Lighting and Sleep Quality in the Elderly: A Systematic Review to Inform Future Research Design
Abstract
1. Introduction
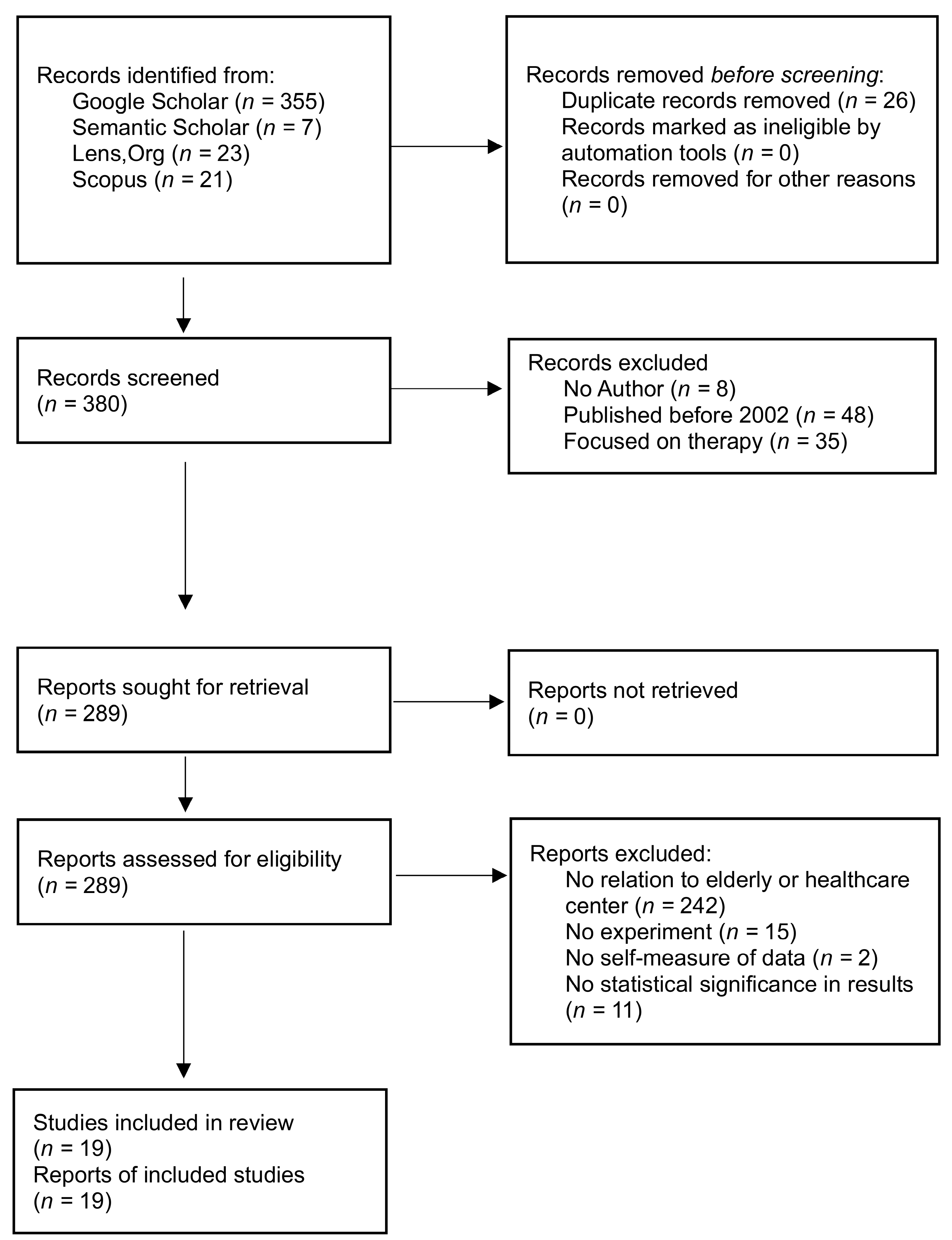
2. Methods
2.1. Data Sources
2.2. Study Selection
- Only peer-reviewed journal articles are included to focus on the latest research findings.
- Since ipRGCs were established in 2002 by David Berson and serve an essential role in controlling and changing the human circadian system [37], only studies published after 2002 are included.
- Studies solely on light medication or light therapy are excluded, as this review focuses on architectural lighting aspects instead of medical lighting.
- Only studies reporting empirical data on the effects of light on elderly people’s sleep quality were considered.
- Studies with all experimental designs are included.
- Studies without light interventions or controlled light exposure are considered, as long as the measurement of light exposure with analysis on the effects of light on sleep quality or factors relating to the sleep quality of elderly people is included.
- Only studies with statistically significant results are included to focus on proven relationships between sleep quality and light for elderly people. Although it may limit generalisability and introduce potential bias, this will increase the quality of results by focusing on interventions with demonstrated effectiveness.
2.3. Light Therapy Selection
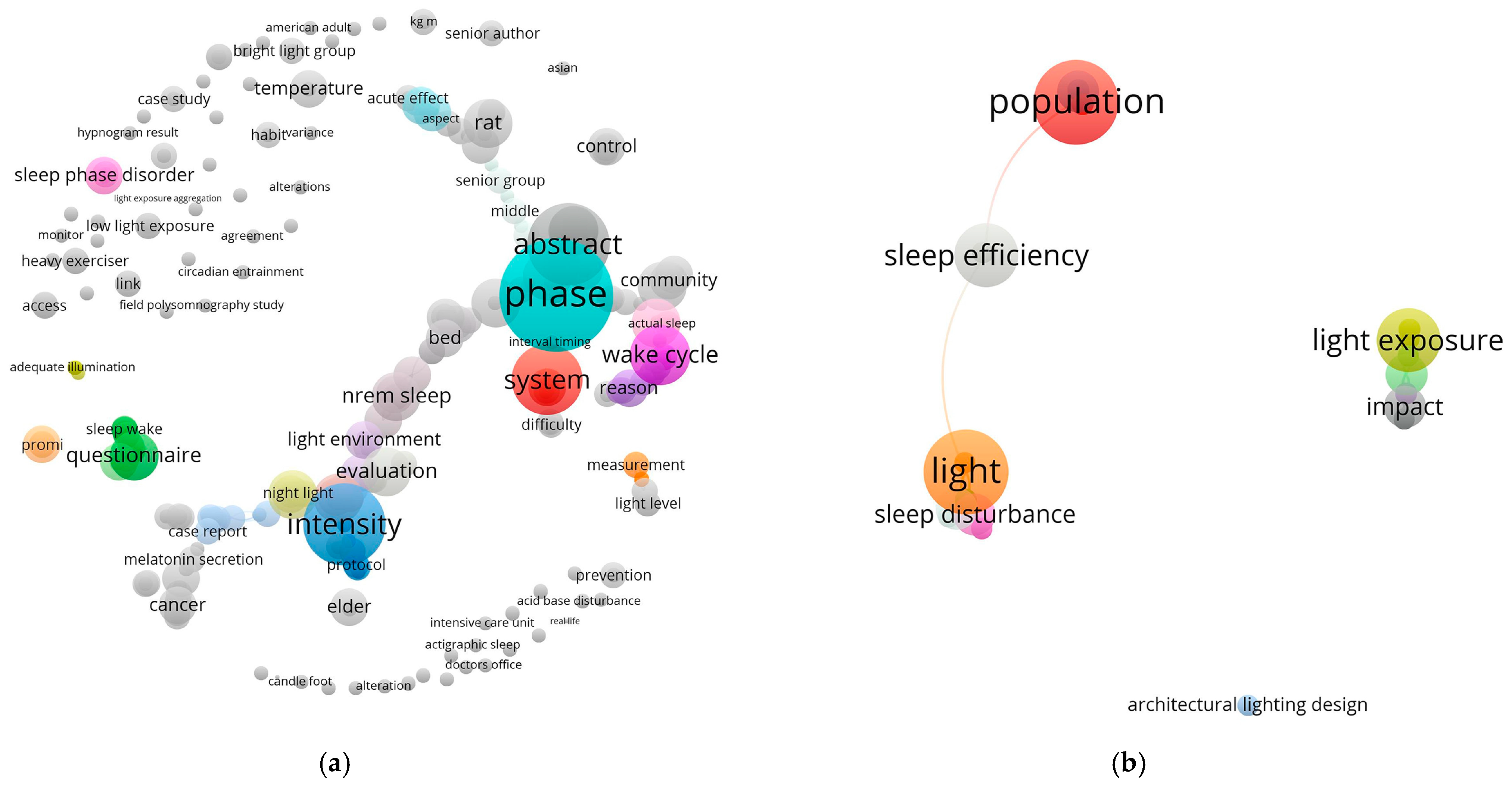
2.4. VOSviewer Key Word Analysis
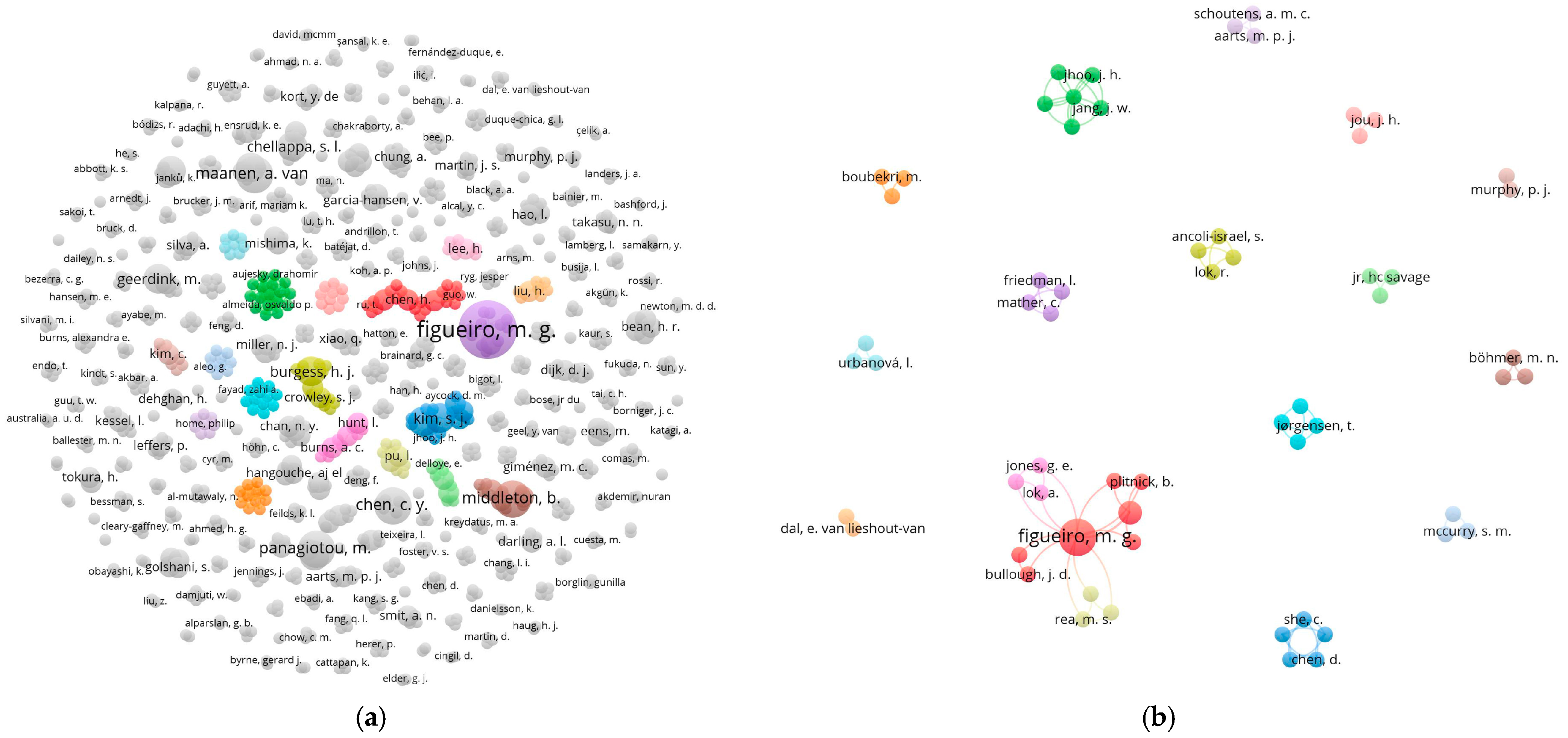
2.5. VOSviewer Bibliographic Analysis
3. Results
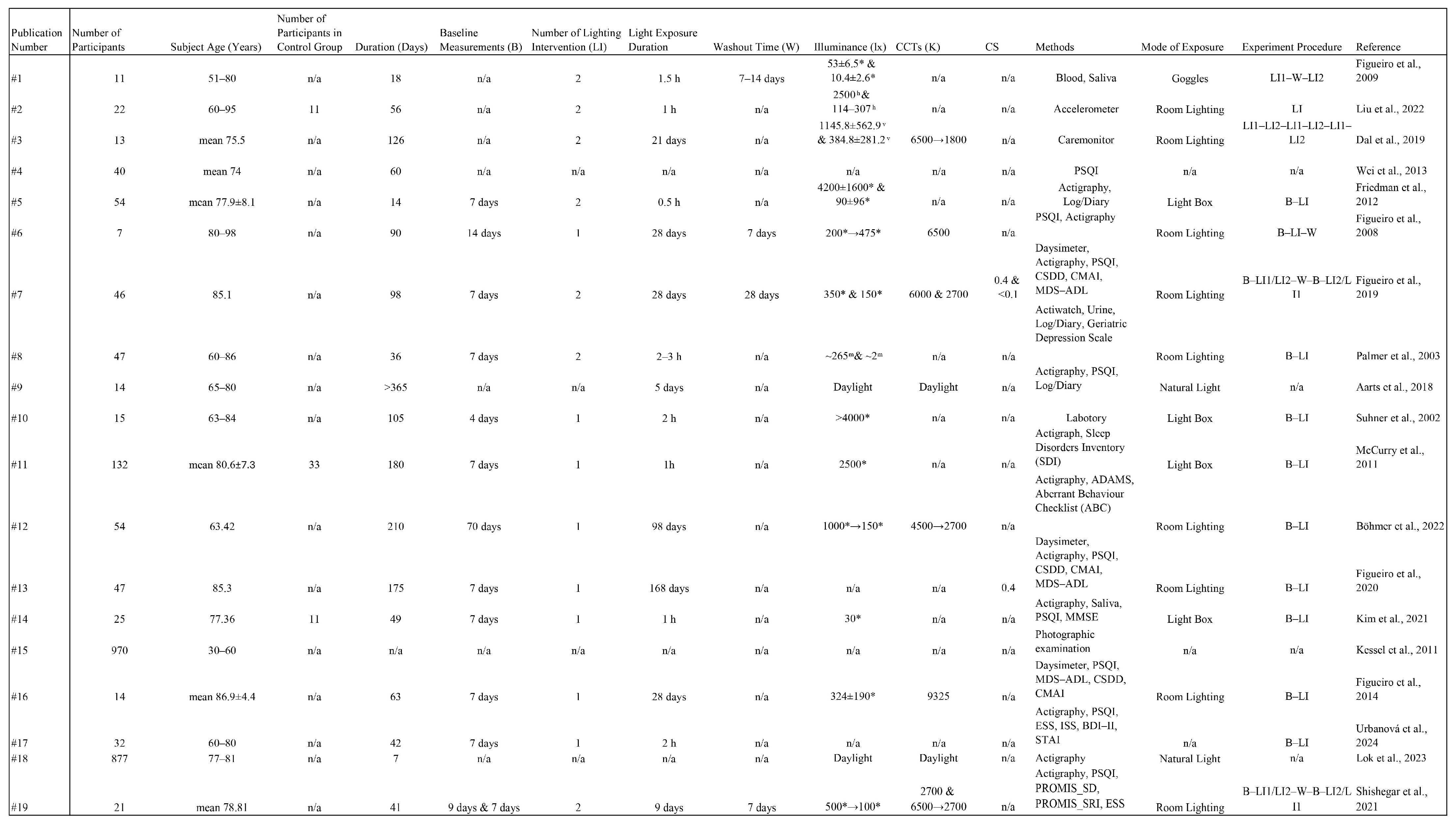
3.1. Methodology Analysis of 19 Selected Publications
3.1.1. Publications Without Baseline Measurement
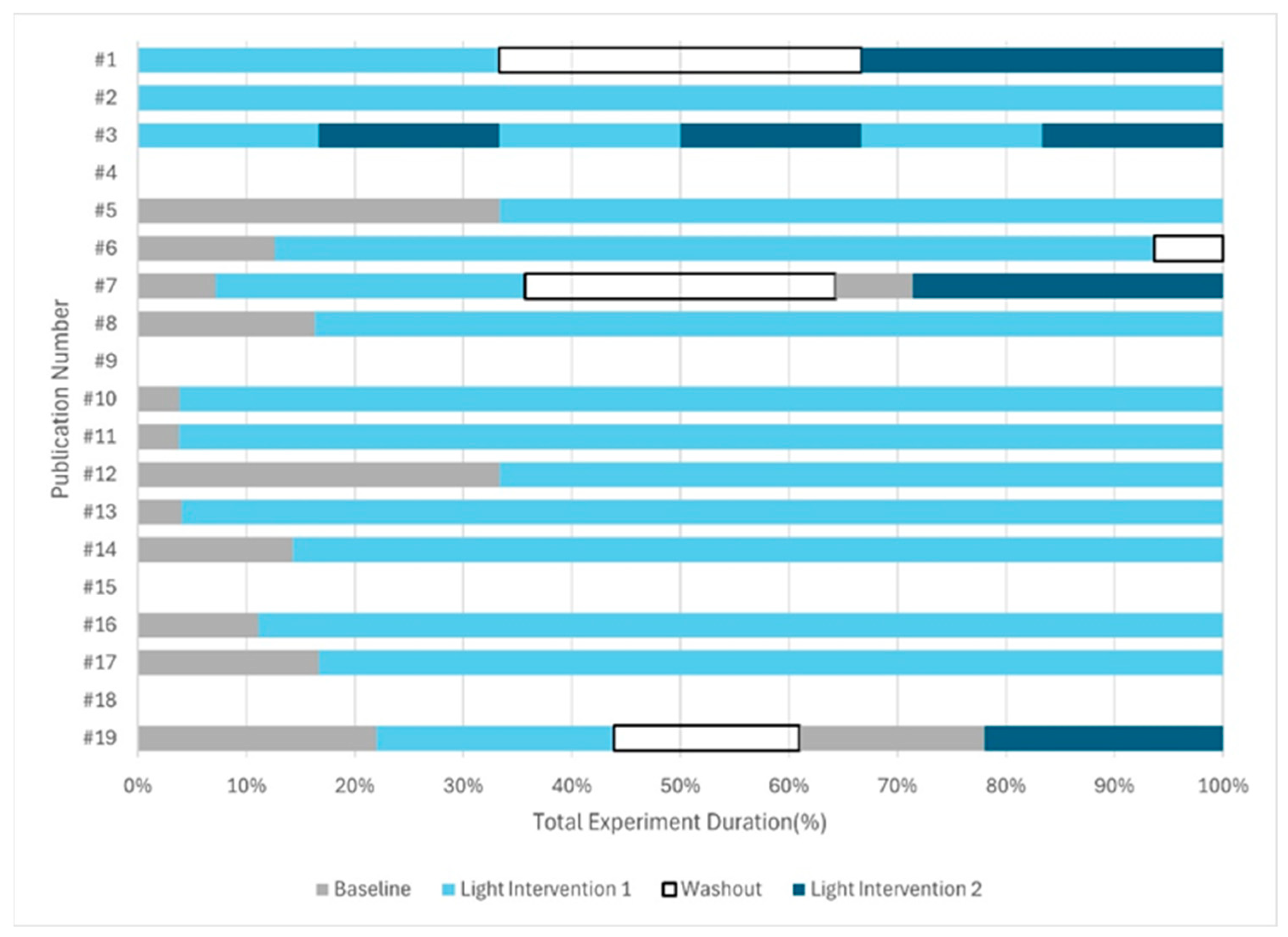
3.1.2. Publications with Light Intervention
3.1.3. Publications with Baseline Measurement
3.1.4. Other Limitations
3.2. Six Key Parameter Analysis of 19 Selected Publications
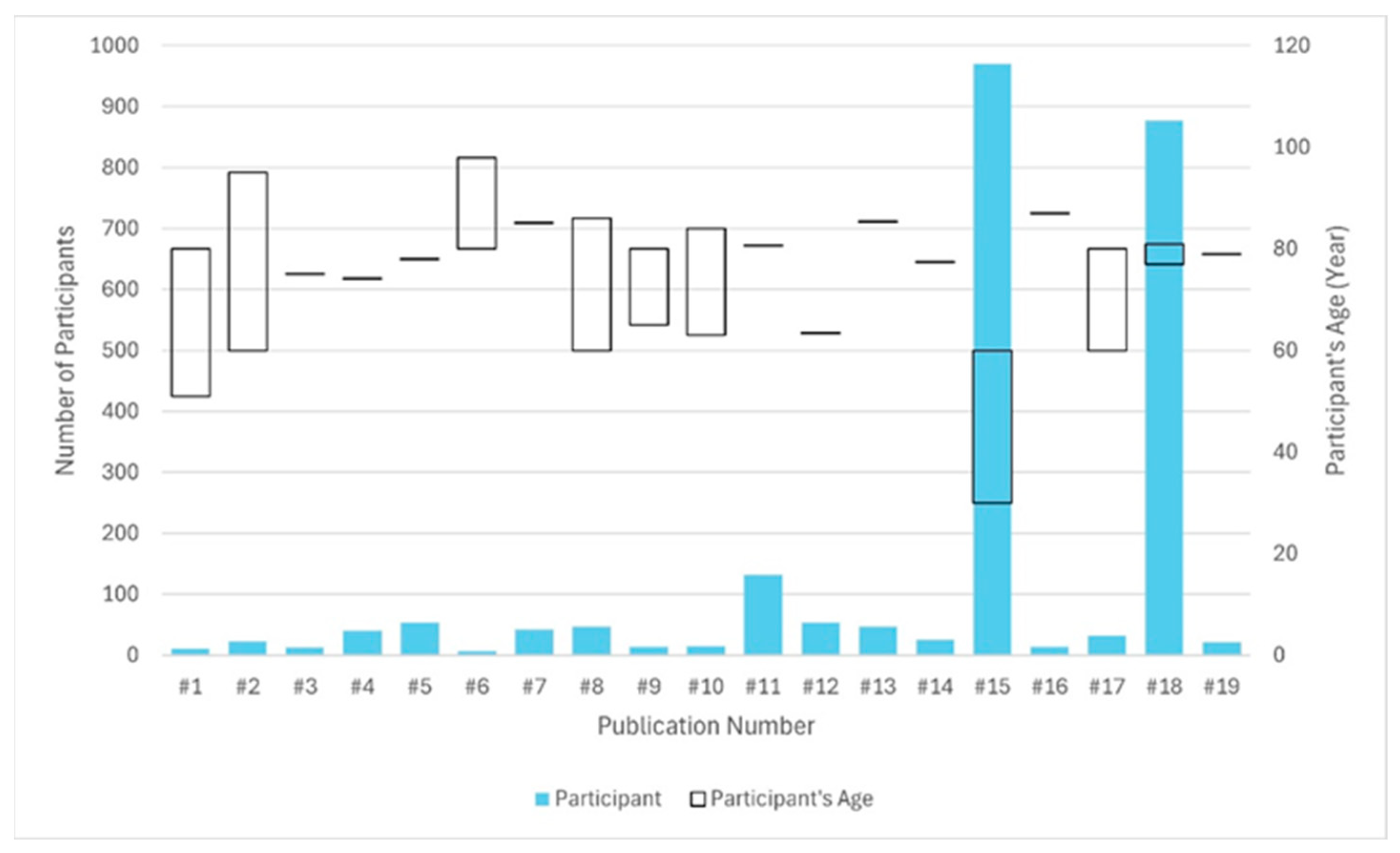
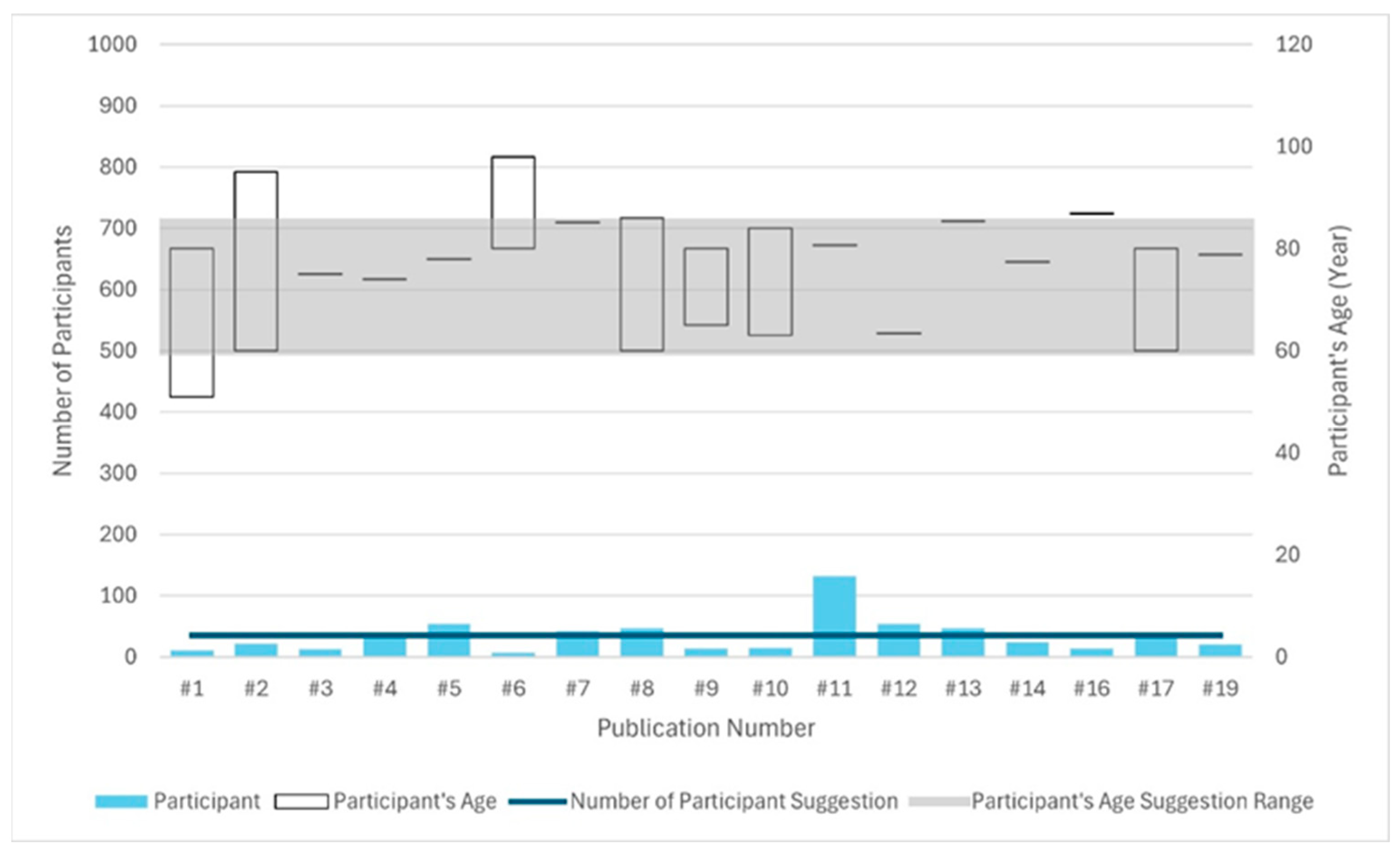
3.2.1. Participant
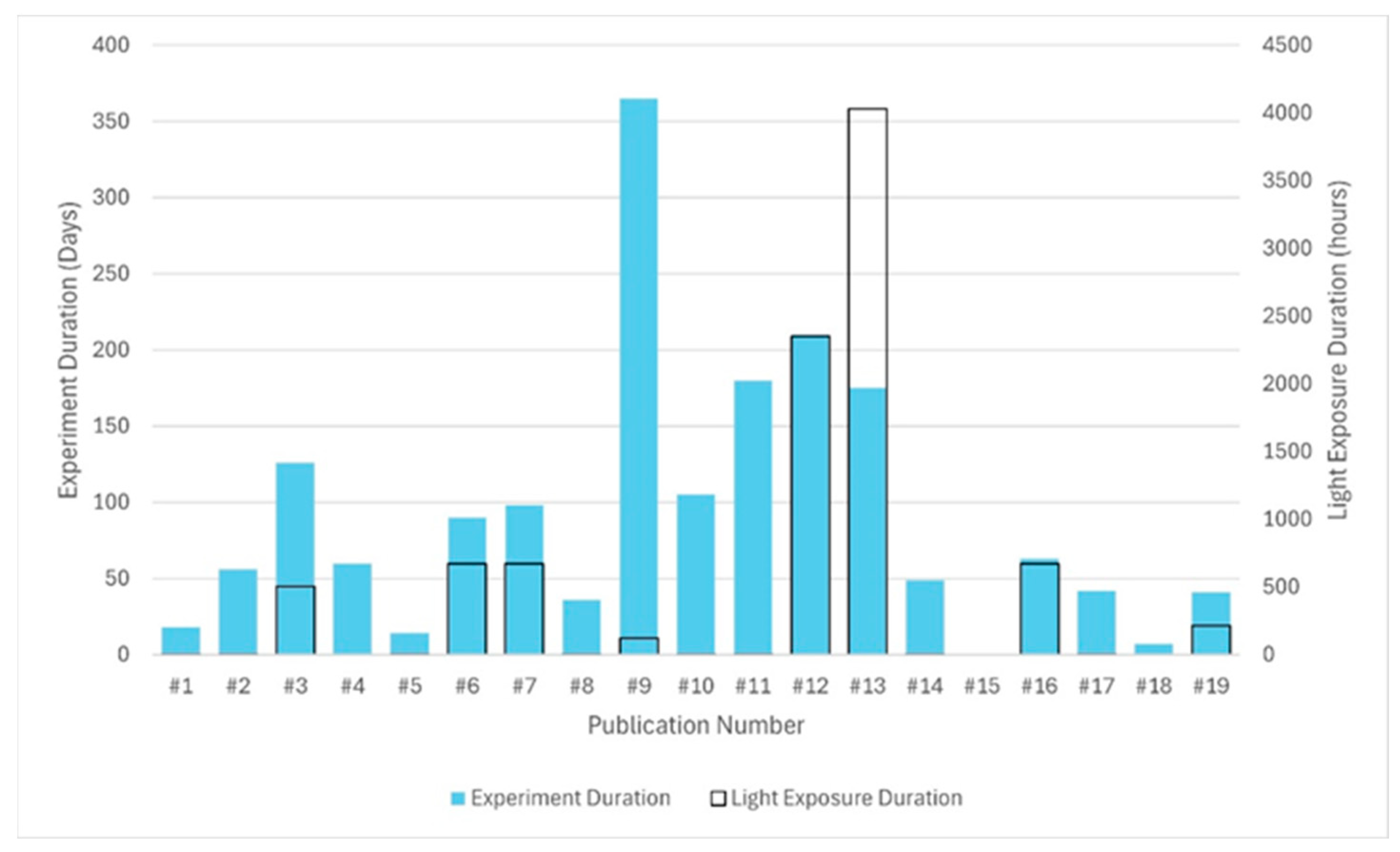
3.2.2. Experiment and Duration of Light Exposure
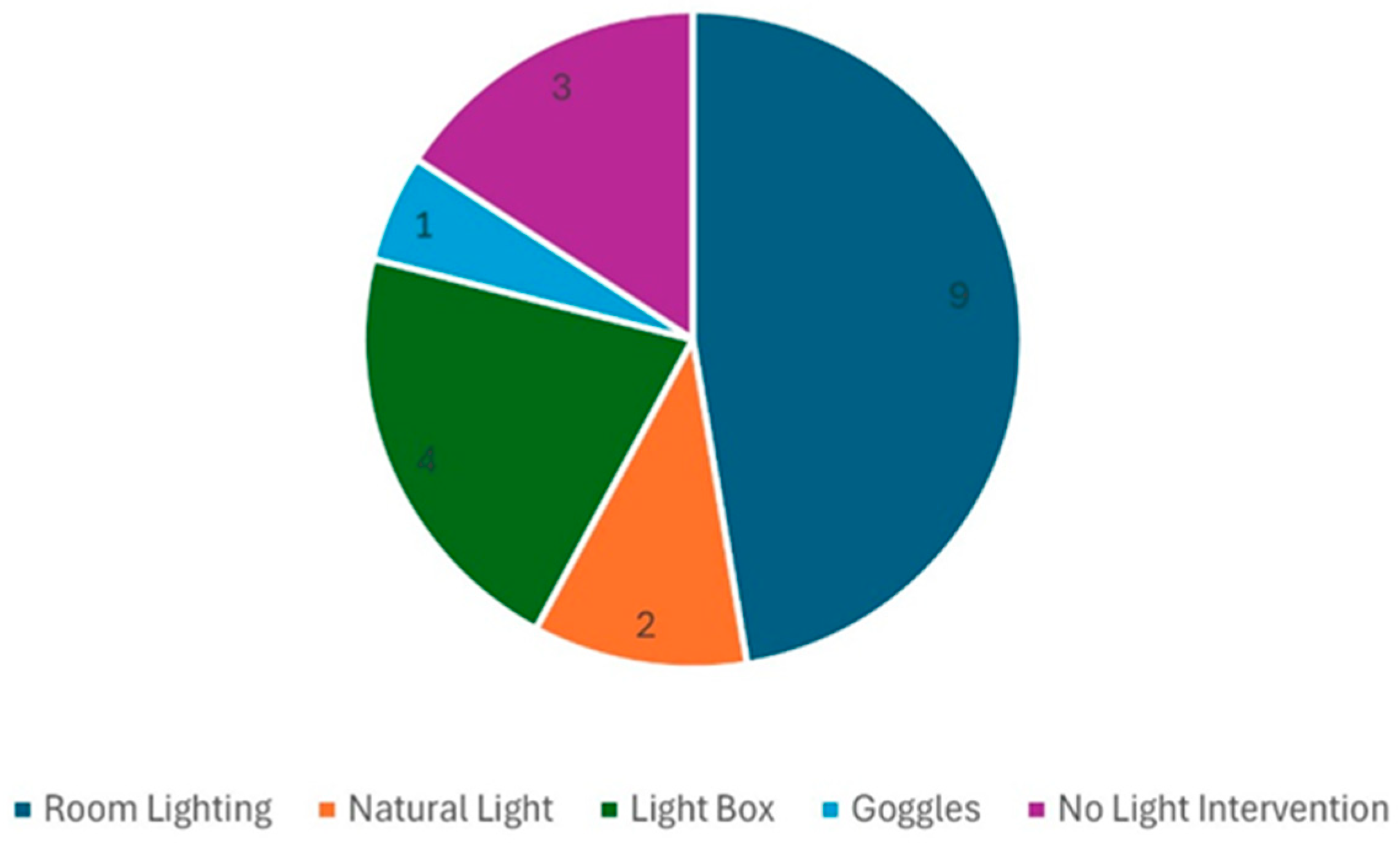
3.2.3. Mode of Light Exposure
3.2.4. Lighting and Light Interventions
3.2.5. Experiment Procedure
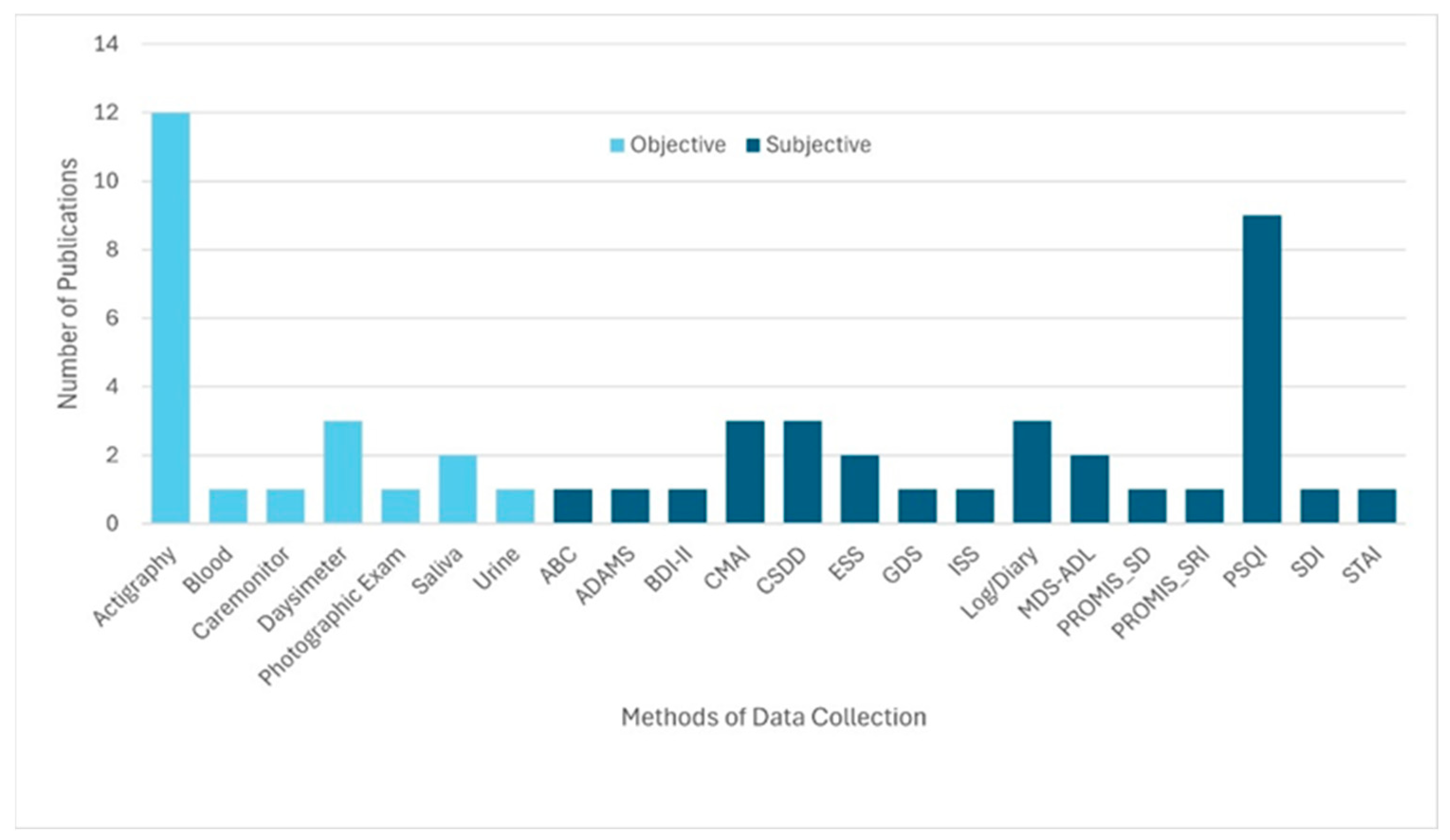
3.2.6. Method of Data Collection
3.3. p-Value Analysis of the 19 Selected Publications
3.3.1. PSQI and p-Value
3.3.2. Actigraphy and p-Value
4. Discussion
4.1. Participant
4.2. Mode of Light Exposure, Experiment, and Duration of Light Exposure
4.3. Lighting and Light Interventions
4.4. Method of Data Collection
4.5. Cohen’s d on PSQI of 19 Selected Publications
4.6. Participant Inclusion Criteria
4.7. Allowance of Medication
4.8. Participant Control and Measuring of Light Interventions
5. Conclusions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| URL | Uniform Resource Locator |
| IpRGCs | Intrinsically Photosensitive Retinal Ganglion Cells |
| CCT | Correlated Colour Temperature |
| PSQI | Pittsburgh Sleep Quality Index |
| CSDD | Cornell Scale for Depression in Dementia |
| CMAI | Cohen–Mansfield Agitation Inventory |
| MDS-ADL | Minimum Data Set-Activities of Daily Living |
| SPD | Spectral Power Distribution |
| MEDI | Melanopic Equivalent Daylight Illuminance |
| dp | Decimal Point |
Appendix A
Appendix B
| Number of Participants | Participant Age | Tb | Number of LI | Duration of Light Exposure | Tw | Mode of Exposure | Data Collection Methods |
|---|---|---|---|---|---|---|---|
| ~14–47 | ≥65 years | ~7 days | ~2 | ~21–35 days | ~4–10 days | Room Lighting | Actigraphy, Daysimeter, PSQI, CSDD, CMAI, MDS-ADL, Sleep Log/Sleep Diary |
References
- Tel, H. Sleep quality and quality of life among the elderly people. Neurol. Psychiatry Brain Res. 2013, 19, 48–52. [Google Scholar] [CrossRef]
- Global Aging Population—Lausanne Movement. Available online: https://lausanne.org/report/demographics/global-aging-population (accessed on 31 May 2024).
- Sewell, K.R.; Erickson, K.I.; Rainey-Smith, S.R.; Peiffer, J.J.; Sohrabi, H.R.; Brown, B.M. Relationships between physical activity, sleep and cognitive function: A narrative review. Neurosci. Biobehav. Rev. 2021, 130, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Palmer, C.A.; Alfano, C.A. Sleep and emotion regulation: An organizing, integrative review. Sleep Med. Rev. 2017, 31, 6–16. [Google Scholar] [CrossRef] [PubMed]
- Reid, K.J.; Martinovich, Z.; Finkel, S.; Statsinger, J.; Golden, R.; Harter, K.; Zee, P.C. Sleep: A Marker of Physical and Mental Health in the Elderly. Am. J. Geriatr. Psychiatry 2006, 14, 860–866. [Google Scholar] [CrossRef] [PubMed]
- Figueiro, M.G.; Bierman, A.; Bullough, J.D.; Rea, M.S. A personal light-treatment device for improving sleep quality in the elderly: Dynamics of nocturnal melatonin suppression at two exposure levels. Chronobiol. Int. 2009, 26, 726–739. [Google Scholar] [CrossRef]
- Tähkämö, L.; Partonen, T.; Pesonen, A.-K. Systematic review of light exposure impact on human circadian rhythm. Chronobiol. Int. 2019, 36, 151–170. [Google Scholar] [CrossRef]
- De Lepeleire, J.; Bouwen, A.; De Coninck, L.; Buntinx, F. Insufficient Lighting in Nursing Homes. J. Am. Med. Dir. Assoc. 2007, 8, 314–317. [Google Scholar] [CrossRef]
- Kolberg, E.; Pallesen, S.; Hjetland, G.; Nordhus, I.; Thun, E.; Flo-Groeneboom, E. Insufficient melanopic equivalent daylight illuminance in nursing home dementia units across seasons and gaze directions. Light. Res. Technol. 2022, 54, 163–177. [Google Scholar] [CrossRef]
- Fabbri, M.; Beracci, A.; Martoni, M.; Meneo, D.; Tonetti, L.; Natale, V. Measuring Subjective Sleep Quality: A Review. Int. J. Environ. Res. Public Health 2021, 18, 1082. [Google Scholar] [CrossRef]
- Krystal, A.D.; Edinger, J.D. Measuring sleep quality. Sleep Med. 2008, 9, S10–S17. [Google Scholar] [CrossRef]
- Nelson, K.L.; Davis, J.E.; Corbett, C.F. Sleep quality: An evolutionary concept analysis. Nurs. Forum 2022, 57, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.R.; Liou, Y.M.; Jou, J.H. Ambient bright lighting in the morning improves sleep disturbances of older adults with dementia. Sleep Med. 2022, 89, 1–9. [Google Scholar] [CrossRef]
- McCurry, S.M.; Pike, K.C.; Vitiello, M.V.; Logsdon, R.G.; Larson, E.B.; Teri, L. Increasing walking and bright light exposure to improve sleep in community-dwelling persons with Alzheimer’s disease: Results of a randomized, controlled trial. J. Am. Geriatr. Soc. 2011, 59, 1393–1402. [Google Scholar] [CrossRef]
- Aarts, M.P.J.; Stapel, J.C.; Schoutens, A.M.C.; van Hoof, J. Exploring the impact of natural light exposure on sleep of healthy older adults: A field study. J. Daylighting 2018, 5, 14–20. [Google Scholar] [CrossRef]
- Dal, E.v.L.; Snaphaan, L.; Bongers, I. Biodynamic lighting effects on the sleep pattern of people with dementia. Build. Environ. 2019, 150, 245–253. [Google Scholar] [CrossRef]
- Palmer, C.R.; Kripke, D.F.; Savage, H.S., Jr.; Cindrich, L.A.; Loving, R.T.; Elliott, J.A. Efficacy of enhanced evening light for advanced sleep phase syndrome. Behav. Sleep Med. 2003, 1, 213–226. [Google Scholar] [CrossRef]
- Shishegar, N.; Boubekri, M.; Stine-Morrow, E.A.L.; Roger, W.A. Tuning environmental lighting improves objective and subjective sleep quality in older adults. Build. Environ. 2021, 204, 108096. [Google Scholar] [CrossRef]
- Figueiro, M.G.; Sahin, L.; Kalsher, M.; Plitnick, B.; Rea, M.S. Long-term, all-day exposure to circadian-effective light improves sleep, mood, and behavior in persons with dementia. J. Alzheimers Dis. Rep. 2020, 4, 297–312. [Google Scholar] [CrossRef]
- Schieber, F. Seven—Vision and Aging; Academic Press: Cambridge, MA, USA, 2006; pp. 129–161. [Google Scholar] [CrossRef]
- Kessel, L.; Siganos, G.; Jørgensen, T.; Larsen, M. Sleep Disturbances Are Related to Decreased Transmission of Blue Light to the Retina Caused by Lens Yellowing. Sleep 2011, 34, 1215–1219. [Google Scholar] [CrossRef] [PubMed]
- Turner, P.L.; Van Someren, E.J.W.; Mainster, M.A. The role of environmental light in sleep and health: Effects of ocular aging and cataract surgery. Sleep Med. Rev. 2010, 14, 269–280. [Google Scholar] [CrossRef] [PubMed]
- Zele, A.J.; Feigl, B.; Smith, S.S.; Markwell, E.L. The Circadian Response of Intrinsically Photosensitive Retinal Ganglion Cells. PLoS ONE 2011, 6, e17860. [Google Scholar] [CrossRef]
- Lewy, A.J.; Wehr, T.A.; Goodwin, F.K.; Newsome, D.A.; Markey, S.P. Light Suppresses Melatonin Secretion in Humans. Science 1980, 210, 1267–1269. [Google Scholar] [CrossRef]
- Vandewalle, G.; Balteau, E.; Phillips, C.; Degueldre, C.; Moreau, V.; Sterpenich, V.; Albouy, G.; Darsaud, A.; Desseilles, M.; Dang-Vu, T.T.; et al. Daytime light exposure dynamically enhances brain responses. Curr. Biol. 2006, 16, 1616–1621. [Google Scholar] [CrossRef] [PubMed]
- Gooley, J.J.; Chamberlain, K.; Smith, K.A.; Khalsa, S.B.S.; Rajaratnam, S.M.W.; Van Reen, E.; Zeitzer, J.M.; Czeisler, C.A.; Lockley, S.W. Exposure to room light before bedtime suppresses melatonin onset and shortens melatonin duration in humans. J. Clin. Endocrinol. Metab. 2011, 96, E463–E472. [Google Scholar] [CrossRef]
- Ancoli-Israel, S.; Klauber, M.R.; Jones, D.W.; Kripke, D.F.; Martin, J.; Mason, W.; Pat-Horenczyk, R.; Fell, R. Variations in Circadian Rhythms of Activity, Sleep, and Light Exposure Related to Dementia in Nursing-Home Patients. Sleep 1997, 20, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Shochat, T.; Martin, J.; Marler, M.; Ancoli-Israel, S. Illumination levels in nursing home patients: Effects on sleep and activity rhythms. J. Sleep Res. 2000, 9, 373–379. [Google Scholar] [CrossRef]
- Majid, M.S.; Ahmad, H.S.; Bizhan, H.; Hosein, H.Z.M.; Mohammad, A. The effect of vitamin D supplement on the score and quality of sleep in 20–50 year-old people with sleep disorders compared with control group. Nutr. Neurosci. 2018, 21, 511–519. [Google Scholar] [CrossRef]
- Guu, T.W.; Aarsland, D.; Ffytche, D. Light, sleep-wake rhythm, and behavioural and psychological symptoms of dementia in care home patients: Revisiting the sundowning syndrome. Int. J. Geriatr. Psychiatry 2022, 47, 1659–1670. [Google Scholar] [CrossRef] [PubMed]
- Volicer, L.; Harper, D.G.; Manning, B.C.; Goldstein, R.; Satlin, A. Sundowning and Circadian Rhythms in Alzheimer’s Disease. Am. J. Psychiatry 2001, 158, 704–711. [Google Scholar] [CrossRef]
- Canevelli, M.; Valletta, M.; Trebbastoni, A.; Sarli, G.; D’Antonio, F.; Tariciotti, L.; de Lena, C.; Bruno, G. Sundowning in Dementia: Clinical Relevance, Pathophysiological Determinants, and Therapeutic Approaches. Front. Med. 2016, 3, 73. [Google Scholar] [CrossRef]
- Figueiro, M.G.; Plitnick, B.; Roohan, C.; Sahin, L.; Kalsher, M.; Rea, M.S. Effects of a tailored lighting intervention on sleep quality, rest–activity, mood, and behavior in older adults with Alzheimer disease and related dementias. J. Clin. Sleep Med. 2019, 15, 1757–1767. [Google Scholar] [CrossRef]
- Mitolo, M.; Tonon, C.; Morgia, C.L.; Testa, C.; Carelli, V.; Lodi, R. Effects of light treatment on sleep, cognition, mood, and behavior in Alzheimer’s disease: A systematic review. Dement. Geriatr. Cogn. Disord. 2018, 46, 371–384. [Google Scholar] [CrossRef] [PubMed]
- Friedman, L.; Spira, A.P.; Hernandez, B.; Mather, C.; Sheikh, J.; Ancoli-Israel, S.; Yesavage, J.A.; Zeitzer, J.M. Brief morning light treatment for sleep/wake disturbances in older memory-impaired individuals and their caregivers. Sleep Med. 2012, 13, 546–549. [Google Scholar] [CrossRef]
- PRISMA 2020 Flow Diagram. PRISMA Statement. Available online: https://www.prisma-statement.org/prisma-2020-flow-diagram (accessed on 18 September 2024).
- Berson, D.M.; Dunn, F.A.; Takao, M. Phototransduction by Retinal Ganglion Cells That Set the Circadian Clock. Science 2002, 295, 1070–1073. [Google Scholar] [CrossRef]
- Harzing, A.W. Publish or Perish (Version 8). Available online: https://harzing.com/resources/publish-or-perish (accessed on 18 September 2024).
- Corporation for Digital Scholarship. Zotero (Version 6.0). Available online: https://www.zotero.org/ (accessed on 18 September 2024).
- Suhner, A.G.; Murphy, P.J.; Campbell, S.S. Failure of timed bright light exposure to alleviate age-related sleep maintenance insomnia. J. Am. Geriatr. Soc. 2002, 50, 617–623. [Google Scholar] [CrossRef]
- Wang, Q.; Wu, S.; Luo, Z.; Pu, L.; Wang, X.; Guo, M.; Zhang, M.; Tang, H.; Chen, M.; Kong, L.; et al. Effects of light therapy on sleep and circadian rhythm in older type 2 diabetics living in long-term care facilities: A randomized controlled trial. Front. Endocrinol. 2024, 15, 1307537. [Google Scholar] [CrossRef]
- Stallard, A.; Angel, J. Is light therapy effective in improving quality/quantity of sleep in patients with both dementia and sleep disturbance? Evid.-Based Pract. 2022, 25, 18–19. [Google Scholar] [CrossRef]
- Chong, M.S.; Tan, K.T.; Tay, L.; Wong, Y.M.; Ancoli-Israel, S. Bright light therapy as part of a multicomponent management program improves sleep and functional outcomes in delirious older hospitalized adults. Clin. Interv. Aging 2013, 8, 565–572. [Google Scholar] [CrossRef] [PubMed]
- Akyar, I.; Akdemir, N. The effect of light therapy on the sleep quality of the elderly: An intervention study. Ajan Aust. J. Adv. Nurs. 2014, 31, 31–38. [Google Scholar] [CrossRef]
- VOSviewer. Visualizing Scientific Landscapes. Available online: https://www.vosviewer.com/ (accessed on 6 April 2025).
- Figueiro, M.G.; Saldo, E.; Rea, M.S.; Kubarek, K.; Cunningham, J.; Rea, M.S. Developing architectural lighting designs to improve sleep in older adults. Open Sleep J. 2008, 1, 40–51. [Google Scholar] [CrossRef]
- Figueiro, M.G.; Plitnick, B.A.; Lok, A.; Jones, G.E.; Higgins, P.; Hornick, T.R.; Rea, M.S. Tailored lighting intervention improves measures of sleep, depression, and agitation in persons with Alzheimer’s disease and related dementia living in long-term care. Clin. Interv. Aging 2014, 9, 1527–1537. [Google Scholar] [CrossRef]
- Wei, X.; She, C.; Chen, D.; Yan, F.; Zeng, J.; Zeng, L.; Wang, L. Blue-light-blocking intraocular lens implantation improves the sleep quality of cataract patients. J. Clin. Sleep Med. 2013, 9, 741–745. [Google Scholar] [CrossRef]
- Lok, R.; Ancoli-Israel, S.; Ensrud, K.E.; Redline, S.; Stone, K.L.; Zeitzer, J.M. Timing of outdoor light exposure is associated with sleep-wake consolidation in community-dwelling older men. Front. Sleep 2023, 2, 1268379. [Google Scholar] [CrossRef]
- Gulia, K.K.; Kumar, V.M. Sleep disorders in the elderly: A growing challenge. Psychogeriatrics 2018, 18, 155–165. [Google Scholar] [CrossRef]
- Wilson, E.B. An Introduction to Scientific Research; Courier Corporation: New York, NY, USA, 1990. [Google Scholar]
- Denissen, J.J.A.; Butalid, L.; Penke, L.; van Aken, M.A.G. The effects of weather on daily mood: A multilevel approach. Emotion 2008, 8, 662–667. [Google Scholar] [CrossRef] [PubMed]
- Thomsen, D.K.; Yung Mehlsen, M.; Christensen, S.; Zachariae, R. Rumination—Relationship with negative mood and sleep quality. Pers. Individ. Differ. 2003, 34, 1293–1301. [Google Scholar] [CrossRef]
- Böhmer, M.N.; Oppewal, A.; Valstar, M.J.; Bindels, P.J.E.; van Someren, E.J.W.; Maes-Festen, D.A.M. Light up: An intervention study of the effect of environmental dynamic lighting on sleep–wake rhythm, mood and behaviour in older adults with intellectual disabilities. J. Intellect. Disabil. Res. 2022, 66, 756–781. [Google Scholar] [CrossRef]
- Kim, S.J.; Lee, S.H.; Suh, I.B.; Jang, J.W.; Jhoo, J.H.; Lee, J.H. Positive effect of timed blue-enriched white light on sleep and cognition in patients with mild and moderate Alzheimer’s disease. Sci. Rep. 2021, 11, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Urbanová, L.; Vaníček, O.; Červená, K.; Bartoš, A.; Evansová, K. The impact of sleep education, light intervention and relaxation on sleep and mood in the elderly. Chronobiol. Int. 2024, 41, 567–576. [Google Scholar] [CrossRef] [PubMed]
- Lohr, K.N. Medicare: A Strategy for Quality Assurance; National Academies Press: Washington, DC, USA, 1990; Volume 1. [Google Scholar]
- Armony, J.; Vuilleumier, P. The Cambridge Handbook of Human Affective Neuroscience; Cambridge University Press: Cambridge, UK, 2013. [Google Scholar]
- Zhang, L.; Zhao, Z.-X. Objective and subjective measures for sleep disorders. Neurosci. Bull. 2008, 23, 236–240. [Google Scholar] [CrossRef]
- Wilson, D.B. Practical Meta-Analysis Effect Size Calculator (Version 2023.11.27). 2023. Available online: https://www.campbellcollaboration.org/calculator/ (accessed on 5 August 2025).
- Savva, G.M.; Wharton, S.B.; Ince, P.G.; Forster, G.; Matthews, F.E.; Brayne, C. Age, Neuropathology, and Dementia. N. Engl. J. Med. 2009, 360, 2302–2309. [Google Scholar] [CrossRef] [PubMed]
- Nicholl, C.G.; Wilson, J. Elderly Care Medicine; John Wiley & Sons: Hoboken, NJ, USA, 2012. [Google Scholar]
- International Commission on Illumination (CIE). CIE System for Metrology of Optical Radiation for ipRGC-Influenced Responses to Light (CIE S 026/E:2018). Available online: https://cie.co.at/publications/cie-system-metrology-optical-radiation-iprgc-influenced-responses-light-0 (accessed on 18 September 2024).


| Publication Number | PSQI |
|---|---|
| #4 | 0.037 |
| #6 | NS |
| #7 | <0.001 |
| #9 | NS |
| #13 | <0.001 * |
| #14 | 0.026 * |
| #16 | 0.01 |
| #17 | <0.001 |
| #19 | 0.013 |
| Publication Number | TIB | TST | Light/Dark Ratio | IS | IV | Actual Sleep Time | SE | SOL | Daytime Naps | WASO |
|---|---|---|---|---|---|---|---|---|---|---|
| #5 | <0.05 | <0.05 | NS | NS | ||||||
| #6 | 0.04 | NS | NS | NS | ||||||
| #7 | 0.08 | 0.049 | 0.3 | 0.15 | 0.08 | 0.1 | ||||
| #8 | 0.429 | 0.113 | 0.592 | 0.186 | ||||||
| #9 | ||||||||||
| #11 | 0.28 | 0.63 | 0.61 | 0.89 | ||||||
| #12 | 0.13 | 0.01 | 0.04 | 0.07 | 0.17 | |||||
| #13 | 0.28 | 0.92 | 0.86 | |||||||
| #14 | 0.62 | 0.67 | 0.187 | 0.48 | 0.453 | |||||
| #17 | 0.97 | 0.09 | ||||||||
| #18 | 0.001 | |||||||||
| #19 | 0.001 | 0.001 | 0.005 |
| Publication Number | Number of Participants in Control Group | Duration (Days) | Baseline Measurements (B) | Number of Lighting Intervention (LI) | Duration of Light Exposure | Washout Time (W) | Mode of Exposure |
|---|---|---|---|---|---|---|---|
| #2 | 11 | 56 | n/a | 2 | 1 h | n/a | Room Lighting |
| #3 | n/a | 126 | n/a | 2 | 21 days | n/a | Room Lighting |
| #6 | n/a | 90 | 14 days | 1 | 28 days | 7 days | Room Lighting |
| #7 | n/a | 98 | 7 days | 2 | 28 days | 28 days | Room Lighting |
| #8 | n/a | 36 | 7 days | 2 | 2–3 h | n/a | Room Lighting |
| #9 | n/a | <365 | n/a | n/a | 5 days | n/a | Natural Light |
| #12 | n/a | 210 | 70 days | 1 | 98 days | n/a | Room Lighting |
| #13 | n/a | 175 | 7 days | 1 | 168 days | n/a | Room Lighting |
| #16 | n/a | 63 | 7 days | 1 | 28 days | n/a | Room Lighting |
| #18 | n/a | 7 | n/a | n/a | n/a | n/a | Natural Light |
| #19 | n/a | 41 | 9 days and 7 days | 2 | 9 days | 7 days | Room Lighting |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, F.; Gocer, O.; Hu, W. Lighting and Sleep Quality in the Elderly: A Systematic Review to Inform Future Research Design. Buildings 2025, 15, 3142. https://doi.org/10.3390/buildings15173142
Zhou F, Gocer O, Hu W. Lighting and Sleep Quality in the Elderly: A Systematic Review to Inform Future Research Design. Buildings. 2025; 15(17):3142. https://doi.org/10.3390/buildings15173142
Chicago/Turabian StyleZhou, Fansong, Ozgur Gocer, and Wenye Hu. 2025. "Lighting and Sleep Quality in the Elderly: A Systematic Review to Inform Future Research Design" Buildings 15, no. 17: 3142. https://doi.org/10.3390/buildings15173142
APA StyleZhou, F., Gocer, O., & Hu, W. (2025). Lighting and Sleep Quality in the Elderly: A Systematic Review to Inform Future Research Design. Buildings, 15(17), 3142. https://doi.org/10.3390/buildings15173142








