What Are the Chances of Resilon to Dominate the Market Filling Materials for Endodontics?
Abstract
:1. Introduction and Main Goals of the Paper
2. Possibilities of Application in Endodontics of the Methods of Contextual Matrices’ Analysis to Optimize the Selection of Engineering Materials and the Conditions of Their Application
3. Approach for the Strategic Development Analysis of the Filling Materials
4. The Global Threat of Oral Disease and the General Concept of Sustainable Dentistry Development
5. Goals, Expectations and Tooth Qualification for Root Canals Preparation
6. The Importance of the Endodontic Tools and Lubricants Selection
7. The Modern Obturation Techniques in Endodontics
8. The Filling Materials Selection and Monoblock Idea Reality
9. The Scope and Methodology of Experimental Work
- connection of the filling material with the dentine of the root canal,
- connection of the main stud with complementary material,
- filling of the lateral tubules,
- filling the root delta,
- connection of the material with dentin tubules,
- volume fraction of the sealant,
- leakage on the border of the root canal wall and the filling material.
10. Materialographic Test Results of Teeth Filled with Resilon by Cold Lateral Condensation
11. Strengths, Weaknesses, Opportunities, and Threats SWOT Analysis of the Resilon Application in Endodontics
12. Summary
13. Conclusions
- Treating the worldwide epidemic effects of oral cavity diseases, especially tooth de-cay, requires radical actions following the third UN Sustainable Development Goal.
- The general goal of endodontics, as a part of interventional dentistry within Sus-tainable Dentistry Development, is to save teeth affected by advanced caries and pre-serve the functional features of the stomatognathic system in this way, or at least to be natural pillars of prosthetic restorations, despite the loss of the natural biological properties of these teeth.
- The effectiveness of endodontic treatment and its long-term positive impact to save human health are determined by numerous factors regarding the selection of the site and method of endodontic intervention, the method of preparation and obturation of the root canal together with the selection of appropriate devices, as well as the correct and adequate selection of filling materials.
- Resilon is one of the possible filling materials popularized in endodontic treatment, characterized by the advantage of strengths over weaknesses, but with a simultaneous advantage of threats over opportunities, which indicates the possibility of using the MAXI-MINI development strategy for this material, which in the case of unfavourable development events may fail in further development of this material, although if appropriate paths are found, it may also bring the success that has not yet been achieved.
- The fact that it is not possible to apply the aggressive development strategy of MAXI-MAXI to resilon indicates that this filling material cannot be considered dominant in terms of clinical suitability among endodontic materials.
Author Contributions
Funding
Conflicts of Interest
Notice
References
- Hermann, M.; Pentek, T.; Otto, B. Design Principles for Industrie 4.0 Scenarios: A Literature Review; Technische Universität Dortmund: Dortmund, Germany, 2015. [Google Scholar]
- Kagermann, H.; Wahlster, W.; Helbig, J. Recommendations for Implementing the Strategic Initiative INDUSTRIE 4.0: Final Report of the Industrie 4.0 Working Group; Federal Ministry of Education and Research: Bonn, Germany, 2013.
- Rüßmann, M.; Lorenz, M.; Gerbert, P.; Waldner, M.; Justus, J.; Engel, P.; Harnisch, M. Industry 4.0: The Future of Productivity and Growth in Manufacturing Industries; Boston Consulting Group: Boston, MA, USA, 2015. [Google Scholar]
- Kagermann, H. Chancen von Industrie 4.0 Nutzen. In Industrie 4.0 in Produktion, Automatisierung und Logistik; Springer: Wiesbaden, Germany, 2014; pp. 603–614. [Google Scholar]
- Dobrzański, L.A.; Dobrzański, L.B.; Dobrzańska-Danikiewicz, A.D. Overview of conventional technologies using the powders of metals, their alloys and ceramics in Industry 4.0 stage. JAMME 2020, 98, 56–85. [Google Scholar] [CrossRef]
- Dobrzański, L.A. Role of materials design in maintenance engineering in the context of industry 4.0 idea. JAMME 2019, 96, 12–49. [Google Scholar] [CrossRef]
- Dobrzański, L.A.; Dobrzańska-Danikiewicz, A.D. Applications of Laser Processing of Materials in Surface Engineering in the Industry 4.0 Stage of the Industrial Revolution. Mater. Perform. Charact. 2019, 8, 1091–1129. [Google Scholar] [CrossRef]
- Dobrzański, L.A.; Dobrzańska-Danikiewicz, A.D. Why Are Carbon-Based Materials Important in Civilization Progress and Especially in the Industry 4.0 Stage of the Industrial Revolution. Mater. Perform. Charact. 2019, 8, 337–370. [Google Scholar] [CrossRef]
- Dobrzański, L.A.; Dobrzański, L.B.; Dobrzańska-Danikiewicz, A.D.; Kraszewska, M. Manufacturing powders of metals, their alloys and ceramics and the importance of conventional and additive technologies for products manufacturing in Industry 4.0 stage. AMSE 2020, 102, 13–41. [Google Scholar] [CrossRef]
- Lee, J.; Kao, H.-A.; Yang, S. Service Innovation and Smart Analytics for Industry 4.0 and Big Data Environment. Proc. CIRP 2014, 16, 3–8. [Google Scholar] [CrossRef] [Green Version]
- Jose, R.; Ramakrishna, S. Materials 4.0: Materials Big Data Enabled Materials Discovery. Appl. Mater. Today 2018, 10, 127–132. [Google Scholar] [CrossRef]
- Buer, S.-V.; Strandhagen, J.O.; Chan, F.T.S. The Link between Industry 4.0 and Lean Manufacturing: Mapping Current Research and Establishing a Research Agenda. Int. J. Product. Res. 2018, 56, 2924–2940. [Google Scholar] [CrossRef] [Green Version]
- Brettel, M.; Friederichsen, N.; Keller, M.; Rosenberg, M. How Virtualization, Decentralization, and Network-Building Change the Manufacturing Landscape: An Industry 4.0 Perspective. Int. J. Mech. Aerospac. Ind. Mechatron. Manuf. Eng. 2014, 8, 37–44. [Google Scholar]
- Tay, S.I.; Lee, T.C.; Hamid, N.A.A.; Ahmad, A.N.A. An Overview of Industry 4.0: Definition, Components, and Government Initiatives. J. Adv. Res. Dyn. Control. Syst. 2018, 10, 1379–1387. [Google Scholar]
- Xu, X. Machine Tool 4.0 for the New Era of Manufacturing. Int. J. Adv. Manuf. Techn. 2017, 92, 1893–1900. [Google Scholar] [CrossRef]
- Sipsas, K.; Alexopoulos, K.; Xanthakis, V.; Chryssolouris, G. Collaborative Maintenance in Flow-Line Manufacturing Environments: An Industry 4.0 Approach. Proc. CIRP 2016, 55, 236–241. [Google Scholar] [CrossRef] [Green Version]
- Posada, J.; Toro, C.; Barandiaran, I.; Oyarzun, D.; Stricker, D.; de Amicis, R.; Pinto, E.B.; Eisert, P.; Döllner, J.; Vallarino, I. Visual Computing as a Key Enabling Technology for Industrie 4.0 and Industrial Internet. IEEE Comp. Graph Appl. 2015, 35, 26–40. [Google Scholar] [CrossRef]
- Hozdic, E. Smart Factory for Industry 4.0: A Review. Int. J. Modern Manuf. Tech. 2015, 7, 28–35. [Google Scholar]
- Zhong, R.Y.; Xu, X.; Klotz, E.; Newman, S.T. Intelligent Manufacturing in the Context of Industry 4.0: A Review. Engineering 2017, 3, 616–630. [Google Scholar] [CrossRef]
- Łobaziewicz, M. Zarządzanie Inteligentnym Przedsiębiorstwem W Dobie Przemysłu 4.0; Towarzystwo Naukowe Organizacji i Kierownictwa: Toruń, Poland, 2019. [Google Scholar]
- Bahrin, M.A.K.; Othman, M.F.; Azli, N.H.N.; Talib, M.F. Industry 4.0: A Review on Industrial Automation and Robotic. J. Teknol. 2016, 78, 137–143. [Google Scholar] [CrossRef] [Green Version]
- Vaidya, S.; Ambad, P.; Bhosle, S. Industry 4.0–A Glimpse. Proc. Manuf. 2018, 20, 233–238. [Google Scholar] [CrossRef]
- Lee, J.; Bagheri, B.; Kao, H.-A. A Cyber-Physical Systems Architecture for Industry 4.0-Based Manufacturing Systems. Manuf. Lett. 2015, 3, 18–23. [Google Scholar] [CrossRef]
- Stock, T.; Seliger, G. Opportunities of Sustainable Manufacturing in Industry 4.0. Proc. CIRP 2016, 40, 536–541. [Google Scholar] [CrossRef] [Green Version]
- Schumacher, A.; Erol, S.; Sihn, W. A Maturity Model for Assessing Industry 4.0 Readiness and Maturity of Manufacturing Enterprises. Proc. CIRP 2016, 52, 161–166. [Google Scholar] [CrossRef]
- Kumar, K.; Zindani, D.; Davim, J.P. Industry 4.0: Developments towards the Fourth Industrial Revolution; Springer Nature: Singapore, 2019. [Google Scholar]
- Pfeiffer, S. Robots, Industry 4.0 and Humans, or Why Assembly Work Is More than Routine Work. Societies 2016, 6, 16. [Google Scholar] [CrossRef]
- Wang, S.; Wan, J.; Zhang, D.; Li, D.; Zhang, C. Towards Smart Factory for Industry 4.0: A Self-Organized Multi-Agent System with Big Data Based Feedback and Coordination. Comp. Netw. 2016, 101, 158–168. [Google Scholar] [CrossRef] [Green Version]
- Ardito, L.; Petruzzelli, A.M.; Panniello, U.; Garavelli, A.C. Towards Industry 4.0: Mapping Digital Technologies for Supply Chain Management-Marketing Integration. Bus. Proc. Manag. J. 2019, 25, 323–346. [Google Scholar] [CrossRef]
- Mosterman, P.J.; Zander, J. Industry 4.0 as a Cyber-Physical System Study. Softw. Syst. Model. 2016, 15, 17–29. [Google Scholar] [CrossRef]
- Almada-Lobo, F. The Industry 4.0 Revolution and the Future of Manufacturing Execution Systems (MES). J. Innov. Manag. 2015, 3, 16–21. [Google Scholar] [CrossRef]
- Lu, Y. Industry 4.0: A Survey on Technologies, Applications and Open Research Issues. J. Ind. Infor. Integrat. 2017, 6, 1–10. [Google Scholar] [CrossRef]
- Qin, J.; Liu, Y.; Grosvenor, R. A Categorical Framework of Manufacturing for Industry 4.0 and Beyond. Proc. CIRP 2016, 52, 173–178. [Google Scholar] [CrossRef] [Green Version]
- Dobrzański, L.A.; Dobrzański, L.B. Approach to the Design and Manufacturing of Prosthetic Dental Restorations According to the Rules of Industry 4.0. Mater. Perform. Charact. 2020, 9, 394–476. [Google Scholar] [CrossRef]
- Dobrzański, L.A.; Dobrzański, L.B. Dentistry 4.0 Concept in the Design and Manufacturing of Prosthetic Dental Restorations. Processes 2020, 8, 525. [Google Scholar] [CrossRef]
- Dobrzański, L.A.; Dobrzański, L.B.; Achtelik-Franczak, A.; Dobrzańska, J. Application Solid Laser-Sintered or Machined Ti6Al4V Alloy in Manufacturing of Dental Implants and Dental Prosthetic Restorations According to Dentistry 4.0 Concept. Processes 2020, 8, 664. [Google Scholar] [CrossRef]
- Dobrzański, L.A.; Dobrzański, L.B.; Dobrzańska-Danikiewicz, A.D.; Dobrzańska, J. The Concept of Sustainable Development of Modern Dentistry. Processes 2020, 8, 1605. [Google Scholar] [CrossRef]
- Dobrzański, L.A.; Dobrzańska-Danikiewicz, A.D.; Dobrzański, L.B. Effect of Biomedical Materials in the Implementation of a Long and Healthy Life Policy. Processes 2021, 9, 865. [Google Scholar] [CrossRef]
- Japan Business Federation. Toward Realization of the New Economy and Society (Outline). Keidanren. 2016. Available online: https://www.keidanren.or.jp/en/policy/2016/029_outline.pdf (accessed on 15 May 2021).
- Fukuyama, M. Society 5.0: Aiming for a New Human-Centered Society. Jpn. Spotlight 2018, July/August 47–50. Available online: https://www.jef.or.jp/journal/pdf/220th_Special_Article_02.pdf (accessed on 15 May 2021).
- Harayama, Y. Society 5.0: Aiming for a New Human-Centered Society. Hitachi Rev. 2017, 66, 8–13. Available online: https://www.hitachi.com/rev/archive/2017/r2017_06/pdf/p08-13_TRENDS.pdf (accessed on 15 May 2021).
- Japan Business Federation. Society 5.0: Co-Creating the Future (Excerpt). Keidanren. 2018. Available online: https://www.keidanren.or.jp/en/policy/2018/095_outline.pdf (accessed on 15 May 2021).
- Government of Japan Cabinet Office. “Society 5.0”, Cabinet Office. 2019. Available online: https://www8.cao.go.jp/cstp/english/society5_0/index.html (accessed on 15 May 2021).
- Japan Business Federation. “Japan’s Initiatives–Society 5.0”, Keidanren. Available online: http://www.keidanren.or.jp/en/policy/2017/010_overview.pdf (accessed on 15 May 2021).
- Dobrzańska, J. Analiza Szczelności Wypełnień Kanałów Korzeniowych. Ph.D. Thesis, Śląski Uniwersytet Medyczny w Katowicach, Zabrze, Poland, 2011. [Google Scholar]
- Dobrzański, L.A.; Dobrzański, L.B.; Dobrzańska-Danikiewicz, A.D. Manufacturing technologies thick-layer coatings on various substrates and manufacturing gradient materials using powders of metals, their alloys and ceramics. JAMME 2020, 99, 14–41. [Google Scholar] [CrossRef]
- Dobrzańska-Danikiewicz, A.D.; Dobrzański, L.A.; Szindler, M.; Achtelik-Franczak, A.; Dobrzański, L.B. Obróbka powierzchni materiałów mikroporowatych wytworzonych metodą selektywnego spiekania laserowego w celu uefektywnienia proliferacji żywych komórek. In Metalowe Materiały Mikroporowate I Lite Do Zastosowań Medycznych I Stomatologicznych; Open Access Library VII(1), Dobrzański, L.A., Dobrzańska-Danikiewicz, A.D., Eds.; International OCSCO World Press: Gliwice, Poland, 2017; pp. 289–375. [Google Scholar]
- Dobrzańska-Danikiewicz, A. The methodological fundaments of development state analysis of surface engineering technologies. JAMME 2010, 40, 203–210. [Google Scholar]
- Dobrzańska-Danikiewicz, A.D.; Hajduczek, E.; Polok-Rubiniec, M.; Przybył, M.; Adamaszek, K. Evaluation of selected steel thermochemical treatment technologies using foresight methods. JAMME 2011, 46, 115–146. [Google Scholar]
- Dobrzańska-Danikiewicz, A.D. The development perspectives of Physical Vapour Deposition technologies. JAMME 2012, 54, 103–109. [Google Scholar]
- Dobrzańska-Danikiewicz, A.D. Metodologia Komputerowo Zintegrowanego Prognozowania Rozwoju Inżynierii Powierzchni Materiałów; Open Access Library 1(7), Dobrzański, L.A., Eds.; International OCSCO World Press: Gliwice, Poland, 2012; pp. 1–289. [Google Scholar]
- Dobrzańska-Danikiewicz, A.D. Księga Technologii Krytycznych Kształtowania Struktury i Własności Powierzchni Materiałów Inżynierskich; Open Access Library 8(26), Dobrzański, L.A., Eds.; International OCSCO World Press: Gliwice, Poland, 2013; pp. 1–823. [Google Scholar]
- Dobrzańska-Danikiewicz, A.D. (Ed.) Materials Surface Engineering Development Trends; Open Access Library 6; International OCSCO World Press: Gliwice, Poland, 2011; pp. 1–594. [Google Scholar]
- Dobrzańska-Danikiewicz, A.D.; Dobrzański, L.A.; Sękala, A. Results of Technology Foresight in the Surface Engineering Area. AMM 2014, 657, 916–920. [Google Scholar] [CrossRef]
- Dobrzańska-Danikiewicz, A.D.; Dobrzański, L.A.; Mazurkiewicz, J.; Tomiczek, B.; Reimann, Ł. E-transfer of materials surface engineering e-foresight results. AMSE 2011, 52, 87–100. [Google Scholar]
- Dobrzańska-Danikiewicz, A.D.; Tański, T.; Malara, S.; Domagała-Dubiel, J. Technology Foresight Results Concerning Laser Surface Treatment of Casting Magnesium Alloys. In New Features on Magnesium Alloys; Monteiro, W.A., Ed.; IntechOpen: Rijeka, Croatia, 2012; pp. 1–30. [Google Scholar] [CrossRef] [Green Version]
- Dobrzańska-Danikiewicz, A.D. Foresight of Material Surface Engineering as a Tool Building a Knowledge-Based Economy. MSF 2012, 706–709, 2511–2516. [Google Scholar] [CrossRef]
- Dobrzański, L.A. (Ed.) 1st Workshop on Foresight of Surface Properties Formation Leading Technologies of Engineering Materials and Biomaterials; International OCSCO World Press: Gliwice, Poland, 2009; pp. 1–272. [Google Scholar]
- Dobrzański, L.A. (Ed.) 2nd Workshop on Foresight of Surface Properties Formation Leading Technologies of Engineering Materials and Biomaterials; International OCSCO World Press: Gliwice, Poland, 2009; pp. 1–324. [Google Scholar]
- Dobrzański, L.A.; Dobrzańska-Danikiewicz, A.D. (Eds.) 3rd Workshop on Foresight of Surface Properties Formation Leading Technologies of Engineering Materials and Biomaterials; Raport z realizacji zadania 2. "Analiza Istniejącej Sytuacji w Zakresie Rozwoju Technologii Oraz Uwarunkowań Społeczno-Gospodarczych w Odniesieniu Do Przedmioty Foresightu pt. FORSURF-Foresight Wiodących Technologii Kształtowania Własności Powierzchni Materiałów Inżynierskich i Biomedycznych"; International OCSCO World Press: Gliwice, Poland, 2010; pp. 1–184. [Google Scholar]
- Dobrzański, L.A.; Achtelik-Franczak, A. Struktura i własności tytanowych szkieletowych materiałów mikroporowatych wytworzonych metodą selektywnego spiekania laserowego do zastosowań w implantologii oraz medycynie regeneracyjnej. In Metalowe Materiały Mikroporowate i Lite Do Zastosowań Medycznych i Stomatologicznych; Open Access Library VII(1); Dobrzański, L.A., Dobrzańska-Danikiewicz, A.D., Eds.; International OCSCO World Press: Gliwice, Poland, 2017; pp. 186–244. [Google Scholar]
- Dobrzański, L.A. Effect of heat and surface treatment on the structure and properties of the Mg-Al-Zn-Mn casting alloys. In Magnesium and Its Alloys; Dobrzański, L.A., Totten, G.E., Bamberger, M., Eds.; CRC Press: Boca Raton, FL, USA, 2019; pp. 91–202. [Google Scholar]
- Dobrzański, L.A.; Dobrzańska-Danikiewicz, A.D. Perspektywy i trendy rozwojowe inżynierii powierzchni materiałów. In Inżynieria Powierzchni Materiałów: Kompendium Wiedzy i Podręcznik Akademicki; Open Access Library VIII(1), Dobrzański, L.A., Eds.; International OCSCO World Press: Gliwice, Poland, 2018; pp. 89–157. [Google Scholar]
- Dobrzański, L.A.; Nieradka-Buczek, B. Transparent conductive nanocomposite layers with polymer matrix and silver nanowires reinforcement. AMSE 2018, 93, 59–84. [Google Scholar] [CrossRef]
- Dobrzański, L.A.; Dobrzańska-Danikiewicz, A.D.; Czuba, Z.P.; Dobrzański, L.B.; Achtelik-Franczak, A.; Malara, P.; Szindler, M.; Kroll, L. Metallic skeletons as reinforcement of new composite materials applied in orthopaedics and dentistry. AMSE 2018, 92, 53–85. [Google Scholar] [CrossRef]
- Dobrzański, L.A.; Dobrzański, L.B.; Dobrzańska-Danikiewicz, A.D.; Dobrzańska, J.; Rudziarczyk, K.; Achtelik-Franczak, A. Non-Antagonistic Contradictoriness of the Progress of Advanced Digitized Production with SARS-CoV-2 Virus Transmission in the Area of Dental Engineering. Processes 2020, 8, 1097. [Google Scholar] [CrossRef]
- Dobrzański, L.A.; Dobrzańska-Danikiewicz, A.; Achtelik-Franczak, A. The structure and properties of aluminium alloys matrix composite materials with reinforcement made of titanium skeletons. AMSE 2016, 80, 16–30. [Google Scholar] [CrossRef] [Green Version]
- Dobrzański, L.A.; Prokopiuk vel Prokopowicz, M. The influence of reduced graphene oxide on the structure of the electrodes and the properties of dye-sensitized solar cells. AMSE 2016, 77, 12–30. [Google Scholar] [CrossRef]
- Dobrzański, L.A.; Hudecki, A.; Chladek, G.; Król, W.; Mertas, A. Biodegradable and antimicrobial polycaprolactone nanofibers with and without silver precipitates. AMSE 2015, 76, 5–26. [Google Scholar]
- Dobrzański, L.A.; Hudecki, A. Structure, geometrical characteristics and properties of biodegradable micro- and polycaprolactone nanofibers. AMSE 2014, 70, 5–13. [Google Scholar]
- Dobrzański, L.A.; Pawlyta, M.; Hudecki, A. Conceptual study on a new generation of the high-innovative advanced porous and composite nanostructural functional materials with nanofibers. JAMME 2011, 49, 550–565. [Google Scholar]
- Dobrzańska-Danikiewicz, A.D.; Żmudzki, J. Development trends of mucous-borne dentures in the aspect of elastomers applications. AMSE 2012, 55, 5–13. [Google Scholar]
- Dobrzański, L.B. Struktura i Własności Materiałów Inżynierskich Na Uzupełnienia Protetyczne Układu Stomatognatycznego Wytwarzane Metodami Przyrostowymi i Ubytkowymi. Ph.D. Thesis, Akademia Górniczo-Hutnicza im. Stanisława Staszica w Krakowie, Kraków, Poland, 2017. [Google Scholar]
- Rudziarczyk, K. Modelowanie Stanu Naprężeń w Wybranych Rodzajach Implantów Stomatologicznych Oraz w Otaczającej Je Tkance Kostnej. Master’s Thesis, Politechnika Śląska, Gliwice, Poland, 2020. [Google Scholar]
- Berliński, M. Modelowanie Zależności Między Warunkami Wytapiania w Wielkim Piecu i Składem Chemicznym Surówki z Wykorzystaniem Sieci Neuronowych. Ph.D. Thesis, Politechnika Śląska, Gliwice, Poland, 2018. [Google Scholar]
- Nieradka-Buczek, B. Zastosowanie Nanodrutów Srebra Jako Wzmocnienia Transparentnych Warstw Nanokompozytowych. Ph.D. Thesis, Politechnika Śląska, Gliwice, Poland, 2018. [Google Scholar]
- Kędzierski, K. Charakterystyka Ekologicznych Ośrodków Polimerowych Do Chłodzenia Nawęglonych Stali Niskowęglowych. Ph.D. Thesis, Politechnika Śląska, Gliwice, Poland, 2017. [Google Scholar]
- Szindler, M. Polimerowe Warstwy Półprzewodnikowe Zol-Żel Do Zastosowań Fotowoltaicznych. Ph.D. Thesis, Politechnika Śląska, Gliwice, Poland, 2017. [Google Scholar]
- Achtelik-Franczak, A. Inżynierskie Materiały Kompozytowe o Wzmocnieniu z Mikroporowatego Tytanu Selektywnie Spiekanego Laserowo. Ph.D. Thesis, Politechnika Śląska, Gliwice, Poland, 2016. [Google Scholar]
- Macek, M. Struktura i Własności Aluminiowych Materiałów Nanokompozytowych Wzmacnianych Nanorurkami Węglowymi. Ph.D. Thesis, Politechnika Śląska, Gliwice, Poland, 2016. [Google Scholar]
- Prokopiuk vel Prokopowicz, M. Wpływ Zredukowanego Tlenku Grafenu Na Strukturę Elektrod i Własności Barwnikowych Ogniw Fotowoltaicznych. Ph.D. Thesis, Politechnika Śląska, Gliwice, Poland, 2016. [Google Scholar]
- Czaja, I. Wpływ Nanodrutów i Nanoproszków Miedzi Na Strukturę i Własności Nanokompozytowych Materiałów Polimerowych. Ph.D. Thesis, Politechnika Śląska, Gliwice, Poland, 2015. [Google Scholar]
- Hudecki, A. Nanowłókna Kompozytowe o Bioaktywnym Rdzeniu i Antybakteryjnej Powłoce Na Rusztowania Tkankowe. Ph.D. Thesis, Politechnika Śląska, Gliwice, Poland, 2015. [Google Scholar]
- Mucha, A. Wpływ Nanorurek Węglowych Na Własności Barwnikowych Ogniw Fotowoltaicznych. Ph.D. Thesis, Politechnika Śląska, Gliwice, Poland, 2015. [Google Scholar]
- Górniak, M. Wpływ Organofilizacji Powierzchni Nanorurek Haloizytowych i Nanopłytek Montmorylonitowych Na Własności Kompozytów Polimerowych. Ph.D. Thesis, Politechnika Śląska, Gliwice, Poland, 2014. [Google Scholar]
- Szindler, M. Struktura i Własności Nanostrukturalnych Warstw Antyrefleksyjnych Otrzymanych Metodą ALD Oraz Zol-Żel Na Krzemowych Ogniwach Fotowoltaicznych. Ph.D. Thesis, Politechnika Śląska, Gliwice, Poland, 2014. [Google Scholar]
- Reimann, Ł. System Komputerowego Wspomagania Doboru Materiałów Na Wieloczłonowe Częściowe Stałe Protezy Stomatologiczne. Ph.D. Thesis, Politechnika Śląska, Gliwice, Poland, 2013. [Google Scholar]
- Dobrzańska, J.; Dobrzański, L.B.; Dobrzański, L.A.; Gołombek, K.; Dobrzańska-Danikiewicz, A.D. Is Gutta-Percha Still the “Gold Standard” among Filling Materials in Endodontic Treatment? Processes 2021, 9, 1467. [Google Scholar] [CrossRef]
- Dobrzańska, J.; Dobrzański, L.B.; Gołombek, K.; Dobrzański, L.A.; Dobrzańska-Danikiewicz, A.D. Virtual Approach to the Comparative Analysis of Biomaterials Used in Endodontic Treatment. Processes 2021, 9, 926. [Google Scholar] [CrossRef]
- Henderson, B. The Product Portfolio. Available online: https://www.bcg.com/publications/1970/strategy-the-product-portfolio (accessed on 8 April 2021).
- ICDAS Website. Available online: https://www.icdas.org/ (accessed on 6 April 2021).
- Featherstone, J.D. The continuum of dental caries—evidence for a dynamic disease process. J. Dent. Res. 2004, 83, C39–C42. [Google Scholar] [CrossRef]
- Ismail, A.I.; Sohn, W.; Tellez, M.; Amaya, A.; Sen, A.; Hasson, H.; Pitts, N.B. The International Caries Detection and Assessment System (ICDAS): An integrated system for measuring dental caries. Community Dent. Oral Epidemiol. 2007, 35, 170–178. [Google Scholar] [CrossRef] [Green Version]
- Ismail, A.; Tellez, M.; Pitts, N.B.; Ekstrand, K.R.; Ricketts, D.; Longbottom, C.; Eggertsson, H.; Deery, C.; Fisher, J.; Young, D.A.; et al. Caries management pathways preserve dental tissues and promote oral health. Community Dent. Oral Epidemiol. 2013, 41, e12–e40. [Google Scholar] [CrossRef] [Green Version]
- Pitts, N.B.; Ekstrand, K.R. International Caries Detection and Assessment System (ICDAS) and its International Caries Classification and Management System (ICCMS)—Methods for staging of the caries process and enabling dentists to manage caries. Community Dent. Oral Epidemiol. 2013, 41, e41–e52. [Google Scholar] [CrossRef]
- Ormond, C.; Douglas, G.; Pitts, N. The use of the International Caries Detection and Assessment System (ICDAS) in a National Health Service general dental practice as part of an oral health assessment. Prim. Dent. Care 2010, 17, 153–159. [Google Scholar] [CrossRef]
- Ismail, A.; Pitts, N.B.; Tellez, M. The international caries classification and management system (ICCMSTM) an example of a caries management pathway. BMC Oral Health 2015, 15, S9. [Google Scholar] [CrossRef] [Green Version]
- Marthaler, T.M. A standardized system of recording dental conditions. Helv. Odontol. Acta 1966, 10, 1–18. [Google Scholar]
- Dirks, O.B.; van Amerongen, J.; Winkler, K.C. A reproducible method for caries evaluation. J. Dent. Res. 1951, 30, 346–359. [Google Scholar] [CrossRef]
- Clarkson, B.H.; Exterkate, R.A.M. Noninvasive dentistry: A dream or reality? Caries Res. 2015, 49, 11–17. [Google Scholar] [CrossRef]
- Pitts, N.B.; Zero, D.T.; White paper on dental caries prevention and management. FDI World Dental Federation. Available online: http://www.fdiworlddental.org/sites/default/files/media/documents/2016-fdi_cpp-white_paper.pdf (accessed on 6 April 2021).
- Wierichs, R.J.; Meyer-Lueckel, H. Systematic review on noninvasive treatment of root caries lesions. J. Dent. Res. 2015, 94, 261–271. [Google Scholar] [CrossRef] [PubMed]
- Marsh, P.D.; Head, D.A.; Devine, D.A. Prospects of oral disease control in the future—an opinion. J. Oral Microbiol. 2014, 6, 261–276. [Google Scholar] [CrossRef] [PubMed]
- The 17 Goals. Available online: https://sdgs.un.org/goals (accessed on 1 March 2021).
- GBD Compare. Viz Hub. Available online: https://vizhub.healthdata.org/gbd-compare/ (accessed on 6 April 2021).
- Fejerskov, O. Concepts of dental caries and their consequences for understanding the disease. Community Dent. Oral Epidemiol. 1997, 25, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Reisine, S.; Litt, M. Social and psychological theories and their use for dental practice. Int. Dent. J. 1993, 43, 279–287. [Google Scholar]
- Selwitz, R.H.; Ismail, A.I.; Pitts, N.B. Dental caries. Lancet 2007, 369, 51–59. [Google Scholar] [CrossRef]
- Li, X.; Tornstad, L.; Olsen, I. Brain abscesses caused by oral infection. Dent. Traumatol. 1999, 15, 95–101. [Google Scholar] [CrossRef]
- Scannapieco, F.A.; Bush, R.B.; Paju, S. Associations between periodontal disease and risk for nosocomial bacterial pneumonia and chronic obstructive pulmonary disease. A systemic review. Ann. Periodontol. 2003, 8, 54–69. [Google Scholar] [CrossRef] [Green Version]
- Aleksander, M.; Krishnan, B.; Shenoy, N. Diabetes mellitus and odontogenic infections-an exaggerated risk? Oral Maxillofac. Surg. 2008, 12, 129–130. [Google Scholar] [CrossRef]
- Scannapieco, F.A. Role of oral bacteria in respiratory infection. J. Periodontol. 1999, 70, 793–802. [Google Scholar] [CrossRef]
- Mueller, A.A.; Saldami, B.; Stübinger, S.; Walter, C.; Flückiger, U.; Merlo, A.; Schwenzer-Zimmerer, K.; Zeilhofer, H.F.; Zimmerer, S. Oral bacterial cultures in nontraumatic brain abscesses: Results of a first line study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 107, 469–476. [Google Scholar] [CrossRef]
- Buset, S.L.; Walter, C.; Friedmann, A.; Weiger, R.; Borgnakke, W.S.; Zitzmann, N.U. Are periodontal diseases really silent? A systematic review of their effect on quality of life. J. Clin. Periodontol. 2016, 43, 333–344. [Google Scholar] [CrossRef]
- Sierpinska, T.; Golebiewska, M.; Dlugosz, J.W.; Kemona, A.; Laszewicz, W. Connection between masticatory efficiency and pathomorphologic changes in gastric mucosa. Quintessence Int. 2007, 38, 31–37. [Google Scholar]
- Al-Nawas, B.; Maeurer, M. Severe versus local odontogenic bacterial infections: Comparison of microbial isolates. Eur. Surg. Res. 2008, 40, 220–224. [Google Scholar] [CrossRef]
- Pallasch, T.J.; Wahl, M.J. Focal infection: New age or ancient history? Endodon. Top. 2003, 4, 32–45. [Google Scholar] [CrossRef] [Green Version]
- De Pablo, P.; Dietrich, T.; McAlindon, T.E. Association of periodontal disease and tooth loss with rheumatoid arthritis in the US population. J. Rheumatol. 2008, 35, 70–76. [Google Scholar]
- Felton, D.A. Edentualism and comorbid factors. J. Prosthodont. 2009, 18, 88–96. [Google Scholar] [CrossRef]
- Volzke, H.; Schwahn, C.; Hummel, A.; Wolff, B.; Kleine, V.; Robinson, D.M.; Dahm, J.B.; Felix, S.B.; John, U.; Kocher, T. Tooth loss is independently associated with the risk of acquired aortic valve sclerosis. Am. Heart J. 2005, 150, 1198–1203. [Google Scholar] [CrossRef]
- Bagchi, S.; Tripathi, A.; Tripathi, S.; Kar, S.; Tiwari, S.C.; Singh, J. Obstructive sleep apnea and neurocognitive dysfunction in edentulous patients. J. Prosthodont. 2019, 28, e837–e842. [Google Scholar] [CrossRef]
- Nagpal, R.; Yamashiro, Y.; Izumi, Y. The two-way association of periodontal infection with systemic disorders: An overview. Mediat. Inflamm. 2015, 2015, 793898. [Google Scholar] [CrossRef] [Green Version]
- Abnet, C.C.; Qiao, Y.L.; Dawsey, S.M.; Dong, Z.W.; Taylor, P.R.; Mark, S.D. Tooth loss is associated with increased risk of total death and death from upper gastrointestinal cancer, heart disease, and stroke in a Chinese population-based cohort. Int. J. Epidemiol. 2005, 34, 467–474. [Google Scholar] [CrossRef]
- Burzyńska, B.; Mierzwińska-Nastalska, E. Rehabilitacja protetyczna pacjentów bezzębnych. Nowa Stomatol. 2011, 4, 167–199. [Google Scholar]
- Bui, F.Q.; Almeida-da-Silva, C.L.C.; Huynh, B.; Trinh, A.; Liu, J.; Woodward, J.; Asadi, H.; Ojcius, D.M. Association between periodontal pathogens and systemic disease. Biomed. J. 2019, 42, 27–35. [Google Scholar] [CrossRef]
- Holmlund, A.; Holm, G.; Lind, L. Number of teeth as a predictor of cardiovascular mortality in a cohort of 7674 subjects followed for 12 years. J. Periodontol. 2010, 81, 870–876. [Google Scholar] [CrossRef]
- Takata, Y.; Ansai, T.; Matsumura, K.; Awano, S.; Hamasaki, T.; Sonoki, K.; Kusaba, A.; Akifusa, S.; Takehara, T. Relationship between tooth loss and electrocardiographic abnormalities in octogenarians. J. Dent. Res. 2001, 80, 1648–1652. [Google Scholar] [CrossRef]
- Felton, D.A. Complete edentulism and comorbid diseases: An update. J. Prosthodont. 2016, 25, 5–20. [Google Scholar] [CrossRef]
- Chen, H.; Iinuma, M.; Onozuka, M.; Kubo, K.-Y. Chewing maintains hippocampus-dependent cognitive. Int. J. Med. Sci. 2015, 12, 502–509. [Google Scholar] [CrossRef] [Green Version]
- Stein, P.S.; Desrosiers, M.; Donegan, S.J.; Yepes, J.F.; Kryscio, R.J. Tooth loss, dementia and neuropathology in the Nun study. J. Am. Dent. Assoc. 2007, 138, 1314–1322. [Google Scholar] [CrossRef]
- Henke, K. A model for memory systems based on processing modes rather than consciousness. Nat. Rev. Neurosci. 2010, 11, 523–532. [Google Scholar] [CrossRef]
- Lexomboon, D.; Trulsson, M.; Wårdh, I.; Parker, W.G. Chewing ability and tooth loss: Association with cognitive impairment in an elderly population study. J. Am. Geriatr. Soc. 2012, 60, 1951–1956. [Google Scholar] [CrossRef]
- Hirano, Y.; Obata, T.; Takahashi, H.; Tachibana, A.; Kuroiwa, D.; Takahashi, T.; Ikehira, H.; Onozuka, M. Effects of chewing on cognitive processing speed. Brain Cognit. 2013, 81, 376–381. [Google Scholar] [CrossRef] [PubMed]
- Watt, R.G.; Daly, B.; Allison, P.; Macpherson, L.M.D.; Venturelli, R.; Listl, S.; Weyant, R.J.; Mathur, M.R.; Guarnizo-Herreño, C.C.; Celeste, R.K.; et al. Ending the neglect of global oral health: Time for radical action. Lancet 2019, 394, 261–272. [Google Scholar] [CrossRef]
- Peres, M.A.; Macpherson, L.M.D.; Weyant, R.J.; Daly, B.; Venturelli, R.; Mathur, M.R.; Listl, S.; Celeste, R.K.; Guarnizo-Herreño, C.C.; Kearns, C.; et al. Oral diseases: A global public health challenge. Lancet 2019, 394, 249–260. [Google Scholar] [CrossRef]
- Alwadani, M.; Mashyakhy, M.H.; Jali, A.; Hakami, A.O.; Areshi, A.; Daghriri, A.A.; Shaabi, F.I.; Al Moaleem, M.M. Dentists and Dental Intern’s Preferences of Root Canal Treatment with Restoration Versus Extraction then Implant-Supported Crown Treatment Plan. Open Dent. J. 2019, 13, 93–100. [Google Scholar] [CrossRef]
- Estrela, C.; Holland, R.; Estrela, C.R.; Alencar, A.H.; Sousa-Neto, M.D.; Pécora, J.D. Characterization of successful root canal treatment. Braz. Dent. J. 2014, 25, 3–11. [Google Scholar] [CrossRef]
- De Oliveira, B.P.; Câmara, A.C.; Aguiar, C.M. Prevalence of endodontic diseases: An epidemiological evaluation in a Brazilian subpopulation. Braz. J. Oral Sci. 2016, 15, 119–123. [Google Scholar] [CrossRef] [Green Version]
- Peroz, I.; Blankenstein, F.; Lange, K.-P.; Naumann, M. Restoring endodontically treated teeth with post and cores–A review. Quintessence Int. 2005, 36, 737–746. [Google Scholar]
- Shutzky-Goldberg, I.; Shutzky, H.; Gorfil, C.; Smidt, A. Restoration of endodontically treated teeth review and treatment recommendations. Int. J. Dent. 2009, 2009, 150251. [Google Scholar] [CrossRef] [Green Version]
- Schwartz, R.S.; Robbins, J.W. Post placement and restoration of endodontically treated teeth: A literature review. J. Endodon. 2004, 30, 289–301. [Google Scholar] [CrossRef]
- Nair, P.N.R. On the cause of persistent apical periodontitis: A review. Int. Endod. J. 2006, 34, 249–281. [Google Scholar] [CrossRef]
- Siqueira, J.F.; Rocas, I.N.; Lopes, H.P.; de Uzeda, M. Coronal leakage of two root canal sealers containing calcium hydroxide after exposure to human saliva. J. Endod. 1999, 25, 14–16. [Google Scholar] [CrossRef]
- Hirsch, J.M.; Ahlstrom, U.; Henrikson, P.A.; Peterson, L.E. Periapical surgery. Int. J. Oral Surg. 1979, 8, 173–185. [Google Scholar] [CrossRef]
- Sundqvist, G.; Figdor, D.; Persson, S.; Sjörgren, U. Microbiological analysis of teeth with failed endodontic treatment and the outcome of conservative re-treatment. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1998, 85, 86–93. [Google Scholar] [CrossRef]
- Carrotte, P. Endodontics: Part 1. The modern concept of root canal treatment. Br. Dent. J. 2004, 197, 181–183. [Google Scholar] [CrossRef] [Green Version]
- Dental Endodontics Market (Product-Instruments (Endodontic Scalers & Lasers, Motors, Apex Locators, and Machine Assisted Obturation Systems) and Consumables (Obturation, Shaping and Cleaning, and Access Cavity Preparation); End User: Dental Hospitals, Dental Clinics, and Dental Academic & Research Institutes)-Global Industry Analysis, Size, Share, Growth, Trends, and Forecast 2017–2025. Available online: https://www.transparencymarketresearch.com/dental-endodontics-market.html (accessed on 6 April 2021).
- Endodontic Devices Market Size, Share & Trends Analysis Report By Type (Instruments, Consumables), By End Use (Hospitals, Clinics, Dental Academic & Research Institutes), And Segment Forecasts, 2019–2026. Available online: https://www.grandviewresearch.com/industry-analysis/endodontic-devices-market (accessed on 6 April 2021).
- Dental Consumables Market by Product [Dental Implants (Root Form Dental Implants and Plate Form Dental Implants), Dental Prosthetics (Crowns, Bridges, Dentures, Abutments, Veneers, and Inlays & Onlays), Endodontics (Endodontic Files, Obturators, and Permanent Endodontic Sealers), Orthodontics (Brackets, Archwires, Anchorage Appliances, and Ligatures), Periodontics (Dental Sutures and Dental Hemostats), Retail Dental Care Essentials (Specialized Dental Pastes, Dental Brushes, Dental Wash Solutions, Whitening Agents, and Dental Floss), and Other Dental Consumables (Dental Splints, Dental Sealants, Dental Burs, Dental Impression Materials, Dental Disposables, Bonding Agents, Patient Bibs, and Aspirator Tubes & Saliva Ejectors)]-Global Opportunity Analysis and Industry Forecast, 2017–2023. Available online: https://www.alliedmarketresearch.com/dental-consumables-market (accessed on 6 April 2021).
- Cohen, S.; Hargreaves, K. Pathways of the Pulp, 9th ed.; Mosby: St. Louis, MO, USA, 2006. [Google Scholar]
- Drabarczyk-Nasińska, M.; Kacprzak, M. Nowoczesne leczenie endodontyczne–materiały i metody wypełniania kanału korzeniowego. Borgis-Nowa Stomatol. 2001, 3, 11–14. [Google Scholar]
- Krasner, P.; Rankow, H.J.; Abrams, E.S. Endodontics. Colleagues for Excellence. Access Opening and Canal Location; American Association of Endodontists: Chicago, IL, USA, 2010. [Google Scholar]
- Moreinis, S.A. Avoiding perforation during endodontic access. J. Am. Dent. Assoc. 1979, 98, 707–712. [Google Scholar] [CrossRef]
- Weller, R.N.; Hartwell, G.R. The impact of improved access and searching techniques on detection of the mesiolingual canal in maxillary molars. J. Endod. 1989, 15, 82–83. [Google Scholar] [CrossRef]
- Stabholz, A.; Sahar-Helft, S.; Moshonov, J. Lasers in endodontics. Dent. Clin. N. Am. 2004, 48, 809–832. [Google Scholar] [CrossRef]
- Kimura, Y.; Wilder-Smith, P.; Matsumoto, K. Lasers in endodontics: A review. Int. Endod. J. 2000, 33, 173–185. [Google Scholar] [CrossRef]
- Van der Sluis, L.W.M.; Versluis, M.; Wu, M.K.; Wasserlink, P.R. Passive ultrasonic irrigation of the root canal: A review of the literature. Int. Endod. J. 2007, 40, 415–426. [Google Scholar] [CrossRef]
- Roy, R.A.; Ahmad, M.; Crum, L.A. Physical mechanisms governing the hydrodynamic response of an oscillating ultrasonic file. Int. Endod. J. 1994, 27, 197–207. [Google Scholar] [CrossRef]
- Huque, J.; Kota, K.; Yamaga, M.; Iwaku, M.; Hoshino, E. Bacterial eradication from root dentine by ultrasonic irrigation with sodium hypochloride. Int. Endod. J. 1998, 31, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Hülsmann, M.; Hahn, W. Complications during root canal irrigation-literature review and case reports. Int. Endod. J. 2000, 33, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, J.F.; Rôcas, I.N.; Favieri, A.; Lima, K.C. Chemomechanical reduction of the bacterial population in the root canal instrumentation and irrigation with 1%, 2.5% and 5.25% sodium hypochlorite. J. Endod. 2000, 26, 331–334. [Google Scholar] [CrossRef] [PubMed]
- Saleh, A.A.; Ettaman, W.M. Effect of endodontic irrigation solutions on microhardness of root canal dentine. J. Dent. 1999, 27, 43–46. [Google Scholar] [CrossRef]
- Walsh, L.J.; George, R. Activation of Alkaline Irrigation Fluids in Endodontics. Mater. 2017, 10, 1214. [Google Scholar] [CrossRef] [Green Version]
- Hart, J.R. Ethylenediaminetetraacetic Acid and Related Chelating Agents. In Ullmann’s Encyclopedia of Industrial Chemistry; Ullmann, F., Ed.; Wiley-VCH: Weinheim, Germany, 2000. [Google Scholar] [CrossRef]
- Wujec, P.; Pawlicka, H. Standardowe środki płuczące polecane w leczeniu endodontycznym – przegląd piśmiennictwa. Dent. Med. Probl. 2008, 45, 466–472. [Google Scholar]
- Heling, I.; Irani, E.; Karni, S.; Steinberg, D. In vitro antimicrobial effect of RC-Prep within dentinal tubules. J. Endod. 1999, 25, 782–785. [Google Scholar] [CrossRef]
- Morris, M.D.; Lee, K.W.; Bouillaguet, S.; Pashley, D.H. Effects of sodium hypochlorite and RC-Prep on bond strenghts of resin cement to endodontic surfaces. J. Endod. 2001, 27, 753–757. [Google Scholar] [CrossRef]
- Hryniewicz, T.; Rokosz, K. On the wear inspection and endurance recovery of Nitinol endodontic files. PAK 2009, 55, 247–250. [Google Scholar]
- Hülsmann, M.; Paters, O.A.; Dummer, P.M.H. Mechanical preparation of root canals: Shaping goals, techniques and means. Endod. Topics 2005, 10, 30–76. [Google Scholar] [CrossRef]
- Zuolo, M.L.; Walton, R.E. Instrument deterioration with usage: Nickel-titanium versus stainless steel. Quint. Int. 1997, 28, 397–402. [Google Scholar]
- Tanalp, J.; Kaplan, F.; Sert, S.; Kayahan, B.; Bayirl, G. Quantitative evaluation of the amount of apically extruded debris using 3 different rotary instrumentation systems. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 101, 250–257. [Google Scholar] [CrossRef]
- Pawlicka, H.; Ebert, J.; Prociów, A. Systematyka rotacyjnych narzędzi niklowo-tytanowych. Czas. Stomatol. 2005, 58, 709–713. [Google Scholar]
- Walia, H.M.; Brantley, W.A.; Gerstein, H. An initial investigation of the bending and torsional properties of Nitinol root canal files. J. Endod. 1988, 14, 346–351. [Google Scholar] [CrossRef]
- Anderson, M.E.; Price, J.H.W.; Parashos, P. Fracture resistance of electropolished rotary Nickel-Titanium endodontic instruments. J. Endod. 2007, 33, 1212–1216. [Google Scholar] [CrossRef]
- Duerig, T.; Pelton, A.; Stöckel, D. An overview of nitinol medical applications. Mater. Sci. Eng. A 1999, 273–275, 149–160. [Google Scholar] [CrossRef]
- Buehler, W.J.; Gilfrich, J.W.; Wiley, R.C. Effects of Low-Temperature Phase Changes on the Mechanical Properties of Alloys Near Composition TiNi. J. App. Phys. 1963, 34, 1475–1477. [Google Scholar] [CrossRef]
- Wang, F.E.; Buehler, W.J.; Pickart, S.J. Crystal Structure and a Unique Martensitic Transition of TiNi. J. App. Phys. 1965, 36, 3232–3239. [Google Scholar] [CrossRef]
- Metallurgy: The Alloy That Remembers. Available online: http://content.time.com/time/subscriber/article/0,33009,838687,00.html (accessed on 6 May 2021).
- Bergmans, L.; van Cleynenbreugel, J.; Wevers, M.; Lambrechts, P. Mechanical root canal preparation with NiTi rotary instruments: Rationale, performance and safety. Status report for the American Journal of Dentistry. Am. J. Dent. 2001, 14, 324–333. [Google Scholar]
- Hryniewicz, T.; Rokosz, K.; Rokicki, R. Magnetoelectropolishing process improves characteristics of finished metal surfaces: Intensity of externally applied magnetic field, plus oxygen control, manipulates rate of dissolution in electropolishing. Met. Finish. 2006, 104, 26–31, 33. [Google Scholar] [CrossRef]
- Hryniewicz, T. Wstęp Do Obróbki Powierzchniowej Biomateriałów Metalowych; Wyd. Politechniki Koszalińskiej: Koszalin, Poland, 2007; pp. 1–155. [Google Scholar]
- Rokicki, R.; Hryniewicz, T. Nitinol Surface Finishing by Magnetoelectropolishing. Trans. Inst. Met. Finish. 2008, 86, 280–285. [Google Scholar] [CrossRef]
- Hryniewicz, T.; Rokicki, R.; Rokosz, K. Modifying Metallic Implants with Magnetoelectropolishing. Med. Dev. Diagn. Ind. 2008, 30, 102–111. [Google Scholar]
- Mtwo. The efficient NiTi sytem. Available online: https://www.vdw-dental.com/en/products/detail/mtwo/ (accessed on 7 May 2021).
- Shi, P.; Cheng, F.T.; Man, H.C. Improvement in corrosion resistance of NiTi by anodization in acetic acid. Mater. Lett. 2007, 61, 2385–2388. [Google Scholar] [CrossRef]
- Ibris, N.; Rosca, J.C.M. EIS study of Ti and its alloys in biological media. J. Electroanal. Chem. 2002, 526, 53–62. [Google Scholar] [CrossRef]
- Tan, L.; Dodd, R.A.; Crone, W.C. Corrosion and wear-corrosion behaviour of NiTi modified by plasma source implantation. Biomater. 2003, 24, 3931–3939. [Google Scholar] [CrossRef]
- Cheng, F.T.; Shi, P.; Man, H.C. A preliminary study of TiO2 deposition on NiTi by a hydrothermal method. Surf. Coat. Technol. 2004, 187, 26–32. [Google Scholar] [CrossRef]
- Figueira, N.; Silva, T.M.; Carmezim, M.J.; Fernandes, J.C.S. Corrosion behaviour of NiTi alloy. Electrochim. Acta 2009, 54, 921–926. [Google Scholar] [CrossRef]
- Shabalovskaya, S.A. Surface, corrosion and biocompatibility aspects of Nitinol as an implant material. Biomed. Mater. Eng. 2002, 12, 69–109. [Google Scholar]
- Venugopalan, R.; Trépanier, C. Assessing the corrosion behaviour of Nitinol for minimally-invasive device design. Min. Invas. Therap. Allied Technol. 2000, 9, 67–74. [Google Scholar] [CrossRef]
- Rondelli, G.; Brunella, M.F.; De Nardo, L.; Cigada, A. Corrosion Behaviour of Nitinol Vascular Stents. Adv. Sci. Technol. 2006, 49, 252–257. [Google Scholar] [CrossRef]
- McInnes, P.M.; Wendt, S.L., Jr.; Retief, D.H.; Weinberg, R. Effect of dentin surface roughness on shear bond strength. Dent. Mater. 1990, 6, 204–207. [Google Scholar] [CrossRef]
- Thompson, S.A. An overview of nickel–titanium alloys used in dentistry. Int. Endod. J. 2000, 33, 297–310. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Himel, V.T.; Ahmed, K.M.; Wood, D.M.; Alhadainy, H.A. An evaluation of nitinol and stainless steel files used by dental students during a laboratory proficiency exam. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1995, 79, 232–237. [Google Scholar] [CrossRef]
- Pelton, A.R.; Stöckel, D.; Duerig, T.W. Medical Uses of Nitinol. MSF 2000, 327–328, 63–70. [Google Scholar] [CrossRef]
- Civjan, S.; Huget, E.F.; DeSimon, L.B. Potential applications of certain nickel-titanium (nitinol) alloys. J. Dent. Res. 1975, 54, 89–96. [Google Scholar] [CrossRef]
- Karacay, S.; Akin, E.; Olmez, H.; Gurton, A.U.; Sagdic, D. Forsus Nitinol Flat Spring and Jasper Jumper corrections of Class II division 1 malocclusions. Angle Orthod. 2006, 76, 666–672. [Google Scholar] [CrossRef]
- Lee, D.H.; Park, B.; Saxena, A.; Serene, T.P. Enhanced surface hardness by boron implantation in Nitinol alloy. J. Endod. 1996, 22, 543–546. [Google Scholar] [CrossRef]
- Wadood, A. Brief Overview on Nitinol as Biomaterial. Adv. Mater. Sci. Eng. 2016, 2016, 4173138. [Google Scholar] [CrossRef] [Green Version]
- Cutright, D.E.; Bhaskar, S.N.; Perez, B.; Johnson, R.M.; Cowan, G.S., Jr. Tissue reaction to nitinol wire alloy. Oral Surg. Oral Med. Oral Pathol. 1973, 35, 578–584. [Google Scholar] [CrossRef]
- Jensen, O.T.; Jansen, C.E.; Seo, Y.; Yellich, G. Guided Nitinol-Retained (Smileloc) Single-Tooth Dental Restorations. Oral Maxillofac. Surg. Clin. North Am. 2019, 31, 437–446. [Google Scholar] [CrossRef]
- GT Rotary Files 20/.06 Yellow 25mm. Available online: https://www.dentsplysirona.com/en-ca/products/endodontics/glide-path-shaping.html/Endodontics/Glide-Path-%26-Shaping/Rotary-%26-Reciprocating-Files/Shaping/GT-Rotary-Files/p/TUL-GTR0602025/c/1000671.html (accessed on 7 May 2021).
- ASTM 2063 Shape Memory Ni Ti Alloy Nitinol 55 Nitinol 60 Wire. Available online: https://www.nitinolcn.com/showroom/astm-2063-shape-memory-ni-ti-alloy-nitinol-55-nitinol-60-wire.html (accessed on 7 May 2021).
- ASTM F2063-18: Standard Specification for Wrought Nickel-Titanium Shape Memory Alloys for Medical Devices and Surgical Implants; ASTM International: West Conshohocken, PA, USA, 2018.
- Bojarski, Z.; Morawiec, H. Metale z Pamięcią Kształtu. PWN: Warszawa, Poland, 1989. [Google Scholar]
- Dobrzański, L.A.; Dobrzański, L.B.; Dobrzańska, J.; Dobrzański, J.; Jung, T. Application of nitinol type alloys in teeth endodontic treatment. Processes 2021. (prepared for printing). [Google Scholar]
- Yoneyama, T.; Doi, H.; Hamanaka, H.; Okamoto, Y.; Mogi, M.; Miura, F. Super-elasticity and thermal behavior of Ni-Ti alloy orthodontic arch wires. Dent. Mater. J. 1992, 11, 1–10. [Google Scholar] [CrossRef]
- Launey, M.; Robertson, S.W.; Vien, L.; Senthilnathan, K.; Chintapalli, P.; Pelton, A.R. Influence of microstructural purity on the bending fatigue behavior of VAR-melted superelastic Nitinol. J. Mech. Behav. Biomed. Mater. 2014, 34, 181–186. [Google Scholar] [CrossRef]
- Lin, Z.; Pike, K.; Schlun, M.; Zipse, A.; Draper, J. Nitinol Fatigue Life for Variable Strain Amplitude Fatigue. J. Mater. Eng. Perform. 2012, 21, 2628–2632. [Google Scholar] [CrossRef]
- Thompson, S.A.; Dummer, P.M. Shaping ability of Quantec Series 2000 rotary nickel-titanium instruments in simulated root canals: Part 2. Int. Endod. J. 1998, 31, 268–274. [Google Scholar] [CrossRef]
- Walia, H.; Costas, J.; Brantley, W.; Gerstein, H. Torsional ductility and cutting efficiency of the Nitinol file. J. Endod. 1989, 15, 174. [Google Scholar]
- Mayhew, M.J.; Kusy, R.P. Effects of sterilization on the mechanical properties and the surface topography of nickel-titanium arch wires. Am. J. Orthod. Dentofacial Orthop. 1988, 93, 232–236. [Google Scholar] [CrossRef]
- Mercier, O.; Torok, E. Mechanical properties of the coldworked martensitic NiTi type alloys. J. Physique 1982, 43, C4–C267. [Google Scholar] [CrossRef]
- Miura, F.; Mogi, M.; Ohura, Y.; Hamanaka, H. The super-elastic property of the Japanese NiTi alloy wire for use in orthodontics. Am. J. Orthod. Dentofacial Orthop. 1986, 90, 1–10. [Google Scholar] [CrossRef]
- Miura, F.; Mogi, M.; Okamoto, Y. New application of superelastic NiTi rectangular wire. J. Clin. Orthod. 1990, 24, 544–548. [Google Scholar]
- Saburi, T.; Tatsumi, T.; Nenno, S. Effects of heat treatment on mechanical behaviour of Ti-Ni alloys. J. Physique 1982, 43, C4–C261. [Google Scholar] [CrossRef]
- Sachdeva, R.; Fukuyo, S.; Suzuki, K.; Oshida, Y.; Miyazaki, S. Shape memory NiTi alloys–applications in dentistry. Mater. Sci. Forum 1990, 56–58, 693–698. [Google Scholar] [CrossRef]
- Kapila, S.; Haugen, J.W.; Watanabe, L.G. Load-deflection characteristics of nickel-titanium alloy wires after clinical recycling and dry heat sterilization. Am. J. Orthod. Dentofacial Orthop. 1992, 102, 120–126. [Google Scholar] [CrossRef]
- Kimura, H.; Sohmura, T. Pure Ti thermal spray coating on Ti-Ni shape memory alloys and Ti. J. Osaka Univ. Dent. School 1987, 6, 672–678. [Google Scholar]
- Thompson, S.A.; Dummer, P.M. Shaping ability of Lightspeed rotary nickel-titanium instruments in simulated root canals. Part 1. J. Endod. 1997, 23, 698–702. [Google Scholar] [CrossRef]
- Thompson, S.A.; Dummer, P.M. Shaping ability of Lightspeed rotary nickel-titanium instruments in simulated root canals. Part 2. J. Endod. 1997, 23, 742–747. [Google Scholar] [CrossRef]
- Thompson, S.A.; Dummer, P.M. Shaping ability of ProFile.04 Taper Series 29 rotary nickel-titanium instruments in simulated root canals. Part 1. Int. Endod. J. 1997, 30, 1–7. [Google Scholar] [CrossRef]
- Thompson, S.A.; Dummer, P.M. Shaping ability of ProFile.04 Taper Series 29 rotary nickel-titanium instruments in simulated root canals. Part 2. Int. Endod. J. 1997, 30, 8–15. [Google Scholar] [CrossRef]
- Thompson, S.A.; Dummer, P.M. Shaping ability of NT Engine and McXim rotary nickel-titanium instruments in simulated root canals. Part 1. Int. Endod. J. 1997, 30, 262–269. [Google Scholar] [CrossRef]
- Thompson, S.A.; Dummer, P.M. Shaping ability of NT Engine and McXim rotary nickel-titanium instruments in simulated root canals. Part 2. Int. Endod. J. 1997, 30, 270–278. [Google Scholar] [CrossRef]
- Thompson, S.A.; Dummer, P.M. Shaping ability of Mity Roto 360 degrees and Naviflex rotary nickel-titanium instruments in simulated root canals. Part 1. J. Endod. 1998, 24, 128–134. [Google Scholar] [CrossRef]
- Thompson, S.A.; Dummer, P.M. Shaping ability of Mity Roto 360 degrees and Naviflex rotary nickel-titanium instruments in simulated root canals. Part 2. J. Endod. 1998, 24, 135–142. [Google Scholar] [CrossRef]
- Hasegawa, K. The studies of Ti-Ni shape memory alloy for dental use–the influence of shape memory alloy post on the stress of post hole. J. Dent. Mater. 1991, 10, 509–517. [Google Scholar]
- Marsicovetere, E.S.; Clement, D.J.; del Rio, C.E. Morphometric video analysis of the engine-driven nickel-titanium Lightspeed instrument system. J. Endod. 1996, 22, 231–235. [Google Scholar] [CrossRef]
- Esposito, P.T.; Cunningham, C.J. A comparison of canal preparation with nickel-titanium and stainless steel instruments. J. Endod. 1995, 21, 173–176. [Google Scholar] [CrossRef]
- Evans, T.J.; Durning, P. Aligning archwires, the shape of things to come?—A fourth and fifth phase of force delivery. Br. J. Orthod. 1996, 23, 269–275. [Google Scholar] [CrossRef]
- Gould, J.V. Machinability of Nickel–Titanium Alloys; Report No, 573–4062–1; Report No, AD-419009; Metcut Research Associates: Cincinnati, OH, USA; Office of Technical Services, U.S. Dept of Commerce: Springfield, MO, USA, 1963.
- Glossen, C.R.; Haller, R.H.; Dove, S.B.; del Rio, C.E. A comparison of root canal preparations using Ni-Ti hand, Ni-Ti engine-driven, and K-Flex endodontic instruments. J. Endod. 1995, 21, 146–151. [Google Scholar] [CrossRef]
- Hamanaka, H.; Doi, H.; Kohno, O.; Miura, I. Dental castings of NiTi alloys. Part 2. New casting techniques for NiTi alloys. J. Dent. Mater. 1985, 4, 573–579. [Google Scholar]
- Hasegawa, K. Ti-Ni shape memory alloy for dental use. Trial production of prefabricated straight-slit type posts by electric discharge machining. J. Dent. Mater. 1989, 8, 388–409. [Google Scholar] [CrossRef]
- Wang, F.E.; Pickart, S.J.; Alperin, H.A. Mechanism of the TiNi martensitic transformation and the crystal structures of TiNi-II and TiNi-III phases. J. Appl. Phys. 1972, 43, 97–112. [Google Scholar] [CrossRef]
- Sarkar, N.K.; Redmond, W.; Schwaninger, B.; Goldberg, A.J. The chloride corrosion behaviour of four orthodontic wires. J. Oral Rehabil. 1983, 10, 121–128. [Google Scholar] [CrossRef]
- Thompson, S.A.; Dummer, P.M. Shaping ability of Quantec Series 2000 rotary nickel-titanium instruments in simulated root canals: Part 1. Int. Endod. J. 1998, 31, 259–267. [Google Scholar] [CrossRef]
- Andreasen, G.F.; Hilleman, T.B. An evaluation of 55 cobalt substituted Nitinol wire for use in orthodontics. J. Am. Dent. Assoc. 1971, 82, 1373–1375. [Google Scholar] [CrossRef]
- Andreasen, G.F.; Morrow, R.E. Laboratory and clinical analyses of nitinol wire. Am. J. Orthod. 1978, 73, 142–151. [Google Scholar] [CrossRef]
- Andreasen, G.; Wass, K.; Chan, K.C. A review of superelastic and thermodynamic nitinol wire. Quintessence Int. 1985, 16, 623–626. [Google Scholar]
- Bryant, S.T.; Thompson, S.A.; al-Omari, M.A.; Dummer, P.M. Shaping ability of Profile rotary nickel-titanium instruments with ISO sized tips in simulated root canals: Part 1. Int. Endod. J. 1998, 31, 275–281. [Google Scholar] [CrossRef]
- Bryant, S.T.; Thompson, S.A.; al-Omari, M.A.; Dummer, P.M. Shaping ability of ProFile rotary nickel-titanium instruments with ISO sized tips in simulated root canals: Part 2. Int. Endod. J. 1998, 31, 282–289. [Google Scholar] [CrossRef]
- Edie, J.; Andreasen, G. Surface corrosion of Nitinol and stainless wires. J. Dent. Res. 1980, 59, 528. [Google Scholar]
- Kimura, H.; Sohmura, T. Improvement in corrosion resistance of Ti-Ni shape memory alloy by oxide film coating. J. Dent. Mater. 1988, 7, 106–110. [Google Scholar]
- Kuo, P.; Yang, P.; Zhang, Y.; Yang, H.; Yu, Y.; Dai, K.; Hong, W.Q.; Ke, M.Z.; Cai, T.D.; Tao, J.C. The use of nickel–titanium alloy in orthopaedic surgery in China. Orthopaedics 1989, 12, 111–116. [Google Scholar] [CrossRef]
- Kusy, R.P.; Stush, A.M. Geometric and material parameters of a nickel-titanium and a beta titanium orthodontic arch wire alloy. Dent. Mater. 1987, 3, 207–217. [Google Scholar] [CrossRef]
- Kusy, R.P. A review of contemporary archwires: Their properties and characteristics. Angle Orthod. 1997, 67, 197–207. [Google Scholar] [CrossRef]
- Lee, J.H.; Park, J.B.; Andreasen, G.F.; Lakes, R.S. Thermomechanical study of Ni-Ti alloys. J. Biomed. Mater. Res. 1988, 22, 573–588. [Google Scholar] [CrossRef]
- Stoeckel, D.; Yu, W. Superelastic Ni-Ti wire. Wire J. Int. 1991, 24, 45–50. [Google Scholar]
- Edie, J.W.; Andreasen, G.F.; Zaytoun, M.P. Surface corrosion of nitinol and stainless steel under clinical conditions. Angle Orthod. 1981, 51, 319–324. [Google Scholar] [CrossRef]
- Lin, Z.; Pike, K.; Zipse, A.; Schlun, M. Nitinol Fatigue Investigation on Stent-Finish Specimens Using Tension-Tension Method. J. Mater. Eng. Perform. 2011, 20, 591–596. [Google Scholar] [CrossRef]
- Schäfer, E. Root canal instruments for manual use: A review. Dent. Traumatol. 1997, 13, 51–64. [Google Scholar] [CrossRef]
- Schäfer, E.; Tepel, J.; Hoppe, W. Properties of endodontic hand instruments used in rotary motion. Part 2. Instrumentation of curved canals. J. Endod. 1995, 21, 493–497. [Google Scholar] [CrossRef]
- Schettler, D.; Baumgart, F.; Bensmann, G.; Haasters, J. Method of alveolar bracing in mandibular fractures using a new form of fixation made from memory alloy (preliminary report). J. Maxillofac. Surg. 1979, 7, 51–54. [Google Scholar] [CrossRef]
- Serene, T.P.; Adams, J.D.; Saxena, A. Nickel–Titanium Instruments: Applications in Endodontics; Ishiyaku Euro America, Inc.: St Louis MO, USA, 1995. [Google Scholar]
- Buehler, W.J.; Wang, F.E. A summary of recent research on the Nitinol alloys and their potential application in ocean engineering. Ocean Eng. 1968, 1, 105–120. [Google Scholar] [CrossRef]
- Buehler, W.J.; Cross, W.B. 55-Nitinol unique wire alloy with a memory. Wire J. 1969, 2, 41–49. [Google Scholar]
- Burstone, C.J.; Goldberg, A.J. Beta titanium: A new orthodontic alloy. Am. J. Orthod. 1980, 77, 121–132. [Google Scholar] [CrossRef]
- Sarkar, N.K.; Schwaninger, B. The in vivo corrosion of Nitinol wire. J Dent. Res. 1980, 59, 528. [Google Scholar]
- Burstone, C.J. Variable-modulus orthodontics. Am. J. Orthod. 1981, 80, 1–16. [Google Scholar] [CrossRef]
- Clinard, K.; von Fraunhofer, J.A.; Kuftinec, M.M. The corrosion susceptibility of modern orthodontic spring wires. J. Dent. Res. 1981, 60, 628. [Google Scholar]
- Drake, S.R.; Wayne, D.M.; Powers, J.M.; Asgar, K. Mechanical properties of orthodontic wires in tension, bending, and torsion. Am. J. Orthod. 1982, 82, 206–210. [Google Scholar] [CrossRef]
- Duerig, W. Applications of shape memory. Mater. Sci. Forum 1990, 56–58, 679–692. [Google Scholar] [CrossRef]
- Smith, G.A.; von Fraunhofer, J.A.; Casey, G.R. The effect of clinical use and sterilization on selected orthodontic arch wires. Am. J. Orthod. Dentofacial Orthop. 1992, 102, 153–159. [Google Scholar] [CrossRef]
- Kai, W.-Y.; Chang, K.-C.; Wu, H.-F.; Chen, S.-W.; Yeh, A.-C. Formation mechanism of Ni2Ti4Ox in NITI shape memory alloy. Materialia 2019, 5, 100194. [Google Scholar] [CrossRef]
- Schaffer, J.E.; Plumley, D.L. Fatigue Performance of Nitinol Round Wire with Varying Cold Work Reductions. J. Mater. Eng. Perform. 2009, 18, 563–568. [Google Scholar] [CrossRef] [Green Version]
- Pelton, A.R.; Schroeder, V.; Mitchell, M.R.; Gong, X.Y.; Barney, M.; Robertson, S.W. Fatigue and durability of Nitinol stents. J. Mech. Behav. Biomed. Mater. 2008, 1, 153–164. [Google Scholar] [CrossRef]
- Elahinia, M.H.; Hashemi, M.; Tabesh, M.; Bhaduri, S.B. Manufacturing and processing of NiTi implants: A review. Prog. Mater. Sci. 2012, 57, 911–946. [Google Scholar] [CrossRef]
- Haberland, C.; Elahinia, M.; Walker, J.M.; Meier, H.; Frenzel, J. On the development of high quality NiTi shape memory and pseudoelastic parts by additive manufacturing. Smart Mater. Struct. 2014, 23, 104002. [Google Scholar] [CrossRef]
- Schetky, L.M.; Wu, M. Issues in the further development of Nitinol properties and processing for medical device applications. In Medical Device Materials, In Proceedings of the Materials & Processes for Medical Devices Conference, Anaheim, CA, USA, 8–10 September 2003; ASM International: Novelty, OH, USA, 2004; p. 271. [Google Scholar]
- Morgan, N.; Wick, A.; DiCello, J.; Graham, R. Carbon and oxygen levels in nitinol alloys and the implications for medical device manufacture and durability. In Proceedings of the International Conference on Shape Memory and Superelastic Technologies, Pacific Grove, CA, USA, 7–11 May 2006; ASM International: Novelty, OH, USA, 2006; pp. 821–828. [Google Scholar]
- Shugo, Y.; Hanada, S.; Honma, T. Effect of oxygen content on the martensite transformation and determination of defect structure in TiNi alloys. Bull. Res. Inst. Miner. Dress. Metall. 1985, 41, 23–34. [Google Scholar]
- Frenzel, J.; George, E.P.; Dlouhy, A.; Somsen, C.; Wagner, M.F.X.; Eggeler, G. Influence of Ni on martensitic phase transformations in NiTi shape memory alloys. Acta Mater. 2010, 58, 3444–3458. [Google Scholar] [CrossRef]
- Toro, A.; Zhou, F.; Wu, M.H.; Van Geertruyden, W.; Misiolek, W.Z. Characterization of non-metallic inclusions in superelastic NiTi tubes. J. Mater. Eng. Perform. 2009, 18, 448–458. [Google Scholar] [CrossRef]
- Rahim, M.; Frenzel, J.; Frotscher, M.; Pfetzing-Micklich, J.; Steegmüller, R.; Wohlschlögel, M.; Mughrabi, H.; Eggeler, G. Impurity levels and fatigue lives of pseudoelastic NiTi shape memory alloys. Acta Mater. 2013, 61, 3667–3686. [Google Scholar] [CrossRef]
- Robertson, S.W.; Pelton, A.R.; Ritchie, R.O. Mechanical fatigue and fracture of Nitinol. Int. Mater. Rev. 2012, 57, 1–37. [Google Scholar] [CrossRef]
- Mentz, J.; Frenzel, J.; Wagner, M.F.X.; Neuking, K.; Eggeler, G.; Buchkremer, H.P.; Stover, D. Powder metallurgical processing of NiTi shape memory alloys with elevated transformation temperatures. Mater. Sci. Eng. A 2008, 491, 270–278. [Google Scholar] [CrossRef]
- Frenzel, J.; Zhang, Z.; Neuking, K.; Eggeler, G. High quality vacuum induction melting of small quantities of NiTi shape memory alloys in graphite crucibles. J. Alloys Compd. 2004, 385, 214–223. [Google Scholar] [CrossRef]
- Steegmuller, R.; Ulmer, J.; Quellmalz, M.; Wohlschlogel, M.; Schussler, A. Analysis of new nitinol ingot qualities. J. Mater. Eng. Perform. 2014, 23, 2450–2456. [Google Scholar] [CrossRef]
- Wang, Z.; Everaerts, J.; Salvati, E.; Korsunsky, A.M. Evolution of thermal and mechanical properties of Nitinol wire as a function of ageing treatment conditions. J. Alloys Compd. 2020, 819, 153024. [Google Scholar] [CrossRef]
- Chad Hornbuckle, B.; Yu, X.X.; Noebe, R.D.; Martens, R.; Weaver, M.L.; Thompson, G.B. Hardening behavior and phase decomposition in very Ni-rich Nitinol alloys. Mater. Sci. Eng. A 2015, 639, 336–344. [Google Scholar] [CrossRef]
- Wang, X.; Kustov, S.; Verlinden, B.; Van Humbeeck, J. Fundamental development on utilizing the R-phase transformation in NiTi shape memory alloys. Shap. Mem. Superelasticity 2015, 1, 231–239. [Google Scholar] [CrossRef] [Green Version]
- Shamimi, A.; Amin-Ahmadi, B.; Stebner, A.; Duerig, T. The effect of low temperature aging and the evolution of R-phase in Ni-rich NiTi. Shap. Mem. Superelasticity 2018, 4, 417–427. [Google Scholar] [CrossRef]
- Velmurugan, C.; Senthilkumar, V.; Dinesh, S.; Arulkirubakaran, D. Review on phase transformation behavior of NiTi shape memory alloys. Mater. Today Proc. 2018, 5, 14597–14606. [Google Scholar] [CrossRef]
- Kim, J.I.; Miyazaki, S. Effect of nano-scaled precipitates on shape memory behavior of Ti-50.9at.% Ni alloy. Acta Mater. 2005, 53, 4545–4554. [Google Scholar] [CrossRef]
- Liang, X.; Xiao, F.; Chen, H.; Li, Z.; Li, Z.; Jin, X.; Fukuda, T. Internal friction of the R-phase in single crystalline Ti-50.8Ni (at.%) alloy containing controlled precipitate of Ti3Ni4. Scr. Mater. 2019, 166, 44–47. [Google Scholar] [CrossRef]
- Pourbabak, S.; Orekhov, A.; Samaee, V.; Verlinden, B.; Van Humbeeck, J.; Schryvers, D. In-Situ TEM stress induced martensitic transformation in Ni50.8Ti49.2 microwires. Shap. Mem. Superelasticity 2019, 5, 154–162. [Google Scholar] [CrossRef]
- Hirsch, P.; Howie, A.; Nicholson, R.B.; Pashley, D.W.; Whelan, M.J. Electron Microscopy of Thin Crystals, 2nd ed.; R. E. Krieger Publishing Company: Malabar, FL, USA, 1977; pp. 169, 317. [Google Scholar]
- Honma, T. The effect of aging, on the spontaneous shape change and the all-round shape memory effect in Ni-rich TiNi alloy. In Proceedings of the International Conference on Martensitic Transformations ICOMAT-86, Nara, Japan, 26–30 August 1986; pp. 709–716. [Google Scholar]
- Kainuma, R.; Matsumoto, M.; Honma, T. The mechanism of the all-round shape memory effect in a Ni-rich TiNi alloy. In Proceedings of the International Conference on Martensitic Transformations ICOMAT-86, Nara, Japan, 26–30 August 1986; pp. 717–722. [Google Scholar]
- Koskimaki, D.; Marcinkowski, M.J.; Sastri, A.S. Solid State Diffusional Transformations in the Near Equiatomic Ni-Ti Alloys. Trans. Metall. Soc. AIME 1969, 245, 1883–1890. [Google Scholar]
- Chen, Q.; Wu, X.F.; Ko, T. The effects of Ti3Ni4 precipitates on the R-phase transformation. Scr. Metall. Mater. 1993, 29, 49–53. [Google Scholar] [CrossRef]
- Xie, C.Y.; Zhao, L.C.; Lei, T.C. Effect of precipitates on the electrical resistivity-temperature curves in an aged Ti-51.8 at % Ni shape memory alloy. Scr. Metall. 1989, 23, 2131–2136. [Google Scholar] [CrossRef]
- Xie, C.Y.; Zhao, L.C.; Lei, T.C. Effect of Ti3Ni4 precipitates on the phase transitions in an aged Ti-51.8at% Ni shape memory alloy. Scr. Metall. Mater. 1990, 24, 1753–1758. [Google Scholar] [CrossRef]
- Khalil-Allafi, J.; Ren, X.; Eggeler, G. The mechanism of multistage martensitic transformations in aged Ni-rich NiTi shape memory alloys. Acta Mater. 2002, 50, 793–803. [Google Scholar] [CrossRef]
- Fan, G.; Chen, W.; Yang, S.; Zhu, J.; Ren, X.; Otsuka, K. Origin of abnormal multi-stage martensitic transformation behavior in aged Ni-rich Ti–Ni shape memory alloys. Acta Mater. 2004, 52, 4351–4362. [Google Scholar] [CrossRef]
- Van Humbeeck, J. Non-medical applications of shape memory alloys. Mater. Sci. Eng. A 1999, 273–275, 134–148. [Google Scholar] [CrossRef]
- Ren, X.; Miura, N.; Taniwaki, K.; Otsuka, K.; Suzuki, T.; Tanaka, K.; Chumlyakov, Y.I.; Asai, M. Understanding the martensitic transformations in TiNi-based alloys by elastic constants measurement. Mater. Sci. Eng. A 1999, 273–275, 190–194. [Google Scholar] [CrossRef]
- Otsuka, K.; Ren, X. Martensitic transformations in nonferrous shape memory alloys. Mater. Sci. Eng. A 1999, 273–275, 89–105. [Google Scholar] [CrossRef]
- Otsuka, K.; Ren, X. Physical Metallurgy of Ti-Ni-based Shape Memory Alloys. Prog. Mater. Sci. 2005, 50, 511–678. [Google Scholar] [CrossRef]
- Wang, X.; Li, K.; Schryvers, D.; Verlinden, B.; Van Humbeeck, J. R-phase transition and related mechanical properties controlled by low-temperature aging treatment in a Ti–50.8at.% Ni thin wire. Scr. Mater. 2014, 72–73, 21–24. [Google Scholar] [CrossRef]
- Dautovich, D.P.; Purdy, G.R. Phase Transformations in TiNi. Canad. Metall. Quart. 1965, 4, 129–143. [Google Scholar] [CrossRef]
- Tadaki, T.; Nakata, Y.; Shimizu, K.; Otsuka, K. Crystal Structure, Composition and Morphology of a Precipitate in an Aged Ti-51 at%Ni Shape Memory Alloy. Trans. JIM 1986, 27, 731–740. [Google Scholar] [CrossRef] [Green Version]
- Frick, C.P.; Ortega, A.M.; Tyber, J.; Gall, K.; Maier, H.J. Multiscale structure and properties of cast and deformation processed polycrystalline NiTi shape-memory alloys. Metall. Mater. Trans. A 2004, 35, 2013–2025. [Google Scholar] [CrossRef]
- Tirry, W.; Schryvers, D. Quantitative determination of strain fields around Ni4Ti3 precipitates in NiTi. Acta Mater. 2005, 53, 1041–1049. [Google Scholar] [CrossRef]
- Šittner, P.; Landa, M.; Lukáš, P.; Novák, V. R-phase transformation phenomena in thermomechanically loaded NiTi polycrystals. Mech. Mater. 2006, 38, 475–492. [Google Scholar] [CrossRef]
- Ha, J.H.; Kim, S.K.; Cohenca, N.; Kim, H.C. Effect of R-phase heat treatment on torsional resistance and cyclic fatigue fracture. J. Endod. 2013, 39, 389–393. [Google Scholar] [CrossRef]
- Pelton, A.R.; Huang, G.H.; Moine, P.; Sinclair, R. Effects of thermal cycling on microstructure and properties in Nitinol. Mater. Sci. Eng. A 2012, 532, 130–138. [Google Scholar] [CrossRef]
- Tobushi, H.; Yamada, S.; Hachisuka, T.; Ikai, A.; Tanaka, K. Thermomechanical properties due to martensitic and R-phase transformations of TiNi shape memory alloy subjected to cyclic loadings. Smart Mater. Struct. 1996, 5, 788. [Google Scholar] [CrossRef]
- Uchil, J.; Kumara, K.G.; Mahesh, K.K. Effect of thermal cycling on R-phase stability in a NiTi shape memory alloy. Mater. Sci. Eng. A 2002, 332, 25–28. [Google Scholar] [CrossRef]
- Miyazaki, S.; Igo, Y.; Otsuka, K. Effect of thermal cycling on the transformation temperatures of Ti-Ni alloys. Acta Metall. 1986, 34, 2045–2051. [Google Scholar] [CrossRef]
- Miyazaki, S.; Otsuka, K. Deformation and transition behavior associated with the R-phase in Ti-Ni alloys. Metall. Mater. Trans. A 1986, 17, 53–63. [Google Scholar] [CrossRef]
- Miyazaki, S.; Kimura, S.; Otsuka, K. Shape-memory effect and pseudoelasticity associated with the R-phase transition in Ti-50·5 at.% Ni single crystals. Philos. Mag. A 1988, 57, 467–478. [Google Scholar] [CrossRef]
- Tobushi, H.; Kimura, K.; Sawada, T.; Hattori, T.; Lin, P.H. Recovery Stress Associated with R-Phase Transformation in TiNi Shape Memory Alloy: Properties under Constant Residual Strain. JSME Int. J. A 1994, 37, 138–142. [Google Scholar] [CrossRef] [Green Version]
- Miyazaki, S.; Otsuka, K. Mechanical behaviour associated with the premartensitic rhombohedral-phase transition in a Ti50Ni47Fe3 alloy. Philos. Mag. A 1985, 50, 393–408. [Google Scholar] [CrossRef]
- Tadayyon, G.; Mazinani, M.; Guo, Y.; Zebarjad, S.M.; Tofail, S.A.M.; Biggs, M.J. The effect of annealing on the mechanical properties and microstructural evolution of Ti-rich NiTi shape memory alloy. Mater. Sci. Eng. A 2016, 662, 564–577. [Google Scholar] [CrossRef]
- Huang, X.; Liu, Y. Effect of annealing on the transformation behavior and superelasticity of NiTi shape memory alloy. Scr. Mater. 2001, 45, 153–160. [Google Scholar] [CrossRef]
- Gall, K.; Tyber, J.; Wilkesanders, G.; Robertson, S.W.; Ritchie, R.O.; Maier, H.J. Effect of microstructure on the fatigue of hot-rolled and cold-drawn NiTi shape memory alloys. Mater. Sci. Eng. A 2008, 486, 389–403. [Google Scholar] [CrossRef]
- Khalil-Allafi, J.; Eggeler, G.; Dlouhy, A.; Schmahl, W.W.; Somsen, C.H. On the influence of heterogeneous precipitation on martensitic transformations in a Ni-rich NiTi shape memory alloy. Mater. Sci. Eng. A 2004, 378, 148–151. [Google Scholar] [CrossRef]
- Nishida, M.; Wayman, C.M. Electron microscopy studies of the “Premartensitic” transformations in an aged Ti-51 at%Ni shape memory alloy. Metallography 1988, 21, 255–273. [Google Scholar] [CrossRef]
- Favier, D.; Liu, Y.; McCormick, P.G. Three stage transformation behaviour in aged NiTi. Scr. Metall. Mater. 1993, 28, 669–672. [Google Scholar] [CrossRef]
- Liu, X.; Wang, Y.; Yang, D.; Qi, M. The effect of ageing treatment on shape-setting and superelasticity of a nitinol stent. Mater. Charact. 2008, 59, 402–406. [Google Scholar] [CrossRef]
- Matsumoto, H. Appearance of an intermediate phase with thermal cycling on the transformation of NiTi. J Mater Sci Lett 1991, 10, 408–410. [Google Scholar] [CrossRef]
- Matsumoto, H. Transformation behaviour with thermal cycling in NiTi alloys. J. Alloys Compd. 2003, 350, 213–217. [Google Scholar] [CrossRef]
- Dilibal, S.; Hamilton, R.F.; Lanba, A. The effect of employed loading mode on the mechanical cyclic stabilization of NiTi shape memory alloys. Intermetallics 2017, 89, 1–9. [Google Scholar] [CrossRef]
- Piekielny, M.; Jarmołowicz, M.; Dobrzyński, M. Odporność na cykliczne zmęczenie wybranych endodontycznych narzędzi maszynowych w świetle piśmiennictwa. Inż. Fiz. Med. 2020, 9, 143–144. [Google Scholar]
- Khalil-Allafi, J.; Eggeler, G.; Schmahl, W.W. Quantitative phase analysis in microstructures which display multiple step martensitic transformations in Ni-rich NiTi shape memory alloys. Mater. Sci. Eng. A 2006, 438–440, 593–596. [Google Scholar] [CrossRef]
- Zou, W.H.; Han, X.D.; Wang, R.; Zhang, Z.; Zhang, W.-Z.; Lai, J.K.L. TEM and HREM study of the interphase interface structure of Ti3Ni4 precipitates and parent phase in an aged TiNi shape memory alloy. Mater. Sci. Eng. A 1996, 219, 142–147. [Google Scholar] [CrossRef]
- Cao, S.; Nishida, M.; Schryvers, D. Quantitative three-dimensional analysis of Ni4Ti3 precipitate morphology and distribution in polycrystalline Ni-Ti. Acta Mater. 2011, 59, 1780–1789. [Google Scholar] [CrossRef]
- Xue, D.; Zhou, Y.; Ren, X. The effect of ageing on the B2-R transformation behaviors in Ti-51at%Ni alloy. Intermetal. 2011, 19, 1752–1758. [Google Scholar] [CrossRef]
- Jordan, L.; Chandrasekaran, M.; Masse, M.M.; Bouquet, G. Study of the phase transformation in Ni-Ti based shape memory alloys. J. Phys. IV France 1995, 05, C2–C489. [Google Scholar] [CrossRef] [Green Version]
- Rapisarda, E.; Bonaccorso, A.; Tripi, T.R.; Condorelli, G.G. Effect of sterilization on the cutting efficiency of rotary nickel-titanium endodontic files. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1999, 88, 343–347. [Google Scholar] [CrossRef]
- Plotino, G.; Costanzo, A.; Grande, N.M.; Petrovic, R.; Testarelli, L.; Gambarini, G. Experimental Evaluation on the Influence of Autoclave Sterilization on the Cyclic Fatigue of New Nickel-Titanium Rotary Instruments. J. Endod. 2012, 38, 222–225. [Google Scholar] [CrossRef]
- La Chapelle, C.F.; Veersema, S.; Brölmann, H.A.M.; Jansen, F.W. Effectiveness and feasibility of hysteroscopic sterilization techniques: A systematic review and meta-analysis. Fertil. Steril. 2015, 103, 1516–1525.e3. [Google Scholar] [CrossRef]
- Dioguardi, M.; Laneve, E.; Di Cosola, M.; Cazzolla, A.P.; Sovereto, D.; Aiuto, R.; Laino, L.; Leanza, T.; Alovisi, M.; Troiano, G.; et al. The Effects of Sterilization Procedures on the Cutting Efficiency of Endodontic Instruments: A Systematic Review and Network Meta-Analysis. Materials 2021, 14, 1559. [Google Scholar] [CrossRef]
- Schafer, E. Effect of sterilization on the cutting efficiency of PVD-coated nickel-titanium endodontic instruments. Int. Endod. J. 2002, 35, 867–872. [Google Scholar] [CrossRef]
- Seago, S.T.; Bergeron, B.E.; Kirkpatrick, T.C.; Roberts, M.D.; Roberts, H.W.; Himel, V.T.; Sabey, K.A. Effect of Repeated Simulated Clinical Use and Sterilization on the Cutting Efficiency and Flexibility of Hyflex CM Nickel-Titanium Rotary Files. J. Endod. 2015, 41, 725–728. [Google Scholar] [CrossRef]
- Haïkel, Y.; Serfaty, R.; Wilson, P.; Speisser, J.M.; Allemann, C. Cutting efficiency of nickel-titanium endodontic instruments and the effect of sodium hypochlorite treatment. J. Endod. 1998, 24, 736–739. [Google Scholar] [CrossRef]
- Neal, R.G.; Craig, R.G.; Powers, J.M. Effect of sterilization and irrigants on the cutting ability of stainless steel files. J. Endod. 1983, 9, 93–96. [Google Scholar] [CrossRef]
- Morrison, S.W.; Newton, C.W.; Brown, C.E. The effects of steam sterilization and usage on cutting efficiency of endodontic instruments. J. Endod. 1989, 15, 427–431. [Google Scholar] [CrossRef]
- Haïkel, Y.; Serfaty, R.; Lwin, T.T.; Allemann, C. Measurement of the cutting efficiency of endodontic instruments: A new concept. J. Endod. 1996, 22, 651–656. [Google Scholar] [CrossRef]
- Webber, J.; Moser, J.B.; Heuer, M.A. A method to determine the cutting efficiency of root canal instruments in linear motion. J. Endod. 1980, 6, 829–834. [Google Scholar] [CrossRef]
- Villalobos, R.L.; Moser, J.B.; Heuer, M.A. A method to determine the cutting efficiency of root canal instruments in rotary motion. J. Endod. 1980, 6, 667–671. [Google Scholar] [CrossRef]
- Molven, O. A comparison of the dentin-removing ability of five root canal instruments. Scand. J. Dent. Res. 1970, 78, 500–511. [Google Scholar] [CrossRef]
- Oliet, S.; Sorin, S.M. Cutting efficiency of endodontic reamers. Oral Surg. Oral Med. Oral Pathol. 1973, 36, 243–252. [Google Scholar] [CrossRef]
- Fromme, H.G.; Riedel, H. Treatment of Dental Root Canals and the Marginal Contact between Filling Material and Tooth, studied by Scanning Electronic Microscopy. Int. Endod. J. 1972, 6, 17–20. [Google Scholar] [CrossRef]
- Stefanescu, T.; Popovici, R.A.; Antoniac, I.V.; Galuscan, A.; Tirca, T. Ni-Ti Rotary Instrument Fracture Analysis after Clinical Use. Structure Changes in Used Instruments. Environ. Eng. Manag. J. 2016, 15, 981–988. [Google Scholar] [CrossRef]
- Matei, A.; Pencea, I.; Stanciu, S.; Hristu, R.; Antoniac, I.; Coman, E.C.; Sfat, C.; Stanciu, G. Structural characterization and adhesion appraisal of TiN and TiCN coatings deposited by CAE-PVD technique on a new carbide composite cutting tool. J. Adhes. Sci. Technol. 2015, 29, 2576–2589. [Google Scholar] [CrossRef]
- Inan, U.; Keskin, C. Torsional Resistance of ProGlider, Hyflex EDM, and One G Glide Path Instruments. J. Endod. 2019, 45, 1253–1257. [Google Scholar] [CrossRef]
- Spagnuolo, G.; Ametrano, G.; d’Antò, V.; Rengo, C.; Simeone, M.; Riccitiello, F.; Amato, M. Effect of autoclaving on the surfaces of TiN-coated and conventional nickel-titanium rotary instruments. Int. Endod. J. 2012, 45, 1148–1155. [Google Scholar] [CrossRef]
- Razavian, H.; Iranmanesh, P.; Mojtahedi, H.; Nazeri, R. Effect of Autoclave Cycles on Surface Characteristics of S-File Evaluated by Scanning Electron Microscopy. Iran. Endod. J. 2015, 11, 29–32. [Google Scholar] [CrossRef]
- Nair, A.S.; Tilakchand, M.; Naik, B.D. The effect of multiple autoclave cycles on the surface of rotary nickel-titanium endodontic files: An in vitro atomic force microscopy investigation. J. Conserv. Dent. 2015, 18, 218–222. [Google Scholar] [PubMed] [Green Version]
- Fayyad, D.M.; Elgendy, A.A.E. Cutting Efficiency of Twisted versus Machined Nickel-Titanium Endodontic Files. J. Endod. 2011, 37, 1143–1146. [Google Scholar] [CrossRef] [PubMed]
- Hilt, B.R.; Cunningham, C.J.; Shen, C.; Richards, N. Torsional Properties of Stainless-Steel and Nickel-Titanium Files After Multiple Autoclave Sterilizations. J. Endod. 2000, 26, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Shahi, S.; Zand, V.; Oskoee, S.S.; Abdolrahimi, M.; Rahnema, A.H. An in vitro study of the effect of spreader penetration depth and apical microleakage. J. Oral Sci. 2007, 49, 283–286. [Google Scholar] [CrossRef] [Green Version]
- Silva, D.; Endal, U.; Reynaud, A.; Portenier, I.; Ǿstravik, D.; Haapasalo, M. A comparative study of lateral condensation, heat-softened gutta-percha and modified master cone heat-softened backfilling technique. Int. Endod. J. 2002, 35, 1005–1111. [Google Scholar] [CrossRef]
- Nielsen, B.A.; Baumgartner, J.C. Spreader penetration during lateral compaction of resilon and gutta-percha. J. Endod. 2006, 32, 52–54. [Google Scholar] [CrossRef]
- Johnson, W.B. A new gutta-percha technique. J. Endod. 1978, 4, 184–188. [Google Scholar] [CrossRef]
- Buchanan, S.L. The continuous wave of obturation technique: ”Centered” condensation of warm gutta-percha in 12 seconds. Dent. Today 1996, 15, 60–67. [Google Scholar]
- Bugea, C. Continuous Wave of Condensation. Available online: http://endodontics.styleitaliano.org/continuous-wave-of-condensation/ (accessed on 17 May 2021).
- Barbosa, F.O.G.; Gusman, H.; Pimenta de Araujo, M.C. A comparative study on the frequency location and direction of accessory canals filled with the hydraulic vertical condensation and continuous wave of condensation techniques. J. Endod. 2009, 35, 397–400. [Google Scholar] [CrossRef]
- Nahmias, Y.; Mab, T.; Dovgan, J.S. The Thermo-Hydraulic Condensation Technique. Available online: https://www.endoexperience.com/documents/YTHTTechnique2001.pdf (accessed on 17 May 2021).
- Barattolo, R.; Santarcangelo, F. Otturazione del sistema dei canali radicolari con guttaperca termoplasticizzata: Principi, materiali e tecniche. G. Italia. Endod. 2011, 25, 112–124. [Google Scholar] [CrossRef] [Green Version]
- DuLac, K.A.; Nielsen, C.J.; Tomazic, T.J.; Ferrillo, P.J.; Hatton, J.F. Comparison of the obturation of lateral canals by six techniques. J. Endod. 1999, 25, 376–380. [Google Scholar] [CrossRef]
- Karamifar, K.; Tondari, A.; Saghiri, M.A. Endodontic Periapical Lesion: An Overview on the Etiology, Diagnosis and Current Treatment Modalities. Eur. Endod. J. 2020, 2, 54–67. [Google Scholar] [CrossRef]
- Grossman, L. Endodontic Practice, 11th ed; Lea & Fibiger: Philadelphia, PA, USA, 1988; p. 242. [Google Scholar]
- Muliyar, S.; Shameem, K.A.; Thankachan, R.P.; Francis, P.G.; Jayapalan, C.S.; Hafiz, K.A. Microleakage in endodontics. J. Int. Oral Health. 2014, 6, 99–104. [Google Scholar]
- Krastl, G.; Allgayer, N.; Lenherr, P.; Filippi, A.; Taneja, P.; Weiger, R. Tooth discoloration induced by endodontic materials: A literature review. Dent. Traumatol. 2013, 29, 2–7. [Google Scholar] [CrossRef]
- Teixeira, F.B.; Teixeira, E.C.; Thompson, J.Y.; Trope, M. Fracture resistance of roots endodontically treated with a new resin filling material. J. Am. Dent. Assoc. 2004, 135, 646–652. [Google Scholar] [CrossRef]
- Ferreira, C.M.; Silva, J.B.A., Jr.; Monteiro de Paula, R.C.; Andrade Feitosa, J.P.; Negreiros Cortez, D.G.; Zaia, A.A.; de Souza-Filho, F.J. Brazilian gutta-percha points. Part I: Chemical composition and X-ray diffraction analysis. Braz. Oral Res. 2005, 19, 193–197. [Google Scholar] [CrossRef] [Green Version]
- Dobrzańska, J.; Gołombek, K.; Dobrzański, L.B. Polymer materials used in endodontic treatment–in vitro testing. AMSE 2012, 58, 110–115. [Google Scholar]
- Schilder, H.; Goodman, A.; Winthrop, A. The termomechanical properties of gutta-percha. Determination of phase transition temperatures for gutta-percha. Oral Surg. Oral Med. Oral Pathol. 1974, 38, 109–114. [Google Scholar] [CrossRef]
- Ferreira, C.M.; Gurgel-Filho, E.D.; Silva, J.B.A., Jr.; Monteiro de Paula, R.C.; Pessoa Andrade Feitosa, J.; Figueiredo de Almeida Gomes, B.P.; de Souza-Filho, F.J. Brazilian gutta-percha points. Part II: Thermal properties. Braz. Oral Res. 2007, 21, 29–34. [Google Scholar] [CrossRef] [Green Version]
- Combe, E.C.; Cohen, B.D.; Cumming, K. Alpha- and beta-forms of gutta-percha in products for root canal filling. Int. Endodon. J. 2001, 34, 447–451. [Google Scholar] [CrossRef]
- Li, G.H.; Niu, L.N.; Selem, L.C.; Eid, A.A.; Bergeron, B.E.; Chen, J.H.; Pashley, D.H.; Tay, F.R. Quality of obturation achieved by an endodontic core-carrier system with crosslinked gutta-percha carrier in single-rooted canals. J. Dent. 2014, 42, 1124–1134. [Google Scholar] [CrossRef] [Green Version]
- Donnermeyer, D.; Bürklein, S.; Dammaschke, T.; Schäfer, E. Endodontic sealers based on calcium silicates: A systematic review. Odontol. 2019, 107, 421–436. [Google Scholar] [CrossRef]
- Gandolfi, M.G.; Siboni, F.; Prati, C. Properties of a novel polysiloxane-guttapercha calcium silicate-bioglass-containing root canal sealer. Dent. Mater. 2016, 32, e113–e126. [Google Scholar] [CrossRef]
- Schilder, H. Filling root canals in three dimensions. Dent. Clin. North Am. 1967, 11, 723–744. [Google Scholar] [CrossRef] [PubMed]
- Buchanan, L.S. The continuous wave of condensation technique: A convergence of conceptual and procedural advances in obturation. Dent. Today 1994, 13, 80, 82, 84, 85. [Google Scholar]
- Hand, R.E.; Huget, E.F.; Tsakinis, P.J. Effects of a warm gutta-percha technique on the lateral periodontium. Oral Surg. Oral Med. Oral Pathol. 1976, 42, 395–401. [Google Scholar] [CrossRef]
- Nahmias, Y.; Mab, T.; Dovgan, J.S. The Thermo Hydraulic Condensation Technique. Oral Health 2001, 91, 11–15. [Google Scholar]
- Nahmias, Y.; Serota, K.S.; Watson, W.R., Jr. Predictable Endodontic Success: Part II—Microstructural Replication. Available online: http://www.ecoweek.ca/issues/PrinterFriendly.asp?aid=1000156065&RType=&PC=&issue=12012003 (accessed on 6 April 2021).
- Nahmias, Y.; Mab, T.; Dovgan, J.S. La tecnica di condensazione termoidraulica. L’infor. Endod. 2002, 5, 28–33. [Google Scholar]
- Nahmias, Y.; Bery, P. Due radici palatine nei primi molari superiori. L’infor. Endod. 2007, 10, 48–51. [Google Scholar]
- Carvalho-Sousa, B.; Almeida-Gomes, F.; Carvalho, P.R.; Maníglia-Ferreira, C.; Gurgel-Filho, E.D.; Albuquerque, D.S. Filling lateral canals: Evaluation of different filling techniques. Eur. J. Dent. 2010, 4, 251–256. [Google Scholar] [CrossRef]
- Siqueira, J.F.; Roças, I.N.; Favieri, A.; Abad, E.C.; Castro, A.J.; Gahyva, S.M. Bacterial leakage in coronally unsealed root canals obturated with 3 different techniques. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2000, 90, 647–650. [Google Scholar] [CrossRef] [PubMed]
- Limkangwalmongkol, S.; Burtscher, P.; Abbot, P.; Sandler, A.; Bishop, B. A comparative study of the apical leakage of four root canals sealers and laterally condensed gutta percha. J. Endod. 1991, 17, 495–499. [Google Scholar] [CrossRef]
- Swanson, K.; Madison, S. An evaluation of coronal microleakage in endodontically treated teeth. Part 1. Time periods. J. Endod. 1987, 13, 56–59. [Google Scholar] [CrossRef]
- Friedman, S.; Torneck, C.; Komorowsji, R.; Ouzounian, Z.; Syrtash, P.; Kaufman, A. In vivo model for assessing the functional efficacy of endodontic materials and techniques. J. Endod. 1997, 23, 557–561. [Google Scholar] [CrossRef]
- Torabinejad, M.; Ung, B.; Kettering, J. In vitro bacterial penetration of coronally unsealed endodontically treated teeth. J. Endod. 1990, 16, 566–569. [Google Scholar] [CrossRef]
- Shipper, G.; Trope, M. In vitro microbial leakage of endodontically treated teeth using new and standard obturation techniques. J. Endod. 2004, 30, 154–158. [Google Scholar] [CrossRef]
- Magura, M.E.; Kafrawy, A.H.; Brown, C.E.; Newton, C.W. Human saliva coronal microleakeage in obturated root canals: An in vitro study. J. Endod. 1991, 17, 324–331. [Google Scholar] [CrossRef]
- Oliver, C.; Abbott, P. An in vitro study of apical and coronal micro leakage of laterally condensed gutta-percha with Ketac-Endo and AH-26. Aust. Dent. J. 1998, 43, 262–268. [Google Scholar] [CrossRef]
- Madison, S.; Wilcox, L. An evaluation of coronal microleakge in endodontically treated teeth. Part III. In vivo study. J. Endod. 1988, 14, 455–458. [Google Scholar] [CrossRef]
- Khayat, A.; Lee, S.J.; Torabinejad, M. Human saliva penetration of coronally unsealed obturated root canals. J. Endod. 1993, 19, 458–461. [Google Scholar] [CrossRef]
- Gatwood, R.S. Endodontic materials. Dent. Clin. North Am. 2007, 15, 695–712. [Google Scholar] [CrossRef]
- Shipper, G.; Ørstavik, D.; Teixeira, F.B.; Trope, M. An evaluation of microbial leakage in roots filled with a thermoplastic synthetic polymer-based root canal filling material (Resilon). J. Endod. 2004, 30, 342–347. [Google Scholar] [CrossRef]
- Resilon™ Obturation Material—The New Standard of Care? Available online: https://www.endoexperience.com/filecabinet/Clinical%20Endodontics/Obturation/Resilon/Resilon.Fact.Sheet.pdf (accessed on 1 April 2021).
- Lipski, M.; Woźniak, K.; Buczkowska-Radlińska, J.; Łagocka, R.; Bochińska, J.; Nowicka, A. Resilon i Epiphany nowy materiał do wypełniania kanałów korzeniowych zębów: Badania wstępne w SEM. Mag. Stomat. 2005, 9, 108–112. [Google Scholar]
- Lotfi, M.; Ghasemi, N.; Rahimi, S.; Vosoughhosseini, S.; Saghiri, M.A.; Shahidi, A. Resilon: A comprehensive literature review. J. Dent. Res. Dent. Clin. Dent. Prospects 2013, 7, 119–130. [Google Scholar] [CrossRef]
- Pawińska, M.; Kierklo, A.; Marczuk-Kolada, G. New technology in endodontics—The Resilon-Epiphany system for obturation of root canals. Adv. Med. Sci. 2006, 51, 154–157. [Google Scholar]
- Pocket Dentistry. Gutta-percha Substitute: Resilon. Available online: https://pocketdentistry.com/33-gutta-percha-substitute-resilon/ (accessed on 1 April 2021).
- Mohammadi, Z.; Jafarzadeh, H.; Shalavi, S.; Bhandi, S.; Kinoshita, J. Resilon: Review of a New Material for Obturation of the Canal. J. Contemp. Dent. Pract. 2015, 16, 407–414. [Google Scholar] [CrossRef]
- Barnett, F.; Trope, M. Resilon™: A novel material to replace gutta-percha. Contemp. Endod. 2004, 1, 16–19. [Google Scholar]
- Hammad, M.; Qualtrough, A.; Silikas, N. Effect of a new obturating material on vertical root fracture resistance of endodontically treated teeth. J. Endod. 2007, 33, 732–736. [Google Scholar] [CrossRef]
- Teixeira, F.B.; Teixeira, E.C.N.; Thompson, J.Y.; Leinfelder, K.F.; Trope, M. Dentinal bonding reaches the root canal system. J. Esthet. Restor. Dent. 2004, 16, 348–354. [Google Scholar] [CrossRef]
- Shipper, G.; Teixeira, F.B.; Arnold, R.R.; Trope, M. Periapical inflammation after coronal microbial inoculation of dog roots filled with gutta-percha or resilon. J. Endod. 2005, 31, 91–96. [Google Scholar] [CrossRef]
- Shrestha, D.; Wei, X.; Wu, W.-C.; Ling, J.-Q. Resilon: A methacrylate resin-based obturation system. J. Dent. Sci. 2010, 5, 47–52. [Google Scholar] [CrossRef] [Green Version]
- Resende, L.M.; Rached-Junior, F.J.; Versiani, M.A.; Souza-Gabriel, A.E.; Miranda, C.E.; Silva-Sousa, Y.T.; Sousa Neto, M.D. A comparative study of physicochemical properties of AH Plus, Epiphany, and Epiphany SE root canal sealers. Int. Endod. J. 2009, 42, 785–793. [Google Scholar] [CrossRef]
- Rocha, A.W.; de Andrade, C.D.; Leitune, V.C.; Collares, F.M.; Samuel, S.M.; Grecca, F.S.; de Figueiredo, J.A.; dos Santos, R.B. Influence of endodontic irrigants on resin sealer bond strength to radicular dentin. Bull. Tokyo Dent. Coll. 2012, 53, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Strange, K.A.; Tawil, P.Z.; Phillips, C.; Walia, H.D.; Fouad, A.F. Long-term Outcomes of Endodontic Treatment Performed with Resilon/Epiphany. J. Endod. 2019, 45, 507–512. [Google Scholar] [CrossRef]
- Nair, S.S.; Patil, A.H.; Jain, A.K.; Mali, S.D.; Yadav, P.A.; Agrawal, S.S. Fundamental concept of monoblock in endodontics. Int. J. Adv. Res. 2021, 9, 539–546. [Google Scholar] [CrossRef]
- Andreasen, J.O.; Farik, B.; Munksgaard, E.C. Long-term calcium hydroxide as a root canal dressing may increase risk of root fracture. Dent. Traumatol. 2002, 18, 134–137. [Google Scholar] [CrossRef]
- Aptekar, A.; Ginnan, K. Comparative analysis of microleakage and seal for 2 obturation materials: Resilon/ Epiphany and gutta-percha. J. Can. Dent. Assoc. 2006, 72, 245. [Google Scholar]
- Benkel, B.H.; Rising, D.W.; Goldman, L.B.; Rosen, H.; Goldman, M.; Kronman, J.H. Use of a hydrophilic plastic as a root canal filling material. J. Endod. 1976, 2, 196–202. [Google Scholar] [CrossRef]
- Tay, F.R.; Pashley, D. Monoblocks in Root Canals: A Hypothetical or a Tangible Goal. J. Endod. 2007, 33, 391–398. [Google Scholar] [CrossRef] [Green Version]
- Gillespie, W.T.; Loushine, R.J.; Weller, R.N.; Mazzoni, A.; Doyle, M.D.; Waller, J.L.; Pashley, D.H.; Tay, F.R. Improving the performance of EndoREZ root canal sealer with a dual-cured two-step self-etch adhesive. II. Apical and coronal seal. J. Endod. 2006, 32, 771–775. [Google Scholar] [CrossRef]
- Koch, K.; Min, P.S.; Stewart, G.G. Comparison of apical leakage between Ketac Endo sealer and Grossman sealer. Oral Surg. Oral Med. Oral Pathol. 1994, 78, 784–787. [Google Scholar] [CrossRef] [PubMed]
- Koch, K.; Brave, D. A new endodontic obturation technique. Dent. Today 2006, 25, 102, 104–107. [Google Scholar] [PubMed]
- Lee, K.W.; Williams, M.C.; Camps, J.J.; Pashley, D.H. Adhesion of endodontic sealers to dentin and gutta-percha. J. Endod. 2002, 28, 684–688. [Google Scholar] [CrossRef] [PubMed]
- Li, L.L.; Wang, Z.Y.; Bai, Z.C.; Mao, Y.; Gao, B.; Xin, H.T.; Zhou, B.; Zhang, Y.; Liu, B. Three-dimensional finite element analysis of weakened roots restored with different cements in combination with titanium alloy posts. Chin. Med. J. 2006, 119, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Feilzer, A.J.; de Gee, A.J.; Davidson, C.L. Setting stress in composite resin in relation to configuration of the restoration. J. Dent. Res. 1987, 66, 1636–1639. [Google Scholar] [CrossRef]
- Nakashima, M.; Akamine, A. The application of tissue engineering to regeneration of pulp and dentin in endodontics. J. Endod. 2005, 31, 711–718. [Google Scholar] [CrossRef] [Green Version]
- Lertchirakarn, V.; Timyam, A.; Messer, H.H. Effects of root canal sealers on vertical root fracture resistance of endodontically treated teeth. J. Endod. 2002, 28, 217–219. [Google Scholar] [CrossRef]
- Lertchirakarn, V.; Palamara, J.E.; Messer, H.H. Finite element analysis and strain-gauge studies of vertical root fracture. J. Endod. 2003, 29, 529–534. [Google Scholar] [CrossRef]
- Lang, H.; Korkmaz, Y.; Schneider, K.; Raab, W.H. Impact of endodontic treatments on the rigidity of the root. J. Dent. Res. 2006, 85, 364–368. [Google Scholar] [CrossRef]
- Teixeira, F.B. Ideal obturation using synthetic root-filling systems: Coronal sealing and fracture resistance. Pract. Proced. Aesthet. Dent. 2006, 18, S7–S11. [Google Scholar]
- Williams, C.; Loushine, R.J.; Weller, R.N.; Pashley, D.H.; Tay, F.R. A comparison of cohesive strength and stiffness of Resilon and gutta-percha. J. Endod. 2006, 32, 553–555. [Google Scholar] [CrossRef]
- Watanabe, T.; Miyazaki, M.; Inage, H.; Kurokawa, H. Determination of elastic modulus of the components at dentin-resin interface using the ultrasonic device. Dent. Mater. J. 2004, 23, 361–367. [Google Scholar] [CrossRef] [Green Version]
- Wu, M.K.; van der Sluis, L.W.; Wesselink, P.R. Comparison of mandibular premolars and canines with respect to their resistance to vertical root fracture. J. Dent. 2004, 32, 265–268. [Google Scholar] [CrossRef]
- Pawińska, M.; Kierklo, A.; Tokajuk, G.; Sidun, J. New endodontic obturation systems and their interfacial bond strength with intraradicular dentine-ex vivo studies. Adv. Med. Sci. 2011, 56, 327–333. [Google Scholar] [CrossRef]
- Kqiku, L.; Miletic, I.; Gruber, H.J.; Anic, I.; Städtler, P. Dichtigkeit von Wurzelkanalfüllungen mit GuttaFlow und Resilon im Vergleich zur lateralen Kondensation. Wien Med. Wochenschr. 2010, 160, 230–234. [Google Scholar] [CrossRef]
- Shokouhinejad, N.; Sabeti, M.A.; Hasheminasab, M.; Shafiei, F.; Shamshiri, A.R. Push-out bond strength of Resilon/Epiphany self-etch to intraradicular dentin after retreatment: A preliminary study. J. Endod. 2010, 36, 493–496. [Google Scholar] [CrossRef]
- De-Deus, G.; Namen, F.; Galan, J., Jr.; Zehnder, M. Soft chelating irrigation protocol optimizes bonding quality of Resilon/Epiphany root fillings. J. Endod. 2008, 34, 703–705. [Google Scholar] [CrossRef]
- Shin, S.J.; Jee, S.W.; Song, J.S.; Jung, I.Y.; Cha, J.H.; Kim, E. Comparison of regrowth of Enterococcus faecalis in dentinal tubules after sealing with gutta-percha or Resilon. J. Endod. 2008, 34, 445–448. [Google Scholar] [CrossRef]
- Paqué, F.; Sirtes, G. Apical sealing ability of Resilon/Epiphany versus gutta-percha/AH Plus: Immediate and 16 month leakage. Int. Endod. J. 2007, 40, 722–729. [Google Scholar] [CrossRef]
- Silveira, F.F.; Soares, J.A.; Nunes, E.; Mordente, V.L. Negative influence of continuous wave technique on apical sealing of the root canal system with Resilon. J. Oral Sci. 2007, 49, 121–128. [Google Scholar] [CrossRef] [Green Version]
- Kocak, M.M.; Er, O.; Saglam, B.C.; Yaman, S. Apical leakage of epiphany root canal sealer combined with different master cones. Eur. J. Dent. 2008, 2, 91–95. [Google Scholar] [CrossRef] [Green Version]
- Bodrumlu, E.; Tunga, U. The apical sealing ability of a new root canal filling material. Am. J. Dent. 2007, 20, 295–298. [Google Scholar]
- Bodrumlu, E.; Tunga, U. Coronal sealing ability of a new root canal filling material. J. Can. Dent. Assoc. 2007, 73, 623. [Google Scholar]
- Bodrumlu, E.; Tunga, U. Apical leakage of Resilon obturation material. J. Contemp. Dent. Pract. 2006, 7, 45–52. [Google Scholar] [CrossRef]
- Verissimo, D.M.; do Vale, M.S.; Monteiro, A.J. Comparison of apical leakage between canals filled with gutta-percha/AH-plus and Resilon/Epiphany System, when submitted to two filling techniques. J. Endod. 2007, 33, 291–294. [Google Scholar] [CrossRef]
- Moura-Netto, C.; Pinto, T.; Davidowicz, H.; de Moura, A.A.M. Apical leakage of three resin-based endodontic sealers after 810-nm-diode laser irradiation. Photomed. Laser Surg. 2009, 27, 891–894. [Google Scholar] [CrossRef]
- Wedding, J.R.; Brown, C.E.; Legan, J.J.; Moore, B.K.; Vail, M.M. An in vitro comparison of micro leakage between Resilon and gutta-percha with a fluid filtration model. J. Endod. 2007, 33, 1447–1449. [Google Scholar] [CrossRef]
- Ishimura, H.; Yoshioka, T.; Suda, H. Sealing ability of new adhesive root canal filling materials measured by new dye penetration method. Dent. Mater. J. 2007, 26, 290–295. [Google Scholar] [CrossRef] [Green Version]
- Nawal, R.R.; Parande, M.; Sehgal, R.; Rao, N.R.; Naik, A. A comparative evaluation of 3 root canal filling systems. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2011, 111, 387–393. [Google Scholar] [CrossRef]
- Punia, S.K.; Nadig, P.; Punia, V. An in vitro assessment of apical microleakage in root canals obturated with guttaflow, Resilon, thermafil and lateral condensation: A stereomicroscopic study. J. Conserv. Dent. 2011, 14, 173–177. [Google Scholar] [CrossRef] [Green Version]
- Tunga, U.; Bodrumlu, E. Assessment of the sealing ability of a new root canal obturation material. J. Endod. 2006, 32, 876–878. [Google Scholar] [CrossRef] [PubMed]
- Shashidhar, C.; Shivanna, V.; Shivamurthy, G.; Shashidhar, J. The comparison of microbial leakage in roots filled with resilon and gutta-percha: An in vitro study. J. Conserv. Dent. 2011, 14, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Sagsen, B.; Er, O.; Kahraman, Y.; Orucoglu, H. Evaluation of micro leakage of roots filled with different techniques with a computerized fluid filtration technique. J. Endod. 2006, 32, 1168–1170. [Google Scholar] [CrossRef] [PubMed]
- Kqiku, L.; Städtler, P.; Gruber, H.J.; Baraba, A.; Anic, I.; Miletic, I. Active versus passive microleakage of Resilon/Epiphany and gutta-percha/AH Plus. Aust. Endod. J. 2011, 37, 141–146. [Google Scholar] [CrossRef] [PubMed]
- Stratton, R.K.; Apicella, M.J.; Mines, P. A fluid filtration comparison of gutta-percha versus Resilon, a new soft resin endodontic obturation system. J. Endod. 2006, 32, 642–645. [Google Scholar] [CrossRef] [PubMed]
- Kurtzman, G.M. Resilon Update. Inside Dent. 2007, 3, 1–5. [Google Scholar]
- Hanada, T.; Quevedo, C.G.; Okitsu, M.; Yoshioka, T.; Iwasaki, N.; Takahashi, H.; Suda, H. Effects of new adhesive resin root canal filling materials on vertical root fractures. Aust. Endod. J. 2010, 36, 19–23. [Google Scholar] [CrossRef]
- Ulusoy, Ö.İ.A.; Nayır, Y.; Darendeliler-Yaman, S. Effect of different root canal sealers on fracture strength of simulated immature roots. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2011, 112, 544–547. [Google Scholar] [CrossRef]
- Susini, G.; About, I.; Tran-Hung, L.; Camps, J. Cytotoxicity of Epiphany and Resilon with a root model. Int. Endod. J. 2006, 39, 940–944. [Google Scholar] [CrossRef]
- Leonardo, M.R.; Barnett, F.; Debelian, G.J.; de Pontes Lima, R.K.; da Silva, L.A.B. Root canal adhesive filling in dogs’ teeth with or without coronal restoration: A histopathological evaluation. J. Endod. 2007, 33, 1299–1303. [Google Scholar] [CrossRef]
- Bodrumlu, E.; Uzun, O.; Topuz, O.; Semiz, M. Efficacy of three techniques in removing root canal filling material. J. Can. Dent. Assoc. 2008, 74, 721. [Google Scholar]
- Ezzie, E.; Fleury, A.; Solomon, E.; Spears, R.; He, J. Efficacy of retreatment techniques for a resin based root canal obturation material. J. Endod. 2006, 32, 341–344. [Google Scholar] [CrossRef]
- Ring, J.; Murray, P.E.; Namerow, K.N.; Moldauer, B.I.; Garcia-Godoy, F. Removing root canal obturation materials: A comparison of rotary file systems and re-treatment agents. J. Am. Dent. Assoc. 2009, 140, 680–688. [Google Scholar] [CrossRef]
- De Oliveira, D.P.; Barbizam, J.V.; Trope, M.; Teixeira, F.B. Comparison between gutta-percha and Resilon removal using two different techniques in endodontic retreatment. J. Endod. 2006, 32, 362–364. [Google Scholar] [CrossRef]
- Cunha, R.S.; De Martin, A.S.; Barros, P.P.; da Silva, F.M.; de Castilho Jacinto, R.; da Silveira Bueno, C.E. In vitro evaluation of the cleansing working time and analysis of the amount of gutta-percha or Resilon remnants in the root canal walls after instrumentation for endodontic retreatment. J. Endod. 2007, 33, 1426–1428. [Google Scholar] [CrossRef]
- Azar, M.; Khojastehpour, L.; Iranpour, N. A comparison of the effectiveness of chloroform in dissolving Resilon and gutta-percha. J. Dent. 2011, 8, 19–24. [Google Scholar]
- Üreyen Kaya, B.; Keçeci, A.D.; Orhan, H.; Belli, S. Micropush-out bond strengths of gutta-percha versus thermoplastic synthetic polymer-based systems—an ex vivo study. Int. Endod. J. 2008, 41, 211–218. [Google Scholar] [CrossRef]
- Fisher, M.A.; Berzins, D.W.; Bahcall, J.K. An in vitro comparison of bond strength of various obturation materials to root canal dentin using a push-out test design. J. Endod. 2007, 33, 856–858. [Google Scholar] [CrossRef]
- Sly, M.M.; Moore, B.K.; Platt, J.A.; Brown, C.E. Push-out bond strength of a new endodontic obturation system (Resilon/Epiphany). J. Endod. 2007, 33, 160–162. [Google Scholar] [CrossRef]
- Jack, R.M.; Goodell, G.G. In vitro comparison of coronal microleakage between Resilon alone and gutta-percha with a glass ionomer intraorifice barrier using a fluid filtration model. J. Endod. 2008, 34, 718–720. [Google Scholar] [CrossRef]
- Santos, J.; Tjäderhane, L.; Ferraz, C.; Zaia, A.; Alves, M.; De Goes, M.; Carrilho, M. Long-term sealing ability of resin-based root canal fillings. Int. Endod. J. 2010, 43, 455–460. [Google Scholar] [CrossRef]
- Shemesh, H.; Wu, M.K.; Wesselink, P.R. Leakage along the apical root fillings with and without smear layer using two different leakage models: A two month longitudinal ex vivo study. Int. Endod. J. 2006, 39, 968–976. [Google Scholar] [CrossRef]
- De Bruyne, M.A.; De Moor, R.J. Long-term sealing ability of Resilon apical root-end fillings. Int. Endod. J. 2009, 42, 884–892. [Google Scholar] [CrossRef]
- Deus, G.A.D.; Fábio, M.; Rocha, L.A.C.M.; Gurgel-Filho, E.D.; Maniglia, C.F.; Coutinho-Filho, T. Analysis of the film thickness of a root canal sealer following three obturation techniques. Pesqui Odontol. Bras. 2003, 17, 119–125. [Google Scholar] [CrossRef] [Green Version]
- Pasqualini, D.; Scotti, N.; Mollo, L.; Berutti, E.; Angelini, E.; Migliaretti, G.; Cuffini, A.; Adlerstein, D. Microbial leakage of Gutta-Percha and Resilon root canal filling material: A comparative study using a new homogeneous assay for sequence detection. J. Biomater. Appl. 2008, 22, 337–352. [Google Scholar] [CrossRef] [Green Version]
- Shemesh, H.; Souza, E.M.; Wu, M.K.; Wesselink, P.R. Glucose reactivity with filling materials as a limitation for using the glucose leakage model. Int. Endod. J. 2008, 41, 869–872. [Google Scholar] [CrossRef]
- Kokorikos, I.; Kolokouris, I.; Economides, N.; Gogos, C.; Helvatjoglu-Antoniades, M. Long-term evaluation of the sealing ability of two root canal sealers in combination with self-etching bonding agents. J. Adhes. Dent. 2009, 11, 239–246. [Google Scholar]
- Onay, E.O.; Ungor, M.; Orucoglu, H. An in vitro evaluation of the apical sealing ability of a new resin based root canal obturation system. J. Endod. 2006, 32, 976–978. [Google Scholar] [CrossRef]
- Hirai, V.H.; da Silva Neto, U.X.; Westphalen, V.P.D.; Perin, C.P.; Carneiro, E.; Fariniuk, L.F. Comparative analysis of leakage in root canal filling performed with gutta-percha and Resilon cones with AH Plus and Epiphany sealers. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 109, 131–135. [Google Scholar] [CrossRef]
- Saleh, I.M.; Ruyter, I.E.; Haapasalo, M.; Ørstavik, D. Bacterial penetration along different root canal filling materials in the presence or absence of smear layer. Int. Endod. J. 2008, 41, 32–40. [Google Scholar] [CrossRef]
- De-Deus, G.; Namen, F.; Galan, J. Reduced long-term sealing ability of adhesive root fillings after water-storage stress. J. Endod. 2008, 34, 322–325. [Google Scholar] [CrossRef] [PubMed]
- Pandey, P.; Aggarwal, H.; Tikku, A.P.; Singh, A.; Bains, R.; Mishra, S. Comparative evaluation of sealing ability of gutta percha and resilon as root canal filling materials—A systematic review. J. Oral Biol. Craniofac. Res. 2020, 10, 220–226. [Google Scholar] [CrossRef] [PubMed]
- Barborka, B.J.; Woodmansey, K.F.; Glickman, G.N.; Schneiderman, E.; He, J. Long-term Clinical Outcome of Teeth Obturated with Resilon. J. Endod. 2017, 43, 556–560. [Google Scholar] [CrossRef] [PubMed]
- Karapınar-Kazandağ, M.; Tanalp, J.; Bayrak, Ö.F.; Sunay, H.; Bayirh, G. Microleakage of various root filling systems by glucose filtration analysis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 109, e96–e102. [Google Scholar] [CrossRef]
- Sharifian, M.R.; Shokouhinejad, N.; Aligholi, M.; Jafari, Z. Effect of chlorhexidine on coronal microleakage from root canals obturated with Resilon/Epiphany Self-Etch. J. Oral Sci. 2010, 52, 83–87. [Google Scholar] [CrossRef] [Green Version]
- Shashidhar, J.; Shashidhar, C. Gutta percha verses resilon: An in vitro comparison of fracture resistance in endodontically treated teeth. J. Indian Soc. Pedod. Prev. Dent. 2014, 32, 53–57. [Google Scholar] [CrossRef]
- Baba, S.M.; Grover, S.I.; Tyagi, V. Fracture resistance of teeth obturated with gutta percha and Resilon: An in vitro study. J. Conserv. Dent. 2010, 13, 61–64. [Google Scholar] [CrossRef] [Green Version]
- De Temiño Morante, P.R. ¿Es el Resilon el Nuevo Material de Obturación Endodóntica? Available online: https://gacetadental.com/wp-content/uploads/OLD/pdf/166_CIENCIA_Resilon_obturacion_endodontica.pdf (accessed on 15 May 2021).
- Economides, N.; Koulaouzidou, E.A.; Gogos, C.; Kolokouris, I.; Beltes, P.; Antoniades, D. Comparative study of the cytotoxic effect of Resilon against two cell lines. Braz. Dent. J. 2008, 19, 291–295. [Google Scholar] [CrossRef] [Green Version]
- Donadio, M.; Jiang, J.; He, J.; Wang, Y.H.; Safavi, K.E.; Zhu, Q. Cytotoxicity evaluation of Activ GP and Resilon sealers in vitro. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 107, e74–e78. [Google Scholar] [CrossRef]
- Zarei, M.; Shahrami, F.; Vatanpour, M. Comparison between gutta-percha and Resilon retreatment. J. Oral Sci. 2009, 51, 181–185. [Google Scholar] [CrossRef] [Green Version]
- Somma, F.; Cammarota, G.; Plotino, G.; Grande, N.M.; Pameijer, C.H. The effectiveness of manual and mechanical instrumentation for the retreatment of three different root canal filling materials. J. Endod. 2008, 34, 466–469. [Google Scholar] [CrossRef]
- Taşdemir, T.; Yildirim, T.; Celik, D. Comparative study of removal of current endodontic fillings. J. Endod. 2008, 34, 326–329. [Google Scholar] [CrossRef]
- Iizuka, N.; Takenaka, S.; Shigetani, Y.; Okiji, T. Removal of resin-based root canal filling materials with K3 rotary instruments: Relative efficacy for different combinations of filling materials. Dent. Mater. J. 2008, 27, 75–80. [Google Scholar] [CrossRef] [Green Version]
- Hassanloo, A.; Watson, P.; Finer, Y.; Friedman, S. Retreatment efficacy of the Epiphany soft resin obturation system. Int. Endod. J. 2007, 40, 633–643. [Google Scholar] [CrossRef]
- Tanomaru-Filho, M.; Orlando, T.A.; Bortoluzzi, E.A.; Silva, G.F.; Tanomaru, J.M. Solvent capacity of different substances on gutta-percha and Resilon. Braz. Dent. J. 2010, 21, 46–49. [Google Scholar] [CrossRef] [Green Version]
- Faria-Júnior, N.B.; Loiola, L.E.; Guerreiro-Tanomaru, J.M.; Berbert, F.L.; Tanomaru-Filho, M. Effectiveness of three solvents and two associations of solvents on gutta-percha and Resilon. Braz. Dent. J. 2011, 22, 41–44. [Google Scholar] [CrossRef] [Green Version]
- Dumani, A.; Yoldas, O.; Isci, A.S.; Köksal, F.; Kayar, B.; Polat, E. Disinfection of artificially contaminated Resilon cones with chlorhexidine and sodium hypochlorite at different time exposures. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 103, e82–e85. [Google Scholar] [CrossRef]
- Shokouhinejad, N.; Sharifian, M.R.; Jafari, M.; Sabeti, M.A. Push-out bond strength of Resilon/Epiphany self-etch and gutta-percha/AH26 after different irrigation protocols. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 110, e88–e92. [Google Scholar] [CrossRef]
- Kumar, N.; Aggarwal, V.; Singla, M.; Gupta, R. Effect of various endodontic solutions on punch out strength of Resilon under cyclic loading. J. Conserv. Dent. 2011, 14, 366–369. [Google Scholar] [CrossRef] [Green Version]
- Tay, F.R.; Loushine, R.J.; Weller, R.N.; Kimbrough, W.F.; Pashley, D.H.; Mak, Y.F.; Lai, C.N.; Raina, R.; Williams, M.C. Ultrastructural evaluation of the apical seal in roots filled with a polycaprolactone-based root canal filling material. J. Endod. 2005, 31, 514–519. [Google Scholar] [CrossRef]
- Lyons, W.W.; Hartwell, G.R.; Stewart, J.T.; Reavley, B.; Appelstein, C.; Lafkowitz, S. Comparison of coronal bacterial leakage between immediate versus delayed post-space preparations in root canals filled with Resilon/Epiphany. Int. Endod. J. 2009, 42, 203–207. [Google Scholar] [CrossRef]
- De-Deus, G.; Audi, C.; Murad, C.; Fidel, S.; Fidel, R.A. Sealing ability of oval-shaped canals filled using the System B heat source with either gutta-percha or Resilon: An ex vivo study using a polymicrobial leakage model. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 104, 114–119. [Google Scholar] [CrossRef]
- Baumgartner, G.; Zehnder, M.; Paqué, F. Enterococcus faecalis type strain leakage through root canals filled with Gutta-Percha/AH plus or Resilon/Epiphany. J. Endod. 2007, 33, 45–47. [Google Scholar] [CrossRef]
- Hollanda, A.C.B.; Estrela, C.R.; Decurcio, D.A.; Silva, J.A.; Estrela, C. Sealing ability of three commercial resin-based endodontic sealers. Gen. Dent. 2009, 57, 368–373. [Google Scholar]
- Raina, R.; Loushine, R.J.; Weller, R.N.; Tay, F.R.; Pashley, D.H. Evaluation of the quality of the apical seal in Resilon/ Epiphany and gutta-percha/AH Plus-filled root canals by using a fluid filtration approach. J. Endod. 2007, 33, 944–947. [Google Scholar] [CrossRef]
- Pitout, E.; Oberholzer, T.G.; Blignaut, E.; Molepo, J. Coronal leakage of teeth root-filled with gutta-percha or Resilon root canal filling material. J. Endod. 2006, 32, 610–615. [Google Scholar] [CrossRef]
- Fransen, J.N.; He, J.; Glickman, G.N.; Rios, A.; Shulman, J.D.; Honeyman, A. Comparative assessment of ActiV GP/glass ionomer sealer, Resilon/Epiphany, and gutta-percha/AH plus obturation: A bacterial leakage study. J. Endod. 2008, 34, 725–727. [Google Scholar] [CrossRef]
- Shokouhinejad, N.; Sharifian, M.R.; Aligholi, M.; Assadian, H.; Tabor, R.K.; Nekoofar, M.H. The sealing ability of Resilon and gutta-percha following different smear layer removal methods: An ex vivo study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 110, 45–49. [Google Scholar] [CrossRef]
- Kangarlou, A.; Dianat, O.; Esfahrood, Z.R.; Asharaf, H.; Zandi, B.; Eslami, G. Bacterial leakage of GuttaFlow-filled root canals compared with Resilon/Epiphany and Gutta-percha/AH26-filled root canals. Aust. Endod. J. 2012, 38, 10–13. [Google Scholar] [CrossRef]
- Biggs, S.C.; Knowles, K.I.; Ibarrola, J.L.; Pashley, D.H. An in vitro assessment of the sealing ability of Resilon/Epiphany using a fluid filtration. J. Endod. 2006, 32, 759–761. [Google Scholar] [CrossRef]
- Oddoni, P.G.; Mello, I.; Coil, J.M.; Antoniazzi, J.H. Coronal and apical leakage analysis of two different root canal obturation systems. Braz. Oral Res. 2008, 22, 211–215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Almeida-Gomes, F.; Maniglia-Ferreira, C.; de Morais Vitoriano, M.; Carvalho-Sousa, B.; Guimaraes, N.L.; dos Santos, R.A.; Gurgel-Filho, E.D.; Rocha, M.M. Ex vivo evaluation of coronal and apical microbial leakage of root canal--filled with gutta-percha or Resilon/Epiphany root canal filling material. Indian J. Dent. Res. 2010, 21, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Üreyen Kaya, B.; Keçeci, A.D.; Belli, S. Evaluation of the sealing ability of gutta-percha and thermoplastic synthetic polymer-based systems along the root canals through the glucose penetration model. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 104, E66–E73. [Google Scholar] [CrossRef] [PubMed]
- Dultra, F.; Barroso, J.M.; Carrasco, L.D.; Capelli, A.; Guerisoli, D.M.; Pécora, J.D. Evaluation of apical microleakage of teeth sealed with four different canal sealers. J. Appl. Oral Sci. 2006, 14, 341–345. [Google Scholar] [CrossRef] [Green Version]
- Muñoz, H.R.; Saravia-Lemus, G.A.; Florián, W.E.; Lainfiesta, J.F. Microbial leakage of Enterococcus faecalis after post space preparation in teeth filled in vivo with RealSeal versus gutta-percha. J. Endod. 2007, 33, 674–675. [Google Scholar] [CrossRef]
- Tanomaru-Filho, M.; Sant’anna-Junior, A.; Bosso, R.; Guerreiro-Tanomaru, J.M. Effectiveness of gutta-percha and Resilon in filling lateral root canals using the Obtura II system. Braz. Oral Res. 2011, 25, 205–209. [Google Scholar] [CrossRef]
- Hemalatha, H.; Sandeep, M.; Kulkarni, S.; Yakub, S.S. Evaluation of fracture resistance in simulated immature teeth using Resilon and Ribbond as root reinforcements—an in vitro study. Dent. Traumatol. 2009, 25, 433–438. [Google Scholar] [CrossRef]
- Sagsen, B.; Er, O.; Kahraman, Y.; Akdogan, G. Resistance to fracture of roots filled with three different techniques. Int. Endod. J. 2007, 40, 31–35. [Google Scholar] [CrossRef]
- Grande, N.M.; Plotino, G.; Lavorgna, L.; Ioppolo, P.; Bedini, R.; Pameijer, C.H.; Somma, F. Influence of different root canal-filling materials on the mechanical properties of root canal dentin. J. Endod. 2007, 33, 859–863. [Google Scholar] [CrossRef]
- Bodrumlu, E.; Muglali, M.; Sumer, M.; Guvenc, T. The response of subcutaneous connective tissue to a new endodontic filling material. J. Biomed. Mater. Res. B Appl. Biomater. 2008, 84, 463–467. [Google Scholar] [CrossRef]
- Merdad, K.; Pascon, A.E.; Kulkarni, G.; Santerre, P.; Friedman, S. Short-term cytotoxicity assessment of components of the epiphany resin-percha obturating system by indirect and direct contact millipore filter assays. J. Endod. 2007, 33, 24–27. [Google Scholar] [CrossRef]
- Onay, E.O.; Ungor, M.; Ozdemir, B.H. In vivo evaluation of the biocompatibility of a new resin-based obturation system. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 104, e60–e66. [Google Scholar] [CrossRef]
- Fenoul, G.; Meless, G.D.; Pérez, F. The efficacy of R-Endo rotary NiTi and stainless steel hand instruments to remove gutta-percha and Resilon. Int. Endod. J. 2010, 43, 135–141. [Google Scholar] [CrossRef]
- Schirrmeister, J.F.; Meyer, K.M.; Hermanns, P.; Altenburger, M.J.; Wrbas, K.T. Effectiveness of hand and rotary instrumentation for removing a new synthetic polymer-based root canal obturation material (Epiphany) during retreatment. Int. Endod. J. 2006, 39, 150–156. [Google Scholar] [CrossRef]
- Marfisi, K.; Mercade, M.; Plotino, G.; Duran-Sindreu, F.; Bueno, R.; Roig, M. Efficacy of three different rotary files to remove gutta-percha and resilon from root canals. Int. Endod. J. 2010, 43, 1022–1028. [Google Scholar] [CrossRef]
- Nagas, E.; Cehreli, Z.C.; Durmaz, V.; Vallittu, P.K.; Lassila, L.V. Regional push-out bond strength and coronal microleakage of Resilon after different light-curing methods. J. Endod. 2007, 33, 1464–1468. [Google Scholar] [CrossRef]
- Williamson, A.E.; Marker, K.L.; Drake, D.R.; Dawson, D.V.; Walton, R.E. Resin-based versus gutta-percha-based root canal obturation: Influence on bacterial leakage in an in vitro model system. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 108, 292–296. [Google Scholar] [CrossRef]
- Goldberg, F.; Artaza, L.P.; De Silvio, A. Effectiveness of different obturation techniques in the filling of simulated lateral canals. J. Endod. 2001, 27, 362–364. [Google Scholar] [CrossRef]
- Gharib, S.R.; Tordik, P.A.; Imamura, G.M.; Bagiński, T.A.; Goodell, G.G. A confocal laser scanning microscope investigation of the Epiphany obturation system. J. Endod. 2007, 33, 957–961. [Google Scholar] [CrossRef]

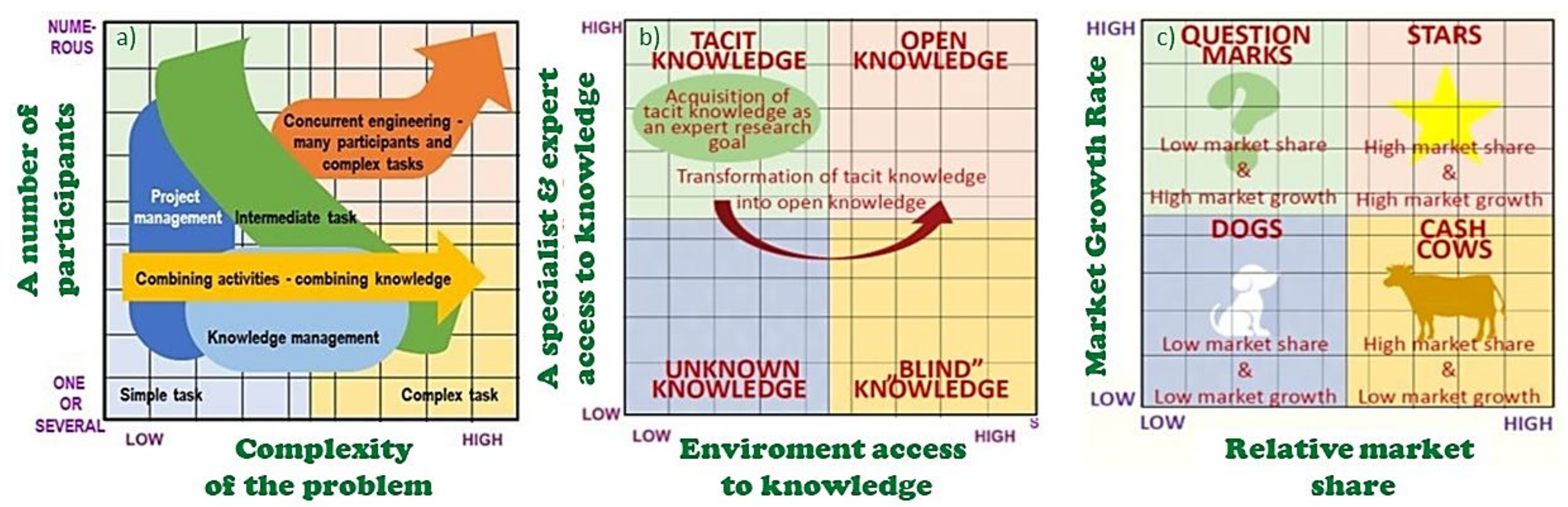
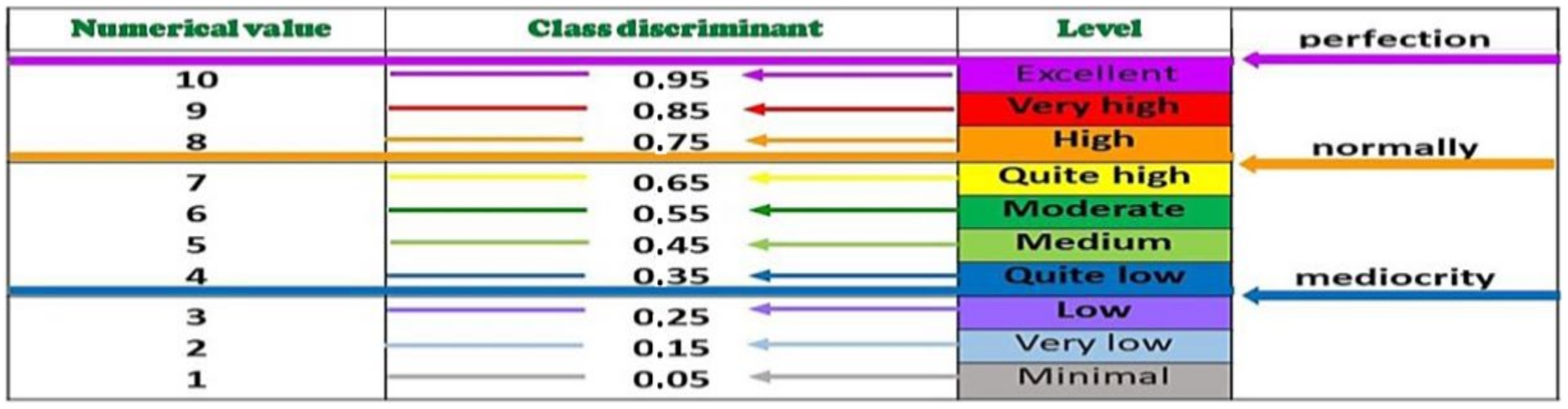
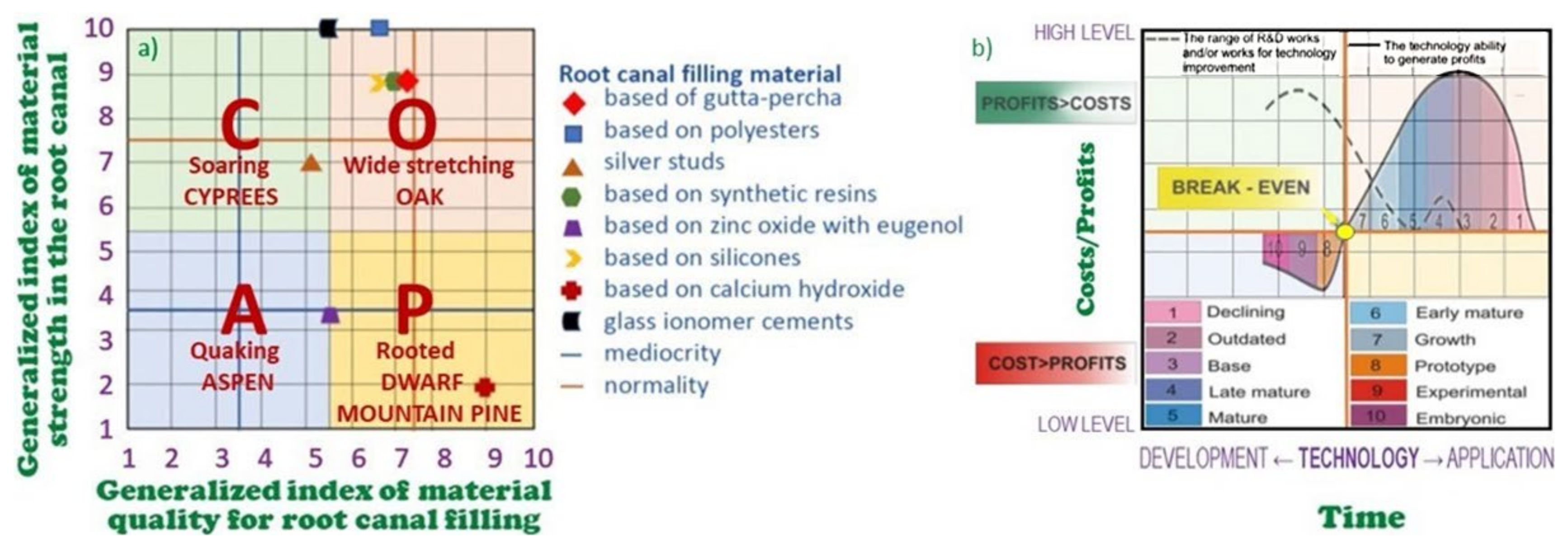
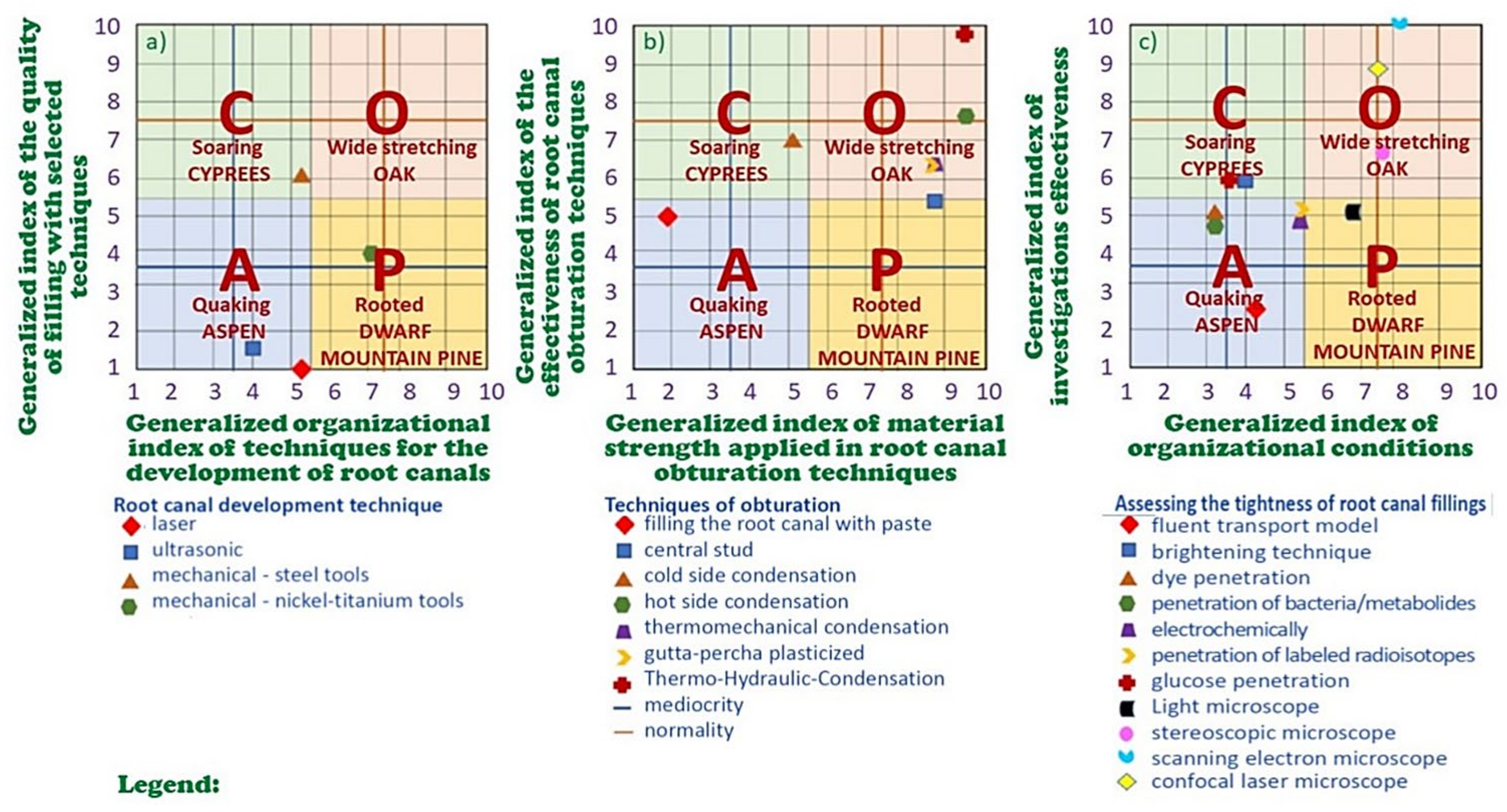
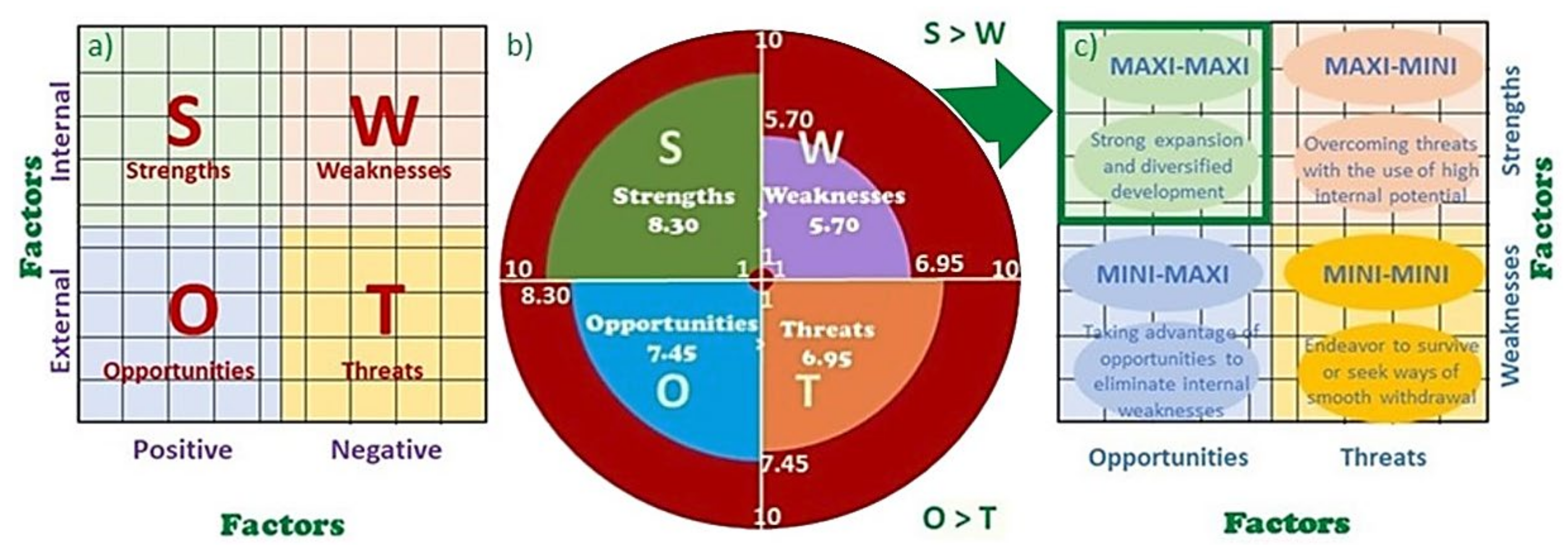
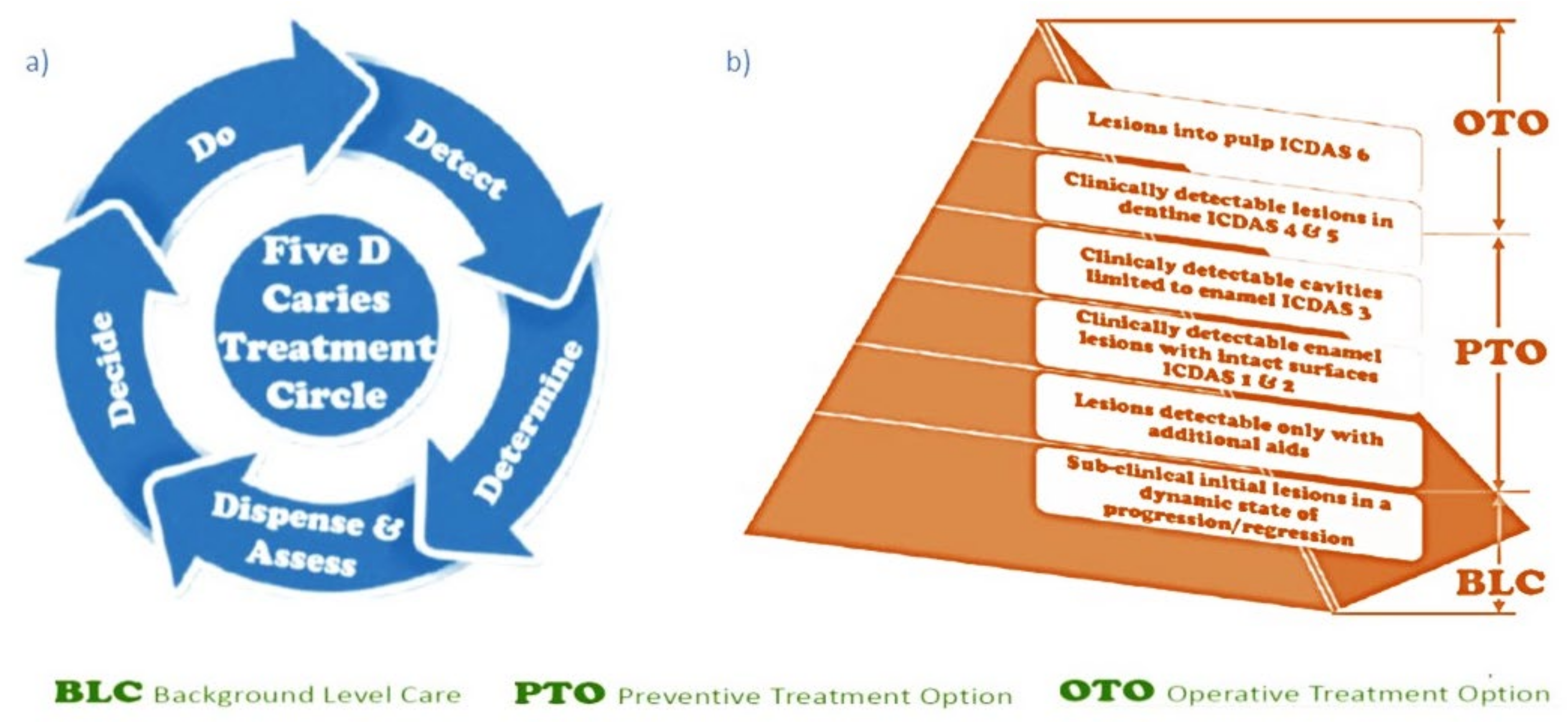
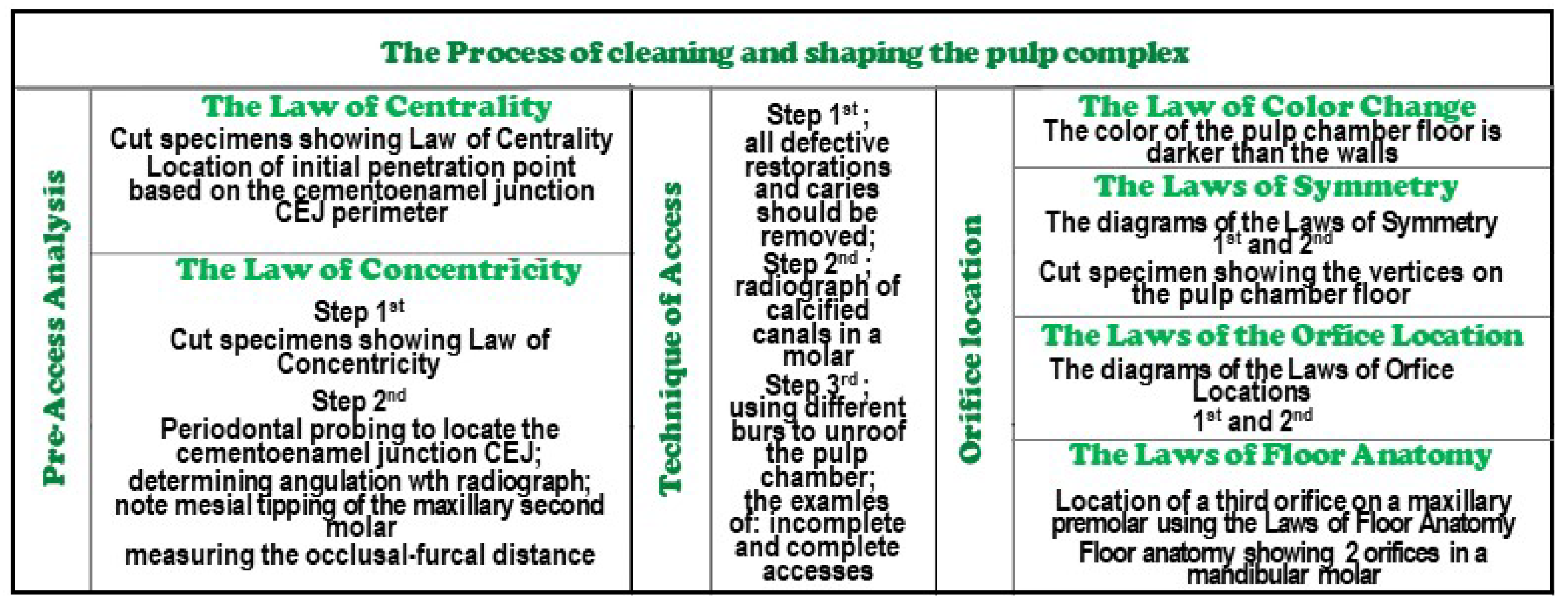
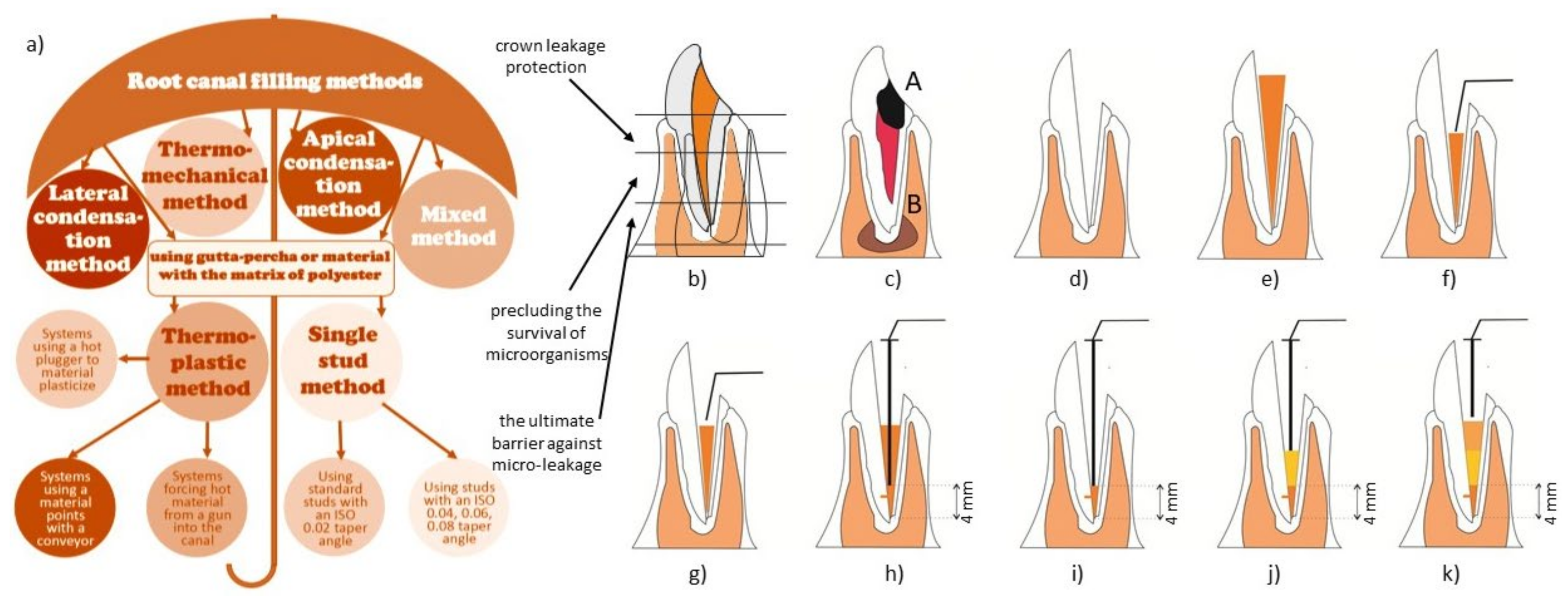


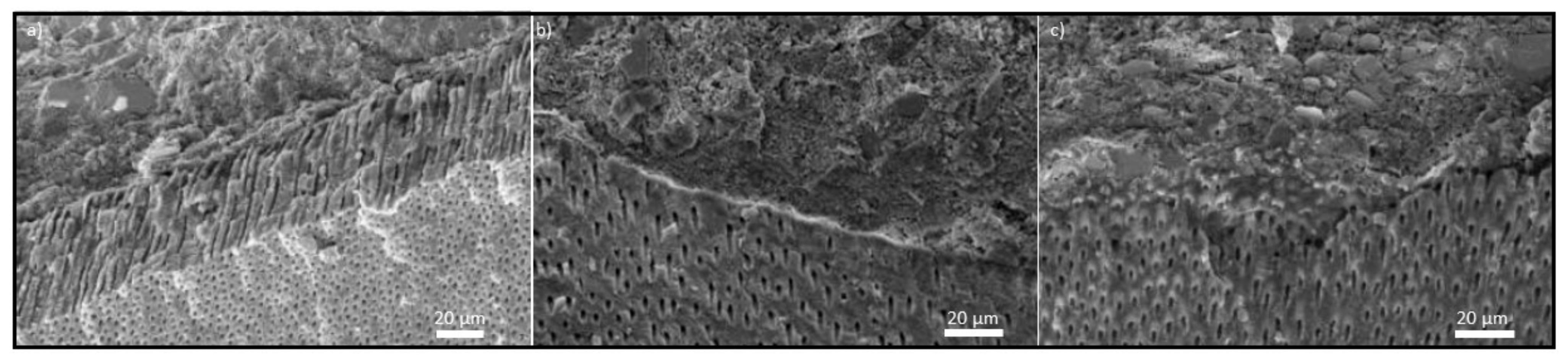

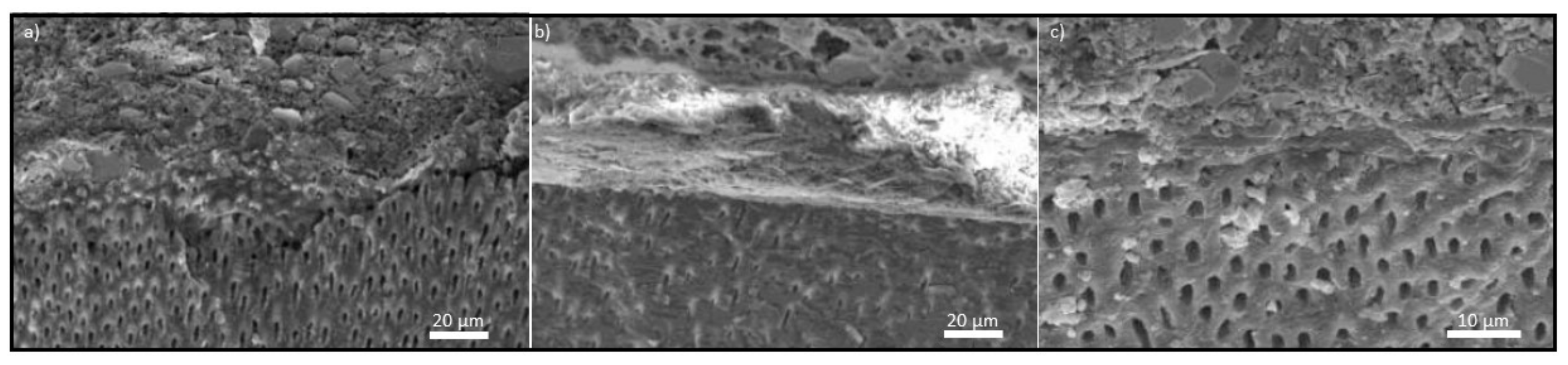

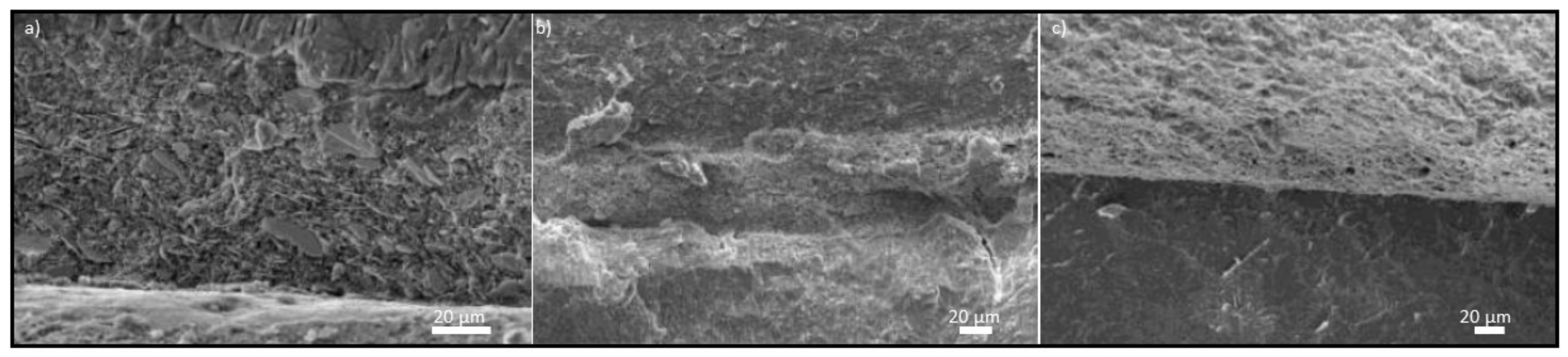
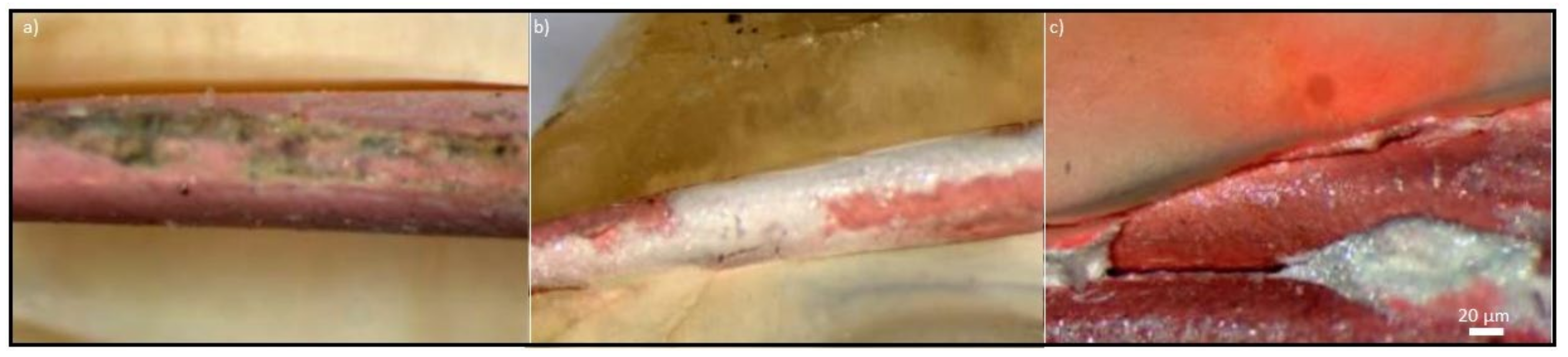
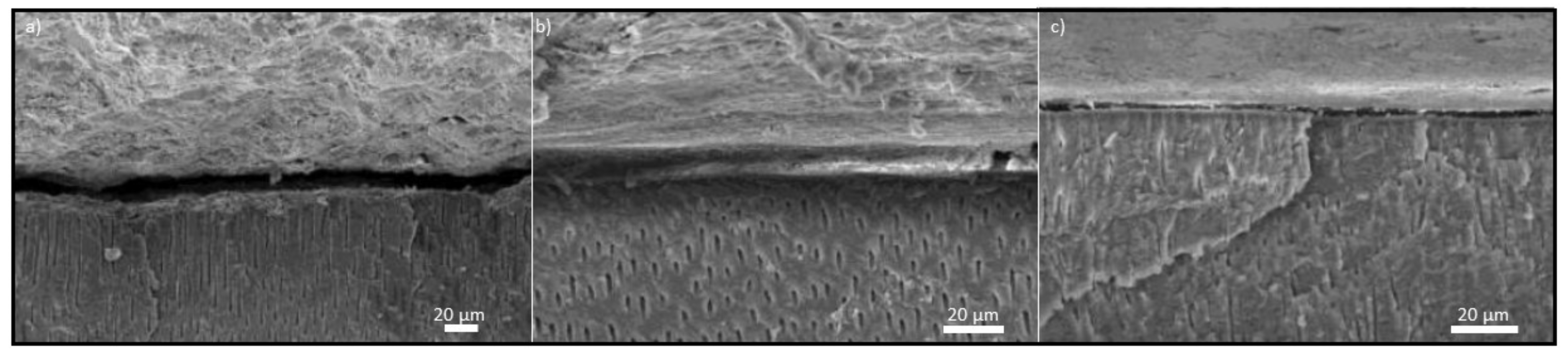
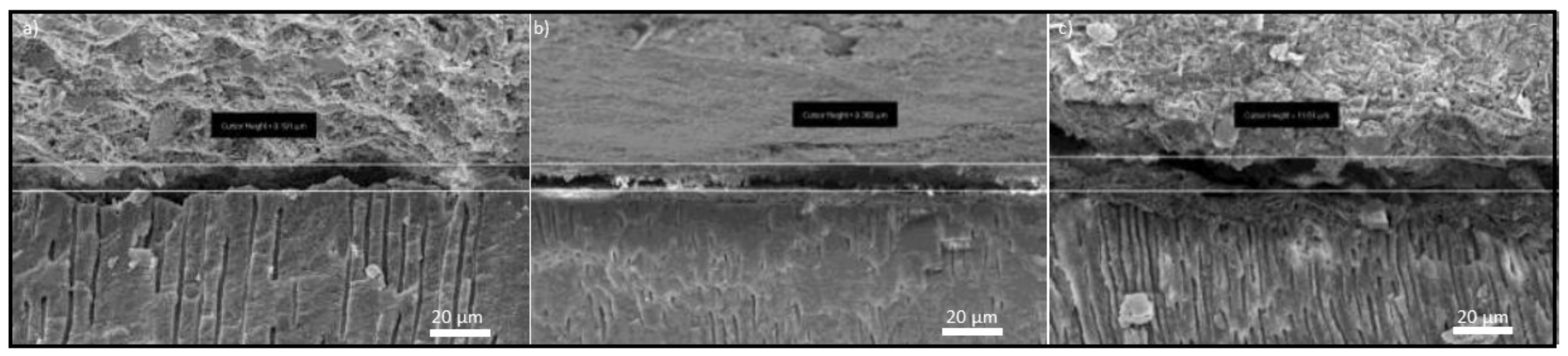
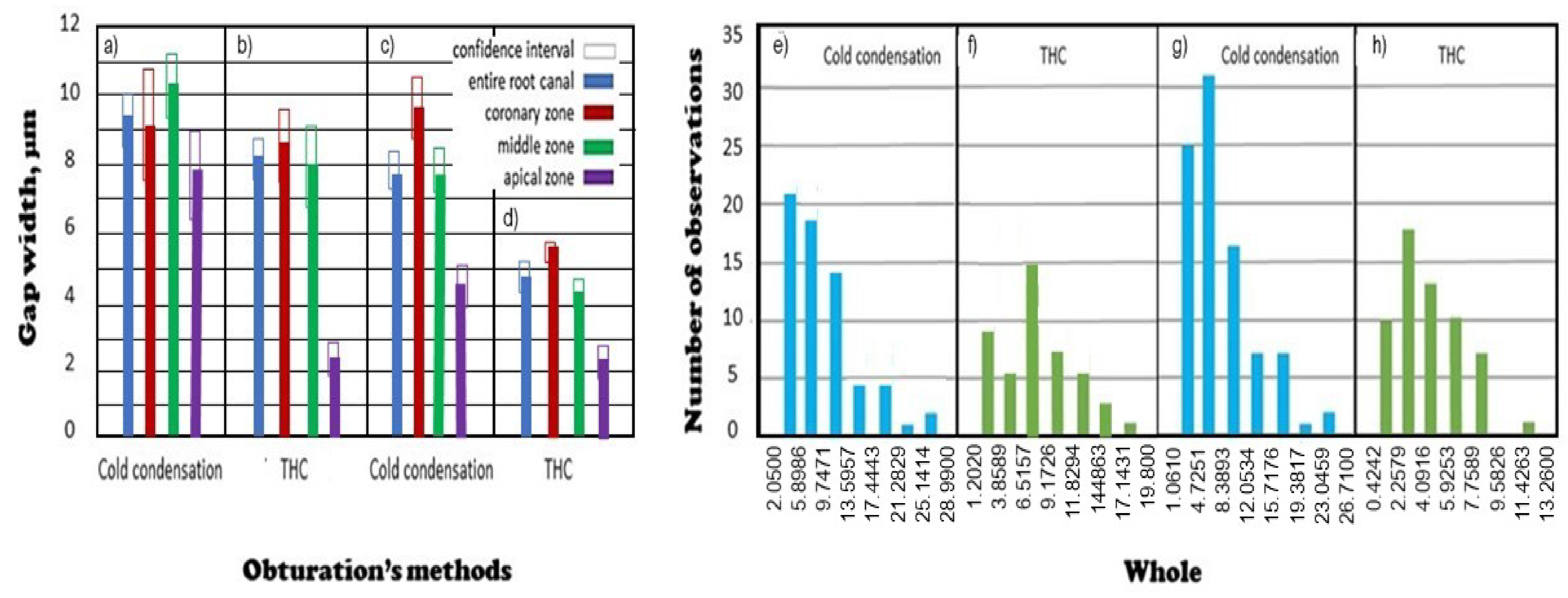
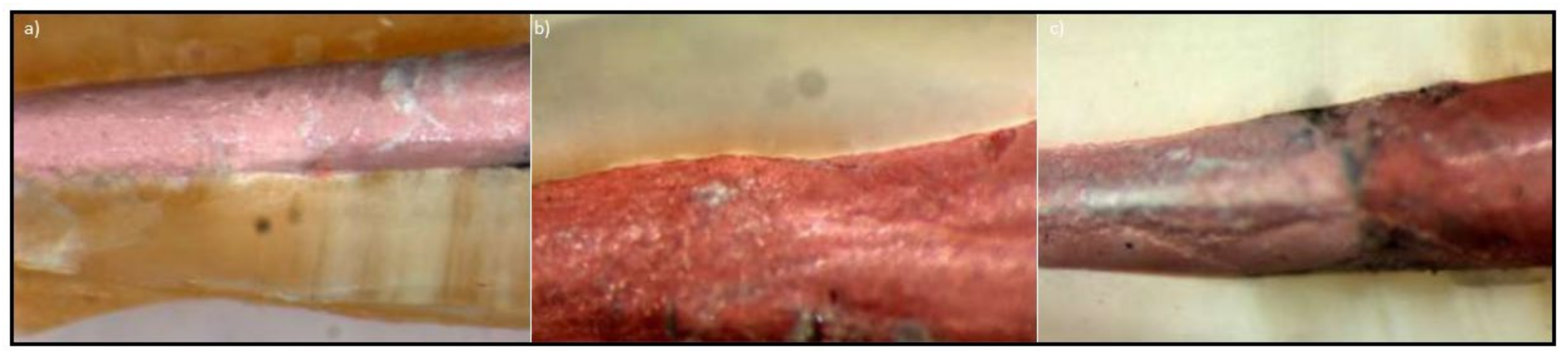
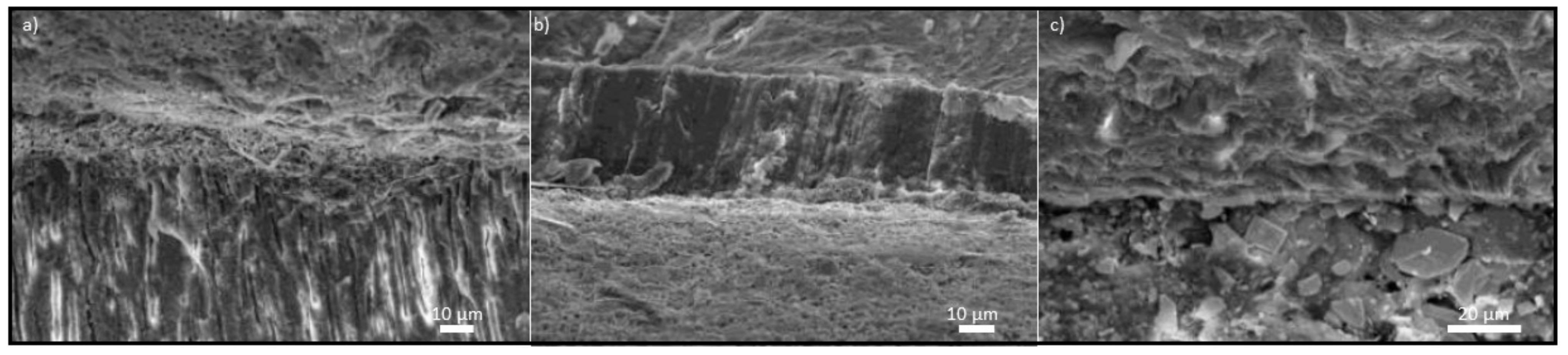

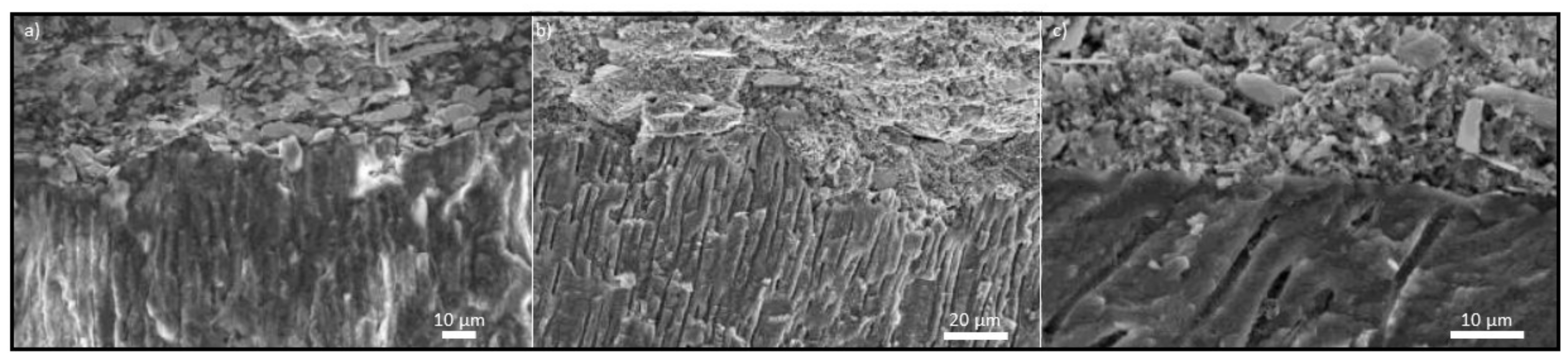
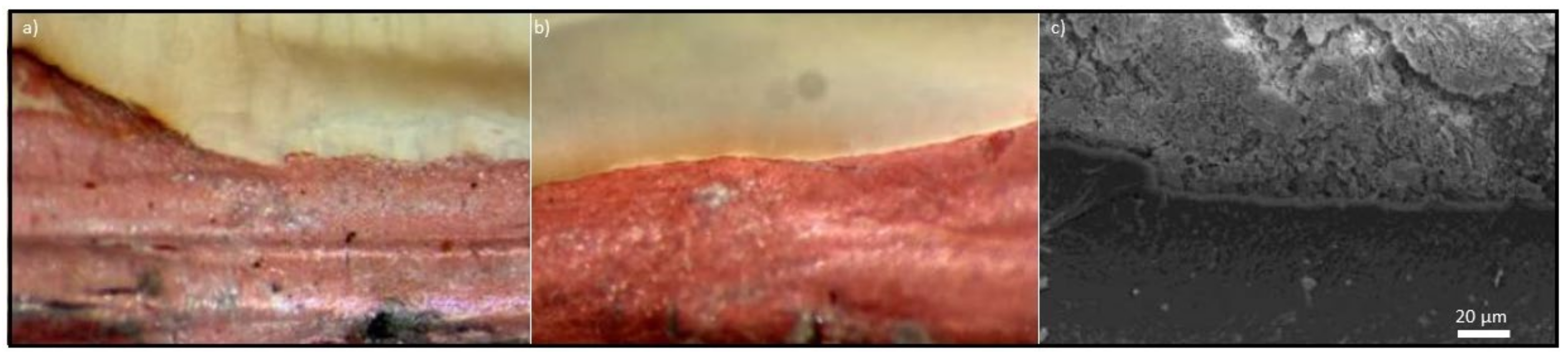

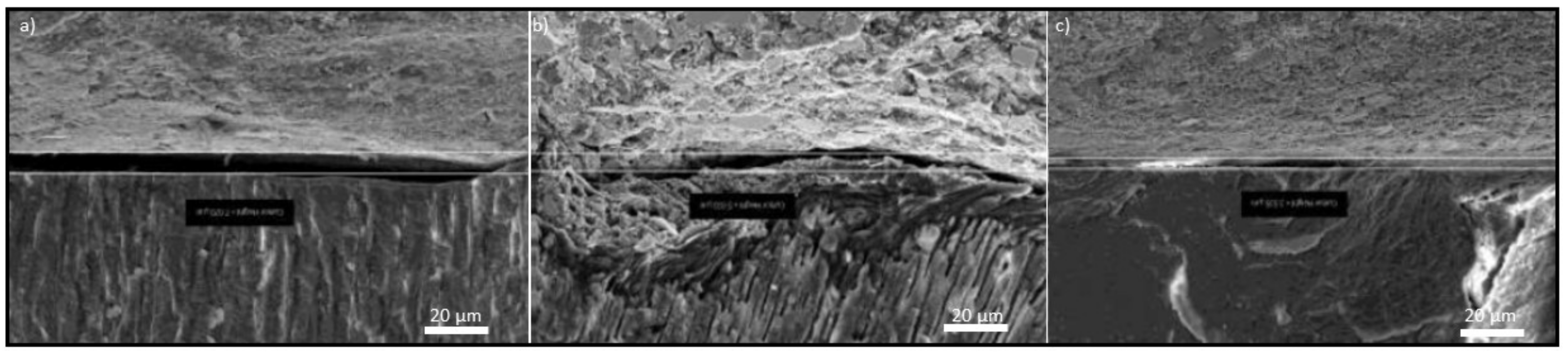
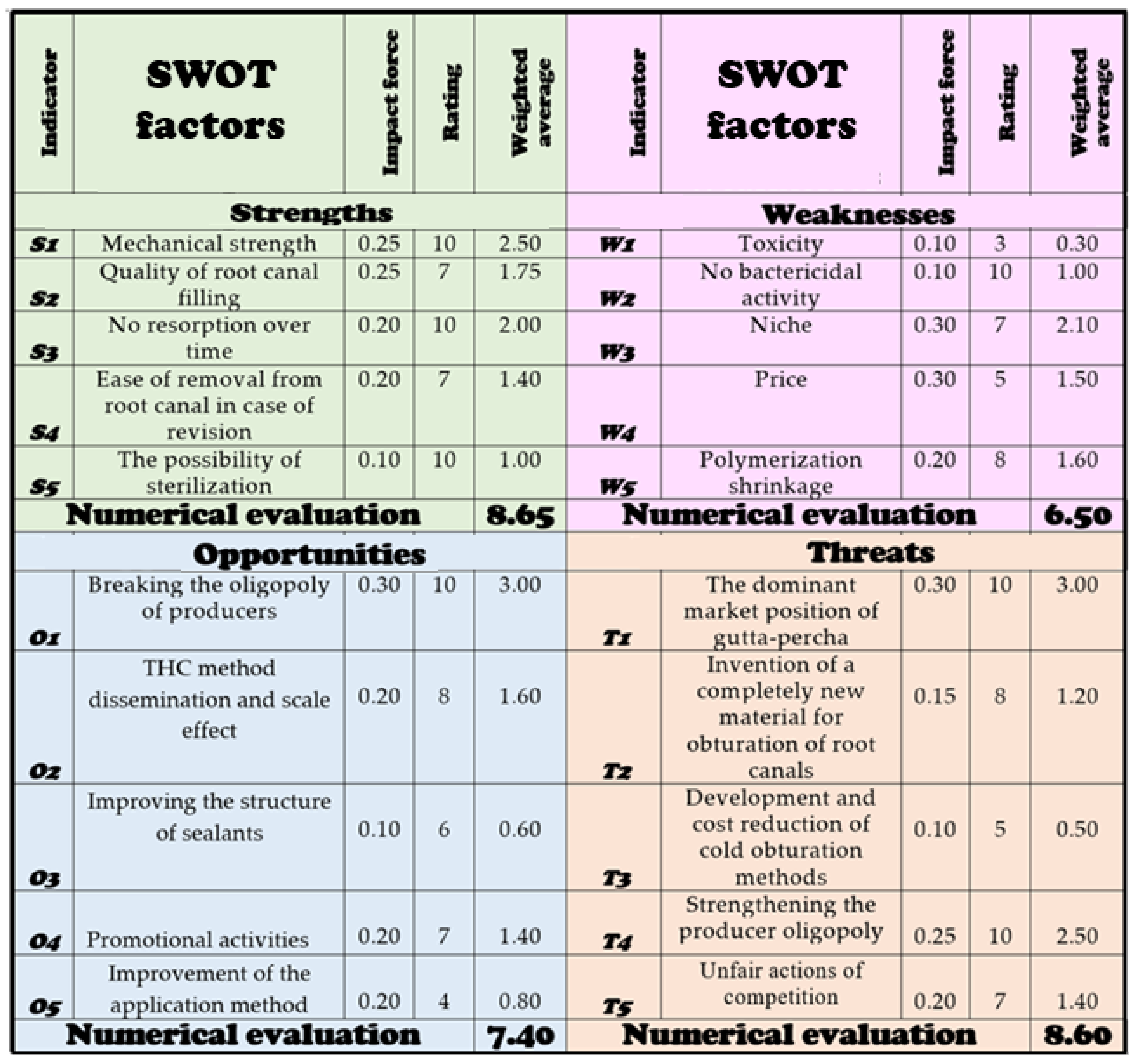
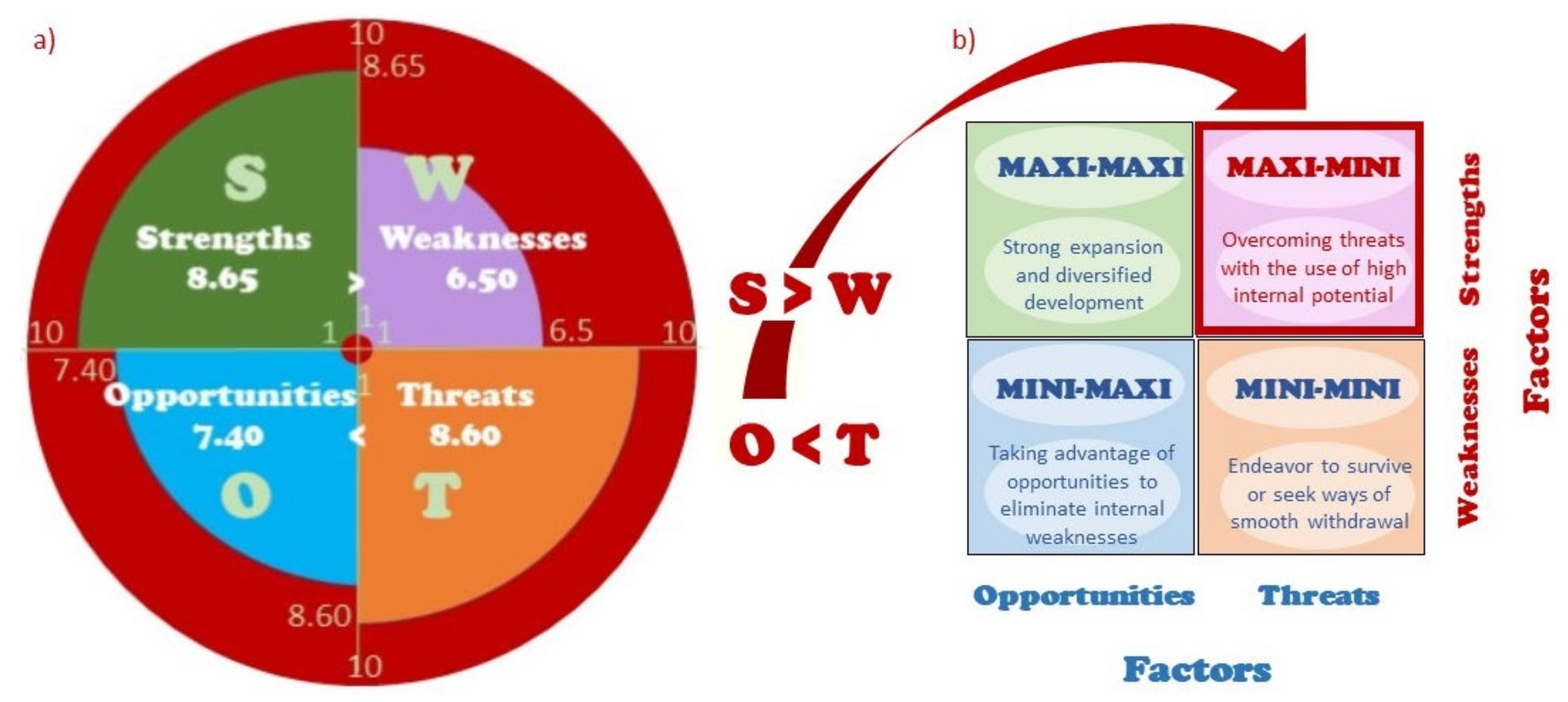
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dobrzańska, J.; Dobrzański, L.B.; Dobrzański, L.A.; Dobrzańska-Danikiewicz, A.D.; Gołombek, K. What Are the Chances of Resilon to Dominate the Market Filling Materials for Endodontics? Metals 2021, 11, 1744. https://doi.org/10.3390/met11111744
Dobrzańska J, Dobrzański LB, Dobrzański LA, Dobrzańska-Danikiewicz AD, Gołombek K. What Are the Chances of Resilon to Dominate the Market Filling Materials for Endodontics? Metals. 2021; 11(11):1744. https://doi.org/10.3390/met11111744
Chicago/Turabian StyleDobrzańska, Joanna, Lech B. Dobrzański, Leszek A. Dobrzański, Anna D. Dobrzańska-Danikiewicz, and Klaudiusz Gołombek. 2021. "What Are the Chances of Resilon to Dominate the Market Filling Materials for Endodontics?" Metals 11, no. 11: 1744. https://doi.org/10.3390/met11111744
APA StyleDobrzańska, J., Dobrzański, L. B., Dobrzański, L. A., Dobrzańska-Danikiewicz, A. D., & Gołombek, K. (2021). What Are the Chances of Resilon to Dominate the Market Filling Materials for Endodontics? Metals, 11(11), 1744. https://doi.org/10.3390/met11111744









