The Association between Perceived Housing Environment and Health and Satisfaction among the Older Adults during the COVID-19 Pandemic: A Cross-Sectional Survey in Northern China
Abstract
1. Introduction
1.1. Background
1.2. Literature Review
1.2.1. Housing Environmental Qualities and Health: General Knowledge
1.2.2. Housing Environmental Qualities and the Health and Well-Being of Older Adults in Foreign Countries
1.2.3. Housing Environmental Qualities and the Health and Well-Being of Older Adults in China
1.3. Research Problems
1.4. Research Questions
2. Materials and Methods
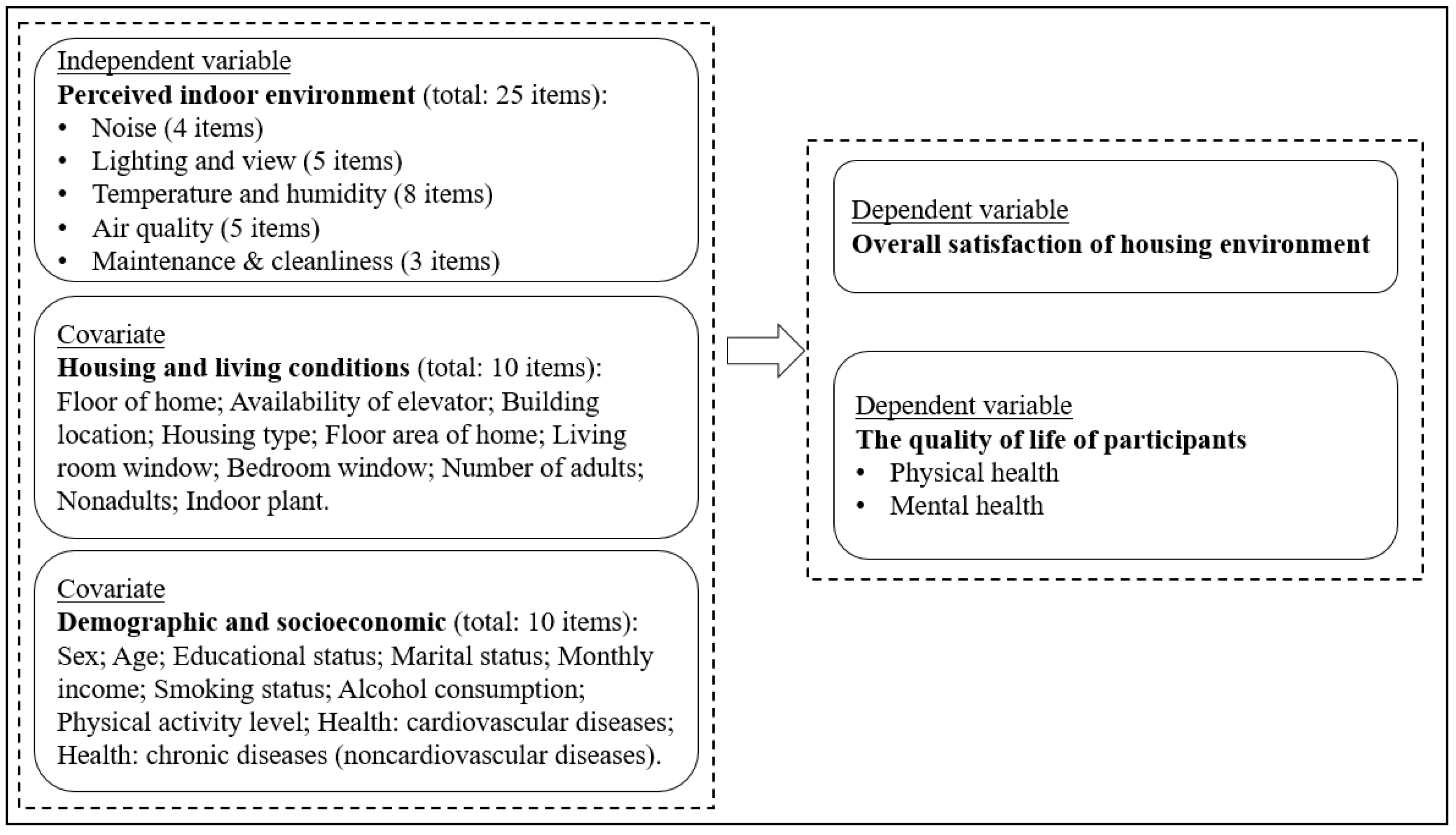
2.1. Conceptual Framework
2.2. Survey and Respondents
- Chinese adults 60 years and older
- normal cognitive functions (no Alzheimer’s disease, normal memory, and logical thinking)
- no serious hearing (hearing aid needed) or visual impairments (suffer from glaucoma or age-related macular degeneration [55])
- receiving care at home
- ability to respond to survey questions
- provided voluntary consent to participate in the study

| Variable | Item | n | Percentage |
|---|---|---|---|
| Sex | Female | 210 | 59 |
| Male | 146 | 41 | |
| Age | 60–69 years | 198 | 55.6 |
| 70–79 years | 122 | 34.3 | |
| ≥80 years | 36 | 10.1 | |
| Educational status | Primary school and below | 80 | 22.5 |
| Secondary school | 89 | 25 | |
| High school | 55 | 15.4 | |
| High school (professional education) | 36 | 10.1 | |
| College | 46 | 12.9 | |
| University and above | 50 | 14 | |
| Marital status | Married | 293 | 82.3 |
| Single | 3 | 0.8 | |
| Widowed | 50 | 14 | |
| Divorced | 10 | 2.8 | |
| Other | 0 | 0 | |
| Monthly income | Below RMB 2000 (USD 300) | 62 | 17.4 |
| RMB 2000–3000 (USD 300–450) | 82 | 23 | |
| RMB 3000–4000 (USD 450–600) | 77 | 21.6 | |
| RMB 4000–5000 (USD 600–750) | 53 | 14.9 | |
| RMB 5000 (USD 750) and above | 66 | 18.5 | |
| Do not want to say | 16 | 4.5 | |
| Smoking status | Never smoked | 230 | 64.6 |
| Current smoker | 41 | 11.5 | |
| Former smoker | 85 | 23.9 | |
| Alcohol consumption | Non-drinker | 171 | 48 |
| Light drinker | 138 | 38.8 | |
| Moderate drinker | 36 | 10.1 | |
| Heavy drinker | 11 | 3.1 | |
| Physical activity intensity | Never | 37 | 10.4 |
| Light | 244 | 68.5 | |
| Moderate | 62 | 17.4 | |
| Vigorous | 13 | 3.7 | |
| Health: cardiovascular diseases | Yes | 154 | 43.3 |
| No | 195 | 54.8 | |
| Health: chronic diseases (noncardiovascular) | Yes | 161 | 45.2 |
| No | 195 | 54.8 |
2.3. Research Design and Measures
2.4. Data Analysis
3. Results
3.1. Description of Housing Conditions
3.2. Scale of Perceived Housing Environment: Principal Component Analysis (PCA) and Reliability
3.3. Descriptive Statistics and Correlation Analysis
3.4. Effect of Perceived Housing Environment on Overall Satisfaction
- Model 1: Model 1 indicated that there was a significant predicting role of the four environmental variables for overall satisfaction (adjusted R2 = 0.520): lighting and view (B = 0.239, p < 0.01), temperature and humidity (B = 0.350, p < 0.01), air quality (B = 0.231, p < 0.01), and maintenance and cleanliness (B = 0.135, p < 0.01).
- Model 2: When housing and living conditions were entered into the regression model (Model 2), the four environmental variables still significantly predict overall satisfaction (adjusted R2 = 0.528), including lighting and view (B = 0.218, p < 0.01), temperature and humidity (B = 0.342, p < 0.01), air quality (B = 0.220, p < 0.01), and maintenance and cleanliness (B = 0.159, p < 0.01).
- Model 3: After controlling for demographic and socioeconomic status and housing factors, Model 3 (adjusted R2 = 0.518) showed the same results as Models 1 and 2: a significant predicting role of lighting and view (B = 0.223, p < 0.01), temperature and humidity (B = 0.344, p < 0.01), air quality (B = 0.208, p < 0.01), and maintenance and cleanliness (B = 0.152, p < 0.01). However, the effects of noise, housing conditions, and demographic and socioeconomic statuses on overall satisfaction were not significant (p > 0.05). Additionally, there were no significant differences among the R2 values of the three models (p > 0.05).
| Variable | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| B | SE | B | SE | B | SE | |
| Constant | 0.097 | 0.198 | −0.610 | 0.494 | −0.623 | 0.563 |
| Noise | 0.040 | 0.045 | 0.051 | 0.045 | 0.062 | 0.047 |
| Lighting and view | 0.239 ** | 0.061 | 0.218 ** | 0.062 | 0.223 ** | 0.064 |
| Temperature and humidity | 0.350 ** | 0.067 | 0.342 ** | 0.069 | 0.344 ** | 0.071 |
| Air quality | 0.231 ** | 0.073 | 0.220 ** | 0.075 | 0.208 ** | 0.077 |
| Maintenance and cleanliness | 0.135 ** | 0.049 | 0.159 ** | 0.051 | 0.152 ** | 0.053 |
| Floor of home | 0.052 | 0.033 | 0.065 | 0.035 | ||
| Elevator | 0.146 | 0.086 | 0.163 | 0.089 | ||
| Building location | 0.003 | 0.025 | −0.011 | 0.028 | ||
| Housing type | 0.071 | 0.047 | 0.074 | 0.048 | ||
| Home area | 0.083 | 0.062 | 0.088 | 0.063 | ||
| Number of adults | −0.049 | 0.027 | −0.048 | 0.028 | ||
| Nonadults | −0.105 | 0.068 | −0.091 | 0.070 | ||
| Living room window | 0.151 | 0.120 | 0.160 | 0.124 | ||
| Bedroom window | 0.033 | 0.236 | 0.007 | 0.248 | ||
| Indoor plants | 0.038 | 0.037 | 0.032 | 0.040 | ||
| Sex | 0.043 | 0.069 | ||||
| Age | −0.005 | 0.051 | ||||
| Educational status | −0.017 | 0.023 | ||||
| Marital status | 0.007 | 0.032 | ||||
| Monthly income | −0.022 | 0.027 | ||||
| Smoking status | −0.001 | 0.044 | ||||
| Alcohol consumption | 0.011 | 0.047 | ||||
| Physical activity level | 0.008 | 0.055 | ||||
| Health: cardiovascular diseases | −0.009 | 0.068 | ||||
| Health: chronic diseases | 0.011 | 0.070 | ||||
| Adjusted R2 | 0.520 | 0.528 | 0.518 | |||
| ∆ R2 | 0.008 | 0.010 | ||||
3.5. Effect of Perceived Housing Environment on Respondents’ Physical Health (PCM)
- Model 1: Model 1 found significant predicting roles for air quality (B = 2.322, p < 0.01) with an adjusted R2 of 0.237.
- Model 2: With the inclusion of housing conditions in Model 2, air quality (B = 2.409, p < 0.01) and home floor (B = 0.847, p < 0.05) significantly predict physical health. However, the increase in R2 in Model 2 was not significant (p > 0.05).
- Model 3: After adding demographic and socioeconomic factors to Model 3, the adjusted R2 value increased significantly from 0.297 (Model 2) to 0.500 (Model 3) (p < 0.01). Compared with Model 2, the effect of noise on physical health was lower in Model 3 (B = 2.214, p < 0.01), and the effects of the home floor (B = 0.792) were maintained at a similar level (p < 0.05). In Model 3, four demographic and socioeconomic variables can significantly predict the physical health, including age (B = −1.404, p < 0.05), marital status (B = −0.732, p < 0.05), cardiovascular diseases (B = 1.726, p < 0.05) and chronic diseases (B = 3.175, p < 0.01). However, factors such as noise, lighting and view, temperature and humidity, and maintenance and cleanliness had no significant effect on physical health (p > 0.05).
| Variable | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| B | SE | B | SE | B | SE | |
| Constant | 32.293 | 2.430 | 25.316 | 6.088 | 20.713 | 6.320 |
| Noise | 0.262 | 0.550 | 0.357 | 0.558 | 0.105 | 0.526 |
| Lighting and view | −0.795 | 0.747 | −1.174 | 0.759 | −1.072 | 0.720 |
| Temperature and humidity | 0.565 | 0.824 | 0.441 | 0.856 | 0.377 | 0.801 |
| Air quality | 2.322 ** | 0.898 | 2.409 ** | 0.921 | 2.214 * | 0.864 |
| Maintenance and cleanliness | 0.066 | 0.606 | 0.041 | 0.622 | −0.336 | 0.591 |
| Floor of home | 0.847 * | 0.409 | 0.792 * | 0.393 | ||
| Elevator | 1.032 | 1.063 | 1.334 | 1.004 | ||
| Building location | −0.119 | 0.313 | 0.321 | 0.310 | ||
| Housing type | 0.310 | 0.573 | 0.094 | 0.538 | ||
| Home area | 1.204 | 0.769 | 1.272 | 0.713 | ||
| Number of adults | −0.289 | 0.339 | −0.118 | 0.315 | ||
| Nonadults | 0.700 | 0.833 | 0.134 | 0.790 | ||
| Living room window | 0.015 | 1.484 | −0.731 | 1.389 | ||
| Bedroom window | 0.179 | 2.906 | 0.960 | 2.782 | ||
| Indoor plants | 0.284 | 0.451 | 0.217 | 0.444 | ||
| Sex | −0.538 | 0.769 | ||||
| Age | −1.404 * | 0.573 | ||||
| Educational status | 0.407 | 0.261 | ||||
| Marital status | −0.732 * | 0.364 | ||||
| Monthly income | 0.133 | 0.302 | ||||
| Smoking status | 0.834 | 0.494 | ||||
| Alcohol consumption | −0.669 | 0.528 | ||||
| Physical activity level | 0.922 | 0.612 | ||||
| Health: cardiovascular diseases | 1.726 * | 0.767 | ||||
| Health: chronic diseases | 3.175 ** | 0.785 | ||||
| Adjusted R2 | 0.237 | 0.297 | 0.500 | |||
| ∆ R2 | 0.060 | 0.203 ** | ||||
3.6. Effect of Perceived Housing Environment on Respondents’ Mental Health (MCM)
- Model 1: Model 1 revealed that noise (B = 2.099, p < 0.01) significantly predict mental health (adjusted R2 = 0.077).
- Model 2: When housing conditions were included in Model 2, the increase in R2 was significant (p < 0.05). In Model 2, the predicting roles of noise (B = 1.934, p < 0.01), elevator (B = 2.726, p < 0.05) and building location (B = −1.258, p < 0.01) were significant.
- Model 3: The adjusted R2 value increased significantly from 0.103 (Model 2) to 0.204 (Model 3) after demographic and socioeconomic factors were entered into Model 3 (p < 0.01). In Model 3, the predicting role of noise was significant (B = 1.445, p < 0.05). In addition, three demographic and socioeconomic variables—educational level (B = 0.853, p < 0.05), monthly income (B = 1.025, p < 0.05), and alcohol consumption (B = 2.227, p < 0.01) —could significantly predict mental health. However, the other four environmental variables (lighting and view, temperature and humidity, air quality, and maintenance and cleanliness), and housing conditions had no significant effect on mental health (p > 0.05).
| Variable | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| B | SE | B | SE | B | SE | |
| Constant | 30.206 | 3.185 | 29.329 | 7.889 | 22.316 | 8.384 |
| Noise | 2.099 ** | 0.722 | 1.934 ** | 0.722 | 1.445 * | 0.698 |
| Lighting and view | −0.075 | 0.980 | −0.413 | 0.984 | −0.073 | 0.954 |
| Temperature and humidity | 1.942 | 1.080 | 1.491 | 1.109 | 1.210 | 1.062 |
| Air quality | −0.407 | 1.178 | 0.118 | 1.194 | 0.056 | 1.145 |
| Maintenance and cleanliness | 1.110 | 0.795 | 0.706 | 0.806 | 0.440 | 0.784 |
| Floor level of home | 0.972 | 0.530 | 0.140 | 0.521 | ||
| Elevator | 2.726 * | 1.377 | 1.752 | 1.331 | ||
| Building location | −1.258 ** | 0.406 | −0.384 | 0.411 | ||
| Housing type | 0.517 | 0.743 | 0.001 | 0.713 | ||
| Home area | 0.201 | 0.996 | 0.342 | 0.946 | ||
| Number of adults | −0.429 | 0.439 | −0.210 | 0.418 | ||
| Nonadults | −0.426 | 1.079 | −0.295 | 1.047 | ||
| Living room window | −0.449 | 1.923 | −0.746 | 1.842 | ||
| Bedroom window | 0.811 | 3.765 | −0.325 | 3.691 | ||
| Indoor plants | 0.178 | 0.585 | 0.305 | 0.589 | ||
| Sex | 1.874 | 1.020 | ||||
| Age | −1.194 | 0.760 | ||||
| Educational status | 0.853 * | 0.347 | ||||
| Marital status | −0.143 | 0.483 | ||||
| Monthly income | 1.025 * | 0.401 | ||||
| Smoking status | −0.699 | 0.655 | ||||
| Alcohol consumption | 2.227 ** | 0.700 | ||||
| Physical activity level | 0.721 | 0.812 | ||||
| Health: cardiovascular diseases | 0.335 | 1.018 | ||||
| Health: chronic diseases | 0.749 | 1.041 | ||||
| Adjusted R2 | 0.077 | 0.103 | 0.204 | |||
| ∆ R2 | 0.026 * | 0.101 ** | ||||
4. Discussion
4.1. Relationship between Key Housing Environmental Factors and Overall Satisfaction and the Health of Older Adults
4.2. Role of Demographic and Socioeconomic Variables
4.3. Proposed Design Strategies
4.4. Strengths
4.5. Limitations
5. Conclusions and Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization (WHO). Adolescent Health and Ageing Data Portal. 2021. Available online: https://www.who.int/health-topics/adolescenthealth#tab=tab_1 (accessed on 1 May 2023).
- World Health Organization (WHO). World Report on Ageing and Health. 2015. Available online: https://apps.who.int/iris/handle/10665/186463 (accessed on 1 May 2023).
- World Health Organization (WHO). National Programmes for Age-Friendly Cities and Communities: A Guide. Switzerland. 2023. Available online: https://www.who.int/teams/social-determinants-of-health/demographic-change-and-healthy-ageing/age-friendly-environments/national-programmes-afcc (accessed on 1 May 2023).
- National Bureau of Statistics of China. China Statistical Yearbook 2021. Available online: http://www.stats.gov.cn/tjsj/ndsj/2021/indexch.htm (accessed on 1 October 2022).
- Ministry of Housing and Urban-Rural Development of the People’s Republic of China. Code for Design of Residential Building for the Aged (GB50340P-2016); China Architecture Building Press: Beijing, China, 2016. [Google Scholar]
- Ministry of Housing and Urban-Rural Development of the People’s Republic of China. Standard for Design of Care Facilities for the Aged (JGJ 450-2018); China Architecture Building Press: Beijing, China, 2018. [Google Scholar]
- Gan, W.; Sanderson, W.T.; Browning, S.; Mannino, D.M. Different types of housing and respiratory health outcomes. Prev. Medep. 2017, 7, 124–129. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). WHO Housing and Health Guidelines. Switzerland. 2018. Available online: https://www.who.int/publications (accessed on 1 August 2022).
- The Office of the Deputy Prime Minster. Housing Health and Safety Rating System: Operating Guidance. London, UK. 2006. Available online: https://assets.publishing.service.gov.uk (accessed on 1 August 2022).
- Pevalin, D.J.; Reeves, A.; Baker, E.; Bentley, R. The impact of persistent poor housing conditions on mental health: A longitudinal population-based study. Prev. Med. 2017, 105, 304–310. [Google Scholar] [CrossRef] [PubMed]
- Jensen, H.A.R.; Rasmussen, B.; Ekholm, O. Neighbour noise annoyance is associated with various mental and physical health symptoms: Results from a nationwide study among individuals living in multi-storey housing. BMC Public Health 2019, 19, 1508. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, E. City dweller responses to multiple stressors intruding into their homes: Noise, light, odour, and vibration. Int. J. Environ. Public Health 2015, 12, 3246–3263. [Google Scholar] [CrossRef] [PubMed]
- National Center for Healthy Housing American Public Health Association. National Healthy Housing Standardolumbia, MD: National Center for Healthy Housing. 2014. Available online: https://nchh.org/resource-library/national-healthy-housing-standard (accessed on 1 August 2022).
- Aries, M.B.C.; Aarts, M.P.J.; Hoof, J.V. Daylight and health: A review of the evidence and consequences for the built environment. Light. Res. Technol. 2015, 47, 6–27. [Google Scholar] [CrossRef]
- Morales-Bravo, J.; Navarrete-Hernandez, P. Enlightening wellbeing in the home: The impact of natural light design on perceived happiness and sadness in residential spaces. Build. Environ. 2022, 223, 109317. [Google Scholar] [CrossRef]
- Nagare, R.; Woo, M.; MacNaughton, P.; Plitnick, B.; Tinianov, B.; Figueiro, M. Access to daylight at home improves circadian alignment, sleep, and mental health in healthy adults: A crossover study. Int. J. Environ. Public Health 2021, 18, 9980. [Google Scholar] [CrossRef]
- Saeki, K.; Obayashi, K.; Iwamoto, J.; Tanaka, Y.; Tanaka, N.; Takata, S.; Kubo, H.; Okamoto, N.; Tomioka, K.; Nezu, S.; et al. Influence of room heating on ambulatory blood pressure in winter: A randomised controlled study. J. Epidemiol. Commun. Health 2013, 67, 484–490. [Google Scholar] [CrossRef]
- Kanno, I.; Hasegawa, K.; Nakamura, T.; Kogure, M.; Itabashi, F.; Narita, A.; Tsuchiya, N.; Hirata, T.; Nakaya, N.; Sugawara, J.; et al. Relationship between the housing coldness/warmth evaluation by CASBEE Housing Health Checklist and psychological distress based on TMM Community-Based Cohort Study: A cross-sectional analysis. Public Health 2022, 208, 98–104. [Google Scholar] [CrossRef]
- Sharpe, R.A.; Bearman, N.; Thornton, C.; Husk, K.; Osborne, N.J. Indoor fungal diversity and asthma: A meta-analysis and systematic review of risk factors. J. Allergy Clin. Immunol. 2015, 135, 110–122. [Google Scholar] [CrossRef]
- Jaakkola, M.S.; Quansah, R.; Hugg, T.T.; Heikkinen, S.A.M.; Jaakkola, J.J.K. Association of indoor dampness and molds with rhinitis risk: A systematic review and meta-analysis. J. Allergy Clin. Immunol. 2013, 132, 1099–1110. [Google Scholar] [CrossRef] [PubMed]
- Liddell, C.; Guiney, C. Living in a cold and damp home: Frameworks for understanding impacts on mental well-being. Public Health 2015, 129, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Lee, C.L.; Shirowzhan, S. Macro-Impacts of Air Quality on Property Values in China—A Meta-Regression Analysis of the Literature. Buildings 2021, 11, 48. [Google Scholar] [CrossRef]
- Wang, J.; Lee, C.L. The value of air quality in housing markets: A comparative study of housing sale and rental markets in China. Energy Policy 2022, 160, 112601. [Google Scholar] [CrossRef]
- Cheung, T.; Schiavon, S.; Graham, L.T.; Tham, K.W. Occupant satisfaction with the indoor environment in seven commercial buildings in Singapore. Build. Environ. 2020, 188, 107443. [Google Scholar] [CrossRef]
- Department of Health. Care Homes for Older People: National Minimum Standards and the Care Homes Regulations 2001; TSO: London, UK, 2003. [Google Scholar]
- Joseph, A.; Choi, Y.; Quan, X. Impact of the Physical Environment of Residential Health, Care, and Support Facilities (RHCSF) on Staff and Residents: A Systematic Review of the Literature. Environ. Behav. 2016, 48, 1203–1241. [Google Scholar] [CrossRef]
- Blatteis, C.M. Age-dependent changes in temperature regulation: A mini review. Gerontology 2012, 58, 289–295. [Google Scholar] [CrossRef]
- Soebarto, V.; Bennetts, H.; Hansen, A.; Zuo, J.; Williamson, T.; Pisaniello, D.; Hoof, J.V.; Visvanathan, R. Living environment, heating-cooling behaviours and well-being: Survey of older South Australians. Build. Environ. 2019, 157, 215–226. [Google Scholar] [CrossRef]
- Sunwoo, Y.; Chou, C.; Takeshita, J.; Murakami, M.; Tochihara, Y. Physiological and subjective responses to low relative humidity in young and elderly men. J. Physiol. Anthropol. 2006, 25, 229–238. [Google Scholar] [CrossRef]
- Jin, Y.; Wang, F.; Carpenter, M.; Weller, R.B.; Tabor, D.; Payne, S. The effect of indoor thermal and humidity condition on the oldest-old people’s comfort and skin condition in winter. Build. Environ. 2020, 174, 106790. [Google Scholar] [CrossRef]
- Falkenberg, H.K.; Kvikstad, T.M.; Eilertsen, G. Improved indoor lighting improved healthy aging at home—An intervention study in 77-year-old Norwegians. J. Multidiscip. Healthc. 2019, 12, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Freeman, E.; Muñoz, B.; Rubin, G.; West, S. Visual field loss increases the risk of falls in older adults: The Salisbury eye evaluation. Investig. Ophthalmol. Vis. Sci. 2007, 48, 4445–4450. [Google Scholar] [CrossRef] [PubMed]
- van der Aa, H.P.; Comijs, H.C.; Penninx, B.W.; van Rens, G.H.; van Nispen, R.M. Major depressive and anxiety disorders in visually impaired older adults. Investig. Ophthalmol. Vis. Sci. 2015, 56, 849–854. [Google Scholar] [CrossRef] [PubMed]
- Grandner, M.A.; Kripke, D.F.; Langer, R.D. Light exposure is related to social and emotional functioning and to quality of life in older women. Psychiatry Res. 2006, 143, 35–42. [Google Scholar] [CrossRef]
- Shishegar, N.; Boubekri, M.; Stine-Morrow, E.A.; Rogers, W.A. Tuning environmental lighting improves objective and subjective sleep quality in older adults. Build. Environ. 2021, 204, 108096. [Google Scholar] [CrossRef]
- Azuma, K.; Uchiyama, I. Association between environmental noise and subjective symptoms related to cardiovascular diseases among elderly individuals in Japan. PLoS ONE 2017, 12, e0188236. [Google Scholar] [CrossRef]
- Riedel, N.; Köckler, H.; Scheiner, J.; van Kamp, I.; Erbel, R.; Loerbroks, A.; Claßen, T.; Bolte, G. Home as a Place of Noise Control for the Elderly? A Cross-Sectional Study on Potential Mediating Effects and Associations between Road Traffic Noise Exposure, Access to a Quiet Side, Dwelling-Related Green and Noise Annoyance. Int. J. Environ. Public Health 2018, 15, 1036. [Google Scholar] [CrossRef]
- Braithwaite, I.; Zhang, S.; Kirkbride, J.B.; Osborn, D.P.J.; Hayes, J. Air pollution (Particulate matter) exposure and associations with depression, anxiety, bipolar, psychosis and suicide risk: A systematic review and meta-analysis. Environ. Health Perspect. 2019, 127, 126002. [Google Scholar] [CrossRef]
- Mulliner, E.; Riley, M.; Maliene, V. Older people’s preferences for housing and environment characteristics. Sustainability 2020, 12, 5723. [Google Scholar] [CrossRef]
- Bian, Y.; Li, L. The Chinese General Social Survey (2003-8). Chin. Sociol. 2021, 45, 70–97. [Google Scholar] [CrossRef]
- Guo, M.; Zhou, M.; Li, B.; Du, C.; Yao, R.; Wang, L.; Yang, X.; Yu, W. Reducing indoor relative humidity can improve the circulation and cardiorespiratory health of older people in a cold environment: A field trial conducted in Chongqing, China. Sci. Total Environ. 2022, 817, 152695. [Google Scholar] [CrossRef] [PubMed]
- Guo, M.; Du, C.; Li, B.; Yao, R.; Tang, Y.; Jiang, Y.; Liu, H.; Su, H.; Zhou, Y.; Wang, L.; et al. Reducing particulates in indoor air can improve the circulation and cardiorespiratory health of old people: A randomized, double-blind crossover trial of air filtration. Sci. Total Environ. 2021, 798, 149248. [Google Scholar] [CrossRef]
- Tao, Y.; Gou, Z.; Yu, Z.; Fu, J.; Chen, X. The challenge of creating age-friendly indoor environments in a high-density city: Case study of Hong Kong’s care and attention homes. J. Build. Eng. 2020, 30, 101280. [Google Scholar] [CrossRef]
- Mu, J.; Kang, J. Indoor environmental quality of residential elderly care facilities in northeast China. Front. Public Health 2022, 10, 860976. [Google Scholar] [CrossRef]
- Leung, M.; Wang, C.; Chan, I.Y.S. A qualitative and quantitative investigation of effects of indoor built environment for people with dementia in care and attention homes. Build. Environ. 2019, 157, 89–100. [Google Scholar] [CrossRef]
- Zhang, F.; Shi, L.; Liu, S.; Cheng, M.; Zeng, F.; Li, J. Satisfaction among the Elderly Living in the Ancient Town of Xiangxi. Buildings 2023, 13, 1334. [Google Scholar] [CrossRef]
- Cui, P.; Zhang, J.; Li, T. Research on Acoustic Environment in the Building of Nursing Homes Based on Sound Preference of the Elderly People: A Case Study in Harbin, China. Front. Psychol. 2021, 12, 707457. [Google Scholar] [CrossRef]
- Li, L.; Sun, N.; Yu, L.; Dong, X.; Zhao, J.; Ying, Y. The Needs of Older Adults with Disabilities With Regard to Adaptation to Aging and Home Care: Questionnaire Study. JMIR Rehabil. Assist. Technol. 2020, 7, 16012. [Google Scholar] [CrossRef]
- Ju, K.; Lu, L.; Chen, T.; Duan, Z.; Chen, D.; Liao, W.; Zhou, Q.; Xu, Z.; Wang, W. Does long-term exposure to air pollution impair physical and mental health in the middle-aged and older adults?—A causal empirical analysis based on a longitudinal nationwide cohort in China. Sci. Total Environ. 2022, 827, 154312. [Google Scholar] [CrossRef]
- Leung, M.; Liang, Q. Developing structural facilities management–quality of life models for the elderly in the common areas of public and subsidized housings. Habitat Int. 2019, 94, 102067. [Google Scholar] [CrossRef]
- Li, C.; Zhou, Y. Residential environment and depressive symptoms among Chinese middle- and old-aged adults: A longitudinal population-based study. Health Place 2020, 66, 102463. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Cui, P.Y.; Pan, Y.Y.; Li, Y.X.; Waili, N.; Li, Y. Association between housing environment and depressive symptoms among older people: A multidimensional assessment. BMC Geriatr. 2021, 21, 259. [Google Scholar] [CrossRef] [PubMed]
- Krings, M.F.; van Wijngaarden, J.D.H.; Yuan, S.; Huijsman, R. China’s Elder Care Policies 1994–2020: A Narrative Document Analysis. Int. J. Environ. Public Health 2022, 19, 6141. [Google Scholar] [CrossRef] [PubMed]
- Kesmodel, U. Cross-sectional studies-what are they good for? Acta Obstet. Gynecol. Scand. 2018, 97, 388–393. [Google Scholar] [CrossRef]
- Haanes, G.G.; Hall, E.O.C.; Eilertsen, G. Acceptance and adjustment: A qualitative study of experiences of hearing and vision impairments and daily life among oldest old recipients of home care. Int. J. Older People Nurs. 2019, 14, 12236. [Google Scholar] [CrossRef]
- Vrdoljak, D.; Marković, B.B.; Puljak, L.; Lalić, D.I.; Kranjčević, K.; Vučak, J. Lifestyle intervention in general practice for physical activity, smoking, alcohol consumption and diet in elderly: A randomized controlled trial. Arch. Gerontol. Geriatr. 2014, 58, 160–169. [Google Scholar] [CrossRef]
- Jin, L.; Huang, Y.; Bi, Y.; Zhao, L.; Xu, M.; Xu, Y.; Chen, Y.; Gu, L.; Dai, M.; Wu, Y.; et al. Association between alcohol consumption and metabolic syndrome in 19,215 middle-aged and elderly Chinese. Diabet. Reslin. Pract. 2011, 92, 386–392. [Google Scholar] [CrossRef]
- Ran, J.; Zhang, Y.; Han, L.; Sun, S.; Zhao, S.; Shen, C.; Zhang, X.; Chan, K.P.; Lee, R.S.; Qiu, Y.; et al. The joint association of physical activity and fine particulate matter exposure with incident dementia in elderly Hong Kong residents. Environ. Int. 2021, 156, 106645. [Google Scholar] [CrossRef]
- Saqlain, M.; Riaz, A.; Ahmed, A.; Kamran, S.; Bilal, A.; Ali, H. Predictors of Health-Related Quality-of-Life Status Among Elderly Patients with Cardiovascular Diseases. Value Health Reg. Issues 2021, 24, 130–140. [Google Scholar] [CrossRef]
- Hao, L.J.; Omar, M.S.; Tohit, N. Polypharmacy and Willingness to Deprescribe Among Elderly with Chronic Diseases. Int. J. Gerontol. 2018, 12, 340–343. [Google Scholar]
- Weuve, J.; D’Souza, J.; Beck, T.; Evans, D.A.; Kaufman, J.D.; Rajan, K.B.; de Leon, C.F.M.; Adar, S.D. Long-term community noise exposure in relation to dementia, cognition, and cognitive decline in older adults. Alzheimers. Dement. 2021, 17, 525–533. [Google Scholar] [CrossRef] [PubMed]
- Thompson, R.; Smith, R.B.; Bou, K.Y.; Shen, C.; Drummond, K.; Teng, C.; Toledano, M.B. Noise pollution and human cognition: An updated systematic review and meta-analysis of recent evidence. Environ. Int. 2022, 158, 106905. [Google Scholar] [CrossRef] [PubMed]
- Durvasula, S.; Kok, C.; Sambrook, P.N.; Cumming, R.G.; Lord, S.R.; March, L.M.; Mason, R.S.; Seibel, M.J.; Simpson, J.M.; Cameron, I.D. Sunlight and health: Attitudes of older people living in intermediate care facilities in southern Australia. Arch. Gerontol. Geriatr. 2010, 51, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Guo, B.; Shi, Y.; Jia, C.; Li, X.; Liu, F. Interior daylight environment of an elderly nursing home in Beijing. Build. Environ. 2021, 200, 107915. [Google Scholar] [CrossRef]
- Ahrentzen, S.; Erickson, J.; Fonseca, E. Thermal and health outcomes of energy efficiency retrofits of homes of older adults. Indoor Air 2016, 26, 582–593. [Google Scholar] [CrossRef]
- Huang, X.; Ma, W.; Law, C.; Luo, J.; Zhao, N. Importance of applying Mixed Generalized Additive Model (MGAM) as a method for assessing the environmental health impacts: Ambient temperature and Acute Myocardial Infarction (AMI), among elderly in Shanghai, China. PLoS ONE 2021, 16, 0255767. [Google Scholar] [CrossRef]
- Grande, G.; Ljungman, P.L.S.; Eneroth, K.; Bellander, T.; Rizzuto, D. Association Between Cardiovascular Disease and Long-term Exposure to Air Pollution with the Risk of Dementia. JAMA Neurol. 2020, 77, 801–809. [Google Scholar] [CrossRef]
- Norbäck, D.; Zhang, X.; Fan, Q.; Zhang, Z.; Zhang, Y.; Li, B.; Zhao, Z.; Huang, C.; Deng, Q.; Lu, C.; et al. Home environment and health: Domestic risk factors for rhinitis, throat symptoms and non-respiratory symptoms among adults across China. Sci. Total Environ. 2019, 681, 320–330. [Google Scholar] [CrossRef]
- Ware, J.; Kosinski, M.A.; Tuner-Bowker, D.M.; Gandek, B. Version 2 of the SF12 health survey. SPINE 2002, 25, 3130–3139. [Google Scholar] [CrossRef]
- Pironi, L.; Paganelli, F.; Mosconi, P.; Morselli-Labate, A.M.; Spinucci, G.; Merli, C.; Guidetti, M.; Miglioli, M. The SF-36 Instrument for the Follow-Up of Health-Related Quality-Of-Life Assessment of Patients Undergoing Home Parenteral Nutrition for Benign Disease. Transplant. Proc. 2004, 36, 255–258. [Google Scholar] [CrossRef]
- Grassi, M.; Nucera, A. Dimensionality and Summary Measures of the SF-36 v1.6: Comparison of Scale- and Item-Based Approach Across ECRHS II Adults Population. Value Health 2010, 13, 469–478. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chiatti, C.; Westerlund, Y.; Ståhl, A. Access to public mobility services and health in old age: A cross-sectional study in three Swedish cities. J. Transp. Health 2017, 7, 218–226. [Google Scholar] [CrossRef]
- Ormandy, D. Housing and Health in Europe: The WHO LARES Project; Routledge: London, UK, 2009. [Google Scholar]
- Lyu, Y.; Forsyth, A.; Worthington, S. Built Environment and Self-Rated Health: Comparing Young, Middle-Aged, and Older People in Chengdu, China. HERD 2021, 14, 229–246. [Google Scholar] [CrossRef]
- Frehlich, L.; Christie, C.; Ronksley, P.; Turin, T.C.; Doyle-Baker, P.; McCormack, G. Association between neighbourhood built environment and health-related fitness: A systematic review protocol. JBI Evid. Synth. 2021, 19, 2350–2358. [Google Scholar] [CrossRef] [PubMed]
- Forchuk, C.; Dickins, K.; Corring, D.J. Social Determinants of Health: Housing and Income. Healthc. Q. 2016, 18, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Wu, F.; Guo, Y.; Zheng, Y.; Ma, W.; Kowal, P.; Chatterji, S.; Wang, L. Social-Economic Status and Cognitive Performance among Chinese Aged 50 Years and Older. PLoS ONE 2016, 11, e0166986. [Google Scholar] [CrossRef] [PubMed]
- Fornell, C.; Larcker, D.F. Evaluating Structural Equation Models with Unobservable Variables and Measurement Error. J. Markes. 1981, 18, 39–50. [Google Scholar]
- Leung, M.; Famakin, I.; Kwok, T. Relationships between indoor facilities management components and elderly people’s quality of life: A study of private domestic buildings. Habitat Int. 2017, 66, 13–23. [Google Scholar] [CrossRef]
- Yaman Sözbir, Ş.; Vural, G.; Ünal Toprak, F. A Study for Testing the Validity and Reliability of the Turkish Version of the Internalized Misogyny Scale. Int. J. Ment. Health Addict. 2020, 19, 1705–1715. [Google Scholar] [CrossRef]
- Ministry of Housing and Urban-Rural Development of the People’s Republic of China. Design Standard for Energy Efficiency of Residential Buildings in Severe Cold and Cold Zones (JGJ 26-2018); China Architecture Building Press: Beijing, China, 2018. [Google Scholar]
- Suzuki, T. Health status of older adults living in the community in Japan: Recent changes and significance in the super-aged society. Geriatr. Gerontol. Int. 2018, 18, 667–677. [Google Scholar] [CrossRef]
- Minghetti, A.; Donath, L.; Hanssen, H.; Roth, R.; Lichtenstein, E.; Zahner, L.; Faude, O. Physical Performance, Cardiovascular Health and Psychosocial Wellbeing in Older Adults Compared to Oldest-Old Residential Seniors. Int. J. Environ. Public Health 2022, 19, 1451. [Google Scholar] [CrossRef] [PubMed]

| Variable | Items | n | Percentage |
|---|---|---|---|
| The floor of your home: | 1 (bungalow) | 96 | 27 |
| ≤3 (multistory) | 69 | 19.4 | |
| 4–6 (multistory) | 106 | 29.8 | |
| 7–9 (multistory) | 29 | 8.1 | |
| ≥10 (multistory) | 56 | 15.7 | |
| Availability of elevator? | Yes | 143 | 40.2 |
| No | 213 | 59.8 | |
| Building location: | City center | 65 | 18.3 |
| Non-city center urban area | 122 | 34.3 | |
| Suburban | 61 | 17.1 | |
| Outer suburban | 26 | 7.3 | |
| Rural area | 82 | 23 | |
| Housing type: | One-bedroom | 24 | 6.7 |
| Two-bedroom | 163 | 45.8 | |
| Three-bedroom | 127 | 35.7 | |
| Other | 42 | 11.8 | |
| Floor area of your home: | <50 m2 | 26 | 7.3 |
| 50–100 m2 | 215 | 60.4 | |
| >100 m2 | 115 | 32.3 | |
| Any windows in your living room? | Yes | 329 | 92.4 |
| No | 27 | 7.6 | |
| Any windows in your bedroom? | Yes | 350 | 98.3 |
| No | 6 | 1.7 | |
| Any nonadults living in your home? | Yes | 123 | 34.6 |
| No | 233 | 65.4 | |
| Number of adults living in your home: | 2.79 ± 1.19 (M + SD) | ||
| Number of indoor plants: | 2.41 ± 0.86 (M + SD) (1 = no, 2 = a little, 3 = some, 4 = a large amount) | ||
| Item | Factor Loadings | Mean | SD | Cronbach’s Alpha |
|---|---|---|---|---|
| Noise | 0.787 | |||
| 1: My home is quiet for most of the day and I can concentrate on my activity. | 0.64 | 3.89 | 0.99 | |
| 2: I am rarely awakened by the noise outside when I sleep at night. | 0.82 | 3.79 | 1.03 | |
| 3: At home, I am rarely disturbed by the outside noise. | 0.85 | 3.57 | 1.04 | |
| 4: How satisfied are you with the noise in your home? | 0.81 | 3.70 | 1.01 | |
| Lighting and view | 0.815 | |||
| 1: The indoor lighting is adequate during the day. | 0.80 | 3.96 | 0.96 | |
| 2: With daylight, I can easily read books and newspapers. | 0.82 | 3.86 | 0.96 | |
| 3: I feel comfortable with the brightness of my home lighting at night. | 0.70 | 3.95 | 0.90 | |
| 4: I am satisfied with the view outside of my home’s windows. | 0.67 | 3.52 | 1.06 | |
| 5: How do you feel satisfied with the lighting in your home? | 0.82 | 3.77 | 0.89 | |
| Temperature and humidity | 0.884 | |||
| 1: In summer, I do not feel hot and stuffy at home. | 0.67 | 3.65 | 0.97 | |
| 2: In spring and autumn, I feel the temperature is ok at home. | 0.75 | 3.96 | 0.85 | |
| 3: In winter, I do not feel cold at home. | 0.71 | 3.56 | 1.07 | |
| 4: In terms of overall temperature environment, how do you feel satisfied with you home throughout the year? | 0.80 | 3.72 | 0.82 | |
| 5: In summer, my house does not feel damp. | 0.74 | 3.85 | 0.89 | |
| 6: In spring and autumn, my house feels neither damp nor dry. | 0.79 | 3.85 | 0.86 | |
| 7: In winter, my house does not feel too dry. | 0.69 | 3.74 | 0.87 | |
| 8: How satisfied are you with the humidity condition in your home throughout the year? | 0.85 | 3.74 | 0.80 | |
| Air quality | 0.793 | |||
| 1: Most of the time. there are few bad odors in my home. | 0.75 | 4.01 | 0.85 | |
| 2: I rarely smell smoke from my neighbors’ kitchens or other odors from the outside. | 0.63 | 3.57 | 1.04 | |
| 3: I do not smell toilet odor at home. | 0.75 | 3.75 | 0.96 | |
| 4: With a good ventilation at home, I rarely feel stuffy. | 0.76 | 3.94 | 0.92 | |
| 5: How satisfied are you with the air quality in your home? | 0.84 | 3.89 | 0.85 | |
| Maintenance and cleanliness | 0.874 | |||
| 1: My home is regularly cleaned, and the floors maintained in good condition. | 0.88 | 3.92 | 0.93 | |
| 2: My home is kept clean and tidy. | 0.91 | 3.77 | 0.92 | |
| 3: How satisfied are you with the maintenance and cleanliness in your home? | 0.90 | 3.86 | 0.87 |
| Variable | Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|---|---|
| Noise | 3.74 | 0.79 | 1 | 0.468 ** | 0.418 ** | 0.504 ** | 0.412 ** | 0.411 ** | 0.130 * | 0.255 ** |
| Lighting and view | 3.81 | 0.72 | 1 | 0.621 ** | 0.666 ** | 0.588 ** | 0.616 ** | 0.120 * | 0.198 ** | |
| Temperature and humidity | 3.76 | 0.66 | 1 | 0.715 ** | 0.505 ** | 0.640 ** | 0.180 ** | 0.234 ** | ||
| Air quality | 3.83 | 0.69 | 1 | 0.615 ** | 0.642 ** | 0.228 ** | 0.212 ** | |||
| Maintenance and cleanliness | 3.85 | 0.81 | 1 | 0.539 ** | 0.137 ** | 0.215 ** | ||||
| Overall satisfaction | 3.88 | 0.82 | 1 | 0.165 ** | 0.174 ** | |||||
| Physical health (PCM) | 41.52 | 7.07 | 1 | −0.002 | ||||||
| Mental health (MCM) | 47.78 | 9.44 | 1 |
| Environmental Factor | Noise | Lighting and View | Temperature and Humidity | Air Quality | Maintenance and Cleanliness |
|---|---|---|---|---|---|
| Present study | + | + | + | + | |
| [31,34] | + | ||||
| [43] | + | + | + | ||
| [44] | + | + | + | + |
| Environmental Factor | Noise | Lighting and View | Temperature and Humidity | Air Quality | Maintenance and Cleanliness |
|---|---|---|---|---|---|
| Present study | + | ||||
| [27,28,29,30,41] | + | ||||
| [31] | + | ||||
| [36] | + | ||||
| [42,49] | + | ||||
| [50] | + |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, F.; Li, Y.; Gao, X.; Du, J. The Association between Perceived Housing Environment and Health and Satisfaction among the Older Adults during the COVID-19 Pandemic: A Cross-Sectional Survey in Northern China. Buildings 2023, 13, 2875. https://doi.org/10.3390/buildings13112875
Liu F, Li Y, Gao X, Du J. The Association between Perceived Housing Environment and Health and Satisfaction among the Older Adults during the COVID-19 Pandemic: A Cross-Sectional Survey in Northern China. Buildings. 2023; 13(11):2875. https://doi.org/10.3390/buildings13112875
Chicago/Turabian StyleLiu, Fang, Yafei Li, Xuezhi Gao, and Jiangtao Du. 2023. "The Association between Perceived Housing Environment and Health and Satisfaction among the Older Adults during the COVID-19 Pandemic: A Cross-Sectional Survey in Northern China" Buildings 13, no. 11: 2875. https://doi.org/10.3390/buildings13112875
APA StyleLiu, F., Li, Y., Gao, X., & Du, J. (2023). The Association between Perceived Housing Environment and Health and Satisfaction among the Older Adults during the COVID-19 Pandemic: A Cross-Sectional Survey in Northern China. Buildings, 13(11), 2875. https://doi.org/10.3390/buildings13112875






