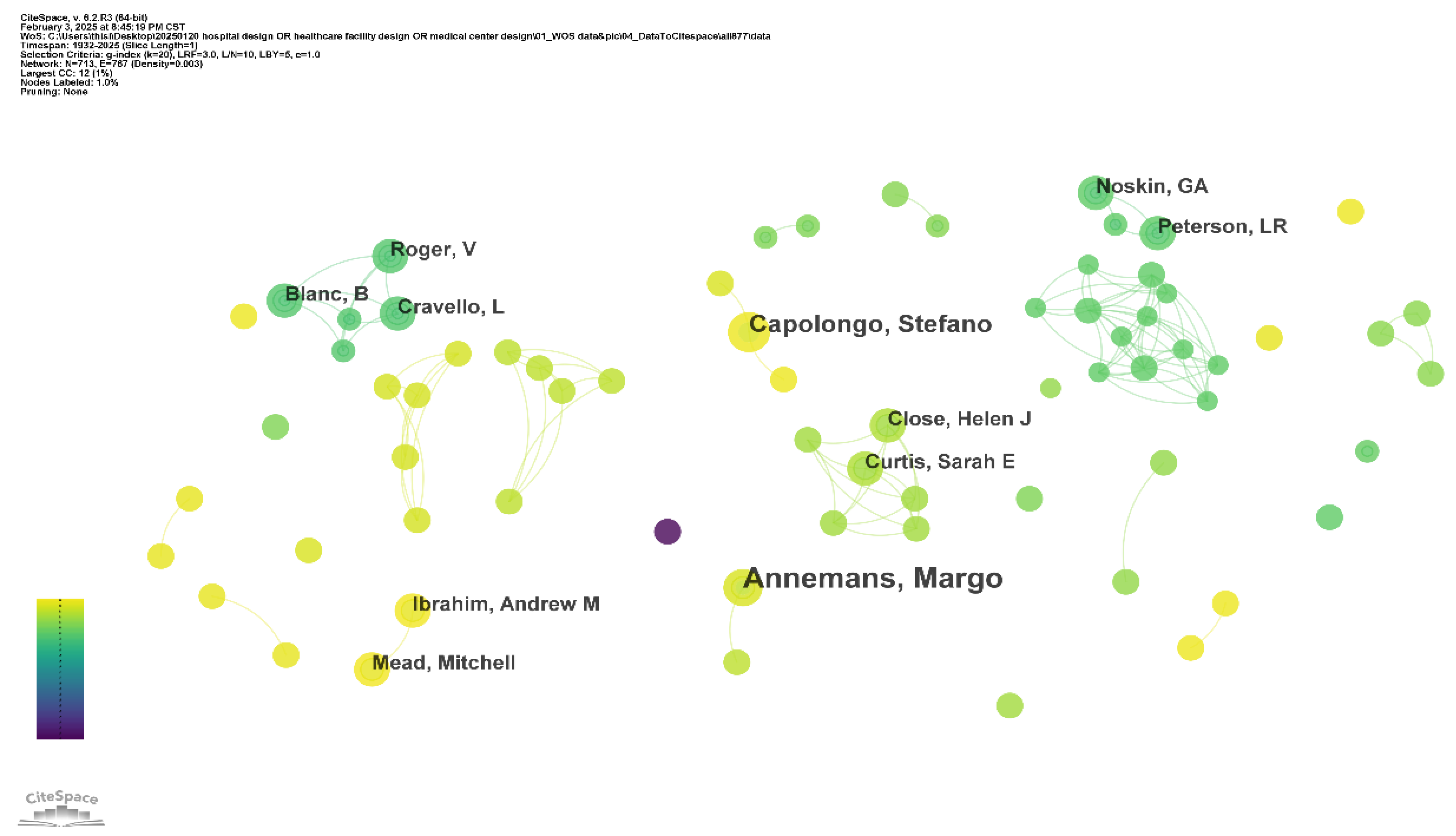
| Author Collaboration | 713 authors, 767 links, network density of 0.003; mostly small groups, with weak cross-group links. Core figures include Ulrich RS, Joseph A, and Chaudhury H. | The field lacks strong central leaders; collaboration is mostly localized. Influential authors provide theoretical and methodological anchors. |
| Highly Cited References | 13 papers with >100 citations (2004–2012 peak). Core works: Ulrich (2004, 2008). | Established EBD as the theoretical foundation; research gradually shifted toward patient-centered and infection control design. |
| Author Co-Citation Network | Key authors: Ulrich RS (central node), Joseph A, Chaudhury H, Hamilton DK, and Pati D. | Indicates strong reliance on EBD pioneers and healthcare design scholars, forming the intellectual base of the field. |
| Journal Co-Citation Network | Core journals: HERD, Environment and Behavior, The Lancet, NEJM, and JAMA. | The field is highly interdisciplinary, combining architecture, medicine, psychology, and nursing. |
| Subject Categories | Core: Public health, nursing, medicine, construction technology, and architecture. Emerging: Medical informatics and computer science. | The field is evolving from medical dominance to multidisciplinary integration, including digital and environmental sciences. |
| Keyword Analysis | Hotspots: “hospital design”, “healthcare”, “impact”, “EBD”, and “patient safety”. Emerging: “mental health”, “framework”, and “environmental design”. | Research focus has shifted from space/function to user-centered outcomes, sustainability, and psychosocial healing; it indicates future emphasis on resilience and system-level frameworks. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, J.; Yeo, Y. Bibliometric Analysis of Hospital Design: Knowledge Mapping Evolution and Research Trends. Buildings 2025, 15, 3196. https://doi.org/10.3390/buildings15173196
Liu J, Yeo Y. Bibliometric Analysis of Hospital Design: Knowledge Mapping Evolution and Research Trends. Buildings. 2025; 15(17):3196. https://doi.org/10.3390/buildings15173196
Chicago/Turabian StyleLiu, Jingwen, and Youngho Yeo. 2025. "Bibliometric Analysis of Hospital Design: Knowledge Mapping Evolution and Research Trends" Buildings 15, no. 17: 3196. https://doi.org/10.3390/buildings15173196
APA StyleLiu, J., & Yeo, Y. (2025). Bibliometric Analysis of Hospital Design: Knowledge Mapping Evolution and Research Trends. Buildings, 15(17), 3196. https://doi.org/10.3390/buildings15173196









